

Treatments are, of course, where the rubber meets the road. The Oct 2016 conference featured a different chemotherapy/autoimmune drug that appears to be helping, a drug that helped one ME/CFS/POTS patient to fully recover, how exercise tests may be uncovering drug combinations to prevent PEM, a supplement that worked too well and others.
(Please note that because I add comments the overviews may not match the presentations.)
Rituximab I – News From Norway
My how time flies. The data compilation from the big 152-person Rituximab trial is ending in just eight months in Oct, 2017. The participants are getting two infusions and a maintenance dose and three sub studies are underway. In October the code will be broken and Fluge and Mella (and a Norwegian filmmaker who will be filming them as they break the code) will know the results.
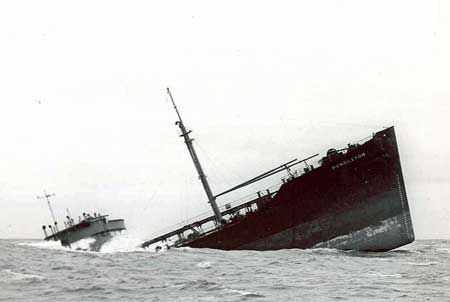
The trial is the culmination of 13 years of effort. It all started in 2004 when two alert oncologists found that the symptoms of one severely ill ME/CFS patient being treated for lymphoma improved dramatically. We now know that this probably happened many times to ME/CFS patient but it took these doctors to dig deeper. One wonders how patient zero is doing now
Fluge originally expected improvement would probably take about three months to show up, but for most it took six months. The ME/CFS patients are not acting like typical patients in other ways, either. About 30% experience temporary symptom worsening that can last for days, weeks or even months. That does not happen in lymphoma. Otherwise side effects, thankfully, have not proven to be a problem.
Fluge wasn’t able to say anything about the results of the big trial but in the 28-person trial about half the patients in that trial had what he called a major response to Rituximab. In the next 30-person trial 67% improved on Rituximab.
After finding that the effects waned over time, Fluge and Mella kept the ME/CFS patients on the drug and found that 2/3rd’s continued to have a sustained response.
It all started in 2004 with two alert doctors and one severely ill ME/CFS patient being treated for lymphoma. One wonders who that patient zero is and how he/she is doing.
Fluge also reported that he sees a high degree of autoimmunity (40%) in relatives of ME/CFS patients. An earlier study found a high degree of heritability in ME/CFS but no other studies that I’m aware of have been done. Isabel Barao of the Simmaron Research Institute is currently engaged in a genetic study looking at families with ME/CFS.
Rituximab II: On the Hunt for the ME/CFS Subset
Everyone knows a Rituximab subset – a subset of patients that respond well to the drug – exists. The big question is how big it is and how to identify it? Long before the big Norwegian Rituximab trial finishes up, researchers are trying to figure out how it biologically identifies the Rituximab responders.
It’s an important question. Because Rituximab is very expensive, identifying responders would help greatly in funding trials in the U.S. and Europe. (Perhaps even the super conservative, super cautious NIH would fund one if we could identify responders in advance. was easy to identify who would benefit).
The Canadian researcher David Patrick is not an immunologist, but proved to be – as he was in the San Francisco conference – an impressive speaker rattling off facts right and left. He listed about 30 collaborators including Drs. Fluge and Mella, Workwell Foundation researchers and Arizona State University researchers in his presentation.

Those stats looked good but Patrick said the test was not nearly ready for prime time. Much bigger studies are needed. One would think that if Patrick can get the money, he should be able to get the samples he needs when the Fluge/Mella’s study wraps up in October of this year.
If the signature is accurate – and it will surely be improved by future studies (If they occur) – it suggested that about 40% of Canadian ME/CFS patients would benefit from Rituximab.
(Patient reports suggest that another potential signature may be being tested by Dr. Peterson and others.)
Another Drug For ME/CFS Discovered?
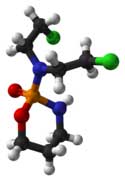
The big drug news at the Conference came with Fluge/Mella’s announcement that preliminary data suggests another chemotherapy and immune suppressing drug called cyclophosphamide works very well in some ME/CFS patients.
Noting that in low doses cyclophosphamide is an immune stimulant, Fluge said he got interested in the drug the same way he got interested in Rituximab: a cancer patient found that her ME/CFS symptoms improved on it. He also received emails from around the world from ME/CFS patients citing similar experiences
Af.ter a small pilot study of three patients showed a clear response, a phase II trial of 40 patients, 1/3rd of whom had tried Rituximab (and presumably failed on the drug?) in two hospitals is under way. Earlier Fluge reported that this trial is getting hospitals more interested in ME/CFS.
Cyclophosphamide (Cytoxan) is an older drug that was approved for use in the U.S. over 50 years ago. It’s inexpensive but Wikipedia reports that it has been largely replaced by less toxic drugs, and that its role now in the medical field is largely as a quick acting agent to bring down immune activity. WedMd states the drug is also used to treat lupus, rheumatoid arthritis and some kinds of kidney disease.
Wikipedia states that “regular and frequent laboratory evaluations are required to monitor kidney function, avoid drug-induced bladder complications and screen for bone marrow toxicity.” WebMD reports that nausea, vomiting, diarrhea, temporary hair loss (with different looking hair coming back) can occur and that many patients experience side effects.
Fluge did say that the first couple of months can be hard on ME/CFS patients – harder in fact than on cancer patients who are taking more of the drug (the same pattern was seen w/Rituximab). The benefits, on the other hand appear to be substantial. Plus, the drug is much cheaper and therefore much more readily available than Rituximab (i.e. many patients could probably pay for it themselves.
We do have to be cautious regarding drug warnings. Rituximab comes with some dire warnings as well but side effects don’t appear to have been a significant problem in ME/CFS yet.
That said, ultimately the biggest benefit from cyclophosphamide may simply be its indication that a broader acting immune drug can work in ME/CFS. While Rituximab is a monoclonal antibody specifically designed to knock out B-cells, cyclophosphamide effects many other cells. Unlike Rituximab, for instance, it effects mast cells. If it ends up working, Fluge said other similar immune effecting drugs will surely work.
Because it could open the door to many more drugs than Rituximab, cyclophosphamide has the potential of being a bigger game-changer. In any event these two drugs (plus Ampligen) do suggest that immune manipulation provides fertile ground for future ME/CFS treatments.
Not all the chemotherapy drugs Fluge has tried have produced positive results. Methotrexate, another chemotherapy and autoimmune drug, produced what Fluge, who has probably seen it all over the years, called “a horrible reaction” in ME/CFS patients. Surely every experiment provides clues as to which parts of the immune system are affected in ME/CFS and how to treat it.
Again it bears noting how active and flexible the Norway group has been. A couple of weeks ago, Dr. Koroshetz of the NINDS sounded like it would be years before the cautious, conservative NIH would even consider funding an ME/CFS trial. Koroshetz is apparently looking for a fait accompli – a drug whose success is near certain. Failure at the NIH apparently comes at high costs, and Koroshetz referred to some stroke trials that devastated the field in the 1990’s. He said the field had still not recovered.
Koroshetz and Collins appear to be hoping that the results of the big intramural study that’s now underway will give them a solid basis for further study and ultimately a drug trial. It’s hard to imagine that study with its immune, brain imagine, exercise, metabolic testing, etc. not giving the NIH a foundation for further work.
An (Old) New Drug for ME/CFS and POTS?-Bateman-Horne Center
Desmopressin I
Complete Treatment using desmopressin of suspected central diabetes insipidus, POTS and/or ME/CFS following a series of adverse immune events
A poster from the Bateman-Horne Center highlighted the complete recovery of a person with severe ME/CFS and POTS – something that doesn’t happen very often – using desmopressin – a drug that’s not used all that much. Desmopressin is used to treat diabetes insipidus (DI) – a condition that some think may be more common than is currently believed in chronic fatigue syndrome.
Diabetes insipidus is characterized by excessive thirst and the production of large amounts of (dilute) urine. It’s entirely different from and should not be confused with the diabetes we’re all aware of. Two different kinds of diabetes insipidus occur; a neurological form that produces a deficiency of arginine vasopressin (AVP), also called antidiuretic hormone (AD), and kidney associated DI that occurs when the kidneys fail to respond to ADH.
Dr. Bateman started her on a trial of oral desmopressin (0.1-0.2 mg twice a day), put her on a pacing regimen and worked to manage her sleep, pain and anxiety. The patient responded immediately to the desmopressin. Within a year of starting it she was almost completely healthy. Over the next year she was able to taper off the drug and remained healthy. She has no symptoms of POTS or ME/CFS.
It’s important to note that DI does not cause the kind of fatigue and post-exertional malaise associated with ME/CFS; i.e. while DI may have been present it was not the cause of the ME/CFS patient’s symptoms. Dr. Bateman was clued into the DI diagnosis by the patient’s high level of thirst and urination.
Dr. Bateman’s conclusion (the patient had hypothalamic dysfunction) indicated desmopressin may have had other effects as well. (Dr. Bateman believes desmopressin’s blood volume enhancing properties were key.)
A 1999 Irish study found that desmopressin and corticotropin-releasing hormone (CRH) significantly increased cortisol output in ME/CFS patients relative to the healthy controls. I was just informed that desmopressin is the precursor for CRH and ACTH in the HPA axis. It’s perhaps now surprise then the Irish study concluded that desmopressin was capable of “normalizing the pituitary-adrenal response to corticotropin releasing hormone” in ME/CFS.
One of the earliest chronic fatigue syndrome studies – way back in 1991 – suggested that problems with a CRH deficiency or “some other central stimulus” was present in ME/CFS. A 2001 study also found evidence of reduced CRH secretion.
Eighteen years later Miwa found that giving desmopressin resulted in reduced orthostatic intolerance, reduced heart rates and improved functionality in five of the ten ME/CFS patients given the drug.
Dr. Bateman believes that catching this patient early may have been crucial, but suggested that long term use of desmopressin could be helpful for a subset of ME/CFS/POTS patients.
Desmopressin #2
Treatment of Postural Orthostatic Tachycardia Syndrome and Management of Myaglic Enecephalomyelitis/Chronic Fatigue Syndrome following West Nile Virus Infection
The Bateman Horne Center reported another successful use of desmopressin and the first published account of a person contracting ME/CFS after being infected with West Nile Virus. (The Simmaron Research Foundation is contributing to the first study to examine the incidence of insect-borne vectors including WNV in ME/CFS.)
This person contracted ME/CFS/FM/POTS after being infected with West Nile Virus. He used compression stockings, increased fluid intake, desmopressin, midodrine, fludrocortisone and propanolol.
The treatments significantly diminished this person’s POTS symptoms, his problems with widespread pain disappeared completely and his functioning improved. His long-lasting post-exertional malaise occurred less frequently and was less severe when it occurred.
Compression stockings and desmopressin appeared to contribute most to the patient’s progress. The authors noted that West Nile Virus is now the most common insect-borne infection in the U.S. They also highlighted the need to evaluate all ME/CFS patients for this infection.
If Not Opioids What Then? Jarred Younger
Spelling out the perils of chronic opioid use, Younger, a pain researcher, showed how more opioids are predictably needed over time to relieve pain. One study found that one year later people using opioids were worse off than those who were not using them. There’s no evidence that opioids are helpful after 3 months.
In fact, Younger asserted that most physicians are not capable of using opioids properly in people with chronic pain. New opioid drugs which do not produce side efforts or addiction are in human and/or animal trials now. Anyone who can find a safe and effective pain-killer will get a huge, huge commercial and scientific payoff and a huge number of people are working on the problem.
If you’ve been on opioids for a long time Younger suggested tapering off of them slowly to see if your pain levels drop substantially. (Paradoxically, chronic opioid us can cause increased pain sensitivity in some people.) If you’re on low dose opioids and they’re still effective after a year, by all means stay on them.
In general, though, he suggested other options and listed 20 of them ranging from spinal cord stimulators to ketamine. (He’s interested in low dose ketamine to reduce inflammation.) Cucurmin tops off Younger’s list of non-drug alternatives for lowering inflammation in the brain, and he noted that cannabis rated much, much better in several National Pain Report Surveys for FM than the FDA approved drugs.
Kratom – from the Mitragyna speciosa tree – has both opioid and stimulant properties. Where its grown the leaves are chewed much like cocoa leaves to relieve musculoskeletal pain, increase energy, appetite, and sexual desire but no studies have been done and Younger worries about the potential for addiction.
If you’re not tracking your symptoms Younger highly recommends doing that every day to find triggers; he suggested that you might be surprised at what you find. (Any suggestions on good symptom-tracking apps?)
Younger noted that the part of the brain that is most critical to pain production is the amygdala – which brings us to a poster.
Amygdala Retraining Techniques for the Treatment of Fibromyalgia: A Randomized Controlled Trial
The third generation of the amygdala retraining technique (ART) invented by former ME/CFS patient Ashok Gupta got a go over by a Spanish research group. Forty-four fibromyalgia patients were assigned to either a relaxation arm or an ART arm. Fibromyalgia Impact, Global Clinical Impression, Five Factors Mindfulness, Hospital Anxiety Depression Scale and two other questionnaires were given.
After six months Fibromyalgia Impact, Depression and avoidance was significantly reduced in the ART group.
Avoiding the Crash
Designing Immunotherapies to Normalize Recovery From Exercise in ME/CFS. Gordon Broderick
Gordon Broderick is going about finding a treatment for ME/CFS in a precise and novel way. First he’s measuring cytokine responses no less than nine times before, during and after exercise. As he watches the immune system implode under the strain, he’s coming up with possible ways to keep it from running off the rails and sparking an inflammatory response that causes the dreaded and disabling post-exertional malaise.
Gordon Broderick is using exercise tests to determine how to stop post-exercise malaise from occurring in ME/CFS
With just nine people assessed thus far the results are still decidedly preliminary, but Broderick’s modeling analyses suggest that first blocking IL-2 and then subsequently boosting IL-17 could turn off the pro-inflammatory cascade Broderick’s finding during exercise and yes, possibly – allow people with ME/CFS to exercise symptom-free.
Needless to say, nobody else is modeling exactly what’s happening during exercise as the Gordon Broderick/Nancy Klimas team at the Institute for Neuro-Immune studies at Nova Southeastern University are doing. This is the same kind of modeling Broderick has been doing with success in GWS. Let’s hope he can get more people into the study and validate his preliminary results.
After decades of using pharmaceutical drugs in his practice, Dr. Peterson said drug trials are needed in ME/CFS but must be large and well constructed. If studies can verify high cytokine levels in ME/CFS patients (as Broderick appears to be doing) no less than 17 cytokine blockers are now on the market. Peterson called those drugs a real opportunity for some.
A Supplement That Worked Too Well?
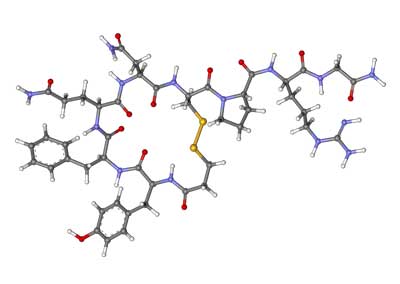
In one of the odder findings -or rather interpretations of findings ever seen in the ME/CFS literature – Shungu found that the treatment he was assessing – N-Acetyl cysteine or NAC – worked too well. After finding for the third time low levels of glutathione, the main antioxidant in the body, in the brains of ME/CFS patients, Shungu tried four weeks of its precursor, NAC (1800 mgs) in 12 ME/CFS patients and 14 healthy controls.
The supplement appeared to work; while MRS spectroscopy indicated brain glutathione levels rose in the ME/CFS patients, levels of free radicals called isoprostanes fell. That suggested that a) NAC penetrates the blood/brain barrier and b) it had reduced the level of inflammation there.
The only jarring note to the study was the overly strong clinical response! The ME/CFS patients symptoms went down so much that Shungu believed a strong placebo response must have occurred and that larger studies are needed to get the full story on NAC. While NAC surely doesn’t have the clinical effectiveness the study seemed to indicate it does, the small study does suggest the supplement may be helpful at increasing antioxidant status in the brain and possibly in reducing neuroinflammation.
The Low Dose Naltrexone Watch
Bateman Likes Low Dose Naltrexone (LDN)
Dr. Bateman is pretty middle-of-the-road in her treatment approach. She’s not out on the skinny branches exploring fringe treatments so when she touts low dose naltrexone as an often good (and inexpensive) treatment, it’s a pretty good idea to assume that it works pretty well. Side effects, in general, she said, are low and those that occur mostly involve sleep.
Younger was at something of a loss to describe optimal dosing regimens saying that dosing was all over the map with many patients tolerating 4.5mgs fine at first. He emphasized, though, that it takes 2 months to tell if the drug is working or not. One month is not enough; some patients respond after that – so be sure to stay on the drug for 8-10 weeks.
Younger also recently said that it appears the LDN may be helpful for depression but studies are needed.
Immunomodulatory Effects of LDN in ME/CFS
Dr Vera at Dr. Klimas’s Institute for Neuroimmune Medicine at Nova Southeastern University in Ft. Lauderdale took a subject that has been on many people’s minds. LDN has been shown to be helpful in fibromyalgia but how effective is it in chronic fatigue syndrome (ME/CFS)?
A retrospective chart review (n=845!) assessed its effects on a number of immune parameters (NK cell number, cytotoxic activity, T-cell activation and cytokines), and found no statistically significant differences in cytokine levels but non-statistically significant reductions in several pro-inflammatory cytokines (TNFa, TNFb, IL1a, IL17). No effect was found on NK cells. Vera noted that because LDN was given with other medications, it was impossible to accurately parse out its effects, and suggested that a study be done. (Dr. Younger is doing that study this year).
An Ampligen Subset Found?
Hemispherx Biopharma has talked for years about finding a biological marker that identifies which chronic fatigue syndrome (ME/CFS) patients Ampligen works on. Instead they came up with something similar – a demographic marker. When the drug manufacturer divided the participants in its studies into longer and shorter duration (2-8 years) patients, it found that shorter duration patients did much better in the exercise test.
Over 50% of Ampligen treated patients vs. 18% of placebo patients demonstrated at least 25% improvement in placebo-adjusted exercise tolerance. The fly in the ointment – there always seems to be a fly in the ointment for Ampligen and Hemispherx Biopharma (HB) – was the weird duration range; neither very short duration patients (<2 yrs) or longer duration patients (>8 yrs) had a statistically significant response to exercise; i.e. the drug didn’t work in them. Explaining that finding will not be easy.
Ampligen got approval in Argentina and its shipping product to Europe for use in an early access program. It also recently raised $1 million dollars in a stock offering but HB also ended its compassionate care program leaving ME/CFS patients without access to the drug and greatly increased the price of the drug. It’s a strange way for a company that has received such support from the ME/CFS community to act. Please sign the petition to have HB put patients first.
Increasing Range of Motion in Adolescents – Does It Work?
Could something so simple as physical therapy help ME/CFS? Dr. Rowe’s data suggests that if it’s done right it can. Rowe, like Broderick, is looking at ME/CFS in a unique way and his hypothesis – that the tendons in adolescent ME/CFS patients are not elongating properly – is a testament to Rowe’s powers of observation.
The problems Rowe has found with tendon elongation in adolescents could help explain why movement, particularly exercise, can be so painful. If the tendons won’t elongate properly as we move our limbs they could be sparking an immune response which translates into pain and fatigue.
But what if therapies were introduced to assist with tendon elongation? Rowe has said that these therapies are the most popular he does with his patients. It didn’t appear to be a slam dunk, but Rowe found that doing those physical therapies (along with other standard treatments) did return adolescents’ range of motion to normal in about seven months and improved functionality and activity levels.
When asked whether increasing their range of motion allowed the adolescents to exercise, Rowe said that increased range of motion did appear to be a bridge to an increased ability to exercise. A further study is needed to assess that.
Several different types of physical activity can be used to increase range of motion. Yoga is one with the proviso that you have to be careful not to overstretch. Tai chi is another.








Cort, this informative
article is fantastic and
encouraging. As always, as a writer of training manuals for big pharma, your writing is second to none and helps so many
of us. Could you comment
about the crossover of
ME/CFS and
fibromyalgia in these
treatments since both
seem to be neuro-immune
diseases?
I really wish fibromyalgia had conferences like these.
Some of these treatments are cutting-edge and I don’t know what their applicability to FM will be. I would think NAC, Rowes Range of Motion therapies and desmopressin – because it boosts HPA axis activity – might apply for some people.
Of course LDN does – people with ME/CFS learned about that from FM.
The really interesting question is whether things like Rituximab and cyclophosphamide do…I have no idea but given the closeness of the two disorders (Dr. Bateman thinks they are all on the same spectrum) it would be fascinating to find out.
We know that antivirals do work for some ME/CFS patients and then here comes Dr. Pridgen developing an antiviral protocol for FM..and now we’re getting some immune studies from FM and possibly an immune blood test.
We really, really need more joint ME/CFS and FM studies
What is the immune blood test called please. And what antivirals for ME so i can ask my doctor for them.
Thank you
Thanks for sharing this knowledge. Have you come across any medicines/treatments and information for Fibromyalgia spasms? Brought on by weather change..cold mostly or lack of proper sleep causes gut and back spasms. I suspect it’s some sympathetic over activity. ..but this part of Fibro is very painful…like wearing a straightjacket. What causes this?
I use an infrared heating pad for spasms. Infrared penetrates into the muscles so it is much better than a regular heating pad. I have Percocet on hand for the really severe spasms that just won’t quit. I rarely take Percocet because of the constipation side effects so it continues to work well for me. Tramadol and Norco aren’t strong enough. Also stay away from sugar, supplement with Magnesium, and try to avoid the cold. Nothing feels better than the sun on my muscles and temperatures 80 degrees and over.
Thanks Bill. I have been using castor oil packs and heating pad…once in a.m. and once in p.m. This seems to help somewhat. I also drink chamomile and some other herbs…and I take magnesium. Recently GP gave me Buscopan to try. I just started. I will see how this goes. Elinatingbsugarand probably wheat would likely help me more. I will look into infrared heating pad. Thanks!
When heat doesn’t do it for my muscle spasms, I use Baclofen, 10mg, and it usually works.
I was supposed to be a participant in an Ampligen trial-12 patients were to start soon.
The process is very slow getting an ok from Health Canada then Bam-the price jumps 167% which knocks out the majority of us. Now everything is on hold.
What do they want us to do? Take out another mortgage?? Go bankrupt??
I don’t know but this patient community has advocated for them for years. They’ve looked past all the weirdness at the company in order to help get this drug approved and now HB does this. I don’t understand it. I don’t see how hitting a rather small number patients in the pocketbook really hard is going to help them. I just don’t understand it.
Cort, do you have any contact at HEB that can explain the sudden change in price and basically cutting off users in the US? I remember Dr. Peterson referencing this coming change in the trial a long time ago. I wonder if it has something to do with the pricing they were able to set in Europe and will be setting in Argentina? Are they expecting significant sales from these areas that required a more solid price? HEB is teetering pretty bad right now with the stock at an all time low, so changing their trial to make it less accessible doesn’t make a lot of sense.
I’m going to try and find out. Hemispherx also let go their long time liaison to the ME/CFS community at the same time. I would think they would be doing better but their stock offering sent the price of their stock down. I don’t know if that’s normal or not.
Hi Katie,
Do you mind elaborating on this 12 person Canadian Ampligen trial? I’m also from Canada and have been in discussions with Health Canada regarding their Special Access Program.
Was your group approved via special access? I’m curious regarding the details of this trial and how it came to be. Thank you in advance 🙂
p.s. I’m glad to see a trend away from opioids. I was one of the patients that developed tolerance and up and up the opioids went. When I got off them I did have a fair amount less pain, certainly much less brain fog. I usually manage well with Nabilone (cannabinoid) and the rare morphine 5 mg.
I think we’ll surely see more alternatives for pain relief in the future.
Normally I’m against killing but this article slahugtered my ignorance.
My rheumatologist had me on a fairly stable regimen that helped, skelaxin, mobic, gabapentin, adderall (helped immensely with ADHD/fibro fog) and 20 mg of OxyContin 2/day with 15 mg oxycodone for breakthrough pain. My husband was transferred to Atlanta 9 months ago, so there I was, starting ALL over. It’s been a nightmare. I went to an Emory pain management doctor, who immediately began lowering my breakthroughs, which is fine, since every doctor I saw treated me like an addict. Last time I saw this doctor, I asked what the ‘game plan’ would be once the opioids were gone and she plainly said there was no ‘game plan’: “Emory’s policy is to only treat pain with muscle relaxants and NSAIDS.” She then handed me a paper with other pain docs if I wasn’t happy with Emory. I said what about LDN, cannabis oil, etc. “Absolutely not.” From what I understand, Georgia allows Anna is oil for only a handful of conditions, one being mitochondrial diseases. I know inflammatory OA is an MD, and possibly FM. Her attitude devastated me. And I know of nowhere else to turn since moving here has been traumatic in itself. I am pretty much home bound. Can anyone familiar with Georgia suggest any doctor or clinic near Norcross? Thank you ?
Interestingly enough, once I began twice daily Valcyte 450mg, my low grade fever of 20 years abated. Consequently, I feel much better and seem to crash less. Lately, I’ve been able to go to yoga classes twice weekly and trail walk with my dogs. I wonder what’s up with the Valcyte research as my situation is purely anecdotal.
Joseph Montoya at Stanford did some research into it but it seems to have stalled. It’s a pity because his results were promising.
Cort,
The stuff about cytokine blockers is really interesting.
Has it been tried in other illnesses that you know of
Yes, Corinne (she’s been blogging on her visits to Dr. Peterson) is doing much better on Remicade…
These immune specific drugs appear to be the wave of the future.
Just had a quick browse, this article caught my eye:
mentions B cells & Rituximab….
http://www.jrheum.org/content/41/5/825.full
What is her blog info please
Very interesting, thanks Cort. I wonder if anyone has or will try drugs like dupilumab, which target the Th2 immune response and are quite safe and well tolerated? These would see like an option well worth exploring.
I think these are the kinds of drugs that will at some point work their way into ME/CFS and FM. Basically we need studies which suggest they may work. Hopefully the intramural study will be of help here.
I know of someone who has benefited a great deal from Remicade. She is certainly not well – but she is much better.
I would like to add a strong note of caution to the use of desmopressin. This drug can effectively raise blood volume and constrict blood vessels, which can be helpful in managing orthostatic intolerance syndromes. But desmopressin must be monitored carefully by a skilled physician, with lab tests, because inappropriate or poor management can result in severe medical consequences, including life-threatening hyponatremia, fluid overload and hypertension.
In addition, while intriguing, Cort’s assessment of the connection to CRH may be overly optimistic. Vasopressin, also known as ADH and AVP, and marketed as the drug Desmopressin, is produced in the hypothalamus, but stored in and released from the posterior pituitary. CRH is also made in the hypothalamus and secreted in response to stress. CRH stimulates the release of ACTH from the anterior pituitary, which in turn leads to release of cortisol from the adrenal gland. It is true that vasopressin and CRH are released in tandem from the hypothalamus, but each goes on to play a different role in the stress response system.
It is my opinion that the main benefit of Desmopression is restoration of more normal circulatory perfusion (delivery of oxygenated blood to all tissues). I believe our first case had an immediate and complete recovery response because we happened to make an early diagnosis and intervene promptly to support the core pathology. In MECFS patients who have been ill longer, the impact of desmopression is much less predictable. While it may provide some benefit to those with orthostatic intolerance, the impact definitely less dramatic. Most of all, it should be managed carefully to do no harm.
Most intriguing to me (and ties in to Cort’s hypothesis) is the the idea that if both vasopressin and CRH were underproduced, or the release inhibited or dysregulated, an illness that looks very much like MECFS might be the result.
Thanks Dr. Bateman 🙂
Regarding Dr. Rowe’s data on PT for tendon elongation in adolescents – any info on whether that would also apply to adults? Or is it strictly a young-growing-body issue?
My own experience…range of motion PT such as myofascial release caused PEM and worsening of symptoms.
I tried LDN for over 6mos and could never teach 4.5mg but remained at 3.5. It did nothing for my inflammation, pain or any of my symptoms.
Methotrexate was a disaster. I was supposed to work up to 20mg but at only 7mg, I experienced steadily climbing liver enzymes, showing extreme sensitivity to its toxicity, and was told by my neurologist that it wasn’t even worth attempting to achieve the goal of 20.