

What can you expect if you have fibromyalgia? Do most people tend to get better or worse? Do people with FM ever recover and, if so, how many people do?
Several studies have examined the progression of fibromyalgia over time. Bearing in mind two things: (a) studies report tendencies which may or may not apply to any one individual, and (b) that studies may reflect the practices of the doctors in the areas the participants in the study derived from, and (c) the studies probably use doctors which do not incorporate many alternative methods into their practices; i,e, your results may vary. With that let’s look at what the studies suggest about the average person’s future with fibromyalgia
The most recent study – which took place in the U.S. – followed 76 FM patients from 20 sites in five regions (West, Midwest, South, Northeast) over two years.
The Study
Fibromyalgia Outcomes Over Time: Results from a Prospective Observational Study in the United States. Caroline P. Schaefer,1 Edgar H. Adams,1 Margarita Udall,2 Elizabeth T. Masters,2 Rachael M. Mann,3 Shoshana R. Daniel,4 Heather J. McElroy,5 Joseph C. Cappelleri,6 Andrew G. Clair,2 Markay Hopps,2,* Roland Staud,7 Philip Mease,8 and Stuart L. Silverman9 Open Rheumatol J. 2016; 10: 109–121.
The participants answered a variety of questionnaires (Brief Pain Inventory-Short Form (BPI-SF), modified (self-report) American College of Rheumatology (ACR 2010) Criteria, Fibromyalgia Impact Questionnaire-revised (FIQ-R), Medical Outcomes Study Sleep Scale (MOS-SS), 12-Item Short-Form Health Survey, version 2 (SF-12), and Work Productivity and Activity Impairment (WPAI) Questionnaire).
The researchers also learned how many doctor, hospitalizations and emergency room visits were made and what prescription medications, physical treatments, nonprescription medications, and herbs, vitamins, or other pain supplements were taken over the last three months.
Results
The fact that over 80% of the patients were on some sort of prescription pain-killer both at the beginning of the study and at the end spoke to the high pain levels people with FM typically experienced.
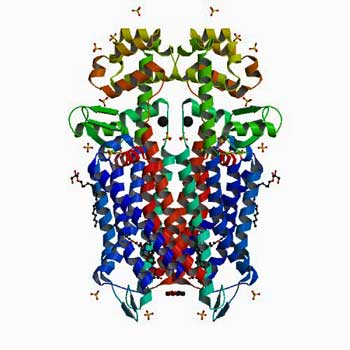
The people with FM in this study used more opioid drugs than any other kind of drug. (This is the mu-opioid receptor that opioid drugs lock onto.)
Opioids Stand Out – Despite the fact that three drugs have been FDA-approved for FM – none of which are opioids – opioid pain-killing drugs were easily the most used pharmaceutical drug with about 30% of the FM patients both at baseline and two years later using them. A weaker opioid, tramadol, is often suggested for FM but more FM patients were on stronger opioids. Not only were more patients on strong opioids at baseline, the percentage of patients using strong opioid pain-killers actually increased over time. This, of course, indicates the important role these drugs play in pain management in FM – and speaks to the concerns several ME/CFS/FM doctors have that increasing restrictions on these drugs will leave some without a important means of help.
It also presents a worry as the chronic use of opioid drugs can actually increase pain sensitivity in some individuals. Paradoxically, some people with FM patients feel less pain after coming off opioid pain-killers.
- Check out New Opioid Drugs Under Development – Relief at Last? Next Generation of Opioid Drugs Under Development
NSAIDS were the next most commonly used drug and muscle relaxants were fourth. The fact that the use of both these drugs declined significantly over the two year span of the study suggested that many found them not particularly helpful.
FDA Approved Drugs Not So Popular – Antidepressants of the SSRI class (Citalopram (Celexa, Escitalopram (Lexapro), Fluoxetine (Prozac), Paroxetine (Paxil, Pexeva), Sertraline (Zoloft) were the third most used drugs, tramadol was the fourth and SNRI’s (Milnacipran (Savella), Duloexetine (Cymbalta) Venlafaxine (Effexor) ) were the fifth most used drugs. Anti-epileptics (presumably Pregabalin (Lyrica), Clonazepam (Klonopin) and Gabapentin (Neurontin) were the sixth most used drug.) Only about 15% of the FM patients used anti-epileptics.
A drop in the use of herb, vitamins and other supplements from about thirty to about twenty percent of patients suggested that about a third of those trying them did not find them helpful either. On other hand about 2/3rds of FM patients using continued using them.
Meanwhile more FM patients (30-38%) began receiving physical therapy over time.
Little Progress in Twenty Years
The fact that their employment status, household income, BMI, and number of disease comorbidities did not change indicated little movement was made in these issues.
There was some good news as well. In general FM patients reported statistically significant improvements in their symptoms (modified ACR 2010 Criteria) and how much pain interfered with their functioning (BPI-SF Pain Interference Index) and in their sleep (MOS-SS Overall Sleep Problems) were observed.
While improvements in pain were made, they were, however, relatively small with only about 15% of patients reported a more than 2 point improvement in pain. Plus even after the improvement pain levels were still very high and another pain indice did not show any improvement. One could come to the conclusion that many FM patients simply became better at functioning despite their pain. Most patients, however, remained quite functionally impaired.
This studies strength was its geographic spread; by following patients from 20 different clinics across five different regions it was able to get a good snapshot of general FM practice. It’s weakness was its relatively small sample size and relatively short duration. It was also impossible to tell which clinics were involved from the study.
Other studies, however, have come to similar conclusions. A very large (n=1555) 2011 5-10 year observational study found that while about 25% of FM patients did experience moderate or substantial improvement in their pain about 35% got worse. In general the levels of symptoms remained high.
Another study suggested that things haven’t changed much in the last twenty years. Despite the advent of three FDA approved drugs for FM and presumably much improved doctor knowledge, a large 1997 7-10 year study came to a disturbingly similar conclusion: the degree of pain, fatigue, sleep problems, depression etc. were all essentially unchanged over time.
It should be noted that several studies show that remissions from fibromyalgia can occur. Full recovery is rare but you can find FM/ME/CFS Recovery Stories on Health Rising and other sites.
Because the studies examined whether or not patients met the criteria for FM, not whether they recovered or not, recovery rates from FM were not reported. However, the small percentage of patients reporting substantial improvements from pain suggests that recoveries are rare
There are several proviso’s to these studies. It’s not clear if the practitioners in any of these studies were using low dose naltrexone LDN or tracking medical marijuana: two alternative treatments probably not available in many doctor’s practices. Given the low number of FM specialists available we can probably conclude that they were not included in the surveys either. It’s possible that FM patients seeing practitioners who use a multidimensional approach that incorporates alternative health practices into their treatment regimens do better as well. Studies to determine whether FM specialists or alternative health MD’s are more effecting at treating FM are vitally needed.
In general, though, these studies suggest that the most FM patients seeing general practitioners or rheumatologists can hope for are modest improvement in pain and sleep. Much, obviously remains to be done.
Some treatments may be on the way. An improved form of Lyrica is in Phase III trials and Dr. Pridgen is raising money to fund his phase III antiviral trial.
High Burden of Illness – Low Funding Continues to Plague Fibromyalgia
Recent studies indicate that fibromyalgia places a high burden of illness both on the patient and their family, and on society. At about 50 cents a year, funding per fibromyalgia patient is, however, amongst the lowest at the NIH. Despite FM’s high prevalence and the high illness burden it imposes on patients and on society the biggest research funder in the world – the National Institutes of Health (NIH) is still clearly disinclined to study it.
Without more study, however, it’s unclear how FM patient’s lives are going to improve. It’s possible that better treatments could come from advances in our understanding of pain in general but that’s uncertain. Determining exactly how the pain and other symptoms in FM are generated and creating treatments to tackle them is the best solution.
That’s probably not going to happen for a long time with the funding FM currently gets. The FM community has the numbers; if it can translate those numbers into effective advocacy it can go far. Given FM’s past history at the NIH (its funding has actually dropped substantially), unfortunately, there’s no reason to expect anything to change absent a strong push from the patient community.








I am living in youngstown,Ohio ad have medicaid insurance. Practicly nobody do anything for me locally, nt to mention ths insurance pay nobdy specialis. Now since they restricting the pin me.I am much worse and heard o the facebook from others ith the same sickess, all of us feel abandoned, and left alone, with our pain, tragedy. I tried pain management it did nothing good, at all!!!
I believe fibromyalgia is a progressive disease and is chronic but can be successfully treated with the guaifenesin protocol. I have been doing it for the past nine years and live a full life, need no other medications besides occasional Tylenol. I sleep at night and wake refreshed. Anyone can learn to do it. It is helpful to be mapped but not essential.
Hello, at first when I first got sick I saw Dr. St Amand and I was I think either on Tramadol or Fentanyl some of it is a blurr due to the chronic pain, my main symptom. When I asked if I could start the protocol, they told me no, because I could not be on any pain medication, I remember feeling hopeless, because a friend who had Fibro and CFS is living a full life. So 18 years have gone by and now I see that a person might be able to use Ultram during the protocol. Is that true? Can a person use Oxycodone during the protocol? I read it is 2 months for every year, damn that would be 4 months, I am afraid of the process of getting worst, that scares me. How long does that process last, the getting worst part? Thank you
Jody, I am doing the G protocol too and getting back to fuller life. I was dx’d 10 mos ago after symptoms for 3 months, and have radically chg’d my diet and some other habits. Anyone who can get it dx’d early and is motivated, intelligent and determined to do the lifestyle changes can do it. In our society, most people look for a quick fix that doesn’t have to chg. our habits, diet etc, also often they can’t find an MD who has positive experience with FM/CFS, and the get lost to Big Pharma and opiates which really bring them down, bringing job and insurance loss, causing family breakdown and disability and depression. I too use only oc. tylenol and sleep well w/o sleep meds. No Fibro fog either. I am 74 yo retired FNP, Living in CA. Linda V.
I have been using “Mucinex” for over 6 yrs. It helps some with the pain. I read more recent research a few yrs ago that says avoiding all salicylates is NOT necessary, which makes it easier to do. I would add the extra-strength Mucinex every AM and PM even if I were on other drugs (which I can’t tolerate, except Cymbalta), Cindy. I don’t see how it can hurt. Some of the positive side effects are: less plaque on teeth plus stronger hair and nails! I think it may aggravate the dry mouth caused by the Cymbalta, but that’s easy to handle. I just have a water bottle with me at all times, and even sip it during the night. I heard about Dr. St. Amand’s protocol from a nurse and read the book right away. She was in more pain than I am, and said she had to set her alarm early every AM before starting on the “Mucinex” so she could get her crying over before going to work! I did notice, when moving/packing if I was out of Mucinex I was in more pain. It definitely makes a difference with no serious side effects. It’s also nice when I have a cold, for the congestion! (I can’t tolerate any other cold meds~they make my blood pressure and pulse race which makes me anxious.)
I have heard this before. But there are different degrees of this illness, and most often people who manage with cough medicine have an extremely mild case of Fibromyalgia.
yes this fibromyalgia is getting better.if you want more informations write to me
To Whom It May Concern:
Since seeing a holistic healthcare provider in Gainesville, FL approximately six years ago all my CFS symptoms have improved DRASTICALLY.
Sincerely,
Bob Cassels
Good to hear Bob! Can you say what worked for you?
I get some relief from alternative treatments but can not afford them on the $1,100.00 diability i get a month.
Darn…That’s rough….Nancy can you say what helped you?
How long did it take you to receive disability?
Of course there were changes from before Fibro to after Fibo.
But these questions on this survey pertain to the time period after getting Fibro and forward, correct, to present day?
Yes….From the time you got fibromyalgia to the present day. Thanks for clarifying that.
I see individuals with fibromyalgia every day of my working life. In my experience recovery is not unusual.
Just two days ago I received a phone call from a 38 year old man to advise me that he had recovered completely.
Six months ago he was housebound on moderately high levels of opioids. He told me that the single biggest improvement occurred when he came off the opioids and subsequently he instituted a range of strategies each one incrementally improving his outcome. He advised me that he is now pain free and back at work.
He adopts a range of healthy lifestyle practices including meditation and specific dietary restrictions on a daily basis. He is on no medications
Here is a link to some inspiring stories of recovery
http://tinyurl.com/z9r9ll2
Thanks. One of my questions is whether people who see the right doctors – FM specialists or the right kind of alternative health doctors – doctors who are probably not captured by the studies – do better. It’s good to hear that maybe they do.
I see twelve stories on that website 🙂
We should also keep in mind that some people who come off of opioid drugs do much better (!) – apparently because opioid drugs over time can INCREASE pain sensitivity.
Unfortunately, it is unlikely that outcome data will be collected from individual health practitioners. This is the only way this question can be answered. There is also so much variation in the diagnostic criteria used between practitioner groups. Even within rheumatology practitioners have widely varying diagnostic criteria.
I’m glad to see a study like this, for what it reveals. So thank you for the write up Cort!
But it seems important to clearly indicate that this study is about the general course of FM…under allopathic treatment, specifically.
We are living in a medical world that is so starkly divided into traditional and alternative medicine. So it seems important to identify which camp of thought a study like this is coming from, primarily so that people who are unaware that there are an entirely different set of options available, do not lose hope immediately.
Many people with all sorts of chronic illnesses find little or no help through traditional routes (i.e. medications) – this unfortunately appears to be true for so many conditions – but do end up finding considerably more success through “alternative” routes (too numerous to name).
I know you are aware of this, Cort (so I don’t mean to imply you aren’t) because you do such a good job covering the CFS/FM news from so many angles, including your readers’, and even your own experiments with non-allopathic interventions. I just hate to think that after all that good research (official and personal) that the general course of FM would be summarized by a study done from such a narrow angle, while what it really only reveals is the general course of FM under allopathic treatment.
If only there were such studies done about the general course of various diseases under allopathic as compared to alternative treatments. That would really be something to see, as both fields need oversight and consumers need a way to compare results.
Because on the flip side, there is currently very little way to check the claimed results of alternative medicine for objective validity…which (other than being unaware of their options) is a primary reason why so many people cling to allopathic routes (often, even when they don’t really work).
I completely agree. I tried to note that by saying that this is probably what an average FM patient seeing an average doctor can expect. I’ll make that more clear. I very much agree that we need studies that incorporate alternative health practices. Dr. Teitelbaum did a study on ME/CFS/FM I believe which indicated that the average patient made considerable progress when taking a multidimensional approach to these illnesses which incorporated alternative approaches.
That’s right, he did. I’d forgotten about that.
But it’s harder, I think, for the average (often already skeptical) patient to take a study like that as seriously as it probably should be, because of the enormous personal attachement he has to the outcome. Even if the study was entirely on the up and up (which I have no reason to believe it wasn’t), he has so much to gain from a positive result. (As does anybody who studies their own product…which includes almost every drug study ever done.)
But maybe I’m biased for having visited one of his associated clinics, and seeing firsthand the enormous amount of wealth one would have to have to follow his protocol.
I hope for a day when there is a neutral third party constantly running studies. I think we’d all benifit from the debate solidly emerging from the anecdotal. Right now, medicine is more a religion than a science. (In my opinion!)
That’s a huge problem Martha. It takes a lot of money to do all the tests and take all the supplements that many alternative health practitioners require. I don’t have the money to do that. The alt health field is in something of a bind; they can’t come up with the money to do the kind of studies needed for insurance companies to cover their treatments. Since they employ a multidimensional approach they can’t do the kind of studies that researchers prefer. Since they can’t prove that their treatments work, insurance companies won’t pay for their treatments which places the burden on the patient to do so.
I was diagnosed with fibromyalgia in 1985 by a very progressive doctor who battled for me to get wide testing, including a brain CAT scan, testing for neurological and autoimmune diseases. I was given a series of shots of Lidocaine down my spine and across my shoulders and after that I was in remission for about 10-12 years. But after being the sole caretaker for my mother for 7 years, and having 5 surgeries in one year it came back with a vengeance, with more pain. I take opiods, klonopin, voltaren. I take aquatic PT and go to a chiropractor who uses an activator – these help overall the most. I also have a form of narcolepsy- sleep paralysis-and degenerative osteoarthritis. I have an appointment with a new rheumatolotist, others I have gone to weren’t any more helpful than my GP. Pain Management has been little to no help, but I am required to be a patient due to state law to be prescribed opiods. When I was able to walk unassisted, an easy form of Tai Chi developed to help balance and joint mobility helped.
Over the last 42 years I have had periods of remission and if asked at the time would have said I was cured. It has come back worse each time and now at 65 I’m mostly housebound.
Doctors in the 1970’s were not kind and I was not diagnosed until 2009. With hindsight I can see a boom and bust pattern and blame a combination of genetics with stress and overwork. So I’m sceptical of ‘cures’ I’m afraid but think an informed work/life balance might have modified the outcome.
I would like to receive your newsletter.
After five years of pain, I have been diagnosed with FM.
With the level of pain I was suffering, I was almost housebound
except for the most essential errands. (I live alone.) With hydrocodone, 2-3 a 24 period, I have my life 85% back. However, at
eight hours, my body starts warning me of a need for medicine and the pain starts up. One night this week I got up at night after 10 hours and took a pill and then forgot in the am. Last night I did
the same thing. I am a bit afraid of taking these strong and wonderful pills…little life force if I don’t but I don’t want to
be so very reliant on them. Any advice other than keeping a journal of when I take them, day or night?
Congrats on finding something. Jarred Younger has said that if the opioids work and you don’t need to keep increasing the dose to keep them working then by all means use them. If you find your pain starts creeping up again that could be a sign of tolerance or even increased pain sensitivity.
It’s helpful to know of Dr. Younger’s views regarding the use of opioids, given that he is a major researcher studying the use of low-dose naltrexone. The current efforts by government to cut off many patients from using opioids when these are the only relief they receive is truly unwarranted when the patients follow the prescribed routine and do not abuse their medication. My well-informed internal medicine MD diagnosed me right away in 2002 when I presented with acute onset of symptoms of severe FM pain (I had been seeing him for several years so perhaps he already had a suspicion that FM was a possibility). He felt that FM likely is not solely one illness, but several illnesses – perhaps yet to be differentiated. I think this makes sense due to the fact that each patient’s case usually requires a unique treatment regimen calling for ongoing trial and error treatment methods and tweaking of medication dosages. It is discouraging to learn of the ridiculously low funding amounts allotted for FM research, given that at least 1-2 % of the population suffers with FM.
The effects of fibromyalgia on the patient and families cannot be stressed enough. I’ve had fibro for about 12 years. My husband became more and more disgusted by my illness and harsher and harsher with his criticism and complaining about my inability to be the person I was prior to my illness.
I became more depressed as time went on and symptoms worsened. I doubted myself that I was sick, I wondered if I was faking!?! Even though I was in pain, extremely fatigued yada yada yada… I had all the symptoms and eventually was diagnosed with fibro.
He made me feel as if I was a hypochondriac and crazy. My work performance suffered, I began missing so much work my job was in jeopardy. My relationships with friends and family changed. Long story short 2 years ago he walked out on me, we’d been together 23 years.
I was devastated of course but strangely enough after he was gone about 3 months I felt a bit better physically, after 6 months a little more improvement. After a year people began saying I was more like myself. This is the 2 year mark this month and I have improved about 40% I’d say.
I still have pain always, I take opioid pain meds every day, an antidepressant and sleep aid. But even though I live alone now I’m making it to work everyday and maintaining a somewhat normal life. My point in all this is that I intellectually knew about the effects of stress on the body for other people, but didn’t realize the effect it was having on me. I had no idea how much stress I had been under until it (he)left me. A blessing in disguise I would say now.
I don’t know if this will helpful to anyone but I can’t stress enough how much stress affects our bodies!! Lol.
Thank you for all your work Cort. I learn so much and feel so validated by the information you present.
That is such a great lesson Martrecia about how impactful healthwise being in a bad relationship can be when you’re already sick. I think it’s the story of fish pooping in a bowl of water. The water gets dirtier so gradually that you hardly notice. The stress wears away at you so gradually that you hardly notice.
I think we just lack the resilience to not have it affect us physically. And then when you’re at that point – how hard it is to move on!
Congratulations on your “escape” and your partial recovery.
I have tried different meds. but they all have side effects like me me feel worse or extra dizzy. Thirty nine yrs. of such much pain, ringing in the ears,dizzyness all the time ( some days vertigo),memory problems in remembering,fatique . It’s not just the pain it’s so much more! The older I get & now being 70 I feel like a recluse cause either no energy it comes in waves but thanks to my dog she helps me mentally and to walk her 15 min. or up to 45 min. depending plus that’s our socializing time as well. I do what I can cause tomorrow is another day. Somedays I do to much and then crash for a few days 2-3.
I take turmeric(anti-inflammation) and ashwagandha for the nerves system to claim it, 3 or 4x a day. Plus,monolaurin,vitamins,& probiotics. That is the best thing for pain the turmeric. I hope soon the brilliant minds of the scientist will come up with something natural instead of drugs. I can’t even tolerate using “Marijuana” in any form. Organic Turmeric is my speed:) God Bless Everyone .
I won’t take this test because it’s not asking the right questions. I went misdiagnosed with Fibro/CFS for 10 years and saw all the best so called Fibro/CFS experts in the USA – spent a fortune fighting something I didn’t have. They had no clue. Finally at the end of 2016 I FINALLY met a Dr. who knew what they were doing. The entire time I didn’t have Fibro. I, along with around 90% plus of Fibro/CFS/ME patients, have what is called Mold Illness, aka Chronic Inflammatory Response Syndrome (CIRS), aka Water Damaged Building syndrome (WDB). There is not a single test one can take for Fibro/CFS, yet with 100% certainty one can be tested for Mold Illness. The treatment is also effective yet can be complex in some cases. Why are we even still talking about Fibro/CFS. We should be talking about Mold Illness and how everyone has gotten Fibro/CFS wrong. Just saw your other new post about Dr. Ritchie Shoemaker. That guy is a hero and the CDC and most Fibro Dr.’s should be ashamed for ignoring his work and research. Thanks to Dr. Shoemaker I finally have a life again.
My fibro pain went off a cliff four years ago after 27 years of modest pain. Anyone who says he hasn’t had days of suicidal ideation with FM is lying and if you look at your short survey, it is congruent. Pretty much, FM gets worse not better as your nervous system ages. I’ve taken about every med through oxycodone (no pain relief, just knocked me out), any supplement with any positive research data, and all non pharm measures I could find…Adv. Barnes massage, yoga, acupuncture, vagus stimulators, etc., various electrical gadgets and I find life on Tramadol, Tylenol, and Ambien to be pretty much living hell. Even specialists have nothing to offer. While some fortunate isolated people may find non-traditional approaches to be helpful, if they really worked for a lot of fibies we’d know it. Currently, I’m starting a group of neural reintegration exercises designed by an elite trainer based on the starting point of the Z-Health I module, to sound really scientific. It is actually a bunch of simple things to jolt your nervous system back to reality, maybe. There’s a consumer version of Fisher-Wallace coming out on Indi I’m getting, probably waste of money but money means zilch when your quality of life sucks. Three years ago I developed constant tinnitus and four months ago treatment resistant GERD, both associated with FM…thank our our friend the vagus nerve for the reflux. Someone smarter than I called FM a life sentence with no chance of parole and, at 69, I suspect that is true for me, though younger people may have better lives. There seems to be no effective advocacy or lobbying for FM, though, and even the ME folks with no official diagnosis do much better, so young fibies better start kicking down some doors or they will have a tough time in our era of shrinking resources.
I have had fibromyalgia and myofascia pain for 67 years. I used many supplements, good diet, alternative therapy (chiropractic, myofascial release, Tai Chi) and moderate exercise successfully to lead a fairly normal life, taking NSAIDS when needed.
Yes, my pain levels have gotten much worse over time, but that is because life happens–car accidents, falls off horses, broken bones, torn ligaments, tendonitis, sprains, osteoarthritis, regular arthritis causing joint deterioration, etc. etc. There are not many 74 year olds who have no pain with or without fibromyalgia, so, of course, the fibromyalgia makes all the ravages of old age worse. It is in that respect that I think fibromyalgia gets worse over time. For the last few years,I have graduated to one tylenol #3 with codine when I go to bed at night so that my arthritic hips don’t keep me up all night.
Treating for bacterial infections, including Lyme and anaplasma, got me out of bed. Dr. St. AMand’s Guaifenesin protocol for FM has pulled out many phosphate deposits which have been causing pain. BRain function is much better. My energy is still low but I am hopeful the longer I am on guai, the better I will feel. I tried everything else for CFS and FM and nothing worked. Age 66. On disability for 26 years.
Like me, I am sure that the small minority of people who will check the boxes for “gotten much better”, will have a story to tell about “HOW” this happened – what they specifically DID that triggered the improvement. I doubt anyone “just got better” either by providence, or with the conventional wisdom available from most sources, including alternative.
So far everyone I have encountered who got better, did it by way of multi-disciplinary self-help, and it always included “pacing” and a regime of plenty of low-intensity activity. Plenty of people are “trying everything” and pursuing multi-disciplinary self-help, but not getting better, because they have not got the right lucky combination of things. I was like this for 20 years, but I worked out what the lucky combination was by connecting the dots between various researcher’s findings, covered by articles on this site (big thanks, Cort). The thing I was doing wrong, was exercising too intensely every time I tried to help myself through basic fitness-building.
You can be doing a lot of “right” things but to no avail, if you are doing SOMETHING wrong. When you stop doing that “something” wrong, and do it right instead, EVERYTHING you were “doing right” starts to have the benefit it was meant to.
I suggest that underactivity, period, would be just as wrong as “overdoing it” (which was my problem), possibly worse. Exertion avoidance does not result in loss of pain, which is what you might assume. The problem is that the loss of condition through exertion avoidance, leaves one vulnerable to provoking pain relapses with exertion of less and less intensity. One cannot exist without SOME exertion, and it is possible to lose so much condition, that shopping for basic needs becomes “over-exertion”.
The only way out of this trap, is to find an activity that is low-intensity enough that you can sustain it without provoking relapses, and then do that level of activity for as much time as you can possibly spare daily. When I turned my condition around, from my lowest ever overall state, I spent 2 to 3 hours per day, for a whole year, doing gentle aqua jogging and using gym machines on very low settings. Even walking was “too much” to start with, other than very slowly.
Low-carb diet, and liberal supplementing with Magnesium, were the other essentials in my multi-disciplinary approach. There is a lot more I could discuss, but basically I think that most self-help approaches do add benefit as long as nothing you are doing is “wrong”, which negates everything else.
The better you get, the more things you can use to benefit. For example, massage therapy is a waste of time and money when you are deep in the grip of full-blown FM. The same goes for pretty much all manipulation and hands-on therapy. Yoga, Tai Chi, Pilates, stretching routines, are all likely to just cause injury and set you back weeks. Your muscles are like rubber bands that have been soaked in concrete. They are no longer stretchable! Feldenkrais is harmless but the benefit can’t penetrate through FM-related body dysfunctions. But as you reach new thresholds of improvement, you can add more and more challenging things to your protocol and get benefit from them.
It is possible that “magic” supplements like CoQ10, “glyconutrients”, MSM, etc are completely useless when you are in the grip of full-blown FM, because they do not get through to where they are needed – the blood and lymph vessels involved, are blocked, or maybe the metabolic channels are dysfunctional. But possibly they accelerate improvement once it is well on the way already.
I married my second husband the year I got ill with CFS and fibro. I was still under the impression that I could beat the beast. After three and a half years of constant, constant stress and being very ill I divorced him and almost immediately started feeling better,especially I had less pain.
I started doing qigong, with the accompanying life cultivation and that is a lifesaver.
I still am mostly housebound but the quality of my life has much improved.I never thought I could feel happy again with this illness, but I can! Having cfs and fibro does not determine me … strange how it may sound.
Also, I take this wonderful supplement Seagreens and liposomal C.
So the moral of the story is that stress in any form is a killer, and that it makes sense to try to eliminate it as much as possible.
Hi ive been dealing with this 20 years odd started from from pushing it really hard out cycle training 110% effort mark funny thing was i’d be really fit&strong that year going like a train in races no mountain was too much done the training camps in spain also.
it seems a family thing also as others have it now.
quacks used to look at you like some fruit when explaining how you feel&many still do it’s only recently that i saw a specialist when cross referred from other clinic where i get my acupuncture that it now looks like they are confirming Fibro! i do have Raynauds also plus having a few other things hopefully checked as been referred by my Quack to rheumy but not the one i wanted to go to which is a Raynauds specialist as ive low BP&heart rate so meds had before dropped it through the floor so like being at sea in a storm swaying all over!
As many other illnesses interfere/modify/alter/add to likes of fibro etc so need/have to be taken into consideration esp with likes of meds! bit like being in bed your pulling covers up further&further now feet are getting colder!so have to find a happy medium.
Mine has changed over the years not always pain but aches plus tiredness has increased esp later/next day get totally burnt out feels like battery died all of a sudden so get instead of doing a lot with a little energy get it taking a lot to do a little seems like never going to do it.bit like with a pair of binoculars see normaly then look through wrong end everything seems a long way a way/tiny.
But few years back i looked into things/worked out etc as im classed as Autistic having asperger’s so see many things that others miss/can’t see/read etc so i tried a female pill called Zoely it’s a more natural E&P found it changed things many things was either gone or altered like bladder issues was great along with pain in base of spine i also walked better as muscles was so tight lost much pain felt better and slept better plus other things only took for a 2 weeks some things returned quicker others longer or didn’t but ones that did some altered in way they was!but the sleep is still better i think as don’t get so much of that ultra short sleep wake up nod off like i used to as in a few hours i could wake 40 times.
I have mentioned it to Quacks with what i found etc but most are so blinkered it’s ridiculous that there even in medicine even people that market it in the UK was poor.
I did say to them about it properly as im through when doing things check everything etc as like the detailed approach i said a short course like a few weeks then a few a week for a while would reset the body as that also brings your T levels up also.
they try to say E is female risky blah blah yet read the list of impending doom that is in box yet they gave me T which odd/funny thing is it has the same list of impending doom plus a whole dictionaries list of other things so another page ending in DEATH! so go figure!
Yet after id been on two lots of T i ended up having a small stroke as it made my BP go sky high! not to mention caused many issues like pains if i touched my forearms you’d think been beaten! sleeping was poor also.
So does Fibro get worse? Well it sure don’t get any better!
I think we learn to modify/live with it&learn about how it effects us so lessen it’s effects for one as i now just sleep if feel like it could be up for a short while and go back to bed or up for a lot longer sometimes can go for really long times or 8/9 hours and that’s it bedtime as each day is different as so many things can effect it.
One of the other things that no one is mentioning is not just the Fibro etc but what else is/has been effected as being a muscle effecting illness so much to consider not just bladder but lungs/airways/chest so breathing for one as i get that but also eye sight/hearing/taste/smell even skin as because it effects the bowels/stomach like CFS does anything that effects the balance of PH/flora in your system is going to have far reaching effects!
Many say but Fibro won’t kill you like MS well yes maybe directly but indirectly!!! as it’s weakening your body all the time so your more open/prevalent to other things that you’d not normally be effected by! so to a degree it’s in a way similar to likes of Cancers/strokes/aids and other deceases in that they don’t kill you directly as by then your getting so weak that often it’s Pneumonia/blood clots or other things that get you but it’s the under lying decease that is responsible
Cort thank you for tenacious reporting and desire to help others! Unfortunately there is so much doom and gloom in the fibro community. Patients are told to “learn to live with it,” by doctors who have realized drug therapy doesn’t work, at least long term. Most doctors, have all but given up on fibro patients obtaining lasting relief.
However there are doctors and patients who do have success with fibromyalgia. However after specializing in fibromyalgia for almost two decades, I can confidently say that traditional medicine alone is a dead end for Fibromyalgia. Chasing symptoms with one drug after another only leads to more symptoms, accelerated poor health, and frustration. Finding and fixing the underlying causes of the symptoms-deficient nutrients, poor sleep, euthyroid or out right hypothyroidism, adrenal fatigue, food allergies, etc. is what works for my patients.
I don’t have all the answers and my approach isn’t for everyone but people can overcome fibromyalgia and the majority of patients who work with me personally, do so. By getting healthy, much harder than appears and easily misunderstood, my patients get their life back.
Fibromyalgia is always in the background waiting to raise its ugly head if they don’t continue to practice healthy habits and avoid the stress that got them off track in the first place. I’ll probably regret this post but I strongly feel someone must let folks know don’t stop trying, don’t give in to the doom and gloom.
Thanks for that message of hope Dr. Murphree. I think we can conclude from the drug studies that while drugs surely help some they are not the answer to significant improvement for most.
It’s good to hear of others making progress. I was really struck by a small Alzheimer’s trial out of UCLA which employed what looked to me like a functional medicine approach which was actually quite helpful in reversing their symptoms – which has been though impossible. It was a small trial but an amazing accomplishment. I think we will hear more from them.
Anyone can read about that trial here – https://www.healthrising.org/forums/threads/reversing-alzheimers-what-could-it-mean-for-chronic-fatigue-syndrome-me-cfs-and-fibromyalgia.4715/
Dr. Rodger Murphree was one of the Fibro Dr.’s who treated me. I’ve seen all his videos, read all his books, taken all his pills, and followed every single piece of advice he had for me. I never faulted him for not helping me because he tried his best and told me that his model won’t work for everyone after I didn’t get better. Lost a little respect for Dr. Murphree when I recently told him about Mold Illness and my misdiagnosis of Fibro that him and many others gave me and in return he blocked me from Facebook. If his stuff is so great why would he block someone for offering helpful advice one time in a respectful way. I was never rude, just let him know I was misdiagnosed and let him know what diagnosis I had after 10 years of a false Fibro/CFS diagnosis. I had noticed earlier that if anyone speaks to him not helping them he will delete them immediately. Dr. Murphree, many studies by Dr.’s who actually know about this will tell you that it’s already proven in many studies that chronic Mold Illness (goes by other names) is responsible for the root cause of what is known as Fibro in over 90% of the cases. You can’t test for Fibro, but you can test for Mold Illness. Some on your treatments will benefit Mold Illness which is why some of your patients improve, but if you added the treatments that many in this “mycotoxin” field know about, you and your patients would benefit. I spent thousands with you and it was all for naught. All together I spent $130K out of pocket and saw about 120 Dr.’s. Each and every one of you got it wrong. Just please don’t plug your ears; if you’re open minded you’ll find that the majority of your clientele are dealing with this. As I told Juno I would be more than happy to speak with you about testing, treatment, etc.
Tramadol is a non-narcotic. It does not cross the blood brain barrier or have any of the side effects you get with narcotics. I’ve been on both!
FYI- although tramadol is not technically classified as an opiate, it works in part by being a mu opiate agonist. It tends not to be as strong or addictive as, say, hydro or oxycodone, but still needs to be treated with respect and caution. People do get addicted and often have withdrawals when trying to decrease or discontinue usage.
I was first put on Tylenol 3 and when it lost it’s effectiveness my MD. prescribed oxycodone and the same thing happened. I’ve now been on tramadol for years, which has not lost it’s effectiveness. I did find that tramadol increased my pain level for the first half hour or so but when I took 1 acetaminophen rapid release with it, that solved the problem nicely. If I’m off tramadol for more than 6 hours I do start feeling mild effects of withdrawal. I’m not worried about being on this pain med however, because it means my having a comfortable life as opposed to a living hell one.
VoiceAmerica health and wellness channel has a 13 week show on “From chaos to calm”. The show airs every Monday at 4pm. Today you can hear the story of a woman who overcame chronic Lymme, migraine and chemical sensitivities.
It’s wonderful that some people have actually been cured or almost of FM. But some comments stress the heck out of me!
I’ve been researching FM and ME and have tried probably everything that has been recommended for ME/FM. I manage to get somewhat better at times but because stress cannot be avoided in life something always happens to push me back down with horrible symptoms of Me and FM. I haven’t had a lot of control over the stress that happens and I have learned to put up healthy boundaries etc. but life is life.
Some people that have gotten better or improved a lot and stayed that way are few and far between. Now of course I’m talking about the combo of ME and FM. When I had just FM, I found pacing, exercise, good nutrition etc. to be very helpful but NOT with ME. All the pacing, light exercise, supplements etc etc since the dx of ME has not changed my path. I have been exceedingly dedicated to improving my health but remain quite sick.
There are many of us that can just barely manage our symptoms of ME/FM and until the etiology/causation of FM and ME can be found then many of us will continue to suffer no matter what we do.
I know of several people who were able to manage FM but when ME/CFS struck – and it seemed to be a severe form of it that did – that was something else entirely.
Lenny Jason has found that a subset of ME/CFS patients – the sicker ones as I remember – don’t really respond to pacing and things like that.
I think that if I could only afford to see a functional medicine doctor that I might have a fighting chance. The rheumatologist that I have seen has no idea what to do. Unfortunately since most of these holistic doctors do not take insurance, or Medicaid, it means that many of us will not get any better. I think that the whole body, and the stress level, has to be considered to get any real relief. I have the snowball effect of thyroid, POTS and possibly CFS.
I have had fibromyalgia for 20 years. I ran a fibro support group for 6 years, and so I’ve met many dozens of folks with fibro and a few with CFS. What surprised me most during those years was meeting very few folks who seemed to fit my own subtype. My fibro has always seemed like a constant evolution of symptoms as the years went on: myofascial pain>profound fatigue>Raynaud’s>IBS>autonomic/ortho challenges>erythromelalgia. I believe I also fit the criteria for me/cfs because often times when I’ve crashed I’ve been “gone” and basically bedridden for days on end. One of my dearest friends seems to share a very similar expression of illness and is ‘evolving’ the same way I did. (I believe Dr. Pellegrino has written about this occurrence, and in his experience, has stated that most fibro people in fact do not improve or recover over time.)
So for me, to ask if fibro gets better over time, I suppose it seems impossible to answer given the range of this spectrum.
It does seem that in too many articles, “fibro” has become framed one-dimensionally as all-over pain, but the other aspects of it (e.g. autonomic) get left behind.
Hopefully the autonomic part will be addressed more over time.
Hi everyone, here’s a great Youtube channel with free exercise routines to help people with chronic health problems, especially fibromyalgia! Hope it helps!
Cocolime Fitness: https://www.youtube.com/channel/UCs7LtZ5QXgCfT-_9RqycTRg
My ME/CFS has gotten better over the past 5 years, however I suffer with many other conditions so my health in general is not good. Most doctors ask me what ME/CFS is! I am so tired of that I just say “never mind” or “it’s like Fibromyalgia.” CFS seems to be either something docs still don’t believe in or they do not understand it to any degree. Tired of the whole thing as I deal with more difficult situations. It is nice that I am no longer using a wheelchair for Fibro and that type of pain is better. I attribute it to my opioid Rx’s and nothing else at this point.
I was first diagnosed with FM about 8 years ago now. In the beginning, Cymbalta (anti-depressant) really helped, but it faded after a while. While searching for treatment options I found a chiropractor. This opened my eyes to holistic medicine. Spinal manipulation and massage really helped. I then further searched for treatment online and discovered natural food. It seems obvious at first, but I cannot say more strongly how the power of natural food can both keep you healthy and heal almost any disease. By natural I mean NOTHING artificial. You also HAVE TO exercise; VERY mild in the beginning – you are in pain! Since practicing this I can honestly say that I’m cured. It is not easy, but will give you a new life or get your old one back.
Congrats on getting better and thanks for sharing how it happened Fraser.
I was diagnosed with Fibromyalgia around 6 years ago although I’m certain I have had it much longer than that. I have suffered from sleeplessness, joint stiffness, severe pains, depression and fatigue. My neurologist prescribed duloxetin 40mg daily (Given as 20mg twice daily), although it did relieve some of the pain, I still suffered from joint stiffness and extreme fatigue. Finally, i started on Fibromyalgia herbal formula i ordered from NewLife Herbal Clinic, this herbal formula did the magic! almost immediately i started usage, i started noticing a general reduction of symptoms including the very severe pains and fatigue. 9 weeks into usage, the disease has totally succumbed to this herbal treatment. The whole pains and terrible fatigue has seized and i am now able to function fully well again. (Visit their website www . newlifeherbalclinic . com ) I’m able to get out of bed in the morning and have more energy to go about my daily activities.
Aiden Lucas
I was diagnosed with fibromyalgia for 3 years, and it was very painful some days. I was taken methocarbamol to relieve the pain. Sometimes it helps and other days it doesn’t. it was killing me for 3 years, doctor said there was no cure. So I tried to live with it and it wasn’t easy.My childhood friend introduced me to Dr George (Good health herbs home),Dr George fibromyalgia herbal remedy cured me within 6 weeks of usage ,am fibromyalgia free now 100%
I have nearly fully recovered from fibro. I fully recovered from pain, pretty severe brain fog and fatigue, tingling, intestinal problems, light sensitivity, and frequent rashes in response to foods and pills/supplements. My energy level is about 85% recovered at this point. This is the only remaining symptom.
After months of experimenting and research, I developed the following protocol:
The most important component for me is thiamine, Vit. B1. I recovered from severe brain fog overnight by taking 20 mg. B1 in a high dose B Complex and vitamin supplement. The brand I use is natural and sourced from whole foods. Over the next six months, I slowly continued to recover. I continued to experiment with other treatments. I added magnesium since B1 supplementation can deplete magnesium (as well as zinc, potassium and a few other vitamins. I found that the high quality vitamins I take covered most of those needs.). In addition, several things were helpful:
– CES devise. I purchased a $100 CES device on amazon to help with insomnia and mood. I use at a low setting, 5 or 6 for 30 minutes for insomnia. Not a 100% perfect cure, but it helps a lot. If I really can’t sleep, I take 500 mg of L- tryptophan.
– Malic acid. I take about 100 mg. daily, which helps with energy levels
– ALC supplementation helped me over the finish line to recovery. It restored my energy levels significantly. However, it can cause insomnia for me. As long as I stick to a very low dose – about a 16th of one pill, I get the benefits without side effects.
– I already maintained a very healthy diet and a daily exercise routine before I experienced fibro. I’m sure this foundation helped. My diet is pescatarian – plenty of organic produce, nuts, and beans. I have been gluten-free for years. I do consume gluten free whole grains – oatmeal, brown rice, quinoa, etc. I have fish at least twice/wk.
When I developed fibro, I found I needed more protein. Eggs are now essential. I eat eggs about 5 times/week. If I start to feel fatigued, a few days of eggs daily really helps. I also eat more yogurt and high quality cheese. I try to eat pasture raised eggs and dairy when possible. I do not eat any foods that contain dyes, additives, etc. I also avoid any additives in supplements. Almost all additives cause rashes for me.
– During the week, I do about 45 minutes of cardio and weight training daily. On the weekends, I hike and practice yoga. As long as I respect my limits, working out is essential for mood, energy and general health.
A number of other supplements that I think have contributed to my recovery include:
– 5htp, I need very little, 100 mg./day
– NAC supplement, 1200 mg./day
– Vit. D, 1,000 mg/ day
– ALA Supplement, 500 mg./day
– Collagen powder daily
– Cutting back on caffeine and alcohol. Caffeine and alcohol deplete Vit. B 1. In the first months of my recovery, limiting caffeine and alcohol was very important. Now, I don’t overdo it, but it’s less of an issue.
– LED red light therapy
– Myofascial release therapy – really helped with muscle pain
Overall, my recovery is a lifestyle, not a one-time cure. It took about six months to recover on the protocol above. However, I would say that Thiamine is close to a cure for me – tremendous improvements on 20 mg. daily.