

A Review of “Human Heart, Cosmic Heart” by Dr. Thomas Cowan

Despite the focus some doctors (specialists such as the late Dr. Lerner and Dr. Cheney) have placed on the heart, most of the latest research is mostly focused elsewhere, leaving the quiet, mostly non-progressive heart issues seen in ME/CFS as a secondary problem – yet one that surely affects the daily functioning of the average ME/CFS patient.
A New View of the Heart
Dr. Thomas Cowan’s new book, Human Heart, Cosmic Heart, turns all that we knew about the structure and function of the heart upside down. More importantly, it may cast a new light on what’s going wrong in ME/CFS from the standpoint of circulation.
For most of us, it’s a given that the heart is a most vital organ and has an important role in the blood circulation in the body. But Dr. Cowan provides a new (yet old) way of visualizing the heart. This model shows the heart as a hydraulic ram, rather than a pump, where geometry and form matter more than any overt force.
In his book, Dr. Cowan asks us to strive for a deeper, more accurate understanding of what makes the heart “tick”. He asks us to ask ourselves whether conventional theories of how the blood circulates in the body actually do fit the “heart as a pump” model. Along the way, we are encouraged to re-consider traditional prescriptions for healing the heart such as low-fat diets and statin drugs and consider some new possibilities.
So how did we get here? The story actually begins with Leonardo da Vinci…a familiar name.
Leonardo Da Vinci
The first conceptualization of the heart was perhaps created as early as 1513 by Leonardo da Vinci. This short video better explains his methods and prescient findings.
[youtube https://www.youtube.com/watch?v=aIj2DL1geIg]
His early drawings and models showing how the heart creates vortices in blood flow through the blood valves is almost entirely correct when visualized next to a modern MRI done today. It’s amazing that he could conceptualize this using a wax model!
But somehow, these models were shunted aside, and in 1628, Dr. William Harvey, an English physician, next conceived of the heart as a pump in his famous book, “Exercitatio Anatomica de Motu Cordis et Sanguinis in Animalibus”. Conventional medicine now considers Harvey as the Father of Cardiology and his ideas regarding circulation have persisted now for over 400 years without review.
Perhaps now is the time for that review.
The Heart as a Vortex – A Facilitator of Circulation
Vortex: Noun, A mass of air or water that spins around very fast and pulls objects into its empty center -Cambridge Dictionary
So, if the heart shouldn’t be thought of as a pump, as we were all taught, how should it be more properly conceptualized? Under the conventional pressure-propulsion model, our blood moves because of the physical squeezing of the heart.
But Dr. Cowan asserts that the heart would never be able to accomplish what it does given the size of our circulation and what we know about fluid dynamics. It’s simply not powerful enough. (The full breadth of these arguments is well worth the cost of the book to explore in detail.)
In short, the structure of the heart itself does not favor the pump model. For example, the heart is thinner at the apex (only one cell thick!) at exactly the place where the pump forces would be the highest; if the pump model were correct, the apex should be the thickest part of the heart instead of the thinnest. We now know definitively that this is not the case.
Second, instead of stiffening at the moment of peak flow as a hose entering a pump would, the aorta – the main blood vessel to the heart – relaxes. When you turn on a hose at maximum pressure, the hose stiffens and straightens out to carry the water away from the source of the tap. The aorta does exactly the opposite: it relaxes.
Instead of a pump Dr. Cowan believes the heart behaves as a vortex which “facilitates the heavier elements of blood traveling down the central axis of a blood vessel and the lighter fluids toward the periphery of the vessel”.
The geometry of the heart supports this view. Within the body the heart can be visualized as a regular, seven-sided, geometric form which resides in a “box” in the chest at a very specific angle. That angle supports the creation of a vortex. The beauty of its placement can’t be explained well in words, so I invite you to view the work of Frank Chester, who has modeled the heart (called a chestahedron) beautifully.
But what does all this mean in terms of circulation, really?
It means that your heart doesn’t actually pump the blood, the action of the fluid does! But this is no ordinary fluid. To understand how the heart is able to move the blood through the body, one also must understand how fluid in our bodies is inherently different. The answer lies in what Dr. Gerald Pollack has termed EZ, or structured, water in his book, “The Fourth Phase of Water”.
Cowan further explains that any time you have a hydrophilic tube, like a blood vessel, a gel layer forms on the surface that carries a negative charge. The positively charged water is dissolved into the middle of that tube. The repulsion between those two charges starts the flow moving. This is the same process trees use to carry water and nutrients up to the heights of their crowns.
This phenomenon occurs even after the blood has nearly come to a standstill in the capillaries at the most distal ends of the body and then has to pick up speed again to begin the return trip back to the heart. Dr. Cowan likens this to a bus trip from San Francisco to New York that stops in the Midwest. No push from behind is going to get that bus going again. So, unless you really want to enjoy the charms of say, Kansas City, the body must somehow create energy at the furthest point from the heart, not the closest.
So, what does the heart do then, if not pump?
The conventional view of the heart as a pump visualizes the heart as a driver of the blood flow out to the small capillaries. Cowan believes, though that the heart is a facilitator rather than driver of our circulation. Its main goal is keeping the flow synchronized – not pumping it. The heart literally is the conductor of life and keeps the rhythm of the body synchronized in time.
So where do heart attacks really come from then, if not from blockages causing reduced blood flow?
Blood Vessels Take Center Stage
In Cowan’s model, the blood vessels take on a more crucial role. Cowan asserts that much heart dysfunction is actually a result of blood vessel abnormalities rather than the other way around. This is seen as the increased collateral circulation that develops around blockages to provide an alternate route for the blood flow. Most people with blockages have extensively developed collateral circulation. This is how someone with 95% blockage is still able to function at all. The body creates a detour.
Autonomic Nervous System and Brain
So, what ultimately controls the heart? The autonomic nervous system (ANS) and the brain do, of course.
Given that the regulation of the heart is under the control of the ANS, it makes sense that so many ME/CFS patients suffer from heart-related symptoms.
Typically, stress in the heart leads to sympathetic nervous system activation (“fight or flight”) and increased levels of stress hormones like norepinephrine as well as decreased heart rate variability (HRV) – both of which are seen regularly in ME/CFS.
As sympathetic activity is increased, a glycolytic shift occurs whereby energy production shifts from the clean burning of fat in the mitochondria which produces CO2, water and ATP to the dirtier glycolytic pathway in the cytoplasm of the cell – causing a buildup of lactic acid in the muscles, pain, fatigue, etc. Too much lactic acid in the heart muscle and a heart attack is almost sure to follow.
This shift can happen anywhere in the body. If it happens in your leg, you get a cramp. The muscle stops functioning and blood flow eventually washes out the waste products and homeostasis is restored. But two organs in our body can’t ever stop and rest to flush out the excess lactic acid. They are the heart and the brain.
In the heart, cramps and pain are called angina. In the brain, they may present as panic attacks, anxiety, depression or stroke-like symptoms.
Many modern diseases including metabolic disorders such as diabetes feature small fiber system dysfunction. Fibromyalgia has also been classified as a small fiber disease. Pain syndromes in general seem to fall under the umbrella of this model very well.
The ME/CFS Connection
Indeed, one sees a few typically characteristic heart abnormalities in ME/CFS. Dr. Cheney argued that the heart failure in ME/CFS was of a different type and was related to problems in circulation that were dramatically worsened upon standing. Most conventional heart function tests are performed laying down which might cause standing abnormalities in this population to be missed.
Dr. Martin Lerner also found characteristic heart problems in his ME/CFS patients. Typically, his examination included a thorough heart evaluation including ECG, heart ultrasound and an overnight Holter monitor evaluation. Dr. Lerner often found diastolic dysfunction, flattened and inverted T waves, and abnormal cardiac wall motion which he believed was caused by chronic infection with EBV or another one of the herpes viruses.
More recently Dr. Miwa, in a series of studies, has linked small hearts to orthostatic problems in ME/CFS.
Even those of us with the rapid heartbeats of Postural Orthostatic Tachycardia Syndrome (POTS) rarely think too much about the mechanics of the heart. Interventions are mostly directed at symptom relief without much consideration of the organ itself and its underlying mechanics.
Under Cowan’s theory, the small heart issues and problems with preload found in ME/CFS and people with idiopathic exercise intolerance would be a direct result of the lack of energy creation in the small vessels that help propel the blood back to the heart.
The small hearts in ME/CFS appear to result from low blood volume and/or problems with blood vessels that impair venous return to the heart. The heart muscle adjusts by reducing in size.
David Systrom has found that people with idiopathic or unexplained exercise problems (many of which must have had ME/CFS) have reduced “preload”; i.e. reduced filling of the heart. This “heart problem” appears to be due not to some structural heart failure but to blood vessel problems and low blood volume, right in line with the theory of the heart as a hydraulic ram.
Cowan’s hypothesis also appears to agree with Newton’s work which conceptualized the circulatory problems in ME/CFS as a problem with “venous compliance”. Venous compliance is how Dr. Newton has described the ability of veins to “push back” once they are filled with fluid.
Cort, in his earlier Health Rising review, describes this process as, “The fuller of fluid they are, the more the veins should – like a rubber band that has been stretched – exert pressure on the fluid to move. If ME/CFS patients’ veins are non-compliant; that is, if they’re kind of flaccid in response to filling they may not be moving the blood along as they should.”
This certainly appears to be true in ME/CFS and in other people with idiopathic exercise problems.
Treatment
If veins are not doing their job to push the blood back to the heart then exploring treatments that help to strengthen the veins, perhaps using herbs like gotu kola or infrared sauna to increase the amount of EZ water found in the walls of the veins, might prove to be helpful.
Dr. Cowan concludes his discussion of the heart with information on a little-known treatment in the US that is based on a plant called Strophanthus which contains a substance called ouabain. Ouabain is an endogenous cardiac steroid which helps to restore parasympathetic activity by enhancing release of its primary neurotransmitter, acetylcholine.
We have seen other parasympathetic nervous system enhancers be useful at alleviating symptoms in ME/CFS. David Systrom has found that Mestinon (pyridostigmine bromide) can be very helpful for a subset of patients.
However, unlike most drugs, strophanthin/ouabain is identical to the cardiac glycoside produced in the cortex of our adrenal gland. Ouabain is essentially a bio-mimetic neurohormone that has shown great efficacy in preventing attacks of angina and ischemia, as well as heart attacks.
Interestingly, ouabain also converts the lactic acid that may be a problem in ME/CFS into pyruvate so it can be used as a fuel for the heart. Dr. Cowan believes ouabain gets at the very core of what causes heart attacks.
Unfortunately, ouabain does not seem to work the same in skeletal muscle as it does in cardiac muscle. One has to wonder, though, if improvements in cardiac and small fiber functioning wouldn’t ultimately produce other improvements for ME/CFS patients. Certainly, this avenue looks promising for further study and represents a revolutionary new way to conceptualize circulatory diseases of the heart in general.
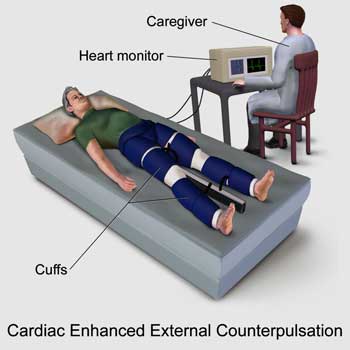
EECP by Bruce Blause – https://en.wikipedia.org/wiki/External_counterpulsation#/media/File:Blausen_0161_Cardiac_Enhanced_External_Counterpulsation.png
Dr. Cowan has found success using ouabain on his cardiac patients in his practice and prescribes it regularly. It has an excellent safety profile in German studies and very few reports of adverse effects.
Ouabain is still occasionally used in Germany and is available by prescription through compounding pharmacies. It is also available as a mother tincture through a company called Teebrasil as well. Dr. Cowan is also working to bring ouabain to the US as a supplement in the near future. Currently, it is available through his office to health care professionals.
Dr. Cowan also mentions another intriguing treatment in the book called Cardiac Enhanced External Counterpulsation. This treatment works for people who are too debilitated to exercise by forcing new collateral circulation to form.
In this treatment, one wears what are essentially large blood pressure cuffs on the legs and buttocks and is hooked up to an ECG. The cuffs then are set to inflate in time with the heartbeat. Currently this is used only as a treatment for angina, but I would love to see it tested in ME/CFS as well.
The Heart of the Matter
Throughout history time humans have spoken about “the heart of the matter” or loving someone with “all our hearts”. It’s no accident that the heart and, not, say the liver, has been used for these metaphors. The heart truly does signify something special that has been represented countless times over hundreds of years in art, poetry and spiritual practices. I guarantee that after you read this book, you will never visualize your heart in quite the same way again.
Finally, Rudolf Steiner’s idea about the three most important “things” for the further evolution of humanity are recounted in nearly every presentation I’ve seen by Dr. Cowan, so it seems fitting to close with them here as well. They are that:
- People stop working for money,
- People realize there is no difference between sensory and motor nerves, and finally:
- The heart is not a pump
Check out Dr. Cowan’s website here.
Dr. Mercola Interviews Dr. Cowan
[youtube https://www.youtube.com/watch?v=wEYrKJDN67w]






I have long suspected that blood vessels and other intersticial fluid vessels, are constricted in FM because surrounding myofascia and muscle tissue are stuck, clumped and knotty.
In this case there is very little that can be done to help, apart from dealing with the muscle tissue problems. Trying to make the blood itself more free-flowing, or trying to make the blood vessel walls more flow-friendly, would be like flushing out a car radiator where the main problem is that the miniature water pipes in the radiator are all squashed.
I believe this is why so many medications that “should help”, don’t – because they aren’t even getting through the blood vessels to the places they need to get to, to provide their beneficial effect. I would argue that the closer the blood-vessel system is to the actual muscle-tissue cells that need the nutrients, etc, the more miniature the vessels, the more the vessels are “squashed” into a flow-reducing condition.
This relates to FM, and specifically FM when the underlying causative condition is myofascial dysfunction (which I believe is “real” FM – the people with EDS, thyroid malfunctions, etc have been misdiagnosed with FM). If CFS does not include this squashed-blood-vessel condition, then other hypotheses are going to be the correct ones for that condition.
Man, I wish there was more research into the myofascia in FM and ME/CFS…
Bravo, Philip. I have the “real” FM and agree with you wholeheartedly (and maybe I need to be using my whole heart, LOL!)
I’ve always said – where does FMS leave off and EDS start? Is the hypermobile type, that they so far can’t DX with genes, what is being called FMS? I’m DXd with both EDS and FMS. But not sure which type EDS I have. Had a rheumatologist assure me I had it and wasn’t any real reason to do expensive testing. Geneticist agreed. Wouldn’t change what we did and they were quit certain I didn’t have the vascular type. So go with the professionals. I’d say either or both is no fun and they are for sure very painful.
Issie
Correction on this comment. EDS has new subset types – many who used to call themselves Hypermobile type no longer qualify to fit this catagory. They anticipate fewer to meet this and have created a lessor symptom catagory yet with similar symptoms but less skin and possibly less flexibility. This is the type I wonder about with FMS. I still seem to fit the HypermobiLe or possibly one of the other genetic catagory.
https://ehlers-danlos.com/what-is-hsd/
Issie
Hi Philip,
“I have long suspected that blood vessels and other intersticial fluid vessels, are constricted in FM because surrounding myofascia and muscle tissue are stuck, clumped and knotty.”
-> Well, I would have said my muscles are tight and compress my veins, arteries and capillaries but that would be not too different.
“In this case there is very little that can be done to help, apart from dealing with the muscle tissue problems.”
-> Actually I may have found something simple and free that works well and reliable in my particular case. I’ll get a bit technical first:
Let us work with the idea that hair vessels indeed do contract in sync with the hart beat. The mechanical equivalent would be a 5 meter long water whose laying on a solid floor. On the left hand side it’s connected to a valve allowing only flow from left to right. The other side of this valve is connected to a water tank at low pressure so that the valve will only open and let drip in water when the 5 meter tube is not completely filled. On the right hand side there is a vertical bend of 30 cm high. The garden whose is made of semi-flexible plastics.
Now step on the whose. The volume inside reduces. As water cannot flow to the left, some has to poor out of the tube at the right hand side effectively being pumped up by 30 cm.
Now wrap the 5 meter whose very tightly in with a strong type of bandage being layed around it in spiral shape. As the bandage provides a lot of tension, it will reduce the diameter of the whose. The enclosed area will be reduced more as area equals pi * radius squared. So enclosed volume is reduced. It will also require quite a lot of pressure to further reduce the diameter and hence enclosed area and volume. The result: you’ll have to step harder on it to get water pouring out off it on the right hand side and the amount of water pouring out of it (or basically being pumped up) will reduce.
So, you do more work and get less flow per time you step on it. That’s quite like our flexible hair vessels embedded into our tight muscles. When I started doing *very* gentle small exercises in order to reduce ridiculous high muscle stiffness over a year ago I noticed the following:
* Within days my mind became remarkably clearer; it has remained ever since; It still is quite limited; I still have my lows but those are fare less frequent and deep
* Within a week I regained much of the control I previously lost over my muscles; before I had increasing events that absolutely nothing happened when trying to move; I did not even feel my muscle was trying to do something at all
* Within a week the extreme pain shoots I had almost vanished; I still have muscle pains, but those daily “9 out of 10” (compared to 3 out of 10 for a wasp bite) type of pain shoots happened only a few times ever since
* Within a week as well my hart resting rate dropped from 90 to 95 (with an unability to reach 100 during exercise) to below 75. Now I usually am in between 65 to 70 with exceptions going between 60 and 75 and very rare exceptions of dropping to 45 – 50 at night
* This in itself however did not improve my exercising ability; it did however remarkably improved my quality of life
Until this blog, I only had a partial clue as to how this happened. Now I think I know. Thanks Cort ;-).
* The improved brain functioning I already contributed to reduced stiffness of neck, shoulder and chest muscle. The brain arteries are the ones with the biggest variation in diameter likely in order to control blood flow going from laying to standing and such. Having the muscles squeeze them reduces this amount of control to a very large extend, providing too poor blood flow regulation
* The reduced hart rate I attributed to better brain functioning but somehow it felt incomplete; This new idea fills the gap; Other arteries around the body are not near as flexible as those going to the head so that didn’t work out; But I forgot about the hair vessels: they are quite flexible; Even without seeing them as a pump it works out. Muscle inflammation creates peroxide/ROS; Ros kills NO; less NO means vessel constriction; vessel constriction means reduced blood flow
* Now add this new theory. If flow is too high due to tight/constricted/strangled hair vessels then you “step on the whose twice in the same amount off time rather then once to get the desired volume”; In this new model this means that the CNS increases heartbeat as a means of synchronization in order to “squeeze” more frequent on the hair vessels to get at least some decent flow out of it; So making the surrounding vessels less constricted by making the muscles less tight should reduce pulse rate. No psychological disorder required ;-).
I do daily some short series of small/tiny exercises loosening neck, shoulder, chest, arm, legs (and recently arm, fingers and feet). This is not enough to make them relaxed but I do notice a clear improvement of the average muscle tenseness. I mainly focus on two moments: getting out off bed in upright position, even at night going to the bathroom; I’ll sit on a chair first and do some of those exercise in order to get blood flow adjusted (copes with orthostatic intolerance to some extend); the other moment is before and after physical exertion (“warming” up and down, but both are far less vigorousness then even walking)
ADVICE 1: As neck exercises done wrong can block important nerves: CONSULT YOUR THERAPIST FIRST!!!
Note 2: I tried medicine increasing blood flow; hot-cold showers and “strong” self massage; all fired back in a major way; massive inflammation flare ups were the result; I believe some constriction “contains” inflammation locally so don’t go mad on vassodilation; I believe that the exercise I do only reduce some of the unanticipated additional constriction the inflammation mechanism isn’t aware off setting constriction to a more optimal value
Note 3: When I would think about what intensity and length a “warm-up” would be for a person with my severity of ME and FM then I have to divide both by a factor of five to come to a “dose” that fits me well; So don’t overdo, even if early results are promising. Don’t step up the rate the first days or weeks; wait for a month and increase; Listen to your body, if it likes the new regime up it again another month later. Backfiring is way to easy when going to fast. If you’re ill for years it’s better to be patient when things improve rather than destroy the opportunity.
Dr Derek Enlander has been using the leg cuff pressure method for treating ME/CFS for years. He also does ultrasound on his ME/CFS patient’s hearts. You can contact him at his office in NYC.
Didn’t know that! Thanks for passing that on OM.
I am not sure Enlander is still doing it. I think maybe the results were not long lasting??
I do remember some pulsation device being talked at at an IACFS/ME conference. I think it was in an abstract…
Dr Derek Enlander You Tube Video ME/CFS
https://www.youtube.com/watch?v=MVYpORKjJRQ
The heart and brain can’t clean out the excess lactic acid as other parts of the body, it was mentioned… sorry this is off topic, but are there treatments, supplements to help cleanse lactic acid from the brain???
They can’t stop functioning while they clear out lactic acid, not that they can’t clear it out at all. The brain uses lactate as a fuel source so the goal isn’t ever zero lactate. It’s a Goldilocks situation, apparently.
Too much lactate is associated with panic disorder. It might be possible to use something like beta alanine to reduce lactate levels overall but I’m not positive. Ouabain will help to reduce lactic acid levels in the heart.
I am disappointed to see this quackery and pseudoscience allowed to be published on Cort’s blog which I have grown to respect and value over the years.
Heart is not a pump? It doesn’t have the strength to pump the blood? And yet we pump the heart when doing CPR, we replace faulty hearts with mechanical pumps and people live. You don’t need to know nything about cardiology to see that these things work.
People with ME/CFS should know better than anyone that even a genius researcher like Dr. Davis needs a whole team, great cooperation, sharing of data and lots of money to figure out what’s wrong, and we’re supposed to believe this Cowan has single-handedly brought down one of the most advanced field of medicine?
Ah, so it’s hard science you are after…how about this article that says much the same thing in the Journal of Cardiothoracic and Vascular Anesthesia from 2015? http://www.sciencedirect.com/science/article/pii/S105307701500124X I think you’ll find Dr Furst posits much the same thing as Dr Cowan.
“R. FURST LOOKS AT THIS QUESTION FROM THREE MAIN ASPECTS. THE FIRST IS EMBRYOLOGIC DEVELOPMENT, IN WHICH HE COMES TO THE UNEQUIVOCAL CONCLUSION THAT THE BLOOD IN THE EMBRYO CIRCULATES BEFORE A HEART EXISTS TO “PUMP.” RATHER THAN THE HEART PUMPING THE BLOOD, THE BLOOD IS AN AUTONOMOUS “ORGAN” THAT MOVES BASED ON ITS OWN LAWS AND RULES.
NEXT, HE LOOKS AT COMPARATIVE ANATOMY AND COMPARES THE CIRCULATION AND HEARTS OF VARIOUS ANIMALS, BIRDS AND REPTILES TO THE HUMAN CIRCULATION. AGAIN, HE COMES TO THE UNAVOIDABLE CONCLUSION THAT THE HEART IS BEST SEEN AS AN IMPEDANCE DEVICE AND NOT A PUMP.
FINALLY, DR. FURST REVIEWS THE COMPLEX STUDIES ON CIRCULATION THAT HAVE BEEN DONE DURING THE PAST 400 YEARS. DR. FURST IS A TRUE SCHOLAR, AND IT’S HARD TO IMAGINE THAT ANYONE HAS A BETTER GRASP OF THE DETAILS OF THE CIRCULATION THAN HIM. IN HIS OWN WORDS:
IN SUMMARY, AN ATTEMPT HAS BEEN MADE TO REVIEW THE CURRENT STATUS OF THE PRESSURE-PROPULSION MODEL OF THE CIRCULATION AND HIGHLIGHT THE NUMBER OF INCONSISTENCIES WHICH HAVE BEEN EITHER EXPLAINED AWAY OR TAILORED TO FIT ITS MOLD. … EVIDENCE PRESENTED IN THIS MONOGRAPH SUGGESTS THAT THE BLOOD IS A “FLUID ORGAN” WITH SELF-MOVEMENT (MY CAPITAL LETTERS) AS ITS INHERENT CHARACTERISTIC” https://fourfoldhealing.myshopify.com/blogs/news/an-invitation-to-join-the-heart-revolution
CPR induces a rhythm that may lead to a return of circulation. It doesn’t work at all by manual squeezing. Physics says that is impossible. So I guess knowing something about cardiology would actually be of benefit!
I looked into it further. Both men (who seem to be quoting each other in circles to give false legitimacy to each other) seem to be promoting alternative medicine called “Anthroposophic medicine”
Wikiepedia: https://en.wikipedia.org/wiki/Anthroposophic_medicine:
Quackwatch:
http://www.quackwatch.org/11Ind/steiner.html
There is absolutely no scientific basis for their claims.
CPR’s purpose is not to restore hearth rhythm but to prevent brain from getting damaged due to lack of oxygen.
Chest compressions in CPR compress the chest and pump the blood out of thoracic and cardiac region to keep the oxygen supply to the brain. They do not return the rhythm, and they totally are the manual squeezing (compressing, more precisely). If chest is already open for surgery doctor pumps the heart with his or her hand inside the chest. It’s called Internal cardiac massage.
(Warning, photo of open human chest)http://www.trauma.org/index.php/main/image/364/
Defibrillation (electric shock) is used to change the rhythm back to normal, and that only in some cases (defibrillation doesn’t restart the heart like shown on tv).
This review is not a critique or analysis on the historical practice of anthroposophic medicine but a review on current perspectives on circulation and a critique of the “heart as a pump” model which has clearly shown itself to have outlived its usefulness with the advent of modern technology and imaging tools.
http://www.rsarchive.org/RelArtic/Marinelli/
References
Marinelli, R., Penney, D.G., et al. 1991. Rotary motion in the heart and blood vessels: a review. Journal of Applied Cardiology 6: 421-431.
Rushmer, R.F., D.K. Crystal. 1951. Changes in configuration of the ventricular chambers during cardiac cycle. Circulation 4: 211-218.
McDonald, D.,1952. The velocity of blood flow in the rabbit aorta studied with high speed cinematography. Journal of Physiology 118: 328-329.
Noble, M.I., 1968. The contribution of blood momentum to left ventricular ejection in dog. Circulation Res. 26: 663-670.
Bremer, J. 1932. Presence and influence of spiral streams in the heart of the chick embryo. American Journal of Anatomy, 49: 409-440.
Manteuffel-Szoege, L., 1969. Remarks on blood flow. J. of Cardiovasc. Surg. 10: 22-30.
Pomerance, A., Davies, M. 1975. Pathology of the Heart London, England: Blackwell Scientific Publications, pp. 538-39.
Taylor, D.E.M., J.D. Wade. 1973. Pattern of blood flow in the heart. Cardiovascular Research 7:14-21.
Kilner P.J., Z. Y. Guang, et al. 1993. Helical and retrograde secondary flow patterns in the aortic arch studied by three-directional magnetic velocity mapping. Circulation 88: 2235-2247.
Arbulu, A., I. Asfaw. 1981. Tricuspid valvulectomy without prosthetic replacement. J. Thorac Cardiovasc Surg 82: 684-691.
Werner, J.A., H.L. Greene, et al. 1981. Visualization of cardiac valve motion in man during external chest compression using two dimensional echocardiography. Circulation 63: 1417-1421.
Irisawa, H., M. F., Wilson, R.F. Rushmer. 1960. Left ventricle as mixing chamber. Circulation Research 8:183-87.
Brecher,G.A. 1956. Experimental evidence of ventricular diastolic suction. Circulation Research 4:513-18.
Lowell, L.B., L.S. Adamson. 1980. Relationship between blood flow direction and endothelial cell orientation at arterial branch sites in rabbits and mice. Circ. Res. 48: 481-488.
Stonebridge, P.A., C. M. Brophy. 1991. Spiral flow in arteries? The Lancet 338:1360-61.
Thanks for your nice comments about the blog Gel :). For me I’m really in no place to assess the validity of Cowan’s hypothesis and it’s certainly possible that he goes too far. I was caught, though, by the connection between the small hearts of ME/CFS patients and their preload problems which are blood volume and blood vessel related. (Systrom is beginning a study of that in ME/CFS.)
I did a pubmed search of vortex and heart and found numerous studies assessing the two. I have no idea if they go as far as Cowan – I imagine they probably don’t – but vortex dynamics are definitely being researched as a diagnostic tool. The most recent concludes: “These reference values enable the assessment of various cardiac conditions in any clinical situation.”
BMC Cardiovasc Disord. 2017 Jan 9;17(1):21. doi: 10.1186/s12872-016-0444-7.
Vector flow mapping analysis of left ventricular energetic performance in healthy adult volunteers.https://www.ncbi.nlm.nih.gov/pubmed/28068909
Nat Rev Cardiol. 2014 Sep;11(9):545-53. doi: 10.1038/nrcardio.2014.75. Epub 2014 Jun 3. The vortex–an early predictor of cardiovascular outcome?
https://www.ncbi.nlm.nih.gov/pubmed/24889521
Ann Biomed Eng. 2015 Jan;43(1):26-40. doi: 10.1007/s10439-014-1101-x. Epub 2014 Sep 4.Left ventricular fluid mechanics: the long way from theoretical models to clinical applications. https://www.ncbi.nlm.nih.gov/pubmed/25186434
Interesting reading is the work of AS Salmanov (1875-1965) a famous russian doctor who spend the last years of his life in france ( so one has not to speak russian to read his publications) He points to the important role of the capillaries which are “contractile pulsating organs.”the primary motor is the venous current, the wonderfull automatism of the heart is secundary”
THe total suface of the capillaries in the human adult would be 6300 m2, a ribbon of one meter large and more than 6km long. Hence he emphasizes the importance of the fysiopathology of the cappilaries in all chronical diseases.
Are there recent publications about capillaripathy and chronic diseases?
would be 63.000 m2 and their total length 100.000 km
So one can suppose they play a crucial role in human fysiology and fysiopathology.
That’s a good topic to search! I will check it out.
Hi Chrisbe,
I’m super interested and fascinated by what you shared about the Russian doctor AS Salmanov.
I have searched online and cannot find one thing!
Could you tell me how/where you found out about him? And how or where I could find out too?
Thanks!
Jenny
I did 30 sessions of EECP. It was not beneficial for my muscle condition, which manifests itself as delayed onset muscle soreness and injury following exertion (FM?). I also observed no improvement in energy. This therapy is designed to promote alternate channels of blow flow around blockages in coronary artery disease. I don’t think it is applicable for CFS or FMS.
Is the Institute Of Medicine sponsoring this site as listed at the top?
My understanding after looking into this EZ water stuff is that yes the heart is a pump but other mechanisms (possibly electrical charge driven?) may be assisting the flow in the smallest blood vessels.
http://pubs.acs.org/doi/abs/10.1021/la4001945
Oh my gosh…I’m glad you asked the Institute of Medicine is not sponsoring this site – the Open Medicine Foundation (OMF) is sponsoring – has contributed to it. We will fix that right away. Embarrassing…
“Ouabain is a cardiac glycoside that acts by inhibiting the Na+/K+-ATPase sodium-potassium ion pump.[5] Once ouabain binds to this enzyme, the enzyme ceases to function, leading to an increase of intracellular sodium.”
I wouldn’t think this would be desirable for people with ME/CFS. We already have enough trouble keeping potassium and magnesium inside the cell without sabotaging it even more.
Sodium channel blockers decrease the excitability of the cell. That is why they are used as anti-epileptics in some cases. I don’t think decreased excitability is inherently a bad goal in MECFS.
Obviously, more research needs to be done to know if it would be helpful or not generally for ME/CFS.
An alternative that doesn’t require a script is Huperzine A. It helps with acetylcholine in the body and crosses the blood brain to improve brain function. Helps with blood flows. And I can vouch that it helps the brain fog and seems to be helping my POTS and stamina. Other great help is pregnenolone.
Of course, those that have seen my comments know – I disagree with traditional treatments for POTS. In my case, supressing what most people call “symptoms” – I call “compensation”. Many of the things the body does may seem uncomfortable and may flag as an inappropriate lab – but, very well could be the bodies adjustment to try to stabilize itself. My trying to block these “compensations” was wrong for me. I found moderating things to a tolerable level and trying to work on “core” causes much more effective.
There are some really good studies showing effects with calcium channels – in particular N calcium channel receptors and some having antibody response here. For me, Using mast cell med that not only stable mast cells but also is a calcium channel blocker and vasodilate veins – has also been a big help for me. Tramadol also works on this.
There are also some POTS people being found to have antibodies to NMDR receptors – glutamate regulators. I recently heard that of someone who is being treated for this at Mayo.
https://www.ncbi.nlm.nih.gov/pubmed/11920920
Seems not only is POTS, but CFS has an autonomic nervous system malfunction. Maybe CFS people are having autoimmune issues too —-like some of us POTSies. My two best additions are Huperzine A and pregnenolone of recent.
https://www.ncbi.nlm.nih.gov/pubmed/20360246/
There is another antibody being found to have issues in CFS – TRPM3. if you note the above article pregnenolone helps with this. Here’s an article showing it’s connection in CFS.
http://onlinelibrary.wiley.com/doi/10.1111/cei.12882/full
Pregnenolone also helps with calcium and muscle contractions. Which would help with blood flow.
https://www.ncbi.nlm.nih.gov/pubmed/20360246/
Issie
Some caution with Pregnenolone is advised, as it is common for it to cause heart rhythm issues in some people.
So true! I recently switched from 150 mg of Source Naturals after my level failed to rise over 6 months. 30 mg of BioMatrix sublingual was enough to make my heart start going nuts so I had to back off! I’m hoping to see an improvement in my labs finally too.
I read a work, possibly this one but I think another, about 20 years ago on the same subject so I knew this was going to quote Steiner at some point. It was one of Steiner’s beliefs or mystic perceptions, that the heart worked as described in this article.
I’ve perused a number of Cowan’s books over the year but I never realised he was actually trained as an M.D. I always thoughts of him as a herbalist.
Thanks Cort for an interesting article.
As I understand it, CPR works by restoring some oxygen delivery to the heart. Old ideas that we are pumping blood around the body are no longer thought to be accurate. That is why you must fully “recoil” (come up off the chest) after each compression in CPR, so that the coronary arteries can back fill (the heart gets its blood during diastole).
I would wonder about how this theory applies to non-human, especially non-mammalian animals that have hearts. I am certain that our simple version of the heart as a pump is not the whole story. Blood is a complex organ in itself. Nevertheless, that doesn’t mean that this current theory is accurate either. The importance is in keeping an open mind, and not believing that we already know everything. By “we” I mean we medical practitioners.
I cannot currently evaluate the theory. I don’t have enough information. It needs to be looked at by someone with a strong understanding of physics and a mind open enough to see something new if it could be real… not so open that the brain falls out! 🙂 Thank you, Cort, as always, for stimulating our minds!
This is the core problem in ME/POTS Cort. I know a case from a patiënt who had a ultrasound scan standing, it shows diastolic dysfunction! For me this is objective and very serious proof of a bloodflow problem. I would like see more research on this phenomenon.
I agree with comments that of course the heart is a pump. It would have been more accurate for the authors to say that it’s not the only factor in regulation of blood flow.
http://www.cvphysiology.com/Cardiac%20Function/CF010
Interesting study on regulation of intestinal blood flow: https://www.ncbi.nlm.nih.gov/pubmed/10945962
As far as the reason our blood flow might be too low being our faulty thinking (ANS/brain fight or flight theory); oh sure. Because CFS is psychiatric or “brain overreaction”. Uh huh. Let’s ask NIH for more money to “research” that. Again.
Venous compliance – that concept is behind compression socks for diabetics. And why Dr. Peter Rowe recommends compression garments and swimming/pool exercise (deep water compresses our blood vessels).
In CFS we don’t typically get angina from lactic acid buildup in the heart, or plaque. We get “atypical angina” which is not from clogged arteries but from low blood flow. Which bring me back to my theory that if we have various connective tissue defects like EDS, the blood vessel walls may be leaky and not able to maintain proper pressure under certain circumstances. For anyone that’s into heavier reading, I think that research into bioheat transfer might be worthwhile instead of looking at our so-called “faulty thinking” as a source of low blood flow. http://bioheat.umbc.edu/files/2015/07/Chapter2_2007.pdf And/or looking into oxyhaemoglobin dissociation curve: http://medical-dictionary.thefreedictionary.com/oxyhaemoglobin+dissociation+curve
I think our muscles are one of the few things that may be working consistently well in EDS and ME/CFS FM. I find that despite my degrading connective tissues, if I can get into a deep water pool or body of water and exercise I know I can reliably strengthen my muscles to carry more than their share of body burden vs gravity. Muscles are not connective tissue as far as I understand.
Thanks again Cort. What I think is missing from the discussion is why we have low blood volume and how that would affect the circulation from this vortex viewpoint. For years, I have believed that there was an underlying problem with the way my cells processed water (frequent urination, excessive sweating, not flushing lactic acid), and florinef supposedly helps some people with their CFS symptoms. It seemed to do a good job for me in the beginning.
“We have seen other parasympathetic nervous system enhancers be useful at alleviating symptoms in ME/CFS.”
I can’t get my head around this… can someone please explain? If many CFS patients have low blood pressure/volume then WHY does parasympathetic system enhancers help? The parasympathetic nervous system is the rest and digest system so it lowers heart rate and blood pressure. How does its activation help for people whose blood pressures are already low? (I just can’t get my mind around the logic of it!)
Dr. Cowan describes the ME/CFS heart, microcirculation, and autonomic dysfunction perfectly. The studies back it up too, as well as the solution which is strophanthus. This should definitely be highly paid attention to by any cardiologist treating an ME/CFS patient.
Thank you for sharing this journey into a reimagined understanding of the heart’s role in ME/CFS. It’s inspiring to see a willingness to challenge conventional models and embrace new ideas that could improve treatment. Dr. Cowan’s work offers a unique perspective, especially for conditions like ME/CFS where traditional explanations often fall short. Your openness to exploring different theories is a testament to your commitment to better health, and I hope this path brings fresh hope and meaningful relief on your journey.