

Being in chronic pain is no fun, that’s for sure. Think of any area of your life – your work, your relationships, your mood, your finances – and see if chronic pain doesn’t impact it negatively.
But is being in chronic pain itself dangerous? Some in the medical profession give chronic pain short shrift. They assert that it’s the result of a false alarm from your central nervous system; i.e. while it’s uncomfortable, it doesn’t constitute a threat to you physiologically.
The pain in FM is certainly different from normal pain. Normal or “nociceptive” pain results from a tissue injury, while the “pathological” pain in FM is believed to derive mostly from the central nervous system. A tissue injury (that should heal) is the problem in normal pain; a wounded or dysfunctional central nervous system (which may not heal) is the problem in FM.
Perhaps not surprisingly given its origin, pathological pain also tends to be more associated with mood disorders than does nociceptive pain. It’s also associated with a whole array of other central nervous system problems (cognition, sleep, problems with other stimuli). That’s apparently what happens when you tweak a good portion of the central nervous system.
But does all that central nervous system tweaking add up to actual physiological problems? Afton Hassett and Daniel Clauw think it might.
They point to evidence suggesting that simply being in chronic pain may increase one’s risk of coming down with a cardiovascular or neurodegenerative disease, or cause cognitive declines or even, yes, contribute to an earlier than usual death. First they looked at mortality.
Mortality
In truth the evidence regarding FM and/or chronic pain and early death is mixed. One large FM study found an increased rate of death from suicide and interestingly, accidents, but not an increased rate of mortality otherwise. A Danish study found no evidence of early deaths in people with chronic pain.
A large 2009 English study found quite significantly increased deaths from cardiovascular disease and cancer in people with widespread pain – the kind of pain people with FM have. A 2001 study that found similar results but was flummoxed as to why – stating, “At present there are no satisfactory biologic explanations for this observation”. A 2014 meta-analysis reported that having widespread pain was indeed associated with small increases in mortality from cardiovascular disease and cancer.
Premature Aging
But what about aging? Regarding physical functioning, the news was not good. With regards to aerobic endurance 80% of women with fibromyalgia did not meet fitness standards, 66% failed lower body strength and balance/agility tests. The findings suggested that many women with FM don’t meet the fitness standards experts recommend for maintaining physical independence as they age. (The study recommended more exercise.)
Likewise FM patients appeared to have aged twenty years in a cognitive study. They performed worse on all cognitive tasks than age-matched healthy controls and performed similarly to healthy controls 20 years older.
Our brains, like the rest of our bodies, change as we age. In fact they get smaller. A recent study examining the brain volume of FM patients suggests that their brain volumes are a bit smaller than expected – another possible sign of more rapid aging.
Next the authors move to a direct biological measure that studies have directly associated with aging – telomere length. Telomeres – the end-caps of chromosomes – shorten as we age. Because they can also shorten in response to biological stressors, telomere length is thought to reflect one’s “biological age” as well. Decreased telomere length has, in fact, been associated with a number of diseases including cardiovascular disease, cancer and diabetes as well as early mortality.
The news in FM overall wasn’t all bad: FM patients had only a “trend” towards shorter telomeres vs. healthy controls, but within the FM group, the higher the pain an FM patient was in, the shorter their telomeres were. Being in severe pain and being depressed tweaked their telomeres a bit more.
A small follow-up study suggested that those short telomeres were associated with premature brain volume loss in three parts of the brain – all of which were associated with pain processing. That suggested that the biological stress imposed by FM – whether it involves inflammation or oxidative stress or whatever – was hitting that part of the brain hard.
Conclusion
The study evidence isn’t completely consistent, but does suggest that being in body-wide pain (perhaps because of inflammatory processes and/or inactivity?) as opposed to being in chronic pain, may modestly increase one’s risk of cardiovascular disease or cancer and perhaps even early death. Reductions in telomere length coupled with reductions in the volume of pain processing centers in the brain suggest that FM patients are indeed taking a biological hit from being in pain much of the time. Plus studies indicate that they are way behind the 8-ball with regards to cognition and to functioning as they age.
The fairly sparse – because not many studies have been done – it does suggest that people with FM may have more difficulties as they age than healthy people.
Daniel Clauw, one of the study authors, has been championing fibromyalgia for decades. Clauw hoped this review, which was published in 2015, would demonstrate that being in chronic pain has real and significant physiological consequences.
During the approval of Lyrica for FM in 2008 the skeptics came out. In a NY Times article “Drug Approved: Is Disease Real?“, Dr George Ehrlich, a rheumatologist, suggested that people with FM simply can’t handle modern life. Most people, he said, ”manage to get through life with some vicissitudes, but we adapt. People with fibromyalgia do not adapt.”
Almost ten years later, it seems the NIH agrees – it spends somewhere around $1 per FM patient per year, and has reduced FM funding by 30% over the past five years. (That occurred during a time when the NIH was purportedly paying more attention to pain research. Pain research funding has, however, remained flat.)
The fact that Clauw wasn’t able to refer to more studies was in itself an indictment of the neglect being shown FM. The scientific literature around a disease that effects so many people should be packed full of longitudinal studies that examine brain volume, central nervous system functioning, cognitive processing, etc. over time. Recent chronic fatigue syndrome studies, for instance, suggest that a hyperactive immune response early in the disease gives way to an under-active immune response later. One wonders what longitudinal studies of pain and stimuli processing pathways would reveal in FM…
A recent review, “Illness Perceptions and the Burden of Disease in Fibromyalgia“, though, outlined the difficult time many FM patients have trying to get help. Calling the typical health care journey “lengthy and complex”, they reported that patients are “likely to receive suboptimal or inappropriate pharmacotherapy”. The authors asserted that, “major improvements in FM recognition and management are urgently needed.”
Other studies show that fibromyalgia poses severe burdens on both patients and society. A French study found that FM imposes, “a substantial economic and human burden on patients and society”. Very high rates of unemployment and substantial direct costs for medications and physician visits characterized Canadian FM patients. FM patients saw the doctor more, had more comorbid disorders, and cost the Canadian medical system significantly more than patients with other chronic illnesses.
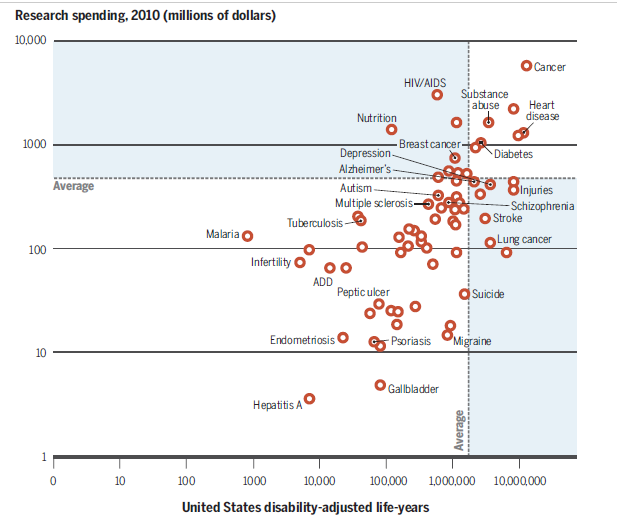
Check out migraine at the lower right – high burden of illness and low funding. Fibromyalgia is nowhere to be seen.
Bill Gates’s Institute for Health Monitoring and Evaluation is designed to address the health inequities in the world. By focusing on burden of illness it has revealed that many health dollars have been spent on diseases that relatively speaking, pose less consequential burdens on society. The IHME, for instance, has shown that migraines pose larger illness burdens on society than many better funded diseases. If research institutions were focused on doing the most good for the most people they would clearly focus more funding on migraine. (It continues to get pitiful funding.)
What’s really pitiful, though, is that the IHME doesn’t even include fibromyalgia – one of the most common pain disorders in the world – in the list of disorders they track. Why? Probably because fibromyalgia is so under-funded that the studies have not been done that would enable them to do that. In the NIH’s analysis of burden of illness and funding, fibromyalgia is nowhere to be seen.
It’s very possible that people with FM are aging more rapidly than usual; the reduced physical activity that comes with FM by itself could be causing that. Any person with FM probably wouldn’t be surprised by that news. The kind of distress caused by FM must, anyone with the disease would feel, have consequences.
What they would be surprised by, though, is that a disease which affects them so considerably, could still given such short shrift by researchers. THAT is distressing.








Great article Cort, we need to stand up strong on 12 May for ME/FM Awareness day to educate people.
I feel like I am an old grandma, but only 43 years.
Keep up your great work, I love your articles.
Thanks….I love being passed on the walkway by 70 + year olds gabbing away while I struggle to put on foot in front of the other…That kind of really seals the deal for me.
I will be 78 in July. I have had fibromyalgia for at least 40+ years. This past couple years has been extra difficult. The pain and overall discomfort has gotten worse. And there is no treatment for it. I have been on lyrica for the last 15 years. It is not as affective anymore, but there is nothing else. I’ve aged 10 years in the last 2.
I am 43 and know exactly what you mean. Yet no one around me seems to understand. I walk around most days feeling “lazy” unable to accomplish much, so frustrating.
We ABSOLUTELY NEED MORE FUNDING FOR RESEARCH INTO FIBROMYALGIA!
Excellent article, Cort. It’s a travesty that we haven’t made more progress. I will be observing ME/FM Awareness Day. It seems that we are the educators!
Most of the studies are focussing only on the pain in FM. Unfortunately, for me and many patients fatigue is as bad and sometimes a worse problems. I hope future research and medications take fatigue seriously too.
Agreed! Hopefully the research on fatigue in ME/CFS and cancer fatigue will translate to FM. To do that we need ME/CFS patients in FM and vice versa.
Brit’ Bunny in sc.
I’ve had cfs/fm since I was 51 years of age. I’m now 80 years. I don’t know how it would feel to ‘grow older’….I went from a middle aged woman to an old woman in 6 months…..I am now homebound and my 87 year old husband is my care-giver. I love life even with pain and fatigue. Thank you Cort for all you do for us.
I’m afraid that many days now, after 30 years of this, I don’t care if my lifespan is coming to a close.
I feel the same way. Even though I try to enjoy life, that black cloud of pain & fatigue is always there. I’ve had this since I was 36 & now I’m 58. Dying younger would satisfy me because it’s such a hard, difficult struggle everyday.
Please hang in there Gina – check out our recent fibromyalgia clinical trials update – there are some big ones going on this year which could help with treatments.
Thanks for this excellent review, Cort. It’s depressing to know that our suffering isn’t being studied or addressed, but it’s somehow comforting to have a bit of an explanation for why I’m so clumsy and stupid feeling and really old for my age. I too experienced going from feeling my usual age in my mid-50s to feeling more like I was in my 80s practically overnight. I’m extra wrinkled now and have such a hard time finding words, and many days much of anything. The double whammy for me came about 2 years into having fibro. It was then that I came down with ME/CFS. The combination, about a decade ago, is what caused me to be unable to work or have much of a social life. I agree that I wouldn’t look too forward to living an extra long life.
I agree that we definitely need more funding for research for Fibromyalgia. It’s very disheartening to know that we’re not really even being studied. It just makes that pain & fatigue that much more depressing & like they don’t even care to fund for research into this.