

Byron Hyde M.D. is a Canadian physician who has focused his practice on chronic fatigue syndrome (ME/CFS) patients for the past 30 years. In 1988, he founded the Nightingale Research Foundation to “explore, understand and treat the patients disabled with Myalgic Encephalomyelitis, Chronic Fatigue Syndrome (M.E. and CFS), fibromyalgia-type illnesses and post-immunization injuries”.
In 1992 he edited and published the 752-page The Clinical and Scientific Basis of Myalgic Encephalomyelitis and Chronic Fatigue Syndrome which in some ways has yet to get matched. He has an extensive database of over 3,000 ME/CFS/FM patients dating back over 20 years.
Missed Diagnoses and M.E.
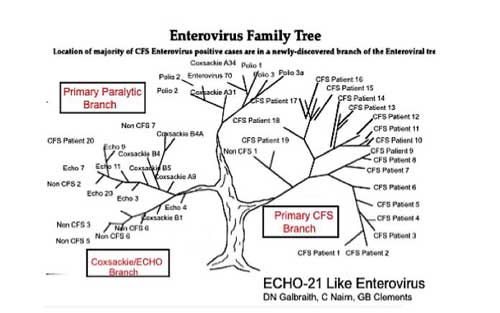
His controversial hypothesis is that ME/CFS is made up of two classes of illness: a condition called myalgic encephalomyelitis (M.E.) caused by an enteroviral infection, and another class of illness – known as chronic fatigue syndrome – which represents a false diagnosis. Hyde believes that M.E. patients are being mostly felled by enteroviruses belonging to a newly discovered branch of the enteroviral tree. (Other branches include the paralytic polio causing enteroviruses.)
Hyde, who is still practicing, is known for his extensive testing regimens. He asserts that people with true ME have a recognizable onset and distinctive brain signature that PET or SPECT scans will pick up. All the others almost invariably have another illness which testing, if enough of it is done, will pick up. (Some ME/CFS physicians will probably balk at that second conclusion…)
Hyde believes that a “large number of these reputed CFS patients have a treatable disease and with proper examination could be back to school and work.” He’s essentially agreeing that ME/CFS is a wastebasket diagnosis. He differs from others who’ve used that term in that he believes that people with ME/CFS are really do have an illness – just not ME/CFS.
It’s a stark thesis, one which one commenter pointed out, would, if taken to its logical conclusion, end research into this “disease” (!). (It would also boost research into enteroviruses and “M.E.”). It also appears to leave aside the possibility that the comorbid diseases associated with ME/CFS might have a common core.
Hyde’s thesis presents an opportunity and a problem. If he’s right then a significant subset of “ME/CFS” (how large is unclear) have a disease that may be able to be treated, if they can only get diagnosed.
Of course, some people with chronic fatigue syndrome (ME/CFS) and/or fibromyalgia see many doctors and go through years of expensive testing to no avail. Others, perhaps in the majority, get more limited testing done. The difficult question, given the expense of getting tested in the U.S. and elsewhere, is when is enough testing enough?
How Much Testing Have You Had Done?
Hyde said it’s impossible to say how many people diagnosed with chronic fatigue syndrome actually have M.E. or vice versa. He does provide some ways to determine what group he thinks you’re in, though. Since enteroviral infections generally occur from June to November with a blip at Christmas, and often (but not always) occur in epidemic form (i.e. other people are getting sick around you), if your illness didn’t start then, then you probably don’t have M.E.
A SPECT or PET scan done according to his protocol will then confirm or deny ME. If you don’t have ME you should, he believes, get more extensive testing done. He described his findings from some recent “chronic fatigue syndrome” patients in an email.
I just got off the line with a US patient I was seeing on SKYPE/FACE TIME: he has been diagnosed with CFS, but in reality he has Hughes Syndrome (antiphospholipid syndrome). This is a very nasty genetic illness and his grandmother had a diagnosis of lupus. Dr. Hughes from St Thomas Hospital in London only first discovered the disease after 1985. So it is understandable it was missed for his grandmother who may have had Hughes Syndrome and not lupus.
Yesterday I saw a lovely teenage girl who looked like she was going to melt in front of me and was totally incapable of standing. She had been ill for 5 years and it was like her muscles were made of ice melting under a hot sun. She had not only severe POTs, missed by over 10 physicians, she also had one of the most classic cases of Ehlers Danlos with her carrying angle bent backwards by 220 degrees, (also missed), and I have only started to examine her.
On examination she also had a significant heart defect that had been totally missed. She’s been Ill for 5 years and no one had done a cardiac workup.
Two weeks ago another CFS patient was here for the first time and she had a missed heart disease and she has never been examined.
When I asked if any missed diagnoses in particular stood out, Dr. Hyde said
Cort, there are so many it is ridiculous. I would have to go through a few hundred or even thousands of patients to adequately answer that question. He suggested though, that one area that people with gradual onset might want to focus on is the heart.
One thing is certain, any patient with a diagnosis of acute onset or gradual onset CFS should have a complete cardiac assessment including, since most of these things can be either corrected or cured: example: (1) ECHO, (2) 48 HR Holter when they are told to run up steps, stand at attention for 10 minute without moving, go to a shopping centre (all these things will have an effect on the Holter(3) Stress ECG on a tract or bike, (4) Carotid Doppler. Up to 10% will have a significant missed cardiac illness.
Another recently emerging possibility is hepatitis B immunization:
I am also a very pro immunization physician but recombinant hepatitis B immunization is another matter. I have had 3 deaths and over 100 cases who have chronic, chronic illness following within one week of the second or third immunization with RHB. If you don’t know this, these people are called CFS.
The basic problem, Dr. Hyde believes, is that most doctors are not curious enough. The biggest problem with a chronic fatigue syndrome diagnosis is that for most doctors it ends the search. Either the doctor believes the illness is mental and sends them to a psychiatrist/psychologist, or doesn’t know what to do with it and discharges the patient, leaving them on their own.
What is more the problem is how physicians examine patients. The lack of physical examination and history taking has become pervasive. They tend to have a set group of blood tests and if they are normal then you treat the patient with an anti-psychotic of which there must be many, many dozens.
I think all physicians, when they do medical school, should be obliged to read the 1990’s book, On Fatigue by the incredible Italian author from the University of Turino, Dr. Angelo Mosso, one of the most beautiful books ever written on the understanding of the cause of fatigue.
Mosso devised a technique to open up the skull and insert water to study the shrinkage of the brain when abnormal fatigue set in. You can see this today if you do a circulating blood volume on real ME patients. They all have significantly decreased blood perfusion to the brain, some even as high as 55% decrease on SPECT circulation study.
Looking For Original Incline Village/Lake Tahoe ME/CFS Patients
Despite the fact that Dr. Hyde has been studying patients from the original M.E. outbreaks for years (he says 80% had enteroviral infections) he’s never been able to talk to any of the original Incline Village / Lake Tahoe patients. Please contact him at the Nightingale Foundation if you’re interested. There would be no charge for the consultation.
Hyde recently published a long and for many patients possibly quite familiar story of physician inattention which (a) outlines his concerns regarding the medical profession and (b) provides a dramatic backdrop for his assertion that undiagnosed enteroviral infections are rampant in M.E. Along the way, Dr. Hyde suggests that if the polio vaccine engineered decades ago had covered a few more enteroviral strains “M.E.” would not exist, and worries that new enteroviral outbreaks in Asia may soon start producing more M.E. cases in the West would not exist either.
Check out “Amy’s” story below.
The Terrible Tale of Amy Brown
Byron M. Hyde, M.D.The Nightingale Research Foundation. 121 Iona St., Ottawa, Ontario, Canada, K1Y 3M1, www.nightingale.ca. Nightingale gives permission to print & distribute this publication at no cost as long as the Nightingale logo is attached..
This story is about a lovely nine year old schoolgirl who lives with her family in an amazing and sometimes turbulent country called England. It once had one of the best public health systems in the world. It is still a country full of good and kind people and great physicians, but sometimes physicians are too busy and miss important illnesses. This is such a story.
Amy has two younger sisters in school and two older working brothers in their early twenties. The family has a friendly female dog, Winnie, who sometimes piddles on the floor when she is too excited and, of course, the two sleepy guinea pigs whose names are Betty and Primrose.
The family lives in a charming and tidy community where they own their own modest and happy home complete with a climbing rose bush beside the front door. Amy is one of those children who loves her family and who is active with her numerous friends. She enjoys her local school. She is an active sports participant. In fact there is little to distinguish Amy and her family from many thousands of happy girls and hard-working families across the United Kingdom. Let us call her Amy Brown of England to protect her identity, as long as you remember Amy Brown is not Amy’s real name and this is not a fairy tale.
Amy’s medical history is of no particular interest to this story either since, other than routine minor colds, she has always been a healthy child. There has been no history of a serious illness. She has received all of her recommended immunizations. Were you to meet Amy and her two younger sisters, I have no doubt you would find them the most charming of children. Theirs is a healthy extended family with no history of any psychiatric disease, no depressive disease or schizophrenic history. In fact the only significant family medical history I was able to uncover was two or three persons in this hard working extended family with a history of migraines. Amy’s family is the kind of bright, hard working English family the nation has been built upon. These are good people. Amy is a great girl, the kind you would want to have as a daughter or sister. But then the wicked witch arrived in the form of an innocuous virus.
Let me also tell you this is both a true story as well as a mystery story.
I don’t want you just sitting back there relaxing. I want to invite you to try to unravel this mystery with me, since her doctors did not. In fact, approximately fifteen doctors were to see and reputedly examine Amy, both family physicians and the physicians in the two hospitals where she was taken to. They all missed the obvious diagnosis. Can you unravel the mystery? Try!
There is a basic tenet in classical and modern medicine, which is, a complete medical history and a thorough physical examination should be done to arrive at a correct diagnosis. To my knowledge this principle is taught in every medical school in the world. I hope I am mistaken, but it appears, that not once was Amy thoroughly examined, and that not once was a complete medical history taken by any of the nine principal physicians and the six additional physicians who were superficially involved in Amy’s investigation and care. This failure then lead to near catastrophic consequences.
Please do not take this story as solely a criticism of English physicians. Many of my patients in Canada tell me they are only allowed to see their physicians from six to eight minutes. They are only permitted to ask one question before they are ushered out the door. It may be there is a worldwide contagion of assembly line medicine. Fortunately, most of the Canadian physicians to whom I refer patients take incredible care in properly listening to and examining patients. I know that similar excellent physicians can still be found in the UK.
But in many ways this is a puzzle so first let me give you a hint. The story is a bit like those Russian wooden Matryoshka or Babushka Russian nesting dolls, one inside the other. As soon as you open one doll, there is another inside, and another…
Matryoshka or Babushka Russian Nesting Dolls
The First Matryoshka Doll
All was well until the Christmas season of December 2014. It was the 23-24th of December and Amy and her family were going to their mother’s aunt for Christmas. It was about then when Amy developed a slight headache. Initially, no one took much notice. It wasn’t all that significant. But by the next day Amy was getting a bit listless and the headache was getting worse. So she stayed overnight at her aunt’s. The next morning her Aunt phoned Amy’s mum to tell her Amy now had an elevated temperature. Amy’s temperature had shot up to 40C (40 C =104 Fahrenheit). (normal is 37 C = 98.6 Fahrenheit.) It was assumed at first she had the flu or perhaps the headaches were the beginning of the family’s migraine. Everyone was sure it would pass. They kept her in bed and everyone thought it would soon be better with a bit of loving care, just like any bad cold or flu.
But Amy’s “flu” didn’t get better and, although the temperature went down somewhat, the headaches became increasingly severe and now there was a significant diagnostic rash breaking out on her hands, around and inside her mouth and perhaps elsewhere.
So they phoned their family physician for an appointment. He agreed to see Amy at the beginning of January in his office. When he first saw Amy, he didn’t appear particularly concerned. He didn’t do much of an examination. After all, it was a cold or flu.
In fact this doctor saw Amy on three brief occasions during the next ten days and over this period she was becoming increasingly symptomatic, increasingly ill. Her headaches had now become unbearable. By then, Amy’s skin lesions were now breaking out on her hands and wrists, inside her mouth and around her lips. Nobody looked at Amy’s feet. The doctor diagnosed herpes and put her on a herpes antiviral medication. Amy was not getting better. The medicine didn’t help at all.
The fourth time Amy showed up at the doctors, if it was possible, her symptoms were worse, but now there was a new physician present. Amy was almost comatose. At this point Amy’s headaches were so unbearable she must have felt she was going to die. In addition, she now had difficulty passing urine. She was very weak and she had difficulty standing without falling.
A doctor might have diagnosed Amy’s attacks as a form of syncope. But they didn’t. At times, Amy even had difficulties maintaining normal consciousness. Physicians might have then diagnosed encephalitis. But they didn’t. She had profound muscle weakness and pain. She had pain in her stomach and chest but the worst was her head pain, and her head often felt like it was exploding. And unlike Winnie her dog, Amy now had difficulty passing water but there was no obvious urinary tract infection. Her doctors might have diagnosed interstitial cystitis which can be seen in some entero-viral infections. But they didn’t.
This new physician (and fourth visit to the doctor’s) apparently did not know what to do or what was the matter, so he correctly sent the parents and Amy off to a regional hospital.
On the first visit to the regional hospital the doctors diagnosed Amy with a post viral illness and sent her home almost immediately. It doesn’t seem that any substantial history was taken. Let me remind the reader, this was the fifth medical visit of a very ill child and no real or significant history or physical examination appears to have been done.
Amy’s parents were now frightened and almost immediately her desperate parents took her back to the hospital where this time she was admitted. At sometime here, a blood test was taken for herpes simplex but it came back normal. The rash was obviously not herpes. However, as far as I know, no other diagnosis was made concerning the rash, the fever, or the headaches. If at all possible, Amy became increasingly worse. Nor was her weakness, her terrible headaches or her falls getting any better. The doctors then told the parents that Amy was having seizures. So they ordered an electro-encephalogram and prescribed anticonvulsants.
Electro-encephalograms were done. The parents were told there was no obvious seizure activity yet the doctors still prescribed anti-seizure medications and sent her home. According to the parents, due to the perceived attitude of the physicians, they were beginning to believe the doctors thought Amy was having psychotic episodes and biting herself in the mouth. ,
If she wasn’t before, now Amy was now not only frightened but scared out of her wits and so were her parents. Nothing constructive was being done for their daughter.
The parents were not receiving any practical assistance from the local physicians or the local hospital so on discharge they took Amy to a major hospital center 25 miles away to see a cardiologist. There, Amy was again hospitalized. The rash was still around Amy’s lips and inside her mouth and on her hands. No one looked at her feet. The headaches were terrifying and Amy was by now half frightened to death. She was nine years old. Her pain was relentless. She was understandably scared out of her wits and started to scream with the pain.
nother physician examined her mouth, which was sore, and diagnosed the significant swollen mouth lesions as due to Amy biting herself. However, Amy wasn’t biting herself.
The physicians also ordered a Holter Monitor, (a 24-hour ECG), to monitor Amy’s heart. This is a machine which can demonstrate irregularities if done correctly. The Holter was also found to be normal. Of course it was normal, since Amy was lying down during the entire time. A Holter cardiogram only makes sense if there is (a) a fundamental timing mechanism problem or (b) if the patient has an autonomic dysfunction. To diagnose autonomic problems the patient must be active so the doctors can tell how the heart responds to activity. They didn’t have her move, or stand, or even climb stairs or walk with the machine.
All the tests were normal. Of course the tests were normal. If you have a fracture of the ankle, you don’t do an X-ray of the head. Do the wrong test and you get the wrong answer. At this point, the doctors appeared to take Amy’s case as a definite psychotic manifestation and placed her on both narcotics and antipsychotics. This is a child with no personal or family history of any psychiatric illness.
What would you do if you were Amy’s parents? Put yourself in Amy’s position. She is nine years old with a headache so bad she thinks her head is going to explode. What would you do?
I have not been privy to any of the many physicians’ records, only the mother’s and Amy’s history. But it appears that none of the now several physicians had made any significant diagnostic or treatment progress. The following is a partial list of what was diagnosed:
List of reputed diagnoses
- Herpes simplex lesions on and around her mouth, which was incorrect,
- Seizures, (epilepsy) with a normal EEG, which was incorrect,
- Normal heart action as seen on Holter, which was incorrect had she been active,
- Psychotic episode associated with screaming. The screaming was correct but Amy was not psychotic, nor were her parents,
- One physician noted the mucosal lesions inside her mouth to be due to Amy biting herself. This again was incorrect. This was the classical findings of what ?
- The hand-lesions were diagnosed by another physician. He diagnosed this as hives. He never looked at the mouth lesions, or the feet for that matter. No one did. This was not hives. Again the lesions were the classical stigmata of what disease?
- Finally, the doctors diagnosed Chronic Fatigue Syndrome (CFS). This is always an incorrect diagnosis, because there is no disease called CFS. CFS is a syndrome based upon a set of symptoms associated with hundreds of different diseases. Most frequently the term CFS is used by physicians in place of either hysteria or anxiety neurosis. CFS is NOT Myalgic Encephalomyelitis. What is the difference?
Chronic Fatigue Syndrome or CFS is in effect a non-diagnosis. Doctors may tell the patient otherwise but for most physicians CFS is just a pseudonym for hysteria or a new name for a psychotic or anxiety neurosis. It is used since CFS as a term is more acceptable to the parent or child than telling them your child is crazy. But usually the doctor thinks one thing and the patient hears another. In reality CFS can be a multitude of very serious missed diagnoses, but that is not what most doctors believe. Most doctors use CFS to mean the patient or their parents are “hysterics.”
What is the correct treatment for CFS? There can be no correct treatment since CFS is (a) not a disease, and (b) represents a group of symptoms common to dozens of different pathologies, each with either a correct specific treatment if any treatment exists. In modern western medicine, a correct treatment is associated with a defined patho-physiology.
CFS is a very dangerous word: In the UK, CFS is an exceedingly dangerous term. Even a parent saying their child may have CFS is enough for some doctors to SECTION the child (to remove the child from the parents care) and place the child in a psychiatric institution, i.e. in protective custody.)
In fact, it appears that the only correct diagnosis given in Amy’s case to date was a post-viral illness, a diagnosis given in the first hospital. But the next question not asked by any of the doctors should have become, which virus? Following the negative herpes and relatively normal blood tests and normal cardiac tests, the quest for the actual virus appears to have been forgotten or was perhaps now unimportant to the slowly accumulating number of physicians. It seems the collective misdiagnosis has now become that of a psychiatric manifestation. For a physician, a psychiatric diagnosis is a great diagnosis since it absolves the physicians from doing any further investigative tests.
Even the difficulty to urinate (urinary retention), the diagnosis that sent Amy to the first hospital, was one additional good clue to the correct diagnosis and, along with the classical rash on her hands and mouth, all appears to have been forgotten.
So dear reader, for the first Matryoshka doll…what is your medical diagnosis? I am sure hundreds of people in the UK will have correctly diagnosed Amy’s illness, something her physicians had failed to do.
How many of you will have got the diagnosis that the doctors had missed? But for those of you who have not, let me give you another clue. Any one of the doctors could have just gone online to the national virus reference and read what viral illness was current when Amy fell ill. It also helps to know what viruses cause a Hand … and Mouth rash and what are the possible consequences to such a disease? It is incredible and most unfortunately for Amy, no single physician appears to have had taken the time to do answer that simple question or to understand the consequences of their failure.
But there was a very major diagnostic clue all of the physicians should have noted. The following are pictures of Amy, something which all of the doctors saw when they first saw Amy Brown. Those lesions on and around Amy’s red swollen lips also extended into Amy’s mouth. They were on her hands. Nobody remembers if the HFM rash was also on her feet.
So what is your answer to the classical diagnosis, which should have been diagnosed and investigated for complications?
The answer to the first Matryoshka Doll, to the first diagnosis, is
!!!Hand Foot and Mouth Disease!!!
The First of the Matryoshka or Babushka Russian Nesting Dolls
A big star if you got the first answer right, the one that approximately ten physicians or more missed. Hand Foot and Mouth Disease!
What didn’t Amy’s doctors do correctly?
- Each of the physicians missed a simple diagnosis. How could even a medical student have missed such a simple diagnosis of Hand Foot and Mouth Disease?
- If they didn’t know how to make such a diagnosis, all they had to do was to look at the viral database to ascertain what viruses were then current. Not one of the physicians did this search.
- They didn’t do a spinal puncture (lumbar puncture) to see if Amy had encephalitis or meningitis to explain her near catastrophic headache. With this incredible headache, that would have been an acceptable normal test to do.
- Yet not one of the many physicians appears to have ordered appropriate viral studies once they knew they had made the wrong diagnosis. Perhaps they did but I have no information suggesting such a relevant test was performed.
- No dermatologist appears to have examined the three HFM stigmata or diagnosed the rash once it was proven not to be herpes simplex.
- Not one physician ordered a HMPAO SPECT of Amy’s brain. It is perhaps the easiest way a physician can clearly define an encephalopathy. Modern software would show exactly what areas of the brain had been injured. It wasn’t ordered. (Is it possible England is so antiquated it doesn’t have Segami Oasis Neurogram software?)
- Apparently, according to the mother and Amy, the circa ten or more physicians didn’t once examine Amy with her clothes off. This non-action would have failed any medical student. In fact, during the first 4 visits to the family doctor, not once was Amy undressed and even the skin of her extremities examined. In the first or second hospital, not one of the doctors examined Amy without clothing to determine the extent of the rash. One doctor did see the rash on the hands and fore arms and described it as hives or an allergic reaction. Later, at least one doctor saw the severe rash in Amy’s mouth and suggested she was biting her gums. Incredible. It is incredible that no physician put the hand foot and mouth rashes together. No physician appears to have examined the whole body.
- It also appears that none of the physicians had done a complete history. Once again a reason to fail any medical student.
You might ask how 10 or more very well trained physicians allowed any of the above to occur. Very easy! By the time a third or fourth physician sees a patient, and certainly when the 10th physician sees a patient for the same illness, physicians often don’t take a history and don’t do a complete physical. Why? They each assume it was already done. One begins to wonder if there are physicians who haven’t seen a child or a woman’s body without clothing since they first dissected a cadaver in medical school.
A good history! A good physical! These are essentials to all medical students who wish to graduate, yet one wonders how frequently good histories and physicals are done by physicians once they have received their degree. Did any single physician actually see the rash for what it was?
Revenge
Amy Brown was now home again and it was only then the parents saw the incorrect history and physical the consultants had done in the two hospital centres. They were understandably upset. So, on the 25th of April 2014, approximately four months after Amy first fell ill, Amy’s dad called the hospital doctor regarding Amy’s report to complain of the poor treatment and incorrect history. Amy’s father had reason to be angry, but it appeared the doctor then became even angrier. He wasn’t going to take any of this guff. Exactly five days later after the father’s phone call, the doctor retaliated by issuing a Section 47 on the 30th of April 2014. Retaliated is a harsh word, but I believe there is no other suitable word to describe the doctor’s reaction.
What is Section 47?
Section 47: Being sectioned in the UK means the state has the authority to take the child away from the parents and place the child in a psychiatric institution. Section 47 takes away parental rights. This has happened too frequently to misdiagnosed children in the UK. In this case, the sectioning of Amy due to revenge to the father’s criticism might even be considered criminal. In America it would have been grounds for a legal action against the physicians and the hospital administration for many millions of dollars.
Not only in England, but in Canada and the United States and perhaps in many different western countries, when the physician doesn’t know what is wrong, when the often inappropriate tests come back normal, they too often diagnose PSYCHOSIS. In the UK, when the patient is a child, this child be sectioned. The social services are called and they come and seize the child and take the child or youth away.
From the physician’s point of view, in most western countries, there are several advantages to giving a psychotic diagnosis. All physicians are obliged to give a diagnosis, which is essential in all medical record keeping. The medical licensing boards demand a diagnosis. With a diagnosis comes an arbitrary treatment. If the patient’s illness is deemed psychiatric, the physician can then refer them over to a psychiatrist.
The psychiatrist assumes that the physicians know what they are doing and have excluded all infectious and anatomical medical conditions. Now the physicians can relax and get back to real patients. Psychiatrists have tens or even hundreds of anti-psychotic medicines to experiment with, even if the patient isn’t psychotic. However, in my experience, most smart psychiatrists immediately notice there has been a diagnostic error if there is not a true psychosis and release the patient from psychiatric care. They then call the physician and suggest there is a medical cause for this illness.
So why can a good psychiatrist make the correct inference when the GP or specialist internist can not. Because psychiatrists usually take the time to first listen to the patient and take a correct history.
So our great young girl, Amy of England, has been sectioned and the physicians at the major hospital have phoned the child protection agency to pick up our girl and take her away from the family into a nice psychiatric treatment centre.
Then a small miracle occurred…
The social welfare officer came to the family’s house, examined Amy, spoke to her and her parents, and must have decided it was the doctors who were mad and not Amy. So social services did the right thing and left Amy in the loving care of her parents, her sisters, her puppy and the two guinea pigs.
But possibly as a precaution, Amy is sent to a school where there were real psychotic children. On the first day one of the psychotic children at the school attacks the teacher and beats her up, injuring the teacher. Amy’s parents immediately withdraw their child from this inappropriate school.
Unfortunately, inappropriate sectioning of a child has another very dramatic effect on all such families in England. The families become rightfully frightened of their children’s welfare and tend to avoid all physicians. I assume the doctors are happy since they don’t hear from this family any more and they have now totally forgotten the patient.
The Second Matryoshka Doll
The second is an easy Matryoshka Doll to diagnose.
Amy first falls ill with hand foot and mouth disease. The disease becomes chronic and Amy develops:
- A major cognitive weakness and difficulties reading,
- Visual changes,
- The worst headache she has ever experienced,
- Significant muscle weakness and pain causing difficulty walking, and something else, causing difficulty standing. Have you guessed what that may be?
- Gastric difficulties,
- Our dear Amy of England now remains chronically disabled, in pain and terribly exhausted upon even minor intellectual or physical activity.
Anyone who has been there or seen anyone in their family with this collection of findings would immediately know the answer:
The Second Matryoshka Doll
Amy has encephalitis and a myelitis and specifically a Myalgic Encephalomyelitis!!!
Over two years pass and Amy is still ill. Not acutely ill as she was, but still bedridden and largely house bound. So the parents call me in Canada and ask my advice.
Why me?
First: First of all the mother knows I am not going to take her daughter away and place her in a psychiatric care institution. Her daughter is safe.
Second: I am a Canadian physician who was invited to come to London on the 6th of March 2010 to address the combined committee of the House of Parliament and the House of Lords at Westminster, on the diagnosis and investigation of Myalgic Encephalomyelitis. I have been invited to speak in the UK at least fifteen times over the years. I have also been working, almost exclusively with M.E. patients since 1984 and edited and was principal author to a textbook on Myalgic Encephalomyelitis. So I am generally known in the UK.
I will review my talk at Westminster at the end of this article.
A Phone Call from Amy’s Mum
On July 6, 2016, I received a phone call from Amy’s mum and on the next day I spoke with her and her daughter Amy on SKYPE. You already know the history but this is what I discovered
- Just before Christmas 2014 the illness began with mild headaches gradually increasing until the headaches were totally unbearable. This continued in an acute form for several weeks and in a sub-acute form and until the present time,
- Within two days of the headaches beginning, a significantly high fever occurred that lasted for at least 4-7 days,
- At approximately the same time, Amy developed a peri-oral skin rash both around the lips and inside her mouth. There were also skin lesions around her hands and forearms (her parents did not remember if there were foot lesions). The doctors diagnosed Herpes Simplex and treated her for this despite the herpes test coming back negative. The treatment had no effect,
- Later they diagnosed hives, an allergic condition,
- Amy developed difficulty urinating,
- Then Amy noticed persisting muscle weakness associated with pain,
- There was a gastric and chest area pain,
- Amy was having falls when she got out of bed or tried to go to the washroom,
- During much of this time she had acute and persisting chronic upper GIT difficulties,
- Then, as the severe headaches ebbed, the parents noted that Amy’s heart rate was significantly elevated even lying in bed and she had chest pain. Understandably, the parents took Amy to see a cardiologist in the more distant second hospital.
- They had gone to several physicians, first locally, who had diagnosed herpes. Then they went to a regional hospital where they diagnosed a postviral illness and eventually hospitalized her. The parents then took Amy to a major hospital centre were she was initially diagnosed with seizures. The physicians diagnosed epilepsy despite there being a totally normal EEG. Since the tests were all normal doctors appear to have decided Amy was a hysteric and suffered from a psychotic illness and sectioned her.
Many of the several findings noted above were the typical prodromal signs of paralytic poliomyelitis and more specifically what was once referred to as Missed Polio, usually meaning there was no permanent paralysis and deaths were rare. They are also the frequent symptoms of Myalgic Encephalomyelitis. There are no differences between the signs and symptoms of Missed Polio and M.E. Only time and distance separate the two names.
Both the history and the photographs sounded to me like a typical case of Hand Foot and Mouth disease (HFM). This is, in most cases, a minor illness that appears in children from 1-5 years. In older children and adults the consequence of HFM disease can be much more unsettling as they were with Amy
The Third Matryoshka Doll
To understand the third Matryoshka doll you need to do a bit of homework. It helps if the reader, and the physician know their medicine and understand
- hand foot and mouth disease (HFM disease),
- the enteroviral causes of HFM disease and what injuries these viruses can cause when either mild or severe cases arise,
- the enteroviral cause of Myalgic Encephalomyelitis and its relationship to both HFM disease and to paralytic poliomyelitis.
There would have been no difficulty diagnosing Amy correctly if she had fallen ill prior to 1954 and not in 2014. In 1954 Amy would have been diagnosed with a mild or a “missed” case of poliomyelitis. She had all the findings to make this diagnosis.
Then in 1955 the Salk polio immunization was introduced and shortly after, poliomyelitis disappeared in most of the western world, but not M.E., which often accompanied paralytic polio epidemics. What has been forgotten is that up to 1955, certainly in major poliomyelitis epidemics, it was noticed there were always a significant number of Myalgic Encephalomyelitis patients mixed in with the paralytic cases.
There were several major exceptions. One was the 1934 Los Angeles epidemic. Another was the 1957 Royal Free Hospital epidemic in London. In both of these epidemics, more M.E. cases occurred than paralytic polio cases. It was during this second London epidemic that the name Myalgic Encephalomyelitis was first used to describe M.E. and the term “Missed Polio” tended to disappear from the physician’s lexicon.
What is also now largely forgotten is that the three enteroviruses discovered and named after 1949 as polio 1, 2 and 3 (Brunhilde, Lansing & Leon strains) were not the only enteroviruses causing flaccid paralysis and death. The last major epidemic of paralytic poliomyelitis in the Soviet Union was none of the three so-called polio viruses. It was a similar enterovirus to polio, called Coxsackie. Thousands of people died or were paralyzed.
Unfortunately, this Coxsackie virus and the other enteroviruses causing paralysis and M.E. weren’t included in the Salk and later in 1961, the Sabin oral polio immunizations. If it were possible and if the entire enterovirus family had been included in the immunization, I believe there would be no new cases of Myalgic Encephalomyelitis today and no cases of flaccid paralysis and death caused by the other enterovirus infections. Also, Amy would not have fallen ill and become seriously disabled.
Let us review Amy’s disease for you. First, HFM disease in humans is not the same disease with a similar name, Foot and Mouth disease (or Hoof and Mouth Disease), that farmers infrequently see in cattle and cloven hoof livestock in Europe. This does not spread to humans.
I would like the reader to understand that all viral infections have a spectrum or degree of injury. Most viral infections are simply bothersome or give no symptoms yet may cause the patient to become immune from subsequent identical viral infection. The same virus which caused no injury to some people can also cause significant and sometimes chronic illness and at times death. The difference depends upon many factors related both to the virus and the person infected.
Hand Foot and Mouth Disease (HFM) In children tends to be a relatively mild disease, particularly when it occurs in children from age one to five. Yet these HFM viruses are very similar to the several different paralytic polo-viruses in that they have only about a 5% genomic difference from polio viruses.
Like poliomyelitis, most of these infections pass by without serious consequences. Most people do not even fall ill. Like the 3 different enteroviruses which cause polio, Hand Foot and Mouth disease is also caused by several different but similar enteroviruses. Like polio, less than 5% of the several Hand Foot and Mouth viruses go on to cause serious chronic illness. But many enteroviral illnesses tend to vary in their destructiveness with age.
In severe cases like our Amy Brown, some patients fall seriously ill with:
- muscle weakness,
- encephalopathy,
- pain syndromes
- cognitive difficulties,
- paralysis and sometimes death.
- in some cases such as with Amy, the area of the brain related to POTS or dysautonomia is injured.
This has been happening regularly, particularly in Southeast Asia, and has spread to North America, Europe and the UK. Thousands of children and adults in Southeast Asia have fallen ill, some have become chronically ill, some have been paralyzed and many died during the past 10 or more years. It has spread to North America and to Europe and England.
Epidemic paralytic poliomyelitis may never have existed until 1881 when it was first reported as occurring among twelve people in an isolated single room school in northern Sweden. Then from 1881 until 1905, when the first major paralytic polio epidemic broke out in Sweden and Norway, few physicians took much notice of polio. Some even called it mass hysteria. It was only after 1905 that paralytic polio became a world threat.
The increasing instances of non-polio paralytic virus infections around the world over the past ten years makes me concerned that soon, a new and possibly massive epidemic could soon occur in the west as it has over the past ten years in China and Southeast Asia.
Over recent years I have seen several teachers who have fallen ill due to this virus. Sometimes students tend not to be very ill, so they go to school and can infect their teachers who then fall very ill with what many know as Myalgic Encephalomyelitis. Not all of those injured are associated with significant pain but all of them are, in effect, a missed encephalopathy. In my experience with adults, it has occurred most often amongst students, teachers and health care workers.
When HFM occurs in either primary or secondary school children in Canada, in most children it is not a very serious illness so they are sent to school and their teachers sometimes pick up this illness as an encephalomyelitis. In my experience some adults tend not to have skin lesions.
In children and adults with HFM disease, particularly with enterovirus A 71, the illness can be significantly worse. The epidemic and sporadic disease, Myalgic Encephalomyelitis (or M.E.) is one of the more common chronic effects. The urinary and other symptoms that sent Amy off to the first hospital are common findings in both polio and M.E. infections.
The Poliomyelitis and M.E. enteroviruses are similar but have adapted to different loci in the body. Above the brain-stem and in the brain, the very similar enteroviruses that cause M.E. injure small blood vessels supplying the cognitive and administrative neurons. However, due to the protective organization of the brain, there are multiple blood supply sources to neurons in the brain, so death from M.E. is rare. It is also possible that the major M.E. pathophysiology is arteriole cuffing and that autoimmune forces then play a significant role around this cuffing causing disease chronicity.
So which of the enteroviruses seriously injured Amy Brown? We know it was an enterovirus because Amy fell ill with HFM disease. But we don’t know which enterovirus. HFM disease in humans can be caused by several enteroviruses and the doctors didn’t bother to check which one. So the guess is yours.
There are probably more than three such enteroviruses causing HFM disease. The most recent and most common enteroviral (EV) causes of HFM virus and HFM associated M.E. in the UK are probably the following:
Type 1: Hand Foot and Mouth (HFM) Disease due to Enterovirus 68: One of the several causes of enteroviral HFM disease circulating in the UK in July to December of 2014, the same year Amy first fell ill, was EV 68. This virus, EV 68 (enterovirus 68), not only causes HFM disease, it is also the same virus killing and causing flaccid paralysis and muscle weakness in older children and adults. EV 68 is a disease entity almost identical to polio 1, 2 and 3 that has occurred across North America and Europe during the past few years but was particularly present in 2014, the year Amy first fell ill. To date, there is no immunization for this viral infection or for that matter for any of these non-polio enteroviruses. There is specifically no immunization against any of enteroviruses, including EV68 or EV71.
Type 2: Hand Foot and Mouth Disease Coxsackie A 6: In exactly the same time period, during the winter of 2014-2015 when Amy fell ill, Drs. C Sinclair and E Gaunt et al in Edinburgh identified a cluster of 16 HFM disease patients caused by Coxsackie A6 and published in the medical journal Euro Surveillance (2014, Mar 27;19,12:20745.0). This Edinburgh cluster was probably the tip of the iceberg. I have no doubt thousands of children and adults in the UK fell ill with this illness and like Amy have been misdiagnosed. The reader can be fairly certain that up to 5% of those patients who fell ill in the UK are now, like Amy, chronically ill, misdiagnosed, and some placed into a psychiatric institution as they tried to do with Amy.
Type 3: Hand Foot and Mouth Disease EV 71: This enterovirus can also cause HFM disease and also herpangina (a more generalized rash). It is also associated with more severe illness, high-grade fever (body temperature above 39°C like Amy), flaccid paralysis, encephalitis, pain syndromes, aseptic meningitis, cardiopulmonary and neurological complications. A large number of patients have died in Southeast Asia with severe illnesses, including AFP, aseptic meningitis, encephalitis, pulmonary edema or hemorrhage, and myocarditis (heart injury) or worse. Our Amy certainly had one of these infections but her many physicians somehow forgot to test her for enteroviruses, the major cause of HFM disease.
Amy’s mother sent me photographs she had taken of Amy, which once again were typical hand foot and mouth disease skin lesion and typical locations. The doctors thought (a) the exterior skin lesions were herpes and (b) the ones in Amy’s mouth were due to Amy biting herself.
I have no evidence that the physicians in either hospital suggested HFM disease or tested for enterovirus or did a lumbar puncture. Spinal fluid analysis done early in M.E. have demonstrated CNS neuron damage with positive oligoclonal banding. At least two of these HFM viruses were current in England when Amy fell ill with what sounded like an encephalitis. These HFM viruses can and do cause meningitis, encephalitis, acute flaccid paralysis or myelitis and it is difficult to understand why Amy was not at least tested for these severe illnesses.
The description to date, given to me by the mother, was classical of both HFM disease and Myalgic Encephalomyelitis. I had already seen four teachers ill with Myalgic Encephalitis in Canada who had students ill with hand foot and mouth disease. Enteroviruses, depending upon the age of the patient, can give very different degrees of illnesses, varying from unnoticeable, to mild, to severe. The same type of enteroviruses, depending upon the individual infected might cause gastritis, or pain syndromes, pulmonary complications, cardiac disease, paralysis, or death. Enteroviral M.E. is just like polio where most infected patients at first had no visible illness and yet up to 5% of these patients were paralyzed or died.
Still in Canada, I wrote a letter to Amy’s hospital doctor and suggested to her mother that she take Amy back to the physician with the letter in which I suggested certain enteroviral tests and an HMPAO brain SPECT, which would demonstrate perfusion brain injury, if this existed, as I believed. This would change Amy’s illness from the incorrect psychiatric diagnosis to a physical one.
The parents followed my suggestions and took Amy back, but the specialist stated she wouldn’t do any of the suggested tests since they were invasive. In Canada we do these suggested tests on a regular basis and in 30 years we have never had any patient injury. I believe this reply by the UK physician might have represented a tactical position, because if the test was performed and demonstrated significant disease, the physicians would have been embarrassed. So once again neither Amy nor her parents were listened to and were once again dismissed. The doctors had made up their minds and this girl was to be sectioned for psychiatric illness. End of story.
Ethical Problem
There was now a major problem. With an adult ill for almost three years, you can give advice and suggestions. It is then up to the patient to make any decisions.
However, when the patient is a youth now 12 years old, ill without a correct diagnosis for almost three years, if the local physicians aren’t interested, what can one do? This is clearly a situation no moral physician should abandon.
So I asked the mother if she wanted me to do a house call. She said yes. So my wife and I flew to the UK and arrived at their home in England on a balmy February day. It just happened to be a school holiday so mum and the three girls were all at home. The following is what I found.
This was a house with an understandably worried mom, two happy and lovely children and a girl who was now 12 years, stranded by the medical community for over two years. Amy was lying in bed trying to read a book. The dog Winnie and the two guinea pigs, Betty and Primrose were quite contented. The children’s father was at work. Except for Amy, they appeared like any above normal intelligence family.
Amy appeared a bit timid and withdrawn. Amy’s mum told me her daughter had been emotionally traumatized by the several physicians she had encountered, so I decided to spend the first 30 minutes chatting with Amy and her sisters, hoping she would become used to me. Then I asked if I could examine her. Mother and daughter agreed, and with my wife, mum and the two sisters gathered around I examined Amy. According to the mother, during the course of her illness, no physician had seriously examined Amy before.
I started by taking Amy’s blood pressure and heart rate. It was relatively normal at 88 beats-per-minute (bpm) with a blood pressure (bp) of 109/76 mg of mercury. These findings would be considered normal for her age, although 88 bpm might be considered to be a bit rapid for someone lying down in bed.
I asked Amy to stand and her heart rate immediately rose to 116 beats per minute (bpm). Much too fast, but it quickly settled down to 105 bpm, still much too fast for someone doing nothing but standing. At the time, I thought this rapid heart rate might be explained as a result of her lying in bed but, since she had been a little more active recently, I doubt that was the cause. I then proceeded to take Amy’s blood pressure for 10 minutes and this is what I found.
| Time in
minutes |
Left Arterial
Blood Pressure, mgm mercury |
Heart rate
bpm |
Amy is standing 2 inches away from her
bed, not talking and trying to stand still. I am sitting immediately in front of her to catch her should she fall or collapse. |
| In bed | 109/76 | 88 | Lying prone |
| 1 standing | 118/79 | 105 | Standing at attention, not moving or speaking |
| 2 min. | 105/82 | 110 | |
| 3 min. | 118/80 | 118 | |
| 4 min. | 124/81 | 129 | |
| 5 min. | 144/73 | 128 | |
| 6 min. | 124/85 | 133 | |
| 7 min. | 123/81 | 130 | |
| 8 min. | 61/30 | 81 | A precipitous fall in her blood
Pressure occurs. Amy loses consciousness and she falls onto her bed. I lift and massage her legs and she regains consciousness within15 seconds. |
| ? | |||
In other words, on an across the ocean SKYPE interview: it took 20-minutes to suggest the diagnosis of Hand, Foot and Mouth Disease (HFM) and 30 seconds looking at the photographs the mother had taken and already shown to the doctors, to confirm the diagnosis of classical Hand Foot and Mouth disease.
Then at Amy’s home it took a bit of kibitzing, a 10-minute examination and no expensive equipment other than a classical sphygmomanometer (blood pressure cuff) and stethoscope available in every physician’s office, to diagnose a classical dysautonomia and to definitely classify her with POTS (Postural Orthostatic Tachycardia Syndrome). It is my belief this is a measurable injury of the insular cortex area of the central nervous system area which is one of the areas regulating blood pressure, heart rate and normal peripheral artery contractibility. This simple history and examination explained Amy’s illness, also her repeated falls and short losses of consciousness which, along with the classical (HFM) mouth lesions, had been erroneously dismissed as a psychosis
Let me repeat this since it is important in diagnostic medicine: In my experience with SPECT brain mapping, patients with dysautonomia demonstrate a significant hypo-perfusion injury to the Insular Cortex area, easily documented with a SPECT brain scan and appropriate Segami Oasis software. I believe this typical dysautonomic injury was what the physicians had misdiagnosed as a seizure.
What is Missing?
We require viral proof Amy’s illness was due to hand foot and mouth disease caused by one or more of the viruses listed above. It could have been performed easily at the beginning of Amy’s illness. Why wasn’t this done by any of her physicians? Really, there is no excuse.
The UK has some brilliant enteroviral research centres including (1) St. Thomas in London, (2) Oxford University, (3) Leeds, (4) European Centre for Disease Prevention, (5) Edinburgh, (6) Reading, and the list undoubtedly goes on. There is no indication Amy’s stools or gastric mucosa were ever tested for enteroviruses. There is no indication a routine HMPAO brain SPECT was done to diagnose Amy, which would indicate if the brain and insular cortex had suffered injury. This could still be performed if HMPAO is used. There was no gastric mucosa biopsy to demonstrate chronic enteroviral infection. This still could be done. A normal MRI or CT scan doesn’t show physiological brain injury. These only demonstrate gross anatomical damage, not micro-vascularization and neuron injury.
It is not good enough to say these tests are invasive. This is just an excuse to not do what is necessary to prove a diagnosis and advise the patient and her family correctly. In addition to the brain SPECT it wouldn’t hurt to also do a 3 tesla MRI/MRA of the brain to rule out any other CNS injuries caused by or associated with this infection. At times in adults there is an associated vascular pathology localized in the same area. (MRA is a magnetic image test of the brain’s blood vessels.)
The only good news is that Amy is young. Given time, she will slowly improve and hopefully get back to school to achieve great things. If she were in her twenties to forties, after two years there would be a lower chance of significant recovery. In adults, untreated chronic disease can cause its own permanent disabilities. In children, depending upon the degree of injury, this is less likely to occur. Because no appropriate tests were done we do not know the extent of the injury.
Amy also represents a typical severe case of Myalgic Encephalomyelitis (M.E.), a significant central nervous system hypo-perfusion injury causing major cognitive and administrative brain dysfunction. Every one of my M.E. patients have a significant and usually severe hypo-perfusion injury of the left anterior temporal lobe, and particularly the area known as Brodmann 38. But once again, no diagnostic brain SPECT was ordered for Amy.
Unfortunately, M.E. is a severe CNS illness dismissed by too many physicians. Amy also represents a typical case of Myalgic Encephalomyelitis, caused by the same enteroviruses that caused Amy’s Hand, Foot and Mouth Disease. This is not simply a criticism of UK physicians, it is a diagnosis missed by too many physicians not just in the UK but in much of North America and Europe.
This is a typical story of Matryoshka Dolls, one puzzle inside another, explained by the following equation:
Acute Illness + Enteroviral Infection + Hand Foot and Mouth disease = Chronic brain hypoperfusion injury of the temporal lobe and limbic system M.E. + Dysautonomia
Amy’s illness might be viewed as a typical and dangerous case of child neglect, not by the parents, but by the British medical community that was supposed to serve her best interests and the best interests of all children and adults in the United Kingdom
It is obvious Amy cannot go to any school with untreated POTS. Although she could have good home schooling provided by the state, it has not been provided. My assessment of the mother and children is that they are all of above normal intelligence but that neither adequate medical assistance, nor educational assistance has been provided for Amy. The family only required normal and correct medical help, a simple history, a simple medical examination and a basic knowledge of infectious disease by her physicians. Yet this normal care was not delivered, by the medical health services and the 14, perhaps too busy, physicians who failed to properly take a history or to adequately examine this child or to come to the correct and obvious diagnoses.
The question remains: why did Amy’s multiple physicians fail Amy? Some U.K. patients believe that British physicians are obliged to follow a quota system and must see too many patients each day. I don’t know if this is a valid belief. Britain has great physicians but obviously mistakes were made.
Further Notes on the 6th of March 2010 Meeting
The Westminster Talk to the Committee of the House of Commons and Lords.
Myalgic Encephalomyelitis (M.E.): M.E. is not a myth. It was investigated, very well described and championed by many brilliant physicians, including the following:
- Sir Donald Acheson, KBE, who was the late Chief Medical Officer of The United Kingdom, (1983-1991)
- Alexis Shelokov in the USA, a co-inventor of the Salk polio immunization and Director of Vaccine Research, and member of the President’s White House Scientific Committee and by
- Melvin Ramsay who supervised the care of the nurses, physicians and health care workers who fell ill with M.E. at the Royal Free Hospital in London during the combined polio and M.E. epidemic in 1955
The cause of M.E. is not a myth. In the over 60 documented epidemics of Myalgic Encephalitis, the only causative viruses recovered, were enteroviruses. The majority of M.E. sporadic cases occur from June to December, the same period when enteroviruses do most of their harm in the north temperate zone. When known, in M.E. and paralytic polio epidemics the lowest incubation period tends to be from 3-6 days.
M.E. is not a myth, nor is it Chronic Fatigue Syndrome. M.E. is a well-known epidemic and sporadic enteroviral disease that prior to the invention of polio immunization in 1955, tended to occur at the same time and in the same location as paralytic poliomyelitis. M.E., like polio, is a biphasic enteroviral disease, acting much like the three enteroviruses known as polioviruses.
They enter the body through the gastric tract (GIT), then spreading to the entire body but specifically to the central nervous system or to the heart. However, whereas polio primarily injures the brain stem and spinal cord causing death or paralysis and to a much lesser degree an injury to the brain itself, the several M.E. enteroviruses noted earlier in this paper, tend to primarily injure the brain above the brain stem causing a variable chronic encephalitic condition.
To a lesser extent they also injure the brain stem and spinal cord. This variable chronic brain injury of M.E. depending upon where and how severe the brain injury may be, can scramble and disable the brain’s memory, retrieval, processing centres, pain and balance centres, and in worst case scenarios, the autonomic nervous system.
Chronic Fatigue Syndrome: CFS is in many ways a non-disease. It was reputedly the invention of the late Dr. Stephen Straus of the National Institute of Health in Bethesda, Maryland. When I was invited to speak to the House of Lords and Common’s committee, I noted that Chronic Fatigue Syndrome or CFS had such a multitude of changing diagnostic criteria due to the fatal errors in this original first Straus definition.
Dr. Straus’s ideas were published in 1988 as: Chronic Fatigue Syndrome: A Working Case Definition. The definition was based upon the erroneous view that the Lake Tahoe M.E. epidemic in August of 1984 was an epidemic illness caused by Epstein Barr Virus (EBV). (EBV is the primary cause of what is called Glandular Fever in the UK and in North America called Infectious Mononucleosis.) To attest to the perfection of the Straus definition, 16 eminent “physicians” and researchers signed this document published in the Annals of Internal Medicine. Curiously, the majority of the 16 were not physicians, nor had the majority ever seen any kind of patient and more specifically, with few exceptions, had never seen a patient with the so-called Chronic Fatigue Syndrome.
Stephen Straus, the reputed inventor of this term, was also (1) one of the three secret peer review members of the renowned and excellent New England Journal of Medicine and also (2) the chairman of the NIH money-granting body overseeing CFS grants. As a member of the peer review he blacklisted the excellent paper by Dr. Dan Peterson et al, one of several physicians who had first-hand knowledge of the Lake Tahoe epidemic. I believe well over 40-60 million dollars was then dispensed to many of the 16 members who first signed Stephen Straus’s definition and to his academic friends.
Tragically, if a researcher didn’t support the Straus faulty definition, they received no NIH grant. I believe a whole lot of scientific misinformation then occurred in order to first obtain grants but ultimately to actually invalidate their findings, since no such disease exists. The first signatory of the definition, Dr. Gary P. Holmes, was a PhD student at the Centers of Disease Control and Prevention, (CDC), who then left to practice medicine in Texas, and as far as I know received not a penny. Why? In 1987, Holmes produced an honest research paper essentially stating Steven Straus’s theory was erroneous and EBV had nothing to do with the epidemic in Lake Tahoe. This caused Dr. Straus to blow up in my presence on receiving the news of Holmes’s publication. Holmes then immediately left the CDC and for all practical purposes never again looked at the mythical “CFS.”
CFS doesn’t exist but represents many undiagnosed, serious debilitating diseases that have not been diagnosed adequately or at all. Some of these desperately and chronically ill patients have M.E. Some have one or multiple missed significant illnesses. Too many have been falsely dismissed as psychiatric patients or anxiety neurosis. Rarely are any psychiatric patients. Like Amy, they too are in need of care.
Meanwhile, the wonderful Amy Brown, lies at home, not abandoned by her family, but abandoned and misdiagnosed by her physicians and unfortunately, also by England.









Very powerful. Thanks Cort. I agree that there are subtypes but the research does seem to be indicating that the illness+metabolic syndrome+autonomic dysfunction+auto immunity deserves its own moniker. Most chronic diseases have subtypes where only genetic, bacterial or viral diseases enjoying causes that are easily denominated. For example Alzheimer’s is linked to diabetes. Arguing for the label of CFS to be taken seriously would seem to be the best way to get the type of testing he wants to then identify components done.
Very good point Chris.
I’m not sure where Hyde stands on whether CFS always or most of the time represents a missed diagnosis. (Sometimes the way he writes suggests that he doesn’t always find another diagnosis) but losing the CFS moniker would stop research into it (!).
Hyde is essentially agreeing that most of the time (all of the time?) ME/CFS is a wastebasket diagnosis – perhaps because there is no diagnostic test.
The real problem is how do you treat the infections. Currently, I have a bronchial infection that won’t go away. After trying anti-biotics that made me feel worse, I have decided to try high dose vitamin-C therapy – up to bowel tolerance. I would prefer to do it by IV, but there is no doctor locally who will. So getting back to the gut and enterovirus. A friend of mine cured her CFS by doing Chlorine Dioxide enemas which is still on my bucket list. Anyway, I am using this latest infection and anti-biotic prescription to work on Ken Lasessen’s ME/CFS model by using different probiotics and herbs. My past experience with that has not worked, but try, try again. One more thing for the readers to consider and Ken also recommends is Niacin. I suggest 500mg 3x a day for a few months and see if it helps. It has been used to treat depression and has helped people with Ulcerative colitis recover when done as part of an enema. Its important to check you liver enzymes every 3 months, but 3000mg a day is not uncommon as dosage for certain conditions.
agree with you on the “cfs” thing at this point. We need things to move forward and actually need the stupid moniker as its known….maybe me/cfs is better but honestly we can’t afford to quible over the name anymore. We have to keep moving forward with everything we have got. I do love Byron Hyde and think he has alot of excellent research and understanding of the disease but lets move on from the name debate….just my opinion.
My thanks for the great report.
I was just thinking about the Rituximab trials and I got an idea, based on an uneducated guess, as to what could be happening:
Assume that CFS/ME is a virus in the B cells and CNS. Rituximab kills off the infected B cells, but patients are still sick because the virus is still in the CNS. Then, gradually, new uninfected B cells are generated and they kill off most of the virus in the CNS, causing remission. Gradually, however, the new B cells are themselves infected and rendered impotent and the patients relapse. The explanation for why severely ill patients get no relief could be because their B cells are quickly infected by the virus as soon as they are produced, since their CNS is so overloaded by the virus.
A possible cure would be to develop an anti-viral that would target the virus in the B cells so that they could keep working effectively.
My one year old grandson became infected with HFM Disease in 2015. This was “common” in central Florida according to his babysitter. Local doctors miscommunicated information such as “adults don’t get this” and “adults don’t get a rash”. My grandson started head banging and eye poking behavior in immediately after the virus started clearing up. I noticed regression in his mental development. This lasted close to a year and now at age three has subsided. He occasionally shows agressive behavior not present prior to the illness.
I contacted the CDC to ask for information on HFM Disease and was given no credible information other than their website stated it was “mild” and often asymptomatic.
Along with my grandson, I at age 64 I became very ill with severe headache, decreased mental function, rash and fever and afterwards trigeminal neuralgia. I cannot imagine a child being ill with this horrible virus. I wondered if the headbanging behavior was in response to his having a headache. A vaccine needs to be made for Coxsackie virus. The CDC must ackowlege its severity.
I have had CFS for many years after EBV, CMV contracted while working in a hospital’
I wonder if its better if one does not have M.E. since except for Dr. Chia’s equilibriant or some powerful and not always effective immune drugs that can have serious side effects (interferon), I don’t what people can do for enteroviruses. I was struck by the fact that Dr. Hyde suggested that given Amy’s age that she should get better over time on her own.
Having three of the things listed here (POTS, Ehlers Danlos, APS) I can relate completely. Sadly it took me to be in my 40s before I started getting correct DX. The most recent my being in my mid 50s. Also my sister and I both got what appeared to be polio after a vaccine at the early age, for me, of 8. This has been lifelong and it’s not going away. I think we were genetically predisposed to things and had possible epigenetic changes to activate. Sad there are not more docs like this who will look for it.
Issie
Issie I have Eds type 3 also, i think genetics is involved…at least for some…
I’d had a post-viral/CFS diagnosis for over a decade when I went to a new doctor following the sudden death of my long-time doctor. He changed the correct diagnosis to “post-divorce depression”. The second opinion doctor diagnosed “? depression” and the specialist he sent me to assured me that we would try all 300 brands of anti-depressant until we found the one that worked for me. He prescribed something I’d previously had a bad reaction to and been told not to take, and when I pointed that out to him, he refused to change the prescription, repeatedly arguing “it’ll be fine.”
A couple of days later I was talking to a doctor from another medical group, who pointed out that because I was single, my malpractice claim would die with me; they were more interested in protecting their colleagues from a lawsuit than in getting me proper treatment, and were willing to go to the extent of prescribing something that would kill me.
If I took what they prescribed, I’d be dead. If I didn’t, they could vilify me as non-compliant.
I found a new medical group.
Glad you got out of there…
Thanks, Cort.
Thank you. (Pat was the one who showed me Dr. Hyde’s report.)
Cort, thank you for this remarkable account. I can identify in so many ways. I don’t want to go on and on, but I too, was sidelined by so many doctors who could not explain my pain and fatigue and additional symptoms. I got tossed into the fibro/CFS/ME wastebasket with nary a history or full body exam–for decades. In fact, with a recent noticeable increase in fatigue and unintended weight loss, my PCP ordered a CBC and after it came back ‘normal’ pronounced me ‘fine.’ She suggested that my increased symptoms were from ‘stress.’
Not wanting to let the matter drop, I continued to seek medical help and now have found I have endometrial hyperplasia–and possibly the beginning of cancer–not just ‘stress.’
Because medicine is so driven by economics, I have found the necessity to ‘become my own doctor.’ Not convinced that my past Dxes were fibro and CFS/ME, after hours and hours of research I came upon EDS, and fortunately maneuvered into getting a geneticists appointment (it wasn’t easy). Correct!
Unfortunately, doing all this research has made me realize how much medicine doesn’t know–while making us, as patients, believe that it does.
Thank God for the Internet! And people like you, Cort, who take the time to bring research to the patient community!
I still believe that medicine has a long way to go, and am also skeptical that Dr. Hyde’s viral hypothesis can explain everything–but we do need more curious and thorough doctors like him!
There’s the problem — if blood tests are normal, the doctors will pronounce you “fine” despite your reported symptoms. No interest in doing more blood tests to find out what’s wrong.
One doctor did a bunch of blood tests that SHOULD be normal with CFS (because I don’t have lupus or diabetes or thyroid) and that was enough to convince him that I was faking. I suggested tests that should be abnormal with CFS, and he just kept arguing that the first bunch were all normal, therefore there could be nothing physically wrong with me.
I tried to get into a clinical trial for fibromyalgia, and they did a not-previously-done blood test, which was so high that “it must be lab error” so I had to go back for another blood draw, which would be sent to another lab. The first one was 9x normal, the second was 10x normal. When they called to tell me I was too sick to be in the trial, the subject turned to if it was 10x normal on a day that I was able to take 3 buses and a hike to get to their office, how high must it have been a couple years before when I was effectively bedridden?
The good news is, I now have proof that I’m not faking, there is something physically very wrong. Even if doctors still aren’t sure what it is or what to do about it.
It scares me to death how often doctors ignore or dismiss symptoms because they can’t figure it out.
I have ME/FM and recently had surgery. For some reason all the doctors thought my much increased BP and pulse while laying in bed hardly moving was “normal”. No, normal for me is max 110/70 and resting pulse is 70. In hospital my BP was 148/96 and pulse 118 again while I was resting and still, how in anyone’s mind, health practitioner or not, finds that normal!! I was sent home in a snow storm in that condition, and not able to take in even fluids. I lost 10 pounds in less than a month. I felt like I was in a factory, just another sheep to push along.
Having worked in the medical world for 40 years and having both CFS and fibromyalgia, I’ve been so disappointed in the multitudes of doctors I’ve worked with and seen personally. The really good ones who try hard to help are few and far between. Sadly I can truly identify with what he describes here. I’ve learned to ask to address individual symptoms, one or two at a time, during appointments and avoid using the terms CFS or fibromyalgia due to the stigmas still attached to them.
Thank you so much for a very interesting article.
There is one thing I have been wondering about for years but to which no doctor or Google-search can give me an answer. Perhaps someone here has a similar experience?
Prior to the onset of my ME (which we believe were triggered by a stomach bug), I received one too many Hep-B immunizations due to an incompetent doctor. My GP was worried afterwards as I had too high a count of hep-B (??) in my blood and he kept checking my blood for a while until it went down. 14 years later when I finally got the ME-diagnose there were no longer any antibodies in my blood and hence the neurologist thought I had never been immunised. She could not explain how this can be the case, neither can any other doctor. Does anyone here know why or have a similar experience ?
Hepatitis B vaccine as a possible culprit–does Dr. Hyde or anyone else suggest ways to counteract it, after it has taken effect? (In my case it was not the initial cause, but my symptoms worsened when I had “flu” a few weeks after the vaccination and did not recover to my pre-flu condition. Previously, I had mostly recovered from “flu” several times.)
Strangely, that’s similar to me. Due to a lapse in follow-ups, I had two jabs and missed the third. Years later, I had two more on separate occasions. It finally seemed to work, but something was up. I caught shingles at 22 and I knew then my immune system had been compromised.
It started with an idiopatic hypersomnia, then, i’ve been diagnosed with ME/CFS following 10 years of not being able to overcome atypical infectious mononucleosis.
My specialist doctor at sleep study center manage to keep me « functional » by using 70mg/d of Vyvanse and 15mg/d of Dexedrine. The risk/benefits of taken these meds worth it, because without it, i would be completely bedridden.
But could it be harmful in the longterm to keep functioning with borrowed energy ? Cause I can feel that my energy is synthetic and always were off. And with stimulant, it is easy to push over my capabilities, then end up crashing. Not to say that one day without them sends me directly into a crash and imbalances.
My GP looks like she never know what to do with me, it’s also seems like she often did recommandations that could have been possibly more harmful then doing nothing. She also dismiss most of my symptoms saying that those are normal symptoms for ME/CFS patient, and rarely seek if it’s really from my CFS Dx.
Also, she referred me to go and re-do my hep B immunization because recent bloodwork showed I wasn’t immunize anymore even if I already had all my shots. Should i go on with her recommendation or would it be harmful to do it ?
For a better background, actually i’m 27 y.o. and got sick since I developed an infectious mononucleosis in 2009.
The most important information I’ve taken away from this is that well under 1/2 of people who think they have CFS think they’ve had extensive medical testing! I think it’s imperative that only people who have had extensive testing should be participating in research on CFS.
More important is to define what “extensive testing” is. I’d prefer not to rely on subjective “beliefs” of what extensive testing is and is not.
Ultimately you are correct. But if a person doesn’t “feel” he’s had extensive testing, he should be looking for answers in places other than a CFS diagnosis.
Agreed. That’s a great question…What constitutes exhaustive testing for Dr. Hyde?
This story is way too long. As a patient, I mostly interested in new finds of diagnostic methods, and treatments.
It is very long! You might try the print button at the bottom of the page and print it out and read it in parts
Sometimes the truth takes a long time to explain. Without the truth you can have no new diagnostics or treatments. In this story many doctors failed to help the patient because they thought a thorough exam would be “way too long”, or their bosses thought so. If you are always in a hurry you are likely to miss the truth of illness, diagnostics, treatments, and almost anything else at all that matters in the universe.
Great article! I hope every doctor and politician reads this.
As my husband is a pediatrician I always have the suspicion that maybe he brought home a virus from the hospital he worked on, to which he was somewhat immunized from being in that environment.
When I finally was directed to the local CFS expert, the nurse and I recognized each other from riding the bus together.
Since no one I knew had CFS, the eternal question has to be whether she transmitted the virus by giving me a mint or a Kleenex from the pocket of the sweater she wore all day at the office.
Great work Cory
I am Irish and fell ill at same time as polio outbreak in our area in 1960 aged 12 yrs so facinated about possibility of polio virus causing my problem. My mother would not help me with exact timing but she did move from the condemned primary school September 1960 so that says something
I’ll now for 57 years
I fell ill suddenly with neck and chest pain and a high fever in 1978 while nursing in a childrens ward. I was hospitalised two weeks later seriously ill in the same hospital with viral pneumonia and pleurisy. Blood tests were taken and confirmed Coxsackie B infection. I was sent home and recall being barely able to move with weak muscles.
Six months later I was rehospitalised with “post-viral depression” and given anti depressants.
Thus began a journey of 10 years in the wilderness consulting at least 20 doctors and physicians. I was exhausted, semi-bedbound(having 3 young children) had to cope.
My heart rate was constantly above 120. I was referred for cardiology testing but none confirmed anything but inexplicable tachycardia so I was sent home.
After 10 years a nurologist confirmed ME as a diagnosis but did not do any further testing. At least this put my psychiatric diagnoses to bed!!!!
22 years later at age fifty I went into heart failure and was diagnosed with cardiomyopathy after another three cardiologists dismissed my symptoms as nothing for a woman of my age.
I am in Australia and now finally I do have a physician who takes me seriously and has been working to achieve optimal wellness for me. It is now 40 years since I fell ill.
What a difference a vaccine for Coxsackie virus would have made Cort!
No kidding Maggie…My gosh, what a story. I hope that your doctor is helping…
PS my three young children developed Hand & foot and mouth disease and were diagnosed quickly by our GP. I do not recall now if this event was close to the time I fell ill but may have been as all were between 2 and 6 at the time. Interesting thought!
I nursed child polio patients in 1948 & also during a severe spinal and bulbar epidemic in Nairobi in 1957/8 during which we were given the original Salk Vaccine. Also seriously ill in Singapore diagosed with Encephalopathy. I found this article compulsive reading. It is obvious that some viruses remain lurking in their favourite places in our body, often causing the immune system to be on continuous red alert. Can we please omit the CFS from our terminology? Chronic fatigue is rightly applicable to many diseases and well named ‘a waste basket’ diagnosis when applied to ME.
I have had ME since 1980, not as bad as it was but still at times rather like running into a brick wall. Thanks to Dr Hyde for being a free thinker and Cort for the contuing information.
Thank you for sharing this story! I read one of Dr. Hyde’s books some years ago, after gettting ME/CFS symptoms and appreciate all he is doing to help!
Glad to hear he is still working and helping patients.
Thanks so much, Cort, for this article and the video of Dr. Hyde! He has specialized in careful diagnostic workups and recommendations for exact testing, both to establish diagnoses as well as to establish disability for legal purposes. He works with international as well as Canadian patients. I have long respected his very intelligent and independent perspective though the whole story on ME/CFS is still
emerging.
As a patient, I find more openness and respect now among my available physicians who still have no training in “ME/CFS”, to try testing and treatment protocols that they consider reasonable, but this is still an uphill effort as it continues to put the burden on patients to try to educate and direct their doctors. I imagine that others of us who go to the few specialists in our field still have this problem in that these specialists are interested or knowledgable in working with only some particular perspectives and aspects of this illness. I have heard that some patients feel they need to go to several different ME/CFS specialists for different aspects of treatment.
All this is to say that while knowledge is accumulating in its patchwork fashion, I only wish that our doctors and researchers would get together and collaborate more, so that our days of neglect and mistreatment, then attempts at finding knowledgable helpers, or our fervent efforts at educating ourselves and our doctors, could come into a state of integration and a better way forward.
I’ve gone to several IACFS conferences, and I can assure you that the researchers are sharing info.
The problem is that the average doctor won’t go to an IACFS conference to learn anything. The last time it was near here, I offered to pay my doctor’s registration fee (or for his physician’s assistant) for the one-day patient conference [we get the same topics as the doctors, just in abbreviated form so it can be crammed into a single day instead of two or three days], and was turned down because he “didn’t want to become the CFS doctor”. He’s CFS-friendly, believes I’m really ill, but most of what he knows is because I taught him. He does seem to read when I send him a printout of my notes from the conference.
And with the stigma, I suspect that’s why most doctors won’t go to an IACFS conference to learn anything — they don’t want to ruin their professional reputation by becoming the go-to guy for a disease their colleagues don’t believe.
There’s also the issue that many of our patients are on Medicaid, which doesn’t pay doctors well; they’d lose a lot of income if they switched from employed/insured patients to treating a lot of disabled people.
I had ME for a year after influenza A in grad school (which lead to aseptic meningitis and a year of being ill), but I recovered and spent 10 years in fairly good health until I got sick on a trip to Japan in early December, 2012. I never recovered and a month later, woke up with arms and legs paralyzed (after which, ME symptoms occurred and worsened over the years). My ME/CFS specialists both thought reactivated EBV could have caused both the aseptic meningitis and temporary paralysis (I’ve been tested for “known” enteroviruses commonly associated with ME, and those antibody and PCR tests were negative). My question for Dr. Hyde would be this: if a one-time enterovirus injury to the brain occurred, rather than an ongoing disease process, wouldn’t one be able to recover reasonably well with time, such as stroke or brain injury patients? I know TBI can cause people long-term problems, but three people I know who suffered moderate strokes or severe head injuries in 2013-2015 are all doing much better than I am, and I have done fairly extensive neuro-rehab.
Wow! Dr Hyde makes so much sense. The heart/pulse rates are interesting because recent research indicates that the heart works ‘overtime’ when people with this illness were upright. That would explain the extra strain on the heart and the constant feeling of imbalance. It would also explain why I still experience what is termed as ‘low grade fever’. I instinctively felt that this was my immune system still fighting ‘something’.
Perhaps research should now concentrate on finding a way to get rid of this virus.
Wow. Thank you Cort and thank you Dr. Hyde. We went through something very similar in 1986 with our son, then age 6. A doctor outside our HMO found titers suggesting recent EBV infection, but the HMO docs did not or could not consider this. He had a 104 fever for a week, then had terrible irritable bowel, urinary frequency -40 pees a day, pain in fingers/toes, nighttime hunger, sleep problems, depression! ( had been a very happy child), had learning issues and had an IEP. Had panic attacks. Wow. The doctors said he just needed more attention, but I was a stay at home Mom.
Two of his friends had something similar, but much milder. Finally around age 10 he started to improve. I begin to wonder if this was EBV virus or an undiagnosed enterovirus?
What a nightmare for parents. Who has had a SPECT scan???
I love Dr Hyde and all he is doing and has done to help patients. I do fit the description of m.e. pretty perfectly only I got in in jan 10 years ago, still remember the day. My diagnosis is technically fibromyalgia and I would bet a good lot of us with m.e. have their official diagnosis as fibromyalgia with an ever growing list of other oddities and ailments….the thing is though,most all of us do not have access to fantastic and knowledgeable/caring drs. like Byron Hyde, so though it greatly pains me to say this, I do not think we can afford to argue over the name “m.e. or cfs, BECAUSE we need some help and there are not many doctors who will even write cfs down even if you are told to your face they believe you have m.e. and have actually read “Oslers Web” (this has actually happened to me) So, is it right to be in a nameless state of diagnosis for many, when at least they might learn to help themselves if they fit the m.e. pattern. I don’t think so. Being believed is HUGE especially when one is so ill. Yes, we need more Byron Hyde type drs, more curiosity, more appropriate tests, in all my years I have never gotten a pet scan. why? but finally i have some other added uglies like chronic migraines, occipital nueralgia,b12 defficiency, vit d defficiency,IBS/chronic stomach inflammation of “unknown origin” and peroneal nerve damage which may or may not get worse so i have foot drop(apparently this is probably within my control as I must be doing something like chronically crossing my legs, I’m not and I don’t) It just gets so old, I think until there is more of a united front ,we have to go with whatever diagnosis we can get within the limited finances,time and energy levels, ability to travel, etc…etc…we have. I just think, though i hate the name cfs, we have to consider that there are alot of people out there with m.e. who really have their clinical diagnosis as fibromyalgia or perhaps cfs…i find drs right chronic fatigue down willing ly but they don’t want to have their name near the “syndrome” part. SIGH. Too bad Dr. Hyde can’t clone himself and be available to us all.
Fyi Dr Naviaux released new research into autism and the cell danger response a day or two ago. The drug suramin reduced the symptoms of ASD for a short period in kids with the condition.
This is great news. I wonder how many of us have kids on the spectrum or with ADD or ADHD? Anyways, anything that helps children get correctly diagnosed (and helps) is great news
This article made me cry. I SO wish I had competent help. I’ve been sick since 1996 and have never had any kind of a full workup or exam done by anyone.
I thought I had had good testing done, until I read this article. I have been sick since 1996, and had “every test we can think of” I had never even HEARD of most of the tests Dr Hyde recommends. Guess I haven’t been tested well. Lord only knows what is actually going on with me. The more I learn, the more I realize how little help I have been given. I too got the “psychiatric” diagnosis (turns out the antibiotic I was on for too long causes hallucinations, especially when the antibiotic is for a severe sinus infection with incredible vertigo, add some intense hallucinations to that, and it’s hard to feel sane, and easy to accept their diagnosis) and got sucked down the rabbit hole of the psych meds making my health worse, I got more frustrated and depressed by it all, which proves I’m crazy, you know, and in need of more meds…
What I have worked out over the years is it’s more than one thing, some is structural damage from a bad car wreck, some is an infection and it’s fallout, some is damage from excess medications, some is due to other old damage. Everything interacts and the complexity is amazing. The thing I have learned to do for it are a bizarre balancing act, this will trigger that which triggers that, so I HAVE to avoid the this even if it’s “not socially appropriate to do so”. The mix is a mess, and doctors look at me and say “Mess! Must just be crazy! See? Does weird non-appropriate things and claims it helps!”
Sigh. I wish there were competent doctors I could find who had a clue, and had a solution. I’m SO tired of doing this alone, after being damn near killed by the medical profession, I don’t trust any of them. Add “paranoid” to my psychiatric diagnoses list…
Yes, Rachel, I think you are on the right track. Many people, including researchers, conflate meditation, mindfulness, and relaxation. These should be carefully defined and distinguished. The type of meditation that I teach and practice is usually known as mindfulness meditation, and it is taught in Mindfulness-Based Stress Reduction and Mindfulness-Based Cognitive Therapy (and also other similar interventions for eating disorders and treatment of addiction). This type of meditation is NOT a form of deliberately induced relaxation. This does not mean that deliberately induced relaxation is not a good thing… it certainly can be a good thing. But it is a different kind of “good thing” than mindfulness meditation. Certainly there are better ways to induce “relaxation” than to have the person sit upright and very still, engaged in the mental work of focusing and re-focusing attention, noticing and labeling all phenomena that arise in the mind… At the same time, the training engages the mind in practicing a compassionate stance toward all phenomena… so perhaps it would be best described as mental practice in attention and compassion (or acceptance, or non-reactivity, these are all closely related).
faux bague bulgari http://www.aluxury.nl/fr/
I would love to hear more!
It is nice to see recognition of Dr Hyde’s hard work. However, Dr Hyde is my Doctor and you have failed to mention the most important issue that Dr Hyde advocates.
Myalgic Encephalomyelitis is not the same as CFS
ME must show inflammation in the brain & Spinal Cord for diagnosis
CFS does not require inflammation for diagnosis so no testing for inflammation has been conducted.
CFS as per Fukuda 1994 and SEID 2015 does not require brain & spine inflammation. If a patient has been diagnosed with CFS using these American Criteria and this is what American Doctors use then there has been no tests run for Inflammation. American research uses the Fukuda 1994 and lately have added Jason 2010 (no inflammation tested). When Fukuda/Jason research finds inflammation there has been no prior testing of participants to see if they had inflammation prior to the research. Patients with ME are misdiagnosed with Fukuda or SEID so the researcher has no idea if any or all of his participants had CFS or ME from the beginning. ME needs to be ruled out before diagnoses of CFS. It is especially important in research because mixing the 2 together has created decades of insufficient treatment.