(The metabolomic findings in ME/CFS and reports that high carbohydrate foods have a sapping effect suggest that ketogenic diets – which increase fats and proteins and severely limit carbohydrates – may make sense in ME/CFS and fibromyalgia. Thanks for Lori for allowing Health Rising to publish her ketogenic diet success story. Lori is not well yet but she is greatly improved. As with every recovery/recovering ME/CFS/FM story please note that these are heterogeneous disorders and that your results may differ.)
Lori’s Story
I just could not get on top of my fatigue. When the doctors couldn’t convince me I was just getting older they diagnosed me as depressed. Lori
Beginnings
In April of 1996, in the seventh month of pregnancy, I was put on bed rest for pregnancy-induced hypertension. I was a full-time registered architect, healthy I’d been preparing for pregnancy for a year with a normal level of stress.
The same week – four states away – my mother was diagnosed with cancer.
An only child, father long deceased, the next year and a half ended up being blur of caring for a nursing infant and traveling back and forth for Mom’s surgeries and radiation. In the middle of it, I came down with a virus that hit my infant son as well. I remember him bundled on my chest, sleeping in my childhood bedroom in a recliner since neither of us could breathe lying down.

A day felt like a 20-mile hike with a 50 lb. backpack, with a toddler. On occasions my knees would buckle, unable to keep me upright simply walking across the room. Naps were mandatory, but non- restorative.
The Big Relapse
Three years later, I was beginning to recover. After my son went to preschool, I went home and slept. We were able to manage a short family vacation. Then my son ended up in the hospital with complications from a tonsillectomy. The day we brought him home from the hospital after a week of sleeping (badly) on a window seat next to his bed, I found out I was pregnant.
I cried. I was exhausted and could not imagine getting through another pregnancy safely. As fate would have it, I miscarried several weeks later.
The cycle continued, however, I just could not get on top of my fatigue. When the doctors couldn’t convince me I was just getting older they diagnosed me as depressed. Antidepressant therapy did help, but if it somewhat brightened my mood, it was no help for the fatigue and inertia I was experiencing.
I had not practiced as an architect since my son was born, but I had at least kept up my license and continuing education. Now I was forced to put myself on inactive status because I couldn’t understand the technical information I was required to study.
After a minimal pass at vacuuming and cleaning the bathroom in preparation for a childhood friends visit, I spent the next day in a rocking chair, attempting to will myself to verticality. I began to have flares of pain in my arms and upper chest – so tender that shifting the covers to turn in bed was excruciating.
I am extremely fortunate to have a husband who knew me ‘before’. Although he did not understand what was happening, at least he supported my attempts to find a solution. Even if my cognitive processing had slowed dramatically I was still an information junky at heart. I started digging online and ordering books through the library.
I visited a holistic clinic and met the first health professionals who actually *believed* my issues rather than dismissing them. I learned about adrenals and hormones and supplements and met people who had been living with this so-called ‘chronic fatigue syndrome’ for a dozen or more years. That seemed like eternity.
1-Percent Solutions
I committed myself to what I called “1-percent” solutions. If something might help, I’d give it a shot. If I noticed improvement, I kept it going. I participated in a double-blind trial of an anti-viral for fibro. A clinic focused on chronic fatigue and fibromyalgia opened 6 hours away, and I finally had a slew of medical testing that documented a host of potential problems, which were addressed with supplements and medication. I tried Xyrem but eventually stopped.
I settled into an existence that at least did not include any new major setbacks. If I guarded my energy – and I certainly did – I could make it through a well-planned week. Near-daily naps of 3+ hours were critical, as were at least one weekend day in bed. Improvements were slow, but the fog was lifting a bit.
The clinic was sold, and with the new fee structure too steep to continue, I limped along on my own. I switched to a local endocrinologist for thyroid medication. Since he could not understand the rationale for my former treatment protocol, my medication changed. Handing my huge file to a new nurse practitioner, her eyes practically popped out of her head, “I don’t know what to do with this!”, she said. At least she was honest.
At this point it became obvious to me that I was probably never going to improve significantly. I knew I was one of the lucky ones. I was relatively ‘high functioning’: I could manage up to a 20-hour work week, and perhaps minimal house work. But if my schedule changed abruptly, even a single event or change of plans, the stress would wipe me out for several days.
Florida’s heat and humidity were miserable as well. Even mental concentration resulted in perspiration, which resulted in dehydration, which resulted in pain, which resulted my sleeping 20 hours at a time.
Help For Sleep
In October-2015 my husband recommended that I see his pulmonologist to schedule a sleep study. I’d had two sleep studies before (which showed “markedly disturbed sleep”), but this study indicated I had a combination of central and obstructive sleep apnea. At long last, I had an auto-pap, a specialized type of continuous positive air pressure (CPAP) machine that adjusts pressure based on ongoing feedback.
I was no longer waking with my heart pounding and a headache when my brain ‘forgot’ to tell my diaphragm to breathe. The hope that the CPAP treatment would set off a cascade of benefits – better more energy and weight loss didn’t materialize. I settled for better sleep.
In early June-2016 I had the opportunity to start swimming. By swimming, I mean ‘getting in cool water and moving around a little’. It was a huge relief to get a break from the misery of Florida’s summers. I could stop perspiration episodes faster, and so, managed to decrease some pain. Sticking to strokes where my arms were even with or below my heart helped. The crawl was out – I couldn’t catch my breath, even at a snail’s pace. The sidestroke, lazy backstroke and a modified dog paddle were my friends. Floating was heaven. At least I was outside.
Even as swimming provided relief, and with 15 lbs. gone from the gentle exercise, my weight was still up to nearly 245 (I’m 5′-10″), 95 lbs. above my lowest adult weight. I was taking two antidepressants and thyroid medication, and I was still having days when I was in bed more than I was out. If I worked, it was in the afternoon because I couldn’t drag myself out of bed until mid-day. And every morning when I woke, I thought that if I felt like this when I was just over 50, the rest of my life looked pretty bleak.
The Nutritionist
In September, my husband came home from a check-up with his cardiologist with a mandate – see a nutrition counselor. “She’ll change your life,” his cardiologist said. When my husband came home from his first appointment, I read the material he was given for the ‘low carb, high fat (moderate protein)’ (LCHF) program he was to try. Before this, if anyone would have said I’d ever give up carbs, I’d have laughed in their face. But when I read that LCHF can be beneficial for inflammation I decided I’d keep my husband company in his quest.
We purged the pantry and refrigerator. Our new limit was about 20 total grams of carbohydrates a day. Within a couple of days, the reflux that plagued my nights was gone. Within a few more days, the pain in my arms was reduced by about 90 percent. Brain fog began lifting. My husband and I went on a vacation and stayed true to the plan the entire time and came home having lost weight (!). Not even a couple of off plan items during the holiday season changed my progression to health.
A Ketogenic Lifestyle
A ketogenic diet has not been a 1% solution, but much, much more. I feel like a whole person again. Lori
By this time, I was monitoring morning glucose and using a breath analyzer for signs that I remained in ketosis – when the body has made the switch from using fuel created from carbs to fuel created from fat. Insulin production, without carbs to induce it, dropped. Having gotten past the ‘keto flu’ of adapting to fat burning by paying attention to adequate salt and magnesium intake, I was now (miraculously!) no longer tempted by carbs, or even hungry very often.
I began a mild form of IF (intermittent fasting), meaning that I stopped eating after supper and didn’t have anything except water or broth until about 9 the next morning. It was a natural progression of no longer needing to eat every few hours. If my body was a fuel truck, it was no longer reliant on the ‘carb’ gas tank’ – my body was drawing directly from its main tank of body fat for energy.
I began waking for the day at 7 in the morning after about 8 hours of solid sleep. And I was up for the day. I would do yard work (YARD WORK!) or whatever else that needed doing, then later have a nice cup of coffee with heavy cream. Later I might have an omelet with sausage or bacon. For dinner we might have roasted chicken (with the skin), and a big salad or broccoli with cheese. I’ve even found a low-carb dark chocolate mousse for special occasions.
An “Exceptional Patient”
Last week I saw several doctors for the first time in many months for most of them. My endocrinologist reviewed my weight loss (down 50 lbs. since last year) and told me I’d made his day. My family practitioner was very happy to see my triglycerides at 70 (rather than three times that number) – she has given orders for additional testing to determine cholesterol particle size as some cholesterol has increased.
Although she’d never mentioned it before (when was she going to tell me I was pre-diabetic?), she noted that my previous 118 fasting glucose has been reduced to 83. I no longer have reactive hypoglycemic episodes. My pulmonologist said I was ‘an exceptional patient’. I have dropped (with the doctor’s direction) down to a half dose of one antidepressant, down from full doses of two medications. I felt like they were sticking gold stars on my forehead.
When I read an article on Health Rising, I was far enough along in my LCHF journey to appreciate the idea that for some of us, the processes that allow our bodies to make energy may be broken, and that alternative fuel pathways may allow a work-around for some of us. That seemed to make sense from my recent experience in changing my eating.
In one of the biggest cliches, I haven’t felt this good since my mid-20s. My belts ran out of loops. I’ve had to replace about a quarter of my wardrobe. When I asked my husband to describe the changes he’d seen in me, he said I had not double or triple increases in energy, but ‘exponential’ increases. I’d agree with that.
Getting Bonked
Since October I’ve done a lot of reading on the science behind the benefits of a LCHF diet. I’ve never been a runner, but during a video describing the differences between athletes on a LCHF regimen vs. those who carb load for a marathon, I learned the word ‘bonking’.
The term is used colloquially both as a noun (“hitting the bonk”) and a verb (“to bonk halfway through the race”). The condition is also known to long-distance (marathon) runners, who usually refer to it as “hitting the wall”. The British may refer to it as “hunger knock,” while “hunger bonk” was used by South African cyclists in the 1960s. It can also be referred to as “blowing up”. Wikipedia
According to Wikipedia, bonking refers to sudden fatigue and loss of energy caused by a depletion of glycogen stores in the liver and muscles. In other words, hitting the wall.
Athletes who are fat fueled don’t ‘bonk’. Since the last two decades for me have been essentially one never-ending bonk, the relief has been incredible. In addition, the presence of ketones in the body has been found to turn off the inflammation response that causes so many problems.
A ketogenic diet has not been a 1% solution, but much, much more. I feel like a whole person again.
May – June 2017 Update
The above was written in February. Since then, I am at a quarter dose of my remaining antidepressant with my doctor’s supervision. I am closing in on 60 lbs. lost and am finally at the 200 lb. threshold.
Inline skates – a reward for crossing the ‘one-der-land’ threshold – stand waiting. I recently returned from a week’s retreat where I had no control over food preparation. Through making good choices only, I was still in ketosis upon arrival home and had dropped an additional pound for a new low. I continue to be pain free.

In June I started to ramp up my swimming to minimum 5X a week (1000 strokes each) and am working at least half time, with a full summer ahead. (The office building we are in will be made into a bed & breakfast, so we will be moving, with a full slate of projects on the books to keep on top of. I love being back at work with my husband.) In addition, I crossed the ‘onederland’ line, having finally gone below 200 lbs. My in-line skates, which I promised myself as a treat for reaching this, are now MINE!!!
Lori
The Free Online Keto Summit Begins on June 15th
The Keto Summit presentations can be viewed free – on the day of the presentation – for all who register. If you’d like to view the presentations at your leisure you can buy the Summit.
Some of the things you will learn include:
- Simple, easy ways to test whether or not your body is burning fat and ketones.
- Things you MUST do properly on a Keto Diet in order to avoid common problems.
- Supplements that can help you get into ketosis (and feel better).
Many Summit presentations are provide practical tips for ketogenic dieters including “Practical Keto”, “How to Interpret Your Blood and Lab Tests”, “Why Water is Critical”, “What to do if Your Keto DIet is Not Working”, “Ketogenic Diet Pitfalls”, “The Myths and Facts of Supplements”, “When to Use or Not Use a Keto Diet.”
- Coming up next – a review of the “Keto-Clarity” book
RESOURCES
Suggested Reading – User Friendly:
- Keto Clarity: Your Definitive Guide to the Benefits of a Low-Carb, High-Fat Diet – Eric Westman MD, Jimmy Moore – “This book includes exclusive interviews from twenty of the world’s foremost authorities from various fields bringing their depth of expertise and experience using this nutritional approach. Moore and Westman clearly explain why ketosis is normal, how this nutritional approach is being used therapeutically by many medical professionals, a step-by-step guide to help you produce more ketones and track your progress, real life success stories of people using a ketogenic diet, and more.” – Check out a review here.
- Cholesterol Clarity: What The HDL Is Wrong With My Numbers? Jimmy Moore, Eric C. Westman – “Within the pages of this book you’ll learn invaluable lessons, including: Why your LDL-C and total cholesterol numbers may not be as important in determining your health as your doctor may think. The undeniable negative role chronic inflammation plays in your health”
Suggested Reading – for the Science-Minded (Technical):
- The Art and Science of Low Carbohydrate Living – Jeff S. Volek, PhD, RD and Stephen D. Phinney, MD, PhD – “Carbohydrate restricted diets are commonly practiced but seldom taught. As a result, doctors, dietitians, nutritionists, and nurses may have strong opinions about low carbohydrate dieting, but in many if not most cases, these views are not grounded in science. Doctors Volek and Phinney share over 50 years of clinical experience using low carbohydrate diets, and together they have published more than 200 research papers and chapters on the topic.”
Suggested Watching (the tip of the iceberg):
Low Carb Down Under (channel)
Inflammation and the Low Carb High Fat Diet
Names for further videos (search “keto” plus the following names):
Stephen Phinney, Jeff Volek, Eric Westman, Thomas Seyfried, Gary Fettke, Tim Noakes, Dominic D’Agostino, Sarah Hallbert, Robert Lustig, David Perlmutter
More Ketogenic Diet Resources on Health Rising
- Starter videos For Ketogenic Diet Beginners
- Getting Clear on Ketogenic Diets (for Fibromyalgia and ME/CFS): A Review of “Keto-Clarity: A Definitive Guide”
- How a Ketogenic Diet Boosted Courtney Craig Out of a Relapse
- A Ketogenic Diet Menu
- Ketogenic Diet Resource Page
- Dorothy Walls and Paul Jaminet Talk on Ketogenic Diets
- Using Cronometer to Create A Mitochondrially Supportive Diet






It’s great that she’s doing so well. But if just going on a high protein low carb diet were ‘enough’ to bring energy and health back to ME/CFS patients we’d be seeing a whole bunch more folk getting better. It makes me wonder if she just had impaired energy production and thyroid issue or a definable case of ME/CFS. There are a lot of genetic mitochondrial disorders that are not ME/CFS.
Actually I think you could say something about every recovery/recovering story. If it was just antivirals, or taking high amounts of iron, or avoiding mold, for some people the right combination of rest and mind/body therapies…we would see a lot more people getting better.
There is not “just going on anything” in these diseases – they’re just too heterogeneous. However, if you haven’t tried a ketogenic diet – it’s probably a good idea to try one…For me it’s not a panacea but I do feel a bit better.
I have a girlfriend who really has improved immensely since being on this diet, but she had also retired from work around the same time, which in itself is a big deal when fatigue is your issue. I found the diet change didn’t help me that much, and may even have resulted in a kidney stone. I am vegetarian and ate quite well anyway, with more ‘good’ fats and protein, in comparison to her ‘typical North American diet’ of coffee and carbs
To add to Cort’s point; I am sure that the ketogenic diet is part of my own success story and others too, but in all cases, it is not the only thing. I have never heard of anyone making significant improvement without doing a combination of several things. Besides the ketogenic diet, I think it is all-important to be doing exercise at the right intensity, as much as possible. It sounds to me like Lori is doing this, if even by luck rather than careful design. Supplementation also is important, and in my case I would have to say that magnesium was highly important, but I needed to keep increasing the dosages, and then it became important to balance other elements as well, using Hair Tissue Mineral Analysis as guidance.
Approx. 70% of the fibromyalgia sufferers also suffer from adrenal glands exhaustion.
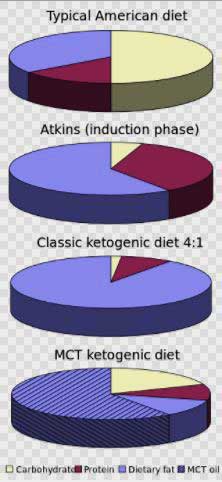
Keto is high fat modest protein and very low carb. Macros are 75%, 20%, 5% respectively. It is NOT high protein that,would be Atkins!
LCHF / structured experimentation worked for me. I am absolutely convinced CFS is a metabolic disorder and that symptoms are essentially due to starvation at the cellular level (bonking … also look up symptoms of catabolism). Driving down insulin by going low-carb high fat makes a huge difference … possibly by stabilizing circulating nutrients. In my case LDHF wasn’t enough. I also avoid processed food, keep to low insoluble fibre foods, low bacterial count foods, and to eat lunch as the big meal of the day, and keep to small dinners early. I only eat breakfast if I am hungry … fasting 18 hours/day is great! Reasonable activity is very helpful and eating is absolutely needed after a bigger workout … yes you can be active .. you just need to eat afterward. Weight loss and not being so hungry was a happy side effect. Figuring out what works and what doesn’t for you is key … individual differences seem to be large … test .. re-test … approach this like you are a baby … i.e you know nothing.
Thanks for sharing that. How are you doing now health-wise?
I’ve had great success with the keto diet as well. There may be a few very simple reasons why more people aren’t reporting positive effects.
First, it’s a pretty extreme diet. I’ve literally had trouble finding enough fat to eat at times. We’re not used to eating this way and frankly, it feels wrong. But if you don’t get enough fat you won’t stay in ketosis. Being on a low carb diet but not in a state of ketosis is hell. In fact I’d say that might be a way to explain to people who don’t understand our conditions how it feels!
Second, she mentioned the Keto flu. Many people have an awful time trying to get into the state and adjust to it. The symptoms could be overwhelming if you’ve already got CFS. I quit the first time I tried a ketogenic diet for that reason. Luckily, if you get enough salt and a couple other minerals you can minimize that.
But once you get a feel for what you can and can’t eat, it’s incredible. My PEM is still present after nearly a month on the diet but I’m returning to work 1/2 time. I can feel my strength building. I don’t know if my body will be able to fix itself completely but I can totally vouch for her story. It’s a massive improvement.
Last year I began setting up a study to test the keto diet on Mendus.org but was skeptical. I’m not any longer and will get the study going as soon as I can.
Congratulations! Looking forward to hearing more including how you got over the rough spots.
I have to disagree. You say if this diet was all she’s saying it is, we’d see a whole bunch more folk getting better. You’re presuming people will all try it and try it for long term. We know that’s not true. Look how many people know smoking is bad for them but do it anyway. People who are overweight know what they should do, but millions don’t and carry on eating the foods that are bad for them.People often don’t do what’s best for them. In my experience, people are far more likely to depend on what the doctor does for them than take things into their own hands. Especially with conditions that are difficult to diagnose and had a label of “all in the mind” people will take drugs that are offered because it gives them a sense of validation. When you’ve been ill for a long time we often just give up and think this is our lot and some just don’t have the time,money or ability to study for themselves and find out what else may help. I think it’s pretty obvious that diet is going to be the answer for lots of our health problems. There won’t be a one size fits all because we have multifacted problems, but there will certainly be diets like the LCHF one which will certainly make life more liveable and will definitely be a cure for some. If the problem is with the mitochondria it doesn’t matter what you label it, the symptom is going to be energy insufficiency.
1. High protein is NOT ketogenic, high fat is.
2. There is NO ‘just going’ on a true ketogenic diet, it’s extremely strict -less than 20 gr carbs a day- and there are countless pitfalls -like thinking that just high protein will do, not to mention the always everywhere temptatations of our sugar-addicted society.
$9.99 for a Book on Amazon I guess this Answers this Topic
Did anyone here watch the summit when it first aired? Was it useful?
I’ve gone low-carb (not keto) a few times, and it feels very good. But I get terribly constipated. How is this dealt with?
Magnesium. You almost certainly need it anyway as a supplement, and in large doses. Going Ketogenic also reduces hydration because sugar plays a role in this, and as Lori says, you need to use Magnesium to compensate. Increasing the dosage “until it restores bowel function” is probably as good a guide as any. I also got horrific calf muscle cramps (early in the morning) until I had the dosage of magnesium high enough. Potassium and sodium matter too if you don’t get enough of them.
I recommend Hair Tissue Mineral Analysis to guide these supplementations more accurately, and also you will find out what other elements are depleted and what toxic ones are elevated, which all helps to working out the best treatment and getting improvement in condition.
One thing to remember, you needn’t always take magnesium orally. It can be very soothing to sit in a bath with Epsom salts – magnesium can be absorbed through the skin. I had the leg cramps too – still will on occasion. A massage therapist gave me a tip which sometimes works – if you’re in the midst of a calf cramp, place the foot of the non-cramping leg on top of the other foot. With the cramping leg, do your best to push up against the bottom of the ‘good’ foot as you push down with the ‘good’ foot. It can unlock the muscle spasm.
Obvious also she has a clear 100% undiagnosed case of Ehlers-Danlos Syndrome even in the exercise mentioned she maintains swimming or roller blades this is identical to what EDS Patients can do at certain stages, she is still stuck on the CFS type diagnosis she no doubts has a connective tissue disorder a Genetic Born condition. I do not consider her recovered at all…
You might be right, but Lori also might be an entirely typical CFS case actually making improvement. I am an FM case, not a CFS case, but her path to improvement is very similar to mine and I most definitely am not an EDS case.
Wouldn’t mind a good bonk… sorry couldn’t resist
🙂
??
Very happy for Lori. I’ve just started 2. Questions
Any suggestions for ‘constipation’
Im taking tons on watet salt and magnesium.
2.any ideas for affordable keytone moniterring
Thx for article and your website
Tc dan
The standard constipation things – take a disolvable fibre supplement eg. Benefibre here in Australia, and or use a slippery elm supplement.
I don’t have personal experience with constipation from this or any diet, if anything my problem was around the other way.
Keytones monitoring. Depends how you define affordable?
The cheaper but less reliable option, but I think most people use it, it saliva strips or urine strips.
I’ve ordered a diabetes blood test kit for $50 for accuracy. I think I need to keep buying more strips, possibly $1 each! Hopefully I can find them cheaper. But with blood you can just do once a week to check you’re staying in ketosis.
I’ve only been doing Ketogenic for 3 weeks. I’ve lost a little weight. I’m wondering whether I’m actually in ketosis. I find it easy to keep going as I enjoy the food and I feel full. I seldom get cravings or consider cheating.
I don’t know if my energy has improved. I started this without that as a factor, just wanting to lose weight.
When I submitted my story to Cort, I told him I’d monitor the comments and try to answer any questions posted.
First, I’m not surprised at the “she must not have what I have” type of comments – and it’s possible that I don’t, of course. I’m am flexible in hips and legs and fingers, but I do not have ED. I started swimming for relief from heat, and in the beginning, I’d do some neck stretches, or just float. That was my “swimming” in the beginning. It has taken me a year to work up to 1000 strokes, and I don’t (can’t) do it every day. The photo above was taken when I was trying my new rollerblades on the back driveway. I haven’t been off my property, and it is too warm here for street skating – it’ll be another six months before it will be cool enough for skating.
As for the comment “if just going on a high protein low carb diet were ‘enough’ to bring energy and health back to ME/CFS patients we’d be seeing a whole bunch more folk getting better”, I want to be clear that this is a low carb high FAT diet – protein is adequate, but not emphasized. Approximately 75% to 80% of my calories come from fat. At no time during the article did I say that I was cured. I have been at this a very long time – lot of therapies tried (and discarded) over a couple of decades. Yes, it may be that I’ve finally cobbled together enough of my 1% solutions so that a ketogenic diet served as my tipping point.
Aiden, Cort asked if I could recommend any resources, so I listed a few for people who don’t know what a ketogenic diet is. At no time was the intent to suggest a $10 book to cure you.
Madeleine & Dan – the constipation issue…I have a lot of coconut oil in my diet, so it is not as much an issue for me. I don’t use exogenous ketones very much (although I will if I feel like I have overdone and my body is not keeping up); however, my husband has been successful for a dose or two of MCT oil.
Lucy – 😀
Hi Lori
Did you ever have allodynia,that also drains my energy. Also, I found out my cholesterol is getting high and I have some protein in my urine. Do you think I would be ok on a high fat diet? Should I just have the good fats or the bad fats like you did with the skin in chicken?
I had big time allodynia. I had both the tender skin and the sunburn skin (even in my ears!) Don’t hit me for this guys, but Lyrica has actually handled not only that but all of my nerve related pain. This is so interesting. I can’t wait to get started!
Good for you Martha. Lyrica does work for some people! 🙂
I hope you’re still answering questions! I’ve just found this article while researching fibro and keto…..as I’m laying in bed with yet another flare. Very interested to know a current update on ur status and if you are still on keto.
Dan – on monitoring. I have a breath analyzer, but it is expensive, and truthfully, *how* you breathe into it is very important, and I didn’t seem to naturally have the knack for getting air out of the bottoms of my lungs without feeling like I was suffocating. I’ve made my peace with it now, but I am never in the high ‘red’ range. Perhaps that’s just normal for my body.
The urine strips are the cheapest, but there are some drawbacks…if you are using exogenous ketones (like MCT oil), you may just be measuring that coming out, not whether or not your body has fully adjusted into fat adaption. Some say that they stop working after a while, some say that’s bunk. They still show a ketone level for me. Not everyone is overweight (my situation), and I can’t tell you what you should expect the results to be if you are in ketosis but actually using the ketones up so that they aren’t being excreted.
Sadly, the gold standard is blood monitoring: if you have circulating ketones. I know the strips are horrendously expensive. I haven’t used them, and those who do might check once a week.
If you are just beginning, I’d go for urine strips. Just don’t be concerned that they aren’t on the far end of the color spectrum. Anything that is not the neutral control IS ketosis. They are intended for monitoring ketoacidosis for diabetics, so just realize that.
For me, it has been just as helpful to monitor blood glucose, and that is (relatively) inexpensive.
P.S. None of the websites or books or videos are mine. I provided them as potential references. The keto summit is also not mine.
I’m really pleased Lori’s feeling better. I tried the Ketogenic diet last year and it made me ill. I think that everyone is different and I understand why people search for that one thing that will relieve them of their symptoms and make them feel better. Maybe this diet will work for some but not for all. I’ve found that the diet put forward by T. Colin Campbell (The China Diet) a low fat, wholefood plant based diet is working for me, at least I’m noticing an improvement in my levels of fatigue, but that doesn’t mean it will suit everyone.
I think it’s very important to listen to our own bodies. A long time ago, a naturopath told me that when trying treatments it is important to only try one at a time. That way, you know which treatment is to blame. To be honest, the beginning of keto can be rocky, mostly due to low electrolytes. I had nausea to the point where I didn’t want to eat sometimes. Fortunately I’d been warned to watch for this and what to do. If my pain level or fatigue level had increased, I’d have dropped keto like a hot potato.
I read somewhere that because the body stores hormones in fat, and fat is what comes out of the cells to be processed into ketones when on a ketogenic diet, our hormones can feel pretty rocky as well. I don’t know if this is true, but it felt like it sometimes. I tried going all the way off my last dose of antidepressant, but after 3 weeks off, I had to admit I was completely ‘loaded for bear’ and that it would benefit me to return to (a lower dose of) AD and stay on it for a while longer. My body told me good and clear, but it took a while for me to hear it.
Me too – all sorts of lousy side-illnesses for several months as I lost weight. Part of this is that your fat can have many toxins deposited in it, when your renal system is overloaded or impaired in its ability to deal with toxins.
I would have had 25 years worth of toxins stored there, people who get onto the right approach early in their lives will bounce back far quicker. I am still getting flare-ups here and there after 3 years, I believe this is because deep deposits of toxins, eg in big, long-immobile core muscle tissue and abdominal fat, are still being flushed out.
Feldenkrais treatment is getting me good gains in posture and control and balance and range of movement, but I am sure each time, more toxins are dislodged, going elsewhere until they too are finally processed out by the renal system.
I think regular low intensity exercise and just plain “movement” is important to keep the toxins on the move rather than deposited in one place. Yes, just “moving around in the water”, in the early days, is part of my story too. Spa pool even more helpful because of the heat – but problem with overheating lasting hours afterwards, needed to be mitigated by doing the spa first, then the main swimming pool, in which I would cool down.
Be careful to cook your veggies.Everyone is recommending Mediterranean diet. No one is telling you that Mediterraneans traditionally cook their nightshades,kale, spinach… Nightshades contain poisonous alpha-solanine that is destroyed by cooking. Think: Mediterraneans eat a lot of nightshades. If they were so bad for as, they would all be crippled. They are not, because they know how to prepare their veggies. Tomatoes? When they are ripe, they contain much less solanine.
If anyone is considering this ketonic diet firstly be aware that high protein levels put a lot of pressure on the kidneys and liver,
Also be aware that animal proteins are linked to inflammation in the body and inflammation of the blood vessels endothelial cells
Yet plant proteins and plants in general reduce inflammation.
The good news is you can still do a safer high protein and high fat diet on vegetable based diet i.e. a vegan ketogenic diet.
Some of the best fats actually come from flaxseed oil and other lipids you can get from ‘Evening Primrose oil’, ‘avocado oil’ ‘Cocoa butter’ etc all with differing omega 3, 6 etc ratios.
I know we ME/CFS patients can’t be body builders but it’s worth checking out the group of vegan bodybuilders called ‘PlantBuilt’ who recently collectively won 32 medals during the 2017 Naturally Fit Games.
Vegan Bodybuilders Win 32 Medals at 2017 Fit Games
http://vegnews.com/articles/page.do?pageId=9607&catId=1
Here’s a link to the plant based vegan ketogenic diet
http://ketomotive.com/vegan-ketogenic-diet/
Again, a ketogenic diet is not a high protein diet. It is a high fat diet. I eat about 20 grams of carbs a day, that’s about 5% of my calories from carbs. 75% to 80% is from fat. The balance (15% – 20%) is from protein.
Agreed, I’m just showing it can be done without animal products, if people check out those fats I mentioned from certain plants have very good omega ratios. As for avoiding carbs some of the vegetable protein powders are 87% protein. Many plants are low in digestible carbs too, like green leafy vegetables.
It’s important to be aware that animal products can appear to the immune system as a foreign body, which can trigger inflammation and worse could cause ‘Cross-reactivity’ meaning our antibodies could attack similar proteins our own body produces. Which is a hypothesis for some autoimmune diseases.
I suspect ME/CFS is a rogue antibody that is attacking a byproduct (i.e. protein/peptide/metabolite) produced from our own cells (most likely neural/nerve cells) during exertion.
Some people may not have that problem, but others may do, so worth knowing there is an alternative plant based option that can be adjusted to fit a ketongenic diet.
🙂
It may help you to know that I’m a Rich Roll fan and read his blog, even though I’m an omnivore. I’d say most of my carbs on a normal day are from veg, and a good bit of my fats are from nuts/seeds (macadamias, especially, but I keep per day to about 20 grams due to carbs). While I’m not disagreeing with you on the inflammatory effect some may experience, for me the benefit of turning off the insulin production and thereby turning off the inflammatory response through ketosis has been a godsend. I’m fortunate that I have no issues with dairy as well, since that can also limit choices. I occasionally take a detour from the path, but this has led me to *mostly* a whole foods menu. I have a bucket of protein powder – the lowest carb I could find – but I haven’t used much as I don’t like the texture/taste. Whether or not a ketogenic way of eating is possible while only plant-based is a common question on some keto forums. In general, it is said to be doable, but harder, with more prep and research.
Lori, Thank you for sharing. Prior to getting well did you experience neurological-type symptoms, like: tremor, restless legs syndrome, tinnitus, visual dusturbances, dizziness, urinary frequency, night sweats. Did you have low grade fevers? Extreme sensitivity to heat? Did you feel your best in the evening ( on a typical day)?
I am thinking that these individual histories and careful classification of symptoms may help us define sub groups – which seems critical to better understanding.
Hi Merida – First, I would qualify by saying I do not consider myself well, perhaps just ‘wellish’. But before keto: tremor – occasional, usually related to reactive hypoglycemia, although my endocrinologist was concerned it was the thyroid med; RLS – yes, although it has been a good decade since it was an issue and I took medication for it; tinnitus – YES, it continues, although has dampened quite a bit…it was ramped up like crazy when I went off the last antidepressant and was one of the reasons I decided to go back on; visual disturbances – no, except I’m on LED screens way too much; dizziness – yes, mostly related to postural hypotension, and I can still have episodes, although they are very minor now(cataplexy in the very beginning, though); urinary frequency – no; night sweats – HA! How about ALL THE TIME sweats (I’m post menopausal by 7 years, so this isn’t hot flashes, those are different) – sensitivity to heat has been huge; low grade fevers – no, my body temperature usually ran on the low side of normal; and as for what time of day I felt best, if I didn’t manage to fall asleep by 10:30 PM, 11 PM to 2 AM were my most productive hours. That last part has really changed. Now I wake normally by 6:30 and do a couple hours of house-related things before going to the office.
Hi Lori,
I am happy this worked for you, I am just wondering how long it took before you noticed the improvement in your symptoms, not just to lose weight. I did an elimination diet last year for gut issues which was no carb and I lost weight (although I wasn’t all that much overweight), and I still mainly stick to the diet but I have had no improvement at all in my symptoms (I have had M.E for 25 years). I do eat a v v small amount of carbs as I found no carbs at all made me feel really ill. I eat linseeds and chia seeds for the constipation problems. It is a little complicated as there are quite a few veggies I can’t eat, (I also follow the FODMAP diet for my gut issues) and I definitely can’t tolerate coconut oil. My fats are from nuts, seeds, dairy, butter, oily fish and meat but I only eat red meat once or twice a week. Thanks for your help,
Michelle
It depends on the symptoms, really…the first to go was GERD, and that was virtually immediate. It took a few weeks for a large ‘area’ of pain to dissipate. What I mean is that most of my pain was at chest level and above (including arms). There was some large muscle pain in legs and back as well, but it was less intense on a regular basis. Then I was left with pain in hands and wrists, which could be awful at times. That took 5 to 6 months, and I was actually surprised when it went because I didn’t think that it would since the rest of the pain had disappeared fairly early on. As for brain fog, I suppose it started to lift a few weeks in and just got better and better. Probably as I became firmly fat adapted. Energy-wise, probably the same, with a couple months in really starting to notice that I didn’t think about naps and would voluntarily start chores or projects and follow them to completion.
I’m at the point now (8+ months in) that there doesn’t seem to be a rhyme or reason to what my body decides to focus on. I’m losing weight, and that’s great, but I started keto for inflammation, so by that metric it’s a success. Because of all the health issues I’ve had, my body has a lot of healing to do. So if I get stuck on weight loss, I might notice that all of a sudden my skin is smooth and not-so-dry.
Insulin sensitivity is huge for me, so I think the enormous cutback on carbs has taken stress off my body in that way. My energy level, while certainly greatly improved, even better doesn’t fluctuate so wildly as it used to. I still will come across some food that turns out to be something I should stay away from, but at this point, I have a pretty good list of safe foods that I stick to. I’m just getting better at combining them!
Michelle,
When you say “no carbs” do you mean no grains, or are you avoiding things like cauliflower and blueberries, despite their tiny amount of carbs?
I have always felt sick on low carb / low fat / high protein diets. I would get blood sugar crash type symptoms.
I’ve found low carb / moderate / high fat has eliminated those side effects.
The keto diet says “20g” of carbs, but that is really a maximum cap. Some people make the mistake of actually trying to take this in. I think it’s just to allow for the time you amount of carbs in the green vegetables you’ll need to eat for nutrients.
Since we are hypometabolic and we can not use carbohydrates properly for energy, why not try this diet? We love our carbs but if it could give us back some of our life it would be worth it. No bad side effects. Why not?
It’s been clear to me since I got sick that carbs are not good for me. If I ate sweets I had to have something like peanut butter with them or I would feel weakened. Starches such as potatoes and grains tend to leave me exhausted. I just didn’t think I had the discipline to lose the carbs. Actually it wasn’t nearly as hard as I thought it would be.
Eating as much fat as you want almost makes up for the lack of sweet things. 🙂
I was lucky in that it was just the right time to do this, and my husband already was, so we reinforce each other. If someone would have told me a year before that if I’d change what I’d eat and the pain would disappear, and I would have energy and not nap, and that I would lose 60 pounds and be back to work, and I’d laughed. I was mentally prepared to try, and I did my homework first. Also, my husband and I see a nutrition counselor – that helped in the beginning to know what potential pitfalls would be. Those visits are good accountability as well.
There *are* bad side effects – the ‘keto flu’ which is similar to the CFS crash we spend our daily lives trying to avoid. Also, there are a percentage of us that are low BMI, underweight, and have lost even more weight with CFS, so… losing more weight represents a bad side effect.
It’s not a win win. Like anything it needs to be weighed up with individual health condition and pros and cons. Nothing is one size fits all.
Lori,
Thanks again for your helpful comments. A ketogenic diet was suggested to me by a double- board certified doc ( in medical nutrition). My niece is doing this ketogenic diet and lost 100 pounds – she was very overweight. And at least one of her kids is showing some of the signs/ symptoms we all seem to share.
Wow – 100 lbs! Your niece will be a great resource!
I got an “autoimmune” cookbook for Xmas. It is Paleo with no eggs or dairy. Lots of saturated fats, protein and veggies/fruits. No carbs or sugar. It made a huge difference so it is worth a try for anyone.
As for pain and sleep issues, try medical marijuana if you can. I have been able to lower or eliminate some meds thanks to this combo approach.
I’m a much better cook than I used to be. Before, I was an (awesome!) baker, but now, no bread, no cake, no pasta, so I’ve had to learn new stuff. It’s amazing how good things taste once I got that craving for ‘sweet’ out of my day!
I tried a very low-carb diet on the advice of my specialist. It took a month (with dangerously low energy) for the fat-burning to start. It seemed to be done through adrenaline – I developed constantly tingling/frizzing fingertips, and sleep all but disappeared. I felt desperately hungry all day every day. My brain was clearer in some ways but sleep deprivation was an equal problem, plus I was on edge the whole time. Wired-and-tired, my original symptoms.
I couldn’t tolerate these new/old symptoms for more than a few weeks so gave up.
How was your fat intake during that month? From what I’ve read the hunger seen while doing a low carb diet can be taken care of by eating lots and lots of fats. That’s my experience as well. It’s critical to eat lots of fats.
Very high indeed, but it did nothing for my hunger and I didn’t seem to burn it for energy (a feature of ME/CFS is poor fat metabolism, I read somewhere). I used to be able to drop weight at will with no great difficulty….
The adrenaline can certainly be an issue. There is something called ‘dawn phenomenon’ where your body will kick out cortisol, then adrenaline, when your blood sugar gets low. During the day it didn’t bother me because I decided whenever I got hunger or cravings I’d eat something with a lot of fat in it. It was more of an issue at night – like waking up too early and not being able to go to sleep because my body said my blood sugar was low. A very long time ago when I worked with a naturopath for cortisol and adrenal issues, he had me try Seriphos (the original formula) which is said to turn off the excess cortisol production. I hadn’t taken any in years, but I stocked up again after I started keto just for this reason. It has helped enough to keep me on keto.
In *general* I sleep much better in the long run. Actually quite different sleep than the last 20 years. I don’t even think I move I’m just so deep. It was 9 hours last night, and although I know I dreamed, any memory was gone as soon as I was awake. Before, I’d had complex, vivid dreams with dream hangovers lasting at least until the next night. In a way, I miss that, because they were so entertaining. But I like my sleep better. About once a week I have a night where I wake at 3 and just have too much adrenaline going to fall back asleep, so I will do laundry or something for a couple of hours. My husband has the same issue – but he doesn’t do laundry!
I suffer from night-time hypoglycemia on a low-carb diet – lots of night sweats, terrifying nightmares, many every night. That alone is enough to dissuade me from trying a ketogenic diet again.
Opinions on Dr Myhill’s protocol? Why or why not follow? Is there a nutritionist or someone in the US that I can work with remotely or does anyone know of someone in Northeast US (I’m an hour from Syracuse, NY)?
I was stabilized in 2012 at year 13 in disease, when the proverbial hit the fan. Massive relapse followed by all kinds of new problems like sleep apnea, weight gain, back problems, cognitive, all symptoms worse.
It is only now that I am digging into what is new in ME/CFS research & treatment and I am pleasantly surprised, so maybe this is uninformed question.
Another resource for people to consider is “The Wahls Protocol” by Terry Wahls, M.D. She is a doctor who came down with M.S., and by changing her diet has gone from being in a tilt wheelchair to biking to work. Her eating plan sounds much like what is discussed here, with an additional emphasis on eating a wide variety of vegetables (and lots of them) for the nutrients and micronutrients.
One thing I like about her book is that she lays out a carefully worked out plan for transitioning into a keto diet, including menus.
I’ve improved somewhat on the first 2 stages of her eating plan, although I’m nowhere near 100% compliant. I’ve also lost ~30 lbs and kept it off for a couple years. So, no miracle cure for me, but another 1% improvement. Next for me is tackling the keto part.
Lori, Thank your for sharing your journey. Although ME/CFS may be many different conditions, stories of hope are extremely important and one never knows when one might recognize themselves in someone else’s story. Since energy is such an issue, and it takes a lot of energy to make a change, for me it is vital to hear about the different paths, what they entail, what the results were for fellow sufferers. I need to know there are many different avenues for partial recovery – it allows me to continue trying. Thank you again for sharing.
Hi!
I suffer from moderate to severe CFS/ME FIBRO
for over 10 years.
I recently started Keto diet 4weeks agao (60kg) 20g carb 50gprotein 90gfat.
I suffered flu symptoms for a week and felt worse than ever.
Then went back to normal feeling bad.
I dont know about getting tested.I do use urine strips that show moderate ketosis..
I dont have a Gall bladder and often felt liverish but this has diminished quiet a bit since starting on Keto diet.
Is it OK for me to continue without a Gall Bladder and can you give me any help and advise?
many thanKS,Karen
I just started on keto diet 3 weeks ago. My interest was sparked by your story, Lori, and I began to research the possibilities. I have lived with ME/CFS since 2003, along with a host of other problems – obesity, diabetes, depression, cardio-vascular disease. I decided the keto diet was the best choice for me because I want to get my blood sugars and blood pressure lower.
So far I feel it is going well: using urine strips show consistent ketosis since day 2, and I have lost a little weight. I have not felt any energy improvement yet, but I do not feel any worse than usual. I am just a beginner so I want to see what a few months bring!
just one thought ladies & any gents dragging their hangdog butts feelin miiiiiiightyyy lowwwwwwwwwwww
say it again doctah ahm feelinn mighty lowwwwwwwww
a middle age dude,skinny as a rail formerly with 11 inch forearms
wt 117 in socks & skivies, noticed damn muscle cramping at the factory round age 55 tiny leg calf muscle twitches,,increased fatigue & poopout the last third of the workday,( only tuesday)
less dexterity in my classical guitar hobby
I hypothesize men,as a rule,get treated by dr bluecoat whomever the hell it is like a dead mouse,,you cannot argue with them,they do not listen,40 years of medicine ‘cutting edge new treatments at ‘ take you pick of big city medical centers,,,, donbother me son,times a wastin you aint sick
Lori, In the last three years ME/CFS symptoms have ruined my life. Now I am out of bed and doing better. I still can not work much but my quality of life is better . Over the years I have been searching for other people who have been helped by a low carb diet and your story seems so much like mine. I think we may have a lot in common. Thank you for writing your story.
I can not tolerate high carbohydrate foods or I feel terrible. One slice of cake can make me feel bad for days. I like your idea of bonking that is what I felt like as well when I was in bad shape.
Like you I have a cpap machine that helps me sleep and now I only sleep 8 hours a day.
I only gained 20 lbs but after losing 10 lbs on a low carb diet I am starting to feel better.
The cholesterol level in my blood is very high but statin drugs make me feel terrible. So I can not take them. I had a CAC scan and I have no build up to worry about.
The only pill I take is magnesium 300 mg per day. My sister also has ME/CFS as do 3 of her children.
How have your energy levels been since you wrote your story in 2017 ?
I am wondering, once in ketosis – for those of you who have enjoyed a marked increase in energy – how long did it take to feel that? I have been in ketosis for a few weeks and haven’t increased in energy yet.