Subsets, Subsets, Subsets
Everyone with ME/CFS who’s been around a bit must ask themselves at some point, “Do I have what she or he has?” Some people do great on treatments that others fail on. Some people get really, really sick while others maintain at least a modicum of health. The variety of symptoms, treatment responses, illness progressions, even illness triggers is astonishing. For every person who remembers the exact day their illness came crashing down, there’s another who doesn’t remember the day, week or even month they became ill, because their illness came on gradually.
There’s the relapsing-remitting group which gets better and then worse, the plateaued group in which things remain much the same for decades and the progressive group where the illness gets progressively worse – sometimes to levels rarely seen in any nonlethal disease.
Most researchers concluded decades ago that ME/CFS must be littered with subsets. Just what those subsets are is a critical question, because as Jared Younger notes – a treatment that works for one subset probably won’t work for another.
Some subsets appear to be showing up. Dr. Peterson’s atypical subset typically has an unusual onset, an unusual course, has unusual comorbidities and is sicker than the rest of us. The immune systems of short duration patients (one subset) are on fire while the immune systems of longer duration patients (another subset) have run out of gas.

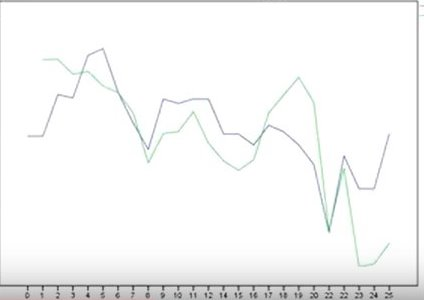
Younger’s “good-day, bad-day” study is an example of what the NIH does best: throw a boatload of money (> $1,000, 000 over three years) at a complex study. Younger’s study allows him to track which immune factors track with a person’s fatigue. A substance that rises and falls depending on how fatigued a person is, very likely has something significant about it.
The scale of testing is extraordinary. The study includes seventy people with ME/CFS, 20 healthy controls and 20 fatigued people with thyroid issues. The study involves twenty-five straight days of blood sampling from all 110 people, and each sample is tested for 51 substances associated with inflammation. If my math is right, that’s approximately 140,000 tests for inflammatory substances over the life of the study. Each person will also report their fatigue levels daily on a personal handheld computer. All this data will be thrown into a computer to see what patterns emerge.
It’s still early yet – the study is slated to run for several years – but in his YouTube video, Younger reported that some patterns may be starting to emerge.
The Infection Group?
C-reactive protein (CRP) levels are tracking with fatigue in about thirty percent of the ME/CFS participants. This suggests that a significant number of ME/CFS patients may have an underlying infection that’s popping out during their bad days.
 C-reactive protein is an “acute-phase” protein produced by the liver which shows up early in an infection, in cancer or in response to a tissue injury. Once immune cells called macrophages come into contact with dead or dying (infected) cells they release a substance called IL-6 which triggers the production of CRP (and fibrinogen) by the liver. When CRP binds to the surface of those cells, it gets the complement system involved which, in turn, helps more macrophages to find, engulf (phagocytyze) the infected cells and begin clearing them away.
The key to high C-reactive protein levels is plenty of dead or dying cells – something which usually occurs in the context of some infection (bacterial, viral, fungal), inflammatory diseases, malignancy or injured tissues. A very large (n=1125) fibromyalgia study recently found increased CRP levels in FM. It’s not clear how high the CRP levels in the ME/CFS subset was relative to other diseases. but what is clear is that the high CRP levels would probably be swamped by the lower CRP levels in the two other ME/CFS subsets; i.e. CRP would not be elevated in the group as a whole.
Autoimmune diseases like lupus, Scleroderma, polymyositis, and dermatomyositis, on the other hand, generally have little effect on CRP levels. (In fact, one researcher proposed that CRP protects against autoimmune diseases.) That brings up the next group.
The Autoimmune/Autoinflammatory Group?
A substance called fractalkine – which is elevated in many autoimmune and inflammatory disorders – is tracking with the fatigue levels of another third of ME/CFS patients. Fractalkine, whose release is also triggered by damaged cells, promotes the production of pro-inflammatory cytokines.
Fractalkine is released by T-cells and other immune cells, endothelial cells and, most prominently, in the central nervous system.
In contrast to CRP, fractalkine is elevated in autoimmune diseases like rheumatoid arthritis, Sjogren’s syndrome, systemic lupus erythematosus, and scleroderma, as well as diseases associated with systemic inflammation. In rheumatoid arthritis fractalkine directs immune cells to the joints. Fractalkine is also elevated in systemic inflammatory diseases like atherosclerosis and inflammatory cardiomyopathy.
Because fractalkine appears to be intimately involved in producing pathological pain, one wonders if these are the fatigue and high pain patients. One study has found increased fractalkine levels, not in the blood, but in cerebral spinal fluid in fibromyalgia. The study suggested that damaged neurons were triggering fractalkine release.
Because fractalkine plays a prominent role in producing inflammation, anti-fractalkine agents are being examined. Several existing drugs and supplements (baclofen, Apo-A1, resveratrol, epigallocatechin-3-gallate) may be able to suppress fractalkine production.
The Non-Immune Group?
In the last third of patients, Younger hasn’t yet found a pattern, which suggests that the fatigue symptoms of this group may not be driven by the immune system. This, Younger suggested, could be a metabolic or other group.
Conclusions
Younger’s “Good Day – Bad Day” study is looking for biomarkers in an entirely new way. Very different from the one-time shots at assessing immune problems that we usually see, Younger’s study is tracking immune changes as they occur over time and pulling out the immune factors shown to be most associated with fatigue. Many other symptoms exist in ME/CFS, but as Dr. Lerner used to say, when the fatigue lifts the other symptoms follow.
Thus far the study suggests that the fatigue in ME/CFS may be being produced differently in the three subsets of patients: by an ongoing infection in one, by an autoimmune or autoinflammatory process in another, and by something outside the immune system in the third.
The most intriguing thing about Younger’s study is its intensity. No one has examined the immune basis of fatigue in ME/CFS with Younger’s intensity. It’s no surprise, then, that Younger is getting results (CRP, fractalkine) new to ME/CFS – results that also, interestingly enough, fit with what we already know. Infection and autoimmunity, after all, have long been thought to be present in ME/CFS. Younger’s early results suggests that they are present – but in different sets of patients.
If Younger’s early results prevail and are validated, we should ultimately see radically different treatments for the two different subsets – immune activators and anti-pathogen treatments for one, and immune suppressants for the other. We’ll also see studies focused on each subset and that could make all the difference in research.






And all it took was money. So many mysteries surrounding this illness could have been solved years ago by giving adequate grant money to research. Bad Name ME/CFS
The good news is that if we can get the money and do the big studies then the breakthroughs of the last decade or so in data mining and being able to analyze huge datasets could be really helpful.
How severe were these patients ?
Methodology ?
Are there patients with both
Elevated CRP and fractalakine
I don’t know and I don’t know! You can find the study parameters (hopefully) using a link in the blog.
If immune patients symptoms are triggered by a dormant virus, what is the trigger that suddenly sets off the immune response? Stress, fatigue, allergies, other illnesses? We know viruses remain wo any symptoms for a lifetime, so why is it suddenly prompting the immune system in some people and not others? On another note: keep up the great work! Love reading these study results and insights to finding a cure.
Great question! Any one who can answer that question may have found the key to ME/CFS – at least for a major subset of individuals.
It didn’t only need money, it needed a researcher with a good idea. Give him some credit too ….
I agree! Money makes the world go round so when str the drug companies hoing to jump on the opportunity to be the first to treat is and start using thrir lobbying money for that! And that yhe government loses more money nc we csnt work bc we have no yreatment than they epuld if we wete treated and got good health benefits we could remsin working and not losing our careers we worked so hard for?!
Very exciting to see these early results Cort!
Another great article Cort! Sounds very promising!! Yay!
Er… wonder about those of us who have chronic infections, suppressed immune systems, AND autoimmune problems together?
Seems like the immune system is very complex and full of surprises…
Oh yes. I have no doubt that the situation is probably more complex than this..There is, for instance, the connection between infection and autoimmunity that shows up from time to time. It never seems to be as simple as it first seems.
None of my doctors would listen for one minute to a study about 70 people. Very sad this isn’t being done on 10,000, which is the amount of group testing my doctors always mention, if they are to believe a medical study. This includes my POTS doctors as well. Maybe after this a huge study will be warranted. But probably the money will be gone, thanks to the GOP. Thanks for the study!
Yeah, that’s my situation also. It makes for quite a treatment dilemma. I guess the only logical approach is a sequential treatment that deals with infections first with antivirals and other things depending on the pathogen(s), then immune suppressants/autoimmune paleo diet/rituximab(?) to quell the autoimmune aspect, and then nutritional support and/or carefully selected immune boosters to get the immune system working again. But each of these steps is difficult to accomplish.
“chronic infections, suppressed immune systems, AND autoimmune problems together”
That may not be all that contradicting. A healthy person sits in a comfortable “middle position”, far away from either underactive or overactive immune system.
In many systems, as a system starts to fail margins get thinner. Even whilst staying at the middle position both the distance between normal and too few and the distance between normal and too much start to get less. If the system get worse just a small deviation from the normal is enough to get out of the thin remaining safe zone between too few and too much. The system lost its stability and went to being metastable. In fact this is some kind of description of losing homeostasis.
While most people consider only losing distance to too few OR too much, losing distance to both is quite normal too. When being in that zone, even small perturbations can go up either immune deficiency or auto immunity. Alternatively, one subsystem may go deficiency and another go auto immunity. Or they may oscillate between both in time…
Being in this theoretical position, one can expect to have easy back-fires when taking meds or going new approaches. Going very slow or low dose at first may be the better option here?
I mean autoimmune illnesses, from my basic non-doctor understanding is that they involve your body’s own cells being attacked by your immune system many times. I would think while your body is trying to kill its own cells that it would leave the over-worked system into the opertunity for more infections. Didn’t they prove MS and lupus flares can be triggered by infections, partly?
Hi Shy,
I’m not sure if we look at this the same or not. What I meant is that auto-immunity is often told to evolve from the immune system being to aggressive attacking not only real threats but also the bodies own cells.
Having an overworked system that fails time and again to tackle the real pathogens, the body may tune it to be a bit more aggressive so it stronger attacks the real pathogens but risking it to regularly attack some own body cells.
Some may say that an inefficient immune system can’t be aggressive because then it wouldn’t be inefficient anymore. I don’t think this to be true. Compare it to a police force being unable to stop riots. They start gentle when they think they can control it but start getting more and more aggressive charging at rioters and arresting anyone that may look like they might riot some time soon (=auto immunity like).
Fascinating ideas coming out of this – will be looking forward to hearing more!
I’ve been under treatment for ~year and the antiviral, stimulants, gabapentin, LDN have so far had no/very minimal effects. Been on an antibiotic (just for ME/CFS-inflammation) for a few months now and my inflammation went down so much I’m discovering I was hypermobile all along. I dropped 3 ring sizes and no weight. You can feel my bones again, it’s been 10 years or so since I’ve been able to! Fascinating stuff, I have since onset figured I lean in the class of autoimmune ME/CFS subtype.
Hi Shy, I’m a bit confused by your comment (yay brainfog), but I would very much like to understand it. How would an antibiotic decrease ME/CFS inflammation? Did you have SIBO or some other bacterial infection that was causing inflammation? Also, was “hypermobile” a typo, or are you saying that now that you have less inflammation, your joints can move their full range of motion, which for you turned out to actually be above normal. That’s really wonderful that the antibiotic is helping you!
I was hypermobile as a kid (beyond normal range of motion, bendy fingers, beighton scale). Since losing the inflammation- I can do the “tricks” again. Not nearly as severe as some people with EDS but most likely in the hypermobility spectrum now! My joints felt, for lack of a better term- “congested” stuffy, cottony, and cramped, painful, etc. before. My specialist (ME/CFS) put me on minocycline. I don’t know where she pulled that from, but it did something- the first med I’ve been on during this illness that had some effect somewhere that actually was noticeable to me- and others. I do not have any active bacterial infections, from what I understand it is being studied that antibiotics have general anti-inflammatory properties. A normal person may take an NSAID for that but I cannot due to bleeding ulcers from them!
Which antibiotic are you on? Mino?
Yes minocycline!
What antibiotics did you take?
Minocycline
Dr Cecile Jadin used a 6 month rotation of antibiotics to help patients and Ken Lassesen blogs on the concept. The idea is trying to return your micro biome to a state that returns your immune system to homeostasis. I think it is a very complex system and that trying to figure out what subset there are to provide symptomatic relief will not fix the problem.
Interesting
I wonder, would someone whose CRP blood tests always come back normal be excluded from the CRP subset or would this just be a case of getting tested on a “good” day. Mine have come back as normal many times
In the video he states that people can have normal crp levels. He is looking for fluctuations that occur with fatigue.
It’s probably the same as with the leptin study; leptin levels weren’t elevated relative to what is considered normal but they were higher when people with ME/CFS were in a fatigued state. Broderick has found that given the right immune context immune factors don’t have to be elevated to have large effects.
So, “normal” CRP levels probably don’t necessarily mean that you’re not in the CRP subset.
My son and i both have below range c reactive protein, during our most severe times of illness.. i have autoimmune diseases as well and apparently have low hormone levels. My health never recovered after EBV and developing Hashimotos. Then my Pituitary shrunk along with the Hashimotos, which has effected other hormones, but i have not been properly tested. I have H Pylori too. My son has gut infections, with fatigue and brain fog, not diagnosed with cfs, but i was. We both take many anti inflammatory supplements. Maybe this lowers inflammation, but i am very ill, bedridden now.
This is very exciting. I was part of a 25 day blood draw, when Dr. Younger was at Stanford. I’m wondering if Dr.Younger will be looking at past studies as well. I had a strange reaction to having my blood drawn for the 25 days. Around day 14 , I noticed I was becoming agitated. By day 25, my behavior was unlike me. Road rage. Five days after my last draw, I returned to my “normal”. (No road rage before or since). I spoke with Dr. Younger about this. No one else had this issue. I would have done the draw again to see if it was the result of the blood draw.It’s been several years and I still wonder about it. Now, I’m wondering if they checked my blood, for some of these new areas they are looking at, what would show up?
This is for Emily, there was no reply after yr comment.
But my illness and your’s are identical?? Wow from ebv to pituitary? I don’t know what sublet we are, but it would be the same : )
Thanks, Cort!
Your updates are manna for us hungry-for-info hoardes!
I’m so curious to see what the differences are in immediate vs gradual (my case) onset. Also, I believe mine was triggered by a surgery vs a virus, so I think I’m in the minority in both category? Anyone else out there in this unusual subset? I read on a mito website that general anesthesia (surgery) is very bad for mitochondria.
I had major abdominal surgery and chemotherapy upon cancer diagnosis. I’d been in the best shape of my life and fully functional before treatment.
This stressed my immune system and a combination of infections reactivated and seems to have caused autoimmune antibodies as well.
They were lurking there all along, just waiting for my body to be stressed.
Maybe you have a similar situation?
Dear Learner1,
Could be! So frustrating. I hope they’re studying the post-surgery folks.
Best wishes,
Shelby
I developed ME/CFS following my second round of chemotherapy (following surgery for cancer). I became so ill they stopped the chemo treatments. My white blood cell count has never returned to normal. I wonder if that puts me in the immune camp, or if a latent virus surged while the chemo had my immune system down.
I often wonder how often CFS has been triggered by chemo?
According to this paper:
http://theoncologist.alphamedpress.org/content/12/suppl_1/4.full
http://theoncologist.alphamedpress.org/content/12/suppl_1/4.full
Cancer related fatigue (CRF) continues for months and even years following completion of treatment in approximately one third of cancer survivors, and they don’t know the cause.
I wonder how many of those people would turn out to have CFS (with PEM, and other defining symptoms), if doctors were better at diagnosis. No one at the cancer center diagnosed my CFS.
Even for those who do not have CFS, it seems very likely there is an overlap in the causes of CRF and CFS.
Does anyone know if someone has ever explored the incidence of CFS in cancer survivors?
Perhaps if that connection could be made it would open up new research funding sources.
Cancer related fatigue is common; it’s a darn shame that ME/CFS patients are not being studied alongside CRF patients and vice versa. I agree that it’s a potentially important funding source.
learner1,
Think you are talking my story. I always had a very reactive immune system ( allergies) but was rarely sick until a chiro adjustment that injured my neck and pelvis. Had enormous energy prior to this.
I understand that they hyperextend people’s necks to intubate for surgery. Also, if you are having major gut issues appreciate that scar tissue can hold the bowel in odd positions – can cause kinks and twists.
This article leaves me wondering if I am in the third group. No autoimmunity, I’ve just been retested again this year, CRP always tests high or at least never zero. I have had chronic relapsing CFS and fibromyalgia after the first years of unrelenting fatigue. And now, pacing and having retired from work have allowed me some respite from pain and fatigue, which can come back the minute I overdo at anything, no matter how trivial. I have never regained my previous central nervous system stability and balance, nor have I regained my pre-CFS brain. I am 64. I hope to have some answers in my lifetime.
I was hoping for answers, too, but I’m 67 now & has had this since 1987!
So C-reactive protein may be relatively low in a patient, but it rises and falls with fatigue level, while staying in the “normal’ range. Is this true of the fractalkine level? Can a one time high measurement of fractalkine suggest autoimmune activity?
This is correct, Cort please amend the article accordingly. CRP are normal range but fluctuant
I wonder for those of us on adderall or antivirals, or other possible medicines would suppress our immunity markers in blood work. So they would appear to be normal? I know on a day with adderal my Cortisol was 9 early morning..without taking it was 9? You think it would be the opposite. The adderall would raise it?
I know I used to have severe panic attacks..if I were to ever take something like adderall then my stress levels would fly thoug the roof..now its like a constant low grade stress instead of panic..I think my body, and mind knows it hasn’t the energy to panic anymore..
We don’t know what the absolute levels of fractalkine are in that subset but they could certainly be in the “normal” range.
I’m always looking for what may help. Found this on white mulberry and Curcumin. Couldn’t find an RX listed as helping fractalkine. Appears it is good in some forms and not good in others.
https://examine.com/supplements/morus-alba/
Artherosclerosis
A study in HUVEC cells (endothelial) with the leaves of Morus Alba at 400mcg/mL (deemed a physiologically relevant dose citing this study[87]) is able to inhibit the expression of P‐selectin and fractalkine induced by resistin, with similar potency to 20uM Curcumin (both fully abolishing the effects of resistin) thought to be related to attenuating NADPH oxidase activity (abolished with Morus Alba, reduced to 30% of control with Curcumin).[88] Resistin induces P-Selection and fractalkine expression in endothelial cells, which increases monocyte adhesion and may be pro-artherosclerotic[89] and in HUVEC cells Morus Alba was shown to inhibit monocyte binding to a potency correlating greatly with NADPH oxidase activity.[88]
Issie
I love that Jared Younger shares his videos with us and updates what his findings are.
I echo Susan. Does anyone know what import a one-time fractalkine measurement might mean? Would that be useful?
I shall ask my naturopath if he will test for it out of curiosity. Since I have no pain, I don’t think my levels will be high.
I love the stream of info you send, especially about all these tests I have never had during 35 years of ME/CFS in Australia. I don’t know whether to be relieved or envious regarding investigations you all seem to have routinely. From severe illness I have improved to a state of being functional at home, as long as I rest after a shower cooking, making my bed, etc. but wiped out by chemicals in food or the air. Hence home is best. To Diana I hope answers come in your lifetime, At age 86 I am not holding my breath. Go Jared Younger, well done.
Audrey Brimson, Australia has several research groups working on ME/CFS, so it’s not a complete desert 🙂 The trouble is that their findings aren’t working their way to GPs; most of whom still follow the CBT/GET model.
Cort, I think Jared’s early results show great promise. I do have a query with one aspect of his methodology. By coming in for 25 consecutive days, participants with all but the mildest ME/CFS are bound to accumulate PEM. This would make their symptoms steadily worsen, rather than fluctuate as per Jared’s hypothesis. I wonder how this will affect the trial’s results.
wow, what an extremely good point!
I agree. Good point! Didn’t think of that….It could mean more bad day than good day results. I’m sure that Jarred thought of this. I wonder what his take on it is…
Excellent point!
I thought the same thing. I expected to see fatigue go slowly up. Did they have to commute to a lab for the blood draws? I can’t even leave my house for anything, I get sooo sick. They’d have to come to my house, and even then the presence of a person, having to talk, hear voices, etc. would make me far worse. I’m thinking these are moderately affected patients at best.
PS. And 24 days in a row! I have to recover for days after someone comes over, even for a short time. I cannot imagine this.
Yes. They must be moderately effected….How interesting it would be if someone could come to more severely effected peoples houses and test them as part of this study…..The more severely effected are getting studied in the CDC’s latest version of the multisite study.
“This would make their symptoms steadily worsen, rather than fluctuate as per Jared’s hypothesis.”
Fiona, I’m not sure I understand your point. The patients in this study are reporting their fatigue levels, which fluctuate wildly from week-to-week. Jared doesn’t predict what pattern their fatigue should follow – he is simply reporting empirical data. His cautious hypothesis seems to be that there are different mechanisms driving the fatigue, and those mechanisms may be inferred by observing correlated blood markers.
Your hypothesis is that “participants with all but the mildest ME/CFS are bound to accumulate PEM”. In other words, you predict everyone’s fatigue will increase over the course of the study. We’re only shown data from two patients, one whose fatigue trends down, the other whose fatigue goes down but then rebounds to the initial level, so there’s no data here to support that argument.
Are you more generally suggesting that PEM is independent of blood chemistry? If data were collected that support that idea, then that might point toward another mechanism. Neurological? (Perhaps that is the third group!)
Really interesting. Perhaps it explains why Rituximab in Fluge/Mellas studies makes 1/3 well, 1/3 better and leaves 1/3 without results!
unfortunately my body doesn’t do good days (or seriously bad days for that matter but that’s when I severely overdo it which I can then only blame myself for) but what it dóes do is with tiny spasms recover from a former stealth infection in different parts of my body so I no longer think of subsets but in brains, thyroids, hearts & adrenals being infected in different spots (and by different bugs?)
This is really exciting, and interesting but I’m wondering why he has only used CFS/ME sufferers who have thyroid problems? Makes me wonder if the results are more likely to be linked to this rather then CFS/ME, and therefore how reliably the results can be extrapolated to CFS/ME sufferers who do not have thyroid problems. Maybe it would have been good to have another test group of CFS/ME sufferers with no thyroid problems for comparison…?
As I understood it the ME/CFS group didn’t thyroid issues but the fatigued, healthy control group did.
I love this man. Just shows what can be done when a scientist starts to look at actual data from patients. Contrast this with the psychiatrists!
I especially appreciate that this is so important that it needs to be said early. I would hope that publication could be fast tracked because of the considerable importance of these results. He is not only identifying subsets but biomarkers, the holy grail for researchers.
Actually Tatt, CReactive Protein is just a vague inflammatory marker which can even just signal obesity. If a patient has elevated levels and are overweight, the doctor will just tell them to lose weight. And psychological stress can elevate C reactive protein levels. Remember, Jared Younger first started investigating ME as a psych. expert. I do think he’s still seeing ME through a psych lens.
https://friedmansprout.com/2015/04/01/how-does-a-ketogenic-diet-affect-you-part-3-c-reactive-protein-a-marker-of-inflammation/
“CRP is considered a marker of inflammation. The liver makes CRP when inflammation in the body is present. High levels of CRP are influenced by genetics, high stress, exposure to environmental toxins and a sedentary lifestyle. Diet can also impact CRP levels, especially diets high in refined and processed foods.”
I really wish everyone would look up these terms that Jared Younger throws out to see if he’s truly researching just ME and infections. So far everything he’s been researching can be attributed to psychological stress, which is what he started out researching ME as in the first place – a psychological problem. When we praise him as if he’s researching something other than a run of the mill vague inflammatory marker we make ourselves look like gullible, biologically uneducated fools. And we don’t spur researchers on to greatness.
Just to say, 30 years in and not doing so well at the moment, I am profoundly grateful to the researchers doing this work for us, as well as to you, Cort, for keeping us up-to-date. A pox on the PACE studies and the Lancet, but I am very thankful to know there are people who really are fighting for us. Maybe, just maybe, there will come a time…
It’s great to know another country is doing so much research. We are lacking so much behind in England. I started with an awful lot of tiredness in my early 30’s following an episode in isolation unit in hospital. My notes said viral meninges. Ten years later I had a routine knee op and ended up with CRPS, this seemed to have a knock on effect with Fibromyalgia. However it took 14 years to finally get a diagnosis of CFS and Fibromyalgia. I also have had borderline results for lupus and at the moment borderline thyroid. (My mother had Fibromyalgia and systemic lupus) I’ve also been tested for Sjogrens as have severe dry eyes. Gabapentin and pregablin have had little effect. As far as I know my CRP levels are within normal range. Occasionally have been a little higher. However we don’t seem to get any tests done on a regular basis in this country sadly. I do wonder which of the three sub sets I would come under. I really look forward to your articles, it gives us all hope that someone out there is actually doing something about these awful illnesses
2 subsets found by NIH/NIAID one with double copies of tryptase gene also second one triple tryptase gene found the other thing I see now is People diagnosed with EDS3 Hypermobile can have multiple crossovers
types like EDS3 with Classical or Vascular EDS or some other combined types.Also, I have seen Genetic test one gene from each Parent they have Born CVID Common Variable Immune Deficiency & this can be
missed by Normal immune system workups. I am also seeing as mentioned numerous times (HFI) hereditary fructose intolerance & it can cause Syncope episodes & severe fatigue, one young Teen
diagnosed at Birth with (HFI) was experiencing severe profound fatigue the Doctor involved did a simple blood test for Vitamin C he was deficient in Vitamin C he was given a safe Vitamin C & put on
allowed foods to increase his Vitamin C intake the Paper Published on this was titled ‘Doctor Why is my Son so tired’also I have seen People misdiagnosed with EDS3 a third phase trial now at the NIH say it is
EDS type IX they measure blood serum Copper if low it is likely EDSIX they use Copper injections to surpass the Gut. There are diets online for (HFI) on foods to avoid, remember a simple slice have Bread
contains sucrose so do countless food products even store bought Bacon has sucrose added…Aspartime, Fructose, Sorbitol, Sugar, Fructose, Fructans, Fruits, vitamins, medicines etc. see Boston HFI Lab
online the list is long. Also Spontaneous Spinal Fluid Leaks found by Dr. Ian Carroll at Stanford & another Young Woman in the UK underwent microscopic Surgery at her veins in her neck it was done
by a neurosurgeon based in Germany, the procedure cost over +30,000 Euros not covered by the UK NHS She was diagnosed in the UK using an ultrasound to detect the abnormalities & her Story was posted on EDS UK
Awareness site from a newspaper in the UK it also has a Video attached she claims to be now getting her life back. Check your blood works first Copper serum to rule out EDS IX low copper or Wilson’s Disease
high copper, Vitamin C levels without your Vitamins & other tests mentioned above & folic acid/ferritin may not be good it is added to countless foods as well…
I forgot to say a simple test also is(ANA) Antigen Nuclear Antibody rule out/in Sjogren’s it is also an autoimmune marker for other things do not do the Eye paper test it misses (ANA) it is the Gold Standard Test
The only truly positive way to find Sjogrens is a lip biopsy. There are many false negatives on the antibody testing. Also, I know of some who have it and have minimal dry eyes or mouth and are positive with a lip biopsy. It is being found more and more in people with dysautonomia.
I too question where EDS stops and FMS starts. Are they one and the same or two separate things? Having both DXs……I wonder.
Issie
With Fibromyalgia, ME/CFS,Hashimotto’s (autoimmune into the mix), etc…I wonder where I would be in the ME/CFS subsets. I was relapsing/remitting for many years. For the past 4 years, I’ve been progressively been getting worse, forcing me to be mostly homebound for the past 3 years.
Such great news! Thanks for covering this, Cort. And big thanks to Jarred Younger for his dedication and tenacity (not to mention brilliance). It’s so good to know that research into the causes of the illness is being conducted.
I don’t know if he mentioned it in the video, but there are anti-fracklanin drugs being investigated. Somewhere
http://acrabstracts.org/abstract/safety-and-efficacy-of-e6011-an-anti-fractalkine-monoclonal-antibody-in-a-first-in-patient-phase-12-study-in-rheumatoid-arthritis/
Very interesting article. Thanks, Cort.
This explains fracklaine a little better, shows possible connections.
http://www.healthrising.org/blog/2017/05/14/fibromyalgia-neuroinflammation-fractalkine-chronic-pain/
Issie
Just get a valid Lyme test and you will know the answer to many questions. Yes so many misdiagnosis. It can lie dormant for years. Give the Igenex test to start out with since that it the current best test but not full proof either
Jared Younger’s tests may be fine, but his theories of trying to fit ME into an infection or virus are ridiculous.
What fractalkine and CRP have in common is that they are both used for tissue repair. If ME starts with a vulnerability, perhaps genetic or perhaps induced/exacerbated by anti-cholinergic drugs, then our bodies will respond throughout our lives trying to maintain connective tissue homeostasis.
God almighty. When will researchers finally turn their paradigm around and look at the connective tissue repair aspect of our immune system? We start out life with the ectoderm, endoderm and mesoderm sending out signals to create, dissolve and repair tissue. That doesn’t stop when we’re born. That continues throughout our life. Genetic connective tissue disorders are largely unrecognized and under-researched. Ground substance, as another commentor on Health Rising has pointed out many times, is the basic ingredient in all our fluid and solid connective tissue, including our blood plasma.
Anyway, for those interested, two studies showing that CRP and fractalkine are not just indicators of virus or bacteria, that they are also involved in tissue disease:
https://www.hindawi.com/journals/mi/2014/480941/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3168703/
For those who point out that some “contract” ME after a virus, mold, bacteria, etc: May I suggest that may have simply been the trigger to a genetic disposition. Like an underlying genetic disposition is inborn and parasites, etc. trigger IBS. Or genetic predisposition is inborn and puberty, chocolate trigger acne. Or a genetic predisposition is inborn and a virus and Aspirin triggers Ryes Syndrome. For ME it may be an genetic disposition is inborn (likely connective tissue related like EDS or Sjorgens) and injury, virus, bacteria, mold, etc. and perhaps anticholinergic meds which affect connective tissue signalling triggers ME. Those who build ME slowly over years may just be experiencing smaller triggers over time. An antibiotic here, an injury there, overwork (sleep deficit affecting quality of collagen production) and grooming products/chemical exposure worsening ME slowly.
I’ll bet never in a million years will NIH fund Jared Younger nor anyone else to examine if anti-cholinergic drugs, grooming products, pesticides, etc. are a trigger for those genetically disposed to develop ME.
Ly, it would be interesting to hear what direction you think the research should go based on your understanding of EDS (or any connective tissue disorder) as a likely predisposing condition for ME/CFS. Do you know enough to speculate upon potential future interventions? It would be curious to genetically screen CSF patients for all connective tissue disorders. Seems like it would be relatively easy and cheap (enough) to do.
Cort, thanks so much for another great article!
I was wondering, though: You write that autoimmune diseases generally have little effect on CRP levels. But in several autoimmune rheumatological diseases it does! In Rheumatoid Arthritis, for example, elevated CRP is one of the main markers. (https://medlineplus.gov/rheumatoidarthritis.html#cat_92) Same with Polymyalgia Rheumatica (https://medlineplus.gov/polymyalgiarheumatica.html#cat_92) and others.
Judging by this, I’m not sure the CRP group would necessarily be an infection group?
Does Younger connect CRP with infection and not with autoimmune diseases?
Thank you for all your work!
Yes, I found some overlap as well. I think in the interests of time Jarred probably provided a broad summary but it is a bit more complex than autoimmune vs infection….CRP levels are increased in some autoimmune disorders (and not at all in others). CRP is also elevated in people with poor sleep (another potential confounding factor) and cardiovascular disorders.
Cort, I’ve been trying to post on the forums but I guess I don’t have the sufficient privileges yet. I’ve had pretty good success with the B cell suppressing drug Rapamycin and now I’m considering adding Mycophenolic Acid. My success with Rapamycin makes me think I’m part of the autoimmune inflammatory subgroup, which seems to respond to any B cell suppressing drugs. Rapamycin and MPA are way more affordable than Rituxan and have less side effects than Cyclophosmide. I’d love to make a post to share my experience. I participated in the Light’s most recent experiment in SLC and they were really interested in studying Rapamycin and two other B cell suppressing drugs. My cell trend autoantibodies were 4 out of 7 positive and I’d love to see if they are coming down with Rapamycin treatment. Both Rapamycin and MPA can lower autoantibodies.
Hi blogger, do you monetize your website ? There is easy method to earn decent money every month,
just search on youtube : How to earn $25/hour selling articles
Love the videos. Thank you Jared Younger!
Not to be contrarian, but I don’t buy immune function as the only–or even primary–factor determining duration. I first became too sick to work in 1982, had periods when I could work for a while until May 1994 and haven’t been able to work since. Yet my immune system fires off all cylinders all the time. I never–NEVER–catch illnesses going through the community; cuts and burns heal immediately without scars; and I eat foods that are covered in mold and are otherwise well into decomposition (because I can’t get out to shop & therefore dare not throw away what I have) with never so much as a stomach ache, much less food poisoning. I don’t know anyone else as impervious to illness from external causes as I am–which is clear evidence of a powerful immune system–yet ME/CFS took me down 35 years ago and has never let me go.
I hope those with connections to the researchers will at least report my situation, before everyone signs off on immune function being the determinant of disease longevity.
I think your story indicates, like others have, that there must be subsets in this disease.
Have any study been done where mice (without immune systems)
have been innoculated with serum or plasma from ill patients?
What a tremendous site (and community) you started here Cort.
Thanks. I don’t think it has but hopefully it will.