

The “Global Pain” Diseases
There are two kinds of “pain” in fibromyalgia. There’s a more ordinary kind of pain – the burning, stabbing, aching, etc. usually associated with some type of injury (even though no overt physical injuries are present in FM), and then there’s an unusual kind of stimuli induced hypersensitivity generated by such things as lights, odors, touch and temperature.

Harte can readily explain the first kind of pain; it comes from the central nervous system. Enhanced pain signaling (central “sensitization”) in the spinal cord and brain causes non-painful stimuli (such as touch or movement) to register as painful- he’s having more difficulty explaining this second kind of pain. That’s because sensory signals like lights and odors bypass the spinal cord where the pain augmentation process in FM is believed to begin. Lights and odors go from the eyes and nose directly to the brain.
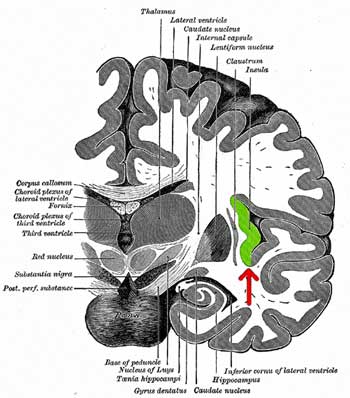
There is a central stimuli processing place in the brain, though, where all these signals merge. Called the insula, it seems to struggle with pain signals in FM as it ramps up its activity when faced with even mild signals. It’s as if it can’t figure out how to deal with them.,Over-reactive insulas have also been found in chronic fatigue syndrome (ME/CFS).
The goal of this study was to see if the insulas of people with fibromyalgia went a little bananas when faced with sensory stimuli. Sixty-two people (42 with FM) were given a pain stimulus (pressure-pain thumbnail test) and a visual stimuli test (flashing blue/yellow checkerboard) likely to be perceived as unpleasant by FM patients. During the visual test, 44 people were given a functional MRI (fMRI) at the same time to see which areas of their brains were being affected.
Seventeen study participants also participated in a double-blinded Lyrica trial to see how Lyrica affected brain functioning in FM. That study, whose results are not published here, found that Lyrica did indeed normalize insular functioning.
Results
One interesting takeaway from the study. Lyrica reduced the insula hyperactivity in response both to pain and visual stimuli. That indicates that one drug can help with both pain and stimuli issues. The study may also explain why Lyrica is only somewhat effective in FM: the neurons in the insula that drive FM pain are a bit different from the neurons that Lyrica affects.
The researchers hope to use their protocol to identify drugs that are more effective. Because FM is a disorder characterized by poor integration of stimuli (pain signals, lights, sound, etc.), they believe that simple visual stimuli tests could be used to target drugs that effect all the kinds of pain that FM patients experience.
Complex Illnesses
The insula is a “higher-order” brain organ; in fact, it’s the end of the road for sensory integration in the brain – it’s where researchers believe the brain forms a complete picture of the body.
One of the most interesting organs in the brain, the insula plays an important role in both physiology and emotion. The insula is in charge of adjusting the body’s physiology (heart rate, temperature, blood sugar, etc.) is associated with awareness and cognition and lights up in the presence of fear. It’s also involved in determining “anticipation”; i.e., if just the thought of doing something makes you feel ill, that could be your over-active insula talking.
The insula, however, is not where the sensory problems in FM begin. An earlier study indicated that under-activation of more basic stimuli processing areas in the brain called the somatosensory cortices may lead to over-activation of the insula.
The insula hyperactivity in FM isn’t confined to the insula either; a hyperactive connection between the insula and another area of the brain called the “Default Mode Network” (DMN) is also associated with increased pain in FM.
The study demonstrates a central problem in FM: researchers have yet to identify the core brain or other problem that lies at the heart of FM. The list of brain problems found in FM is a long one: gray matter reductions, amped up pain producing and tweaked pain reducing central nervous system pathways, altered connectivities between different parts of the brain, and hyperactivity of the insula. A recent study which found baroreflex problems suggests that problems standing (orthostatic intolerance) is probably common as well.

The study also underlies the potentially vital role fibromyalgia could but isn’t playing in chronic pain research. FM has the grace of being one of the only “pure” chronic pain conditions. Unlike rheumatoid arthritis, low back pain, or complex regional pain syndrome, researchers don’t have to account for damaged hands, back injuries or inflamed limbs when trying to understand a complex pain syndrome. At least right now, FM is largely believed to simply be a multisensory pain processing system run amok.
Because FM is “purer”, studying it should make it easier for researchers to get a clearer picture of how pain processing can go awry. That understanding would not just benefit FM patients, but virtually every other chronic pain condition. Harte noted that the study reinforced their “hypothesis that a global state of CNS sensory amplification may play a role in the pathogenesis of chronic pain disorders”. Unfortunately, with the NIH still spending pennies on FM research (it’s one of the NIH’s poorest funded diseases), that opportunity is largely being missed.






Interesting! NOW HOW DO WE GET MORE FUNDING????!!!!
We fight for it. In particular we get the NIH to do an Institute of Medicine report on gaps in research funding. That – a report from a respected source – really helped in ME/CFS.
Also, I really think if we did a comprehensive approach which shows that the NIH is neglecting many “women’s” diseases which cause a lot of distress but which do not kill could be really effective. Burden of illness is becoming a bigger thing and the NIH is completely ignoring it in these diseases.
Funnily enough I my mind was wandering onto a related issue this morning. In Britan the mottos is Cancer is king, therefore cancer gets vast funding both in research and in treament despite tiny returns (often around three years of less of impaired quality life).
At the same time there is a growing mood in the public that people with intolerable pain or intolerable quality of life should not have to go to Dignitas in Switzerland to choose to end their life humainly.
Nobody as yet though has joined the dots and thought ‘If these illness cause death to be a better option, they should be prioritised as though deadly’.
Of the six people I know personally and well that suffer ME, four are severe. Of those one actively wants to go to Dignitas, one is hovering. Three with severe ME and one with moderate ME think their lives are fairly pointless and unfullfilling.
The one with severe ME who lives a more fullfilling lifestyle is able to do so only due to very high finanical support from parents (they bought an adapted bungalow, a high quality motor scooter, expensive tools for hobbies et-cetera.
The cost to society from diseases like ME/CFS and FM which cause people in their working years to have to stop working is surely greater than for cancers which show up when we’re elderly. If the big funders would figure “burden of illness” into their calculations things would change.
I have had fibromyalgia for over 30 years. I just turned 78. I have also been using lyrica for over 20 years. It’s effectiveness has decreased considerably, but there has been little done to find a replacement. The fibromyalgia started with severe migraine headaches. Those have disappeared over time. I just had an MRI done of my brain. I have been having memory problems. After consultation with a neurologist who put me through some verbal memory quizzing, diagnosed me with onset dementia. I am wondering if there might be a connection in these diagnoses.
Unfortunately the hoped for replacement – mirogabalin – the expected replacement for FM – unexpectedly failed (!) – https://www.healthrising.org/blog/2017/07/08/mirogabalin-fibromyalgia-drug-fails/
There is Pridgen’s drug combo to look forward to (trial next year)..
I don’t know about dementia but given the cognitive problems I experience when I overdo it – I wouldn’t be surprised at all. We need a lot more studies!
Dr. Pridgen believes there is a connection.
I hope you are aware that memory problems are an integral part of this disease. You need to see a Neuro Psycologist and have them determine whether you have a new diagnosis of dementia or you are really having symptoms of fibromyalgia. I also have Complex Regional Pain Syndrome with my Fibro. There are definite cognitive problems associated with these diseases and it’s important for you to get a good diagnosis. I r perienced rxtreme memory problems 24 years ago when I was first diagnosed which one therapist compared to a stroke patient. When your bodies symptoms have so many messages to interpret it can become overwhelmed and start shutting down. It’s similar to a gate keeping theory where it will only allow a certain amount of stimulus be interpreted and then it shuts down. Good luck and I hope you get solid answers soon.
I had to do a double take on the $1 a year for each person!
I cannot take any of the three f/m drugs d/t severe side effects. I am now after years of struggling with this down to standing/walking only eight minutes at a time per my physical therapist because after that my system becomes overwhelmed again.
I can remember recently reading a piece of research that confirmed a long standing hypothesis of mine that the Thalamus was involved in ME sensory issues. That showed lowered ‘Thalamic Volume’ – in other words ours are smaller.
The Thalamus is responsible for signal damping and filtering of all our senses. It’s the bit of the brain that stops people hearing trains when they live next to a railway line.
I wonder how the Thalamus and the Inula relate both functionally and in terms of nervous system wiring? I.e. does the sensory nervous system first connect the the Inula and then the Thamalus, or first the to the Thamalus and then the Inula?
Since they are both showing abnormal levels of activity, that order of wiring may indicate which is causing the issue.
Hi Brian, I too have been interested in the thalamus for several years. That, plus a similar interest in connectivity (increased or decreased) between the thalamus, insula, ACC, amygdala, sensory cortex, dorsolateral PFC, medial PFC, etc.
A little over a year ago, my pain and tinnitus reduced massively after a course of high dose vitamin D3 (plus cofactors like magnesium, K2, zinc, boron). At the time I attributed this improvement to reductions in inflammation (via TREG induction, etc); the thalamus and insula were not on my mind at the time. Now I think modulation of connectivity may be involved. D3 improves myelination and the production of various nerve factors (e.g. BDNF, GDNF, NGF).
My D3 levels got too high, so I stopped for awhile. The pain didn’t come back. I’ve since resumed D3 supplementation at a more reasonable level (10,000 IU most days) and have been experiencing a reduction in hypersensitivity to sound, light, and emotional faces.
Thank you Cort, great article. I can’t tolerate Lyrica but am so glad I can use the Alpha-stim device. I’ve had FM for 28 years. As well as pain I used to have sensitivity to light, sound, smells and vibration. I had major difficulty coping with the London underground. Now thanks to microcurrent cranial electrical stimulation (CES) I have no problems on the underground. Perhaps CES is reducing the hyperactivity of the insula?
Hi Linda. I have had FM for 25 years. I tried ab Alpha-stim a couple of years back but didn’t feel it helped. I wish it would as it is preferable to medications. Acupuncture is helping at present.
Wow, another area of the brain 2 years ago it was the vagus nerve, which I am a guinea pig in a phase 2 research little off shoot study on Fibrmyalgia with the acupuncture needles in the ear tens stimulating the Vagal Nerve to relieve pain.
When I used it a little over 2 years ago there was some changes in my pain. Enough for me to undergo a Vagal Nerve Block which proved very helpful with severity PTSD,Anxiety, and Allodynia. As well as spinal pain and overall pain.
I just hope I get machine and not control group. Also, funny thing I had two diseases as a youth only people with compromised immunities get. And experienced Allodynia though not painfully long before Fibrmyalgia in symptoms in 91. Curiouser and curiouser.
Yo ya escribí en mi libro,UNA TEORÍA ATREVIDA. EDUARDO CASASNOVAS SUSANNA.
http://eljardindeloscuriosos.com/?a=libro&id=702&tag=una-teoria-atrevida, todo el tema de la Ínsula ligada al dolor y las sensaciones antes de ser enviadas al cerebro.
Curioso que poco a poco toda mi teoría se ve apoyada por nuevos estudios científicos.
Sin embargo tengo la sensación que el dolor pasa por la Ínsula como reflejo, no como receptora, quizás se satura. Podría ser que en la SQM sí actúe como receptora del dolor pero no en Fatiga Crónica ni en Fibromialgia.