

Researchers and doctors get interested in ME/CFS in different ways. Many have a personal connection, but for David Systrom, a pulmonologist, it was all about demand. He didn’t seek chronic fatigue syndrome patients out – quite the contrary. When Systrom was given control of a clinical cardiopulmonary lab, he started doing invasive cardiopulmonary exercise tests (iCPET’s) on people with exercise intolerance. Once word of that got out, chronic fatigue syndrome, fibromyalgia, POTS and other patients starting pouring in.
It wasn’t the patients seeking Systrom out – it was their doctors; they finally had a place to send their strange exercise intolerant patients to. Rheumatologists, cardiologists, neurologists, and infectious disease specialists have gladly sent their patients his way for years. It’s not a small number. Systrom suggests that 10 percent of people with exercise intolerance fit this profile. Those referrals have lead to 1,500 highly sophisticated exercise tests, about 700 of which were done on people with ME/CFS/FM/POTS.
Systrom’s had his eye on chronic fatigue syndrome (ME/CFS) for a while, but up until now he’s been looking at exercise intolerance in general. That’s why, despite the fact that he has one of the biggest, and certainly the most sophisticated, database of exercise results in ME/CFS, he’s mostly unknown to researchers and patients.
Armed with a grant from an anonymous donor to The Solve ME/CFS Initiative (SMCI) to support his work, Systrom, is for the first time focusing a study solely on ME/CFS.
Invasive Cardiopulmonary Exercise Testing (iCPET)
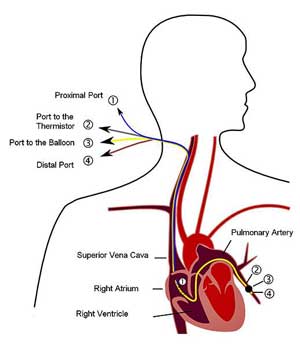
Systrom has taken exercise testing in ME/CFS to the next level with his invasive cardiopulmonary exercise testing (iCPET). Non-invasive cardiopulmonary exercise (CPET) testing can do a lot of things. It can demonstrate that exercise intolerance is present, define the aerobic and anaerobic contributions to exercise, determine if lung problems are present and others, but with an iCPET researchers can dig much deeper.
Systrom’s an acknowledged expert in the iCPET field; in 2013 he was the senior author of the first review paper on iCPET and in 2016 he co-wrote the first methodology paper explaining how to do it correctly.
Invasive CPET’s involve the insertion of catheters into the pulmonary artery and radial arteries that monitor blood flow, oxygen content and other factors. These catheters allow researchers to determine if the problems with oxygen are occurring in the lungs or in the muscles, where oxygen uptake is occurring and so on. Because iCPET can determine changes in venous blood O2 occurring with exercise, they’re able to determine how much oxygen the muscles are using. The technique can therefore be used to diagnose mitochondrial issues.
iCPET tests needed to identify three under-recognized causes of exercise intolerance, the third of which concerns ME/CFS: preload failure or the inability of the blood vessels to provide the heart with enough blood to pump effectively. Several studies suggest that preload failure is causing the small hearts in ME/CFS.
In the 2013 review article Systrom explained what happens (or should happen) when we exercise.
- Muscles need oxygen to generate energy.
- During exercise, increased breathing (ventilation) in the lungs and increased gas exchange between the lungs and blood provides more oxygen to the blood.
- First the heart increases it’s stroke volume so that it can shoot more blood out to the muscles.
- Once the heart maximum stroke volume is reached, the heart rate begins to increase in order to pump out more and more blood.
- In order to provide the increased levels of blood to the heart, the veins leading to it enlarge so that they can accommodate more blood.
It’s All About Oxygen
First, aerobic (oxygen-oriented) energy production mostly prevails. When the limits of aerobic metabolism are reached, though, one’s “anaerobic threshold” is reached. At that point, a non-oxygen way of producing energy called anaerobic metabolism becomes prominent. Two toxic byproducts of anaerobic metabolism, lactate and CO2, build up and cause fatigue, pain, etc. (Anaerobic thresholds are identified during the CPET test by an abrupt increase in CO2 levels). Here’s the key part for ME/CFS, FM and POTS patients from Systrom’s 2013 paper:
“People with low anaerobic thresholds; that is, people who quickly exhaust their ability to generate energy aerobically and rapidly enter into anaerobic metabolism have one of two problems: either the oxygen isn’t getting to the mitochondria in their muscles or the mitochondria aren’t taking it up….
THREE PATTERNS
In a June interview, Systrom stated that about half of his patients have POTS/ ME/CFS or FM. When he tests them, a couple of different patterns show up – a pattern of dysautonomia, which reflects problems with the blood vessels, and reduced oxygen uptake pattern reflecting other problems.
- Dysautonomia – the primary problem is inadequate venoconstriction; i.e. the autonomic nerves are not constricting the veins enough to propel sufficient amounts of blood (i.e. oxygen) to the heart for exercise or other activities to take place. Damage to the nerves in the arteries may be present as well.
- Reduced skeletal muscle oxygen uptake -the mitochondria are not taking in as much oxygen as they should.
- Genetic issues – are not nearly as common as the other two, but Systrom can at times find genetic issues.
TWO MAJOR PROBLEMS
(1) Dysautonomia, Small Fiber Neuropathy and Autoimmunity
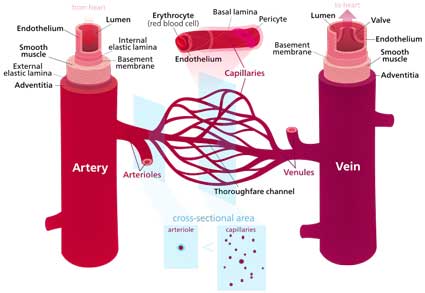
A recent study suggests he may be right. That study found damage to the autonomic nerves regulating microcirculatory blood flow to the lungs in fibromyalgia. Every measure of lung functioning (carbon monoxide transfer factor, carbon monoxide diffusion capacity, alveolar capillary membrane volume and pulmonary capillary blood volume) was significantly reduced in fibromyalgia patients. Further analyses found that the reduction in lung diffusing capacity was probably due to a significant reduction in lung capillary volume; i.e. the microvascular volume of the FM patients’ lungs had declined.
The authors proposed that the receptors on the endothelial cells that cause FM patients’ blood vessels to dilate have been so overstimulated over time that they’re not responding to signals to dilate anymore. That leaves them constricted and results in reduced blood flow.
Systrom regularly does autonomic nervous system testing in his patients. Skin biopsies demonstrate autonomic nerve loss in approximately 70% of his ME/CFS/FM/POTS patients. (He’s apparently the first to start looking for SFN in ME/CFS). He uses classic rheumatologic serology to look for signs of an autoimmune disease such as Sjogren’s (lip biopsy) and Guillain-Barre Syndrome. He uses a paraneoplastic antibody panel from the Mayo Clinic to look for more esoteric autoantibodies. Autoantibodies to acetylcholine are showing up frequently. Acetylcholine is a neurotransmitter needed for muscle function and is the major neurotransmitter in both branches of the autonomic nervous system.
Ganglionopathy
When the skin biopsies turn up negative, Systrom turns to a ganglionpathy (damage to a nerve ganglia) that’s presenting an impediment to blood flow – to explain what’s going on. Nerve ganglia are structures that contain numerous nerve cell bodies. An active EBV or other infection (aka Van Elzakker’s vagus nerve infection hypothesis) or a hit and run infection that could be damaging these ganglia.
(2) Reduced Oxygen Uptake
Because Systrom has the ability to measure blood oxygen levels prior to and after the muscles have used it up, he can tell how much oxygen the lungs are taking in and how much is left over after the muscles have taken it. He’s finding that the blood oxygen levels in ME/CFS patients’ veins are simply too high; i.e. not enough oxygen is being taken up by their muscles when they exercise. The oxygen is in the arteries, but the muscles are not taking enough of it up. That’s a big clue.
The Gist
Systrom has built an extensive database of exercise results in ME/CFS/FM and POTS using invasive cardiopulmonary exercise tests
Systrom’s studies indicate two main problems are present. Autonomic nerve problems are impeding blood flows in the veins and probably the arteries and reduced oxygen uptake at the mitochondria is present.
The autonomic nerve problems in the endothelial cells lining the veins is probably responsible for the reduced preload and small hearts found in several ME/CFS studies.
The autonomic nerve problems are likely related to and a continuation of the small fiber neuropathy found in FM. Systrom has found evidence of extensive SFN in ME/CFS and POTS patients as well. Systrom is working with Anne Oaklander to investigate the SFN in these diseases.
Systrom believes the autonomic nerve problems are probably caused by an autoimmune process. Antibodies to acetylcholine are showing up in his tests.
Reduced oxygen uptake at the mitochondria is reducing energy levels and causing toxic byproducts to accumulate during exercise. The reduced oxygen uptake is probably due either to damage to the autonomic nerves lining the arteries, to a shunt that is depriving the slow-twitch muscles of blood or problems with mitochondrial energy production. Reduced oxygen uptake is found in about 80% of his ME/CFS/FM/POTS patients.
Most people with these diseases hyperventilate during exercise resulting in increased CO2 levels, fatigue and other symptoms. Systrom believes the hyperventilation is probably due to small fiber neuropathy and problems with the metaboreflex.
Systrom has found Mestinon (pyridostigmine bromide) very helpful in his exercise intolerant patients.
Systrom’s new study funded by an anonymous donor will attempt to get at the molecular heart of the exercise intolerance occurring by measuring metabolites three times at two different parts of the body during exercise.
Systrom suggested that damage to the adrenergic nerve fibers resulting in problems in the arteries (similar to that occurring in the veins) could be hampering blood flow to the muscles. Failure to divert enough blood to the slow twitch muscle fibers could also be resulting in a “de facto microcirculatory L-R shunt” which causes blood pooling and reduces blood flow to the mitochondria. Mitochondrial problems all by themselves are another possibility.
This isn’t the first time low oxygen uptake to the muscles has been found in ME/CFS. Natelson and McCully found the same way back in 1999 and in 2003. They attributed the low oxygen delivery and alterations in blood flow to autonomic nervous system issues. Low oxygen uptake also fits well with metabolomic and exercise study findings suggesting that low energy production is present. Systrom finds low oxygen uptake in about 80% of his ME/CFS, FM and POTS patients.
Hyperventilation, Exercise and Dysautonomia – When I asked him about exercise, he noted the huge interplay between dysautonomia and the hyperventilation he commonly finds during exercise in many ME/CFS/FM/POTS patients. Systrom finds that the overwhelming majority of patients hyperventilate during exercise.
That hyperventilation is probably being caused by a dysfunction of the small nerves that regulate the metaboreflex. The metaboreflex increases blood flow during times of low oxygen by increasing heart rate and heart contractility. (Perhaps an over-reaction to low oxygen environments occurring during exercise cause increased heart and breathing rates; i.e. hyperventilation?) However it happens, rapid breathing or hyperventilation increases CO2 loss through the breath and lowers blood CO2 levels during exercise, causing pins and needles, brain fog, fatigue and other problems.
How CO2 is being regulated in ME/CFS/FM/POTS patients is another subject of key interest to Systrom and his team.
Treatment
Mestinon
An old and not much used drug called Mestinon (pyridostigmine bromide) has, surprisingly, turned out to be Systrom’s ace in the hole regarding treatment. He’s treated hundreds of patients with it over the past three years. Some people find that the drug has given their life back.
As often happens, a single patient helped produce a major treatment breakthrough for him. It has, Systrom said, “really helped many people”. The Mestinon saga started with one of his most difficult POTS patients – a man with known mitochondrial myopathy and extensive dysautonomia. He’d been in and out of the hospitals, but his million dollar workup had availed him and his doctors little: he was just the kind of patient that Systrom typically sees:
After comparing notes with a Toledo neurologist, Systrom tried Mestinon and couldn’t believe how much better the patient got. After that, Mestinon’s become a cornerstone of his treatment plan for exercise resistant patients with autonomic nervous system problems. He can chart the results – an increase in aerobic functioning – in followup iCPET tests. (Mestinon might conceivably be helpful with small fiber neuropathy, as well.)
Mestinon doesn’t do anything for the mitochondria, but by promoting better nerve firing it increases blood (and oxygen) flow to the mitochondria in muscles. It also increases blood volume. It may even be healing small fiber neuropathies.
He occasionally finds treatment-resistant Mestinon patients, but not often. Side effects can include gastrointestinal issues and diarrhea and twitching muscles….If these happen he suggests that patients take a drug holiday and start again. I asked him about someone I knew who experienced severe exhaustion on Mestinon – he indicated that that was very rare.
While on Mestinon, he has his patients slowly build up their exercise regimen. Using a recumbent bicycle is best. Short-term, high intensity training might be helpful as well, but he doesn’t have enough data on that.
Other second-tier treatments include
-
-
- Florineff – See Florinef for Chronic Fatigue Syndrome
- Midrodrine – see Midodrine for Chronic Fatigue Syndrome
- SSRI’s
- Atriatide – redistributes blood flows away from the gut
- Intravenous IgG / Rituximab – (requires solid evidence of SFN)
-
Systrom’s First ME/CFS Focused Study
Funded by a (really smart!) donor, Systrom’s ME/CFS study is being run through The Solve ME/CFS Initiative (SMCI). Using the invasive CPET Systrom, Systrom will be able to sample the blood in two body locations at three time points. He’ll be trying to get at the molecular basis of the problem for the first time.

Through his proteomics and metabolomics tests Systrom is trying to get at the molecular roots of the exercise intolerance seen in ME/CFS
Not only will Systrom be getting information on exercise (heart rate, anaerobic threshold, ventilation, etc.) but he’ll be directly measuring the metabolic changes occurring during exercise as well. Unusual metabolites showing up during aerobic respiration could provide clues, for instance, that could indicate how aerobic energy production is broken in ME/CFS. He’ll also be looking for protein biomarkers using proteomics. He hopes the plasma signatures he finds will help uncover the underlying pathogenesis behind chronic fatigue syndrome (ME/CFS). He’s also hoping to identify which patients benefit from IVIG.
It’s encouraging how many researchers are beginning to circle around the blood vessels. Fluge and Mella are testing endothelial cell (the cells that open and close blood vessels) functioning in both the large and small blood vessels in their Rituximab study. They believe blood vessel problems are preventing sufficient amounts of blood getting to the muscles.
Their endothelial cell Rituximab substudy will determine if endothelial cell functioning – necessary for proper blood flow through the muscles – is associated with severity and if Rituximab enhances it. If Rituximab does improve blood vessel functioning, it may be killing the B-cells that are producing autoantibodies that are whacking the blood vessels. A cardiovascular study is also reportedly underway at Stanford.
As we’ve seen, Systrom also believes an autoimmune process attacking the blood vessels is underway. The finding last year that autoantibodies to the adrenergic receptors on endothelial cells are present in postural orthostatic tachycardia syndrome (POTS) suggests a similar process is occurring in POTS patients.
Nobody can yet prove that ME/CFS is, at least in a part, an autoimmune disorder, but we seem to be hearing the word autoimmunity with increased frequency these days. Recently Dr. Mark Davis reported that everything he’s seen immunologically suggests ME/CFS is an autoimmune disorder. Ron Davis reported that his filtering experiments suggest that the problematic factor in the blood that appears to be messing with energy production in his tests is an autoantibody.
Systrom considered applying for the NIH Research Centers grant but decided that the small amount of money the NIH provided wasn’t enough to justify creating a research center; he believes applying for single ROI grants will be more cost-effective.
With his extensive database on exercise results, his interest in exercise intolerance and now his grant from an anonymous donor, Systrom is like a gift that is falling into our laps. Hopefully, with this grant to the SolveME/CFS Initiative (SMCI), Systrom will edge himself more and more into the ME/CFS/FM research community and we’ll see much more of him in the future.







I find this really surprising as testing for autoantibodies to acetylcholine are also a way to diagnose myasthenia gravis, one of the illnesses that needs to be excluded before diagnosis of ME/CFS can be made. One would think that majority of people with ME/CFS would have already gotten this test done.
Unfortunately, I was negative to acetylcholine and muscarinic receptors and mestinon did nothing for me. Maybe because I’m severe? I assume severe ME patients would never find their way to Dr. Systrom.
Yes, they are. I’m pretty sure that I haven’t had the test done but I haven’t had the workups that many have. Here are the tests that can be done in Mayo’s Paraneoplastic panel. One of the reasons for the panel is
“Differentiating autoimmune neuropathies from neurotoxic effects of chemotherapy”
ANN1S Anti-Neuronal Nuclear Ab, Type 1 No Yes
ANN2S Anti-Neuronal Nuclear Ab, Type 2 No Yes
ANN3S Anti-Neuronal Nuclear Ab, Type 3 No Yes
AGN1S Anti-Glial Nuclear Ab, Type 1 No Yes
PCABP Purkinje Cell Cytoplasmic Ab Type 1 No Yes
PCAB2 Purkinje Cell Cytoplasmic Ab Type 2 No Yes
PCATR Purkinje Cell Cytoplasmic Ab Type Tr No Yes
AMPHS Amphiphysin Ab, S No Yes
CRMS CRMP-5-IgG, S No Yes
STR Striational (Striated Muscle) Ab, S Yes Yes
CCPQ P/Q-Type Calcium Channel Ab No Yes
CCN N-Type Calcium Channel Ab No Yes
ARBI ACh Receptor (Muscle) Binding Ab Yes Yes
GANG AChR Ganglionic Neuronal Ab, S No Yes
VGKC Neuronal (V-G) K+ Channel Ab, S
Test ID Reporting Name Available Separately Always Performed
GD65S GAD65 Ab Assay, S Yes No
WBN Paraneoplastic Autoantibody WBlot,S No No
ARMO ACh Receptor (Muscle) Modulating Ab No No
ABLOT Amphiphysin Western Blot, S No No
NMDCS NMDA-R Ab CBA, S No No
AMPCS AMPA-R Ab CBA, S No No
GABCS GABA-B-R Ab CBA, S No No
NMDIS NMDA-R Ab IF Titer Assay, S No No
AMPIS AMPA-R Ab IF Titer Assay, S No No
GABIS GABA-B-R Ab IF Titer Assay, S No No
NMOFS NMO/AQP4 FACS, S Yes No
NMOTS NMO/AQP4 FACS Titer, S No No
CRMWS CRMP-5-IgG Western Blot, S Yes No
LG1CS LGI1-IgG CBA, S No No
CS2CS CASPR2-IgG CBA, S
Can you say that in English 🙂
All very clever…..does cfs just bring on the desire to use big medical words……how about just keeping it more understandable.
My wife has cfs symptoms and is wearing me down
What on earth can be done to alleviate…..we are circa 75 are we destined to spend rest of our life with it??
I try my best to make it understandable but talking about the research requires using the words that describe it. I wouldn’t say you’re destined to have this for the remainder. I think significant improvement is possible.
Actually I made a mistake with the auto antibodies. Auto antibodies against the acetylcholine receptor, ganglionic variety are showing up now and then, not the autoantibodies, apparently, to myasthenia gravis.
Low titers of g-AhCR antibodies are found in 5% of the healthy population, and about the same percentage of POTS patients. Low titers are not associated with the. severity of autonomic symptoms seen in POTS, per Mayo researchers who discovered the antibodies and looked for them extensively in autonomic disorders like POTS.
More likely, the muscarinic receptor 1-3 (and possibly 4) antibodies are a possible culprit. These have been found in almost all POTS patients tested to date. However, they do not explain the sympathetic excess, to if they do occur, it is likely in the presence of adrenergic receptor antibodies, which have also been found in almost all POTS patients tested to date. Steven Vernino, the guy who discovered the g-AChR antibody, is currently working on muscarinic 1-3 antibody research in POTS.
Where is this doctor? Sorry if I missed it in the article.
brigham young in MASS.
Brigham and Women’s Hosp in Boston, MA (not Brigham Young).
What’s the name of the neurologist in Toledo, OH?
I got an appointment with Dr. Systrom. My treating physician is at Brigham and the earliest I could see him was a year out in July 2020 which of course was canceled due to Covid-19. I haven’t been rescheduled yet. My drive is 3 hours to be treated by doctors who know and believe that these illnesses are real and that did the complete workup that Cort described. I was found to have residual problems from TBI, SFPN, Long Fiber Neuropathy of the upper body, and POTS by Dr. Novak who is a specialist in POTS. All the doctors that treated me in Boston all had PhDs, even the person who did the EMGs, and my local physicians back home treated me even worse because of their insistence that it was all psychosomatic. Doctors don’t like to be embarrassed. Hoping to see Dr. Systrom this year. Also, you can have muscles act like Myasthenia Gravis but don’t have it. For Instance, my 3 sleep studies showed that my diaphragm muscles lost signal from the brain causing central sleep apnea. This loss of signal is consistent with Myasthenia Gravis.
So interesting – thanks for relaying that Paul. Long fiber neuropathy as well and I hadn’t heard of the diaphragm muscle issue….That is really something. I hope you can see Systrom.
Are you sure it is not autoantibodies against the nevrotransmitter acetylcholin it self and not autoantibodies against the reseptor he is taking about? This is an important difference. I do not think it is commen to test for autoantibodies againt the nevrotransmitter when suspected M. gravis, but against the reseptor
I asked my Dr about trying Mestonin last year and he said that my magnesium levels were too low for it to be safe. I don’t think I asked why this was relevant but maybe someone here knows??
One website said it does interact with magnesium “Mestinon may interact with other medications, including succinylcholine, magnesium, methocarbamol, corticosteroids, local anesthetics, and aminoglycoside antibiotics. ” but I haven’t been able to find any specific interactions with it yet.
We are perpetually in magnesium deficiency
Get magnesium shots to boost M most effectively at the cellular level. Dr Cheney and MyHill recommend .1cc of MG and Taurine injected 2x a day
Incidentally I do well on Choline supplements.
Very interesting, is there a published research protocol for Systrom’s ME/CFS study?
Not that I know of. I would like to have one actually. 🙂
thanks Cort
Is Dr. Systrom still accepting patients into his study??
I don’t know but I doubt. The study is a small one – 20 patients and I’m not clear how many controls.
I thought Ron said it wasn’t an autoantibody. I’ve prob got it wrong. He did say it was a high molecular weight ‘ something’. A lot of people at the conf were implying a ‘something’. Thanks for this Cort, you do a great job !!
Well, one of is right. For the sake of everyone I hope it was me! 🙂 🙂
Ron Davis said that when he filtered the serum the impedance went down to normal, same as for healthy controls. Which means whatever was filtered out has to be bigger than the “sieve” they used. He also said that autoantibodies fit this size.
So his test has shown it could be autoantibodies or it could be anything else which is similar in size.
Thank you for clarifying Tally
I would suggest that you look at useing Low Dose Naltraxone ,look at LDN Reaserch Trust for the information that gave me my life back.
I put my Mom on LDN for stage 4 lung cancer 6 years ago and she is still cancer free. This is not prescribed by internists, primary care or an mainstream MD that I know of. Can you share how you came about this medication?
I think this is very promising work that dovetails nicely with Fluge/Mella.
Much more promising than most… (I think the immune research has kind of run its dash, although I am sure it will have some use/relevance)
Very interesting. Thanks Court! The consultant at the heart centre isn’t going to know what hit him at my next appointment! Whether they will prescribe Neston in for me or not is another matter. I’m on a low dose of Midodrine which helps the ‘little faints’ but the it doesn’t stop the big ones or the days where I repeatedly faint for 8 hours or so….. Fingers crossed this research gets going soon then crosses over into mainstream medicine ASAP.
Fingers crossed indeed. I love that Systrom is trying to get at the molecular roots of this now. I hope he hooks up with other ME/CFS researchers – and kudo’s to anonymous donor who decided to fund him. Time will tell but that person may be making a huge difference.
This is really encouraging findings. When I first became ill (5 years ago) I tested positive for the ‘autoantibodies to acetylcholine’. The doctor was perplexed by the results as I showed no outward physical symptoms of Myasthenia Gravis. Thinking the test results could somehow have been switched or were wrong he ordered a second test. Again it was positive. From there I was sent to one of the top specialists dealing with Myasthenia Gravis in London who after yet a further 3rd test (also positive) and two days being tested in hospital it was agreed I did not have myasthenia gravis. Still, I had severe CFS/ME.
I would very much like to try ‘Mestinon’ and wonder if it’s available from a GP in the UK. I’m going to look into it.
Thank you Cort for the great articles that bring hope and a little light to what can be a very dark and long tunnel.
Interesting Karin. Good luck with your search!
Hi Karin, I was wondering how you got on with trying Mestinon?
I constantly ask, every time there are new findings like these; could the explanation still be in muscle and fascia tightness, a consequence of something else (such as hydration and renal system issues). I don’t think it has ever been possible to exclude this hypothesis. Dysfunctions being studied may in fact be “downstream”, whether in the Central Nervous System or the Immune System – these dysfunctions can be triggered, can they not, by their “flow” and “signal” mechanisms being blocked by actual biomechanical issues?
Resolving the biomechanical issues, if possible, may lead to the CNS and Immune systems healing themselves? I have FM not CFS, but working on hydration and detoxing and mineral balance; and carefully paced exercise to build the “low aerobic threshold” and avoiding going anaerobic with its toxicity implications; and a diet intentionally depriving the muscles of “dirty” carbohydrate fuel; over the last 4 years now, I have made steady improvement (and this is after 25 years of debilitation and decline). There are other elements as well, I believe I have a wholistic protocol that works on the assumption that basic intuitive nursing of the muscles and especially the fascia, and being careful about what “feeds” the fascia (reducing “bad” feeding i.e. toxins, and increasing “good” feeding i.e. hydration) allows the other nasty complex issues that researchers are delving into, to resolve themselves.
Philip, your post makes the most sense to me at this time. I’ve dabbled with a similar path. I would love to get more info on the folks u learn from or protocol. I’ve had CFS/ME with O.I. for 17 years. Dr. Myhill books help and a keto type diet I guess bypassing the Glucose pathway or something. I think Ron at Stanford is studying this too. Can I email or fb u to get more info by chance?
Could bloodthinners be useful for bloodflow problems? Cort? Anyone?
Interesting question. Dr. Holtorf uses heparin in his patients and some studies years ago suggested thick blood was present.
At my worst, 12 years ago, I had super thick sludge for blood. I was on heparin for a couple of years, as well as fish oil. I still take fish oil and have had no problems with blood thickness since then.
Inflammation causes thick blood. You can use low dose aspirin like mast cell patients do. It will give oxygen to your tissue and cells (and potential bacteria and virus hate oxygen).
Don’t combine it with other blood thinning supplements if possible.
Why on earth would Susan consider ingesting a synthetic drug based on fossil fuels which are nerve toxins if fish oil is working for her? Synthetic poisons which are ubiquitous in our drugs, foods and textiles are probably the largest source of inflammation in North America. The body must produce white blood cells to fight off these poisons – white blood cells die quickly as they fight to the death. If our lymph system is overburdened in getting rid of dead white blood cells, our blood suffers. The best thing to do is to avoid fossil fuel derivatives in our daily lives as much as possible.
Plasma proteins like albumins, globulins and fibrinogen make up about 8% of our blood plasma and are important to maintaining blood viscosity and blood pressure. It’s still my theory that ME involves underlying (various) connective tissue disorders and thus affects our blood plasma which is liquid connective tissue.
dejurgen – I think you’re on to something regarding measuring what’s going on in legs vs arms. To build on your thoughts, you may be interested in reading about exertional rhabdomyolysis; a condition where cell walls burst during overexertion and proteins flood the kidneys faster than they can be processed. Interestingly, anti-inflammatories will make the condition worse as these drugs also have to be filtered by the kidneys. Seems that temperature and hydration are important factors. Ehlers Danlos (a connective tissue disorder) patients are recommended to exercise in
water. Deep water’s hydrostatic pressure maintains blood pressure and keeps temperature stable throughout the body, maintaining proper blood flow.
I don’t know about CFS, but not for most POTS patients. The issue isn’t that the blood is too thick, it’s that the veins don’t constrict to push the blood back up to the heart. Also, many POTS patients have low blood volume, so I think a blood thinner would actually make our symptoms worse.
LY,
What “…synthetic drugs based on fossil fuels “ are you referring to?
I have had me/cfs-fibro for over 30 yrs. Long ago I took way too much advil rx and rx 12 hr enteric coasted aspirin till my stomach said no. now i manage ok with rotated chinese herbs that are from reputable comp and acupuncturist. You can take thinks like peonia, mastic, myrrh, siegesbeckia…-but they must be rotated and my herbs change super quickly now. I know when one isn’t working & I need another.
You may find this interesting. It’s an old thread and I recently updated it. https://www.dinet.org/forums/topic/15826-blood-letting-blood-draw/?_fromLogin=1#replyForm
Issie
Thanks, Cort. I haven’t found a link to the actual study that you’re referring to.
Most of the blog came from an interview. Systrom did do a big study that outlined his findings in this group of patients. You can read about it here – https://www.healthrising.org/blog/2016/07/04/exercise-intolerance-fibromyalgia-chronic-fatigue-pots-explained/
The next study will be the ME/CFS study that’s underway now.
The autoimmune angle certainly fits in my case. My illness(es) have come in a cascade over time, gradually adding yet another every few years.
Not sure if people are aware, but once a person has one autoimmune illness, they’re at much higher risk for another. That’s because in reality, it’s likely the same process simply manifesting in various organs or parts of the body.
I began with a diagnosis of Hashimoto’s hypothyroidism in the early 1990s, was eventually diagnosed with fibromyalgia in 1997, and by 2009 was suffering with significant CFS. I had no idea they were connected at the time, of course.
Over the last few years I learned a great deal about the origins & proper treatment of autoimmunity (hint: it begins with not eating gluten & healing the gut lining) & I saw some improvements. I lost weight without trying & my energy level improved slightly.
Then this year I took things to the next level by switching my diet to the AIP (autoimmune protocol of the paleo diet) & that has made a world of difference! I know I am settling down the autoimmune responses at the source. My energy & endurance is improving. My pain doesn’t scream as loudly. My antibodies (at least for my thyroid) are lower. If I had known all the other antibodies to check, I could watch those go down, too. I’m not cured because this is a chronic illness which requires diligence to manage. I must continue to pace myself, it’s just that the boundaries have expanded. I certainly still need to manage stress with smarts. But I’m grateful that now I’m able to stand in the kitchen more to prepare different kinds of healthy food. (In the past I couldn’t stand for more than a few minutes.) And I’m sleeping better. I’m even thinking about the possibility of tapering down a couple different meds.
The key point is that this approach is affecting the disease process where it begins. it is not simply covering up the end symptoms with a pill. If we don’t stop the autoimmunity, where in our bodies will the illness strike us next?! Now that’s gluten-free food for thought!
If anyone else has any of the commonly co-morbid illnesses I do, then working on your diet & lifestyle is certainly worth it. There is now a ton of information available on-line.
My best wishes to everyone on their own individual journeys.
Thanks for passing on your success Serenebeth. I had never heard of the autoimmune version of the paleo diet. From one website I see that it along with the usual victims it eliminates chocolate (!), eggs (ouch) Gums (guar gum, Tara gum, Gellan gum, Gum Arabic),Nightshades (tomatoes, potatoes, peppers, eggplant, paprika, mustard seeds, all chili’s including spices). Allows no vegetable oils (NOTE: olive oil, lard, palm oil, cultured grass fed ghee and coconut oils are permitted)and no culinary herbs from seeds (mustard, cumin, coriander, fennel, cardamom, fenugreek, caraway, nutmeg, dill seed)
That’s quite different!
I have dysautonomia and profound fatigue and muscle exertion problems in setting of Sjogrens Syndrome. I just started FODMAP for IBS-type sxs, Anti-Inflammotory Diet, and Allergy elimination diet. Noticing some benefit at this early stage in decreased gut problems, acid reflux, brain fog.
I too was diagnosed with Hashimoto’s disease in the 90’s. I read about micobacteria being the cause and that low dose long term antibiotics were being used to treat it. As I recall I was on doxycycline and tetracycline for a while. I also used heat when I felt pain in my thyroid as the indication was that the micobacteria had a thick waxy shell that protected them. My thinking was the heat would damage the micobacteria. I had Hashimoto’s for about ten years and have been free of it for about fifteen years. NO Pills. I think I have had minor fibromyalgia on and off for years. I think infection and maybe a quirky immune system is at play in many autoimmune disorders. The Hashimoto’s started after a real bad cold and sore throat though it took time to develop.
serenebeth I posted a comment below in the wrong spot. I too had Hashimoto’s disease for ten years and have been disease free for about 15 years. Please see below. I think at the root of most autoimmune disease is infection.
I’m a patient of his and have had this test. The test is rough(there is nothing fun or easy about having a neck catheter placed and a tube pushed down into your heart while 100% awake and then having to exercise on a bike) and I definitely wouldn’t recommend it to those who are severely ill. Kudos to the many patients who are willing to be guinea pigs for the sake of having better treatment available someday. Mestinon helped me a little bit with POTS for about 4 months and then it pretty much stopped working. It helps speed up gut motility if one has gut motility issues. Not quite sure why mestinon is working for some and not others. I imagine that it is a matter of severity and/or a matter of different root causes.
Good for you for getting through the test.
I am also a patient of Dr. Systrom’s and am currently 1 month post CPET – I have been on Mestinon for all of this time and have been having some side effects (nausea, dizziness, blurred vision and headaches) but have noticed that my intestines have woken up – that in itself is enough to keep me going for a while. I go back next week to do follow-up testing and speak with Dr. Systrom more. I am also a patient of Dr. Oaklander’s and feel positive about my future despite the failures in medication trials I have had thus far – so much work is starting to focus on SFN. I will post more after next week. Thank you, Cort, for writing about this. I have shared it with family and friends – it makes things easier to understand.
I am so glad that Dr. Systrom and Dr. Oaklander are working together on SFN in the skin – and apparently underneath it as well. Good luck with the Mestinon.
I am wondering how your experience and treatment has been under Dr. Systrom and Dr. Oaklander. Could you provide an update, please?
hi there, how did you get on with taking the mestinon? thank you
Hi Anne,
thanks for doing this heavy effort for all of us! It can’t have been comfortable at all.
I have a small but important question for me to understand this experiment: Am I wright that the only exercise done during the test was riding a bike and that two tubes were pushed into your body: one in the hart vein and one somewhere in the arm?
If so, it could be an important clue: the arm does not need to exercise that much in cycling compared to the legs so O2/CO2 levels at the arm (and to a somewhat lesser extend at the hart vein) could be having the opposite reaction of those at the leg muscles. Under this hypothesis the supposed too low blood flow could increase the blood flow way too few to the leg muscles by not being able too.
Hyperventilation/overbreathing could then be a small partial solution towards pushing as much as possible oxygen through this “too small highway lane to the legs muscles”. That would lead to rather high vein oxygen levels almost everywhere except in those leg veins where it would be quite a bit too low. If that would hold to be true, it would put things in quite another light (including overbreathing when not doing exercise).
Kind regards,
dejurgen
I am impressed with your intuitions, please keep contributing here. I have long been hypothesising that the exercise intolerance in fibromyalgia at least, is due to tissue tension and deformations, simply constricting the flow of blood through vessels, especially where they pass through the fascia.
I have also noted that cycling does not provoke anywhere near as severe intolerance and premature anaerobic condition, as weight-bearing exercise like walking or jogging. I hypothesise that the deformation of tissue and fascia and the blockage of blood flows, is more severe in the vertical position for some reason. Researchers should be investigating this.
I have noted in my own case, that my strength and stamina is highly erratic depending on posture; I could always do a seated leg-press of 400kgs but could not simply squat down (i.e. supporting my own body weight). I have been slowly gaining the ability to squat down (along with many other lost abilities) as I have been following my own multi-disciplinary protocol.
The extremely limited muscle range of movement is, I believe, due to muscle tissue at vital points, particularly around joints, being stuck together and forming painful clumps. Of course all vessels that have to proceed through these clumps, are constricted.
Hi Philip,
I too do better at *electrical* bicycling. I get the squat difficulties too: it’s very hard to get well balanced load on the body without “tension hot-spots”. Even for healthy people it is renown to be troublesome for injury. However I do better at low-strength low-speed exercises with balanced loading and few friction to the tendons. Seated leg press should balance load quite evenly over muscles/tendons/… with larger cross section, but still until today I would have avoid seated leg press as much as disastrous GET.
I may have been wrong. Well done, I envision it to repetitively send slow waves of contraction and expansion trough the entire legs and part of the abdomen. That’s basically almost everything beneath the hart e.g. more prone to blood pooling. In *ideal* circumstances a well controlled slow series of quite significant contractions and expansions could clear out part of the blood pooling, especially with the one-way valves in the leg veins.
If the exercise is done slowly and well below too much force, it would require modest energy needs, leading to only modest blood flow needs. The waves of expansion and contraction would act as a decent sized blood pump providing blood to the exercising muscles. In very ideal situation, this and the reduced blood pooling could reduce hart-preload problems and supply both exercising muscles and the rest of the body with sufficient blood.
Do you happen to have significant lower pulse at rest compared to when you were at your worst? Do you happen to be able to leg press with regular hart beat and breathing? Do you happen to get back to “normal” quickly (compared to other exercises) if you don’t exaggerate?
I’ll try and adapt it to my situation and see what I can do with it. Won’t use any weights anytime soon though. If I remember correctly you started out very slow and light too. Plenty could go wrong so I’ll be careful. Still, if it worked out you must have keen observation skills to have selected such unlikely exercise in order to improve.
Dejurgen; Yes, I think your explanation is right, I am very grateful that you have made sense of these contradictions for me. That is, squatting involves immediate full load, tricky balancing (requiring constant fast muscle corrections) blood pooling due to vertical position initially, and immediate loss of “blood pumping” by the muscles. A seated leg press involves no blood pooling because the legs/body orientation is almost horizontal on average, and the effort can be completely rationed and built up gradually, recruiting muscle fibres and “pumping” blood as you go.
I did not mean that I have used seated leg presses as part of my successful regime, I merely noted that I could press large weights all along even when at my worst with FM. I never did it very often. I also never checked my heart rate then. Perhaps I should do this sometime out of interest.
Everything I have concentrated on doing a lot, is “easy”. Mostly it is “cardio”, staying within 65% of maximum heart rate. And under these conditions I do recover very fast. In fact my “power” has steadily risen for the same heart rate, so that I even embarrass some very athletic people next to me in the gym, when I am sustaining the same power as them and my heart rate is much lower. But they can increase their effort and heart rate still more and completely out-do me in power output and calories burned, and I must discipline myself to not try and “compete”, just stay at the intensity level that will build and heal me, and not suffer relapses.
Yes, my resting heart rate is much lower now than it used to be. In fact I can produce quite reasonable power on an exercise machine now, while below the heart rate that used to be my resting heart rate! (It used to be 90 and it is now 60. I did lose a lot of weight too, thanks to low carb diet and “fat burning” exercise intensity).
To try and “train” myself in some of the challenging weight-bearing movements, I do a lot of these while in a large (public) spa pool. My muscles are warmed up and my body weight is partly supported by water. Squats are something I do a number of repetitions of. I also kneel, and bend backwards. I have many other movements which would be destructive “on the floor” but doing them in the spa pool is possible and therapeutic. I have been experimental, but also got a lot of ideas from Yoga and Feldenkrais. I have gradually become capable of more and more Yoga positions while “on the floor”.
One must focus on relaxation and stretching of muscles, but the rule is that the stretch must be “with the muscles relaxed”. Trying to go into positions where muscles are tense, just to do a stretch, means that damage is being done rather than therapy. While your fascia is still “sticky” and there are still a lot of knots and lumpy stuck muscle fibres, you have to remain within much more severe limitations. My gains have been very slow and gradual. It is important to be rehydrating and de-toxing the fascia, with diet and supplementation and mineral re-balancing (use Hair Tissue Mineral Analysis), and avoid generating toxic waste byproducts of exertion (by avoiding anaerobic exertion).
I am really pleased if others can get the same gains as me, by doing the same things. Sincere best wishes. I am also lucky that I made a career change 17 years ago that has made my life much more lower-stress. Stress reduction (somehow) is probably an essential ingredient.
In my experience, fire breathing in Kundalini yoga seems tonizygenate my muscles and free me to do more demanding exercise, though post fatigue can still be a problem.
Thank you for enduring the test! It will help all of us!
Thank you for participating in trial.
Years ago I had a test of my blood gasses done – no invasive catheters; it involved one poke in an artery (in a hospital – not to be done in a regular lab) and one in a vein. Why go all the way to the heart to measure venous gasses?
I get crazy from all the small studys (like 10 or 20 persons) that are not significant and where they allways find something instead of a few good large studys like montoya’s that are significant. And I also get crazy that almost no researchers are doing another ones study over at the same way to validate the results. And it makes me mad that (small studys) are even not capable off selecting by gender, age, lengt and severity of illness. And that with a desease with so many different definitions (criteria) and such a heterogene population off patients. What a waist off money…. I do not say that he did not a good job but the study from the solve cfs.org for 20 patient????
I feel your pain- but we are where we are; this is a donor funded study – and quite frankly we’re luck to have it. The donor has ME/CFS, found Systrom, liked what he’s doing and is funding more research. That’s a very pro-active patient; it’s also very unusual!
One thing that I didn’t put in the blog because I didn’t understand it was that Systrom stated, if I remember correctly, that the study was more powerful than it looks, given its size. I’m not sure why that’s so.
Ron Davis’s severe ME/CFS study is about 20 patients as well I think. These studies are going to gather a ton of data – hopefully they will provide findings that lead to bigger and better studies.
Thank you Cort for understanding my pain. I have been almost 100% bedridden for so long and it gets worse and worse. And after all these years of reading and hoping they are still mostly in the small sise studies. I simply can no more.
May I ask you something? I forget what I read immediatelly when I am capable of reading in the first place.
Is your brain good enough to make a short list of the scientists who are doing big controlled studys and what they are doing?
And ofcourse I am thankfull for the person who donated the money for the study.
It seems to me that an argument can be made for stress being a causative factor coincidental to Systrom’s findings of blood vessel and endothelial constriction, as stress is a known systemic constrictor. Further reasoning might lead that there is a limit or threshold where stress enters the picture as the causitive factor which continues the
described process even after the originating stress is removed, but further constriction progresses when stress returns, causing vacillations in severity… .
I believe stress is one of a number of factors that in combination, tip the victim into a “vicious cycle” condition where the “disease” has its own momentum and it is no longer possible to resolve by addressing any one of the trigger factors, such as stress. This is why the only people who have used self-help strategies with success, have been following multi-disciplinary protocols that address multiple contributors to the vicious cycle, and give the body a chance to break out of it.
@P. Hayward. Sounds right to me.
Further, when ‘uber-stress’ re enters the PWC’s lifestyle the result is PEM.
It’s at this point I suppose Sysrom can record excessive alterations in his
Pulmonary measurements, i.e. greater constrictions.
Hi Cort,
I read “hyperventilation raises CO2 levels during exercise” in your blog. Please note that it is very likely the reverse: hyperventilation vents too much CO2 leading to too few CO2 in the blood. See https://en.wikipedia.org/wiki/Hyperventilation.
“When alveolar ventilation is excessive, more carbon dioxide will be removed from the blood stream than the body can produce. This causes the concentration of carbon dioxide in the blood stream to fall and produces a state known as hypocapnia.”
I wondered about the same! Thanks for the great article, Cort!
I was a national level athlete in my late 20s. I have had CFS in various degrees at least since 2001, when I was hit by a car and broke a few bones; Was out of work for 3 months, then bedridden a year 2 years later. Then in 2014 I retired early at 55, unable to stay awake through a work day. Then the CFS got even worse after a flu shot, leaving me at a 1 on the 0-10 Energy Scale for months.
I now bicycle 2x/wk with a group of retirees for exercise, and have been doing it 2 years.
I appear to ‘hyperventilate’ when bicycling up inclines & I can not breath hard nor fast enough; It scares the others in my group. HR jumps to 90-100% of max, and I still feel like I am starved of oxygen. I am gasping hard the whole way, going only about 4-5 mph up a 6% grade. I do NOT get light-headed, and I do not feel muscle ‘lactate burn’. After 2+ years of bicycling, Flat rides are easy, but my heart and oxygen usuage system can not handle any added load.
My blood tests show high EPO, high ferritin, high red blood cell count, high iron, as though I have been training at 8,000 ft altitude, not 200 ft. It shows my body has adapted to a low oxygen environment. My EKG and Stress Test are normal.
I technically should be great at doing sea-level hills, & not be the slowest in the group.
However, my HRV (heart rate variability) is always low, showing a non-responsive Vagus nerve.
It is an example of how the CFS-infected blood is carrying a healthy amount of oxygen, but it is NOT getting used by the mitochondria and muscles like it should be.
As a bicyclist and wannabe athlete of sorts, I find it very frustrating to get ‘beaten’ by 70+ year olds, some of which have had triple bipasses.
Thanks for reporting this, Cort, though I, also, don’t know what to make of small studies (even with high significance levels, apparently) that require nasty invasive procedures and are evaluating multiple disorders and variables. The great diversity of symptoms with FM, for example, does not inspire me to take strong meds, especially off-label, when I may have a subtype with different symptoms and possible different etiology and pathophysiology. I think the diversity of symptoms also fragments study of these disorders, as well as the patient population’s ability to mobilize and get more research done.
I think you are right about the possibility of “subtypes” of FM that may not respond to identical treatments, but I believe that the vast majority have the same essential dysfunction, in the muscle fascia. Possibly there are multiple different paths to this dysfunction but I believe all of them involve loss of “lubricant” property in the fascia ground substance, and that hydration issues are typical, along with sluggish removal of toxins of any kinds (externally introduced or by-products of infections, and by-products of energy production, which all patients will have in common).
The externally introduced toxins will be different for each person, as can be the location of undiagnosed chronic infections. But even clearing these things up won’t be adequate, as FM has its victims trapped in a vicious cycle of dysfunctions. The heightened central nervous system keeps muscle fibres taught, which perpetuates chronic pain and creates clumps of stuck muscle fibre in the tensed and foreshortened position – which in turn aggravates the central nervous system. Initially one of the triggers was stress, along with the toxins and the hydration issues; but removing the stress won’t reverse the vicious cycle on its own. Furthermore, the sabotaged flows of blood and lymph fluids and even nervous system signals, cause muscles to function prematurely anaerobically and add to the post-exercise toxins lingering (natural clearing processes also being sabotaged).
I am skeptical that any one magic-bullet “medication” will ever “cure” this condition. Cortisone injections have been observed to release stuck muscle tissue, as has “trigger point therapy” and needling and other hands-on therapies, but the condition “always” returns. Unless, I suggest, a multi-disciplinary protocol is being followed that minimises ALL the factors that contribute to relapse.
Low ATP and oxygen is what causes rigor mortis. CFS is low ATP and low oxygen uptake.
I think FM is just mild rigor mortis.
Thankfully zombies are not usually around to complain about the extreme pain.
“Dysautonomia – the primary problem is inadequate venoconstriction; i.e. the autonomic nerves are not constricting the veins enough to propel sufficient amounts of blood (i.e. oxygen) to the heart for exercise or other activities to take place.”
There is an ongoing discussion between too much or too few venoconstriction in ME/CFS. While venoconstriction can let more blood return to the hart (and thus reduce hart preload problems) it does not necessarily mixes well with ME’s low blood volume problem. It’s like squeezing a tube of toothpaste: it works very well when then tube is full but when the tube is too empty getting the last bit out of the tube is an enterprise in itself.
Blood gets more viscous when flowing slower (aided by low blood volumes and volumetric flow in ME patients) so in ME patients too much venoconstriction could be quite problematic.
First, there is our often tight muscles. Tight muscles act like “pressure-preload” on the blood vessels and could be enough to seriously “pre-constrict” hair vessels too “almost closed”.
Second, Naviaux describes Dauer well. Part of it is producing enormous quantities of H2O2 especially in overexerted parts of the body. H2O2 reacts with NO in an equilibrium reaction to form H2O and NO2. When there are ridiculous amounts of H2O2 the reaction shifts to converting the vast majority of NO to NO2. NO is likely the very best vassodilator so almost eradicating it likely further squeezes the hair vessels to near-closed and does so even more at exerted body parts.
Then there is the generally low blood amount and flow often found in ME patients. If blood flow is too low at rest it likely only gets worse when exercising. In a hydraulic system with insufficient flow, flow distribution does depend more on ratios in hydraulic resistances than on having low resistance for the desired part. This could lead to an “odd” form of blood flow regulating when vassodilation potential in exercising muscles is very limited: constrict all the other remaining vessels even more then those too the working muscles. It would fit ME well: constricting the entire blood flow to the rest of the body in order to have a larger portion of the limited bloodflow going to a working muscle would reduce blood flow in the entire rest of the body to a trickle… …resulting in massive blood pooling and severe hart preload problems… …all in a delayed PEM like fashion.
As the main vassodilator NO is likely even less available in the working muscle then in the rest of the body, that would be quite unfavorable to get the ratio better for the working muscle. So this mechanism would not work. However there are options to get the ratio favorable:
Overbreathing or hyperventilation. CO2 is vassodilator number two. Breath out as much CO2 as possible so that the CO2 level in arteries is very low. Then CO2 content in the veins will have a much larger relative ratio. It will still be moderate in the veins connected to “resting” tissue and a lot higher in working out tissue providing relatively less constricted hair vessels in the working muscles. Hyperventilation may therefore be another symptom that has at least a functional part (rather than us being disfunctional/neurotic).
Stretching it even a bit further/(too far?). There is a third common chemical that causes vassodilation: lactic acid. Could the muscles (and brain) going quickly into *a mix of aerobic and* anaerobic stage be a desperate adaption of our bodies to constrict the working tissue less then the resting tissue? If so the body would be *really* desperate.
Anyway, both hyperventilation and shifting body chemistry to go quickly into a mix of aerobic and anaerobic working would result both into a automatic mechanism that diverts blood flow too the parts with highest blood flow demand without having to regulate it (no need to know where that high blood demand is, works even under conditions of poor brain and/or nerve functioning).
It does correlate with the measured strong drop in brain blood flow after exercising. It does also correlate with the observed delayed and prolonged body wide increase in lactic acid that is unique in our disease. Having prolonged body wide deep vassoconstriction increases oxygen shortage to tissue and therefore lactic acid production over a long time.
In this view poor blood flow and odd breathing problems would be deeply intertwined and self sustaining so hard to get out of the viscous circle. It draws in some early aspects of PEM too. It does seem to have potential to be a core problem to me.
Prolonged severe body-wide hypoxia should lead to body-wide reperfusion injury followed by massive inflammation. Massive inflammation thickens blood leading to future blood flow and pooling problems…
Prolonged poor blood flow should also temporarily reduce immune functioning by less white blood cell patrolling giving opportunistic pathogens changes to have multiplied a lot by the time blood flow restores, likely *temporary* necessitating a strong immune reaction risking auto immunity in and nearby blood vessels.
When poor breathing muscle function combines with poor lung blood flow and reduced brain and nerve functioning it could give rise to those very deep breathing problems type “who did just reduced air oxygen levels from 20 to 5%?” that takes weeks, months or worse to recover from.
The combination of all of this would somewhat describe a disease with many different ways in, a PEM mechanism, a mechanism to convert a single or a few initial problems to a whole array of problems, a lot of different individual differences between patients and a very strong mechanism maintaining said disease.
Sorry for the too long post,
dejurgen.
I love your comments!!!!
I posted this comment earlier and Cort hasn’t posted it yet (for some reason my comments get looked at by moderator and we can’t figure out how to let them just post without a go between.)so if it comes up twice…
I have been trying to sort why when I snorkel I have issues with hyperventilating. I discovered (there is a whole thread about my trying to sort this on the POTS website DINET) some snorkel tubes can cause you to rebreathe CO2. After awhile of this, I go into a severe POTS “attack”, with hyperventilating and muscles go to weak. I realized I was trying to expel CO2 with the hyperventilating and attempting for more oxygen, but until I slowed down that and got my breathing under control things didn’t improve.
Along with these events, I would have more issues with blood pooling and worse POTS. Severe dizziness, tachycardia, nausea and all that goes with it. (I have since found out I have APS with a positive Lupus Anticoagulant – basically too thick blood). I also have severe issues with inflammation.
I have found I do better to vasodilate rather than vasoconstrict. Possibly the too thick blood may be a factor here. (There is a fine line how much I do this lest it create more problems with Dysautonomia.) I happen to be a HyperPOTS person with really high NE levels with standing. I feel that even though this is extremely uncomfortable it may be my bodies compensation to aid blood flow. I do feel there are reperfusion issues and it does contribute to more inflammation.
Finding that I’m now positive for CIRS (Chronic Inflammatory Response Syndrome) and that in itself can cause more inflammation,more issues with thick blood, osmolarity issues, MCAS, etc…..it’s all another piece of the puzzle.
Using midodrine was a horrible thing – causes constriction of blood vessels. And Mestinon caused me SEVERE brain, mood, emotional issues. Was one of my worst experiments. And I have tried them all pretty much. I continue to say, our body is very intelligent and some things we may consider a symptom could be a compensation. Make sure you know the function, what your doing and why. Putting on the wrong bandaid could cause more problems. But, on the flip side – some have really been helped by these medicines. But they are a different subset type than me.
Issie
Hi Issie,
Thanks for sharing your snorkel story. It very well may be a valuable “data point” to check ideas against.
For some time now I too gave up on fighting against symptoms. It didn’t brake my decline in health. If a symptom happens to be (also) functional, fighting it costs three times: once money or effort spent; once treatment or medication side effects and once loss of an adaptation mechanism.
Now I try to find out what benefits symptoms or dysfunctional behavior may have first and once I have a good candidate I try and test if I could reach the same result at lower cost. In this example of hyperventilation my reasoning goes as follows:
* Could it be countering the inability to dilate sufficiently the blood vessels in the tissues at work?
* Could day to day efforts to reduce tension in tissues body wide achieve similar results?
* If so, could the end result be a combination of less blood pooling, better hart-preload and better blood flow at rest with better blood flow in both tissue at work and the rest of the body when exercising leading to less need to hyperventilate?
* If those advantages would arise, could it reduce inflammation and oxidative stress over time leading to better general blood flow and form a small positive circle countering the vicious one?
* If those very optimistic hypothesis would work out well (in well controlled circumstances and depending on subgroup) I would prefer it any day over taking Valium to calm my nerves in order to breath slower.
I’ll look into your website and look into LY’s EDS angle sometimes soon but I’ll first try and see if I can work with Philips ideas about exercising. I get the feeling he may be onto something.
p.s.: when my comments needed to be moderated I had misspelled my email address. Maybe yours has an unusual character or format the software does not recognize as valid?
To add to this, there is the issue with osmolarity (salt levels, mine too high) and being in salt water – increasing salt. Too low ADH levels – leading to dehydration and inability to hold onto fluids. (A part of CIRS.) Water compression on entire body. And exercise exertion from swimming. All this contributed to thickened blood and a need to try Dilate. Possibly constricting blood vessels more. Therefore, the hyperventilating was possibly a compensation. I also realized it was better for me not to use my arms and just my legs to swim. This was to get blood flowing upwards to where I needed it. (Larger pumping action.)
I also have too tense muscles. Us EDS people do this to keep ourselves held together and upright. Trying to prevent subluxation. But, I have found a very mild muscle relaxer, at night, to be very beneficial for the pain I experience. I use a Bentyl. It’s normally given to people for IBS. Mayo docs found this an interesting choice and one they had not used before. But that and a Tramadol has been my best POTS meds. To date. It helps with my autonomic nervous system response and the pain of EDS and FMS.
Again, sometimes what may be considered a symptom is a compensation. It may be the better of the two evils.
Issie
Interesting. I think we have constriction when we are at rest and dialation when we are active. The cause is a dysfunctional autonomic reflex. It is the other way around. I believe. But i can be wrong. It is very difficult because there can be a lot of problems. I agree this is the core problem in ME/POTS. For every ME patiënt with hyperventilation.
Hi Gijs,
I get my idea of too much contraction from the time I was in an awkward backfiring CBT/GET program. As the program progressed I got worse and worse.
Remarkably, my resting hart-rate and exercise-to-exortion hart-rate became closer and closer in the process. It ended being 85 to 90 at sleep and 90 to 95 sometimes falling of the treadmill. I couldn’t get my hart-rate to the target value set by the program. That was a clear and repeated observation.
Whilst it’s much harder to estimate how well the hart contracts I had the distinct impression it was equally poor to very poor and painful during night as during exercise. If that guess would be somewhat correct then it would combine with the near constant hart rate to a very poor variation in cardiac output. (With his invasive CPET method, good doctor Systrom likely has valuable data on it). There also may be subgroups here as well.
If my cardiac output would have been near constant, I find it hard to imagine how it correlates with body-wide constriction during rest and body-wide dilation during overexertion. My imagination is limited however.
As exercise should get a significant larger portion of blood flow to the exercising muscle and I suppose the total blood flow remains rate limited, it remains hydraulically speaking optimal to further contract the resting parts and increase blood flow at the exerting muscle. At the exerting muscle I believe NO to drop sharply due to excessive H202 production counteracting the dilating effect of increased CO2 and lactic acid concentration (relative to rest/rest of the body). The net affect could vary between mild constriction (but less than in the rest of the body) to mild dilation.
That would leave sufficient “room” for the relatively strong increased local blood flow in the muscle that should be accompanied by the mechanical contraction of the active muscles. Contracting and extending muscles has a strong effect on local blood flow due to repetitively “squeezing the blood tubes”. In the legs it is aided by one-way valves. With overall dilating blood vessels and muscle action stimulating blood flow I would very much expect stronger cardiac output as seen in healthy exercising people.
Also, I struggle to see how exercising, which should lead to more H202 production if I understand dr. Naviaux correct would coexist with too much dilation.
Anyhow, since I managed to have my muscles less tense (which I believe lead to less pre-constricted blood vessels) I have a much stronger variation in hart-rate and far less pain in the hart region which I believe means better hart contraction. In part it overlaps with better baseline health. I must admit, much of it remains guesswork unfortunately…
I’m happy to see increased attention and a variety of new ideas centering around the blood vessels so I’ll keep reading different opinions like yours with interest ;-).
I am hugely encouraged by Dejurgen’s hypotheses – I think this is exactly where researchers should be looking. I haven’t thought it through as deeply as Dejurgens has, but my own experience with successful self-help recently after years of stumbling and failed experimentation, suggests that the causes and solutions are in the areas Dejurgens is discussing.
I still tend to think there is something significant that is different between FM and CFS, but at the very least there is a majority of those diagnosed with FM and a significant subset of those diagnosed with CFS, that suffer from the fascia / muscle tissue / micro-vessel dysfunction. Maybe this condition needs its own new name, so that people who have “FM” and CFS for other reasons, can be separated out and studied to discover what those other reasons are.
Re “pre-loading” – I have experimented with the Valsalva Maneuver and I think it provides a brief surge of added capability in demanding situations such as squatting down. The first time I tried it, I nearly passed out; but I quickly got used to it. In fact I now deliberately do it during some Yoga routines when I am already in a demanding position, and I think it may just force the circulation through some of the tightened locations and add to the overall improvement.
I am now also getting new breakthroughs in range of movement as a result of doing Feldenkrais routines; one of the major effects of Feldenkrais is from re-training the central nervous system to “release” opposing muscles during specific movements. I think this is a most helpful complement to all the other de-toxing and “care of the fascia” and mobility routines that I am doing.
What can one say except “Wow”. Very impressive DeJurgen 🙂
Hi Cort,
Thank you for providing your great blogs that acts as a starting point for fruitful discussions and cooperation.
I would struggle far more in both improving my health and talking sense without you collecting, selecting and structuring your information very clear. You do a lot of valuable and hard work. Thanks a lot!
Please remember as said: my posted ideas are half-baken. When I think them over and over before I post them you made many new blogs so that discussion moved to the new topics. Then I mis the many useful comments, points of view and arguments making progress a lot harder.
Still my vision remains: collaboratively collect enough experience to up the pacing protocol a notch or two. I believe there are already enough pieces of the puzzle on the table to do that. Together we can make it happen ;-).
I am curious as to how many of the people with POTS are testing their Heart Rate Variability (HRV) at home (thus Vagus nerve health), and are following Dr. Martin Lerner’s ‘CFS Protocol’ to boost ATP production. Low ATP, low CoQ10, & low trace minerals = low heart ejection output, just like a weak battery in a car. EKG is usually normal.
After having CFS since 2001, I have been doing The Protocol of 5 things for 2 years now, plus taking selenium (200 mcg + what is in multi vit), iodide (Iodoral, one tablet/day) and electrolytes for heart health as per Dr. Joel Wallach and Dr. David Brownstein’s recommendations.
I also eat low carb (<100gm/day), 20% protein, the rest in healthy fats. At 1300 cal/day, my 170 lb weight is stable.
Sleep (now 5.5 hrs/nt from 3.5), resting heart rate (now 60 instead of 80), exercise recovery time (now 2 days instead of 3-4), and muscle aches have all slowly improved. Recently can read books again, instead of just magazines & websites with just 1-2 page articles or play Gummy Drop on my phone all day; It means my brain is waking up.
Up to a 4 on 0-10 CFS Energy Scale, from a 1.
I hope others are trying the Lerner Protocol, which is also used by Dr.Myhill, Dr. Montoya, and a lot of other CFS specialists.
You lost me completely at: “Breath out as much CO2 as possible so that the CO2 level in arteries is very low.” How is that possible? How does any amount of exhaling affect the CO2 in the arteries?
Sorry – this was a reply to deJurgen’s August 18 post.
This article may hold the answer to a prayer I wrote out back on 8/23/98 and have prayed regularly since. “A healing of damaged brain tissue and malfunctioning mitochondria. Oxygen would be effectively utilized at the mitochondria level, and that blood would flow efficiently to the cellular level, carrying oxygen effectively and picking up the lactic acid and CO2 waste and carrying it away to be properly disposed of in the body thus allowing me to exercise without symptoms.” (As only an exercise specialist/cardiac rehab RN with CFS could articulate).”
I will be discussing this with my MD.
It also confirms that my number one medicine over the past 25 years of living with CFS/ME/POTS is the best medicine ever–Prayer. I chronicle my journey of living a fulfilled life even with a the severe limitation of CFS/ME/POTS in my latest book: Pray 10K, which is available as a free Kindle download on 8/18/17 and 8/19/17 at https://www.amazon.com/dp/B0744YXBVK.
Thanks for your work on this issue and for being an answer to prayer at least for some and I hope for me too.
If prayer worked, you wouldn’t have this disease to begin with. Prayer has been studied, see e.g. http://www.nytimes.com/2006/03/31/health/31pray.html?mcubz=3
Prayer AND meditation CAN work if you can get feedback from your Greater Self, Guardian Angels, Jesus, Yoda, Tony Robbins, or whoever that little voice is in your head that tells you what you need to do to heal. If you then follow your gut instinct, you are then usually right.
With CFS, it usually involves rebuilding the immune system, detoxing, and replacing missing trace nutrients. The needs differ amongst each one of us.
Most people do not know how to pray and meditate effectively, so prayer just becomes “Wishful Thinking” instead of a tool.
I doubt these studies of prayer do not separate out the two subgroups.
Why would you demean this person who has managed to get thru her hard times with prayer? I’m an old woman now, have had a lot of spiritual changes & have come to the conclusion that what works for someone is the thing they should use. As long as one isn’t praying for harm to someone else, what could possibly be bad about it? At least it’s good thinking that’s going into our poorly abused universe. I’m extremely grateful to the person who supplied the money for this research. We should all be the same. (This was for someone else’s comment about what should be done, not you.) I wish all of you well as I’m old enough to know what old age itself also does to our bodies. Thanks for reading!
God is all loving but not all powerful. Given that, prayer can be hit and miss.
Metaphysical things are impossible to study. According to scientists homeopathy can’t and doesn’t work yet I know for a fact that I have had some really good outcomes from it.
Yes, it’s called the placebo effect. Very powerful.
“Blind” studies have proven homeopathy doesn’t work. 100% BS. But for those who believe in such medications, if it makes you feel better, there is no reason to stop….
I suppose bigger overexertion correlates with bigger overbreathing, so I turned things upside down this year.
When I feel an increased need for breathing I start to pace down. It seems to be one of the earliest indicators for onset of overexertion/anaerobic phase. I like it far more then guessing how much I can do a day and awaiting if it was good enough to avoid PEM. It also gives better indication of what type of activity and how much of it is too expensive.
By better knowing what type of activities are more expensive I can pace less vigorously down by still get better pacing results over time. It works fine with physical exercise but is a poor indicator for overexerting my brain.
“…By better knowing what type of activities are more expensive I can pace less vigorously down by still get better pacing results over time…”
YES! My experience exactly! For cardio exercise, I believe that monitoring the heart rate and keeping at around “fat burning” intensity – 65% of maximum – is right. But then there are lots of other situations like “exertion of strength” and having to be in different postures; and I am still experimenting and have no general rule for myself yet. I got some VERY bad advice from a public health system physiotherapist 5 years ago and spent several months doing explicit “muscle strengthening” (on the surmise that stronger muscles could be operating more within their capability all day if they were stronger). This was a disaster for me – I kept at it too long but concluded that it was increasing my chronic pain, causing de facto injuries that got continually more and more painful at certain spots, foreshortening muscles and decreasing range of movement. When I abandoned it after 6 months, my knees anterior and my quad muscles were so aflame with pain on exerting them, that I almost couldn’t stand up out of a chair any more (and the chronic tension and hardness was like rocks under the skin); and my rotator cuffs were so sore I could barely even wave my arms around with no load at all. 4 years later I am mostly considerably better than I was at any time even prior to this debacle, except the rotator cuffs, which have still not even recovered back to “mere ordinary FM pain levels”.
But it was this debacle that helped me rethink everything and try a different approach that has now actually proved to work.
I guess this, in a small way, explains why I can still have decent O2 levels on my home O2 finger monitor and still have debilitating weakness. I can have a resting O2 of 93-95 and just by icreasing deep breaths bump it to 96-99. But if you’ve got O2 in the blood in the veins but it’s not getting into the muscles or being efficiently used, guess that’s a ‘duh’. And drat…every time there is some glimmer of hope, like the mention of Mestinon there is some caveat. I also
developed Addison’s (adrenal failure) and take full replacement corticosteroids, one of the things apparently it interferes with.
I hope I’m not duplicating a post. Don’t have time right now to read them all. Was wondering if this 02 issue explains why for me, FM /ME/ CFS shares several symptoms with mountain climbing altitude sickness, where there is less oxygen available for the blood to absorb. It seems there are some actual medications that could be tried. I hope to pursue these.
Thank you so much for writing this Cort. I got a script last week and within hours felt its effect . I took too much at first but have now settled on 15 mg twice a day . What a difference it has made ! At higher dose ( 45mg) I had sleep problems – insomnia . But at 30 I don’t . I have been ill for well over 30 years . I am on a tonne of the usual fibro cfs meds also, but mestinon has taken away the fatigue and PEM. I am worried that it may not last , as that has been a pattern over the years, but am so annoyed that my CFs expert here in NZ never recommended it. She said she’s been using it for the last at least 10 years and it helps about a quarter of her patients. She gave me no guidance on how to take it – just 60 mg once a day. Boy I’m glad I didn’t do that !! I have been diagnosed as having Dysautinomia by a cardiologist . Beta blockers helped but because of the cold I couldn’t take in winter ( propanalol 5 mg twice a day ). My heart rate used to sit at about 100. I went to a funeral over the weekend which would normally flatten me for days . No flattening . It feels very weird . I wake up and actually feel stored from sleep .
I can’t thank you enough for writing this .
Hi, I saw your article on successful treatment of CFS w/ Mestinon. I recently started it and have felt well for 18 days in a row – a first since my CFS diagnosis 25 years ago. Specifically, the brain fog has lifted, my exercise tolerance has improved, I recovered from a URI in a week instead of it lasting a month, I have experienced about an 85% decrease in nightly hand neuropathy along with shoulder and neck pain and arthralgias, and a decreased inflammation throughout my body. I have only experienced one episode of heart palpitations and lightheadedness. I feels like Mestinon addresses CSF at the cellular level in a way that has been missing to date. I look forward to hearing more about your work with Mestinon & CFS.
Great to hear AT! Keep reporting back please. 🙂
At-what dose mestinon are you on-thx
– A warning, to consider –
Great that this works for many patients.
However, I would like to add that I had bad experiences with Mestinon myself.
I developed severe muscle weakness, to the point that I could not walk without a walker because my feet hurt so much. It felt like I was walking solely on the bones of my feet. My legs also became very weak. I am already housebound/bedbound and this setback was not what I needed. Furthermore, I became so exhausted I could barely talk, felt out of breath and I developed panic attacks from just being upwards.
Most symptoms diminished within 2 days of stopping the medication. Now two months later, I’m still recovering from the energy setback.
Not saying you shouldn’t consider using Mestinon, just that you know that it’s never without risks. Hope it works better for you than it did for me!
Thanks Al, for the cautionary tale. Nothing seems to work for everyone and most everything seems to really whack someone.
I hope that you get back to baseline soon. 🙂
I’m resorting back to this article and posts to ‘re-read’ as yesterday I got a prescription of ‘Mestinon’. Having tried so many approaches and treatments, I’m open to trying just about anything. 6 years ago when I first became ill, the ‘only’ blood test that showed up with a positive result was the ‘Acetylcholine receptor antibodies’ test (usually to determine Myasthenia Gravis). I didn’t exhibit any features of MG so nothing further was done with this result. However, armed with Cort’s article and other info I’d gained I headed to my local GP (in UK) reminding him of my positive blood tests (4 of them) 6 years ago for the acetylcholine antibodies. The result being he has reluctantly given me a prescription for Mestinon. I took the first tablet yesterday (I’m starting out slow, 15mg twice a day) . Will report back on how things go.
On another line of thought prompted by some of the posts above, does anyone find that upon waking their body feels so depleted and exhausted to the point it’s as though they have literally been undertaking some form of exercise throughout the night. So many times I wake in this state and having felt as though I were dreaming all night and often exerting myself in the dream in some way. I’ve often wondered could it possibly be that my body is reacting as though I’m actually awake, in that it’s producing the lactic acid and somehow is treating the reaction of the exertion and exercise in my dreams in the same way it would if I were awake, thus causing the crushing exhaustion on waking ? I know this sounds peculiar but I just had to share the thought and wondered if others experience this ?
Hi Karin,
I used to wake up feeling as tired as I was when I went to bed or worse. I’d lay there for quite a while waiting for the feeling to lift a little – sometimes it did. It has since improved greatly and I like getting out of bed most days now and just wait until a reasonable hour comes along (ie: 0500 many days).
I wonder whether some of us experience “triggers” from dreams.
My own area of interest comes from a trauma perspective showing that life experiences (from very very subtle that I never thought would qualify to overt) creates patterns in our nervous systems that keep us in altered states of regulation. From this perspective, experiences that remind our brains (usually also at very subtle levels and usually subconsciously) can retrigger or further promote the pattern of altered regulation. This isn’t psychological – it’s physiological. And I wonder how much of these triggers keep us in states of relative “freeze.” Working with nervous system regulation (such as using trauma therapy) has helped me a lot. My sleep isn’t fantastic yet but is much better, as is my energy.
First, excellent article Cort. I am not a patient of Dr. Systrom’s and have not had iCPET Test. However, I have had the paraneoplastic and autoimmune dysautonomia panels from Mayo and test positive for several autoantibodies (N-type Calcium Channel, GAD65) plus the anti-muscarinic/cholinergic and a few others.
I think some people confuse the anti-nicotinic autoantibodies of myasthenia gravis with the anti-muscarinic autoantibodies (which can be tested by Cell Trend in Germany).
After 2-3 yrs of having a “CFS” diagnosis (plus POTS, Hashimoto’s and then MCAS), I finally got the proper testing and treatment which for me was high dose IVIG & Rituximab (which I see from your article are also on Dr. Systrom’s list as second tier treatments).
In cases of proven autoimmunity, I think they should move up to first tier treatments and Mestinon does not work for all patients (and my one attempt w/it caused me respiratory depression).
IVIG & Rituximab have put me into remission and my diagnoses ultimately turned out to be Autoimmune POTS, LEMS, Autoimmune Autonomic Neuropathy (plus the Hashi’s & MCAS). If turned out that I did not have CFS after all and (in my own case) it was a waste basket diagnosis that did not lead to the right treatments.
I am sharing this everywhere in the hope it helps others. I am in remission now and can walk, drive, have normal muscle and breathing strength again, no longer have allergic reactions, and no longer use wheelchair. I wholeheartedly believe that IVIG & Rituximab are the right treatments for autoimmune cases like mine.