

Caroline returns with a not uncommon story of a complicated chronic fatigue syndrome (ME/CFS) diagnosis. From fibromyalgia to Ehlers-Danlos syndromes to postural orthostatic tachycardia syndrome (POTS) to mast cell activation syndrome (MAST) to intracranial hypertension to mold sensitivity (and more), the number of alternate or comorbid diagnoses associated with ME/CFS is growing. Now Caroline brings to our attention a new one – cerebral spinal fluid leaks.
I saw Dr. Ian Carroll, an expert in cerebral spinal fluid (CSF) leaks from Stanford University, for the first time recently. He spent 1.5 hours with me and was very thorough, asking me a series of detailed questions he uses to assess patients for possible CSF leaks (see below). I have ME/CFS and hypermobile Ehler-Danlos Syndrome (hEDS) and was referred to him by my autonomic specialist at Stanford because my orthostatic intolerance (OI) picture is a bit muddy and because hEDS, a connective tissue disease, is a risk factor and can cause aneurysms and spontaneous leaks from the dural sac (the tough outermost membrane of the spinal cord and brain).
Spinal leaks can be caused by an abrupt event, such as whiplash or a spinal tap, or can be spontaneous, which is often the case for people with hEDS. Although abrupt leaks are often spotted by doctors because they cause characteristic orthostatic headaches (headaches that arise or worsen upon standing), spontaneous leaks are often much harder to detect and require a specialist like Dr. Carroll to catch and diagnose because the symptoms, such as fatigue, nausea, and postural orthostatic tachycardia syndrome (POTS), are non-specific and thus overlap with other conditions.
Carroll told me stories of people who spent years suffering with an ME/CFS or POTS diagnosis only to go on to recover with a simple blood patch, a surgical procedure that uses your own blood to close holes in the dura. People with this condition report getting a new lease on life after a successful patch. For this reason, if a leak is suspected, it is worth looking into because, unlike most everything else in ME/CFS, there is a fairly simple and effective fix for it.
Several clues tipped off both my autonomic specialist and Dr. Carroll to the possibility that a cerebral spinal fluid leak could be causing my symptoms:
- Heart Rate Not Greatly Increased During Standing but very symptomatic nonetheless – I have been diagnosed with adrenergic POTS, but don’t experience the big rise in heart rate (HR) like many with ME/CFS do. Yet I experience symptoms as if my HR is much higher – mainly dizziness, nausea, extreme fatigue, sweating and other symptoms that elicit an overwhelming need to sit or lie down. For years I had no shame and would plop down to the ground wherever I was – in line at Target, etc. I finally got a rollator for these instances and now use an electric wheelchair, both of which have helped immensely in managing my orthostatic intolerance. All of this is suggestive of a leak…or POTS.
- Standing worsens migraines – I don’t get orthostatic headaches, but standing does worsen my migraines when I have them, and I have pulsatile tinnitus, another sign of a leak. I had a spinal tap for a C-section and fell ill shortly after.
- Spinal tap – I had a spinal tap for a C-section and fell ill shortly after, but this could be explained by ME/CFS as well (pregnancy is a trigger for many because it lowers immune status)..
- Mother died of brain aneurysm – Also, my mother, who likely had hEDS, died of a subarachnoid brain aneurysm at the age of 53. While this is not the same as a CSF leak, it is indicative of weak connective tissue. I also have bone lesions on my spine, which may be impacting the dura. Amazingly, I’ve never had an MRI done.
Dr. Carroll started by asking me about head pain while I was sitting. I always have head pressure but quite honestly it is the least of my concerns, that is, until I do too much and post-exertional malaise (PEM) kicks in and cranial pressure mounts. PEM is the cardinal symptom that sets ME/CFS apart from all other illnesses and involves a worsening of neurological and immunological symptoms following exertion.
Dr. Carroll had me lie backwards on the examination table leaving my head slightly lower than my heart. That position brought on stabbing pains in the crown of my head and a sensation of mounting pressure. Next, he had me spin around and put my head in the usual position on the table, slightly elevated, and the pressure and pain went away. It returned when I sat up, but not nearly as bad as when my head was slightly lower than my body.
One thing I said seemed to catch Dr. Carroll’s attention: I told him that I’ve always been lucky because I have been able to use my brain for the most part. I spend countless hours in bed and enjoy doing research and writing. Some days this will give me PEM, but most days I can handle it. ((I am moderate to severe and am obviously very different from people on the more severe end of the ME/CFS spectrum who can get PEM from reading, writing, and/or even watching Netflix).
Dr. Carrol said the fact that I can function cognitively when in certain positions, but not others, suggests problems with cranial pressure are present. He seized on this to suggest that perhaps it is not PEM I am experiencing, but a leak. Both PEM and CSF leaks overlap substantially.
Through the looking glass
Many more conditions probably overlap with ME/CFS than most doctors are aware of. Ehlers Danlos Syndrome, intracranial hypertension and spinal fluid leaks are three possibilities that are probably missed by most doctors.
I was first diagnosed with Lyme, another similar illness, but this was a likely misdiagnosis. I was relieved to finally find a medical home with ME/CFS after being sick for 11 years (as much as one can be relieved about having ME/CFS, but having the right diagnosis, whatever its prognosis, is essential for getting the right treatments). ME/CFS is a much better fit for my symptom picture than Lyme because I get PEM quite readily.
Last April, another Stanford neurologist explained to me that he is seeing an increasing number of patients with a suite of symptoms similar to mine – migraines, dysautonomia, GI problems (nausea, lack of appetite, vomiting), and fatigue. These patients, he reported, typically have hEDS.
This was the first time in my 11-year medical career as a patient that a physician brought up hEDS with me. The neurologist’s quick assessment suggested that I might have the condition. During more formal tests by my autonomic specialist last month, he gave me a 9 out of 9 Beighton Score, meaning I am extremely hypermobile. (The guidelines for diagnosing hEDS have recently been revised and underscore some of the other serious complications that can arise from this condition.)
I’ve always noticed that I do best when I’m in bed – not flat, but with one or two pillows to prop me up. Dr. Carroll said that even at this fine scale orthostatic issues can exist in patients with cerebral spinal fluid leaks? Sitting up is far too fatiguing, unless I am reclined substantially and my head and back are supported (which is true of many with ME/CFS and POTS). Standing up is out of the question.
It Is What It Is
When I received my hEDS diagnosis last month some people encouraged me to consider how hEDS, apart from ME/CFS, might be contributing to my illness. Some have even gone as far as to suggest that I and similar patients don’t actually have ME/CFS and that all of my symptoms can be explained away by hEDS, and more recently, spinal leaks. At first I bristled because I have always thought of myself as having fairly straightforward ME/CFS – known onset and trigger (mono), PEM (or so I thought), and the many symptoms so many of us deal with on a daily basis.
In thinking this through more, I’m still convinced that I experience PEM. When I overexert, I experience a burning sensation in my limbs, brain and spine and get horrible brain fog. I may get a slight fever and sore throat – suggesting immune activation has occurred – which is not part of hEDS or spinal leaks to my knowledge. I can also get PEM from emotional or cognitive exertion, which have nothing to do with orthostatic position. Other symptoms during PEM are less clear – worsening of POTS, extreme fatigue, and brain fog. These symptoms could be explained by a spinal leak as well.
I have had to open my mind and consider that many of my symptoms could be explained by hEDS and leaks, while also being open to the idea that all three conditions can occur simultaneously. In this case, the challenge becomes learning how to parse symptoms and determine which condition is giving rise to particular problems. At the end of the day I’m less concerned about labels, and more interested in the truth. On this journey I have been amazed at how dearly people want to hold on to their diagnoses and shoehorn others into theirs. I get that to some extent because each illness has its own culture. My motto these days seems to be, “It is what it is.”
So, what is it? ME/CFS, hEDS, CSF leaks, pseudotumor cerebri? All of the above?
Dr. Carroll’s take is that I’m complex. He thinks I have spontaneous leaks and pseudotumor cerebri. Pseudotumor cerebri refers to a condition of excess CSF in the brain, causing increased cranial pressure. (It is called a pseudotumor because many people present as if they have a brain tumor – yet there is no actual tumor involved). The worsening of my head pain when my head is slightly lower leads Dr. Carroll to think I have a pseudotumor. The orthostatic symptoms make him suspect I have cerebral spinal fluid leaks.
I learned from him that two drugs I’ve been on for the past year to treat a chronic mycoplasma infection – doxycycline and minocycline – can increase cerebral spinal fluid (CSF) and cause pseudotumor cerebri. This creates a conundrum because treatment for the leaks could cause the pseudotumor to worsen by increasing cranial pressure. For now, Dr. Carroll wants me off the minocycline and we will do an MRI to see if leaks are a possibility.
Evaluating leaks, unfortunately, is as much an art as it is a science. A trained eye is required to catch the subtler spontaneous leaks Dr. Carroll believes I am experiencing. Even then, a CT myelogram which involves injecting a dye into the spinal canal fluid might be required. (Because this test itself can cause a leak, doctors are wary about doing it unless they have a very good reason for suspecting a troublesome leak). This type of imaging allows for a closer look at the spinal canal, cord, and nerve roots.
My work up will consist of starting with an MRI and being referred to a headache specialist. Dr. Carroll works with an assessment team, and the first question they will ask him before agreeing to more invasive explorations like a CT myelogram will be “What has she tried for managing her headaches?”’. Dr. Carroll rattled off at least five headache drugs I had never heard of, which surprised him given I’ve been such a head-achy person my whole life, and developed migraines in 2013.
He also wants me to do a 48-hr bed challenge where I lie completely flat on my back (no pillow) for a weekend, getting up only to use the toilet with the aid of my electric wheelchair. If my nausea, head pressure, and fatigue abate, he says this is some compelling evidence for a leak. Personally, I appreciate that he is not rushing in with a myelogram.
A criticism about ME/CFS I sometimes hear from the hEDS community is that of course you are going to feel worse over time if you stay in bed (exercise is one of the most important treatments for people with hEDS). When you do get up, you will feel bad due to deconditioning, or so the argument goes.
I get why my hEDS friends think this, but you don’t have ME/CFS it could be hard to understand the neurological symptoms that extend well beyond orthostatic symptoms. Another version is that all of this could be explained by a CSF leak, and in this case of course you feel better while in bed than when standing up. Again, this is different from PEM in my experience.
Still, I need to keep an open mind. If I have leaks and they can be fixed, I would love to know which of my symptoms would peel way and which would remain. I suspect I would be able to stand for longer periods, but I would still end up back in bed with PEM. Until I know more, I’m going to remain open to all diagnoses, with ME/CFS remaining the top contender for now. Stay tuned.
- Take the Beighton test to see if you might have EDS.
- Losing a Beloved Career to a Chronic Illness: Caroline’s ME/CFS Story – read Caroline’s blog on her wrenching transition from being a conservation biologist to disabled.
____________________________________
Here is a look at the questionnaire (yes/no) Dr. Carroll and his team use to assess patients. It is easy to see why there is so much overlap with ME/CFS!
Headache quality:
- Headache worsened within 30 minutes by upright posture?
- Headache improved within 30 minutes of becoming recumbent?
- Headache largely absent upon awakening in the morning?
- Headache worse as the day progresses with prolonged upright activity?
- Headache worsened by dehydration?
- Headache worsened by exertion?
- Occipital area prominent in headache location?
- Head or neck pain worse on bending over?
- Pain worsened by sneezing, coughing, bowel movement or Valsalva?
- Adventitious sound in the head especially the sound of fluid rushing in the back of the head upon going from lying to sitting or sitting to standing?
- Neck pain or stiffness?
Symptoms related to brainstem compromise or cranial nerves:
- Visual blurring
- Double vision
- Facial numbness or pain
- Sense of imbalance
- Hearing changes (phonophobia, muffled hearing, tinnitus)
- Tinnitus
- Sense of ear fullness– like ears need to be popped
- Photophobia
- Altered taste
- Unusual or non-present smells
- Nausea with or without emesis
Spinal manifestations:
- Interscapular pain
- Radiculopathy
Subdural fluid collections:
- Subdural hygroma
- Subdural hematomas
Central dural sinus thrombosis
Central nervous system:
- Seizures
- Cognitive dysfunction
- Tremor
Endocrine disorders (due to pituitary stalk traction):
- Hx of elevated prolactin
- Hx of galactorrhea
- Hx of any endocrine disorder
- Hx of hypothyroid
- Hx of any pituitary anomalies
- Amenorrhea
Inciting events:
- Headache started with a defined trauma
- Whiplash accident
- Chiropractic care
- Spinal surgery or trauma
- Known osteophyte impinging on spinal dura
- Neck trauma
- Intentional or unintentional dural puncture as in lumbar tap or spinal anesthesia
- Skull trauma (bilateral black eyes, intranasal surgery)
- Transphenoidal surgery
Additional symptoms:
- Well identified time at which head symptoms began or became markedly worse
- Orthostatic lightheadedness
- Orthostatic tachycardia
- Orthostatic syncope
- Fatigue
In addition to Stanford, there are a few other doctors in the US who have this level of specialty, including Cedars-Sinai and Duke.
Check out Melissa’s ME/CFS spinal leak recovery story.








Dr. Jose Montoya recently took interest in the cerebral spinal column fluid leaks and spoke of it at the London conference.
And Caroline is a Montoya patient.
That is great news, Erik! I didn’t know Montoya was thinking about leaks. Seems like an important thing to consider when doing a differential diagnosis.
I suspect I have a leak. Also did full blood work about 4 months ago showed I have high cholesterol. Well I went to the ER last night because the left side of my face went numb and was tingling. Which I told them about 8 months ago I was having neck pains on my left side and pressure in my head. Well the ER did some blood work on me and are now saying my thyroid is low which 4 months ago was not. I have a MRI from 2007 that said paracentral disc protrusions are present at C4-5 C5-6 and C6-7 the largest of these is at C6-7 in the left paracentral region where there is probable involvement of the existing left C7 nerve root .suggest clinic correlation probable small postercocentral C7-T1 disc protrusion. So I looked that up yesterday which makes me suspect I have a leak. I had this MRI done in 2007 because of issues I was having which they diagnosed me with fibromyalgia. My regular dr that I just started seeing said I have a sinus issue because when she looked in my left ear she saw fluid. I told all this to the Dr in the ER last night and he refused to listen to me and also said I have sinus issues but could not give me a steroid shot for it because of my low thyroid.
My Daughter has P.O.T.S n EDS. We suspect a CFS Leak as 16 years she’s had a constant headache that NEVER goes away. Chronic n constant. Not even Pain meds can give her but a little relief. Heart rate standing is 130, Dimming but DOESNT pass out but feels as though she will. Her Grandma, Aunt n 2 Cousins all have it but Ashley’s is the worse. She broke her C2 n Transverse Formen 2013. Everything is unbearable, Severely exhausted n lost all appetite lost 70# n it malnutrition’s. Heart Drs n Neurologist said she’s gotta live with it. Can’t take her Beya blocker anymore her pulse goes too low on it. In dire need of help. She has Medicare n Full Medicade. Can he help her please???
https://med.stanford.edu/profiles/ian-carroll
This link has contact info for Dr. Carroll at Stanford.
I’m so sorry to hear of your daughter’s suffering. I hope she gets the help she needs as soon as possible.
Caroline, your blog and this article are among the most helpful I have read. Thank you.
In going to Stamford , most ME/CFS patients would have started with Dr. Montoya. I know you figured out you had neurological symptoms, but how and who did you connect with at Stamford to arrive on the path you are on. It would be very helpful for me to know where to begin the route.
Sincerely,
Patty Duetting
Hi Patty – I started in the Chronic Fatigue clinic at Stanford and was referred to neurology because I was complaining of neuropathic pain. I had no idea that the real value in that referral was much greater. They have helped me with migraines, sleep issues, dysautonomia, and now these investigations with spinal leaks. It was the EDS connection that got them to take notice of me, not so much the ME/CFS. But they understand that both ME/CFS and EDS can give rise to similar symptom sets and that people with ME/CFS should not exercise, which drives EDS docs crazy because movement is the best treatment for this condition. Not so with ME/CFS (!). I think they would be good for non EDS types as well.
Hi Caroline, thank you so much for your blog. I feel as if the Universe made me read ALL of the info in the ProHealth article for a reason. I have been suffering severally since a whiplash accident (bad one) since 2009. It all started with tinnitus within 4 days and my symptoms became progressively worse! I’ve been diagnosed with POTS, primary ? Chrinic Lyme Disease, EDS, Spinal Cord Injury. Chiari, Thoracic Outlet Syndrome I even had my first cervical ribs, bilaterally along with my scalene muscles removed, neck surgery at two levels, migraines the list goes on and on! I really need a Dr that understands all of this! May I ask, did you have to have a referral to get your foot in the door to to see someone for your CFS? I’m not worried, my primary is awesome but I just want to do it right… my trust in mainstream is completely diminished at this point! Thank you for your time!! ?
Have you been properly tested for Borrelia and the other Co-infections?
Your symptoms sound very much like those of us with tick infectious diseases.
Can cause these leaks from drilling through tissue, demyelination of never, crossing blood brain barrier.
You mentioned being treated for infection – there’s more to that piece of the puzzle.
Dr. Novak in San Diego is very very good at treating current and post lyme and tick infections.
All you described matched up very much.
I wish you more Health and Healing
Just thought I would jump in. I don’t know what Dr. Novak does but Caroline in other blogs described being treated antibiotics for Lyme disease for several years. Unfortunately it didn’t work.
I have EDS and I suspect I have a leak, I have all of these symptoms and have been taken by ambulance to my community hospital twice this week by ambulance bc my episodes of syncope were so bad. I was afraid it was a stroke bc I also have a carotid dissection. They can’t find anything but they also do not know what to look for with EDS. I asked them to look for CCI, chiari and a leak but they are not at all familiar with these conditions. I am so miserable and I know something is very wrong. I don’t know what to do when there are no specialists in my area and no one takes my state insurance. I am completely disabled by this condition.
The CSF leak forums on facebook are very informative and you can ask the members for advice on finding a specialist. Just search CSF Leaks on facebook. There are many people who have helpful knowledge, advice and contacts after going through similar suffering. Also see the above link for contacting Dr. Carroll. I hope you find the help you need as soon as possible.
Thank you for putting your expertise and heart into this for all of us. I know it comes with PEM, so triple thanks.
This has hit home for me as I am currently recovering from a patch! I am quickly approaching my 3 year anniversary of overnight viral onset of ME/CFS. I started looking into the idea of a CSF leak just 2 months ago given some past history with spinal HA’s from epidurals related to prior knee surgeries and lumbar punctures and realized that many of the symptoms cross over with ME/CFS as mentioned above.
Unfortunately, I called Dr. Ian Carrols practice and was told it is at capacity and is no longer taking new patients (sound familiar?) I then sent my imaging to Dr. Schievink, a neuro surgeon at Cedars-Sinai in LA. 6 weeks later he sent me an email suggesting I have an epidural blood patch but thought my symptoms were not likely due to a long standing leak.
10 days ago I had a local anesthesiologist perform the EBP, ordered by my neurologist, and am following the post EBP protocol recommended by the neuro radiologist at Cedars-Sinai who performs their patches (it does differ grately from the standard EBP where they have you lie flat for 1 hour and then let you return to your life).
So far I have had relief of my deep inner ear pain as well as the suboccipital HA that would progress as the day went on which is wonderful. Unfortunately it has not helped my eye pain, light/sound sensitivities, POTS, PEM or sleep to mention some of my ME/CFS symptoms.
Given my response I will pursue a CT myelogram to try and identify the location of the leak, which can be very difficult, and will likely follow up with another patch or seek out specially care in LA or at Duke (if I can tolerate the travel which is a huge question mark as I am currently 85% home bound). I believe that I am yet another complicated case with both a leak and ME/CSF (I do not have EDS)- no one hit wonder of a cure, but any relief is grately appreciated!! It is worth looking into if you fit the criteria…
If anyone is interested here is the link to the 1st annual CSF leak symposium which was held at Cedars-Sinai this last October with video of all the speaker presentations:
http://spinalcsfleak.org/symposium/symposium-2017/
Thanks for relaying your experience and providing the link to the 1st annual CSF Symposium (who knew?) and good luck!
Fascinating story! Thank you for sharing your experience. It sounds like in your case you have both ME/CFS and leaks – no fun. It is interesting to learn about which symptoms were peeled away after you got your blood patch. Sounds like it brought you some relief, but not a full recovery. That makes sense if you have ME/CFS. I’ve heard that Cedars-Sinai is also a center of excellence for slow leaks. Glad you found your way there. I was already in Stanford neurology and that is the only reason why Carroll agreed to see me.
So awesome to see there is a CSF leak symposium on the books!
Nicole, thank you for the information in your post. I have been diagnosed with EB, ME/CFIDS, Fibro, POTS, and have been hospitalized several times with combinations of symptoms. Crohn’s Disease, migraine headaches,brain fog, severe, body pain, nausea, severe deep ear aches, bleeding ulcers…..how do I present my concerns as a “total” challenge, and not “just” the presenting problem? How does one become eligible for the type of “testing” “trials” as mentioned above. I am willing to travel to such a facility if I knew how. I have been ill since1994 and went on disability retirement 1996. Thank you for your response.
How did you get on disability.? I am 62 and work at company in my home. But due to brain fog, fatigue, depression and pain from EDS, I can’t function. How hard would it be to get help?
Thank you very much for this article! If you don’t mind I’m going to cross post it on the EDS section of Inspire.
I’m a hEDSer and have many of the same symptoms as you! I also have excessive fatigue and suffer from PEM–as well as autonomic dysfunction (probably hyper-POTS like you) and a lumbar cyst blocking my spinal cord. As you know, Chiari and Tethered Cord are not unheard of with EDS too. Unfortunately I’m on the wait list for Dr. Montoya (could take years) and am campaigning to see Dr. Safwan Jaradeh who is one of the rare autonomic dysfunction specialists.
I believe there are some, as yet known overlapping causes of the fatigue in EDS and CFS/ME as they share such similar symptom profiles. Please keep writing as your insights will be helping across different patient populations! And I do hope you find things that will help you! Thank you!
Thank you so much for this post! I so appreciate you sharing.
Caroline appears to have access to some good specialists. It’s really good to hear what they are thinking and the different possibilities that are present
It seems the only tool used so far is Allopathic…a hammer. Here are some spanners,screwdrivers,ratchets,etc…Y’all might give’rolfing’, osteopathic manipulation,supplementing with dmso,vit ‘c’,B complex,coq10,NAC,serrapeptase, wobenzm,transdermal mg,homeopathics, essential oils,bach flower essences,cell salts,lugols iodine,alkaline diet,PEMF,Low-level laser therapy (LLLT) a try…it works for me [30 yr cfs/fm, lots of m/bike vs car,swimming pool,roofing,pro auto mech,etc mishaps]
Hi Caroline,
Thanks so much for taking the time and precious energy to put all this information together. There are many similarities between your story and my own (Acute infectious onset, POTS). And recently a new PT pointed out marked hyper-mobility, and suggested possible hEDS and chiari malformation. And, after reading your article, I need to add CSF leak to the list to “chase” as well, as I appear to have most, if not all, of the cardinal symptoms.
You also express many of the same lingering points of confusion (especially those regarding diagnosis) that I’ve wrestled with over the years. ME? CFS? POTS?….
The full complexities of diagnosis are too great to go into here, but your last two articles did bring up one specific question for me….
I know that PEM has come to be the “defining factor” for CFS/ME, but it is unclear to me how unique it really is, amongst people suffering from various chronic illnesses?
I know, for instance, people with various dysautonomias experience what they often call “payback” (increased symptoms as a return for increased activity). And many people who have various autoimmunities have to be very careful about how much they do in order to not trigger significant fatigue, and a rise in other symptoms. Which seems very like PEM to me….
I’ve, personally, ended up wondering over the years if the emphasis on PEM in CFS/ME is mostly because it can be used as a consistent objective measurable datapoint (when looked for in a specialty lab), but also, to importantly and clearly separate the condition from depression (which tends to improve, at least somewhat, with exercise).
But the primary basic age-old objection to the term Chronic Fatigue Syndrome (as a term/diagnosis that we should accept as legitimate at all) is that fatigue is the natural state of pretty much all chronic illness…because the body is in crisis (whatever crisis that is), trying it’s best to heal, and trying to keep up with the demands placed on it. If the demand exceeds the body’s current capacity, then it stands to reason that some sort of payback period will be felt (PEM?), where the body’s basic function is temporarily even more strained then at baseline.
(And I’m not sure how much this subject of PEM has been looked into outside of CFS, because in many comparable conditions – in terms of the levels of disability and fatigue – there are so many more seemingly important areas of research…like the immune system, the brain, etc.)
In my understanding, you, and I, and many of us, may fit the diagnostic criteria for CFS, including classic PEM, but the underlying factors causing those symptom patterns in each of us may be very different.
Even if the central “cause” of CFS is soon determined to be something seemingly very specific, like mitochondrial dysfunction (just for instance), my understanding is that almost anything that affects the body’s access to (or ability to generate) the basic building blocks of energy (and cell function) could theoretically cause mitochondrial dysfunction.
So even some people with primary hEDS (and secondary CSF leak) could end up with mitochondrial dysfunction…possibly as a combined result of things like impaired digestion through GI tracts that tend to be more prone to damage and leak (and therefore malnutrition, systemic inflammation, autoimmunity), poor blood (and oxygen) return to the brain due to “floppy” blood vessels, maybe even a “leaky” blood-brain barrier, and “leaky” cell membranes that leave the important interiors more prone to damage by toxic exposure….and so on.
But so, too, could people with primary mold exposure, or chronic infection, or post-infectious neurological damage, end up with the same “central condition”, such as mitochondrial dysfunction (again, just as an example).
Dr. Terry Wahls’ book, about her recovery from MS, largely focuses on mitochondrial dysfunction as the underlying pathology. (Confusing…but also kind of nice to see that even the experts who are most personally affected by chronic illness are eagerly “crossing the boarders”.)
Anyway, that’s my shortest take on the complex subject!
…but maybe you, or somebody else here, can clarify this point on PEM?
Thanks again for your articles Caroline, and best of luck with your new line of pursuit.
Martha
Marthalauren – It’s like you are residing in my head! As I mentioned, I found myself being a bit defensive the other day when someone in an EDS group claimed that ME/CFS could very well be EDS. I said, sure, but what about PEM/PENE? “What even is PEM,” they asked. Everyone describes it as a worsening of symptoms upon exertion. By that definition many other conditions could be viewed as having PEM. Many people with dysautonomia and autoimmune conditions describe a payback period, as you point out. Is that PEM? I don’t know. For me, immune activation (low-grade fever, body widespread body pain, swollen glands) seems to be the only thing that might separate PEM from the payback phenomenon. Of course there are objective measures, like the 2-day CPET – this is where ME/CFS seems to differ pretty dramatically from other conditions. We call PEM the hallmark symptom of this illness – but how does PEM differ from what is seen in these other diseases?
I know one way: the more we are in PEM, the sicker we seem to get. That is not the case for EDS alone: exercise actually helps, even if there is a payback.
Your point about chronic fatigue being a general illness symptom is a good one. I’ve often wondered about how to reconcile Bob Naviaux’s work on the Cell Danger Response and how it as a highly-conserved response to an assault – whether viral, bacterial, environmental. He claims that abnormal persistence of the CDR lies at the heart of many chronic diseases. I realize that CDR and PEM are not necessarily one in the same, but if impaired energy metabolism is what is at the heart of PEM, and CDR or a hypo-metabolic state is largely responsible for this, then it would stand to reason that this sort of mechanism could well be found in other illnesses (?).
I guess it all hinges on how we define PEM. If it is a worsening of symptoms upon exertion, then it is not unique to ME/CFS. I do think PEM is real and there are clearly elements that are unique to ME/CFS, I just struggle with how loosely it is defined and have yet to see a satisfying (aka scientific) description for it.
Thank you for taking the time in your physical condition to share all you’ve been through. I have CFS/FM which started with infectious mono and never been the same since. I’m 76 so its been 40 plus years and I’m continuing to get worse. I live alone and my family doesn’t understand how very sick I am. Also, I live on Cape Cod, Ma and don’t have the professionals for my care. I would feel blessed to have help because this is a very lonely illness when you don’t have support. May God bless you and thank you for all your information. It really has helped me.
Hi Caroline,
Thank you for your return thoughts on PEM. I agree: very real, and, the typical forward-feeding cycle of PEM, once you are in it, is probably very different than a lot of the “payback” periods that many people experience with other conditions. Once you set “it” off, “it” tends to sets more of “it” off. Whatever “it” is….(PEM)? And I think that is unusual…but I agree, judging by some of the literature/theories you would think it would be described more often in (at least) some other chronic conditions as well.
One possible point of hope for you: after my PT pointed out my hyper-mobile/hyper-extendible joints, and after I’d done enough reading to convince myself that some form of joint hyper-mobility was likely playing into my condition (wether it is inherited or acquired), I began a SUPER gradual self-created reconditioning program, with particular focus paid to my spine. I have always had terrible thoracic spine pain and unbearable chronic headache with this condition (one reason why the csf leak stands out as a real possibility for me too). And (you probably know) one of the main theories for why joint hyper-mobility may be able to cause ans dysfunction is through excessive vertebral movement, particularly the first few which house the brain stem (the ans control center).
Fortunately I got out of the chronic headache a year or so ago (mostly by changing my focus to one of autoimmunity after a positive ANA test: MY first evidence that something other than, or in addition to, CFS/ME was going on.
But many other symptoms, including POTS still remained.
So I laid out a whole (spine-healing) program for myself, with a focused eye on relieving the pain in my spine, bringing gentle circulation to/through it many times a day, super gentle stretching, and very very gradual strengthening.
For the first few weeks I got the familiar lash-back that I am familiar with, with increased pain, and all other system-wide symptoms. AlI was able to do was this sort of PT, eat, sleep, and recover…day after day after day.
But…after about six weeks of doing the exact same thing every day, I felt myself begin to turn a corner in a way that I never have in 17 years. And since then my symptoms continue to improve…including…I now appear to be out of the continuously-being-triggered PEM cycle.
If I stepped out of my routine all of a sudden and did too much, I’m sure I’d find myself in it again soon enough. But for now, as long as I keep on course, follow my routine, I feel markedly better than I have since falling ill. And I’m slowly being able to add in more actuvity that would have historically caused severe backlash (PEM): housework, even standing work (like dishes), and walking much longer with relative ease.
So that’s all just to say, I totally identify with the “diagnostic whiplash” that you describe, but if my experience is any indication of a broader truth (again…who knows?), then getting more specific information and/or diagnosis can make your efforts more focused, and possibly (hopefully) radically more effective.
And…for anyone who suspects the health/function of their spine (in any way) in the genesis of their other symptoms (including ans dysfunction)…I encourage you to look into it!
Take care!
Martha
Hello, thank you for the wealth of information you’ve shared here. One thing I thought of reading your comments here was that actually mast cell activation disorders that improperly release histamines can be comorbid with Ehlers Danlos and POTS. That means you could have an allergic reaction with histamine released against things that you can’t have created an actual antibody against. Things like heat or exercise are possible triggers. Some people have it bad, for example there is EIA, exercise induced anaphylaxis. Have you been evaluated for this? It fits pretty well with what you said, the PEM symptoms you’ve described could be immune related, and could perhaps fit with an exercise induced mast cell reaction?
I can so identify with Kathleen Riley’s comment. I am 74 and have suffered with ME/CFS for over 40 years…began after a strep throat. I live alone and my family doesn’t begin to understand. I have numerous other issues too…including Parkinson’s. In the last year I have thought about “leaving”, but each time God showed me a reason for why I need to stick around. I would be lost without Him!
Question: What pecentage of ME/CFS suffers commit suicide?
Glad you found a rock to hang onto. A mortality study suggested that rates of suicide may be increased in ME/cFS.
I’m being “forced” to once again explore the causes and “cures” for ME/CFS. I was diagnosed after a viral Illness left me bedridden for months in 1991. I was 24 years old and 6 months out from a traumatic c-section, and 12 months out from the death of my 14 month old daughter. Virus plus trauma = CFS? I had slightly elevated WBC for months, swollen lymph nodes, and severe POTS. While I have recovered, I have never been the same since that first episode.
Throughout the 26 years since I have had intermittent relapses of POTS, anxiety,depression, brain fog, hypersensitivity to light, sound, smell and taste, brain fog, severe PEM, migraines and chronic headaches. These relapses can least weeks for the milder ones or months for the horrendous ones. I currently find myself in that dark place once again. Like most episodes it starts with POTS that shows up out of the blue.
The migraines I have experienced have always been somewhat better after sleeping, even if they return later that day wether minutes or hours. But isn’t this the case for most migraines? Almost all of my episodes include migraines and chronic daily headaches. These do not seem to be position related.
I was diagnosed 10 years ago with undifferentiated connective tissue disease which is a way of saying “you likely have an autoimmune disease but we don’t know which one”. They Based this off of a slightly elevated ANA
6 years ago I was diagnosed with Chronic Lymphocytic Leukemia. Which, to me, seems like another symptom of this entire mess.
Like most, I’m a complicated patient. I’m tired. The frustration at not being able to consistently carry out normal life is gut wrenching. This is taxing my marriage, my ability to work, my ability to exist in a beautiful, bright, noisy world.
Thank you for sharing your story and giving me new food for thought.
Yes – another complicated patient! One wonders what is the tie that binds? What could be underlying all these problems. It’s a fascinating question and I’m still astonished that the medical profession is not more interested….
Thank you Caroline and Cort for this critically important blog. Yes, one person in my support group, very ill, could actually hear a dripping sound in her nasal cavity. I mentioned to please ask her doctor about this, and ask about a possible CSF leak. Partly because she had a dx of CFS, this was never taken seriously. There was no investigation.
Even for people who do not have EDS the issue of spinal fluid pressures/ circulation is critical. To even begin to understand the problem it is essential to look at the decades of work by osteopaths and sacroiliac-occipital chiropractors. There is a craniosacral pump, a sophisticated hydraulic type mechanism that circulates spinal fluid – even against gravity, from the sacral bulb to the brain and back. There is a minute motion between the occiput and sacrum, and specific motion of all the cranial bones. Cranial bones are not fused. Of course, the structure and attachment of the dura is a basic part of this.
I have maintained ( many years- and written to many researchers) that this is why women are the predominant sufferers of CFS/FMS – wider, inherently more unstable pelvises.
Blessings to all.
Boston Mass General Hospital Neurology Harvard Professor has found in IBS Fibro CFS a condition called ‘apparent autoimmune Small Fiber Polyneuropathy by using a small needle head size
biopsy it is also known as (aaSFPN)the test is available across the Globe there are treatments they just completed a trial using
Gamma Globulin it was announced in the News on TV & a Press release as well around Nov.17th,2017. They have been working on
this from early 2012 or 2013. She also said the term CFS IBS Fibro are misdiagnosed they had (aaSFPN) all along…They now see this in up to 50% of patients.
Caroline, such an interesting case! I, too, have hEDS, POTS, and have Pseudotumor Cerebri with Secondary Spontaneous CSF Leaks. It has been a very long journey for me. It took 5 years of illness and being passed from doctor to doctor with no one knowing what was wrong before I was finally diagnosed with EDS, and then it was basically “I can’t do anything for you”. There was nothing on the Internet, no support groups, no where to turn, so I just continued on in pain, but with a few more specialists than I had before. I began seeing a Neurologist for daily headaches at about that time, and continued seeing her regularly for 10 years, consistly reporting daily headaches that became unbearable by late afternoon, to the point of being incapacitating, but were relieved by laying down. She put me on migraine meds (which happen to lower Intracranial pressure / CSF production), even though I expressed my concern that it was my understanding that migraines do not occur every single day. And then one morning I awoke to Fluid in my ear, and on my pillowcase, and a small amount of blood in a ring around the wet spot on my pillow. My Neuro couldn’t fit me in for 4 days. She sent me for a brain MRI. She told me everything came back normal. I eventually got a referral to a wonderful Neuro Ophthalmologist, have been treated for leaks and for Pseudotumor Cerebri. But I’ve learned a lot. I’ve learned to get a copy of every image disk and report and to read it myself. The brain MRI from several years ago actually showed Empty Sella, which really should have prompted someone to question whether it was due to high Intracranial pressure, or another possible reason. In retrospect, it was high pressure that blew a leak out my ear; it has been high pressure that has blown spinal leaks; it is surmised that it has been high pressure that has caused meningeal divriticulum at every level of my spine from C3 to Sacrum. Connective Tissue Disorders are not kind to the Dura!
I wish you the best as you navigate your way through the rare disorder world and their comorbidities. Try to choose the least invasive testing possible, should you find it advantageous to investigate the leak perspective. And if I can offer any advice at all, avoid Rebound High Pressure. There are some really great support communities on Facebook, and I highly recommend getting input from patients who have had experience. Best wishes for strength and healing ???
Wow…such high intracranial pressure…what a story. Thanks so much for sharing that. So much of Health Rising is passing information so that others can benefit – thanks for doing that.
High intracranial pressure is another thing that is hardly talked about but obviously needs to be investigated more fully – https://www.healthrising.org/blog/2014/06/04/pressure-building-cerebral-spinal-fluid-chronic-fatigue-syndrome/
Cort, Google (aaSFPN)you will see a lot come up from Boston Mass General Hospital Neurology, as mentioned above She finds 50% of patients diagnosed with CFS Fibro IBS are actually is a wrong diagnosis this also would explain Why 50% are non-responders in Clinical Trials…Imagine for decades one is told they have CFS/ME etc & all along they have instead ‘apparent autoimmune Small Fiber Polyneuropathy by skin biopsy testing…Once diagnosed they then go through a long list of illness that could be making someone Sick a process of elimination including Hep C must be eliminated…There are countless underlying Causes of (aaSFPN)it could also prove why CFS/ME has been so elusive but the question sill rises what about the 50% who have true ME/CFS Fibro IBS etc.? If you have difficulty finding said links message me on Facebook Aidan Walsh p.s Their work started off with a Dept of Defense Grant on Gulf War Illness
Hi Faith, Cort, & Caroline,
I’m reading this almost a year later but wondering which groups specifically on Facebook & other ways I can find support with the exact problems you’re discussing? Thank you in advance!
Faith, I am just like you!
Might you consider talking with me?
Dear Faith,
I am not sure if you will receive this but my story is just like yours and I could use some help with navigating my future steps. I am bed bound at the moment and not able to raise my children. I, also, have a leak and diverticula cysts along my spine. If you have time, could you email me?
Carol
Hi, good article.
Thanks for sharing, keep it up good work.
Wowza. I have been having these symptoms for 11 years. The head pain and pressure is enough to make one want to go to the great beyond. Thank you for this blog – something to look into- although, for me, that alone is a monumental task. Sigh.
I was first diagnosed with a Pseudo Tumor I had an opening pressure over 500+ they said at Univ. of Miami it was the highest the Neurologist ever recorded in 30 years as a Doctor I wonder now if it
was Rebound High Pressure headaches as a result of a leak I have had trauma injuries in the passed from whiplash to sciatica injuries numbness in legs & a fractured neck I was Boxing as well been knocked
down but always got back up to continue never been knocked out…Diagnosis is a long list from Syncope tilt Johns Hopkins 80/30, POTS like symptoms, tachycardia, diastolic dysfunction, CFS, Fibro,
IBS, EDS3 not screened for (VADS) or other types of EDS never seen by Genetics or Metabolic Doctors, Negative Hep. B, C Neg. HIV blood tested but not Genetic test done for CVID, immunologist said not CVID immune
markers said Normal ranges, tested for tryptase Normal at 10 the haematologist said it is not Systemic Mastocytosis. MRI appears Normal once one done they said read in Montreal as Normal then brought it to
Miami it was ‘not normal’ enlarged ventricles & meninges said Miami Neuro who then did emergency LP 500+…Infections tested? Antibodies Lyme Antibodies EBV CMV ECHO COCSACKIE Positive to Stratton test &
Garth Nicolson test…I woke up with a fractured neck one day seen by X-ray right angle was fractured this can happen in Stiff Person Syndrome (SPS) from spasms while asleep I have had issues where my
right Calf muscle locks up becomes hard as rock lying down must get up tap my foot to make it stop & my toes have locked in a down forward position these are also seen in Stiff Person Syndrome (SPS) as well a
rare Neurological disease which I do not think is rare it is underdiagnosed & I have seen it diagnosed in this patient population so a simple (GAD) Antibody test should be considered which I will do in
January. Small Fiber Neuropathy skin biopsy is also seen in (SPS) I have even seen CVID in (SPS) as well but not all have this combined…I have never had the small fiber biopsy test done. (GAD) Antibody test
is always crucial it can also lean to ranges of Diabetes as well so a Normal 5 & below can rule out lots so I will do the test Privately Meedichecks in the UK does it for about £99.00 I have seen a 250 range
come back in patients pointing to (SPS) & Small Fiber Neuropathies (SFN)
Forgot to mention as far as leaks I do have times where I could be out walking & clear liquid runs down my Nose & at Home I am always using Kleenex for a runny Nose & also happens as I eat as well, my left Ear always Pops blocks also very itchy I have heard one can leak into Ears with Spinal fluid leaks & I have a History of Otitis Media which may have not been at all…It could have been Leaks all along
Hey Caroline! Thank you for this well-articulated piece! I’ve just sent you an email to your Sonoma State email address, but not sure if that’s the best way to get in touch. I’m also a California EDS/POTS/possible leak sufferer 🙂
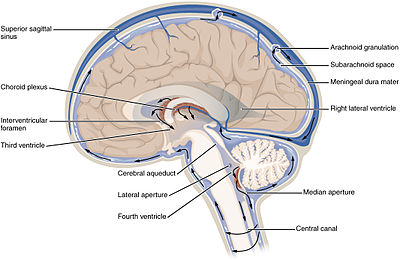
The brain is protected from physical trauma and infection by a clear fluid called cerebrospinal fluid, or CSF. The diagnosis of a CSF spinal fluid Leakage begins with a complete evaluation that includes the patient’s current symptoms, past medical history, and a physical examination.
No, it has lymphatic vessels where viruses, fungi and bacteria can enter.
See https://www.thelancet.com/article/S2352-3964(15)00137-1/pdf
MarthaLauren – Could you share the details of your gentle spine-healing program? I’m having great difficulty in stretching without causing significant spinal-related issues, and just don’t what to try next. Thanks for any information that you can share.
The phenomenon you describe around PEM sounds a lot like the allergic reaction of Mast Cell Activation Syndrome, a common comorbidity of EDS. Treated often with Zantac and Zyrtec every day. Or Cromolyn sodium or quercetin.
Hi Caroline, how have you fared since this blog was posted? Did you have and EBP? How are your overall symptoms?
Thanks and Best Wishes
Carolyn, do you know of any doctors in the NYC/ NJ area who treat for potential CFS leaks? All of the doctors I have seen in the past 2.5 years, since my symptoms started, disregarding to possibility of a CFS leak. I really just want to get back to my old self again without chronic headaches, dizziness, neck pain and all the other strange symptoms that go along with my mystery illness Thant no one can diagnose because my diagnostic tests are all normal! Any referrals are welcome.
Jackie, I highly recommend going to Duke. There’s only 3 main facilities; Stanford (Dr Ian Carroll) Duke ( Dr Gray, Dr Malinzak, Dr Kranz) and Cedar Sinai ( Dr Schievink)
I went through something very similar. After learning hydrocephalus, syringomyelia, Chiari Malformation were not helping my leaks. Spontaneously are known to happen, however other issues can going on. Keep your chin up and don’t give up.
Oh boy! I can see now why my Dr thinks I’m the most complicated patient he’s seen.
After 20 months of consistent headaches/migraines.
I don’t even know where to begin getting this addressed.
I’ve had/have:
hEDs
Partially resected pituitary tumour via transenphoidal surgery with a post operative CSF leak surgically repaired. My pituitary stalk is still slightly deviated by the remaining tumour remnant.
Reactive hypoglycaemia.
Neck injury – anterior whiplash with disc bulges and Psoariatc Arthritis at that site including modic 1 end plate uptake.
Chronic Pericarditis.
POTS
Originally diagnosed with PVFS after multiple coexisting viral infections infections.
Hashimotos.
Breast Cancer – no chemo or radiation.
Specialist just use me as a human ping pong and we’ve tried every headache/migraine treatment we can think of. But it’s all good ….. Because I look great ??? (I’m not sure if sarcasm is a symptom?)
I arrived here doing a search because I’ve noted an increasing left sided nasal discharge that is thin (but slightly mucousy) and salty
Where do I start?
Thanks.
Hi Walking Miracle – Scroll to the bottom of the blog to see the checklist that Dr. Carroll uses. Some of the terms might need to be looked up, but see if any of the items ring true for you. Also, Dr. Carroll advocates doing a 48 flat test – where you lie flat for 48 hours, getting up only to toilet. If your symptoms improve, then worsen when you do get out of bed after 48 hrs, this could be a sign of a leak. The first step is getting a special type of MRI – with and without contrast. However, just because leak does not show up here does not mean you don’t have one.
The other side of the coin is cranial hypertension, also a problem in people with EDS. If you feel worse when feeling completely flat, this could be a sign of cranial hypertension.
The whip lash might be the most likely culprit if you are leaking, although spontaneous leaks can arise in EDS.
I recommend visiting the Spinal CFS Leak Foundation’s site – they are excellent and very generous in sharing resources. https://spinalcsfleak.org/ Perhaps you can find a specialist through them? Good luck! – Caroline
From Japan.
I have seen many cases unique to Japan.
Many patients with chronic fatigue syndrome and fibromyalgia have been diagnosed with cerebrospinal fluid leak.
They can not be cured even if they receive blood patches several times.
I guess this is caused by over-diagnosis by diagnostic methods developed only in Japan.
The doctors diagnose using RI cinching that is considerd unreliable in ICHD-3.
Of course, I hope real patients with CSF leak will be cured through right diagnosis and treatment.
But it seems that many patients have been misdiagnosed and received ineffective treatment.
I think this is a huge issue with Japanese patients.
Cort. What do you think about it?
I’ve got this same cluster of conditions from hEDS and have had huge relief from fatigue and pain when I began taking nattokinase. Maybe hypermobile people are more prone to buildup of fibrin, since our tissues are more prone to leakage/injury? So far no side effects from the nattokinase. Despite being deconditioned from years of illness, I can walk about an hour a day, whereas before I could barely walk for 5 minutes. It’s not a cure for everything, but it helps with my 2 worst symptoms.
Can there be a leak in the brainstem ?
Could PEMF help Ed’s and can?
So sorry to hear it hasn’t worked out yet. Good luck!