

The FDA is clamping down harder and harder on opioid drugs, but it’s the Justice Department that’s probably sending the chills up some doctors’ spines. The Justice Department’s Opioid Fraud and Abuse Detection Unit, which operates in 12 states, last year benefited from the addition of 12 veteran prosecutors. Just recently, the feds began using new profiling techniques that will make it much easier to expose doctors they believe are prescribing too many opioid painkillers.

The feds continue to tighten their squeeze on opioid painkillers – but what are they doing to provide alternatives?
This comes as recent statistics indicate that the war on opioid painkiller produced deaths has been a bust so far. Opioid painkillers killed 42,249 people in the U.S. in 2016 – a 28 percent increase over the 33,000 lives lost to opioids the year before. Two years of declining life expectancy in the U.S. – an unheard of finding in the modern age – are attributed to increasing deaths from legal and illegal opioid drugs. Many of those deaths have occurred when people addicted to opioid painkillers hit the black market looking for relief via heroin/fentanyl. Deaths from these types of opioids more than doubled from 2015 to 2016.
Half the states in the U.S. now place restrictions on how many opioids doctors can prescribe, and there’s more to come. Last month in the Financial Times FDA Commissioner Scott Gottlieb stated that the FDA was going to make it more difficult for doctors to justify prescribing more than a few days worth of opioids.
The squeeze is on. Opioid painkillers are not disappearing by any means but they’re going to be harder to come by as time goes on. With nearly 100 million people in the U.S. being prescribed an opioid painkiller every year, any significant reduction in opioid drug use is going to open a large void in pain relief. How that’s going to be filled – if indeed it is filled – will occupy the rest of this blog.
That question is an important one for everyone with fibromyalgia or chronic fatigue syndrome (ME/CFS) who suffers from pain – even if you’re not using opioid painkillers. That’s because the reductions in opioid drug use will result in a need to find alternatives, possibly economically lucrative alternatives.
Behavioral approaches to pain are being increasingly touted but they will be covered in other blogs.
Medical Marijuana to the Rescue?
At first glance, medical marijuana seems to be a prime choice to step in where opioids have failed. It’s now readily available; more than two-thirds of Americans live in areas that have legalized medical and/or adult use of marijuana. Approximately 2 million Americans use cannabis to treat a medical condition. It’s recently been legalized in California and Nevada and has been legal in Oregon, Washington and Colorado where legalization is proving to be an economic boon.
Perhaps more importantly, several studies suggest that legalizing medical marijuana results in significant drops in prescription opioid drug use, hospitalizations, and even deaths due to opioid drugs as opioid users switch to the safer drug.

After calling the opioid epidemic an national emergency, the Trump administration began putting the squeeze a possible alternative – cannabis-based products.
Given the public attention (but not money) the Trump administration has given to the opioid epidemic, one might think they would be opening the spigot for more research into one of the possible substitutes for opioids, but not so. In fact, the opposite may be happening. Recently, Trump’s attorney general, Jeff Sessions, rolled back Obama era rules stating that federal prosecutors were not going to spend their precious time and money going after marijuana users, producers and providers in states that had legalized the drug.
It’s not clear whether the Trump administration will go so far as to attempt to stifle the popular and economically lucrative marijuana industries springing up. Marijuana sales top $1 billion, bring in hundreds of millions of dollars in sales taxes, and the industry employs thousands in Colorado. That number is sure to be dwarfed in California.
The new guidelines are sure to produce something of a chilling effect in the growing cannabis industry, however. Despite the study evidence suggesting cannabis could be part of the solution to the growing opioid drug crisis, the Trump administration views cannabis as part of the problem.
“Today’s memo on federal marijuana enforcement simply directs all U.S. attorneys to use previously established prosecutorial principles that provide them all the necessary tools to disrupt criminal organizations, tackle the growing drug crisis, and thwart violent crime across our country,”
Poor Research Environment Continues
The federal government did relax some restrictions on cannabis research but the plant is still difficult to get, leaving research stifled. UCLA’s Cannabis Research Initiative (CRI) states it is “one of the first academic programs in the world dedicated to the study of cannabis”.
The program openly states that its main priority is finding ways to use cannabis to reduce opioid use.
“One of our top priorities is to conduct the world’s first human study using cannabis as a treatment to potentially reduce opioid use in chronic pain patients on opioids. We are amidst our nation’s worst opioid epidemic, which is killing an American every 16 minutes, and killing 33,000 Americans a year. Worst of all, the epidemic is only accelerating, and there is no end is in sight.”
Yet of the Initiative’s 14 research projects underway, eight focus on the negative effects of the drug (mostly on adolescents) while only four pursue therapeutic possibilities. None yet focus on how cannabis might supplant opioid drugs as pain-killers.
The reason – no money – and the many barriers to research that remain. In “Medical Pot is Our Best Hope to Fight the Opioid Epidemic” Rolling Stone noted that the CRI “has scientists, clinics and a study design all lined up” but essentially no funding. With virtually no government support or interest from pharmaceutical companies, one of the few academic centers devoted to cannabis research is “pretty much dependent on philanthropy.” More Americans are being killed very year than died in the Vietnam war, yet the federal government cannot fund research into one of the few potentially viable alternatives to opioids.
That’s a shame. The Initiative’s director, Jeff Chen, told Rolling Stone that he believes cannabis may also be able to reduce the addictive problems associated with opioids.
“If there is a chronic pain component, the cannabis can address the chronic pain component. We also find opioid addicts have a lot of neurological inflammation, which we believe is driving the addictive cycle. We see in preliminary studies that cannabinoids can reduce neurological inflammation, so cannabis could be directly addressing the inflammation in the brain that’s leading to opioid dependency.”
That suggests that cannabis by itself or in combination with opioid drugs could reduce the levels of opioid drugs needed and the addiction problems that is causing the opioid fatalities.
New Classes of Pain Drugs
Meanwhile the FDA’s response to the pain-killer epidemic is to focus more efforts on approving opioid-type drugs formulated to deter abuse and to make it easier to treat overdoses. No effort that I can tell is being made to identify or support the real need: new classes of effective, non-addictive, non-opioid pain-killers. The FDA is missing the forest for the trees.
What about new drugs, though? With the feds cracking down more and more on the 20 billion dollar U.S. market for opioids, the economic windfall for a pharmaceutical company could be huge. Plus the FDA is under the gun to approve pain drugs – pressure that may have lead it to fast-track an anti-nerve growth factor, monoclonal antibody drug called Tanzemub. Tanzemub, if approved, will likely be very expensive but it may be an option for those in chronic, intractable pain.
Aside from Tanzemub, Seeking Alpha was able to only identify one other new pain drug in Phase III trials and only four in Phase II trials. Reports on the 11th Annual Pain and Migraine Therapeutics Summit from the Pain Research Forum suggested that right now the pain treatment glass is more empty than full but that options are emerging.
Next Generation Opioid Drugs
Perhaps the most exciting options are next generation opioid drugs that reduce pain without producing nasty side-effects like dependence, tolerance and addiction. New technologies that have allowed researchers to understand how opioid receptors work are enabling them to target receptors that reduce pain without activating those that produce side-effects.
Next generation opioid drugs may be able to get by the addiction problem (but will they work for chronic pain?)
Oliceridine – Just three days ago the FDA granted a new drug application for Oliceridine – the first of the next generation opioid drugs to make it into clinical trials. Oliceridine isn’t going to turn the world around; it’s an injectable drug destined for hospital settings but it does present a first look at the possibilities these new opioid formulations present. Thus far, Oliceridine has been as effective as morphine while producing fewer side effects (reduced nausea, vomiting, respiratory problems). Oliceridine is being marketed for hospital settings in part because it, like other opioid drugs, appears to be far more effective at reducing acute, not chronic pain. Whether any of the new opioid formulations can surmount the problem of lessening effectiveness over time is a major question.
PZM21 – The hullabaloo over PZM21 demonstrates the fraught world of the next generation opioid painkillers. When news of this drug popped in August 2016, Bloomberg News called it “The Drug That Could End America’s Painkiller Epidemic“. Other media outlets jumped on the bandwagon. This drug, which resulted from a new understanding of the mu-opioid receptor opioid painkillers bind to, appears to produce few side effects including reduced dependence and addiction. Nothing has been heard of this drug since 2016 but it’s believed human trials may begin in the next year or two.
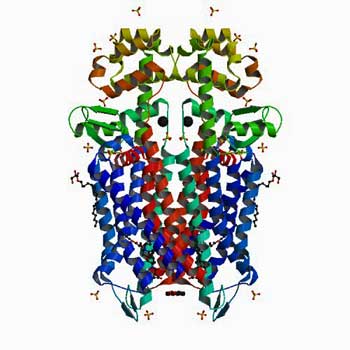
Opioid Breakthrough – Just last week, researchers at the University of North Carolina School of Medicine announced they’d produced a breakthrough in understanding at a very detailed level how the opioid receptor works. They synthesized the drug using 3-D imaging of the active receptor – the first time that had been done. Because the new drug has yet to be tested in human or even animal models, it will be years before it might come to market. Still, the team expects the breakthrough will allow drug companies to modify current drugs to reduce side effects and novel drugs to show up over time.
“These molecular insights promise to accelerate the structure-guided design of safer and more effective k-opioid receptor therapeutics.”
Voltage Gated Sodium Channel Blockers
Because voltage gated sodium channels turn on and off the pain signals in nerves, they provide a way to get at pain production very early in the game. No need with these drugs to quiet the brain down with opioids or other drugs; simply turn off the signals going to the brain in the first place. Nav 1.7 is the channel that’s received the most attention and drugs that effects it are in clinical trials.
One drug trial (BIIB074) in trigeminal neuralgia succeeded in everything but meeting its primary endpoint (unfortunately) and the company will continue working with it.
Migraine Drug Wows
The Pain Research Forum (PRF) reported that a new migraine drug, Erenumab, wowed participants at the 11th Annual Pain and Migraine Therapeutics Summit in San Diego. The PRF reported that the drug – which is an antibody aimed at the calcitonin gene-related peptide (CGRP) – has been successful for a large subset of migraine patients in several trials. In 10-20% of patients it has abolished migraines altogether.
According to the Relief website, the journey of a CGRP target drug in migraine has had a fraught history. Big pharma was very high on it until almost at the last minute when in 2011 signs of liver problems were seen in some recipients and years of work was abandoned. Other companies, however, picked up the pieces and began trying to knock out CGRP using antibodies. Four companies are now in a race to produce the first effective anti-CGRP antibody drug.
Allodynia will be particularly interesting as its presence predicts that a migraine sufferer will fail to respond to migraine drugs. Poor responders to migraine drugs, on the other hand, fared best in anti-CGRP trials.
Because CGRP appears to play a key role in the sensory stimulation problems in migraine, it’s possible CGRP drugs could help in allodynia (central pain sensitization), fibromyalgia, ME/CFS and perhaps diseases like chemical sensitivities.
Conclusion
No quick drug answers to immense pain problems facing U.S. consumers loom. Given the enormous costs and suffering chronic pain produces the few options being produced are paltry indeed. One has the feeling that for all the press about the opioid epidemic and its costs – including an unprecedented two year drop in life expectancy in the U.S. – the federal government remains mostly unengaged in producing long-term solutions to the problem of chronic pain.
When fibromyalgia and migraine – two of the most common chronic pain problems effecting tens of millions of Americans – receive about $1 per patient per year in funding, it’s hard to argue that the federal government has gotten serious about chronic pain.
Despite some movement, politics is still, unfortunately, bollixing up one of the prime opportunities for pain relief – cannabis derived drugs. The Trump administration’s move to return to a hostile stance on cannabis is unwelcome and short-sighted.
Progress on producing safer opioid drugs is, thankfully, continuing and we can expect more drug trials in the future. Whether or not the new drugs will be effective in battling chronic pain is unclear, however.
The much bally-hoo’d sodium channel drugs have run into some obstacles, but given the central role these channels play in pain production, research is expected to continue.
Finally, the race is on to produce a breakthrough migraine drug – the first ever specifically produced for migraine. If the anti-CGRP drugs win out they may have applications for other pain sensitivity conditions like FM, ME/CFS, allodynia and chemical sensitivities.
Drugs aren’t the only solution. The NIH is pouring substantial resources into understanding how neurostimulation may be used to modulate nervous system functioning. A hyperbaric oxygen chamber fibromyalgia study is underway in Israel and Dr Natelson is pursuing vagus nerve stimulation in GWS.







The clampdown on opiods is very scary for those of us that are suffering from extreme pain. I am one of them. In 2017, i tried to end my life as I did not want to suffer anymore.
I believe in the right to choose how I live. It is NOT up to the decisions of politicians and medical professionals who dont live with pain every single day.
Thus, I have been given a life sentence without parole. Research wont help me as my time will run out before big pharm comes up with a new solution.
I, like many othets, will die in pain.
Cort,
I am so glad that the health reasing campaign was such a succes! Better then other years.
thank you for all the articles you write and keep us updated!
Thanks! Yes, it was very gratifying (and relieving)!
Being a person who suffers from pain, this opiophobia is very upsetting and I believe the governmental approach is misguided–but that’s not what I want to talk about.
Everybody is so different in what really works for them; medical marijuana does not work well for me, I have not been allowed to try nasal ketamine, OTC and other usually prescribed drugs don’t really fully control the pain, CBT, mindfulness and meditation are helpful but a joke when it comes to severe pain.
Norco does do a good job and a certain plant who’s non-Latin name begins with ‘K’ also works well–but the availability of both is coming into question.
Currently I’m trying Low Dose Naltrexone (LDN). It can takes weeks to get to full effect and it doesn’t work for everyone. Also if one has a ‘flair’ there is not much to take in addition for relief (excepting the above mentioned excluding opioids).
A while back there was a interesting article here about a ‘bed of nails’ mat which promoted less pain by stimulating the body’s endorphins. LDN blocks the opioid receptors which keeps more of the body’s endorphins in circulation–hence reducing pain.
I had a very interesting experience which might point to a new direction in pain control (at least for experimenters like me). As I said LDN doesn’t entirely cover my pain–that is until I had a biopsy which left me sore and suffering. I was very surprised to notice that a day or so later my over all body pain dropped substantially and so I am theorizing that it produced more endorphins than normal and the LDN helped them stay in circulation–kind of like a push-pull of natural pain control.
I don’t want to ‘flog or stab’ myself to stimulate pain in order to have the LDN be more effective, but the idea of tricking the body to work towards a more effective way to manage pain is an intriguing one.
I’m close to my 23rd year dealing with FM. My Doctor(Canadian) first prescribed Tylenol #3 and after awhile when it lost it’s effectiveness he prescribed Oxycodone. Before too long, this more powerful opioid lost it’s effectiveness as well. He then was able to get Tramadol from Health Canada through the ‘compassionate programme’ since it still was not available in our Country. I’ve been on Tramadol for many years now and I get the same pain relief every time. It does, however have a peculiar side effect. It actually causes more pain for the first 1/2 hour or so, before providing that blessed relief that lasts for 3-4 hours. I found a way to circumvent this problem by adding I extra strength rapid release Tylenol(acetaminophen)which is less expensive, to the Tramadol.
Taking too much Tylenol creates it’s own problems though, as it can negatively affect the Liver. The daily dose should not exceed 8, which I still feel is way too much. I was questioning staff at Health Food Stores on what can detox Tylenol from the Liver and they all recommend Milk Thistle. So now I’m taking that every day for extra insurance.
My Medical Doctor went to a pain conference in the U.S. last summer and came back from it very confident about Tramadol’s effectiveness and safety. I read years ago that it does have an opioid base to it, but it works differently, in that it prevents the re-uptake of Serotonin. I also find that Tramadol also gives me more energy and I’m more alert. I’m not sure if that would be true for everyone. Tramadol is a generic now and very inexpensive, so if your Doctor prescribes it for you, make sure it’s not a more expensive brand name.
Tramadol gives me migraines! But I’m happy it works for you! Please be careful how much Tylenol you take!
Tramadol is the only med that helped me to return to work, it worked better than the high dose morphine that replaced it One day taking the first pill of a refill, there was absolutely nothing,zero. Doc gave refill, Went to lower volume pharmacy and it worked again. That was the last. Same label – FRUSTRATION
The article states clearly that the people overdosing are doing so after going to the blackmarket seeking relief. Which they wouldn’t be, if the government would keep it’s nose out of things it doesn’t belong in, like medicine. If you aren’t my treating physician, then you don’t know what kind of pain relief I need. But you think you know enough to cut back the amount of medicine I receive by threatening my doctor with jail time if he prescribes what I do need. So he cuts me back, now I’m in constant, unbearable pain, and I go looking for relief where ever I can find it. And you end up with another overdose, because a dealer isn’t a doctor. The GOVERNMENT and their crusade against medications that work is what is behind the increase in the overdose increase in this country, not the medication. Put the blame where it belongs.
Good point. One logical outcome is that the restrictions may lead more to seek out the black market.