

We propose that chronic idiopathic spinal fluid pressure dysregulation underlies both FM and the clinical entity of symptomatic Tarvlov cysts, which both present as peripheral neurological disorders. The authors
This is the third in a series of blogs providing overviews of new hypotheses for fibromyalgia and chronic fatigue syndrome (FM, ME/CFS). (It is also part I of a three part head and neck series on fibromaylgia and ME/CFS).
Whoever ends up explaining fibromyalgia is going to have to explain the wide variety of symptoms found in it. A group from Belgium – a country not particularly known for its biological interpretations of diseases like chronic fatigue syndrome – believes that FM patent’s brains and spinal cord are under too much pressure.
Fibromyalgia and unexplained widespread pain: The idiopathic cerebrospinal pressure dysregulation hypothesis. M. Hulensa,⁎, W. Dankaertsa, I. Stalmansb,c, A. Somersb,c, G. Vansantd, R. Rasschaerte, Bruyninck Med Hypotheses. 2018 Jan;110:150-154. doi: 10.1016/j.mehy.2017.12.006. Epub 2017 Dec 5.
Tight Sleeves
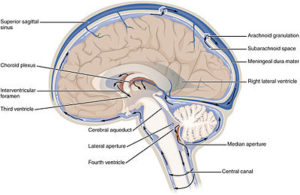
More specifically this group believes that high spinal fluid pressure in the sleeves of the spinal nerve roots of FM patients is compressing those nerves causing a “polyradiculopathy” or pinched sensory nerves across the spine. These pinched sensory nerves are in turn causing pain and other symptoms across the body. The difference between these pinched nerves and the pinched nerves we ordinarily think of is that spinal fluid pressure, not structural problems, are the cause.
Certainly something is going on in the head and upper bodies of FM patients. Upper body pain, feelings of pressure in the head and head pain are common. The researchers argued that the peripheral neuropathy (numbness, tingling, electric shocks, burning sensations, allodynia, weakness) and reduced muscle strength studies have found could all be caused by increased spinal fluid pressure.
Interestingly, they propose that the deep muscle pain FM patients sometimes feel could be due to damaged and/or lost small nerve fibers in their sensory nerves. (Dr. Oaklander has also proposed that small nerve loss inside the body may be causing many symptoms in FM.) They believe that high levels of pressure are causing degeneration of the sensory nerve roots. Nerve conduction studies showing demyelination is present in some FM patients buttress, they say, that finding.
The authors also propose that the gastrointestinal problems so common in fibromyalgia could be caused by compression of the nerves in the lower spine.
Fibromyalgia Mimics
They note that similar symptoms to FM (upper body pain, facial pain, cognitive problems, gait issues, reduced gray matter volume and others) also occur in several diseases associated with increased cerebral spinal pressure (Idiopathic intracranial hypertension (IIH) and Idiopathic normal pressure hydrocephalus (INPH)).
Tarlov Cysts
High spinal fluid pressure may be causing Tarlov cysts as well. Tarlov cysts are cerebrospinal fluid filled sacs which form inside of the sheaths surrounding the dorsal root ganglion’s nerve roots. (The dorsal root ganglion are clusters of nerve cell bodies found in nerves emanating from the spinal cord. They convey sensory and other information to the spinal cord.)
The authors believe Tarlov cysts provide a kind of buffer for the sensory nerves against the increased cerebral spinal fluid pressure emanating from the spinal cord. (Tarlov cysts are also believed to result from inflammation, trauma or disease).
When small, these cysts often cause no symptoms, but when they are larger they can, by putting pressure on the sensory nerves, cause pain, tingling, muscle spasms, muscle problems, and/or pinched nerves. For some reason, women are more likely to suffer from them.
Chiari Malformation
The Intracranial Hypertension Research Foundation reports that Chiari malformation, which occurs when a bone in the back of the head is pushed down into the spinal column, blocking the circulation of spinal fluid, may be more common in people with IH. Chiari malformation has been found in some FM patients. One 200 person+ study, however, found that FM patients had about the same percentage of chiari malformation (@3%) as the healthy controls.
A Chronic Fatigue Syndrome (ME/CFS) Connection?
The cerebral spinal fluid fibromyalgia hypothesis is interesting given the small 2013 chronic fatigue syndrome (ME/CFS) study suggesting that high intracranial pressure and headaches are common in people with ME/CFS.
Twenty percent of the 20 study participants meet the international criteria for idiopathic intracranial hypertension (IIH) and so were reclassified as having that condition, and treated. Even more interesting were the 85% of ME/CFS patients who, without having high spinal fluid pressures, nevertheless benefited from reductions in spinal fluid pressure.
None of the responders had the major clinical signs (papilloedema, visual disturbances) doctors look for to suspect IIH. When their spinal fluid pressure was reduced, they reacted just like IIH patients do – they felt better; i.e. they experienced reduced headaches, heightened alertness and reduced fatigue that lasted anywhere from a couple of minutes to several weeks.
Dr. Higgins concluded that the normative values for IIH are probably incorrect and that some people, perhaps many people, suffer from IIH at far lower cerebral pressures than is currently expected. They also display different symptoms (little eye involvement) from traditional IIH patients.
In a recent blog, ME/CFS/FM/POTS/EDS patient, Caroline Christian, reported that her Stanford neurologist suspected she was suffering from spontaneous leaks of spinal fluid and “pseudomotor cerebri” or excess cerebral spinal fluid and increased cerebral spinal fluid blood pressure. People with this condition usually have worsening head pain when their head is slightly lower than their body. Dull headaches, often at the back of the head and worse at night or first thing in the morning are common. The increased pressure can produce temporary problems with blurred vision or even blindness and double vision.
Personally, Dr. Higgins’s study and the FM hypothesis brought to mind a spinal tap which left me feeling unusually relaxed and clear for a couple of hours. I also know of a person whose ME/CFS/POTS virtually disappeared for three weeks following a spinal tap. A Canadian doctor is reportedly working on a paper highlighting the unusual changes she sometimes sees in her ME/CFS/FM patients after spinal taps.
Assessing Cerebral Spinal Fluid Pressures
Unfortunately, assessing cerebral spinal fluid pressure is not easy (it usually requires a spinal tap). Plus, as we’ve seen, normative CSF pressure values may not be very normative in ME/CFS/FM and some people with seemingly normal CSF values can benefit significantly from a reduction in pressure.
The authors of the article suggested that the following tests be done to assess the presence of high intracranial pressure: spinal tap, sensory testing using a pin-prick test, strength testing, knee and Achilles tendon reflexes tests, a tandem gait test, a revision of the MRI to detect possible nerve root dilations and TCs, NCS/EMG, and measurement of the retinal nerve layer thickness using an optical microscope.
Treatment
Treatment for increased cerebral spinal fluid pressure usually consists of carbonic anhydrase inhibitors (such as acetazolamide (Diamox), Methazolamide (Neptazane), furosemide (Lasix) and topiramate (Topamax)) which reduce CSF levels.
The Intracranial Hypertension Research Foundation reports that spinal fluid pressure rises when the body can no longer effectively absorb or drain it. Ray Perrin has some ideas about that – his work will form the second part of HR’s FM and ME/CFS Head and Neck Series.
Health Rising’s Fibromyalgia and ME/CFS Head and Neck Series
- Pt. I – Pressure Mounting: Is Fibromyalgia Caused By High Pressure in the Brain (Intracranial Hypertension)
- Pt. II – Ray Perrin – Reduced Lymphatic Drainage in ME/CFS/FM
- Pt. II – Dr. Rowe – Spinal stenosis and ME/CFS







I wonder how this work might also relate to chronic migraine?
Exactly my thoughts as a person with fibromyalgia and migraine.
Intercranial pressure may have unexpected causes. I have had a diagnosis of Chronic Fatigue Syndrome since 1984. I have had many treatments from many doctors, some helpful, others not so much, but I am reasonably functional compared to many.
I was, however, frustrated with the lack of continuing improvement and decided to explore the possibility of Mast Cell Activation Syndrome. This seemed to fit my lifetime health history.
I was tested and found to have numerous contact allergies. The doctors decided to put me on a trial of small doses of two antihistamines along with Zantac and Singulair. The next morning, my vision was blurry. When this didn’t improve off the meds, I went to my optometrist who found high eye pressure and sent me directly to a glaucoma specialist.
I was diagnosed with narrow angle glaucoma and had laser surgery which seemed to correct the problem.
Several weeks later, however, my left eye became bright red, the eyelid droopy, vision blurry and I had hellish headaches. My eye pressure skyrocketed and I was sent for an MRI with contrast.
The results of this test were that I had a carotid cavernous fistula. This was confirmed by a angiogram. Th CCF involves a connection (fistula) forming between an artery and the veins behind the eye. If it is not diagnosed and treated quickly, you can lose your vision or even have a stroke. My CCF was resolved through a nearly five hour operation where a neuro-radiologist threaded catheters through both groin arteries and into the brain where he used platinum coils to separate the artery and the veins, relieving the pressure. After the operation, I had double vision for a month that required patching one eye. This is improving and the headaches are gone. CCF is very rare (1/100,000), but I can’t help wondering if it is related to the CFS I have had since 1984.
For the love of all things bright and beautiful! Have any of you with migraines, neck pain, and intracranial pressure ever had an MRI?
I was born without the band of nerve fibers that connect the right and left hemispheres of the brain. It’s a condition called complete agenesis of the corpus callosum. I also have a Chiari malformation, migraine disease (24/7/365), and intracranial pressure.
Perhaps if you had your doctors look into the neurology – not psychology, but neurology of your heads, your all-over body pain would lessen enough to finally be able to function, and get back to staying awake.
wow i definitely have the intracranial issues and headaches & neck pain. worse from mild toxin exposure, worse from cold, & worse after exercise, worse if sick… but this is a new perspective. i tried ldn twice-couldn’t take it my dr wants me to try a minute dose this time & see if that helps. herbs help, craniosacral helps, thermafore heating pad helps, acupuncture helps
The timing of this post is terribly interesting to me because I’m meeting with a neurovascular surgeon this week for an IIH assessment. I rarely post here because I don’t usually have any answers to anything, but this is the rare topic where I might actually have relevant knowledge. Here goes!
I consider myself an ME/CFS patient because the fatigue is my biggest complaint and I have many of the same co-problems that developed around the same time (severe POTS, sensory sensitivity, cognitive problems, body pain, IC and increased allergies). But I’m clearly a different subset than some, because the onset wasn’t viral and a 2-day exercise test showed no drop on the second day. I do have some version of EDS or Marfan but had no significant problems till “whatever this is” began, so I see that as a probable risk factor but not the explanation.
Besides the usual ME/CFS stuff, I’ve had a constant headache behind my eyes for the past 12 years, plus a feeling of “inside-going-out” pressure in my head and buzzing in my ears. They developed over about a year, but over the same period as the fatigue and other symptoms. I’ve had multiple brain MRIs over the years (including a standing one for Chiari), and they’ve all been read as totally normal.
The direction of the head pressure finally made one of my doctors wonder about IIH and give me a trial of Diamox. The drug immediately took away the headache and other head symptoms, but side effects made me too sick to continue. I wasn’t on it long enough to know whether it had a positive effect on anything beyond the head pain and pressure, but my mood did seem better in an organic way (beyond “I’m happy because my head doesn’t hurt”!).
So, don’t know if one person’s experience can mean much, but my takeaway is that any IIH subgroup might be less likely to be post-viral, more likely to have connective tissue weakness, and more likely to have headache and other “head symptoms” (pressure, sounds in ears, vision problems or dizziness).
Also, if you have EDS and are wondering about IIH, be aware that the pressure measurements tend to work differently than in normal people. One of the big EDS-IIH experts, Kenneth Liu, says in one of his talks (available on YouTube and you can probably find it by searching those two acronyms) that he doesn’t understand why his procedure even works because EDS people tend not to have pressure readings that are very high. Dr. Pocinki’s theory is that that’s because of stretchy veins — if you increase the fluid in a metal pipe, the fluid pressure will read higher than if you add the same amount to a stretchy water balloon. But the water balloon itself is still under increased stretch, and it’s more “bulgy” and might press on other things nearby. Increased problems, but no increased pressure…. Makes sense to me, at least, but beware that some neurologists may just look at the pressure numbers alone and say you don’t have IIH, even if you have other symptoms.
“..if you increase the fluid in a metal pipe, the fluid pressure will read higher than if you add the same amount to a stretchy water balloon…”
Important question: what role is fascia’s stretchiness or lack of it, likely to play in pressure measurements in crucial analyses including this spinal fluid one?
I don’t know but I would think that connective tissue problems would apply here….(???)
There is connective tissue – fascia – around everything. For example, irritable bladder in FM is almost certainly related to the inelasticity of the fascia envelope in which the bladder is located. I have long hypothesised that the extreme vulnerability to rapid physical collapse when attempting high exertion levels, especially in certain postures, is because inelastic and stuck fascia is squashing crucial blood vessels and other vessels. It would not surprise me if there are locations where fascia elasticity is essential for the mitigation of spinal fluid pressure, simply by “yielding” when the pressure is high enough. Even if the spinal fluid is contained within tissue that is not fascia, there will be fascia directly adjacent to it. Tightness and stickiness in the fascia throughout the body has major implications for all manner of things that are hardly even begun to be understood.
Even the skull is not an immobile hard shell; it is several separate bony formations connected by connective tissue, which in normal healthy people have some freedom of movement relative to each other. Craniosacral therapists distinguish the tightness and immobility of this system in different patients, and FM patients always have an extremely tight “skull”. This almost certainly has consequences for the pressure of the cerebro-spinal fluid within it and furthermore, for the freedom of flows of this and other intersticial fluids. “Movement” almost certainly acts as a natural “pump” for the shifting of fluids around the body, and there are consequences including stagnation, toxicity and further adhesions, when the surfaces between which fluids must flow, are tight, stuck and dehydrated.
https://www.anatomytrains.com/blog/2017/07/24/q-tom-hydration-fascial-matrix/
Very interesting, to think of rigid fascia as causing higher pressure. I’ve always wondered if abnormally tight fascia was implicated in FM/CFS.
Can physical injury like whiplash and car accidents be causing intracranial hypertension? I know traumatic physical injury can trigger the onset of symptoms. This article seems to expand beyond physical causes, however I’m equally interested in a strictly anatomical cause of I. Hypertension.
Yin yoga is a style that works on fascia. It has helped me greatly with pain and symptoms.
“Can physical injury like whiplash and car accidents be causing intracranial hypertension?”
I learned this week from my physical therapist that the brain plus the spinal cord are located in one big bag containing the cerebral spinal fluid. That makes sense. So it is a bag shaped like a ball (brains) with a very long tail/cord (spine). This bag is located in fascia, like all organs apparently are.
She told me that in order to explain what the exercises she proposed physically did: pull gently on the “cord” and reshape the “bag” with the brains in it. That helped to “reshape/redistribute” the brains a bit and explained the difference in pressure/pain (amount, type, location) I said I felt when trying the exercise or when I did similar things before. She also explained me how craniosacral therapy could help with that and how it would do that. Before it seemed to be a “new-age” therapy to me.
=> So if gently doing exercises puts strain on this bag/fascia surrounding it and can gently reshape the brains form, then a violent whiplash should do far more then that. I could see it put a shock wave on the brain far greater then a bump/concussion can do, with deforming it in a damaging way. I see it also put a lot of stress on these (inner and outer?) bags possible causing tearing and scars (that are *very* often less flexible). When scars are bent they sometimes crack time and again before being completely healed, increasing the scaring.
The exercise I asked her was one to improve blood flow in the arms, but I gained something far more valuable I hope. I have been quite happy with my exercises to “activate” the leg-blood-pump. Helped really well. I found it a shame there couldn’t be such pump for the brain as the brain is not made to do physical exercises. But this may open a path to activate my newly discovered brain-blood-pump.
IMPORTANT NOTE: neck exercises by themselves can be dangerous when done wrong. Trying to use neck exercises in order to “deform-reform” the brain so that it has its own blood pump adds considerable risk and is really experimental. So being very careful AND gentle AND discussing what exercises are safe with a good physical therapist is an absolute must for anyone even considering this!!!
It may also explain why my neck exercises were at the basis of my first clear improvement of health. They seem to do a lot then just making the veins between hart and head more flexible.
Thanks, Jessica, and thanks again Dejurgen, you never cease to provide insights! That is exactly as I guessed it should be thought of.
I didn’t know about Yin Yoga (how does it differ from “Yoga”?) but Robert Schleip’s books and papers deal with the fascia and how to mobilise it through movement routines. He calls the concept “Fascial Fitness”.
I have also been lucky to find a massage therapist in my area who has had training from Schleip himself, and understands fascia. His hands-on skills are excellent and have benefited me. However, I think it is highly important to understand the fascia as having relative degrees of lubricity / adhesiveness and FM, I strongly hold, is a condition of adhesiveness in the fascia throughout the body.
The problem with “releasing fascia” is that it can be so tightly stuck, and this is all over the body, so that all you do is injure yourself. Schleip is dealing with people who are largely healthy, and does not seem to investigate or discuss FM at all, or the possibility that a body-wide fascia systemic dysfunction exists as a disease in its own right. Also, “releases” quickly reverse as the underlying toxic “glue” is still swamping the entire body and even being produced and added to.
I believe I have proved that it is essential to “de-tox” and hydrate and mineral-rebalance and adopt strict exercise “pacing” so that the “glue” is being cleared out (slowly) and not being added to. See my comment elsewhere on this thread about Feldenkrais, too. Feldenkrais gets muscle fibres embedded in deep complex systems, finally “stimulated into movement” possibly for the first time for decades, which mobilises reservoirs of toxins from those locations.
Phil, I’ve been reading your comments about fascia with great interest. I suspect that many of my frustrations with pain are secondary to trying to move – especially when trying to reach, stretch, bend, and lift- because of tight fascia. I used to be athletic and could do fairly advanced yoga. Now I can hardly move and feel as if I am made of cement. All if this started 30 years ago when I noticed that I was having difficulty running/jogging. My legs started feeling heavy and stiff. I have tried many types of therapy to loosen fascia, but only to make my symptoms worse. Even stretching programs for people who have pain make me worse, even if pacing and only doing a couple of minutes per day.
I noticed your comment about bladder problems in FM being related to stiff fascia. I wonder if that is what is wrong with mine? A diagnosis of IC (interstitial cystitis) is what I was given, yet none of the treatments for that condition have helped me.
Has anyone questioned why some of us have tight/sticky fascia? What triggered all of this? Personally, I had a few accidents that I can’t help but wonder if somehow laid the groundwork for all of this. One accident was being thrown from a galloping horse, another a bad water-skiing fall, and then the many snow skiing falls, plus more minor accidents. These happened in my teens and 20’s, and my ME/CFS/FM didn’t begin until age 32.
I have had 2 frozen shoulders in the last few years (I’m now in my 60s) and a surgeon who operated on one shoulder had a terrible time trying to get a scope into my shoulder due to scar tissue.
Are there others who have had any similar experiences?
TwoWishes, I’m an EDSer too. Maybe you have CCI… Here’s a link; http://www.thepainrelieffoundation.com/craniocervical-instability/
It’s not uncommon with EDS…
That was great info to share Two Wishes. How did you go at the neuro vascular surgeons?
I love this! Yes patients with EDS have low pressure readings and have IIH. This is so true.
I would like to add here that I have dysautonomia for past seven years but it was mild. I didn’t have pots but other conditions that high stress levels cause in a normal human body. My body was 24*7 in stress mode not because I had mental trauma but coz my body was in this state due to some problem. I was a very happy kinda girl I never had stress in my life.
But then one year back I read about cranio sacral therapy and I tried it on my own on my skull. And just after trying it I developed pulsatile tinnitus and POTS. I think I circulated CSF more than it was required. And now I also have pappileodema and sound and light sensitivity.
I am not able to find out that whether any neck structural problem (like chiari or CCI) caused dysautonomia and it caused IIH. Or IIH caused dysautonomia. But dysautonomia started 7 years back and IIH one year back. Its so confusing. I am trying to find out answers. Dont know how long this journey will be. So difficult to live like this.
I like this theory!
Why no mention of Chiari and syryingomyelia causing Syrinx in the spinal canal?
Because I’m still learning 🙂 and the authors did not mention it.
My wife has NPH (normal pressure hydrocephelis)and has a Brain Shunt for this. Is it possible the shunt is not adjusted right and is causing excess pressure? She has been diagnosed with Fibromyalgia and suffers with depression, fatigue, brain-fog and headaches. I don’t think her neuro Dr. is aware of this pressure problem.
My goodness, Roy, it sounds like telling her neurologist about the NPH and shunt is really important. I believe they can adjust the amount of cerebrospinal fluid that is shunted off, and it might improve so many of the symptoms you mention that she suffers with. Best of luck with this. And bless you for taking care of your wife.
Aah life. In the last 48 hrs I have put together the pieces in my own body that this post addresses. Very happy to find this in my inbox. I am at the point of have blurred vision, pulsatile tinnitus, worst in the morning and constant dull and foggy headache that worsens when I lean over, especially in the back of my head. Hmmmm,
I am a craniosacral and lymph therapist. Lymph therapy, either manual or with a lymphstar (very cool machine) has been holding things at bay on and off for years and keeping me functional enough. Next week I will get in with a CS friend who has taken a new class on glial work.. I do believe craniosacral work, especially w an advanced practioner could be a piece of the puzzle for this. I’ll keep y’all posted.
A lot of these descriptions of symptoms are familiar to me too. Here’s the way I described my sensations to many practitioners. Like a helmet on my head, with the straps done up far too tight. Like my brain is made of lead, and suspended in hydraulic fluid at high pressure.
I am inclined to agree with the researchers observations, but disagree that they have found the original cause of FM. The dysfunctions they observe are consistent with a primary dysfunction in the fascia body-wide, leading to a vicious circle of consequences which include high spinal fluid pressure.
The way that a rare subset of FM sufferers including myself, have been able to reverse our condition, is much harder to explain with a “spinal fluid pressure first” hypothesis. It is, however, easy to explain increased spinal fluid pressure as a consequence (one among many) of body-wide fascia dysfunction.
The more I learn and the more experience I get with self-help strategies to beneficially add to my protocol, the more convinced I become. The big discovery of the last 12 months, for me, has been the effect of doing Feldenkrais “Awareness Through Movement” lessons, of which there are hundreds, designed to “re-set” the recruitment patterns of the body’s highly complex and interleaved system of muscles. If you try to study muscle diagrams, it becomes apparent that expertise in the musculoskeletal system is something that can only be gained through many years of dedicated study.
But it is sufficient for me to believe that around the body, different people have different degrees of dormancy in the use of many muscles. Sedentary lifestyles, occupational postural immobility, bad habits, etc result in many “stagnant” locations where there are muscle fibres and their fascia interleaved. This stagnation can lead to adhesions and toxicity. People with FM are extreme cases of this, throughout the body, because one or more systemic dysfunctions has heightened the adhesiveness and the toxicity throughout the body.
I have had a hypothesis for a few years to explain why my condition has improved with pacing, plenty of low intensity activity, avoidance of anaerobic exertion, massage of the Qi Gong and Fascial Release type, stretches in a spa pool, paleo diet, de-toxing and mineral balancing. Since I started doing Feldenkrais lessons, I believe that I am continually mobilising new reservoirs of toxins that were still trapped in spots where muscles were not being recruited as they should be. I get flare-ups of pain particularly in the lower legs and feet, as overall I make progress to new levels of function and fitness.
So releasing the adhesions and mobilising the toxins is a long, slow process – it is nearly 5 years for me now and I rate myself as 80% recovered. It is necessary to lay a foundation of de-toxing from the start and then stick to it patiently as one gradually achieves unsticking of fascia and the release of reservoirs of toxins at the locations of those numerous, nasty lumps, knots, corrugations etc that hands-on therapists can feel in FM patients but which are dismissed by arrogant “mainstream” research gatekeepers as “unscientific” and irrelevant.
Hi Phil – thankyou for your very detailed post with so much information. I’m interested to know more about how you’re releasing toxins? Just brief points would be useful, so I can start to try the same. Your treatment plan seems to be working really well for you and that’s fantastic news. Very best wishes, Kate
I have been co-operating with different alternative health practitioners, particularly using Hair Tissue Mineral Analysis as a diagnostic tool. There are a number of approaches to de-toxing; I have not done any of the really drastic ones like “liver cleansing”. But my HTMA results over time suggest that I am successfully detoxing purely by diet, appropriate exercise and hands-on treatment, and mineral balancing. For example, if lead and cadmium are a problem, taking large doses of sulphur helps to flush these out. There are many known “antagonist” trace minerals, sulphur has been a very important one for me. Magnesium is of major importance in everyone with FM. HTMA shows elevated Calcium and deficient Magnesium as a rule; it took me years to see Calcium down to normal levels and Magnesium up to normal levels, with large daily doses of Magnesium. Hydration is essential even to the extent of provoking frequent urination.
A paleo diet helps by minimising the intake of toxins. Avoiding anaerobic exercise minimises the toxic waste by-products of this metabolic system. Burning fat for energy rather than carbs, and remaining aerobic or below, avoids adding to the toxin load.
I do not just say I am 80% better than what I was 5 years ago, I am continuing to improve and am constantly gaining the ability to do things I have been unable to do for decades. Like: bending at the waist and touching my toes; doing a quad stretch with foot pulled up behind me; and squatting down “on my haunches”. A milestone I have nearly reached, and am working on, is the ability to “sit on my heels”. Another one I am working on, is the ability to “tumble forwards” from a sitting-on-the-floor position and rise straight to my feet. I attend regular gym classes called “Body Mechanics” as well as doing Feldenkrais “lessons” as often as I can spare the time (following online ones for myself).
Climbing stairs was agony 5 years ago and is now pain-free; the same goes for standing up out of a chair. A real difficult one is “sustaining a jog” – it is one of the paradoxes of FM that this is so disproportionately difficult compared to sustaining other forms of exertion. In the last couple of years my performance on a bicycle has risen to match that of some of the fittest people in my age group; yet trying to jog, I will mostly still collapse after 200 yards, the “energy shutdown” I experience seems to me to be similar to POTs. I have twice experienced seeming “breakthroughs” with being able to sustain a jog for more than a mile and yet these were exceptional occurrences that I cannot rely on “next time”. Something very strange is going on in my musculoskeletal system and energy metabolism! But progress is in the right direction.
This resonates for me. I was diagnosed with IIH in 2/15, and after a lot of recovery I was thankfully determined to be in remission after 2 years. Along the way I ended up with a diagnosis of fibromyalgia. I still get migraines, and if I’m ill (i.e. flu, cold) I still get intense high pressure symptoms, but for the most part I’m 75% functional. I do believe that though I am in remission from IIH, my daily pain, headaches, brain fog and other fibro symptoms are related to raised intracranial pressure in my brain and spinal cord. Thank you and best of luck to all of you who struggle!
Congratulations Sara. Did anything in particular help you out?
Hi Cort, thanks for all that you do. I credit my remission to learning g self lymphatic drainage. Of course I’ve gone down the rabbit hole with research, viral testing, genetic testing, epigenetics, supplements and diet. I’d love to recover from FM and a host of other issues I have, but at least my high pressure is under control for now
Can you tell us what treatment helped with your IIH
How does this link to Cortene?
Or rather, how can this be a result of a deregulated HPA axis?
Thanks, Cort. I have FM and don’t have many of these symptoms and am going to assume that these folks are wrong or seeing a subset of folks. I’m not signing up for a spinal tap, something on my non-bucket list. I’m going with Dr. Bruce Gillis’ s hypothesis about HPA screw ups of cytokines and chemokines and waiting for his clinical trial. One thing new hypotheses do is stimulate everyone to reinterpret them in the context of their own hypotheses since none of us really know the answer. I guess you could call that anti-confirmation bias.
The posts that interest me are the ones that mention 75% and 80% reversal or recovery. That is really all that matters as a first step. The wider picture is understanding all the root causes in specific detail, so that recovery can be made mainstream
I have been dx with ME/CFS/FM. I also had hydrocephalis (enlarged ventricles in the brain) possibly since birth according to the doctors. Several years back I started losing my balance and falling frequently; it progressed to the point where I couldn’t sit erect without support, and I had motion sickness with every move I made. Since having a vp shunt inserted nearly 4 years ago, I have got out of a nursing home and have been living independently for over 18 months. The FM pain that was severe and didn’t respond to painkillers is much reduced now as are brainfog, migraines, other headaches and the myriad other symptoms. I wouldn’t recommend a shunt as a cure, but it ties in with this theory.
What type of testing can be done to determine intracranial hypertension? Would a neuroquant MRI do the job?
A lumbar puncture is the main test that can confirm IIH but an ophthalmologist can test your eyes to see if you have papilledema (swelling and pressure on the optic nerves and discs), a neurologicist who will order a CT scan and/or an MRI to rule out other options ie a brain tumor etc and then will order a lumbar puncture to confirm. I was diagnosed with IIH in may 2017 after my optometrist referred me to the ophthalmologist to do more tests and these tests were what determined my diagnosis. x
neurologist not neurologicist. x
Hi Cort any chance of a piece on the Australian (Griffiths University) research? It seems one of the most promising CFS research streams.
Why are old studies ignored?
https://www.hindawi.com/journals/jir/2014/938576/
Sorry, meant to put a couple more:
https://www.ncbi.nlm.nih.gov/pubmed/20109177
https://www.nature.com/articles/s41598-017-11506-4
This is very interesting to me as when I had tests for multiple sclerosis in 2016 my lumbar puncture found my pressure to be very high (28.5 I believe) and the doctor who was looking at the results was of the assumption I would need it reducing every few months.
Over the next few weeks my symptoms virtually reduced to 0. I was then diagnosed with M.E and Fibromyalgia and the neurologist refused to take the advice of the administrating doctor into account, and I haven’t had an LP since, despite the positive effects it had on me. He did put me on Topiramate though for ‘migraines’ which have hardly helped, whilst the rest of my symptoms have got worse.
I have cfs/me with intra-cranial pressure, although that’s subjective – I have never had it measured. Should I ask my doctor to prescribe Diamox, and if so, what should be the dosage?
Great blog post, Cort! The link between perineural cysts and radiculopathy and FM is an interesting one. In theory, many organ systems could also be impacted, depending on where the cysts are. Since I wrote my piece on this I have since been diagnosed with perineural cysts, which are called Tarlov cysts if they are in the sacral area. Such cysts are more common in EDS.
Another interesting thing to note…some of the treatments for ME/CFS can exacerbate pseudotumors. For example, minocycline, used to treat Mycoplasma and other bacterial infections (and has neuroprotective qualities), increases CSF, which increases pressure. Many of us are prescribed florinef for POTS and low blood volume, but this drug cannot be taken with diamox according to Dr. Carroll because they have opposing actions. So it’s a bit of a messy thing if you have a mixed-disorder. He pulled me off both drugs and I will be giving diamox a try this spring.
Hi Caroline,
You and I had a little exchange following one of your own blog posts here at HR. I always find your stories and comments interesting, particularly because you and I appear to have shared a similar path through all this: Epstein-Barr, CFS/ME, POTS, lots of alternative explanations, and now EDS, possible CSF leak, etc.
Would you be interested in connecting outside of this forum? I love these forums for sharing general information about these conditions, and I’ve recently joined a local group for EDS here in Portland, which is proving helpful. But I’d love to have a way to check in with you once in awhile as well, as you progress through your search. I’m interested in how you’re continuing to make the switch from seeing yourself as a CFS-er to an EDS-er, or, if you’re like me, trying to combine both bodies of thought/research? (This is where I don’t overlap with many in the EDS groups.)
Only if you’re up for it!
You could answer me here, or look me up on Facebook. (Last name Eickmann.) 🙂
Hi MarthaLauren,
I have been on a similar path as well. Wondering if you are in Portland, Oregon. I’d love to connect with someone here in town who knows what this is like.
Hi Barb, I’m sorry – I don’t see any way to reply to your message below, so I am replying here to my own. I’m afraid you might not see it, but if you happen to, then yes, I am in Oregon, and I’d be happy to connect with you in some way. I think the easiest for you (and safest for me) might be for you to email Cort directly to get my email. (You can direct him here to let him know that I ok’d that.) Hope to speak soon!
Strangely enough, Cheney and Peterson didn’t have any FM type people in their 1985 outbreak.
When the “tender point” people came from out of town, it was quite a surprise to them.
Not like the Tahoe malady, but clearly something equally mysterious and bizarre.
Thank you once again for all you do for us Cort! Great work pulling this info together. Wow.
Cort you need to talk to Dr Pamela Cuddihy in Bolton ON ( google fibro pain clinic Bolton). She does ocular ultrasound to diagnose ICP. You don’t need a lumbar puncture or spinal tap. It’s a simple 1 min test. Almost all her FM patients have it. She has the clinical data to support it
Ha! Thanks! She’s the doctor I was referring to who is gathering data and hopes to publish a paper. I haven’t talked to her yet, though. Thanks for the reminder 🙂
Cort,
Dr. Diana Driscoll has a complex theory about the interrelationship between POTS, IIH, and EDS. She has historically focused treatment on bringing pressure down with the same drugs you list above, but more recently has come to focus on underlying causes of chronic inflammation (I believe, I find her a bit hard to follow). But her baseline theory of why the CSF is backing up and building up in pressure is an autoimmunity aimed at the drainage points lining the brain that would otherwise allow the fluid to be absorbed normally into the bloodstream.
(If you are interested in another perspective of someone with the same basic observations as Perrin, but an alternate root explanation for why the system is behaving in that way.)
Thankyou so much for all that you do for us cort, and for compiling this information.
would cranial osteopathy help this
Hi Cort,
Thanks for getting the website online again. At least over here it had very poor availability the last week. At such moments one realizes even more how much your work would be missed if too few people would help funding your site ;-). Thanks for all the good work the past years!
Being late reading this blog due to technical problems, I’ll post some early thoughts before the topic/comments “die out”.
Mechanically speaking, moderate to low blood pressure and high ICP are not the most “logical” combination. Factors that can still enable it that I can see could be:
A) brain edema or brain water retention, often caused due to brain inflammation (swelling due to inflammation).
B) poor back-flow of blood from the brain to the hart; brain edema could indicate that blood flow from the brain to the hart may be (even) more problematic then flow from hart to the brain.
C) too much CBF production
D) too few CBF removal
While this is no more then a mere rehearsal of what is in the blog, some extra information can be puled out of these IMO:
E) if the brain is long time swollen (A), then CBF volume should be automatically adapted downward by the body. Why does it not happen? Is the system broken or would it cause other problems like for example too few remaining CBF to safely protect the brain from grinding against skull and bones? This is asking if reducing ICP a lot has significant risks.
F) Woman in general are a lot more prone to edema (mainly legs, hips) then men. Could increased ICP be an expression of this too? If so, it may be the “non-gravity” variant of edema. Non-gravity as classic chronic edema is often noticed visually by swollen legs as excess water is puled down by gravity. One major force able to hold excess water on top of the body is capillary forces. This could indicate that here edema is occurring mainly at the smallest capillarities in the brain. This may also be the most vulnerable part to inflammation, hypoxia, brain-blood barrier damage due to radicals, poor blood reflow to the hart and obstruction of blood vessels due to debris like uric acid deposits.
G) Increased ICP reduces blood flow in the “classic” blood flow model: the difference between blood pressure and ICP divided by the resistance of the capillaries is proportional to blood flow (in the brain). So increased ICP would reduce brain oxygenation. Reducing it may be tempting, however if the blood flow would be hampered on the “returning to the hart” side then mechanically speaking a somewhat higher ICP may help removing pooled blood from the brain. Reducing ICP then could increase brain swelling. Complicated dilemmas.
I) https://en.wikipedia.org/wiki/Intracranial_pressure : “In patients who have high ICP due to an acute injury, it is particularly important to ensure adequate airway, breathing, and oxygenation. Inadequate blood oxygen levels (hypoxia) or excessively high carbon dioxide levels (hypercapnia) cause cerebral blood vessels to dilate, increasing the flow of blood to the brain and causing the ICP to rise.”
=> vassoconstriction and hyperventillation is common to us patients and help reduce volume of the brains by reducing total volume of the blood vessels and blood flow to the brain. Another dilemma and maybe another reason why we “must” hyperventillate (and have low blood volumes)
=> Maybe this could be the “slider” dividing a common “parent” disease into ME, FM or a mix of both. Increasing blood flow to the brain (with this same common ME/FM “parent” disease): less ME but higher ICP and hence FM. Reducing blood flow to the brain: less ICP and FM but more ME. Go for the middle ground: have some of both to a lesser extent (then when your body would set it to either FM or ME, not compared to other patients).
=> This could also explain my experience with Dixarit/Clonidine. Shortly after taking it I literally felt the pressure in my head rising. It felt like if my head was filled with blood more then ever. It even felt like my eyes would pop out of my head due to the increased pressure. My brain fog reduced a lot and really fast. Unfortunately a few days later my legs started to falter in a really big way: reduction in steps per day by a factor of ten, strongly increased pain levels and near-inability to move even if I pushed/focused really hard.
J) “Treatment for increased cerebral spinal fluid pressure usually consists of carbonic anhydrase inhibitors (such as acetazolamide (Diamox), Methazolamide (Neptazane), furosemide (Lasix) and topiramate (Topamax)) which reduce CSF levels.”
=> interesting to note that on https://en.wikipedia.org/wiki/Carbonic_anhydrase_inhibitor , medical use it states: “Carbonic anhydrase inhibitors are primarily used for the treatment of glaucoma. They may also be used to treat seizure disorder and acute mountain sickness. Because they encourage solubilization and excretion of uric acid, they can be used in the treatment of gout.”
=> So according to wikipedia, a main medical pathway is to increase excretion of uric acid. This ads to my recent idea that uric acid crystal formation may play an unexpected role in ME/FM. If interested, see https://www.healthrising.org/blog/2018/01/28/depression-fm-chronic-fatigue-anti-inflammatories/
Dejurgen; one thing I am wondering is whether the reduced gravitational flow downwards, of fluids, is simply because the fascia is not allowing as free flow of these fluids as it would be in normal healthy people.
I have been hypothesising for years that “tight fascia constricts important vessels” but I have only just woken up to the fact that the fascia itself is highly hygroscopic, and fluids “flow” THROUGH the fascia tissue itself, from cell to cell.
https://mindfulmvmnt.org/2017/03/22/fascial-fluid-dynamics/
I am more convinced than ever, that ignorance regarding the fascia, is the problem with FM “research” running down blind alleys all the time.
A mechanical pumping system requires valves to function well. The hart and some blood vessels do have these. I do not see this in the fascia.
I can however see the fascia function as a big sponge. As such it can not only hold liquids, but also transport them. Think about having a cord/threat/cotton wire… in a bottle with water on one end and above it a pot with earth and a plant drawing water from it.
Most systems I can think of this way transport water only slowly. But in some combinations it can go quit a lot quicker. Think about a big sponge laying in a pool of water on the right hand side. Squeeze the sponge and on the left hand side water will drip out of it. If nothing is underneath the sponge, that water is removed permanently from the pool. Release the sponge and new water is absorbed from the pool. Squeeze again…
The rate of squeezing (muscle action) in combination with the quality of the sponge can increase the speed of transport a lot. I call it transport rather then pumping as it goes no particular direction. I can see this speed go down if the tissue contains a high percentage of scars. Different tissue density then normal also can and will influence fluid balance and transport. The effect is hard to estimate but likely “less optimal” as our tissue is evolved to fit the purpose as good as possible.
Complex stuff that can go all ways. I see more potential in the “inelastic or lose bag” idea. Imagine a muscle inside fascia contracting. If the fascia bag is very elastic and under tension the fascia will follow the contours of the muscle well both when relaxed and contracted. If the thickness of the fascia changes when contracting the muscle then fluid will redistribute over many centimeters of distance. If however the bag is inflexible it will just bulge locally, transporting fluids over far smaller distances in most cases. The water will just go in and out the bulges staying around them locally.
Again, it can go many ways with this concept. Might help to experiment with a piece of wet meat (before baking it) and deforming it when it is wrapped in a tense elastic foil and doing the same with the piece of meat in a bag that is not under tension and made of thicker plastic. Just to visualize the idea better.
If this “transport fluids” in the fascia idea worked out, I’d imagine the fascia being both sufficiently elastic and being a tight fit around the organs in all circumstances is the key. Transporting fluids around the body may be less important then keeping fascia always in a good range of moist. If muscle action squeezes fascia locally dry (poor quality thin and overstreched fascia or local bulges for example) then it loses its lubricating action. Such would be hard to observe statically as in rest moisture would return, only friction damage would remain. That would easily lead to not seeing the connection “fascia running for a short term dry(er)” and “damage due to no lubricant” as the lubricant is available when observing it in rest. Is it clear what I mean?
Hi Phil,
in order to refine/test my ideas around blood vessels/toxins/fascia further it could help me if you could check/correct/complement the onset of your FM disease. Feel free to answer “it wasn’t like this” if you wish not to go into detail ;-).
If I recall well it was:
* During a period of relatively good (seemingly) health.
* During a period of intense (work related?) stress.
* During a period of intense sporting. Did intensity go up significantly before this period? Did type of exercises change significantly before this period?
* After a significant shift towards more muscle-building exercises (legs, all-body?). Is this correct? If so, did you eat a lot of animal protein? Did you supplemented your diet with concentrated proteins (refined, like proteins from a jar) like many sporters do? Did you eat few or much alkali food like veggies?
Thanks in advance,
dejurgen
Hi Dejurgen,
I think the way you envisage the fascia is correct, and I cannot understand why so many trained experts are not looking harder in this area for FM understanding. Schleip and colleagues are researching fascia, but focusing only on local injury / dysfunction on the one hand, and normal aging on the other.
To answer your questions:
When I first started to decline into FM symptoms, I had:
Exceptionally good (seemingly) health and fitness.
Intense work related stress.
Intense sporting activity. In my teenage years I had become more focused on academics and learning and mental recreation (chess, war-games) and was not fit. But I realised that my health was declining because of this once I started work, and took up cycling and became very fit and competitive quite quickly. Note that Schleip says that Cycling is one exercise regime that does not mobilise the fascia much.
I paid no attention to muscle-building exercises (legs, all-body?) at this time, or once I had succumbed to FM. This was something I tried after nearly 20 years with FM, on bad advice from a physiotherapist as a potential “aid” to coping with FM. It made me so much worse so rapidly, that this was part of gaining new insights about what the condition might be, and what might really help it. In principle, I had to do something “the opposite of” muscle-building, and also “the opposite of” high intensity exercise, which I also noticed was provoking long flare-ups of increased pain and immobility. “High intensity” of course, for someone with chronic long term FM, meant “trying to sustain a jog for 1 minute”. Or even trying to walk too fast up a moderate slope.
“and took up cycling and became very fit and competitive quite quickly. Note that Schleip says that Cycling is one exercise regime that does not mobilise the fascia much.
I paid no attention to muscle-building exercises (legs, all-body?) at this time, or once I had succumbed to FM.”
Would it be correct to say that during that period your muscles “changed” quickly in size/structure? I could imagine the following:
* high work related stress: highly inflammatory mainly brain but also body wide.
* if quick muscle growth or structural change (slow/fast fibers…): muscle growth/reforming is quite inflammatory locally.
* diet: unanswered question: inflammatory like most western people or high amount of meat with increased hunger going with sports and few green veggies?
* likely add hidden existing weaknesses
* now a additional ingredient: ?fast muscle growth or changes in structure? Then the growth rate of the fascia bag holding the muscle may have poorly matched the fast growth rate of the fascia bag(s). That would be a good recipe for tearing/scaring/wrinkling (clots and knots, after delayed growth of too much stretched fascia to match new muscle size and shape?) and poor lubricating function increasing the friction of scars and knots on muscle fiber and other fascia.
In the growth mismatch hypothesis I see too slow fascia growth as more likely then too fast. Fascia are like tendons. They have poor blood flow in general. Poor blood flow not only means poor repair but slow growth too. May be a poor match with your sudden change in lifestyle and male hormones that allow for fast muscle growth.
Too small fascia bags may not only overstretch them and thin them, but could also cause a “packed banana effect”. Imagine a curved banana in a too small plastic and tense bag: it’ll create a cavity on the inner radius. Compare it to muscles: it may pull them out of their correct shape (poor muscle loading, creating injury), tear the fascia from the muscle damaging both and create the cavities that allow fluid/lubricant to be squeezed far too much out of the fascia so that they lose their function.
Maybe your idea could even connect to EDS: rather than too small a bag (fascia), it’s not hard to see them too big in hyper-mobility. That’ll create a too lose bag increasing friction and leaving to much space/cavities at both ends of the muscle.
Doesn’t mean I believe FM is all fascia, but it may describe part of it to a varying degree from patient to patient.
Interesting that the drugs that successfully treat this are used for altitude sickness. My illness started when I moved to Santa Fe, NM which is at 7,200 feet (2,200 m). When I spend time at sea level my symptoms are greatly reduced.
Does anyone know the connection between heqd/brain pressure and inability to sleep when the pressure is worse the insomnia is worse. anything that will help? I also have ringing in ears , looser the head the louder the ringing.any thoughs suggestions welcome would vasodilators help?
Question for Cort: Do you know when the Dr. Ray Perrin article will be posted? He was mentioned in the 2014 article but I have not seen any additional information posted about his treatment. Thank you.
Working on it. 🙂
I’m not sure if anyone is still reading these posts, but re: sticky/tight fascia, I would like to know if many people have had accidents that may have led up to developing this problem? Personally, I had several significant accidents – horse backing riding, snow and water skiing, a few years earlier – and I can’t help but wonder if those accidents predisposed me to developing fascia problems. I was always athletic, and was running, biking, skiing, etc. when I got FM/ME/CFS, but I started having difficulty with all movement and I’m thinking that tight fascia is the common denominator.
This a vary interesting article and your proposed correlations are certainly sensible and worthy of review. I would like to add another condition which seems to correlate as well. Your article could well to some people with certain connective tissue disorders. An example is Ehlers Danlos Syndrome, particularly the hypermobility type, once known as type three. A new nosology was published in 2017 by an international team, who continue to work together to update the nosology as new findings are made. What was once a condition considered to be beneficial if one had an interest in ballet or becoming a contortionist— today it’s recognized as potentially very disabling, often with intractable pain, some who have it also suffer with Chiari Malformation as well as spinal fluid buildup at the base of the skull. There are many crossovers in this article and as such I felt it relevant to share this as it is now understood EDS is not to rare, though it has some serious implications. Many living with it have been diagnosed with fibromyalgia, although many with hypermobility type eds also have fibromyalgia. While that certainly doesn’t mean many with fibromyalgia have EDS, it’s become recognized that there are in fact many who present with fibromyalgia or chronic fatigue type symptoms who also present with hypermobility and as such ought to be getting assessed by a geneticist for Ehlers Danlos Syndrome considering its potential health implications for them as well as potentially for their generic relatives, and the fact that many serious problems can ideally be avoided if one is diagnosed and then monitored for signs of potential concerns. Thank you for a thoughtful and insightful article. I hope to see some follow up studies to further investigate the well founded ideas proposed.
Thanks Pola for sharing that. We will certainly be hearing more and more about EDS as it becomes more recognized and the research proceeds. I will be on the lookout for EDS research 🙂
Great blog on fibromyalgia. As a licensed massage therapist this helps me to understand people Better who live in this condition. I know personally that massages could help alot of these people suffering. Maybe you can do a study on that? I would be interested to hear your findings. Thankyou! ?
Thanks for the insights Cort. I’m newly dx’d w hEDS and IIH experiencing wicked fatigue, head pressure (worse in morning/night), orthostatic intolerance, brutal tinnitus and low back pain. I’m in Chicago, struggling to find any local docs to help. My imaging/tests look normal but I feel like I am dying. The fatigue and bone pain is rough. Trying to learn more so I can continue to advocate on my own behalf. Traditional medicine is leaving me hanging…wanted my comments to be part of this thread so I can be privy to relevant updates and/or any studies that come along. Thanks!
Good luck Melissa.
Please check out cerebral spinal fluids on HR as well.
Melissa my daughter goers to college in Chicago. She sees dr Barboi in Evanston for her POTS he is seriously smart and spends a lot of time in the initial visit. He has helped my daughter a lot.
https://www.healthgrades.com/physician/dr-alexandru-barboi-3f8rx
It’s crazy that you all lump POTS in this. All four of my kids have dysautonomia one is POTS level. I developed FM after a car accident and subsequent ACDF
Do any of you know of a forum for those with fibro and Intracranial Hypertension for a younger subset? My daughter is looking for more of a support group of like people that she can speak with that have her symptoms and since this is such a technical medical forum it would not quite fit the needs that she is looking for since it is so technical in nature. She is in her 20’s with both diagnosed. Thanks to all in advance, I love reading your data it is fascinating!
Hey There,
I can’t seem to find Pt. II – Ray Perrin – Reduced Lymphatic Drainage in ME/CFS/FM anywhere on the website despite using all search terms.
Was it published? Very keen to read.
Thanks.
I have been diagnosed with Fibro and I believe I have EDS but I cant find any Dr. in my state to test for it. I also have spinal issues, most notably a Thoracic Syrinx. No one is saying it but I think the Syrinx is causing my Fibro. I would love if anyone has research into this I can read.