

Opioid Painkiller Crackdown
The news regarding opioids has been mostly bad for fibromyalgia (FM) and chronic fatigue syndrome (ME/CFS) patients. Restrictions on opioid pain killers could put these medications at risk for FM patients battling one of the most painful diseases known. Surveys suggest that opioid painkillers are more commonly used than the three FDA approved drugs for FM and may be more effective.
In a recent interview, Dr. Lapp, an ME/CFS/FM practitioner with decades of experience under his belt (now retired), expressed the frustration that he as a doctor caring for FM and ME/CFS patients has experienced at the possibility of these drugs being excluded.
Shame, shame on the critics who state that opioids should never be prescribed to persons with FM or ME/CFS. They should suffer this kind of pain for just a day or two! Based on little evidence, mostly in laboratory animals, they predict that opioids should not be useful in PWCs. However, survey after survey of patients with fibropain list opioids at the top of the list as most effective for pain relief. Why ignore the real life data?!
And why make people suffer based on theoretical data? I agree that opioids should be avoided whenever possible, but not excluded if needed.
The CDC’s recent announcement that it may have greatly overstated overdoses caused by opioid painkillers is probably too little and too late to reign in the opioid frenzy that has gripped the medical community.
Silver Lining
There may be a silver lining to the opioid crackdown, though. The NIH’s announcement of its Heal Initiative (Helping to End Addiction Long-term) on April 4th promises something that fibromyalgia and ME/CFS patients greatly need – more funding for pain research. The Initiative will almost double funding on opioid misuse and pain from 600 million dollars to $1.1 billion a year.
(Rejecting the Trump administration’s attempt to cut NIH funding by 22%, Congress instead increased the NIH budget by a cool $3 billon (8.3% increase) and used part of the money to pay for the Heal Initiative.)
No studies that I know of have assessed opioid addiction rates in fibromyalgia, but given the light opioid typically used (Tramadol), my guess is that they’re not particularly high. That makes half of the HEAL Initiative, which is focused on understanding who is most vulnerable to addiction and figuring out how best to treat it, not particularly exciting.
It’s About Time
The other half of the HEAL Initiative, however, which is devoted to developing new pain treatments, is tremendously exciting. Why it took an epidemic of opioid-related deaths – most of which are probably due to illegal drug use – to finally move the NIH to tackle the immense problem of chronic pain is unclear.
An Institute of Medicine report about ten years ago forced the NIH to recognize that it was vastly underspending on chronic pain, but this is the first major effort I know of that is specifically and strategically targeted at producing new treatments for chronic pain.
The HEAL Initiative will fund efforts in several areas that might benefit FM and ME/CFS research efforts.
Uncovering How Chronic Pain Starts – the Biomarker Discovery Study
The NIH will launch a longitudinal study that will identify biomarkers that help explain and predict why some people develop chronic pain after an injury or other event while others recover. Several studies have already identified brain changes that occur in the early stages of a pain event that seem to predispose some people to developing chronic pain.
This project could provide key insights into fibromyalgia. Studies indicate that FM is a common end point for people in pain: a significant subset of people with any pain condition will at some point come down with fibromyalgia. Hopefully the NIH will put aside its decades of neglect of fibromyalgia and use this new effort to specifically examine how pain in one spot transitions into body-wide pain plus issues with sleep, fatigue, cognitive function, stimuli sensitivity, etc. Even if it doesn’t, understanding how the transition from acute to chronic pain occurs would undoubtedly be helpful for our understanding of FM.
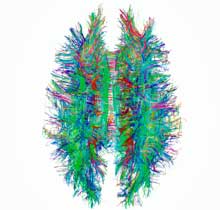
Cutting Edge Brain and Nervous System Technologies Emphasized
The NIH’s new focus on the brain in the HEAL Initiative and the 2013 Brain Initiative can only be helpful for FM and ME/CFS. For one, expect new scanning techniques to come on the scene which allow researchers to assess what is occurring in the brain in much finer detail. At the same time, the SPARC program sparks new insights into how the peripheral nervous system (the system that transmits pain signals to the brain) works, and how to tweak it to reduce those signals.
Private-Public Partnerships to Develop New Pain Drugs
The NIH will use private-public partnerships to share data and spark new insights into the development of new pain drugs. It will also be digging deep into pharma’s enormous portfolio of “potentially promising but abandoned” drug compounds that never made it to market to develop new non-addictive pain medicines.
Faster, More Effective Drug Testing
Finally, the NIH is going to tackle an enormous problem – the complexity and expense of drug testing – by creating a new clinical trials network which will speed up the testing of compounds. The NIH asserts that this new network will allow weaker compounds to get weeded out more quickly and better compounds to move to more extensive testing more efficiently. It states that a more “flexible clinical trials network will significantly accelerate the development of effective therapies.” If the drug testing regimen in this country needs anything, it needs more flexibility; let’s hope this new effort works and becomes a model for other kinds of drug testing.
The Cannabis Question
But what about perhaps the most effective pain reliever available? The National Pain Report’s fibromyalgia treatment surveys suggest that cannabis is far and away the most effective treatment for pain in FM. Another survey put fibromyalgia at the top of the list of diseases which were most improved by the use of medical marijuana.
The DEA continues its bizarre practice of classifying cannabis as a schedule 1 substance, which, along with heroin, LSD, mescaline and ecstasy, has a high potential for abuse and no medical benefits. The DEA asserts, rather remarkably, that marijuana has a higher potential for abuse than cocaine, methamphetamines and oxycodone – all of which, according to the Harvard Political Review (HPR), have less restrictive classifications.
Recently, the FDA opened the doors to more medical research, but cannabis’s designation as a federally outlawed substance, the HRP reports, “makes clinical trials extremely difficult, if not impossible to conduct”. The HRP outlined the decade-long effort of a University of Mass. researcher to build a medical marijuana research facility.
President Trump stated he was “100%” behind medical marijuana” during his campaign, but his attorney general Jeff Sessions recently rescinded the Cole memo which basically told the states that the feds would back off on medical marijuana prosecutions so long as the states obeyed certain guidelines. After the DEA, in a change of pace, agreed to allow new facilities to grow cannabis for medical research (only one does so now), it received 26 applications from growers. Sessions then canceled the initiative insuring that only small quantities of cannabis will be available to researchers. Likewise, the Dept. of Veteran Affairs recently announced that it would not fund any cannabis studies to treat pain or other conditions.
This is despite the fact that polls suggest that 94% of Americans support medical marijuana legalization and 64% support outright legalization of the plant. Meanwhile, Big Pharma – which stands to lose big time from cannabis legalization -contributes large amounts of money to anti-cannabis campaigns.
Most cannabis research (70% of the top 50 studies) focuses on potentially negative outcomes of cannabis use, but some trials on neuropathic pain, cancer, chronic pain, low back pain, epilepsy, etc. are proceeding.
Conclusion
Six hundred million more dollars a year into pain and opioid research is a lot of change. Even if FM is not specifically studied, it’s hard to imagine that patients with this “quintessential pain disorder” will not at some point benefit dramatically from the insights gained.
The new techniques developed to study how the brain and peripheral nervous systems work will obviously allow FM researchers to better understand this complex disease.
A new or a couple of new classes of pain drugs that work more effectively and have fewer side effects would be a huge help. A drug doesn’t need, after all, to be created specifically for a disease for it to work effectively. Many people with FM benefit from opioids – a class of drugs which animal studies suggest should not work in FM – but which obviously does.
The Trump administration has put more barriers in the way of more cannabis research, but some clinical studies are underway.







I wrote a lengthy comment. It disappeared after I provided the requested info and hit submit.
I really apologize Alice. I know what its like to lose good work like that. I hope you can gather yourself at some point and do it again. I’d like to hear what you have to say.
If you’d like to email me it I can make sure that it gets in there safely.
I find it best to write the comment in pages or word and then copy and paste it into the reply. That way if it gets lost in the system, you still have a copy.
I use email drafts in the same way after being burned (and burned up) one too many times. Type it there, where it is saved in the draft folder if you make a boo-boo, and when all done drafting and proofing then copy and paste the finished product into the website on which you are communicating your thoughts.
As a 23 year patient of FM/CFS/ME,I will tell you the opioids are the best reliever of pain for me. I am not addicted,but dependent on these drugs. I also took all 3 drugs for FM/CFS/ME. Did not help & had horrid side effects! I hate that the government has required the PM doctors to allow their patients opioids OR benzos. We have pain & high anxiety! Not fair to patients who have a long record of being responsible!!!Looking forward to new research!
Let’s hope we get safe and more effective drugs from it. In the National Pain Report’s survey opioid pain killers were the second most effective drugs for FM patients. They did far better than the big 3 overall.
I was a patient of Dr. Lapp, and am still at his practice. He is an amazing doctor in his field. I have ME/CFS/FM as well as other chronic illnesses including a rare disease called Behcets. It causes awful skin ulcer flares, and even when some doctors can visually see the source of my pain, they are not willing to prescribe narcotics. It is truly unfair to people who take these meds as prescribed and for severe pain, that addicts are ultimately deciding our medical rights.
I’ve reduced my opioid pain med due to the hurdles we were forced to jump over. First of all you cannot get a refill without seeing a Dr. How many of us miss appointments because we to sick to get out of bed? So missing one appt & having to wait 30 days for the next one I had to stretch my 30 day Rx to 60 days. The Dr said “since to already lower the dose on your own do you want to deduce your dosage?” I said yes even through I have more pain, spend much more time using heat or cold therapy I felt like it was worth it. Of course months later I missed another appt and was going through some extreme personal problems & forgot to reschedule the appt. my 30 day Rx had to be stretched to 90 days. What is the point of the warning label “do not stop taking this medicine” if you can’t get a refill? The opioid hype was the biggest insult, plus not accurate for people with chronic pain. It was and is beyond cruel in my opinion. People are left with very little choices to manage chronic pain. The comment made by Jeff Sessions “take 2 Bufferin” had me crazed with anger. Bufferin? Do they even make it anymore?
I absolutely agree that anxiety and pain quite frequently go together….I just spoke with my brother tonight about that. I have been ill for thirty years and at least years ago it was easier to be treated with pain pills and benzo’s when necessary but now it’s horrible. One has to choose which is worse? I think that the two work in tandem at times when one has to do things that are very difficult and of course for sleep. My doctors are no longer prescribing for sleep. So we have to choose what is bothering us the most and quality of life is no longer an option; it’s now all about survival. I just wish that doctors could live our lives for just a day or two.
I’m a 34 year old Fibromyalgia sufferer and I can agree with you on pain medicine. The 3 Fibro drugs did nothing for me!
You are not alone at all. I think most people are in your boat. Here’s to better things.
blew out my brain fog and increased my energy tremendously.
Two years into Methadone I tried Ketamine infusions. I knew I needed an anti-inflammatory. Being on blood thinners made this nearly impossible. Ketamine took my inflammation down in a miraculous way. My pain was greatly diminished and my energy soared.
I was able to get two separate rounds of Ketamine. Each time I received great benefit. Unfortunately insurance does not cover these infusions and they are quite expensive. I really could use another round, but can’t afford it.
I really wish more research would be done on Ketamine as a chronic pain reliever. I’m experiencing so much pain again and it really angers me that there is something that helps me, but I can’t afford it.
Thanks for this encouraging post Cort.
Wow, I posted the comment above but the entire first part was deleted. I talked about Methadone. I’ve been on a very low dose of 15 mgs for 4 years and it’s helped tremendously. Not as you would expect though. I got relief mostly from brain fog and fatigue.
I’ve
never heard of methadone as an option. It would be amazing to have decreased brain fog and increased energy! Is there any good documentation on this for my doctor to see? Thank you, and so glad you’ve found something that helps you!
Hi Lorraine
I just came across your post and its the first time I have heard anyone a part form myself getting relief from fog and fatigue with narcotics..
I had been put into hospital in Jan 1999 (6 months after a car accident … neck injury and consequent diagnosis of Fibromyalgia.
I was hospitalised as I had lost nearly half my body weight from terrible vomiting constipation and diarrhoea .. that terrible IBS!
I could not tolerate oral medications and as a last resort was tried on this new Patch (new back then) It was Fentanyl..
I have never felt like I was on any medication at all let alone a narcotic and often wondered whether I was given a placebo….
But my pain lessened … it became bearable and something happened that had never happened with any of the other medications was that many of the symptoms went like the itchiness, I could wear clothes without having to rip them off because of the weight of them or the feel. The sweating was much less and I was not so sensitive to smell light or noise but the fatigue was much less and my specialist often told me he thought my fatigue was part of my pain cycle. The brain fog was not as bad and I could do more mentally.
I understand that what works for me may not work for you at all or in the same way but no option should ever be removed based on fear mongering trying to solve issues that do not pertain to us…
On a bad day I am still bed bound but my quality of life has been lifted to what it was without the patches. If my dose is dropped or I miss a dose my symptoms return to full power like they were when first diagnosed.
I live in daily fear that some doctor or govt decision will reduce or even worse remove my dose of Narcotic…
Life is a hard one to live on any day so don’t remove the only treatment that has ever worked…. & I have tried everything.
I am encouraged to see researchers becoming interested in why “some people with an injury go on to contract FM while other people do not”. I strongly believe they need to look for multiple pre-disposing factors. If there is “one” factor that is “the” common one, it is probably genetic. But everyone who gets FM, seems to have had multiple provocations that coincided, possibly very unluckily (or maybe they wouldn’t have got FM).
Re the potential represented by “natural substances” for pain relief, I used to be skeptical about “conspiracy theories about capitalists” but after decades of experience I am prepared to believe that there are many policy areas where government is being perverted by vested interests perpetuating the opportunity to make undeserved profits. When it comes to drugs versus natural substances, if something is effective but cannot be patented and earn somebody profits, it will be dishonestly suppressed for as long as possible. Even Congressman Trey Gowdy, a genuine Conservative, recently grilled the classifying authorities on Marijuana, in Committee.
It is very worrying to learn from this article (thank you Cort), that even authoritative research into Marijuana so as to be able to derive safe medicinal extracts, is being hampered by the perversely draconian regulations. I am a law-abiding Conservative guy myself and have never touched Marijuana or anything like it, but I am in the process of being alienated by corruption in government which is supposed to be “representing my interests”. “Protecting me” should include protecting me from evil profiteering capitalists, and letting technology, research and free markets provide the benefits they can. Government should not be suppressing potentially massive benefits for society so as to protect the profiteering of people in the one percent.
Maybe we need to get into the activism de jour mode and do a march on Washington DC, using some slogan like “Painful Lives Matter, Too” or “Opioids Save Lives, Too”
Would be pretty dramatic to see thousands of chronic pain sufferers in wheelchairs, using walkers, lying on wheeled cots wheels and being pushed or pulled, etc., outside regulatory and legislative office buildings and right up to Capitol Hill.
Yes!
I think your idea is wonderful!
Great article Cort, thank you. I have been on LDN (low dose naltrexone) for the past three years and it has helped with fibromyalgia pain but not fatigue. Just recently I stopped the LDN because I needed a narcotic for acute neck pain (my neck’s a mess!) and I have seen a huge increase in energy level. For the first time in years I’m doing things again. We’ll see if the opioids continue to help. I hope so and I’m excited about research for a new pain medicine. Too bad the medical marijuana isn’t available for me…. maybe one day…..
Screw you people. I have legally been using Opioids for back pain for over 20 years (with NO addiction problem) but since I changed from my first Pain Management M.D., the three since have all wanted the amount CUT (so the Oxycodone DOES NOT WORK AS WELL! And YOU KNOW WHO YOU ARE, SANTA MONICA DOCTORS!) Thank GOD for Cannabis. I have been using that DAILY since the early 1970s, and it does indeed provide some relief for my chronic back pain. My Primary M.D. had just put me on one of the new Migraine Prophylactic injectables, which I have just started today, so it’s too soon to see how it may work. but up to now my migraines have been TERRIBLE!!
I have been suffering for YEARS! Chronic Fatigue, which my Brilliant M.D. tried one of the first Biologics for, once a week in each leg FOR A YEAR, and it’s almost completely gone! My back pain, which I’ve had for DECADES, was helped by Cannabis, starting in the early 1970s through now, and my first Pain Management M.D. put me on a cocktail of Opioids which worked VERY well. But the two Pain doctors I’ve had to see since him have only wanted to reduce the dosage! Is that STUPIDITY? Then there are my Migraines, which NOTHING helped until there were things like Sumatriptan. I use that now, but my Brilliant M.D. is starting me on one of the new prophylactic Migraine injectables. I’m just starting them today, so I can’t yet comment on them. I hope they work because at the moment I suffer from DAILY, debilitating migraines.
Good luck!
I live in the UK and have been in Oxycodone ER for 2 years in and off, Jon stop now for a year. I switched to the IR 6 months ago. I have had multiple spinal surgeries, severe Osteoarthritis and developed Fibro, after the 1st surgery.
If it wasn’t for Oxy, I’d have thrown myself off a bridge by now. Reduced fatigue, less pain, it’s been a lifesaver. But, I’m clucking with withdrawals even if I’m later then 1/2 hour with my doses. Plus cannot sleep through without taking one.
Hormones have been a godsend too, testosterone, oestrogen and progesterone.
I managed to quit Citalopram too.
I feel for anyone in the US being restricted, it’s cruel. It’s an insidious condition, I wouldn’t wish it on anyone.
I contracted CFS/ME on 3/21/86. I know this date well because it was the second week of my honeymoon when I landed in St. Thomas. The next 7 years were hell with severe flu-like symptoms without a 5 minute break. I was a programmer at Honeywell in Arizona at the time and they did everything they could to get me fired, thinking I was on drugs. I took every medical test possible from Cigna Health and all came back negative. One doctor at a private clinic experimented on me by giving me gamma globulin shots for a few months. It was the only thing that took away the flu like symptoms. I have told every doctor since but they just shrug it off and never have looked into it. I thought if I could get a few more injections maybe it would be gone. But I will never get the chance.
It has been downhill ever since. I was an athlete in multiple sports. At my peak I attained computer certifications that fewer than 100 people in the world had (MBA, MCSE, MCNA, MCSA, MCNPS, MCNE, ECNE, CNE, MCPS, NETB, NSA, CCENT, CCNA). But I could not be consistent because as I went from doctor to doctor, they would cut me off the opioids, I would miss work or look terrible or go back into the brain fog, and that was the end of that job. I have lost my house, family, reputation, everything. I now live in poverty and was forced to work for myself.
My current doctor (I will provide her name to anyone interested) absolutely will not budge. No pain relief. She has no knowledge of the disease coupled with the typical doctor God complex. She is the fifth doctor I have tried on the Oregon Health Plan and I have to give up. I am trying to find an attorney now that will work on contingency.
Opioids gave me my life back. I was able to get out of bed, the brain fog would clear a bit and I could work. It is so unfortunate that illegal drug use has caused such a crack down on legal responsible use. I am in hell now seeing all my effort as a young man wasted because of this disease. I am facing homelessness and struggling to stay where I am. And the pain is driving me to wonder if this life is worth it anymore.