Hormones?
Certainly the nervous system plays a major role in producing pain. The immune system with its inflammatory processes and ability to create sickness behavior is certainly in the discussion, but hormones? Many women are well aware that hormonal fluctuations can boost pain levels, but could the sex hormones play a role in the genesis of the pain women and men with fibromyalgia experience?
It turns out that the evidence rather strongly suggests that they might. A major gender gap in the incidence of both fibromyalgia and chronic fatigue syndrome (ME/CFS) suggests that sex hormones must play at least something of a role in these diseases. Animal studies indicate not only that females are more sensitive to pain but also that that sensitivity can be altered by changing their hormone levels.
The fact that that gender gap appears only when girls reach puberty strongly suggests something’s up with the hormones in fibromyalgia. Reports abound of improved pain and fatigue during pregnancy for some women with ME/CFS/FM. Plus several studies indicate greatly increased rates of gynecological disorders in ME/CFS.
Studies indicate that sex hormones affect the activity of pain receptors, the central pain-processing pathway in the brain, inflammation in the spinal cord, the microglia in the brain and opioid pain processing. Two sex hormones in particular – testosterone and progesterone – appear to have pain diminishing properties, and progesterone has anti-inflammatory and neuroprotective effects as well.
Given the abundant evidence indicating that sex hormones can indeed affect pain, it was no surprise to see Jarred Younger at the University of Alabama at Birmingham publish on this subject. His recently published study was small but intense. The fact that only eight FM patients participated in the study means we can’t know if their results apply to the FM population as a whole, but that wasn’t the point of the study. The point was to generate enough exciting data to get the next, bigger study funded, and in that Younger surely succeeded.
Younger belongs to a newer generation of researchers and he’s doing different kinds of studies. Instead of taking one measurement and hoping it reflects what’s going on in the body over time, Younger has taken people with ME/CFS or FM and tested them every day for almost a month.
Then he’s correlated their biological data with their symptom data in order to try to understand what’s going right when they’re feeling better, and what’s going wrong when they’re feeling worse. The daily blood draw studies clearly take a lot from both the participants and the staff (no weekends off) but the results have been fascinating. Immune factors, for instance, have popped out which nobody expected to pop out.
The Study
In this study Younger measured testosterone, progesterone and estradiol levels as well as cortisol in 8 women with FM for 25 days straight while having them record their pain levels. He found that both progesterone and testosterone were inversely correlated with pain levels; that is, the higher the FM patients’ progesterone and testosterone levels were the lower their pain was.
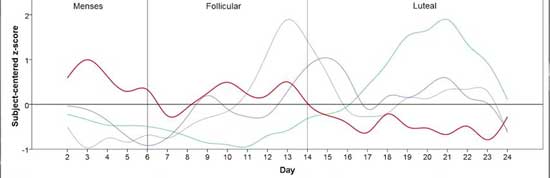
The green line is progesterone (highest in the luteal phase); the red line is pain. Note how they diverge in these fibromyalgia patients.
Progesterone level fluctuations by themselves altered pain levels by about 25%. By themselves, neither estradiol or cortisol levels had any effect on pain except when progesterone levels were low. Low progesterone in combination with high cortisol produced the highest pain levels. Women will probably not be surprised to hear that pain levels were highest during the menstrual period when sex hormone levels were at their lowest.
Younger noted that this was the first time pain levels and sex hormone levels had ever been tracked on a day-to-day basis in humans, but a very large (@10,000 person study) also found that lowered sex hormone levels (estrogen, testosterone, androstenedione, and 17-hydroxyprogesterone) were associated with an increased prevalence of chronic muscoskeletal pain.
The Stress Pain Connection
What exactly is going on is still a mystery, but some hypotheses exist. Progesterone could be tamping down inflammation or modulating nervous system activity.
Hillary White, PhD notes that stressful situations usually reduce pain levels but that the opposite tends to occur in FM. Pain levels in the body are reduced during stressful situations when a neuropeptide called substance P converts testosterone to estradiol.
Estradiol then upregulates the production of the endogenous (self-produced) opioids which cause pain relief. She believes the lower testosterone levels found in FM (and other pain disorders) prevent this inhibitory pain network from functioning properly. Once that inhibitory pain network goes off the rails, pain sensitivity spikes higher and higher, and instead of stress reducing pain, it provokes it.
The cortisol/progesterone interaction Younger found suggested that high stress (high cortisol) combined with low progesterone was a recipe for more pain in FM. White is not the first to propose that stress enhances pain in FM. Dr. Martinez-Lavin proposes the same thing in his book “Fibromyalgia: When Stress Becomes Real Pain and What to Do About It”. Eighty percent of the FM/ME/CFS patients taking the poll (which is still open) on the blog strongly agreed with the statement “I notice that stress is associated with pain or discomfort”.
Other studies suggest that when estradiol levels are low, higher testosterone levels are needed to engage the inhibitory pain pathways. The study suggested that taking oral contraceptives or hormone replacement therapy may indeed affect pain levels in FM. In his video, Younger noted that men with higher testosterone levels are less likely to come down with fibromyalgia.
The Bigger Picture
The cortisol/progesterone interaction Younger found was fascinating and significant, but Younger believes many more factors probably come into play. He wondered what a study exploring adrenal and thyroid hormone levels, neuropeptides, neurotransmitters, cytokines, and other factors might find and even suggested that “an optimized set of analytes could predict most pain fluctuations in fibromyalgia.”
Finding out what blend of hormones, neurotransmitters, cytokines, etc. are setting off the pain signals in FM and ME/CFS would, of course, be a huge step forward. Since the body is essentially a set of complex networks which interact with each other, the only way to truly get at the changes that occur is to assess what’s happening in those networks. Younger clearly wants a chance at doing that.
It wasn’t so long ago that we simply didn’t have the computer capacity or statistical methods to do such data intensive studies. The one-off studies which use one data point to try to understand a massively complex body that is changing over time still have their place, but more and more studies which intensively sample patients over time to try and get a grasp of the mechanics behind illness are getting underway.
Dr. Klimas’s intensive sampling regimen during and after exercise is uncovering why exercise is so difficult in ME/CFS and Gulf War Illness. Dr. Systrom is doing a similar protocol using invasive CPETs in ME/CFS. Dr. Lipkin and Dr. Hornig are assessing immune factors over a year in ME/CFS. Lenny Jason is tracking what happens to college students after infectious mononucleosis as some come down with chronic fatigue syndrome (ME/CFS).
The New Normal?
Even though sex hormones appear to play a significant role in producing pain in FM, the levels of these hormones in FM patients were actually “normal”. Perhaps it’s time to redefine what normal is in the context of illness. The research in FM, POTS, ME/CFS and Alzheimer’s suggests that “normal” levels of sex hormones, iron, leptin, cytokines and other factors may not be so normal after all. Cytokine levels were “normal” in the Montoya/Davis immune study which nevertheless strongly implicated them in fatigue severity in ME/CFS.
These findings suggest that when a different biological context such as a disease is present, the rules of normality no longer may apply. A factor which appears to be within the normal range may, in these changed systems, be having unanticipated effects. Within the context of fibromyalgia, “normal” levels of progesterone and testosterone may actually be too low. Higher, but still normal, levels of cortisol in combination with low, but normal, levels of progesterone may cause pain levels to shoot up. Dale Bredesen’s functional medicine approach to Alzheimer’s seeks to create optimal instead of normal levels of many nutrients and metabolic factors.
In two studies, Hillary White PhD used testosterone gel to successfully reduce pain in fibromyalgia. Her testing revealed that blood testosterone levels of the women entering the study were in the lower half of the normal reference range for their ages. Using the gel normalized, and slightly increased, their testosterone levels to just above the reference range. (The gel does not appear to be FDA-approved.)
A third of the women reported a 50%, or greater, decrease in pain. Forty-two percent were reported to have a 33%, or greater, decrease in pain. Tender point sensitivity was significantly reduced. Libido was significantly increased. The treatment had no effect, though, on headache severity, sleep, anxiety or depression. White also found reductions in fatigue and has proposed that her testosterone gel can help with the intractable kind of fatigue found in chronic fatigue syndrome (ME/CFS).
Tricky Treatments
Hormones are tricky. Doctors prescribed progesterone/estrogen in post-menopausal women for years thinking it protected them from heart disease only to have a very large study indicate that it actually increased their risk of blood clots and strokes and had no positive effects on heart disease. Since then further studies indicate that synthetic progesterone/estrogen is generally effective and safe for women younger than 60 or within 10 years of menopause while women over 60 or over 10 years after menopause may face more problems. A doctor’s advice is crucial in making a decision in this complex subject.
Seeking to get a boost, healthy middle-aged and older men have been downing testosterone in the billions of pills. Testosterone supplementation, though, doubled the risk of heart attacks in older men and tripled it in middle-aged men with prior heart problems. Some trials have not found increased risk, but like other hormones, once you get on testosterone, it may not be possible to get off. That said, for people with low hormone levels, hormone supplementation can be quite helpful.
White reported that the American Society for Reproductive Medicine’s Princeton Consensus Statement recommends treating women with gonadal hormones if clinical symptoms such as diminished sense of well-being and chronic fatigue are present. The North American Menopause Society recommends treatment with gels or creams (not pills) for symptoms of decreased sexual desire, if blood monitoring is done. Several alternative MD’s report using testosterone successfully in some of their FM and ME/CFS patients. Kent Holtorf’s 2009 review asserts bioidentical are safer and more effective than synthetic hormones. Several medical societies caution against using them.
Fibromyalgia, like ME/CFS, might very well be cured by using multiple factors that edge the system back to normal. The good news about both FM and ME/CFS is that, aside from small nerve fiber problems – which may be able to be ameliorated – evidence of tissue destruction is rare. Hopefully, Younger’s study is one step on the path to understanding the multitude of factors that result in FM and finding the right combination of treatments to set them right.
Jarred Younger on the Study







Makes sense. My CFS was so much better when I was pregnant
“Doctors prescribed progesterone/estrogen… …only to have a large study indicate that it actually increased their risk of blood clots and strokes”
Immunothrombosis is the improvement of immunity strength through locally increasing thrombosis in the small capillarities. It works by trapping pathogens and keeping them local, preventing them from spreading throughout the body and allowing to concentrate immune cells around the trapped pathogen. See https://en.wikipedia.org/wiki/Intravascular_immunology under the section immunothrombosis. Downside is increased risk of thrombosis.
Better pathogen fighting and thus less pathogens may lead to less inflammation as in “Progesterone could be tamping down inflammation or modulating nervous system activity.” Less pathogens sounds nice for ME even more.
From my research, this statement is definitely NOT TRUE, and refers to the old testing using premarin (horse derived estrogen) and progestin (synthetic progesterone)…
“Hormones are tricky. Doctors prescribed progesterone/estrogen in post menopausal women for years thinking it protected them from heart disease only to have a large study indicate that it actually increased their risk of blood clots and strokes and had no positive effects on heart disease.”
This is a common misperception. Actually using bio-identical hormone replacement DOES have protective effects for the heart, brain and many tissues. I wish this was not still touted as it was related to a study done so many years ago with a limited study group.
Thanks Fiona for prompting me to dig deeper. 🙂 I’ve amended the blog to incorporate what I learned.
I looked up more on the Women’s Health Initiative study. A 2013 study by Manson (https://www.whi.org/SitePages/WHI%20Hormone%20Trial%20Findings%20Questions%20and%20Answers.aspx) reviewed the results from the over 100 studies (!) which came out of the WHI project which followed 27,000 women (!) over 13 years. (Now that’s a research project!).
In general it concluded that except for hip fracture the combination estrogen – progestin was not helpful but that estrogen alone was generally helpful.
Estrogen-plus-progestin increased the global index of combined illness and death by 12% during the treatment period. Estrogen-alone had no effect on overall illness and death, although risk was reduced for women in their 50s and increased for women in their 70s. After stopping, there were no hormone effects in either trial.
Estrogen-plus-progestin increased coronary heart disease risk by 80% during the first year but only by 18% over the entire treatment period; this risk did not differ by age.
The authors concluded that in general the combination therapy was not recommended for long term use but could helpful when used in the short term particularly for women entering menopause. (https://www.npr.org/sections/health-shots/2013/10/04/229171477/the-last-word-on-hormone-therapy-from-the-womens-health-initiative) It should be noted though that the increased risk was generally quite small overall – just 19 extra cases of coronary heart disease for women over 70 in the 10,000 person cohort.
Breast Cancer: Estrogen-plus-progestin progressively increased breast cancer risk to 24% over the entire treatment period, with cancers diagnosed at a more advanced stage. This risk remained elevated over the total follow-up time of 13 years. Estrogen-alone decreased breast cancer risk, an effect that became statistically significant over the total follow-up time of 13 years.
Stroke and Blood Clots: Both estrogen-plus-progestin and estrogen-alone increased stroke risk by about one-third during the treatment period. These regimens also increased the risk of blood clots in the legs or lung, although this effect was greater for estrogen-plus-progestin than for estrogen-alone. The increased risks of stroke and blood clots were not seen after women stopped treatment and did not differ by age group.
Hip Fracture: Both estrogen-plus-progestin and estrogen-alone decreased hip fracture risk by 33% during the treatment period. After stopping, this risk slowly increased, but was still lower in women who had taken estrogen-plus-progestin and similar in women who had taken estrogen-alone.
This study was done on oral contraceptives which require higher doses than done with gels or creams.
A recent study found that women with low hormone levels do not have the side effects of those with normal hormone levels and can benefit greatly. – http://www.latimes.com/science/sciencenow/la-sci-sn-hormone-therapy-safe-20170912-story.html
The North American Menopause Society states that hormone therapy appears to work well for many women who are within 10 years of menopause or are younger than 60. It’s less sanguine about women 10-20 years after menopause or who are older than 60. That said some women may still benefit. It’s a risk/benefit analysis.
I couldn’t find the bioidentical hormone study. I’m sure its there but I just couldn’t readily find it but I did provide a link to Kent Holtorf’s bioidentical review study.
It’s clearly a complex subject!
Was very helpful to me. My hormones are really messed up fromFibromyalgia chronic. Had about 38 yrs. 77 yrs old. I was low in estrogen test was only 3 normal is 80 my Dr. said.My tester one was very very high having hot flashes, my breast swell don’t go down. My pelvis cramps and the clitoris is spastic very painful my left ovary is all left from partial hysterectomy at age 24 and it cramps sometimes. My Doctor tested my hormones was ok . But the osteopath doctor sent 4 vials of blood to Texas and results totally different. Showed low estrogen high tester one and I was always hot for sex. Doctor said it was the high tester one giving me this symptom very uncomfortable truly. Was very moist in vagina and breasts were so sensitive and sore often. Now using 100 mg progesterone and a little estradiol at bedtime nightly . Have improved a little but still am miserable at times. My rheumatologist has only seen 3 ladies with these symptoms over his years of practice. I also have 8 other immune problems besides related to arthritis or stomach and heart issues under control . Would love to be included on a study if you have one in future. My phone is 580.231.3575 in Enid , Oklahoma. Thank You Diane L.
Fiona, what you say I uphold completely. The WHO study was based on entirely false information, using equine based eostrogen and synthetic pogestin, but, even in young doctors, these false beliefs are used to the detriment of women.
Plant based oestrogen, and natural progesterone protect women starting, and all the way through the menopause. Where I live (England), NICE have completely changed their stance on hrt. Many women could have been saved from suicide had these things been known when the skewed WHO research changed everything for women’s suffering for the worse.
I think this is really interesting and hope Dr. Younger can research this more. Not sure how prevalent or straightforward the hormone correlation is – I have been on birth control pills for a long time now that maintain my hormone levels and yet my FM pain has only worsened in the 15 years I have had it, despite starting birth control later on. I do agree that menstruation increases pain. But take for example that the link between estrogen and developing autoimmune disease is anything but clear and simple. 9 out of 10 lupus patients are women and it seems to abate during pregnancy but the connection has been studied for decades and it is still not fully clear.
It’s very true that this is a really complex subject. I too hope that Younger can do that multifactorial study and try to figure out more in what biological context hormone therapy works and what biological context it doesn’t. White believes that in the context of low testosterone estrogen just won’t work well (!). Similarly Younger found that high cortisol levels inhibit the hormones from keeping pain under control.
I’ll bet there are other interactions which serve to enhance or reduce the pain inhibiting effects of hormones.
Your experience is what I expected to encounter. Much like with lupus or multiple sclerosis, I believe the steroids in birth control that mimic sex hormones may provide temporary relief, but in the long run, they shut down the body’s production of natural hormones, which are the best defense against the disease.
So, women are left in a worse situation and almost dependent on birth control to find any relief because their body’s production of the hormones has dropped so low.
“Yay”. I am a peri-menopausal woman with M.E./CFS. I’ve never had fibromyalgia-type pain until a couple years ago. I noticed that when I started having changes in menstruation-shorter cycles, 21 days, then irregular altogether, I started having more body pain & worsening fatigue.
It makes sense that when anything interrupts the hormone cascade (Pregnenolone, Cholesterol, Cortisol, Progesterone, Estrogen, Testosterone) that the body will prioritize Cortisol, the life adapting, anti-inflammatory hormone. I recently started getting more PMS symptoms. Maybe it was because of the sudden decrease in regular exercise, from fatigue and pain, but I looked up my genetic potentials (www.promethease.com) and saw that I have a potential to not metabolize estrogen and some medications.
I took, and continue to take, Calcium D-Glucarate (glucoronidation, liver detox pathway) regularly, and DIM 2 weeks before my expected period. In 3 days of taking either my PMS symptoms (breast tenderness) disappeared. I don’t take the DIM anymore because it detoxes my lowering estrogen too much.
I use progesterone cream the last two weeks of my cycle-the “feel good” hormone, & I take pregnenolone, sublingual, regularly for the cortisol & estrogen replacement, and testosterone cream-just a smidge, which gives me energy, yeah, and is salvaging my muscle mass. You can order T cream online…
I can’t say that I have observed an anti-inflammatory effect from any of the sex hormones, but I believe that supplementation takes the burden off the cortisol need, & I clearly needed help metabolizing hormones.
I also supplement with NDT (Nature Throid), which did help my body pain (!), and am weaning off Hydrocortisone. They both saved my life energy wise, & resolved heart palpitations that I think are a disturbance in the hormone cascade-cortisol syphoning? HPA axis derangement from inflammation?
I’m looking into how prostaglandins may regulate cytokines, & my obsessive thought is about how microglia release cytokine pathways, & “once activated, they stay activated in a surveillance state. They can be re-activated.” M.E….
That blows my mind. What if inflammation is the underlying cause of all these cellular dysfunctions?
Link is from 1993, but interesting. Prostaglandins, Interleukins, and Cutaneous Inflammation. https://www.sciencedirect.com/science/article/pii/S1058668783710259
Hi Liana
The website you mention – http://www.promethease.com – do you need to submit a sample of DNA to use this?
I have metastasised breast cancer (the oestrogen dependent type). I had chronic fatigue through 2 decades, from my early 30s and, talking to other women with the same cancer, am interested to find that they were the same. I’m not sure how it would correlate with this study, as I’ve only glanced at it on my phone but I have wondered if high oestrogen levels could have caused the chronic fatigue, as well.
Lesley,
Hello. Yes. You can get your genetic data through 23&me.com It takes a few weeks to get results. Check out http://www.LiveWello.com as well as Promethease once you get your results from 23&me. These websites download your data from 23&me and charge a very small fee to make it easier to see what potential issues you may have. Bonus, you get to know your ancestry! I was shocked to know that I was related to Yakuts in Siberia ; ) You can email me if want to ask about anything else. http://www.sierrahealthadvocate@gmail.com
Fascinating information. My testosterone has routinely tested on the higher side. My homeopath said I have the personality to match those findings. Was diagnosed with FM in ‘04 and CFS in ‘14. Previous to CFS, I was able to manage the FM pain with diet and exercise, but the CFS pain is a whole different beast. Well that and I’m no longer active. Interesting to see where this leads…
I haven’t read the above article or comments but Jonas Bergquuist is doing a study on steroid hormones in ME/CFS. The study is funded by OMF. I haven’t heard when a report/paper is due. Here’s an extract from the OMF site:
“What are the roles of hormones, proteins, and antibodies in ME/CFS? To answer these questions, OMF is currently funding the research of Jonas Bergquist, MD, PhD, a Professor at Uppsala University and a member of our Scientific Advisory Board. Dr. Bergquist is measuring proteins in cerebrospinal fluid and blood plasma from a small cohort of Swedish ME/CFS patients. Some of the latest details and updates on Dr. Bergquist’s research are:
1. Steroid hormonal dysregulation. To determine whether steroid hormones are part of the pathophysiology of ME/CFS, he will measure the levels of 22 steroids in the plasma of patients and healthy controls.”
In 2005 I was in car accident severe whiplash..and minor concussion..head felt floating in jam..told police my name was jessy which is my daughters.. Pain continued 1 year later caught severe mrsa infection.
5 month battle than surgery. Hormones never checked. Til 2011.. My dr was shocked at 48 my levels espically of all forms testesterone were equal to late 70 yr old..along with other deficiences hgh, inf1, inf3binding, etc. I was put on biodentical replacement for a year…my pain improved along with brain fog, depression..dramatically.only chronic fatigue remained…i was diagnosed fibro because they thought I had lyme.butv3 elisha were high postitive 111.126.145
Western negative?
Now im more at chronic fatigue end then fibromyalgia.at 1st 5 years spine joint pain everywhere.
But i did have severe whiplash..feet cavus foot structure, peri neuropathy( most likely Cmt) multi level stenosis cervical…i had to stop hgh shots and biodentical creams bc dr no longer accepted my insurance. But I miss them. I felt so physically strong.little thinhs like carrying grocery bags into house made me proud.
I find the issue with these mixed illnesses is they are to complex for my drs…in RI especially.. My blood work.mri’s. Etc. Are all abnormal…and they don’t know enough about these conditions.i was upgraded to anterior pituitary desease/ disorder…perineuropathy, ostoarthitis, reiters desease, very high ebv 1gg, ebna igg for EBV?
And diagnosed chronic granolomatus kidney desease with small white kidnets and unspecified pathlogical lesion in kidney? Dr. Never mention it.
Now.I am dehydrating constantly, retaining fluid,chronic urinary, bladder, kidney infections…along with skeleton birth defects, along with ADD, learning disabilities, severe anxiety through out mothers family.and not having my fathers health information. Im woried about my children and grandchildren. They already have adhd, learning disorders,and severe anxiety, my grandson has all the clumsiness.lack of coordination that also runs thru family.
But im stuck without centers with knowledged in all these areas…so nothing gets checked into besides mental health..fibro.chronic fatigue and anxiety..
My advise take the testosterone..i rather live while im alive. They survive longer on a couch..
Im trying to findca new endrocrinist..good luck..Rita
go for it !!!!
hello,
thank you for this article! I search for informations about the connection between pain + testosterone. I have CFS+Fibrom. for 5 years, and since 1 year my testosterone level has started to rise (maybe fo genetical reasons, maybe it is the beginning of menopause…), now it is too high (double of the highest reference point of the lab). I noticed acne in my face, much increased libido, high irritability+agression and – to my amazement – decreasing muscle pain, decreasing sensitivity when touching the body, decreasing food intolerance and an decreasing overstimulated nervous system (listening to sounds, music,…)! so at the moment I am not sure if I want to treat the unpleasant side-effects of my high testosterone level(acne, agression,…) because of its “healing power” …..
Loving this page, thanks all for contributing, you are helping my thought processes
🙂
I find progesterone (from depo injection) much reduces fibro pain and also helps loosen up the tight muscles eg hamstrings. Less brain fog and a feeling of calm.
Progesterone? Progesterone is the CAUSE of my increased pain.
I know this because I did several IVF treatments to have my two daughters and the progesterone part was unbearable. My pregnancies themselves were also much more painful than my normal life.
Now, at 47, I am entering perimenopause and have tried every single type of progesterone (in BC pills, micronized, bio-identical gels, various different synthetics) and every single time my pain goes through the roof and stays there until I stop taking the progesterone.
For a long time I thought this was just me. Until one of my doctors (not an FM specialist) told me she had had two patients diagnosed with FM who made complete ‘recoveries’ after having their Mirena IUD taken out.
A quick google led me to discover that Mirena is a progesterone-only contraceptive, which uses a synthetic form called levonorgestrel. Further research revealed there is actually an ongoing class action suit against the makers of Mirena from thousands of women who spent years in pain and discomfort while using it.
All this not to say that progesterone is necessarily bad and everybody should stay away from it, just that there must be a subset of people for whom it actually induces the symptoms of fibromyalgia. I am definitely one of those people.
Jane> please educate yourself more about that. Mirena DOES NOT contain PROGESTERONE (healthy bioidentical hormone)
MIRENA cointans levonorgestrel-which is PROGESTIN (bad one which causes all kind of problems) !!!! Synthetic type of progesterone, but it is not progesterone…..
PROGESTERONE has only health benefits for the whole body.
I find this article and comments very interesting but hard to follow. I am in perimenopause and it’s a living hell!! It started with severe PMS-then I got sinus and allergies that I never had before. I guess your immune system is in overdrive trying to compensate for the fluctuating hormones. I got a virus and bronchitis like I never had before. It took weeks to get over it and shortly after the virus-my joints-muscles and body were in so much pain and I had extreme fatigue and was bedridden for almost a year it was accompanied with a lack of mental desire for life. A gynocologist put me on hormone replacement and within 3 days to a week of taking my estrogen-I was up and walking and the pain was diminishing. I had to take progesterone with the estrogen the second week and the 3rd week-I had to up the progesterone to twice a day and when I upped the progesterone-my symptoms immediately came back. I think they were overdosing me on progesterone (I get it from the compounding pharmacy). I did some google searching and I think you can be allergic to progesterone.
But-I stopped taking my estrogen because I felt so good-and my joint pain and fatigue came right back and I was in bed for 3 weeks/even though I immediately resumed taking my estrogen when I noticed my symptoms coming back. If I didn’t have PMs symptoms-I would (and still) think I have fibromyalgia and chronic fatigue-I know my hormones are causing it but I can’t figure out how or why. Too much?? Too little? Why is my body so affected or sensitive to the decline in estrogen—my blood work showed that my estrogen level was in normal range but thank God the doctor went off my symptoms and not lab work.
I am suffering and it’s disabling even though I still take my hormones-it’s the fluctuations of Perio-menopause I guess….and an area that the medical field don’t care about. I have read that woman who have breast cancer and they take the estrogen blocker medication (armatose sp*) have bad joint pain and fatigue will refuse to continue to take it because they have no quality of life. It makes me wonder how many women are suffering from fibromyalgia and chronic fatigue that is from hormones. I just wish someone knew why this happens to some woman and not others. Another side note-I was on the depo provera shot for about 10 years and stopped in my early thirties-I’m 47 now. Also-if anybody wants to get some good information about hormones—-watch Menopause Barbie on YouTube-I am learning a lot!!!! I highly suggest watching her.
I know this is an old thread but wanted to say, Me Too! I’m in the same age group and have tried progesterone several times in the li ast 25 years, each time it made whatever symptoms I was hoping to help much worse. Esp acne assoc6euth pcos in my 20s ro 40s, and now anxiety, pain and sleep trouble related to menopause.
It’s just not for me.
Brain fog prevents me from understanding how this might be related but DNA test showed 2 mutations involved in estrogen resistance.
I also wanted to say that-it’s the estrogen that helped me to feel better when I started taking it-the progesterone is NOT the “feel good hormone”. It is the hormone that gives you all your PMS symptom and only makes you have a period. Progestins are synthetic progesterones and causes many more adverse side affects.
Estrogen has receptor cells everywhere in our body and is like oil for our joints. The problem is-I don’t think the medical community realizes just how much we need estrogen and how much it affects our bodies in every cell from our brain to our joints and energy levels. More research is needed!! Also-an imbalance at perio menopause of all three of your hormones can cause one hormone to become the dominant one-like testosterone and give you the unwanted side effects. I am telling you that every woman needs to watch this menopause Barbie on YouTube because she explains so much on hormones that it will blow your mind!!!! I just cannot believe that in this day and age so little is known about hormones and menopause that so many women suffer with debilitating symptoms-I am one of them!!
I have just started HRT (organic made from yams, that mimics our version of hormones), I am perimenopausal. My all over muscle pain I’ve suffered from in 5 years has disappeared overnight. My brain fog has gone too!! I’m going back for the testosterone gel in December!! I absolutely agree with what is written above. I too have endometriosis, uterine fibroids and mammory cysts, these are flaring up since starting the HRT, but I don’t care. I’ve finally found something that works on Fibro and the side effects are worth it!! We need to do more studies on people to explore this as a treatment option for fibro, instead of pumping us full of painkiller pills that really don’t work and are dangerous and addictive…….
Yay
Hi marianne, iv had cfs for over 24years but managed to get my health back over the last 12 years until I hit perimenopouse, a year ago my periods went arratic But I was coping until now and the cfs pain ect is back and my doctor has offered my HRT and I don’t know what to do. Did you go on HRT from your doctor or go the more natural route?
Hi
I really related to your article
I’m a 45 yr old Australian male and i tick all the boxes – from my research this is really rare in 45 yr old males
I’ve suffered from this since April 2020, continue to be hospitalised and find it extremely difficult to work as I am on pain meds to function
I’m concerned about how I will be diagnosed and am struggling to see a path forward here
I have more appts in mid Feb and later March
Any advice would be welcomed
Mike,
If you’re taking opioids, they decrease testosterone over time, which makes pain worse. So your treatment may be contributing to your problems. Some doctors recommend taking opiods *with* testosterone, as testosterone escorts opioids across the blood-brain barrier, so they give more pain relief. Here’s a link that explains this phenomenon. Similarly, if you stop opioids, you may find your testosterone increases and pain decreases (over the long haul. Obviously, not during the weaning stage).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7645309/
Best wishes to you.
woah! My testosterone levels are not at all low…
Does anyone know if there are studies showing that there are females with not low testosterone at all?