

Surprises
Off all the cities I drove through on the Vegas to Florida to D.C. to Nashville to Birmingham to Tuscaloosa to St Louis, Kansas City and then on to Denver, Nashville was the biggest surprise. It’s not a big city, but cranes are everywhere lifting new, often striking skyscrapers into the sky. This city is booming!
The energized city wasn’t the reason for the location of the conference, though. Since 1873, Nashville has been home to Vanderbilt University – which contains perhaps the largest autonomic nervous system research center in the U.S.. Vanderbilt researchers were in abundance at the conference.
I have to give a shoutout to the Drury hotel chain. We were planning to do more camping, but after Skye had a horrid reaction to insect bites, except for a stay at my brother’s in DC, we hotelled it from Miami to Nashville, down to Alabama, up to St Louis and then over to Colorado.
After a horrid night at a cheap chain motel (mold ?), we largely went Drury for the rest of the trip and never regretted it. They’re a bit pricey but are clean and comfortable, accept pets, offer a free dinner buffet at night (and there’s something different about their sheets). If you’re traveling in the Midwest and South (or in Denver and Phoenix), they’re a good bet.
The Conference
The biggest surprise for this frequent ME/CFS conference attender was the crowd. The large room was packed to the gills with patients, doctors and researchers. Not only was attendance substantially larger than at the IACFS/ME conferences (how did that happen?) but younger female, probably postural orthostatic intolerance (POTS) patients, dominated. My guess is that the average age of the conference was a good 15 to 20 years younger than at the ME/CFS conferences I’ve attended. Many people come down with POTS during puberty.
Dr. Blair Grubb
The first speaker, Blair Grubb, MD, was perfect to kick off the conference. A dynamic and at time hilarious speaker with years of experience under his belt – Grubb participated in the first tilt-table studies ever – Grubb was full of hoary stories about the bad old days.
Grubb is professor of Medicine and Pediatrics at the University of Toledo. He authored the interesting “Quest for an Underlying Cause of POTS“, found on Dysautonomia International’s website (which features a hilarious slide) – and showed that in addition to about ten other conditions (diabetes, joint hypermobility syndrome, chemotherapy, amyloidosis, sarcoidosis, Lyme disease, Parkinson’s, MCAS), mitochondrial problems, traumatic brain injury and multiple sclerosis can all cause or be associated with POTS.
Grubb’s talk was full of interesting insights. Who knew that it takes about a third of the blood in the body to digest a full meal or that digesting a meal is “the most energy intensive thing anyone can do”. For me that was a reminder – not that one should have been needed after toddling off to bed so many times after a large meal – to eat small meals.
It was interesting to learn that humans are the only truly two-legged animals on the earth. Standing on two legs allows us to run longer than any other animal – so much longer that some hunting cultures actually made a practice of running animals to death – but it comes at a cost. In order to run, you need to relax the arteries to get more blood to your leg muscles while avoiding dropping the blood from your upper body into your legs.
That’s accomplished in a variety of ways – by increasing the heart rate and squeezing the blood vessels in the lower body to keep blood from pooling in the lower body. Plus, humans have developed a unique feature – a blood muscle pump. Most people use the muscle pump only during exercise, but people with autonomic problems also use it while standing.
Grubb noted how extraordinarily interconnected the ANS system is: you can’t change anything, he said, without changing everything,
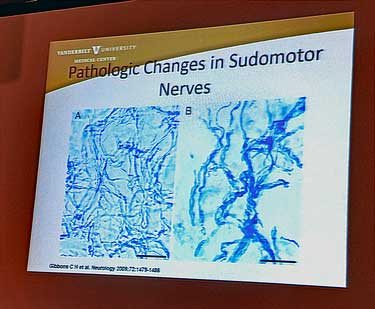
Small Nerve Fibers
The destruction of the small nerve fibers in the skin (small fiber neuropathy or SFN) is a big deal in POTS and fibromyalgia research right now (and with Drs. Kaufman and Systrom reporting similar findings in their ME/CFS cohorts – ME/CFS appears to be next). SFN can also be caused by a wide variety of factors, but the good news is that if you can stop the nerve damaging process, those nerves can quickly regrow. The bad news is that it’s not easy to stop that process.
Some of the really unusual symptoms found in ME/CFS/FM – those weird, hard-to-describe symptoms – could conceivably be caused by small nerve problems. (One person felt like he was sweating constantly, but was actually very poor at sweating. Gabapentin removed that sensation completely.)
If the small nerve fibers in the rest of the body (gut, blood vessels and more) are damaged – which Grubb and it seems everybody believes is happening in POTS, FM and ME/CFS – then watch out. SFN issues could conceivably account for almost every symptom and problem – from fatigue to problems standing to poor energy production – found in these diseases.
Testing
Skin biopsies, which are easily and cheaply done, are the best test (stay away from Qsart), but even skin biopsies can be problematic at times. While nerve fiber density in Caucasians is well known, people of other races can have different nerve densities – and throw off the test.
Skin biopsies are good, but they’re not the be-all and end-all test. Grubb pointed out a 32 year old “mystery man” who, after a year of tests and treatments, still suffers from fatigue, muscle aches, palpitations, discoloration of his feet, etc. His nerve conduction, reflexes and skin biopsy are all normal, but he has reduced sweating in the lower part of his body and his feet are exquisitely sensitive. Something is going on but they don’t know what .. .there is still much to learn.
Causes
The cause of the small nerve damage in the skin is not clear but some clues are emerging. As in POTS, many diseases or conditions have been associated with SFN.
Diabetes – Grubb noted that people with pre-diabetes have nerve damage BEFORE they get diabetes, and that in diabetes, at least, exercise actually helped nerve fibers regrow.
Autoimmunity is the most likely cause of the SFN in Sjogren’s Syndrome (SS) and sarcoidosis, but treating SS and sarcoidosis with drugs does not, oddly enough, improve the nerve damage. That suggests that something other than the autoimmune processes is causing the nerve damage in these diseases. (Sjogren’s Syndrome is going to pop up again and again in the conference.)
Amyloidosis – the accumulation of amyloid guck in the blood can cause small nerve damage. In fact, lots of things, including hereditary neuropathies, too much or too little Vitamin B, alcohol, drugs (metronidazole, statins, nitrofurantoin, bortezimib) can smack these small nerves.
Disentangling what’s harming the small nerves in POTS, FM and ME/CFS is going to be fascinating. Interestingly, the small nerve fiber damage in fibromyalgia appears to be different from other diseases. Besides disappearing, the small nerves in FM that remain appear to be getting smaller. Thus far several studies, including immune studies, have failed to find the cause of the SFN damage in FM.
One animal study, though, suggested that central sensitization may be causing the small nerves to perish, possibly as a protective effect. Once pain levels get too high, the brain may somehow cull the pain-transmitting fibers in the skin as a kind of protective mechanism,
Treatments
The list of possible treatments is a long but not particularly encouraging one. Grubb always seemed, at least to me, more focused on side effects than positive effects. Still, it appears that small fiber neuropathy is not something the medical profession is particularly good at treating or has devoted that much effort to fixing. Repurposed – not new drugs – appear to be the norm. I would be surprised if any drugs had been specifically developed to treat small nerve fiber problems.
Exercise (probably recumbent) can actually help regrow the nerves in some SFN patients. Intravenous immunoglobulin (IVIG) can be very helpful but is horribly expensive, hard to get covered by insurance, can cause headaches (already a problem in POTS) and comes from a lot of donors with all the worries (infections) that can entail. (Lauren Stiles announced that Dysautonomia International is sponsoring the first IVIG POTS trial.)
Norepinephrine-based antidepressants can help, but can mess with blood pressure – not a good thing in a disease with orthostatic intolerance. SNRI’s increase blood pressure – which could help – but make some people worse. Anti-epileptics such as gapabentin and neurontin can cause weight gain and fatigue. Bear in mind that some of these obviously do help, but Grubb wasn’t exactly providing a lot of good news.
More POTS Than We Know (Or The Tests Pick Up)
The symptoms in POTS are very similar to those in chronic fatigue syndrome (ME/CFS). They manifest themselves more upon standing and include fatigue, exercise intolerance, cognitive problems, heart palpitations, chest pain or discomfort, lightheadedness, blurred vision, shortness of breath, headache, nausea, fatigue, and tremulousness. One different symptom is commonly present – the legs of about 50% of POTS patients turn red-blue (acrocyanosis) and feel cold to the touch upon standing.
POTS often starts with an acute stress such as an infection, during pregnancy, after surgery, etc., and like ME/CFS and FM, mostly affects women. People tend to get POTS earlier in life than ME/CFS.
Grubb, being the smart researcher that he is, believes the criteria for POTS are too rigid. Not meeting the criteria doesn’t mean you don’t have “POTS” – it just means the criteria need work. He has patients with all the symptoms of POTS who don’t meet the criteria.
Indeed the test results are quite mutable depending on how the test is done. As Dr. Peter Rowe has pointed out, a tilt table test taken earlier in the day can have quite different results from one taken later in the day. A longer tilt table test pushes many more people into POTS. Plus, a small study performed by Dr. Baraniuk found that a bout of exercise temporarily induced POTS in almost half his ME/CFS patients. There’s still a lot to learn about just what POTS is…
The Big News: Larger Autoimmunity Study Succeeds
The big news in POTS has been the discovery of autoantibodies that are whacking a receptor (adrenergic-1 receptor) in the legs that causes the veins in our legs to narrow or vasconstrict as we stand. The knock on the past autoantibody POTS studies has been their size, but Grubb reported that a much larger antibody study (75 patients) found that no less that 92% of POTS patients had autoantibodies which were attacking that receptor, and other autoantibodies were elevated as well. There will be more on this study and its implications in the second blog.
Grubb said he’d suspected autoimmunity in POTS all along but the testing used to be too expensive. It’s still expensive, but a lot less than it used to be.
The autoimmune finding looks like it’s going to redefine at least a very large subset of POTS patients and possibly the disease itself. Not only that, but it’s affecting other fields as well. Taking a clue from the POTS findings, Dr. Scheibenbogen found evidence of autoimmunity in about 40% of ME/CFS patients. Reports from the ME/CFS Montreal Conference suggest that a follow-up study from another lab is getting similar results.
POTS Treatment
The big question is treatment. The next generation of drugs will probably be biologics that affect the autoimmune processes in POTS. These definitely work better and many more are expected to come on the market over time. Their downside is expense and the potential for significant side effects.
The treatment picture for POTS is mixed indeed. Treatment effectiveness has been spotty – no surprise in such a heterogeneous field. Several reviews mention the long trial-and-error period often needed to find a drug that works – if that happens at all. Many of the treatments produce side effects which render them intolerable as well.
Standard Treatments for Neurogenic POTS
- Hydration, salt loading, reconditioning
- Blood volume expanders – (fludrocortisone, DVAP)
- Vasoconstriction – midodrine, droxidopa
- Heart rate – beta blockers, ivrabadine
- Nerve activity enhancement – pyridostigmine bromide.
Hyperadrenergic POTS
- Alpha/beta blockers
- Clonidine
- Methyldopa
- Biofeedback – Grubb expects more use of this therapy.
No drug has yet been FDA approved for POTS, but an old drug is helping and a new drug to the U.S. is making quite a splash.
- Find out more – Drugs for Orthostatic Intolerance
The Old/New Hope – Pyridostigmine Bromide (Mestinon)
Pyridostigmine bromide (Mestinon) has been around for a long time but it’s often not mentioned as a drug for POTS. Several studies, though, have found that it reduced heart rate. One large study (203 POTS patients) found that about 60% experienced significant improvements in fatigue and heart rates. Mestinon has been a favorite drug of Dr. Systrom’s in both POTS and ME/CFS for quite some time. If I remember correctly, a study assessing its effectiveness either is or will be underway. Check out how Mestinon dramatically helped one long term ME/CFS patient.
The New, New Hope – Ivabradine
While Grubb hasn’t been particularly happy about the treatments available, he’s very high on Ivabradine (Corlanor in the U.S., Procoralan (worldwide), Coralan (in Hong Kong, Singapore, Australia and some other countries), Corlentor (in Armenia, Spain, Italy and Romania), Lancora (in Canada) and Coraxan (in Russia and Serbia).
Grubb said Ivabradine has a 75% success rate: that’s unheard of in this complex condition.
Ivabradine appears to be unique in its ability to affect heart rates without affecting other aspects of cardiovascular functioning such as blood pressure. It’s been available as a heart failure medication in Europe for years. Amgen apparently bought up rights to it in the U.S., got it approved for heart failure in 2015, and then jacked up the price significantly to $4,500 for a year’s supply. Grubb said many of his patients are getting it from Canada.
It’s a drug that’s begging for a good randomized trial. Thus far two prospective open-label trials, three retrospective cohort studies, and eight case reports have examined its efficacy in POTS. All have been successful but none are large or rigorous enough for prime time.
A June 2018 review concluded that Ivabradine lowered HR and provided symptomatic relief of POTS without affecting blood pressure. A 2018 retrospective analysis found Ivabradine (0.1 mg/kg twice daily) improved symptoms in almost 70% of adolescents.
A 2015 study on just eight patients found Ivabradine (7.5 mg) significantly slowed their heart rates both at rest and during tilt without producing significant adverse effects. That study noted that beta-blockers (propanolol, atenolol) can slow the heart rate in POTS as well, but often at the cost of increased fatigue, sleep disorders, and impotence. Those side-effects are apparently not a problem with Ivabradine.
A 2010 case series found the drug reduced symptoms in 55% and fatigue in 70% of POTS patients. The study found a low dose formulation (2.5 mg od) the most effective for most patients. The study suggested that Ivabradine may be more effective in some people when taken in conjunction with midodrine or fludrocortisone.
A small POTS Ivabradine trial (n=20) that’s underway at the University of San Diego should be finishing up about now.
The Struggles of Chronic Illness
Do not be daunted by the enormity of the world’s grief. Love now, Do justly now. Love, mercy, now. You are not obligated to complete the work, but neither are you free to abandon it. The Talmud
Grubb ended on a kind of transformative note. He’s had his own struggles with serious illness – his wife’s death and his struggle with cancer. He was irritable, angry and mean during these struggles – so altered emotionally that he saw a counsellor (you would never think this guy would see a counsellor… :)) and the counsellor really helped.
It can take a long time to reframe your life if you have a chronic illness – to accept that your life for the foreseeable future is going to be very different. Grubb emphasized that, no matter what our condition is, every one of us makes a difference. It was a lovely and unexpected ending to an excellent talk.
The Mayo Perspective – Paola Sandroni
Then came the drill sergeant – Dr. Paola Sandroni from the Mayo Clinic. She was in the big room and I came late to her talk. Looking rather severe and talking in a clipped manner, she was the picture – at least to me – of a Mayo Clinic researcher.
She seemed to be on top of her game when it came to POTS, but when it came to ME/CFS she was wanting – and in the worst way.
Quite a few questions dealt with the Mayo’s “POTS Clinic” which features, she admitted, a “tough love” approach. The goal of the clinic is to increase functionality and reduce isolation. It was originally intended for use in pain patients but will apparently take on just about any condition that is severe enough to disable a patient. It’s now being used in POTS, ME/CFS, fibromyalgia and other conditions.
Thankfully, she didn’t call the clinic a cure but she did, without saying what the clinic considers a “success”, state that the clinic’s success rate is about 70% in POTS and about 50% in chronic pain.
The 8 hours a day, 3 week program can work in the right person. One of the most astounding treatment successes I’ve ever seen involved a young woman with a devastating case of chronic regional pain syndrome (CRPS) in her leg. She was unable to walk or even to put pressure on her deformed foot when she started the program. She left the program much improved and eventually resumed a normal life.
One young POTS patient, whose story was chronicled on Health Rising, used the program to help him fully recover as well. Prior to entering the clinic, he was greatly aided by the iron infusions he took which allowed him to finally exercise, but the program helped him return to full functioning.
Sandroni simply touted the biopsychosocial party line when it came to ME/CFS. People with ME/CFS have PEM, stop exercising, become deconditioned and exercise intolerant. Orthostatic intolerance (OI) is the next logical step.
Among many others, Peter Rowe would have a fit at this. At the Montreal Conference, Rowe agreed that deconditioning can, of course, lead to OI, but cited a soon-to-be-published study showing that the OI is NOT related to deconditioning in ME/CFS. People who are deconditioned with ME/CFS have OI and so do people who are not deconditioned. He hoped that study would put the deconditioning saga in ME/CFS to rest. Let’s hope that Sandroni reads it.
Sandroni was very focused on stress and the stress response in these diseases. She believes that an overly active stress response increases the excitability of neurons which results in central sensitization; i.e. lots of pain, stimuli problems and fatigue.
I have no doubt that central sensitization is part of ME/CFS and FM. Nor do I mind the idea of watching out for negative thoughts that increase one’s pain and fatigue – it’s only natural that those would occur in a chronic illness. But to boil an illness down to those and other basic problems (poor sleep hygiene), as it seemed to me she was doing, was shocking.
It was disappointing to see Mayo show up like this again. I just heard of a patient who, after getting a lot of testing done at Mayo, was told they had chronic fatigue syndrome (ME/CFS) but there was nothing they could do for them. That’s obviously not a great result, but it’s not such a bad result either. The Mayo doc apparently did not pooh-pooh ME/CFS, and he apparently acknowledged that it was real and serious – he just didn’t know what to do with it. That’s a step forward but we obviously have a long way to go.
A Kaufman Interlude
Dr. David Kaufman was one of two ME/CFS practitioners (Theresa McDowell was the second) that I saw at the conference. (Jaime Selzer and Beth Mazur of ME Action, and Fred Friedberg of the IACFS/ME also attended.)

- Check out Dr. Scheibenbogen’s CellTrend Test here.
His major new interest of the last couple of years, though, is mast cell activation syndrome (MCAS) – which, in his experience, is common in ME/CFS. Dr. Kaufman is also finding a very high incidence of small fiber neuropathy (@80%) in his ME/CFS patients. (He tests all of his ME/CFS patients for SFN.) Recently Dr. Systrom reported that 50% or more of his ME/CFS patients are testing positive for it as well. It’s taken awhile but small fiber neuropathy is coming to ME/CFS…
Kaufman’s ascent into ME/CFS was fortuitous – he was an immunologically-based HIV doc who left New York to start a practice, and just happened upon the Open Medicine Institute (which he has since left) where he learned about ME/CFS. He loves his practice and knows of several ex-HIV docs who enjoy the complexity of treating ME/CFS patients.
Kaufman has been practicing a long time but looks to be in great shape and said he loves his work and has no intention of retiring. Here he was – several thousand miles away from his Mountain View practice – learning more about dysautonomia and ME/CFS.
Dr. Maitland from Icahn School of Medicine on MCAS and Dysautonomia
I found the talk much like the field – complex and a bit confusing. This is a field that is still finding itself but it’s clearly full of promise. Mass cell activation syndrome (MCAS) cropped up frequently in the conference presentations. It’s becoming a big deal in dysautonomia/POTS, etc. The big room was packed and afterwards Dr. Maitland was swarmed by patients asking for more.
Maitland was a ball of fire. She has sterling credentials – an MD AND PhD – and is Board Certified in allergy and immunology. An immunologist in a field that knows almost nothing about MCAS, it was clear that she was rather disgusted with the hidebound nature of the field. She said the average time to get diagnosed with immune- mediated disorder was 12 years. Of the 77 training programs on allergy and immunology in the U.S., only a handful inform our future immunologists on MCAS. Clearly at ease, she punctuated her talk with numerous humorous asides.

One of the immune system’s first responders, mast cells are filled with nasty pro-inflammatory granules they’re just waiting to unload when a virus, parasite, toxin, allergen, etc. comes along. Carrying an enormous quiver of immune factors (tryptase, histamine, serotonin, heparin, eicosanoids, lysosomal enzymes, prostaglandins, cytokines, TNF-a, chemokines, etc.), they are armed for battle indeed. A complex process determines which factors a mast cell will release. Occurring across the body, in the gut and the brain they have the potential to produce many different symptoms.
Symptoms
A huge question is what role MCAS plays in POTS, ME/CFS and FM. Does it cause those diseases or is it simply associated with them? White’s 2015 overview “A Tale of Two Syndromes – POTS and MCAS”, published on Dysautonomia International’s website, indicates we still have much to learn about all these disorders. He calls the POTS/MCAS connection “an extremely complicated intersection of two poorly understood illnesses”.
The symptom presentations in MCAS, POTS and ME/CFS appear to be similar but also somewhat different. In his 2013 overview, Afrin describes a truly enormous number of possible symptoms, but White highlighted specific symptoms (recurrent abdominal pain, diarrhea, flushing, itching, nasal congestion, coughing, chest tightness, wheezing, lightheadness), some of which commonly occur in ME/CFS and some of which do not.
A 2010 review reported the following symptoms can be present: anaphylaxis, fainting, fatigue, flushing, rashes, itching, hives, chest pain, rapid heart rate, wheezing, pain, nausea, vomiting, cramping, bloating, diarrhea, GERD, cognitive problems, dizziness, migraine, tingling sensations, and peripheral neuropathy.
Some of the symptoms commonly found in MCAS (flushing, hives, asthma, anaphylaxis and diarrhea) are not particularly common in ME/CFS or POTS. Exercise intolerance – a key feature of ME/CFS – is not mentioned.
Odd sensitivities are an intriguing part of MCAS. If you’re experiencing a sensitivity to something which is obviously not allergy-based; i.e. does not respond to antihistamines, Dr. Maitland believes MCAS might be the cause.
Hypersensitivity Disease
Like so many other hypotheses concerning these diseases, Maitland believes a hypersensitivity plays a role. Instead of a microglial cell hypersensitivity and/or a central nervous hypersensitivity, she believes that trigger-happy mast cells that are over-reacting to all sorts of stimuli are the main problem in MCAS.
Testing
Testing, unfortunately, is suboptimal at best. Maitland said that tryptase is the best current marker but one tryptase test is not enough. In fact, Maitland said, she doesn’t know what a “normal” tryptase test looks like, and three tests are needed, including a baseline test done during symptom exacerbation. (I understand why getting a marker during symptom exacerbation can help, but what I don’t understand is why a key marker isn’t elevated even when I’m in my “normal shitty baseline” (NSB – thank you Trina Berne). My NSB is pretty darn bad…)
A POTS review suggested that a methylhistamine test done within four hours of a flushing episode can diagnose MCAS/MCAD. White recommended measuring histamine, prostaglandins and leukotrienes in a 24 hour urine sample.
A 2017 retrospective study of 117 POTS patients found evidence of increased prostaglandins in 50%, increased methyl-histamine in 16%, but no evidence at all of increased tryptase. It also found that symptoms didn’t differ between POTS patients with MCAD and those without it. The authors believed that 20% of their cohort probably had MCAS.
Interestingly, if you’ve had a colonoscopy done, you can have it restained to see if mast cells are present. Mailand mentioned one woman who’d never recovered from food poisoning whose colon turned out to be packed with mast cells….
Treatment
Treatment depends on “what’s tickling your mast cells”. That means testing for various triggers. Besides the limited mast cell tests available, Maitland does limited allergy testing, rheumatology panel, EDS screen, neuropathy screens, celiac panel, colonoscopy, pathogen screens, and testing for a primary immune deficiency disorder. She mentioned using prophylactic antibiotics and gamma globulin, but oddly enough I don’t remember hearing about quercetin.
A treatment slide on MCAS and Dysautonomia mentioned medications that are rarely used in ME/CFS (fexofenadine, diphenhydramine, cromolyn, pepcid/Zantac, aspirin, omalizumab).
You don’t need a pollen allergy to have an IgE (histamine based) reaction; you can have a histamine reaction to foods, drugs or other allergens. If antihistamines work for you, they may apply to those factors. Because of the many sensitivities Maitland comes across, about ten percent of her patients leave her office with script for compounded meds due to problems with the fillers in prescriptions.
Interestingly, Maitland mentioned low dose doxepin elixir (Sinequan), an old favorite of Dr. Cheney’s. Generally used as a tricyclic antidepressant, Cheney instead used low doses of doxepin for its anti-histamine and immunomodulator properties. Cheney called the histamine receptors the “grand maestro” of the central nervous system and believed that doxepin could calm the over-active nervous systems in ME/CFS/FM and allow healing to take place.
Because Maitland is dealing with a hypersensitive, trigger-happy mast cell system, stress reduction is on the list as well.
MCAS and POTS
There was little on MCAS and POTS in Maitland’s presentation, but MCAS is clearly a subject of great interest to the field and numerous presenters mentioned it.
In his recent POTS review, Raj, a speaker at the conference, stated that a subgroup of POTS patients with episodic flushing have a mast cell activation disorder. Biaggioni also recommended testing for MCAS in POTS if flushing is present and suggested that hyperadrenergic POTS is more common in MCAS-POTS patients.
The flushing can be produced by a wide variety of triggers (exercise, standing, sexual activity, eating, menstrual activity) and can be accompanied by many other symptoms (lightheadedness, dizziness, shortness of breath, excessive diuresis, nausea, diarrhea, vomiting, and headache).
Several presenters simply recommended that practitioners not rely on testing for MCAS and treat for it if they believe it’s present and see what happens.
It’ll be interesting to see over the next five to ten years how all these disorders – MCAS, ME/CFS, EDS, IBS, POTS, FM – come together. Will they merge or split apart?
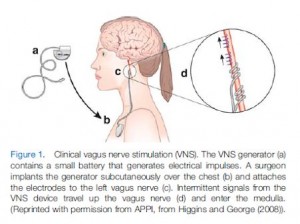
Non-invasive Vagus Nerve Stimulation Helps POTS (Somewhat)
We know that implanted vagus nerve stimulators can do wonders for people with epilepsy, and can help in depression and heart failure and even in fibromyalgia. Benjamin Natelson’s small fibromyalgia study produced some scorchingly good results, even in some really severely ill patients. Natelson, who’s been in this business for decades, said he’d never seen anything like it.
Stimulating the vagus nerve – the largest nerve in our body – suppresses overactive sympathetic nervous system activity and boosts parasympathetic nervous system activity. This results in enhanced anti-inflammatory activity.
Dietrich got interested in vagus nerve stimulation (VNS) after a young girl and a woman with epilepsy found that turning their stimulator on allowed them to endure a tilt table test without getting ill. Given the reduced vagus nerve activity found in POTS (low heart rate variability (HRV), high heart rates (HR’s)), it made perfect sense to try out non-invasive VNS.
Dietrich’s goal was to increase POTS patients’ HRV (low HRV = decreased vagus nerve activity) and to reduce their heart rate. He took 20 patients, put them on the tilt table, and then turned on the stimulator!
Unfortunately, several of his FM patients had high HRV’s (another subset?) instead of the low HRV’s he expected.
He wasn’t able to normalize his POTS patients’ tilt table readings, but he was able to increase the time they tolerated the tilt table test by five minutes and increase the HRV (in those with low HRV). Some symptoms including brain fog and tremulousness improved, and lightheadedness improved significantly, but HR was not reduced and in the end the results were mixed.
This certainly isn’t the end of VNS studies in these diseases. Natelson is now, or should soon be, beginning a non-invasive vagus nerve stimulator study in fibromyalgia.
We’re a long way from knowing how to tweak the peripheral nervous system effectively. Thankfully, Francis Collins realized how many potential therapies we may be missing out on and began NIH’s 1/4 billion dollar SPARC initiative. This high-risk, high-gain initiative is an attempt to learn how to manipulate our peripheral nerves (those in our body, as opposed to our central nervous system) to reduce pain, relieve inflammation, heal heart problems, fix gut disorders and more.
Making Drugs Obsolete: The Electroceutical Revolution – A Fibromyalgia and ME/CFS Perspective
The first day of the conference was over. The only thing missing was a good rest area with couches or beds one could lie down on. (Montreal lacked a good rest room as well.) One day was enough – more than enough, actually, for my partner who, as she did in Montreal, had to skip the next day. I went back to the hotel and rested up.








Thank you so much for this great information and to all the people who are trying to help solve this conundrum of chronic misery.
Thank you Cort, for such a comprehensive summary of that conference. So much information to take in! It fills me with hope that ME/CFS and/or fibromyalgia sufferers can look forward to efficient treatment.
Moreover, all this research might lead to new, more defined diagnosis. At the moment, most ME diagnosis are just a mixed basket of symptoms, very possibly indicating different ailments and caused by different triggers.
Many patients might offer a fertile ground for developing these symptoms, where other people can have been affected by the same trigger(s)and not become chronically sick.
Cort, your blog is priceless and your efforts in keeping us updated are immensely appreciated.
That is a great takeaway. It made me realize that with all the possible syndrome and conditions that have shown up – from MCAS to different kinds of POTS – check out the presentation on hyperadrenergic POTS coming up shortly – to EDS, to other kinds of dysautonomia to the autoimmune subset of ME/CFS – what we really need are better diagnoses – better ways to figure out what’s going on.
“what we really need are better diagnoses – better ways to figure out what’s going on.”
And what can be done easily today is:
* Register all patients diagnosed with ME/FM/EDS…
* Fill the register with developments of the disease over the years
* Compile a list with comorbid diagnosis missed when first diagnosed
* Compile a list with how much % of patients significantly improves after a missed diagnosis is treated; add info on treatment and what lead to the diagnosis.
In my case: if there were a list stating that x % of patients has (probably) insufficient pancreas functioning, that it can be detected in y % of those cases by exceptionally frequent apthous ulcers and too high amylase markers and can easily be partially corrected by supplying the appropriate enzymes in z % of those cases it could have triggered a red flag due to my family and personal history at the start of my disease. Life could have looked different.
Such list, with a determination to make it qualitative, combined with a team of specialists comparing each patient diligently against that list could make quality of life for many patients so much better. That wouldn’t require a single medical breakthrough, just the will to broadly recognize these diseases, adequate funding and determination to successfully execute the plan.
It would allow many patients to stay much more active in their family and even have jobs as early diagnosis and treatment of comorbidities that strengthen the disease is so much more effective then when doing so late in the disease. This could even make the funding a self paying investment when done at the state level.
Hi I was wondering if there has been any new discoveries on this debilitating nuanced disease I S T I ve researched alot and cant seem to find anything at all that causes it or helps it. I just know that my ordeal started right after I got sick with viruses like 4 times in a row and an ear infection. Which in my right ear the pressure has never equalized. Thank you for reading.
I think also anyone with these numerous named conditions above should get tested for Alpha-Gal & do an IGE Total blood test…Magnesium
Stearate should be avoided including lactose in some & gelatine & countless other food vitamin medicines contain numerous of these
ingredients. An EpiPen also should be carried as well & Alpha-Gal is being linked to low blood pressure drops…I looked up McDonald’s
french fries they contain a beef flavoring & other things…Makeup, cleansing products, candies the list is very long & even some contact
lenses, lip balms etc.
Yes, this is so useful and important. Heartfelt gratitude for your great efforts to share with all.
Thanks :).
You’ve done an amazing & thorough job summarizing these presentations, Cort! I couldn’t travel to the conference due to my health and am so very grateful that you’ve shared this information. Thank you so much!
Thanks! The next day was actually more interesting. ?
Having HYPERPOTS subset, MCAS and EDS – this is all of much interest to me. Having these things most of my life has been a challenge. It also runs in my family. Neuropathy also a family problem. Mine getting steadily worse. I’m sure autoimmune is involved. Thanks for the coverage. Looking forward to next two days overviews.
Issie
Super informative, as always. Thank you so much.
Thanks?
I’m wondering why it was advised to stay away from QSART testing. Can you share more Cort? Otherwise lots of good information!
I believe he said it was not particularly reliable I guess you could get a false negative with that.
Did he still recommend Qsart for autonomic dysfunction? Or not recommend it at all?
Awesome article 🙂 I have a question : “stay away from Qsart” – why? I’m scheduled for Qsart at Clevelenad Clinic July 30th. they feel it’s a necessary part of autonomic testing…but I’m not clear on why.
I’m afraid I just have my sketchy notes. I’m sure Qsart testing can be helpful but I think the problem may be that it’s not determinative. If you have a positive test that tells you something but a negative test but a negative test doesn’t mean nothing is wrong. That was my takeaway.
Thanks so much for sharing this Cort! Such great information
I wanted to comment on the idea of exercise and deconditioning. When this program came out about exercise, most of us on the POTS forums were furious. Especially since it targeted younger Children. So many of those on the site I was on, got POTS while being professional athletes, ballerinas and very active and physical people. Some of us have it in extended family with generations having issues. We knew it wasn’t from being deconditioned. Now, do we become deconditioned? Yes, many/most do. But, there are some who have done gradual and increased movement/exercise. Some started out with just a walk to the mailbox. Some who were bad fainters, just a walk to the bathroom. One guy worked up to running a few miles. One guy, who is a doctor BTW, went from complete bedridden to riding his bike miles a day. And now is back in practice. (And I see him as one of my docs.) Some do manage to increase their exercise – therefore are not deconditioned. Do they still have POTS? Haven’t heard anyone say they were 100% cured. Exercise helps because it increases ability of muscles to assist in blood flow. Even if we ride a bike apparatus while sitting on a couch – helping blood flow is a good thing. But this tough love thing is just mean. Not a good way to look at this illness and not child’s fault for being so sick. He shouldn’t be made to feel he is sick due to inactivity. Which comes first…..? Okay off my soapbox.
Oh, and exercise causes mast cells to degranulate. So be careful as you could trigger a very bad reaction. Have medicine on board and handy. I carry an epi pen with me and have liquid children’s Allegra with me. (Seems to take effect faster.) I also use straight GastroCrom, from the vials, if I can’t get to water. I do walk a lot and do light PT. It is absolutely necessary for me. I find it does build my endurance and stamina. (I was at one time in a wheelchair.) But, there are many much worse than me and I won’t fault them for where they are on their journey. I do feel it is important to move. And it has helped me. Deconditioning may contribute, but is NOT the cause.
Cort, I agree with others – you are doing a fabulous job with coverage and making sense of what may be new to you and others. Good job!
Issie
Thanks Issie, your comment demonstrates what a complex and really confounding area this is. The best thing I can think regarding exercise and energy is to do a heart based exercise program to keep you as fit as possible.
Years ago, I passed a Qsart test, but I barely sweat. I didn’t do a full body test, just on my feet.
I have neuropathy in my feet. I also had a nerve biopsy and passed. But I now have very little feeling in my feet at least halfway up. They stick me with pins and I don’t feel them. My dad had it the same way up to his knees and in hands up to his elbows. Both me and my sister present the same with our neuropathy. I have POTS and she has CFS with OI. We both have FMS. But only I have EDS. Her kids have EDS and POTS and one has MCAS too. Mom had MCAS. Her mom had POTS. Go figure. Yes, we are in research projects as a family.
Issie
So glad your family was willing to get into a research study Issie. So much to learn there. So interesting that you’ve lost feeling and yet passed a biopsy! As Grubb said even the best tests are still missing something.
https://youtu.be/ee4Ps5bTZKQ
This is an interesting interview of Dr.Maitland on MCAS that I remembered from one of the EDS sites.
Issie
How does Mayo achieve remarkable results? Easy. Anybody who drops out in disgust or because they get worse is considered “cured”. And of course severe ME patients will never sign up to start with.
Unless the Wessely School psychobabblers are publicly humiliated and driven from the field and their work is thoroughly discredited and retracted, we will be subject to medical abuse for at least another generation.
I think the more good research that is done the less and less we will have to worry about the Wessely crowd.
Thanks so much for this great recap of an event many sufferers are unable to attend. I’m a patient of Dr. Grubb’s; and have been to Mayo. Grubb and his NP Dr. Karabin(PhD) have been the most help with diagnosing my hyperadrenergic POTS. Again, thanks for this great service to the community.
I REALLY enjoyed listening to Dr. Grubb. He was a perfect lead off speaker, full of interesting stories, very personable….he was good. Stay tuned for the hyperadrenergic presentation by Biaggioni.
As always, thanks so much for the amazing work Cort! Looking forward to your Day 2 report. Just wondering if you be writing about Dr Raj’s presentation? I’m interested as I’ll be seeing him in Calgary in the next few months so would be great to learn more about his current direction.
I attended Raj’s presentation and will report on it. It was not ground-shaking but was interesting.
Fascinating and very helpful. I learned so much! Especially, about digestion using a whopping 1/3 of your blood. I knew it could worsen OI, but…no wonder I feel awful when I eat larger meals. I’ll be passing on the info in this blog to others. Hopefully, (pretty please doc), my doc will agree to try some new meds for my OI/Pots. Cort, appreciate your effort to get us all of this info.
That made me think a lot too. 🙂 Trying to cut back.
With ME/CFS and bad orthostatic intolerance—not the POTS version as my heart rate stays low—I have learned to barely eat during the day when I need to be able to be upright. So it is late afternoon to evening when I get most of the day’s nutrition. That is the part of the day when I can sit or lie down freely.
Have had SFN diagnosed for years. One symptom I have which you didn’t mention above is numbness. Sometimes there are strange sharp pains too, and always both muscular aching and central sensitization, but I wanted to say that numbness is an issue too.
Last point is a question, Cort—-What are the autoantibody tests now recommended?
Thank you!
Oxidative stress and sterile inflammation are huge players in neuropathy, chronic fatigue, and fibromyalgia in general. They all lead to mitochondrial dysfunction which creates intracellular energy crisis and numerous related symptoms. These are ideas with growing research evidence and will likely redefine the field in the coming years.
Of course, there can be many causes for oxidative stress and sterile inflammation. The key is to find whats relevant for the patient and address it appropriately.
If Shungu is right oxidative stress is going to be a huge player in ME/CFS patient’s brains. I had never heard of sterile inflammation before. Thanks for passing that new distinction along.
“Sterile inflammation is a common event, triggered by physical, chemical or metabolic noxiae. The different noxiae cause cell stress and hence stress responses. Many types of stress response exist (e.g. unfolding protein response, integrated stress response, oxidative stress), often entangled among each others. Stress responses trigger inflammation. When noxiae persist, inflammation does not resolve, resulting in a vicious circle that has a key role in the pathophysiology of many human disorders, including cancer, metabolic and genetic diseases. Several factors have been proposed to play a role in the different types of sterile inflammation, including redox remodeling, DAMPs, heat shock proteins.”
https://www.frontiersin.org/research-topics/367/mechanisms-of-sterile-inflammation
I hadn’t heard about the term “sterile inflammation” neither. Thanks for learning us ;-).
I believe for some time that if inflammation is low grade and body-wide, then it could be suppressed inflammation because “full, normal strength” inflammation body wide would be lethal as in worse than sepsis. Think about an inflamed swollen purple toe but then for the entire body: one big swollen purple bag…
I recently start to believe we may have massive “interstitial inflammation”, see https://medical-dictionary.thefreedictionary.com/interstitial+inflammation. Amongst others it does:
A) “Hemodynamic changes begin soon after injury and progress at varying rates, according to the extent of injury. They start with dilation of the arterioles and the opening of new capillaries and venular beds in the area. This causes an accelerated flow of blood, accounting for the signs of heat and redness.”
B) “Next follows increased permeability of the microcirculation, which permits leakage of protein-rich fluid out of small blood vessels and into the extravascular fluid compartment, accounting for the inflammatory edema.”
Now imagine what a small wound can do when it comes to swelling. Let me take a pot with boiling water as an example. It’s “only” 100 degrees C. Firmly touch it for a second with the thumb and visually swelling will occur. As heat is the cause, heat shock proteins will form here. As touching the pot only for 1 second with the thumb will not transfer significant amounts of heat to the thumb, a long lasting hot spot won’t occur. So reducing swelling by cooling does not work by taking away the absent heat but by decreasing blood flow.
The point I wish to make is: a small localized insult can create a source of (interstitial) inflammation that can draw plenty of liquid into the nearby interstitial tissue. Doing so with body wide inflammation would highly disrupt water balance in the body and overload the interstitial fluid and the lymphatic system. In the lungs for example that could cause dangerous drowning them in water.
In https://www.webmd.com/lung/interstitial-lung-disease I found:
C) “Interstitial lung disease is more common in people with autoimmune disease”
D) “They may also have a decreased ability to transfer oxygen from their lungs into their blood.”
Having to breath fast/deeply (“hyperventilate”) is common in ME. D) would require us to breath harder then average while still having shortness of oxygen.
The point I wish to make here is: dropping the amount of blood so much that blood flow at the capillaries is only a fraction of normal may be needed to control interstitial fluid in the body and even more so in the lungs.
The https://en.wikipedia.org/wiki/Renin%E2%80%93angiotensin_system has a high “presence” in the lungs and may do exactly what it is designed for: decrease blood volume so much as to allow breathing while not exaggerating/dropping death due to lack of blood flow.
Throwing in a high dose of adrenaline helps to accomplish this. It offers better breathing (prime bronchodilator) so that the renin-angiotensin system can be set a bit less sharp and it decreases blood flow in the less-vital functions to save the vital functions, allowing to decrease long term damage that the renin-angiotensin system does when setting blood volumes soo low for soo long.
Even night sweats could be connected to it. At least for me at night breathing becomes even more problematic (very deep breathing while still lacking oxygen late night). If the lympathic system can pull too few water away from the lungs at night this could help explain the very poor breathing. Night sweating could help here by removing excess interstitial water close to the skin and hence offloading the lympathic system so that it can draw more water away from, amongst others, the lungs.
I found an article describing what you are talking about. This article gives several examples of sterile inflammation. It also links it to autoimmune issues. And in light of this particular subject (POTS) reperfusion issues as a possible connection. (We talked about this on another site – mostly POTS people). Makes sense that this could possibly cause unexplained neuropathies.
My POTS doc, 10 years ago, always felt there were mitochondrial issues – but testing wasn’t there/refined to prove it.
http://www.jimmunol.org/content/191/6/2857
Many of us have MCAS, CIRS and Lyme – all triggers inflammation.
Issie
everybody that comments always sounds so intelligent, it really makes me nervous 2 join in because of the rapid fatiguing neurocognitive situation. I have to use speech to text and I see it putting mistakes on the screen which I have to ignore. Please excuse the things that are spelled and worded incorrectly.
I was really interested in this article you wrote on pots because tachycardia and orthostatic intolerance affects several members of my immediate family including myself. But I’m old enough to have been diagnosed before the idea of pots ever came around. so the diagnosis were separate. I was hospitalized from tachycardia when I was 14 years old. It was horrible. I remember that I couldn’t inhale. But I have two daughters that have it now, one outgrew it when she hit her thirties. I’m currently on what I think is a beta blocker to control my pulse, which it does a beautiful job of, but it makes my already low blood pressure even lower. and since I came down with me CFS my blood pressure is all over the board. every single time I have to go to the doctor it requires maximum effort as I am forced to a mostly bedridden status. I’m only able to get up to use the restroom and get something quick to eat or drink. When I say quick I mean it has to either be edible from the container, or be ready made for the microwave . I have trouble eating a lot of Fresh Foods because this rotten disease stole my teeth. I kept getting infections in my jaw and it was going up into the roots of my teeth killing them. It was horrible. but what’s worse is not being able to chew especially when you need something as natural as possible.
The pots issue in adolescence interested me greatly because my youngest has missed so much school since she was in the fifth grade and she is now entering her senior year of high school. what she’s missing school because of is orthostatic intolerance. Is post exertional and she always has a racing pulse, severe photophobia, blinding headache and extreme fatigue to the point of sleeping and sleeping and sleeping. She also experiences severe vertigo. For any that don’t realize this dizziness and vertigo are two different things. when you have vertigo the room is spinning around you. it has just mortified me to see my child staggering down the hallway running into the walls and then collapse on to me because she is too weak to stand up. I needed it documented because doctors were taking their sweet time since she seemed to recover in a couple of days. so I called an ambulance when she was 15 during the Staggering down the hallway collapsing into me incident. On a side note, I was needing to stay in bed at that time and I was very weak still am. I could barely hold her upright even with her trying to hang on to the counters well I tried to get her to a soft surface that I could get her feet up and her head down on. she actually couldn’t assist me and I was horrified to realize that I didn’t know if I could physically help my daughter make it to the couch. it made me really mad at the doctors though for allowing her to go through these things. When the ambulance got there my daughter was so pale it frightened me. she was actually cyanotic. the paramedic asked me if she was always that pale and I said no. and I kind of whispered that I never seen her lips like that either. I’m so they took her resting blood pressure. Then did the standing even though she had to be assisted with standing without actually holding her. kind of like she was a bopping bag and we were all standing around her so she could Ricochet off of us when she would fall in my direction to far. The paramedic looked at me after the second vitals were taken and told me they were transporting. I wasn’t frightened because I knew how sick she was and had been but still it’s it’s a validation that you really don’t want to have. you want everything to be okay but if it’s not I knew I needed that documented and I needed her to be in the hospital so they could also document it. she still isn’t receiving any treatment for it.
She has had doctors that want her on an IEP at school since she started sixth grade. these incidents happened so frequently they really affect her attendance. The junior high and the high school have refused to give her an IEP. this year they turned her in as a truant for frequent absences even though they were excused by doctor’s note every time. It’s infuriating and I’m too sick to go after them legally. But my little girl who has to come home and take a nap everyday after school at the age of 17 is being treated like a juvenile delinquent for being ill. she can actually be put in juvenile detention if she misses any more school doctor’s note or not. and the woman that is in charge of our case doesn’t care if she has any medical issues. She talks to her like she is not being responsible by not being at school when she is ill. I will be so glad when she finally graduates for her sake. Having this illness that I have has done her a great disservice as I have very little of a support system and I just had to be affected cognitively with the rapid fatiguing so that I can’t organize paperwork or my thoughts. and when I try to speak they do a really good job of trying to divert the subject several times waiting for me to fatigue and they always win because of this stupid me CFS. it’s quite abusive.
I’m actually very very worried that her orthostatic intolerance paired with the tachycardia and always being post exertional, with exertional now meaning just a day at school, coupled with her irritable bowel syndrome and a horrible memory issues and difficulty concentrating which I hear about all the time from the teachers, and I deal with trying to teach her how to do normal things or give her a certain set of instructions just to watch her not remember what I said instantly… I’m scared to death She’s Got Me CFS. The Pediatric form. I didn’t realize it we could present differently then the adult form does. so I really didn’t think that she had it, I didn’t think children and adolescents could get it. and then I saw this horrible title to a paper that have the word pediatric included with me CFS and I thought I have to read it since I have it in case research finds out things that might affect my grown children or my younger child down the line by just being my kids. and the symptoms was like what my daughter’s been going through since she was 10 years old.
I’m curious if there’s a way to treat the pots if pots is indeed what she has. And I’m curious if it combined with her other symptoms equals pediatric or adolescence me CFS. Because I can’t get our doctor to even read the cdc’s site with the updates on it regarding me CFS. I can’t imagine her getting a diagnosis and the doctor that diagnosed me is retired. I feel like my child has a big struggle ahead of her because of the very unfriendly landscape we’ve already met with. and if anybody tried tough love on her I’d have to come unglued because she has used tough-love on herself and made herself so sick at the beginning of every single school year since 6th grade. she does not want to be like this. she has always been extremely active and she hates how little she’s able to do in order to avoid an episode as we call it.
She’ll be 18 in a few months and she wants to go to the local College and work and move out and be independent. I want that for her too but I don’t see it happening anytime soon. I don’t say that to her though. she’s dealing with enough depression and anxiety as it is. and I am no help whatsoever. there’s no dad that cares and I was dumped in 2006 when I got sick with me CFS. I was told they were too young to be somebody’s caregiver and they deserve better. I’ve been alone ever since. just me and my little girl. and she hasn’t had a mom that can even cook a meal since she was 5 years old. It’s horrible! I hope this landscape changes soon so that I don’t have to see my child go through what I’ve been put through. she’s already been put through enough despite being stuck with me for a parent let alone all of the health issues she’s been experiencing along with the accusations of being a rotten kid for something she has no control over from teachers that she used to love so much. I think enough said. if it’s something could help her with the orthostatic intolerance and tachycardia it would be a good thing.
Maschelle,
I am so sorry to hear that you and your daughter are going through this horrible situation. I sympathize with your feeling like you can’t do anything to help. I was bedridden with ME/CFS for much of my children’s lives so I have a good taste of how you are feeling.
It is so unfair that people are treating you and your daughter this way. I am concerned that the fact that they are pushing her will make her health that much worse and cause permanent damage.
Are you living in the U.S.? If so, have you considered K12 online public school? Perhaps it could help her conserve energy by not having to get ready for school and ride the bus, etc. She could even do schoolwork from bed if necessary.
I’m sure your daughter loves you very much and fully understands the extreme lengths you go to to try to help her If she doesn’t fully understand now, she will as she gets older. Please don’t say that she is “stuck” with you. Yes, your health makes life much harder for her than it does most of her friends, but you clearly prioritize her needs above your own and I am sure she knows that, and that means a great deal to her. I’ll be willing to bet that she wouldn’t trade you for anyone else.
We adopted my twin daughters when they were 8 years old, one of who has special needs. I was in good health for the first two years they were with us before I became bedridden with ME/CFS. Their birth parents had prioritized alcohol over the needs of their children. As adults they have said they are glad to have me as a mom in spite of my inability to do the “mom things” like cook a meal or go to the mall etc. My daughter without special needs has told me time and again how glad she is to have been adopted into our family and to have me for a mom. I love them and they love me and that is what matters the most.
This illness may take away most of the things we can DO but it can’t take away who we ARE on the inside.
So sorry to hear of your family issues. Some of us just have the bad genetics and/or epigenetic changes from triggers.
For your daughters orthostatic issues – most of us find compression to help. Some wear full body with support hose, Spanx or abdominal binders. Some find compression socks to help. (I get mine from Dr Leonards and find them to work as well as RX ones.) I get a neoprene abdominal exercise belt and wrap it tight around my middle. (Be sure to wear a thin shirt underneath.) Those things help a good many of us. Make sure to hydrate properly.
There are several websites for POTS people who need to explore and learn. A place to ask questions and not feel so alone. Just knowing others have same symptoms helps. There used to be younger ones on the site too. (DINET) (Been awhile since I was on there.)
Dr Grubb had a site for really young ones. There was good info there. Also some cards that can be printed and given to others describing the complexity of POTS and it’s symptoms. (I haven’t looked there in awhile either.)
There are many blog sites.
Issie
Thank you so much, Cort!
@Maschelle – never hesitate to comment or feel that you can’t talk with those who may be further along in their journey and may have more knowledge on certain things. We all had to start at the beginning and it took a while to learn and discover what we have up until now. Science is always changing and hopefully our research and digging for answers helps that along. When I first started learning, I had to look up so many words to get even a small understanding of what was being said. I intentially talked to those who were way over my head with their comments. I’m very grateful to many for what I’ve learned.
Issie
Here’s Dr Grubbs site and where the Awareness Postcards are. These are good to have with you for doctors, friends and others who may also have POTS. This helps get awareness out and helps others understand what you may be dealing with.
https://www.dynainc.org/resources/brochure
Issie
Cort, do you have the reference for the article for treating POTS with Mestinon? I searched Pubmed and could only find a case study (in Turkish!). I did limit the search to 2013-2014. Thanks!
Singer W, et al. Acetylcholinesterase inhibition in patients with orthostatic intolerance. J Clin Neurophysiol 2006;23:477-82. • Filler G, et al. Pharmacokinetics of pyridostigmine in a child with postural tachycardia syndrome. Pediatrics 2006;118:e1563-8. • Raj SR, et al. Acetylcholinesterase inhibition improves tachycardia in postural tachycardia syndrome. Circulation 2005;111:2734-40.
Here’s a couple I found in a Rowe paper on med used.
Just a personal note – this one can cause anxiety. It did with me. Was actually one of the worst things I tried. But I know of others that it helped. I couldn’t use middodrine either. I don’t need to vasoconstrict as some do.
Issie
Thanks, Cort, for the wealth of information you provide. It is tremendously helpful and has been a beacon of hope throughout my struggles with ME.
After reading your post, and equipped with the appropriate literature, I requested Mestinon from my doctor to reduce my POTS symptoms. He’d never heard of it, but eventually agreed after researching for himself. I’ve been taking it for over a week. I reduced my dosage to 15mg every morning after experiencing some unwanted side effects the first day, but it has otherwise resulted in significant improvements. I’ve been able to get out of the house and participate in activities that others would consider mundane and a hassle, like grocery shopping and standing in a checkout line – no blackouts, no crouching on the floor, and no need for a cane or wheelchair. Yesterday, I even mustered up the courage to take a short canoe ride (with help, of course) and swim in the lake – something I never expected to be able to do again. Without Mestinon, attempting these activities would’ve caused seizures and severe PEM for weeks. I’ve been taking frequent breaks to avoid overexertion, and have remained quite cautious, but I’m hopeful that this drug can improve the quality of life for me and other POTS sufferers.
Cort, I can’t thank you enough for your continuous coverage of the latest findings in ME/CFS/FM/POTS research and for bringing potential treatments, like Mestinon, to our attention.
Hi everyone,
I am just learning about POTS and would love to introduce my product as a solution. My name is Russell Broere and I am the Account Manager for LiquidIV. We have been working with doctors on the West Coast to help replenish the body’s electrolytes in patients with this disorder. We have received tremendous feedback from people with POTS and if you are interested in free samples to see how it may help you, please do not hesitate to reach out to myself, russell@liquid-iv.com, or check out our website. Liquid-iv.com and use promo code (POTS30) for 30% off at checkout.
I hope this can bring some comfort to those with this disorder.
All the best,
Russell Broere
I had chronic fatigue (moderate level) for several years and POTS for the latter few years of it. My health was slowly improving except for the POTS (I had to cook in my office chair and basically lie around like a dog). Mestinon was no good for me. I tried Low Dose Naltrexone and within a week the POTS was improving. It didn’t help me sleep but I wasn’t sleeping anyway, so I persisted with it. It really turned the corner for me and several months later I walked up a steep mountain with no PEM. I stopped the medication after about 9 months and the symptoms didn’t return, other than my usual low blood pressure and I now sleep a bit better after a few more years.
Congratulations Linda! On a scale of 1-10 with 10 being perfectly healthy where would you say you are now?
Thank you for taking the time do this. It is so important to many.
Emphatically yes to both your Qs, Kimberly. Neuropathies are common too w/ Systemic Mast Cell Disorders absent Ehler-Dahlos — incl SM.
Mast cell mediators include substances like leukotrienes that are synthesized OUTSIDE MCs –not merely substances carried, released from w/in MCs. I’m aware of no reason, and see none here, to discuss mediator afflictions in MCAS as different from clinically identical mediator afflictions in SM. As the Vanderbilt pioneers documented decades ago.
Stanford’s leading Anaphylaxis expert underscored at the 2004 Novartis Foundation Symposium hat we can never definitively rule out allergy.
Why this bias against clinical diagnosis? Science involves putting matters to the test, so to speak. When experts did this from collection, analysis of much data on Anaphylaxis, they found the testing now reserved for MCAS to be vastly inferior: way less reliable, largely inapplicable/inaccessible — compared w/ their since “verified” consensus clinical criteria embraced by the WAO and many other Anaphylaxis experts.
Many of us do indeed have a rough time initially w/ oral cromolyn. Yet are able to adjust as we titrate up slowly — ultimately benefitting mightily. So too w/ ketotifen, Xolair. We don’t all adjust, however. Happily, I largely have w/ IVIG infusions for my autoimmune demyelinating polyneuropthy
I was diagnosed with “idiopathic” small fiber neuropathy with many POTS symptoms as well as sensory neuropathy symptoms. It turns out I had pernicious anemia all along, even though my B12 had never tested low! I’m anti-intrinsic factor antibody positive, and my SFN symptoms improved dramatically on weekly B12 injections.
Low dose doxypin and Pepcid AC has really helped my Long haul Covid symptoms such as Mast Cell Activation driven sleep issues and heartburn.
Thanks David. Good to hear about doxypin – I hope to try it soon.