

The RCCX hypothesis blog by Remy is the third in a series of blogs by Health Rising which highlight hypotheses produced by health care professionals which attempt to shed a new light on the chronic fatigue syndrome / fibromyalgia spectrum of diseases.
- What if ME/CFS is an Intelligent Process Gone Awry? – Veronica Mead
- Could Chronic Fatigue Syndrome (ME/CFS) Be a Chronic Form of Sepsis?
______________________________________________________________
Chronic illness is exploding in modern times. Many different causes and treatments have been proposed for these illnesses, but what if there were a common genetic thread linking them all together?
According to Sharon Meglathery, MD, who suffers from this disease constellation herself, that common genetic thread just might be found on the gene complex called RCCX. Combining her own personal experience and family history with her clinical experience working with patients, the RCCX theory of chronic illness was born.
What is RCCX?
RCCX is not your typical genetic “SNP”. In fact, this complex is completely ignored in the standard genetic testing done by companies like 23andme, which helps explain why these common gene mutations (up to 20% of the population) have escaped detection up until now.

Meglathery believes the mixing and matching of genes on the MHC complex, which affects the response to all sorts of stressors as well as the immune system and hormones, may play a role in ME/CFS, FM, EDS and other diseases.
RCCX is, instead, a complex of four different genes, located on the Major Histocompatibility Complex (MHC) region of chromosome 6. Variations in the RCCX complex may contribute to disease susceptibility.
The genes comprising the RCCX cluster code for enzymes and proteins which substantially influence responses to stressors and cell danger signaling. They also affect innate immune responses as well as synaptic and dendritic pruning in the brain, sex hormone levels, fluid and salt balance, and the integrity of the extracellular matrix (ECM).
The genes that make up the RCCX cluster are as follows:
- R = RP1 (also known as STK19)
- C = C4 (complement 4)
- C= CYP21A2 (steroid 21-hydroxylase)
- X = TNXB (tenascin-X)
Essentially, these genes make multiple copies of themselves, which are called copy number variations. They often behave as one unit with the genes deleted and duplicated together, instead of as four separate units. RCCX is the only place in the human genome where genes travel together in this way. Because of this, people can inherit two (or more) rare diseases simultaneously at a much higher rate than would be expected by chance.
The RCCX genes are very unstable and can mix and match, mutating often for evolutionary reasons. This mixing and matching creates family histories filled with the chronic illnesses that are associated with these genes. It is not at all unusual for a patient to have a sibling with one manifestation, a parent with another, and for their children to be affected as well. In fact, this family history pattern may be the biggest clue to detecting RCCX currently available.
These related disorders are wide ranging and variable and likely include the most common comorbidities with ME/CFS, including EDS, POTS, MCAS, fibromyalgia, limbic/sensory sensitivity, immunodeficiency, autoimmunity and autism.
The RCCX complex is theorized to confer an inherited susceptibility to ME/CFS due to the presence of homo- or heterozygous CYP21A2 mutations, with or without co-inheritance of a TNXB mutation, and also with or without a C4 mutation. These mutations may be mild or severe, creating the varying presentations and levels of illness seen clinically.
CYP21A2 Mutations
CYP21A2 mutations can explain many aspects of ME/CFS. It is not uncommon for this illness to begin with an acute stress, such as an infection, and then progress to changes in the endocrine, immunological and autonomic nervous systems.
Dr. Meglathery believes a “21-hydroxylase overwhelm” may play an important role in ME/CFS, FM, POTS and many other diseases
Stress causes the 21-hydroxylase enzyme, coded for by CYP21A2, to become “overwhelmed”. This would explain why there may be many different triggers for ME/CFS, rather than one specific trigger that is the same for everyone affected. Milder mutations may create a sort of stress “switch” whereupon the symptoms are not experienced until a certain threshold is reached.
It is known that carriers of CYP21A2 mutations prior to this overwhelm have an exaggerated stress response and low basal cortisol levels, and this likely creates PTSD wiring in the brain, with dysautonomia and elevated danger responses over time.
This theory also neatly ties in with Dr. Robert Naviaux’s work on the Cell Danger Response in chronic illness, as the mitochondria become stressed and enter into a dauer state.
Under conditions of prolonged stress, those with CYP21A2 mutations who make defective 21-hydroxylase must now make more than double the amount of a normal person in order to try to cope with the stress. This creates a vicious cycle of high cortisol levels during stress along with lower and lower basal cortisol until the 21-hydroxylase enzyme becomes overwhelmed and cortisol and aldosterone levels plummet. In response to the low basal cortisol, Cortisol Releasing Hormone (CRH) is increased, with all the associated negative symptoms of MCAS intolerance and sensitivities.
In addition, progesterone levels can, in time, go from being very low due to the exaggerated stress response to very high during enzyme overwhelm, and along with this, bioactive copper can possibly be depleted. With copper depletion, B vitamins may not methylate properly.
Inflammation and MCAS symptoms from CRH excess and immune dysregulation can cause brain fog and other symptoms, ultimately rendering the affected person increasingly intolerant of stress of any sort. Meglathery believes that much, but not all, of the dysautonomia experienced in ME/CFS and related conditions stems from the aberrant danger response caused by CYP21A2 mutations.
Essentially, Meglathery posits that CYP21A2 mutations can produce a brain that is wired to detect and respond to danger as a result of hormonal influences going all the way back to the womb. Over time, she believes that this “stress wiring” becomes more prominent. The popularity of brain retraining programs, like Gupta or DNRS that help to overcome a particularly large and reactive amygdala state, suggest that many ME/CFS patients have found this to be the case.
In addition, Ron Davis recently presented the hypothesis that people with ME/CFS symptoms are driven to try to “push through” stress, thus keeping the alarm system turned on. Both of these statements can potentially be explained by the CYP21A2 mutations and the RCCX complex associated personality profile.
However, nothing about the RCCX theory suggests a psychological illness as the cause of disease or CBT as a primary treatment. Stress can come from a wide variety of sources, be it physical, emotional or infectious.
TNXB Mutations
The TNXB gene codes for tenascin X, which is involved in the arrangement of collagen in the extracellular matrix. Mutations can lead to abnormal amounts of TGF-beta as well as signaling problems. TGF-beta abnormalities have been found to be associated with endometriosis and other inflammatory sclerotic conditions as well.
Joint hypermobility is associated with TNXB mutations, which sometimes may be severe enough to meet the criteria for Ehlers-Danlos Syndrome.
TNXB mutations can also profoundly affect the function of the Extracellular Matrix (ECM).
C4 Mutations
Mutations in C4, the second “C” in RCCX, also contribute to either autoimmunity or immune deficient states. Complement C4 mutations are the most common causes of immune deficiency. CYP21A2 mutations plus or minus C4 mutations may also serve to explain the “subsets” found by Peterson in his recent research.
C4 also has another interesting wrinkle; it carries an endogenous human retrovirus, HERV-K. The impact of these retroviruses is unclear. Some believe that they are protective, but others believe they are pathogenic and linked to many diseases, like ALS. Either way, the presence of the HERV-K retrovirus should be investigated further.
Testing
Genetic testing with SNP targeting will find only a few of the most common and severe mutations and will miss the rest of those affected by milder mutations. It’s not possible to look up RCCX on 23andme.
The RCCX gene module is easily sequenced, however. The problem lies in distinguishing the pseudogenes from the expressing genes. A highly sophisticated genetics lab will certainly someday be able to characterize these mutations and develop testing that can be used outside the research setting, but so far it is not available.
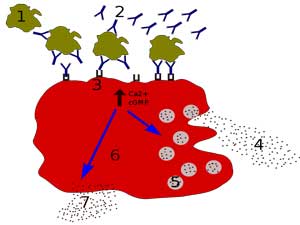
Meglathery believes the RCCX gene complex could be turning on mast cells, producing the mast cell activation syndrome (MCAS) seen in ME/CFS and other diseases.
Presently, clinicians can use a questionnaire, including a detailed extended family history looking for RCCX comorbidities, when seeing new patients. This may be especially useful for patients with hypermobile joints (though patients not being hypermobile does not necessarily rule out RCCX) to identify if the patient seems to fit the profile of a mutated RCCX cluster. Dr. Meglathery always does a physical examination, including a Beighton scale, on all new patients suspected of fitting the RCCX profile.
Dr. Meglathery feels that CRH and its receptors may hold the key to better managing this cluster of disorders. CRH turns on inflammatory pathways as well as mast cells and alters brain development in utero. It essentially turns stress into physical illness. Blocking these receptors or CRH release might prove to have beneficial effects on our population, which is also the hypothesis behind the recent study involving Cortene, a CRF2 agonist.
Measuring cortisol and other steroid hormones directly, unfortunately, is unlikely to be helpful in identifying problems with the RCCX complex. Changes in hormone levels are characterized by rapid and dramatic shifts that are unlikely to be caught at a single moment in time at testing.
Potential Treatment Avenues
At this time, treatment is very much focused on managing symptoms, just like those of us with ME/CFS already do. Since everyone will have different manifestations, the effective treatment will always be unique as well, but typically with some common ground.
Meglathery has found berberine helpful in her practice to decrease the high progesterone caused by the overwhelm at 21-hydroxylase, by shuttling progesterone to androgens and estrogens instead.
Antihistamines can help to treat the symptoms of excessive CRH release as well as other common MCAS medications like mast cell stabilizers. Treating MCAS, if it is present, is very important to lower the overall stress load on the body and stop the acute stress response which pushes 21-hydroxylase into overwhelm.
Hydrocortisone may be an option for treating low basal cortisol, with the caveat that it can exacerbate high cortisol states, lead to adrenal suppression and cause further hormonal derangement.
Polysaccharides like mannose or chitin or monosaccharides like n-acetylglucosamine may be helpful for proper function of the ECM. Treatment modalities such as acupuncture may also affect the ECM in beneficial ways.
For chronic immune deficiencies, IVIG may be useful (though difficult at this time to get approved by insurance). LDN may help as well.
Bio-available forms of copper may also be useful in the case of copper depletion. Meglathery has noted that some people with the presumed RCCX presentation in her practice do respond to bioactive forms of copper, like MitoSynergy, with increased energy, while others do not.
Stress management techniques, such as mindfulness or meditation, as well as trauma-releasing protocols like EMDR may also have value.
Potential Paradigm Shifting Theory
The RCCX complex theory demonstrates a complete paradigm shift in chronic illness that is very exciting. The RCCX complex is a way for researchers to explain the many various ways that chronic illness can present, and then ties them all together under one overarching genetic propensity umbrella.
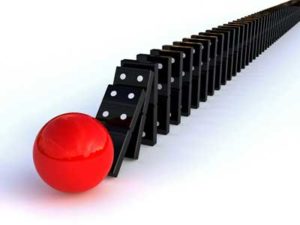
Meglathery’s hypothesis posits that meeting a biological stress threshold may tip people with ME/CFS and other disorders over into disease.
Dr. Meglathery first published her theory on her website in the spring of 2016. She was the first to talk about how meeting a biological stress threshold could send people into disease, rather than any one particular specific trigger. She also was the first to conceive of the idea of a specific associated personality profile, though recently both Naviaux and Davis have also discussed this idea in their talks.
The RCCX theory is also the only umbrella that explains the high rate of autoimmune/immune deficiency diseases and hypermobility within ME/CFS individuals and their families.
The OMF is currently doing a genetics/metabolomics study in collaboration with Naviaux exploring the novel hypothesis that Janet Dafoe has termed “haplogenetics”. In this study, they are exploring the idea that illness occurs in a situation called heterozygosity, which occurs when one copy of a gene (we carry two copies, one from each parent) doesn’t work properly, resulting in altered gene expression. But what if it isn’t just one gene, but the combination of all the genes in the RCCX cluster? Could this be the missing link we are looking for?
Recently, scientific studies have only served to add more weight to the possibility that the mutations in RCCX are, in fact, the common genetic thread linking us all in chronic disease. But, of course, only time, more research and adequate funding will tell the tale for sure.
For further information on this topic, please visit the RCCX website. You can also join the RCCX and Chronic Illness discussion group on Facebook created by Dr. Meglathery.






“Dr. Meglathery first published her website theory in the spring of 2016. She was the first to talk about how meeting a biological stress threshold could send people into disease, rather than any one particular specific trigger. She also was the first to conceive of the idea of a specific associated personality profile, though recently both Naviaux and Davis have also discussed this idea in their talks.”
————————————————-
Dr Erich Ryll of the 1975 Mercy Hospital outbreak was the first to tell me he thought the disease was from having passed a threshold of damage, rather than a particular pathogen.
However, Dr Ryll did not approve of the substance I told him about which was present in the original CFS cluster.
In fact, it really must have struck a chord, for merely mentioning it made him quite agitated.
Interesting. I think Cortene’s hypothesis also suggests that a neuroendocrinological threshold has been passed which it’s difficult to come back from.
Actually, although it does not focus on stress, per se, Gordon Broderick’s modeling work suggests that a new homeostatic set point has been reached in ME/CFS and GWS as well. The system has been pushed by a stressor such as an infection to a new suboptimal biological set point it has trouble getting out of. His and Dr. Klimas’s goal is to push the system back to normality. That brings to mind Dr. Cheney’s reporting that he can push the system towards health but that it often pulls back….
After putting up with CFS/ME for 45 years (20 before diagnosis) & more recently, with Vaso-vagal Syncope, and two auto-immune skin conditions; it’s such a relief that hypotheses & research like this are taking place at last… not, unfortunately, in the UK yet. I’d love to be part of a stem-cell reboot trial!
Still, in the meantime, here are a few suggestions for management strategies.
1) Weekly Vitamin B12 jabs, which change my sleep patterns (from ‘all-night-repeating-dreams’ to deep refreshing sleep). This comes on prescription along with weekly Folic Acid tablet.
2) Daily CoQ10 supplement for energy release.
3) Daily St John’s Wort supplement (natural Seratonin) for stress management.
4) Osteopathy for nuisance spinal inflamation.
5) Music and singing, for mindfulness and breath control.
…and a motto…
“Worrying is the least productive thing you can do”
Nell
Helen, I am convinced from my personal experience ( and being a typical CFS patient) that the spinal inflammation you mention is more than a nuisance. I have also been diagnosed with dysautonomia ( by a neurosurgeon) and have Vaso-vagaled during complex bladder studies where the table I was lying on was raised.
Recent experience : For 2 weeks have been absolutely miserable – completely bed ridden with severe fatigue and weakness yesterday. Went to my acupuncturist and asked him to please align my atlas- today. I got up off the table came home vacuumed, and spent 2 hours doing various house projects , then walked for a mile. Had a brief rest, got dinner, etc etc. Absolutely profound change just by getting my atlas better aligned.
Aligning the atlas is not always easy. I have had several traditional osteopaths who could not do it. And my acupuncturist is not always this successful. Plus, it won’t hold because my sacrum is still chronically unstable.
I appreciate that researchers are trying to sort out the metabolic and immune differences. But no one has stepped back to gain the perspective of how the entire musculoskeletal and central nervous system interconnect to allow healthy energy and function. ?
Thanks for following up on this one Remy, it’s an interesting theory.
Unfortunately, I can’t handle CoQ10, vit B12 or stimulants of any kind as they elevate my BP and pulse making me feel anxious…Am SO glad to hear that there’s hope for future generations, tho! This is the BEST explanation for these debilitating illnesses I have ever heard!
Look up an upper cervical
Chiro. It’s life changing
I would be interested in knowing what the personality profile is that seems to be indicative of this genetic mutation. Thanks, Remy, for covering this complicated research. Your article is very accessible.
Dr. Meglathery’s website is full of information on her complex and intriguing hypothesis. Talking about personality changes can be disturbing given efforts to categorize these disorders as behavioral disorders but I’ll be darned if this disease didn’t bring significant changes to me in the form of feeling wired, having a poor attention span, feeling anxious and having difficulty settling down, poor emotional resilience, being much more bothered by little things – things like that – all of which Sharon mentions.
Something has to account for that and I don’t mind biological explanations that attempt to do so. (One fibromyalgia study was just able to link cytokine elevations to changes in mood.) From Dr. Meglathery’s website – https://www.rccxandillness.com/cyp21a2-mutations-may-be-the-diathesis-in-the-stress-diathesis-model-for-chronic-medical-and-mental-illness-and-may-cause-a-psychiatric-spectrum-caps.html
“As mentioned above, the exaggerated response to stress (spiking cortisol) in infants with CYP21A2 mutations may also result in a brain wired for danger (CAPS) which is stress vulnerable, associated with dysautonomia and emotional dysregulation. With negative events, the exaggerated acute stress response (and perhaps epigenetic effects-see below) could facilitate the development of severe, PTSD-like brain wiring which worsens the dysautonomia and emotional dysregulation, further increasing the acute stress response. This can result in distressing dissociative (dysautonomic, sensory, motor) syndromes via brainstem/limbic system circuits as well as other psychiatric illnesses (predisposes to 4 of the major psychiatric illnesses: ADD, Anxiety Disorders, Mood Disorders, autistic features).”
Are Ron Davies and Janet Dafoe familiar with this theory? Just wondering if it would assist their current explorations. Cort
Ron – uber geneticist – would a great one to assess the hypothesis, that’s for sure. I’m pretty sure he knows of the general hypothesis but I don’t know what he thinks.
My children have hEDS. I have been studying EDS and noticed that each generation gets worse. I think there are environmental triggers that kick this into gear.
Gosh, how many hypotheses are out there? I am certainly losing counts.
I agree but this makes sense to me and I can imagine that an altered state of homeostasis as described would produce a systemic imbalance that could alter gut microbiome, blood pressure,hormones and almost every biological process. The stress could be viral or it could be trauma or any other trigger- or a combination. Perhaps in some cases it is the herpes virus- but not in every case. It would indeed explain ‘sub groups’-yet if the common denominator is the RCCX- perhaps we could all benefit from some sort of re-set. I find that anything that triggers a mild stress response puts my body and mind into a stressed state of overdrive followed by a dreadful crash. I hope Ron and his team may look further into this. Do you include them in your blogs Correct? Good luck with the Pridgen protocol by the way.
For me I wonder about the epigenetics of this. Even if its not possible to track how these genes move around together I would think you would be able to assess epigenetic changes.
That overdrive is very familiar…If you think of Whitney – that’s probably exactly what’s happening. Even small amounts of stimuli send his weakened system into overdrive.
🙂 We haven’t even covered them all! Dr. Theorharides just posted a paper suggested that ME/CFS is caused by mast cell activation in the hypothalamus. ( https://www.ncbi.nlm.nih.gov/pubmed/30076265 )
I guess it’s a good sign, though, that smart people are thinking about this disease.
What we really need is more research that will allow us to winnow down the number of possible hypotheses and (gulp) to allow new ones to come forth. Ron Davis, for instance, is more focused on data collection than hypothesis generation right now. In the end the data will tell all – we just need to collect enough of it.
Me, too. But what if a combination of all the theories is really the cause? Mind boggling, to say the least.
This is a very plausible hypothesis, thank you for posting, and explaining it so well.
“…along with this, bioactive copper can possibly be depleted. With copper depletion, B vitamins may not methylate properly…”
In Hair Tissue Mineral Analysis, I have always had depleted copper, and health practitioners have been anxious about the potential harmful effects of continuing to supplement copper, which is what I want to do, but apparently there are issues with this that practitioners have to be aware of. But maybe our condition is the one that needs ongoing copper supplementation.
I know years ago when I first started to experience issues that were an early warning sign, years before I finally had obviously-diagnosable FM, and I had a HTMA test that showed very low copper and iron as well as magnesium (also a chronic problem), the practitioner gave me very strong copper supplement (as well as iron and magnesium which I had been taking anyway). I never started “feeling better” so quick in my life, as when I started taking these supplements. In fact for a couple more years, I thought I was back to normal health and fitness.
But I think I can see now, the long trends of my condition and the inevitable decline, given chronic ongoing job stress; a Guardia infection and an operation were probably the things that finally tipped me into the “vicious circle” of effects in the body that is full FM.
I also think it very confirming that fluid and salt balance, and the integrity of the extracellular matrix (ECM) are implicated in this hypothesis. As followers of this blog will remember, I have concluded in recent years that FM pain and dysfunction is due to dehydration, toxicity of the intersticial fluids, and adhesions in the muscle fascia and loss of elasticity in the muscle fascia (and associated tissue such as tendons). The vicious circle that is FM, involves adhesions creating blockages, that hinder normal detoxifying processes (especially post-exercise), which then causes increased toxicity, which then causes more adhesions. I also think there may be biochemistry that results in involuntary and parasitic muscle tension; victims are unable to relax even with the most advanced training techniques. Certainly the stressful conditions that led to the development of FM, involved muscle tension that could have been “trained out”, but once the tipping point into the vicious circle has been passed, the tension is completely involuntary and unable to be ameliorated by “mind” techniques. This also exacerbates the development of adhesions in fascia.
I started thinking along these lines several years ago when a physiotherapist wrongly advised me to do muscle strengthening programs (the theory being that stronger muscles would more easily handle daily routines). The palpable manifestations of adhesions were increased significantly as a result, as my regular hands-on therapists could attest. I probably delayed the recovery I have since experienced, by several years, by this exacerbation of the condition; but then again, without this “mistake”, I may never have stumbled across the insights that led me to a beneficial protocol.
So interesting Phil. Dr. Meglathery’s hypothesis is the only one I can remember where copper comes into play. After talking to her it became clear that altered copper levels can have a dramatic effect.
I’m intrigued by this theory too. The emphasis and causation capture my symptoms quite well.
How much copper should we be taking? Is it necessary to have tests done before supplementing? I’m pretty much on my own here in the MidWest as I’ve never found ANYONE who knows anything about my condition! (I’d have to go to alternative practitioners who aren’t covered by our insurance, which I can’t really afford…Plus I’ve had bad reactions to quite a few “natural” supplements including herbs and vitamins, so am wary of trying anything new…)
I think Hair Tissue Mineral Analysis is a good guide. There are good liquid-form copper supplements available. I’d just go by the recommended dose with the supplement, and increase it slowly if HTMA shows continuing copper depletion.
My argument to practitioners who were worried about “taking too much copper” always was, then why is it not lifting the copper result in the HTMA? It does not surprise me at all now, if there is a hypothesis for copper depletion in my condition. I am going to experiment from now on, with copper dosage and see if I can get the HTMA result to increase.
I find it very interesting that Dr. Meglathery’s RCCX theory has popped up here. Several year ago she floated her original ideas on Inspire for the Ehlers-Danlos community where it received mixed reviews. She herself is not a geneticist although later she teamed up with one which seemed to give her explanations more credibility.
There is a sub-type of EDS called Tenascin-X whose variant sits just next to the genes which control part of the HPA axis. And this is where there can be a problem with CAH–or congenital adrenal hyperplasia as well. CAH presents very similar to PCOS. For a while EDS researchers were chasing people who presented with both, thinking that they would be quite common. Alas, they found a few, but not as many as hoped for–but a new category emerged “non-classical CAH.” Unfortunately, testing for the mutation for Tenascin-X is specialized and so they remain a small category in the EDS realm.
When Dr. Meglathery is talking about high progesterone caused by 21-hydroxylase, she is actually referring to some version of CAH.
Before coming across her theory, I suspected that I might have Tenascin-X EDS and could confirm this by testing for CAH, whether sub-clinical or full blown–because of their genetic proximity and influence. Testing for this is very involved. Alas, even though I have the PCOS like symptoms, I have no evidence of 21-hydroxylase problems.
So what to make of (at least part) of her theory? I certainly have problems with fatigue as does about 80% of people with EDS, but I seem to have failed the RXXC explanation…I do have some of her criteria, and not some of her criteria…
I do hope she is on to something…
So much research is needed…
Interesting remark about progesterone Nancy. I read over it.
You wrote “When Dr. Meglathery is talking about high progesterone caused by 21-hydroxylase…”.
In the blog I can find “In addition, progesterone levels can, in time, go from being very low due to the exaggerated stress response to very high during enzyme overwhelm, and along with this, bioactive copper can possibly be depleted.”
-> Would that be high progesterone in the long run of the disease after the initial phase? If so that would fit into some recent ideas I have. On her RCCX website I cannot even find the word progesterone with the in-page search so some confirmation would be nice.
Now what’s the link: https://en.wikipedia.org/wiki/CYP21A1 “Specifically, 21-hydroxylase converts progesterone and 17α-hydroxyprogesterone into 11-deoxycorticosterone and 11-deoxycortisol, respectively”
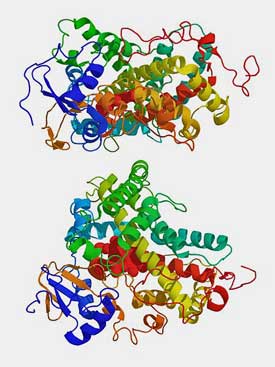
-> This needs/consumes 2 units of NADPH. See the first picture with NADPH above the arrows for the short explanation. It’s in fact indirect through needing 2 times cytochrome P450. This could be a biggy!!
* NADPH is the *only* way to regenerate glutathione from oxidized to reduced. It’s the body’s prime anti-oxidant.
* Glutathione (low in ME) itself regenerates a lot of other anti-oxidants, so those can’t make up for anti-oxidant shortness if glutathione recycling falters (or in the case of ME/FM/… can’t keep up with rampant ROS).
* Glutathione requires a high ratio reduced/oxidized (even lower in ME) in order to have good anti-oxidant properties. Simply supplementing reduced glutathione shortly increases this ratio but soon (risks to) trashes it as the newly supplemented glutathione gets oxidized. That is if the recycling ratio is insufficient and oxidized glutathione is not discarded out of the body or decomposed.
* Glutathione is also important for good folding of many proteins; bad protein folding causes inflammation/immune response and strongly reduces protein production if faulty protein folding rates are too high. As near all enzymes/hormones/cofactors are either proteins or depend on proteins for their production this could potentially slow down metabolism considerably.
* Good glutathione recycling requires the NADPH/NADP ratio to be *very* high. Therefore supplementing NADPH has even more short term effect and bigger chances to have opposite effects soon after then supplementing glutathione.
* NADPH recycling is done primely by converting glucose by the oxidative (aerobic) Pentose Phosphor Pathway (in non-keto diets). A second big supplier is turning the Krebbs cycle away from producing NADH/ATP and let it produce NADPH instead; two substeps of the Krebbs cycle can produce NADPH.
* People on a keto diet use less NADPH (no fat synthesis, see below) and ketones invoke altered gene expression producing far larger quantities of anti-oxidants then usual.
* Biggest consumers of NADPH: fat synthesis from glucose (or lengthening of the chain length of FA); recycling glutathione; producing respiratory bursts using NADPH to let immune cells produce very large quantities of peroxide (ROS) to try and kill pathogens, and to some extend cortisol production and it’s also somehow used for thyroid hormones (thyroid problems are found in a subpopulation of ME patients and some do restore to almost normal on supplementation) and for LDL (“bad cholesterol”) oxidation to arterial walls.
* having a strong immune or auto immune reaction consumes NADPH with a lever: once for producing ROS through respiratory burst and once by consuming glutathione to clear up the oxidative stress produced by the respiratory burst; this strong lever opens up many “common” routes from healty-ish to ME in both a sudden onset and gradual onset way. In fact, it fails to explain *very* few ways to enter this disease IMO.
* Creating ATP is a process that creates *strong* oxidative stress (it demands oxidation of fuel after all, in anaerobic process even more due to large oxygen debt)
* Because of previous, the ratio NADPH/NADH *has* to stay between certain limits. Too high nor too low is good. In case of ME/FM… too low is the problem. Then oxidative stress can get outrageously destructive.
* If NADPH (and NADPH/NADP ratio) falls too low there are only two viable answers long term to prevent heavy permanent damage:
A) turn up NADPH recycling
B) turn down NADH production
A) Means turning up the PPP. As it is far slower then glycolisis it’s best done through (strongly) turning down glycolisis (as seen in ME) impairing both anaerobic (very strongly) and aerobic metabolism (lesser as there are more fuel options); that of course next to upping the PPP itself.
A) Also means: increasing blood glucose (seen almost ubiquitously in ME) as higher blood glucose levels can speed up the PPP.
A) Also means: decreasing fat metabolism in order to allow for higher blood glucose and maximize base energy provided by PPP.
B) Means turning down strongly the Krebbs cycle in order to produce far less NADH/ATP; that leaves us (body and brain) depleted from energy.
A) Also means: turn as much of the already strongly downturned Krebbs cycle into producing NADPH rather then NADH/ATP, further depleting us from energy.
A) and B) Can also be achieved otherwise. If I recall well a recent hypothesis Cort published stated that, when NADH is too low and there are no other options, two NAD molecules can be used to create one NADH molecule. As this is a non-oxidative path IMO this is “OK” if NADPH is too low. This route increases the ratio NADH/NAD that helps metabolism (good) and increases the recycling rate as it is a wasteful way to recycle NAD to NADH. Two birds in one stone. Could happen every time after exhaustion (PEM) and every single night (non restorative sleep, long time needed in the morning to get up and running again). Both caused amongst others by low total NADH+NAD slowing metabolism plus requiring effort and resources to build new supply.
This could also account for high (nor-)adrenaline levels: they push up glucose levels significantly. As such they can push up the PPP and delay the moment NAD has to be wasted 2 to 1 to produce NADH. At least with me sharply rising adrenaline levels during exhaustion precede the start of a crash by minutes and sky rocket high adrenaline often occurs late night (causing wired/nasty sleep).
Side note: it also explains low NK cell activity. They lack the gunpowder (NADPH) to make bullets (respiratory burst/peroxide) to fight the pathogens. It’s like a big army with soldiers having 1 gun and 2 bullets each. They can barely defend themselves.
There is also a direct link between NADPH production and zinc deficiency and a yet ununderstood link between copper deficiency and lipid peroxidation https://www.ncbi.nlm.nih.gov/pubmed/3585543
So far, I found very few things contradicting with this hypothesis. I even see few things not been able to be explained by them in one way or the other.
Correction, I meant to say RCCX not RXXC! Brain sometimes does ‘loops’! 😉
This illness is ALPHA GAL no doubts now 100% it explains why we react to a tee with everything even smells trip us off…They contain ALPHA GAL ingredients from animals it is in everything & ALPHA GAL is an autoimmune disease
A new one to me. For those who don’t know Alpha Gal is allergy to me according to this Wikipedia site – https://en.wikipedia.org/wiki/Alpha-gal_allergy
Some interesting ideas, but parts of the treatment option appear backward to me.
The solution to high progesterone is not androgens, it’s increased conversion to allopregnanolone. This would significantly improves the circadian dysfunction and many symptoms. That said, this is much easier said than done, but simply supplementing allo or direct precursor significantly improved symptoms for me of many conditions I have regardless of progesterone. There may be a relative progesterone/allopregnanolone ratio involved as well (would consider separately, allo is big on its own).
Berberine is probably increasing stress pathways if it leads to higher estrogen. I would never take that for an extended time unless you found an extremely good biochemical reason with lab results or your personal results were truly phenomenal.
On paper this is interesting but I would be very wary of doing those treatments long-term.
Bioavailable copper is easy to get. Eat some beef or veal liver a few times a week for awhile. It feels like crap the day you consume it, but give it a month or two.
(Kinda forgot important tip, in case someone unaware actually tries this: Don’t eat liver if Vit D levels are poor; fix that with sun or UVB light first. Vit A in liver is substantial; but it doesn’t negate liver’s benefits in my opinion unless you’re already cornered. Probably the most important food or one of the best “supplements” you can try, at least once.)
FYI, someone linked a 2018 study suggesting it may be cannabinoids that can increase the Prog->Allo conversion endogenously:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6091574/
Some patients had reported benefits from cannabis or CBD oil already, but there would be chronic, dosage, and circadian issues involved in making this work properly (Allopregnanolone is majorly involved in circadian regulation, and you can probably screw it up doing it backward or abusing it, including tolerance).
This certainly IS a stress disease: to EVERYTHING! Sometimes I think it should be called “Chronic pain disease” not just chronic fatigue. Maybe “Chronic painful stress disease” would be more accurate. But thank you to everyone working on figuring out this conundrum that has eviscerated so many of us.
Studies indicate that pain is very, very common in ME/CFS – not quite a common as fatigue – but one of the most common symptoms.
What if the “driver” behind this illness came from EMFs? That is a steady source of stress because it never stops anywhere around the planet. I’d like to refer you to the work of Dr. Martin Pall, on that very subject. After studying intensely his contentions about the pathological process involved in every single miserable condition, I am convinced he has part of the picture. For me, any time the power goes out, I immediately become so much happier, less stressed and feeling better. That information is only anecdotal, of course, but his outline of the pathway for damage to mitochondria from massive influx of calcium into the cells with the accompanying enzymatic changes is very intriguing.
Dr. Shungu – who validated increased brain lactate levels in ME/CFS – believes Pall is on the right track as well.
I’m a bit confused as to why its stated that this cant be tested for. Why wouldn’t WES and looking at copy number be sufficient?