

“The dramatic response to therapy in this patient is remarkable and could help others who suffer from POTS and MCAS.” The authors
This, the fourth and last of a series of blogs featuring IVIG, and in this case other treatments, was sparked by attending the 2018 Dysautonomia Conference in Nashville, Tenn. It focuses on a case report of a severely ill POTS patient who improved dramatically using a combination of novel treatments – at least novel for most doctors. Whether you have POTS or not, this report is worth reading as it demonstrates the impact a knowledgeable and creative doctor who is willing to entertain non-traditional diagnoses and treatment methods can have on people with complex illnesses such as ME/CFS/FM and POTS.
Case Report
If a doctor wants to spread news of a better treatment approach, there are several things they can do. They can tell their colleagues or speak about it at a conference. Short of participating in a study, though, the best way to spark interest in it is to write up a case report and get it published.
That’s what happened here but this wasn’t your normal case report. Emblazoned across the top of every page of the case report, “Successful treatment of postural orthostatic tachycardia and mast cell activation syndromes using naltrexone, immunoglobulin and antibiotic treatment“,
were the words:
“Novel treatment (new drug/intervention; established drug/procedure in new situation)”
The authors didn’t only illuminate a novel treatment regimen: they applied it to two conditions that many doctors either don’t know about (POTS) or may not believe exists (mast cell activation syndrome (MCAS)).
Brent Goodman at the Mayo Clinic in Phoenix was the MD associated with this case. He’s been on a tear trying to educate other doctors about POTS and MCAS, and the education began early in the case report.
IBS or MCAS or POTS?
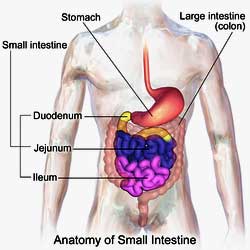
First, the authors noted that about 30% of POTS patients appear to have MCAS – a disease with similar symptoms. Then, they asserted that the gastrointestinal symptoms most doctors associate with irritable bowel syndrome (IBS) are instead being produced by mast cells in the gut or autoimmune antibodies that are messing with the autonomic nervous system, which impacts the gut. It turns out that the gut symptoms caused by mast cell activation (abdominal pain, bloating and abnormal bowel function) are identical to those found in IBS.
The authors also took exception to how most doctors treat POTS. Not enough focus, they asserted, is being paid to non-orthostatic (standing) issues such as the gut. Since POTS affects the autonomic nervous system, it makes sense that it would affect the gut as well, but that aspect of POTS has been mostly ignored.
A Tough Case
They took the hardest of cases – the ones doctors hate to see – to highlight their treatment approach. This woman, now 43 years of age, had desperately tried to get well, seeing 19 physicians in 16 years.
She had been a working professional (a biostatiscian) and self-described high achiever. Her path through the medical profession – which included multiple diagnoses but not much help – will be recognizable to many. So will the individual bootstrapping and research she did which ultimately led her to better health.
She first experienced signs of MCAS (flushing, itching, wheezing, and dizziness and nausea in response to certain foods) when she was 18. Doctors diagnosed her with rosacea and restless leg syndrome (RLS), and she received antibiotics, laser treatment, iron supplements and drugs like Ropinirole (which didn’t work). Her facial flushing improved but her other symptoms continued to worsen. By the time she turned 20 she was having gut problems (bloating/pain, constipation and foul-smelling stools) as well.
In her mid-twenties, she developed orthostatic intolerance, body pain, and weakness and edema in her legs, resulting in disability. Eventually her gut issues got bad enough to have her go on a liquid diet. Her dizziness led a cardiologist to refer her to a neurologist, who, thinking she had Lambert Eaton Myasthenic Syndrome (she did not), referred her to Mayo. In 2006, Mayo diagnosed her with “excessive venous compliance” but, remarkably, all they could recommend were compression stockings and a pysch evaluation! (No blood volume enhancers, no drugs – of the numerous ones available – no dietary recommendations, and they apparently didn’t give her a tilt table test…She declined the psych evaluation.)
Her health continued to plummet. Her thyroid (Hashimoto’s thyroiditis – an autoimmune disease) was the next to go, and then in 2010, three Doppler ultrasounds indicated she had chronic venous insufficiency. Instead of the blood flowing back up to her heart, the blood, when she stood up, flowed back down to her feet. She was having trouble sitting up, let alone standing.
Seeing a gastroenterologist for her gut issues in 2012 proved worthless, but in 2013 she made a discovery that changed her life. After receiving a boost from Claritin, an antihistamine, she diagnosed herself with mast cell activation syndrome (MCAS) and POTS (!). Then she referred herself to the Mayo Clinic in Phoenix, (apparently to Dr. Goodman, the expert in those diseases there), and her self-diagnosis was confirmed.
Using Mast Cell Blockers/Stabilizers to Assess if You Have MCAS
Dr. Jill Carnahan reports that the following over-the-counter drugs or supplements can block MCAS symptoms. If you experience MCAS symptoms and these make you feel better, it stands to reason that you may have MCAS. (Not responding to these treatments, on the other hand, does not mean that you don’t have MCAS.)
H1 blockers
- Diphenhydramine (Allergy Relief, Allermax, Banophen, Benadryl, Compoz Nighttime Sleep Aid, Nytol QuickCaps, PediaCare Children’s Allergy, Q-Dryl, QlearQuil Nightitme Allergy Relief, Simply Sleep, Sleepinal, Sominex, Tranquil, Twilite, Unisom Sleepgels Maximum Strength, Valu-Dryl, Vanamine PD, Z-Sleep, ZzzQuil and many others)
- Loratidine (Claritin, Claritin Liqui-Gels)
- Cetirizine (Zyrtec, All Day Allergy)
H2 Blockers
- Famotidine (Pepcid, Pepcid AC); Cimetidine (Tagamet, Tagamet HB); Ranitidine (Zantac)
Mast Cell Stabilizers
- Cromolyn, Ketotifen, Hyroxyurea
Natural anti-histamines and mast-cell stabilizers
- Ascorbic Acid, quercetin, Vitamin B6 (pyridoxal-5-phosphate), Omega-3 fatty acids (fish oil, krill oil), Alpha Lipoic Acid, N-acetylcysteine (NAC), Methylation donors (SAMe, B12, methyl-folate, riboflavin)
It was not apparently until she met up with Dr. Brent Goodman in 2103 in the Phoenix Mayo CLinic that someone thought to measure her heart rate while standing. A doubling of her heart rate (from 80-160 bpm) within 10 minutes of standing suggested POTS. She also experienced a facial rash, edema, blue hands and Terry’s fingernails and dermatographism (hives).
Terry’s fingernails or Terry’s nails appear white with a ground glass appearance and are missing the lunula – the white crescent shape usually seen on the bottom of the nail. Most of the nail appears white except for a narrow pink band at the tip.
The color changes are believed to result from a decrease in vascularity and an increase in connective tissue in the nail. This commonly occurs in diabetes mellitus, hyperthyroidism, malnutrition, liver failure, and other systemic diseases. Terry’s nails may also reflect aging.
A tilt table test and blood samples confirmed a diagnosis of hyperadrenergic POTS (increase in heart rate >30 beats/min, rise in systolic blood pressure ≥10 mm Hg and serum norepinephrine level ≥600 pg/mL). Further testing revealed impaired sympathetic nervous system functioning in her feet plus low leukocytes, platelets, thyroid (T3 and T4) and elevated 24-hour urine leukotriene, creatinine and prostaglandin levels.
Interestingly, her 24-hour N-methylhistamine levels were normal. None of the other mast cell tests were mentioned. (Jill Carnahan mentions 7 possible MCAS tests)
Her only sign of autoimmunity was a positive antithyroid peroxidase antibody. None of the 19 other antibodies tested for, including Sjogren’s and lupus, were positive. Goodman gave her an MCAS diagnosis on the basis of her having 47 of 48 known MCAS symptoms as well as meeting other MCAS criteria.
- Check out the criteria for MCAS diagnosis here
She was also diagnosed with ”delayed pressure urticaria /angioedema” (DPU), which occurs when pressure applied to the skin is followed by swelling and pain. She was in a tough spot: her POTS left her unable to walk while her DPU left her unable to lie down without pain. The DPU diagnosis did have a silver lining, though; it was what convinced the insurance company to give her IVIG, which did her a world of good.
Treatment
Thyroid replacement stopped her restless leg syndrome (RLS) in its tracks, but a basketful of POTS treatments (midodrine, amphetamine, droxidopa, support stockings, high salt diet) and MCAS medications (cromolyn sodium, monteleukast, antihistamines (hydroxyzine and all over-the-counter H1 and H2 blockers) failed to provide benefits.
Ultra-low dose naltrexone (1 mg every night), however, improved her pain, mood, memory, sleep, flushing, food and odor sensitivities and tingling in her limbs.
IVIG 1.5 g/kg (Privigen) and 125 mg methylprednisolone given once a month had a tremendous effect. Within a week of her first infusion, her fainting, tinnitus, anal outlet disorder and vascular spasms stopped. Her now normal capillary refill time (>1 min before IVIG; <2 seconds after it) indicated her cardiovascular system was responding. (Capillary refill time is the time it takes for the color of the soft pad of a finger or fingernail to return to normal after pressing on it until it appears white.)
Next, a lactulose breath test indicated she was exhaling hydrogen gas and therefore had small intestine bacterial overgrowth (SIBO). (Humans don’t produce hydrogen gas – only bacteria do.)
Rifaximin (550 mg 3 x’s day) for two weeks in combination with a low sulfate/sulfide diet completely eliminated the bloating, abdominal pain, constipation and foul gas she’d experienced after eating for decades. Her LDN was also increased. She was rewarded with another 25% decrease in POTS symptoms and a 43% decrease in MCAS symptoms.
Check out another remarkable Rifaxamin success story below.
The next two IVIG infusions further reduced her body pain, weakness, vertigo, ability to eat and facial changes. Then she reached a plateau; further infusions had no effect.
After 10 IVIG treatments, a tilt table test found that her POTS was completely gone. She needs to stay on the IVIG: without an infusion at least every five weeks, she starts to decline. The doctors aren’t done with her yet. At the time of the publication, they stated that they plan to continue the LDN and IVIG and add new mast cell treatments in the future.
The patient reported:
I feel like I won the lottery last year by discovering LDN, IVIG and SIBO treatment. LDN made me feel noticeably happier, more energetic, in less pain and with better digestion (and these things got better with each dose increase). IVIG was an absolute miracle and within a week gave me a life back, with a huge improvement of numerous symptoms, most importantly fainting, nerve pain and delayed pressure angioedema.
But I still had daily crippling stomach aches and more gas than a field of Holsteins until I took the rifaximin. I can’t believe I went decades feeling so bad when I only needed 2 weeks of antibiotics and a low-sulfur diet!
Now I’m back to standing, eating, sleeping, working, living and feeling exceptionally lucky.
The doctors believe that mast cell activation – not autoimmunity – was most likely driving her hyperadrenergic POTS. They proposed that mast cells activating near autonomic nerves were tweaking her sympathetic nervous system – a similar idea to Van Elzakker’s proposal that localized infections or inflammation near the vagus nerve is driving ME/CFS patients’ symptoms. It’s also not far from Dr. Pridgen’s hypothesis that a herpes simplex virus infection in multiple parts of the body is doing the same.
The authors reported that their case report established a number of firsts:
- the first time IVIG has been shown to lead to significant and sustained improvements in mast cell activation syndrome (MCAS).
- the first reported case of LDN improving POTS and MCAS symptoms.
They hypothesized that the sustained sympathetic activity caused by mast cell activation suppressed the peristalsis in her gut – the wave-like activity that pushes the contents of the gut canal forward. That “dead gut” then led to bacterial overgrowth, SIBO and leaky gut. The leaky gut then further tweaked her mast cells.
They believe the elimination of her SIBO and thus her leaky gut probably helped reduce her mast cell activation. In fact, they held out the possibility that her SIBO and the subsequent leakage of gut materials into her blood stream may have sparked the mast cell activation in the first place.
The POTS Gut Group
Goodman has made it his job to raise awareness around the gut issues in POTS. He reported he’d successfully treated 50 POTS patients with Sjogren’s Syndrome (SS) with IVIG and that IVIG had been dramatically successful in resolving the severe gut problems of another POTS/MCAS patient who had been to the emergency room over 250 times in 15 years for severe abdominal pain and diarrhea.
IVIG can be very helpful but noting how expensive and hard to get IVIG is, the authors emphasized how helpful LDN – an inexpensive drug seldom used in gut issues and POTS – and antibiotics can be in these diseases. Of 11 patients trying LDN, almost 80% reported an improvement in their gut symptoms. After one patient stopped LDN, his problems with standing, body pain, itching (pruritis), hair loss (alopecia), GI symptoms and fatigue returned. These symptoms subsequently subsided after he went back on the LDN.
Goodman also found high rates of SIBO in his patients with gut issues. A chart review of 33 POTS patients with gastrointestinal issues indicated that almost 70% tested positive on the lactulose breath test. Antibiotics improved the GI symptoms in 2/3rds of the patients given them (10/15). (If methane and hydrogen sulfide were present, neomycin was added to the Rifaxamin.)
The Group’s Takeaways
- POTS and MCAS can produce a wide variety of symptoms. Physicians should be aware of that and be open to diagnosing these illnesses.
- POTS does not just cause problems standing. It can also cause severe problems with gut motility, leading to IBS and small intestinal bacterial overgrowth (SIBO). If antibiotic therapy works in POTS, and then the patient relapses, consider that POTS-induced gut motility problems may be present.
- Given the fact that treatments for hyperadrenergic POTS are often not particularly successful, more doctors should consider MCAS treatments in this group.
- Combination therapy (IVIG, LDN) should be attempted.
- If SIBO is present, attempt antibiotic therapy.
Health Rising’s Takeway
- Keep up on the research, keep exploring treatments and find a good doctor! This person self-diagnosed her MCAS and then made her way to a good doctor. That was what made the difference for her.
Your Support Is Needed
Health Rising’s East coast trip provided a gold mine of information, inspiring a wealth of articles. including the one you just read. Upcoming articles from the trip include Dr. Klimas’s exercise study, a possible new treatment for fibromyalgia, talks with Jarred Younger, Avindra Nath, Dr. Pridgen and – on the return home – the folks at the Bateman-Horne Center. Next up on the travel agenda is the Stanford Symposium. Travel provides many opportunities but travel to the East Coast, in particular, is expensive for a small organization like Health Rising which still hasn’t even begun to recoup its trip costs. If you find conference reports and other travel related blogs helpful and want to see these in the future, please support Health Rising.
Articles From the East Coast Trip
The IVIG Series
- An IVIG Chronic Fatigue Syndrome (ME/CFS) / POTS Treatment Success Story: IVIG#1
- Are Chronic Fatigue Syndrome, POTS and Fibromyalgia Autoimmune Dysautonomias? IVIG #2
- The Case for IVIG Treatment in Chronic Fatigue Syndrome (ME/CFS), Fibromyalgia, Small Fiber Neuropathy, and POTS: IVIG#3
- Winning the Lottery: “Novel” Treatments Return Severely Ill POTS Patient to Near Health: IVIG #4
Advocacy
From the Dysautonomia Conference
- 2018 Dysautonomia International Conference I: Small Fiber Neuropathy, POTS, MCAS and Vagus Nerve Stimulation
- The 2018 Dysautonomia Conference Pt. II: Could You Have a Spinal Fluid Leak? An ME/CFS, POTS, FM Perspective
- Dysautonomia International Conference Pt III: The Autoimmunity Revolution in POTS
- “Sticky Blood” – Antiphospholipid Syndrome, POTS, Chronic Fatigue Syndrome and Fibromyalgia – The Dysautonomia Conference #4
- Stagnant Hypoxia – Where Chronic Fatigue Syndrome and Hyperadrenergic POTS Meet?
- Promise Fulfilled – A New Chronic Fatigue Syndrome / Fibromyalgia Practitioner Steps Forth









Thank you so much, Cort, for doing this series on IVIG. Like the patient in this article, IVIG also put my MCAS and Autoimmune POTS into remission. Also like her, I received a diagnosis of LEMS and I also have Hashimoto’s Disease. I even had “Terry’s Nails” for several years, and was told it was due to autoimmunity but this also did not go away until I got IVIG.
In my case, I do have the LEMS autoantibody, and most likely have an atypical form of LEMS, b/c of additional symptoms (severe muscle and breathing weakness). In my case, I also did Rituximab in addition to IVIG but my MCAS went into remission from IVIG alone (before we added Rituximab). But the LEMS, muscle weakness, POTS, etc, did not go into remission until we had the right combo of IVIG & Rituximab.
Unlike the patient in your article, I did not have gut problems, but we are similar in many so other ways. I am now almost at pre-illness levels and can breathe, stand, walk, drive, etc, with no limitations after using a wheelchair for almost four years. I was given a “CFS” diagnosis by multiple doctors in the US in 2013 and told that there was “No treatment”. Luckily, I kept searching until I found my incredible doctor, and later my amazing MCAS specialist, who both fought for me to get proper testing and treatment.
My MCAS, Autoimmune POTS, muscle and breathing weakness, and all the issues that rendered me completely disabled are now gone (hopefully forever but we do not yet know). Thank you for spreading the word about IVIG, it is a life-altering treatment for many people.
Wow… What a story Gingergrrl – a story of persistence and ultimately success – and it took IVIG and Rituximab; that’s why good creative doctor’s who are willing to have patience and try different things is so crucial. We need people who will stick with us.
I was really struck by the fact that none of the POTS therapies worked for this person – presumably because it was mast cell activation all the time… MCAS is something we all need to learn about now.
Thanks again, Cort, and I agree with you that once more doctors are aware of Autoimmune POTS and MCAS, then IVIG will no longer be considered a novel treatment (although it won’t change the insurance companies not wanting to authorize it in the US).
I also wanted to clarify that there are two POTS meds that did help me (atenolol & midodrine) but they were minor symptom relief and did not get to the underlying cause, allow me to walk without wheelchair, or get my life back like IVIG & Rituximab did. But they did stop my HR from going into the 160’s and 170’s all throughout the day and were beneficial in my case.
Thanks for spreading the news on more treatments that helped.
I had never heard of “Terry Nails” before this and I wonder how many people have it. To my dismay it appears that I do. I have no lanula’s hardly at all, and whitened nails with a red band at top. 🙁
I may have commented on this before. If so, please accept this redundancy. Be very careful with trying the regimen for mast cell activation syndrome. In my case, these medications triggered narrow angle glaucoma which led to a requirement for laser surgery.
This is scary. Did you also find symptom relief?
can you send the contact of your doctors to me? i would like to treat my mcas with them
can you share the contact details of your doctors? I would love to deal with them
what is the name of your doctor?
Claritin is also a major medicine in Alpha-Gal IgE Meat Allergy
Also, the downfall with Claritin is it also contains Alpha Gal ingredients like lactose, magnesium stearate & not sure if Animal source but Vegans say it is not VEGAN
Could you tell me the medical journal which published this? I have a cousin with POTS whose physician husband could probably push hard enough for her to receive the IVIG.
It was in BMJ.
Weinstock LB, Brook JB, Myers TL, et al. BMJ Case Rep Published Online First: 2018. doi:10.1136/bcr-2017-221405
I, too, have MCAS and hyperadrenergic POTS, and my doctor started me on .75g/kg/month IVIG a year ago (which he increased 3 months ago to 1.5g/kg/month) with POTS meds (propranolol and Mestinon) and MCAS meds (Benadryl, ketotifen, cromolyn sodium, curcumin, and quercetin, along with LDN.
My doctors found this case study in January, and I was excited to see that I was already on a very similar protocol to the one which helped this patient. I’m not cured, but it has definitely helped my symptoms.
Thanks for posting, Cort!
Glad to hear it. I don’t know why more doctors don’t take the time to do case reports – they are so helpful in spreading the news.
There is a link to the article in the blog. Thankfully you can download this case report for free.
Thank you so much for this article, Cort. It is the most helpful article I have come across so far. It has taken a long time to educate myself — with the help of this website of course 🙂 — but the puzzle is gradually becoming complete. This POTS/MCAS subset is me, albeit in a less extreme form. While I may not have access to treatment yet, because doctors in Belgium don’t take these illnesses seriously at all, I have hope that I can improve by continuing to look for natural alternatives. I have already dug up a couple of studies which say that herbal preparations are just as effective as Rifaximin in eliminating SIBO, so I guess that would be a good place to start!
Those herbal studies were amazing…
Cheaper, Safer, Better: the Herbal Approach To Small Intestinal Bacterial Overgrowth – https://www.healthrising.org/blog/2014/06/25/cheaper-safer-better-herbal-approach-small-intestinal-bacterial-overgrowth/
Good luck!
I have ME/CFS and have suffered from IBS for as long as I can remember. 10 years ago I began taking a probiotic with little improvement, still constipated. On a recent visit to Australia I purchased a local product boasting 64 billion ? per capsule. – PREMIUM probiotic strains, no added dairy, gluten or fructose and no refrigeration required. My gut immediately went into overdrive emitting loud noises, followed by pain and 3 or 4 visits to the toilet per day and sometimes during the night. Imagine my surprise. Can anyone offer a reason as to why this could have occurred?
Probiotics will often worsen symptoms for patients with SIBO, as they already have too many bacteria and they are also in the wrong places (the small bowel). There can be trillion bacteria per mL in the colon, however the small intestine is almost sterile by comparison, a few hundred to a few thousand per mL.
Compounding this problem are the archaea, specifically methanogens. They cause constipation by their production of methane (which slows bowel transit). However, they use hydrogen produced by the other bacteria, which effectively feed them what they need to produce methane. These organisms are NOT affected by antibiotics, however they are controlled by certain types of statins – lovastatin lactone in particular.
Enough hydrogen producing bacteria (what is basically in most probiotics) with an absence of methanogenic activity can cause diarrhea.
So either way, probiotics have been overblown as a solution to many digestive problems – and in reality the places where they are most effective is when there may be imbalances between types of gut bacteria or when exposed to unfamiliar bacteria during travel.
Methanogens ARE affected by antibiotics. Metronidazole, neomycim and possibly nitazoxanide. Not sure where you got the idea that they aren’t.
Lovastatin syn-010 is still in development. Taking a regular statin which is absorbed systemically is not a good idea, IMO.
hi Margaret,
I’ll take a very wild guess. Would you have happened to be severely constipated at the moment?
If so, maybe the transition from the food between the small bowel to the large bowel was blocked so much that the probiotics plus “trapped” food started working in the small intestine and developed too large quantities (in the small bowel where that is not supposed to happen IMO) before they “forced open” the blockade? So much gas production in the small volume of the small bowel could have an “explosive” result.
Don’t know if it is remotely possible, but if you ask an explanation for something weird, I can make up one ;-).
Now I come to think of it, this reasoning might help explain the current oscillating SIBO I have.
* Low bowel epithelial cell activity plus maybe some constrictions or rough scars or inflammation reduce movement speed in the small bowel a lot.
* The same in the large bowel may partly block the valve between both.
* Too much food remains for too long in the small bowel.
* Smallish amounts of bacteria in the small bowel start to multiply and increase both solid and gas volume a lot in a partly enclosed volume.
* Pain and bloating starts in the small bowel. If it is already weakened the extra pressure may cause damage and bleeding.
* A damaged small bowel allows undigested food and bacterial toxins to enter the blood stream and causes blood in the stool.
* A strong immune reactions occurs in the blood stream and in the bowel. One is energy depleted and immune exhausted and the body tries to flush the bowel.
* If one has fructose malabsorption then fructose enters the large bowel. There it dehydrates the large bowel and the body.
* This gives initial diarrhea followed by constipation due to combined dehydration and enough empty place to keep the smaller quantities of food present in the bowel.
* dehydrated feces block the transit from small to large bowel.
* rinse and repeat :-(.
Maybe replacing bread with dry rice crackers in order to correct my Fodmap issues was a poor choice… …even if they are full bran they are dry, have moderate amounts of fiber and little fat.
I had somewhat similar experience with probiotics. My ME/CFS symptoms began after taking a strong Theralac probiotic formula. I only took it for a week, but that was enough. My life has never been the same. I had what I would call conatipated diarrhea i.e. going to the bathroom multiple times a day, passing lots of conatipated stool. Basically, everything I ate would go out the other end, but without diarrhea. Never will I ever take them again.
I didn’t knew LDN did help with gut inflammation. http://www.lowdosenaltrexone.org/index.htm#What_is_low_dose_naltrexone gives very clear pictures on the efect on the gut before and after: convincing! And odd: LDN does “by mobilizing the natural defenses of one’s own immune system” strengthen the immune system rather then weaken like for example hydrocortisone does. And it does help with auto-immune diseases whilst strengthen the immune system. Atypical behavior to say the least.
What struck me most is that stopping LDN treatment did lead to quick return of gut inflammation. I made a link to “Moreover, breath H2S can track the precise evolution of SIBO, even after the eradication of bacterial overgrowth.” in https://www.healthrising.org/forums/threads/testing-for-sibo-small-intestinal-bacterial-overgrowth.6041/. The reason for that link is because I start to suspect I have H2S related SIBO. And it seems to be able to pop up again after longtime reduced IBS symptoms with a single diet mistake and stay longtime after that single mistake. To me that may indicate that H2S producing bacteria can come back very quickly after treatment stops. So I tried to search for links.
The first link I found was that both LDN and H2S seem to interact with the opioid receptors, but the case for the interaction between opioid receptors and H2S is not strong enough so I continued searching.
Best link I did find: cAMP:
* LDN has a strong link to the opioid receptor
* the opiod receptor has a strong link to cAMP https://en.wikipedia.org/wiki/Opioid_receptor
* H2S has a strong link to both the opioid receptor and cAMP “Hydrogen Sulfide Attenuates Opioid Dependence by Suppression of Adenylate Cyclase/cAMP Pathway” https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3880902/
* cAMP has a link to vasodilation https://en.wikipedia.org/wiki/Vasodilation (under vasodilation: “Adrenergic stimulation results in elevated levels of cAMP…”)
* cAMP has a link to heart contraction “PKA enzyme is also known as cAMP-dependent enzyme… …that promote muscle contraction in the heart” https://en.wikipedia.org/wiki/CAMP-dependent_pathway
* cAMP has a link to mast cell degradation and hystamine https://en.wikipedia.org/wiki/Mast_cell
All of the above have a strong link to issues in the blog. Just like with inflammation and auto-immunity, the effect of LDN on cAMP are counter-intuitive.
There are other links between cAMP and ME:
* cAMP related enzymes determine the conversion rate of glycogen into glucose, likely important in ME “PKA enzyme is also known as cAMP-dependent enzyme… …that convert glycogen into glucose” https://en.wikipedia.org/wiki/CAMP-dependent_pathway
* many of us are effected by caffeine in different ways: “caffeine and theophylline inhibit cAMP phosphodiesterase, which degrades cAMP – thus enabling higher levels of cAMP than would otherwise be had” https://en.wikipedia.org/wiki/CAMP-dependent_pathway
* Cyclic AMP is synthesized from ATP by adenylate cyclase” and “Liver adenylate cyclase responds more strongly to glucagon, and muscle adenylate cyclase responds more strongly to adrenaline.” and “It is also involved in the activation of protein kinases. In addition, cAMP binds to and regulates the function of ion channels” in https://en.wikipedia.org/wiki/Cyclic_adenosine_monophosphate
* The cAMP activation of protein kinases is important for “A protein kinase is a kinase enzyme that modifies other proteins by chemically adding phosphate groups to them (phosphorylation).” https://en.wikipedia.org/wiki/Protein_kinase and incorrect phosphorylation is a big thing in ME
* “Many different cell responses are mediated by cAMP; these include increase in heart rate, cortisol secretion, and breakdown of glycogen and fat. cAMP is essential for the maintenance of memory in the brain, relaxation in the heart, and water absorbed in the kidney.” in https://en.wikipedia.org/wiki/CAMP-dependent_pathway
It still are loose links between cAMP and ME but there seems to be to many to ignore. Considering the links I did find I’m a bit surprised the search for “cAMP ME/CFS” did not yield much.
I just read “cannabis for sleep” on the forum, seeing it works very well for sleeping and chemical sensitivities for some people so I did look up if there is a link to cAMP and yes, the search term “cannabinoid receptor cAMP” gives plenty of pages of relations and research between the cannabinoid receptor and cAMP.
Interesting! High THC cannabis in the form of candy works wonders for me with sleep.
Yes, I thought CBD was supposed to be the medical thing, but THC has some medical properties too it seems.
I found a complex scheme on cannabinoid receptor signaling here: https://www.wikipathways.org/index.php/Pathway:WP3869
If I understand it wright then THC acts only in one direction on cAMP via the CNR1 receptor, while with CBD it acts the same as THC on the CNR2 receptor but opposite on the CNR1 receptor concerning cAMP. So as discussed in the cannabis for sleep thread the composition in CBD and THC may indeed be important for its effects on patients if cAMP is important here.
Due to legal reasons and mainly it sticks long in the blood (driving under influence) it’s a no-go for me. And coffee’s effect on cAMP is not as spectacular so I looked for alternatives.
In the same scheme I did see that AEA (anandamide) has directly and arachidonic acid after conversion have the same effect as THC on the CNR1 receptor (probably not as strong, but comparable action).
Phosphatidylethanolcis made in the presence of alcohol and has a very long path from alcohol to some effect on the CNR1 receptor. Seems to inefficient given the drawbacks of alcohol in ME.
Arachidonic acid has pro- and anti-inflammatory properties but more of the pro under conditions of ROS and exercise. Does not seem ideal for us.
Anandamide seems an interesting one https://en.wikipedia.org/wiki/Anandamide:
“The name is taken from the Sanskrit word ananda, which means “joy, bliss, delight”
“Anandamide’s effects can occur in either the central or peripheral nervous system. These distinct effects are mediated primarily by CB1 cannabinoid receptors in the central nervous system, and CB2 cannabinoid receptors in the periphery.[6] The latter are mainly involved in functions of the immune system.”
“Anandamide inhibits human breast cancer cell proliferation.”
“Anandamide is found in chocolate together with two substances that might mimic the effects of anandamide, N-oleoylethanolamine and N-linoleoylethanolamine.”
=> So dark chocolate may have a somewhat similar effect as THC?
Note: I used to say chocolate is a medicine. But it has either of two effects on me: it helps me feel energized and clears my head or it pounds my stomach and takes my head down with it. Depends on some hard to determine conditions.
While I’m looking into cAMP: here is another nice one https://www.frontiersin.org/articles/10.3389/fimmu.2016.00123/full:
“The cAMP Pathway as Therapeutic Target in Autoimmune and Inflammatory Diseases”
“In the immune system, cyclic adenosine monophosphate (cAMP) is well established as a potent regulator of innate and adaptive immune cell functions. Therapeutic strategies to interrupt or enhance cAMP generation or effects have immunoregulatory potential in autoimmune and inflammatory disorders.”
Interesting! I have the same kind of dual reaction to caffeine and chocolate. I am shockingly sensitive to them – a few sips of tea are usually enough to send me flying, increasing my mental clarity and reducing my pain levels.
However, there are times – usually when I’m really tired – that they have the opposite effects – I get exhausted by them. I also used to very jittery and experience painful gut symptoms some hours after drinking coffee.
They can still make me jittery but the gut symptoms have completely stopped I believe; I’m much more tolerant to caffeine than I used to be – an indication that at least in some areas I’m doing better.
Digging deeper in https://www.frontiersin.org/articles/10.3389/fimmu.2016.00123/full (The cAMP Pathway as Therapeutic Target in Autoimmune and Inflammatory Diseases) I did found a few other interesting things:
“Within the immune system, cAMP regulates pro- and anti-inflammatory activities: drugs that elevate intracellular cAMP levels reduce the production of pro-inflammatory mediators and increase the production of anti-inflammatory factors in numerous immune cells.”
=> for ME patients more cAMP sounds good here
“Certain microbacteria and fungi have evolved to hijack the host cAMP axis by introducing microbial adenylyl and guanylyl cyclases (51) and by intoxicating the host cell with preformed cAMP or adenylate cyclase toxins (52–54).”
“Bordetella pertussis, for example, suppresses neutrophil extracellular trap (NET) formation by overwhelming leukocytes with supraphysiologic intracellular cAMP levels”
=> Suppressing NET formation is messing in a major way with innate immunity. NET formation is also important in capturing misfolded proteins, something likely important in ME.
Streptococcus (see recent blog on doctor having ME who improved after getting a Streptococcus vaccination) suis Adenosine Synthase Functions as an Effector in Evasion of PMN-mediated Innate Immunity modifies AMP (directly influences cAMP) and adeosine production directly to escape the immune system whilst surviving in the blood https://academic.oup.com/jid/article/210/1/35/2910567
“evidence strongly indicated that it can convert adenosine monophosphate (AMP) to adenosine”
“play an important role in S. suis 2 escaping human innate immunity in the context of inhibiting PMN’s activity by synthesis of adenosine”
I did find cAMP modulated behavior of Candida albicans (mold type associated with ME) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4601349/, Helicobacter pylori (stomach bacteria associated with subset ME) https://www.spandidos-publications.com/ijmm/7/6/625 and
Also of interest in ME:
“Natural killer (NK)… …Both pharmacological repression and induction of cAMP inhibit perforin-mediated and CD95 ligand-mediated target cell lysis”
=> Too much or too few cAMP reduces NK cell function. That’s a big thing in ME.
“B and T Cells
In addition to innate cell function, cAMP also controls numerous adaptive immune cell activities. In adaptive immune cells, cAMP is essentially required…”
=> Add this to previous comments and it seems to me that cAMP’s potential role in this disease could be huge. Moreover, depending on underlying problem/pathogen a ME patient may require more or less cAMP making treatment outcomes all over the place.
=> In my case the effect of chocolate (cAMP modifier) and to a lesser variation coffee seem to be most correlated to the effect on my stomach (amount of IBS-like symptoms I have when consuming those; my IBS-like symptoms vary a lot ranging from constipation over none to diarrhea). That may well coincide with the current amount of cAMP dependent/modifying stomach/gut bacteria and/or mold/yeast overgrowth.
=> I’d be more then interested if it could be looked into in relation to ME. Maybe it allows for better dividing individuals into subgroups and better targeting cAMP related treatment (more, less or time varying).
Chiming in on dual effect of dark chocolate: got the same. I now use dark chocolate as a digestive aids after a protein rich meal and it seems to help with keeping a clear head. But eating dark chocolate after a carbohydrate rich meal or empty (ish) stomach just knocks me out. Is this the case for you as well?
Hi Moira,
Dark choclolate puts me more often down when my stomach is in a hard to translate state. That state basically describes either having eaten the previous days too much or having some sort of minor infection affecting my stomach. It goes together with the feeling of a heavy head.
As I used to eat low fat it was often low protein too. But I like cheese a lot, so when having a big dish of some bread, some wine and a lot of cheese I was vulnerable too. Might just as well be one of my many newly discovered food intolerances at play too. Or the dried fruit going with it; dried fruit is bad when you are unaware of your fructose intolerance.
Having low caloric meals, which are mainly moderate carb, protein and fat helps me avoiding that state where chocolate puts me further down. For some reason, I’m less affected by chocolate since my health nosedived a few years ago.
Thank you for sharing dejurgen. From your story it seems that proteins help with getting a good effect (or at least with preventing a bad effect) from dark chocolate. I have no idea what the mechanism behind it would be. Maybe the effect of dark chocolate on stomach acid and histamine release in the stomach is involved. Interesting.
Unfortunately in the U.K. the nhs won’t consider or look at any of this. Private drs are expensive and doubtful they would either. None of the depts talk to each other or consider anything a little out of the box.
I’m sure it’s as hard as heck but it’s not impossible apparently. I was shocked to hear about this UK person’s successful IVIG trial.
https://www.healthrising.org/blog/2018/08/11/ivig-treatment-chronic-fatigue-syndrome-me-cfs-pots-success-story/
I’m going to make this as short and easy too read as possible.. Like the case study, I have a ton of these symptoms. This gives me hope! I was diagnosed with Irritable Bowl first then a diagnosis of Crohnes along with Ulcerative Colitis. I’ve had internal bleeding and severe pain in my intestines. I had several test for transit time.. I hold the hospital record for the slowest After 6 hrs for food too pass from stomach to intestine, they stopped the test. I’m positive for Lupus, RA, RSD and I’ve had symptoms of Chronic Fatigue and FMS since Childhood. I’ve known I have Sjogrens for 30 yrs. So much more..Now, I’m being tested for POTs.. I have been taking antihistamines for a couple years. I have a lot of congestion without and noticed they do make me feel better. It’s just been trial and error with all of this and overwhelming at times. I have tried IVIG. Only for a short period of time. There are pages of serious side effects and complications. For example, my first dose was given to me in under an hour! Which almost did me in. I was told my kidney’s could have shut down. I would advise anyone considering this treatment to do your research. Just be careful. I hope if I can get IVIG again that I’ll get a better result and hopefully my new Doctor can follow this regimen.
Some records you wish you didn’t hold! 🙂
Thanks for the warning! Check out this blog for the much slower dose times recommended by doctors who treat these disorders –
https://www.healthrising.org/blog/2018/09/13/ivig-chronic-fatigue-syndrome-pots-fibromyalgia/
Karen, my IVIG infusions were at an extremely slow speed (40) and took 7-8 hours but this not only decreases the risk of allergic reactions, it decreases the risk of blood clots, strokes, etc. I am horrified that they had you do the whole infusion in one hour and glad that you are okay!
Cort, thank you once again for sharing what you have learned. It’s so encouraging to know that others are having positive results, from treatment with IVIG/solumedrol. I received my second IVIG treatment last week and can really tell the difference. I’ve actually been walking, without pain, for the first time in thirteen years! After my first infusion, I think I went almost two weeks before feeling my symptoms come back. I turned back into an old lady, scrunched up, as I walked across the room. I definitely feel more alert, still having trouble with cognition, can’t wait to get my brain cells working again. I’m so looking forward to the Stanford Symposium, wish I was well enough to attend.
There’s a simple explanation for having episodes of chronic abdominal pain with conditions involving autonomic dysfunction, such as POTS, chronic microvascular intestinal ischemia, but gets overlooked by doctors because it causes no obvious pathology to diagnose it from.
Excessive dysfunction of a single blood flow regulator can precipitate intestinal ischemia and POTS, in affecting your cardiac and regulation, can be that trigger.
These ischemic insults result when your system can’t meet the extra demands placed on it for increased bowel blood flow during the digestion process.
Ischemic periods are usually short and, as the bowel can tolerate a 75% reduction of mesenteric blood flow and oxygen consumption for 12 hours, causes little, if any, microscopic changes usually associated with bowel ischemia.
Most typically, the main symptom for this is epigastric pain that occurs soon after eating but it can be a subtle thing that could easily be past off as “just IBS”.
SuzyDee I believe this is what is happening to me…I had a SUDDEN development of POTS…and severe abdominal pain…the ER doctors would never listen to me about the abdominal pain…..I also have an ileostomy so have had extensive abdominal surgeries…..I know my POTS is related to my intestines somehow….also I was put on antibiotics for a urinary infection and my POTS symptoms improved greatly….but I can’t stay on antibiotics forever right…Please tell me if there is a cure or treatment for the Messantery issue…thanks
SuzyDee can you please tell me if there is a cure or treatment for intestinal ishemia…I believe this is what is causing my new sudden POTS symptoms….I kept telling the ER that it was related to my intestines but no one would listen to me….any treatment for this ….???thanks
Heartfelt thank you Cort!! I am Snoopy Dancing over here! Now on the hunt in finding a Dr..