

“Finding an objective neurochemical change in the brains of people who are used to being told that their problems are imaginary is pretty important…” Marco Loggia
Jarred Younger has believed for quite some time that the glial cells in fibromyalgia patients’ brains are spewing pro-inflammatory factors and causing neuroinflammation. That neuroinflammation is, in turn, tweaking their pain and other neurons, resulting in a hypersensitivity to pain, sensory stimuli, sleep problems, cognitive problems, etc.
It’s an enticing idea. If low levels of neuroinflammation are going to be found anywhere, one would think they would be found in FM. The central nervous system issues have been well validated and indirect evidence of neuroinflammation has been found before. No one, though, has actually shown that neuroinflammation is present in fibromyalgia or, if it is present, that it’s being produced by glial cells – until now.
This FM PET scan study was produced by an unusual combination of Swedish and Harvard Medical School researchers. Apparently, upon learning that the Swedes from the Karolinska Institute were doing the same study, the Harvard group suggested that they team up. That Swedish group had recently found evidence of neuroinflammatory proteins in the spinal fluid of people with fibromyalgia. That 2017 study found increased levels of a substance called fractalkine which may play a key role in microglia activation, increased pain sensitivity and allodynia.
Brain Behav Immun. 2018 Sep 14. Brain glial activation in fibromyalgia – A multi-site positron emission tomography investigation.Albrecht DS1, Forsberg A2, Sandström A3, Bergan C4, Kadetoff D5, Protsenko E6, Lampa J7, Lee YC8, Höglund CO9, Catana C10, Cervenka S11, Akeju O12, Lekander M13, Cohen G14, Halldin C15, Taylor N16, Kim M17, Hooker JM18, Edwards RR19, Napadow V20, Kosek E21, Loggia ML22.
You might not be able to find a better group to assess the neuroinflammation in FM than the Loggia group. Marco Loggia, the senior author of the study, runs the Loggia Pain Neuroimaging Lab at Harvard. He’s a younger researcher – he got his PhD in 2008 – who is interested in subjects such as pain and fibromyalgia that many of his predecessors probably would have disdained.
Over the past five years, though, Loggia has co-authored fifteen papers on fibromyalgia or other chronic pain states. In 2015, he was the first to document glial cell activation in chronic pain. A review paper featuring Loggia, Nijs, Meesus, Daniel Clauw and others suggested sleep issues or severe stress could trigger glial activity, which in turn results in central sensitization and chronic pain. A 2016 review paper covered the ins and outs of new ways of assessing neuroinflammation.
Two 2018 studies found neuroinflammation in specific areas of the brain in ALS (precentral and paracentral gyri) and Huntington’s Disease (thalamus and brainstem).
In 2017, it was primary lateral sclerosis (motor regions). (Note how localized the regions of inflammation are…)
All Chronic Pain is Not the Same
Jarred Younger was astonished to find no evidence of neuroinflammation in rheumatoid arthritis patients using heat mapping and magnetic spectroscopy.
Loggia’s findings also suggested that all chronic pain is indeed a complex condition which is caused in different ways in different diseases. That finding suggests that the prevailing practice of treating all pain conditions with opioids is uninformed to say the least.
As did a recent chronic fatigue study, this study found extensive evidence of neuroinflammation in fibromyalgia
Loggia’s 2015 low back pain study found glial cell activation (neuroinflammation) in the thalamus and regions of the somatosensory and motor cortices which represented the areas of the body – the back and leg – where the pain was experienced.
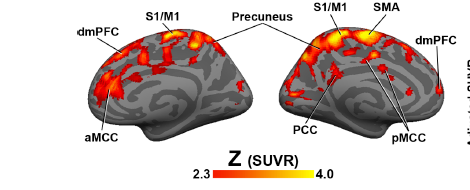
In contrast, perhaps reflecting the more complex nature of FM – which causes pain, sleep, cognition and problems with stimuli, the glial cell activation in FM was much more widespread and occurred in different areas (dorsolateral prefrontal cortex (dlPFC), dorsomedial PFC (dmPFC), primary somatosensory and motor cortices (S1/M1), precuneus, posterior cingulate cortex (PCC), supplementary motor area (SMA), supramarginal gyrus (SMG), and superior parietal lobule (SPL).)
Interestingly, glial activation in the cingulate cortex popped out. Its association with fatigue in Loggia’s study, its elevation in the Nakatomi ME/CFS study, and the central role it appeared to play in Younger’s recent study (unpublished), suggests that this part of the brain may play a central role in both ME/CFS and FM. Loggia suggested that inflammation in the cingulate cortex was likely contributing to fatigue in all three disorders.
The study was small but the results were enhanced by the fact that it took place in two locations: Boston, Massachusetts and Sweden.
Moving Forward
This study comes on the heels of unpublished work by Younger which used heat mapping to assess inflammation in the brain of people with chronic fatigue syndrome (ME/CFS). That study also found widespread neuroinflammation.
Younger’s recent grant to do a heat map study of FM patients will add to these PET scan results, and he’s applying for an NIH grant to do an expanded heat map and PET study in ME/CFS. A Japanese group has reportedly been working on a very large PET scan study in ME/CFS for years, plus Andrew Lloyd was reportedly working on an ME/CFS neuroinflammation study in Australia. If all goes well, before too much time has elapsed we may have substantial evidence that neuroinflammation is indeed present in ME/CFS and hopefully, FM as well.
Treatment Implications
“The findings may open the way for the development of completely new therapies for this currently difficult-to-treat condition.” Kosek, co-author.
“We don’t have good treatment options for fibromyalgia, so identifying a potential treatment target could lead to the development of innovative, more effective therapies.” Loggia.
So, if neuroinflammation (i.e. glial activation) is a “potential treatment target” in FM, what could be done to turn those cells off? There don’t appear to be standardized protocols for reducing neuroinflammation but there are a lot of suggestions. It appears to be a potent field of research.
Fibromyalgia Drugs
Interestingly, the FDA-approved drugs for FM make the list. They may not be the cat’s meow but they can be very beneficial for some, and they may be helping to tame overactive glial cells.
Several mouse studies suggest that Lyrica (pregabalin) can reduce glial cell activation. A 2015 study found that Savella, an “antidepressant”, reduced lactate levels and pain. The authors believed that the high lactate levels were due to over-activated glial cells pumping out pro-inflammatory factors, which increased oxidative stress and promoted anaerobic metabolism. Cymbalta (duloxetine) also appears to attenuate glial activity.
Antidepressants
Antidepressants, surprisingly, are on the list as well. Research suggests that many antidepressants also have anti-inflammatory properties that may be helping the 40% or so of people with inflammation-driven depression.
A 2012 study, in fact, found that all the SSRI’s tested (fluoxetine, sertraline, paroxetine, fluvoxamine and citalopram) “potently” inhibited the microglia from pumping out pro-inflammatory factors.
Low dose Naltrexone (LDN)
Jarred Younger got interested in LDN and then tested it in FM because studies showed it had microglial-inhibiting properties. Several subsequent studies have shown that LDN can be an effective pain reliever. (LDN appears to be able to inhibit the TL4 receptors that turn on the microglia.)
Jarred Younger will soon be assessing the effectiveness of what he believes may be a much more potent form of the drug. More on that coming up soon.
- Learn more about LDN in Health Rising’s Low Dose Naltrexone (LDN) Fibromyalgia and Chronic Fatigue Syndrome Resource Center
An LDN Combo? The Low Dose Naltrexone / Trazodone Question
Who says you couldn’t combine LDN with other drugs to make it more potent? Both LDN and trazodone are believed to have glial cell reducing properties. Interestingly, an LDN/trazodone combination popped up during an SMCI-funded (the former CAA) Biovista search for drugs to use in ME/CFS.
Biovista is a drug repurposing company that claims a 70% success rate in identifying effective drugs. First, Biovista gathered all the information on ME/CFS symptoms, pathophysiology and treatment they could, and then used an algorithm which contained information on “every known gene, pathway, disease, anatomical location, cell structure and other component of potential drugs, etc.” to search for drugs or drug combinations to try. Up popped a trazodone/LDN combination.
Trazodone in itself is an interesting drug. ME/CFS expert Dr. Bell reported that Trazodone was one of his favorite sleep medications. In low doses it’s probably used more as a sleep aid in ME/CFS/FM than as an antidepressant. It’s one of the few drugs able to reduce the alpha wave intrusions that plague FM and ME/CFS patients during sleep. Plus, the IACFS/ME Treatment Primer reported that Trazodone may be able to maintain its effects over time better than any other sleep drug.
Dextromethorphan
Dextromethorphan is another Jarred Younger targeted potential glial cell inhibitor. Best known as an ingredient of cough syrup, animal models indicate dextromethorphan tones the microglia down and can protect neurons from glutamate excitotoxicity, hypoxia and ischemia. As with LDN, low doses are more effective and higher doses may not reduce neuroinflammation. Dextromethorphan is currently under trial in fibromyalgia in Jarred Younger’s Neuroinflammation, Pain and Fatigue lab.
Other Potential Glial Cell Inhibiting Drugs
- Ibidulast – is an anti-inflammatory drug, used mainly in Japan, which has strong neuroprotective effects and was able to go so far as to reduce neuroinflammation in a mouse model of Parkinson’s disease. Numerous trials testing its effectiveness in reducing glial cell activity are underway.
- Copaxone – If anecdotal reports are correct, Copaxone, a multiple sclerosis drug, may be more effective in some people with ME/CFS than it is in MS. Two ME/CFS patients, believed at the time to have MS, reported excellent results from the drug. One later became allergic to the drug, but during the time she took Copaxone, her fatigue essentially disappeared. The Open Medicine Foundation is examining Copaxone in the context of ME/CFS now. Copaxone is an immunomodulatory drug which reduces microglial cell activation in MS, and regulates TNF-1 and IL-10 expression in microglial cells.
- Minocycline – animal studies suggest that minocycline, an antibiotic, can suppress glial cell activity. Interestingly, it seems to do so, at least in part, by activating endocannabinoid (cannabis) receptors, which suggests that cannabis and minocycline might play well together…
- Cannabidiol – the major constituent of cannabis, cannabidiol has been shown to reduce glial activity. Stayed tuned for some cannabidiol success stories coming up shortly, including suggestions about how best to use the compound.
- Moclobemide – antidepressant reduces glial cell activity.
- Imipramine – antidepressant reduces inflammation and glial cell activity.
- Tangeretin – flavonoid reduces inflammation in glial cells.
- Fucoidan – reduces inflammatory production by glial cells.
- Bee venom (melittin) – suppresses inflammatory activity in glial cells.
Check out the latest on Copaxone and ME/CFS
Possible Future Drugs
Fractalkine-Inhibiting Drugs
The good news regarding fractalkine, is that besides being found upregulated in fibromyalgia, it’s been implicated in several neurodegenerative diseases including Alzheimer’s and multiple sclerosis and several fractalkine-inhibiting drugs are reportedly in clinical trials. (It’s also upregulated by viruses.) Three months ago, Kancera, a Swedish-based pharmaceutical development company, added two new fractalkine antagonists to its fractalkine project. Because fractalkine is believe to poke glial cells awake, a fractalkine antagonist could be a major step forward.
Others
A brief survey suggested that the search for better glial cell inhibitors is on. Laboratory studies suggest a wide variety of compounds could help tamp down the microglia. Honokiol, which comes from the magnolia tree and is used in Eastern Medicine, reduced glial activation in mice in a recent study. A culture study suggests that NADPH can inhibit glial cell activation in nerve cells. A fatty-acid amide-hydrolase (FAAH) inhibitor URB597 modulated glial cell activity in the hipppocampus. DTIO (Nec-1, 5-(3′,5′-dimethoxybenzal)-2-thio-imidazole-4-ketone) inhibits neuroinflammation, reduces lactate formation, etc. Two recently discovered molecules could reduce neuroinflammation.
Diets, Supplements and Botanicals
A 2016 study, which found that a high fructose diet resulted in high levels of fractalkine and neuroinflammation in mice, might be bad news for carbohydrate lovers. Anti-inflammatory diets which restrict carbs would seem to be an obvious first step in attempting to reduce neuroinflammation.
- Check out a bunch of dietary ways to naturally reduce inflammation.
N- acetylcysteine (NAC) is an antioxidant and mitochondria enhancer. Shungu (unpublished) reported that NAC supplementation was able to reduce lactate accumulations in the brain and improve symptoms in ME/CFS. NAC is relatively cheap, readily available and is believed to be safe.
Taking magnesium can reduce IL-8. Chondroitin, glucosamine, hyaluronic acid and boswellia serrata may be able to quench several inflammatory chemokines such as IL-8. Omega-3 fish oil and DHA may be able to regulate glial cell activity, and antioxidants such as Grape seed extract, cordyceps, and curcumin (with bioperine) and CoQ10 can help calm the microglia as well.
Jarred Younger produced a long list of botanicals that may be able to calm the microglia, and is testing some of them in Gulf War Illness. They include: cucurmim, luteolin, resveratol, gastodia elata, obovotal, inflexin, pipera kadsura, ganoderma lucidum, berberine, isodon japonicasm, epimedium brevicornum, stephania tetranda, stinging nettle, fisetin, pycnogenol, boswellia and kratom.
Conclusion
Further studies are needed to validate the findings but no one’s surprise neuroinflammation appears to be present and widespread in the brains of people with fibromyalgia. The surprisingly long list of potential microglial inhibiting agents is encouraging (and a bit daunting) and much work remains to identify those that will be helpful in FM and ME/CFS. For now we know that LDN and some cannabis products work well in some patients and Jarred Younger is testing other possibilities. With interest in microglial inhibiting agents growing hopefully the future of this possible new treatment option is a bright one.







“A 2016 study, which found that a high fructose diet resulted in high levels of fractalkine and neuroinflammation in mice…”
I recently found even moderate amounts of fructose to be really problematic for me (see papaya topic in forum), but so far it seems more to be an intolerance/gut problem. But few is known why one is intolerant to something. It could be because the body “knows” it’s bad for it…
But I do not agree with “might be bad news for carbohydrate lovers. Anti-inflammatory diets which restrict carbs would seem to be an obvious first step in attempting to reduce neuroinflammation.”
-> I do fairly well on a balanced diet with very few sugar but many starch like slow digesting carbs. I did in fact return to a diet more moderate in fat and protein when I learned that I had a problem digesting protein (immune reaction to protein!), something that somehow seems closely related to my fructose (FODMAP?) intolerance.
The key for me however is to: avoid sugar, avoid fructose even more so basically avoid most fruit, try and keep my (combined) glucose and fructose blood levels fairly flat, have a wide variety in fat and protein sources so you don’t have to convert stuff from one form to another and have a modest caloric intake.
That, plus keeping the body in a somewhat lower temperature environment should increase NADPH production substantially (“A culture study suggests that NADPH can inhibit glial cell activation in nerve cells.”). As it’s essential to regenerate glutathione it obviously is important in fighting oxidative stress as well.
That had significant positive effects for me. I just have to go back to it again. This food intolerance thing has distracted me from keeping my discipline up lately ;-).
For FM patients, cold is often considered bad for pain levels. As a combined ME/FM patient I was longtime confused by some people reporting heat as good while others saying ice baths are good. I think I understand better now:
* For ME and FM I think higher NADPH production is beneficial.
* For someone who is not hypothermia as I was a few years ago and who lives on a non-keto diet I believe a bit of cold can increase NADPH production. The idea is that it leaves more options for the body to produce NADPH as it has heat as a byproduct. Colder muscles are of benefit here.
* Colder muscles increase chance for damage, stiffness, cramping however so that’s bad for FM.
* Some amount of heat does the opposite, so it seems om must chose the lesser evil.
* However, increased muscle damage is more likely when using your muscles (moving, exercising…) so I learned to have somewhat lower body temperature on average but doing some warm-up in the form of circulation exercises before “exercising”.
* Heat can reduce muscle stiffness. I learned that keeping your body temperature a bit lower and having short heat treatments specific on the muscles helps me better with FM then constant elevate temperatures. It feels like a short heat treatment is enough to let “slide” the stuck muscle fibers back in place a bit. Low “doses” spread over the day seem to help best, but require discipline.
* All the above is for when one can heat his own body up just by burning calories in a colder environment. In the case of hypothermia reverting hypothermia before doing this very likely is required.
* When one has cramping due to cold, it’s a sign that one has gone too far with cold therapy IMO.
I did learn to eat some rice crackers (the foam-like ones, easy to digest) before sleeping to be a sleeping aid. The idea is to keep the blood sugar levels more constant. In doing so, less combined cortisol/adrenaline is needed to create glucose out of glycogen/protein/fat. That’s good for giving your adrenals some rest and have reduced anxiety at night. As a plus, by using less cortisol/(nor)adrenaline for getting glucose into the blood, more is available at the cells for turning glucose into energy. It’s a modification I learned from someone on Healthrising who stated he “loaded up on carbs” for better sleep. I however believe it fits best with a moderate daily caloric intake diet, so don’t just add another load to your daily intake.
Am I the only one who feels better with sugar/carbs? I have severe ME/CFS (not quite bedbound), and mild FM, and my BMI is normal. Every time I switch over to no sugar, lower carb I slowly fall into a slump, especially cognitive, and do better when I add those back in to my diet.
After an exertion, like a trip to the doctors office, I have an extreme craving for carbs and feel better after I load up on white rice or frozen custard. I got gluten free brownies for my birthday and when I was eating one every day I noticed an upswing. I’d like to know if there’s anyone else out there like me.
Also, when I supplemented with fish oil, after three days I experienced depersonalization which stopped when I stopped the fish oil. After seeing Robert Phair’s OMF metabolic trap talk, I now wonder if the fish oil further increased already high serotonin levels (I can’t take any SSRI without severe side effects, but I am a poor metabolizer (liver enzyme profile) for most of those drugs).
Seems like whenever I try to eat ‘healthier’ things go further south for me. Anyone else?
Think my previous reply got lost.
Saw this on YouTube yesterday, quite long but worth it. He mentions the brain needing sugar, could explain why it helps with your fog.
https://youtu.be/jrW1FTc_kyg
Have you tried D-Ribose? I gather it’s needed for ATP and is a ‘good’ sugar. Shame it’s not a bit cheaper!
Regards
Adam
Birdie, You are not alone. I feel much better on a high carbohydrate diet and always have. I tried a high protein, low carb diet once to see what it felt like and I had zero energy and got extremely dehydrated. I used to be a registered dietitian and observed how my patients felt on low carb, high carb, high protein, etc. and saw first hand how each person reacts differently. Now that we have genetic information available I think we might be able to identify why we see individual differences.
It’s an interesting coincidence; I too have discovered recently that I sleep better if I consume a little starchy carbs before bed. I have been continuing to get better from my FM for several years now with a multi-disciplinary protocol that includes a very low-carb diet. I hypothesize that burning carbs for energy adds to the toxin load that causes adhesions in muscle fascia. But I think eating carbs last thing before sleep, does not trigger the energy metabolism to switch away from burning fat for energy, in the way that eating carbs during the day does. I consume something high-fat on getting up the next morning to ensure my metabolism remains directed to ketosis.
Tanja – I have experiences with my own decades of self-experimentation that finally started to make me better, about 5 years ago. I hypothesized for a long time that burning carbs for energy, added to the toxin load that caused adhesions in the muscle fascia. But every time I tried to go low-carb, I suffered dehydration and unbearable cramping; plus I suspect the dehydration worsens the fascia adhesion problem.
But I finally got round this problem by taking high doses of high-quality magnesium with the best possible absorption qualities; using magnesium “oil” externally, rubbed into the skin on the problem areas like the calf muscles; and adding to the diet, low-GI soluble-fibre foods like Konjac (noodles), Flax seeds (flatbread) and Chia seeds. I also drank a lot, and tolerated frequent urination (nevertheless the tendency to urination has gradually declined as my condition has improved).
The other very significant element to my protocol, is doing a lot of low-intensity exercise. Sedentariness is very bad, allowing fascia adhesions to develop; and over-exertion is also very bad, I believe because toxin load is increased from energy production by-products. Keeping moving as much as possible all day is very important. I think the real problem in people with FM, is that we are highly prone to muscle fascia adhesions.
Yes, Birdie, both my daughter and I have ME and FM, and we cannot go without sugar and carbs every day. We crash when we try to go off. I have trouble digesting protein as well, so can’t do high protein, even with digestive enzymes. Frustrating, as we know the sugar probably makes pain worse, but we can think better and have more energy.
@Philip (split in parts): “an interesting coincidence”
Timing of discovery may be coincidence, but that it works quite likely is not. I think there is a (or more then one) solid mechanism behind it that waits to be explored in more detail.
I’ve written the past months several times about the potential interconnections between NADPH / glucose regulating hormones / anxiety / hypothermia / cold treatments / oxidative stress / inflammation / glutathione / protein misfolding.
Glucose has quite an influence over many of these connections IMO, and not always for the worse! When writing about it, I often added “for a non-keto diet” as a ketogenic diet turns on a whole different set of gene expressions. Your observation may help me in better estimating the overall role of glucose in both types of diet. Thanks friend!
It seems people on a ketogenic diet might be able to exploit both the ketogenic advantages and incorporate some improvements making carbs more anti inflammatory in their diet. I go the other way, attempting to make my higher carb based diet a lot more anti inflammatory and have some morning ketones on the side ;-).
As to why it works on a ketogenic diet let me share my initial thoughts:
* Many people hypothise that a ketogenic diet helps because it keeps the blood sugar level a lot flatter.
* It certainly helps to flatten out the high blood glucose peaks often going hand in hand with a higher carb diet. But I do believe this keeps a blind eye on the lower margin. People do need glucose in their blood badly, even people on a ketogenic diet. RBC for example have no mitochondria if I recall correctly. So they need glucose for anaerobe ATP production.
* In ketogenic diets, glucose isn’t so low because the body desires it to be so, but because supply of glucose and components that can be easily and cheaply converted to glucose in large quantities are scarce. Therefore the idea that the body easily can keep glucose levels flat in a ketogenic diet is debatable at least.
* One can say that when something varies between 200% and 50% it varies far for then when something varies between 40% and 20% (for example), but getting to the extreme lows might be pretty bad as well. Saying the latter is better because it’s flat is like saying that a yearly income varying between 40k and 20k is better then have it vary between 200k and 50k. Sure, ketones can reduce the need for glucose a lot, but how low is less then ideal?
* So, during the night people on a ketone diet might have to pillage their free protein supply, scrape a molecule of glucose from as much as possible triglycerides and might have to deconstruct a few more cells to scavenge protein then is ideal… and in doing so they might have to crank their hormonal state to pretty extreme, including significantly elevated (compared to a normal healthy person on a regular diet) levels of cortisol, noradrenline, adrenaline that are not supposed to be high during sleep.
“so can’t do high protein, even with digestive enzymes”
I have outspoken trouble digesting protein as well. Eating papaya helps me a lot with it due to the enzyme papain.
The special thing about this enzyme is that it is one of the very few that starts digesting protein in the stomach rather then in the gut. I believe that makes a strong difference for me.
I believe my problem is that undigested proteins enters the bloodstream either trough damage to the gut lining or even due to heliobacter pylori induced damage to the stomach (recent idea, needs testing). Papaya works better for me then the supplements I tested so far.
In the first case early digestion is helpful, in the latter case essential: undigested protein in the bloodstream causes auto immune reactions. Aphthuous mouth ulcers or adult acne are good indicators IMO for having immune reactions to protein. See my papaya topic in the forum if interested and feel free to share papaya experiences.
(@Philip: wordpress keeps blocking my responses to you)
I eat a high carb, wholefood plant based (vegan) diet. My fibromyalgia, CFS and arthritis have all gone. I try to eat more ‘natural’ sugars. However I don’t find sugar is a trigger for pain. Animal protein and dairy however cause the inflammation and pain to return even in small amounts.
I recently tried minocycline for its anti-inflammatory properties and found that combining it with marijuana made for an unpleasant experience. It’s possible that it wasn’t the combo, just a bad high, but I’d not had that particular experience before. I’d describe it as anxiety coupled with a kind of mild depersonalizing feeling that I’ve come across on some minocycline-related sites.
Cort, I wonder if you have an eye on the Mass General fibromyalgia vaccine trial. EpicGenetics, the FM/a test maker that’s co-sponsoring it, has been peppering my email box and apparently the phase II trial just got the FDA’s green light.
Lastly, thank you for your reporting. You’re performing a real ‘mitzvah’ here-this site provides so much solid info, not to mention some hope.
Ouch! Not a pleasant experience at all. I guess you never know what will happen.
Thanks for your nice words and the heads up on the Mass General fibromyalgia vaccine trial – I had never heard of it. I found it in clinical trials….Really interesting!
https://clinicaltrials.gov/ct2/show/NCT03582085
I’ve taken the FM/a test. My results came out positive on the high side. Some insurers, including major ones like Blue Cross, will pay for the test. My HMO would not pay for it – I took it about a year ago-partly so I could participate in the vacine trial which will be conducted at MGH. I live in Boston. EpicGenetics will be reaching out for participants and I haven’t been contacted yet…. I’ve been to Dr. Oaklanders practice, had the skin biopsy, which was positive for Small Fiber Neuropathy. I requested a script for LDN, which the research assistant was happy to provide. The nice thing about research fellows is they’re open rather than close minded. I have exercise intolerance, and read an article about Dr. David Systrom at Brigham and Womens. Took a while to get into see him, but I had the iCPET test. Unfortunately the results were not insightful – I question whether the test was administered correctly. It was quite a procedure to go through for a disappointing outcome. I was hopeful for answers. The cost of the test was $45+k, the initial office visit $6k. I was really expecting they would identify issues with oxygen delivery. Dr. Systrom did put me on Mestinon – I don’t notice any improvement. Dr. Systrom was wonderful as were the folks who administered the test at Brigham & Womens.
Hey Cort, long time listener,first time caller. I’ve been having health issues coming up to 2 years now which I can’t help believing is ME/CFS or Fibromyalgia( no diagnosis as yet) or something connected to it.
I just wanted to say how inspired I’ve been by your work keeping people abreast of progress in research and all the other resources this website provides as well as by the other ‘patient experts’ who contribute.
I think what you and some of the researchers are doing using social media to build a healthier two way relationship between the medical community and ordinary people with the condition is truly extraordinary. I hope for everyone that this will all bear fruit before too long, and people can enjoy a whole new life. I have faith that it will.
Best wishes from the UK
P.S Sorry it seems we’re sucking so bad at our end with the research. It’s a shame because we have a great tradition in Science and medicine.
Thanks Gareth. It’s interesting about the U.K. They have not helped with their emphasis on CBT/GET but on the other hand they’ve put a much higher percentage of the research dollars into ME/cFS than the U.S. – so when things get turned around and they may be turning around – they may end up being a big help. Let’s hope so.
The focus on CBT is a form of systematized psychological abuse of a whole class of sufferers of actual muscoloskeletal dysfunctions that the medical establishment is too incompetent and arrogant to identify!!! Most likely FM sufferers with psychological problems, have these BECAUSE of the establishment’s psychological abuse of them – brainwashing them that ACTUAL pain in their adhered, pinched muscle-fascia tissues (an obvious physical reason FOR pain), is “in their heads”.
I was wondering how long before some REAL treatment for fibro is offered to us who have suffered for so long.
Hi Cort, I find that Amitryptiline in slow release form helps me the best, while a normal tablet is not bearable.
Excellent report as always.
Finally researchers are getting closer and closer to understanding and proving wide spread inflammation in patients and the cinnection with fatigue and widespread pain. What causes this in the first place and how to treat or manage these diseases hopefully will become much more clear. Also understanding why some meds work for some but not others. LDN makes me very sick and Lyrica caused a lot of weight gain and increased brain fog. CBD oil has helped the best.
LDN didn’t work for me either and we have a couple of CBD success stories coming upl
Love your reporting, Cort!
I’m in the EDS camp, with moderate ME/CFS. (50% of people with Ehlers-Danlos also have Small Fiber Neuropathy, but I’m not one of them).
Having tried a great deal of various medications, supplements, I have to put in my plug for curcumin (Cure-Pro BCM-95) which incidentally does not contain black pepper components. Although I don’t use it for fibromyalgia, I have used it successfully for spinal stenosis/herniated disk/ plus a synovial cyst. At a dose of 750mg. per day, it took 2 weeks to almost completely obliterate my sciatica and neuropathy and has twice saved me from fusion surgery.
For ME/CFS I’m limping along with one Modafinil (works for a few hours), and occasionally 5mg. Adderall ER. I find if take one of each, my energy boost will last two days instead of one. I think that might be a clue that energy is ‘locked’ within the mitochondria (or wherever) and that for some reason, the combination frees it for more than 24 hours.
For pain, it’s Norco, or even kratom. LDN only sort of works. Cannabis is a big bust, but great for sleep!
I think it will be difficult to tailor medication to each individual, especially if autonomic dysfunction is involved. Sigh…
Hope those research dollars keep flowing in! Thanks again!
EDS is a completely different condition to what most of us with FM have. Your pain is completely explainable by the recognised dysfunctions in your muscle and ligament tissue.
It is probably possible for someone to have EDS and the fascia adhesiveness that is the issue in most people with FM. People with EDS usually have extremely high limb range of movement because of the EDS, whereas most people with FM have extreme limitations on movement. Doctors should all perform simple range of movement tests right at the outset of diagnosis, to determine which problem a patient has.
EDS sufferers are “lucky” in that the medical profession does recognise dysfunctions in muscle tissue that obviously cause pain, it is not just “in your heads”. For most people with FM, I argue that there is another dysfunction in muscle tissue that is responsible for generating very real pain, only the medical establishment is too incompetent and arrogant to accept this possibility. Because allegedly the hands-on practitioners who can feel palpable distortions in muscle tissue at the locations of pain, are “not scientific” like, say, an MRI scan.
Hi Philip,
Respectfully, not all people with EDS have flexible ligament and muscle issues. Hypermobiles do, but there are now 13 types and each comes with a separate set of problems, many of which overlap with each other.
Almost all the EDS types have some level of fatigue and pain, and with Hypermobiles especially, that pain can not only manifest as muscle and joint pain, but ‘fibromyalgia-like pain.’
I’m not going to say that it is fibromyalgia proper, but many people with this type of pain get categorized by doctors who do not recognize EDS. Some will diagnose a patient having two different disorders.
Since EDS is my so called ‘area of expertise,’ like fibromyalgia, doctors are at a loss to fully explain the various types of pain experienced by people with Ehlers-Danlos–especially the ‘fibromyalgia like’ pain. Some can be explained by small fiber neuropathy, but others, not so much.
Personally I believe there are some sort of intertwining cause/relationships between pain and fatigue in CFS/ME, fibromyalgia, Ehlers-Danlos and possibly autonomic dysfunction and perhaps more. So far much of this is not adequately explained or proven.
As for how ‘lucky’ people with EDS are, I have to say that most doctors I have visited, and there have been many, know next to nothing about EDS. For many Hypermobiles the amount of pain they experience, much like fibromyalgia’ can not be adequately explained by imaging results.
Thanks for the comment, Nancy. I hadn’t read anything about forms of EDS that did not involve excessively flexible joints. I have told several doctors and other practitioners about the need to check for EDS before diagnosing “FM”.
What you are saying about “FM-like” pain in EDS patients that baffles doctors, leads me to reiterate more strongly what I said: “It is probably possible for someone to have EDS AND the fascia adhesiveness that is the issue in most people with FM.” I bet it is the same thing baffling the doctors in both cases; the “pure FM” cases and the EDS cases with “FM-like” pain.
I certainly agree that co-morbidities are likely and probably common, between EDS, FM, CFS and other conditions. The dysfunctions and deconditioning resulting from one condition, might trigger other conditions as well. I do think, however, that there are distinct factors that need to be defined rather than confused as is often happening at present.
For example, many doctors I have met, have a vague idea that FM and CFS are actually the same thing. Unfortunately, the meaning of some of the terms have become blurred. “FM” has come to mean “CNS dysfunction”, which makes FM a symptom of many different conditions that lead to this CNS dysfunction. A new name is required for the fascia adhesion condition that I am talking about, but of course the medical mainstream needs to accept that it even exists! Devin Starlanyl and others have used the term “Myofascial Pain Syndrome” but I think that as it inevitably includes adhesions and palpable deformations, “pain syndrome” does not do it justice.
My argument for a long time has been that CNS dysfunction could quite logically be a result of real pain signals from so many different places at once, that the CNS is hypersensitized. I do not think the “CNS dysfunction in isolation” hypothesis is at all helpful. Obviously in hypermobility EDS, there is a physical reason for the pain that eventually overwhelms the CNS. I argue that the physical reason for pain that the “experts” are missing in most people with FM (and now I say the same for non-hypermobility “EDS”) is adhesions in muscle fascia, leading to painful “pinching”, lumps and bands that are reservoirs of trapped toxins, and adjacent fascial surfaces dragging against each other like sandpaper instead of sliding smoothly. Of course this is painful!
I said “lucky” in inverted commas for a reason; purely because the physical cause (connective tissue degeneration) has been accepted by the experts rather than being categorised as an “in the head” problem. People with a palpable physical condition that the “experts” are too closed-minded to accept, and who are falsely categorised as having “in the head” dysfunctions are unlucky in a special kind of way. Cancer sufferers would be likewise specially unlucky (even more than they already are) if cancerous growths were not imageable and the “experts” did not believe in them!
That’s great Nancy and thanks very much for giving the specific brand of cucurmin that’s been helpful. I think brand is probably very important for that botanical.
Have you checked out the Synergy combo? I think it’s methylphenidate plus mitochondria enhancers.Jon Kaiser thought the combination was unlocking the energy of the cell. The trial didn’t work out but there was a catch that I’ll be reporting on.
https://www.healthrising.org/blog/2014/05/19/stimulating-energy-mitochondrial-enhancement-synergy-clinical-trial-chronic-fatigue-syndrome/
Cort, thank you for the comment/compliment and recommendation! I will straight away put it on my ‘to do/to try’ list.
One small adjustment, evidently auto-correct made a small mistake in my curcumin listing. The complete identification of it is Euro Medica, Cura-Pro BCM-95. I buy large bottles of 120 count 750mg. for around $80-90. Expensive, I know, but much better than neuropathy and a fusion!
Philip, your ideas about fascia problems are interesting. There was a lecture on http://www.EDSawareness.com presenting evidence that the fascia are not only involved in holding groups of muscle together, but also are very important to proprioception (the perception of where our bodies are in the environment.
EDSers often have horrible proprioception and so are constantly getting scrapes and bruises from knocking into things. This makes me wonder if people with fibromyalgia ‘proper’ also have this problem…
“…That Swedish group had recently found evidence of neuroinflammatory proteins in the spinal fluid of people with fibromyalgia…”
The problem is common to “everywhere in the body”, in the fluid in all interstitial spaces – not just the fluid around the brain and the spine. Recent research has correctly suggested that standardized tests of interstitial fluids would have major diagnostic power. These fluids do move around the body independently of blood and lymph flows. The medical establishment missing this until the year 2018, is like “not knowing about the continent of America” was for exploration and migration and economic possibilities.
It is a classic example of the fable about the blind men and the elephant in the room, when researchers are saying, aha, this substance in the fluid in the brain cavity must be “causing” the cascade of effects that lead to the nervous system “imagining pain”! There are substances in the fluids throughout the body, that are causing problems throughout the body….!!!! What is happening to the brain is like one small part of the elephant!
36 years CFS including 20 years of FM. I’ve tried most of what’s listed above. Low carbing has been disastrous for my gut – diversity very low. Animal fats feed endotoxins, so I’ve added in resistant starch in the form of lentil pasta and red rice occasionally and some berries. But for me, cannabis has been a godsend. Now legal in Australia but access is complex and expensive.
Glad to hear it Jude. Any kind in particular? Several surveys suggest it can be VERY helpful. For me high THC cannabis is a great sleep aid. We have a couple of CBD success stories coming up 🙂
Hi Cort, another great article.
I am wondering if you could add a print button, that way it would be easy to show my doctor these articles. Plus it would be great to show the different medications that might be worth a try.
Thanks, Lynn
Thanks Cruzgirl. There actually is a print button. It’s a little hard to see but it’s at the bottom left at the bottom of the blog. 🙂
I’m wondering why hyperbaric chamber treatment isn’t listed. My understanding that the research done in Israel a few years ago was very promising.
Most of things listed are drugs or supplements. I just haven’t seen hyperbaric oxygen listed as a possible glial cell inhibitor but one would think it presents possibilities for getting at neuroinflammation as one of the reasons for neuroinflammation could be hypoxia.
Just wanted to say that hyperbaric oxygen is considered standard of care in France (for EDS issues, with it’s pain and fibromyalgia-like symptoms).
I’m sure France and Israel are on to something–but which U.S. insurance companies will probably take a long time (if ever) to recognize.
On SBS TV, Insight programme,(Australia), tonight,we learnt nothing new or very helpful. At the very least I suppose it might spread awareness of CFS as it’s referred to down here. It seemed to me that Dr Andrew Lloyd is still promotimng CBT and GET. The whole thing was quite disappointing.
Further to my previous rather grumpy comment( exhaustion and nasty pains all day☹️) I do thank the the patients who appeared on the programme as I know it must have taken tremendous effort, physical and emotional, and no doubt huge payback afterwards.
I changed my diet to a wholefood plant based diet after watching a documentary ‘forks over knives’. I eat lots of beans, pulses, veg and potatoes, rice and pasta. I am now pretty much symptom free from fibromyalgia, arthritis and CFS. I even work as a chef 50/60 hour weeks, I can run 10k easily and only need 6 hrs sleep to function (I even get quality sleep now!). The only time I relapsed was when I decided to start eating a bit of cheese and egg (I was on holiday and there were no vegan options and only a few vegetarian options).
My health is still directly affected by diet, I need to make sure I eat plenty of veg and limit bread and other processed foods. However I haven’t come close to the daily pain, fatigue, sensitivity, brain fog etc I used to suffer from. One thing worth noting is that I’ve never had a sweet tooth so fruit isn’t a big part of my diet. I’ve told numerous friends suffering from fibromyalgia about the effect diet has had on me, however not one person has tried it yet, even after seeing me go from being unable to put shoes on, lift a kettle or reach up to high cupboards or stand for more than 20 mins to being energised and pain free. I’ve even had people say that I didn’t have fibromyalgia as it can’t be cured!
I’m also questioning if James did in fact have FM. How long did you have it ? This isn’t the first time I’ve heard of someone no longer having FM just by changing their diet. It also makes me wonder/believe if some people are genetically able to overcome FM. I think that the people that have overcome FM should be studied extensively !!! Having to live with this horrible disease, hearing about anyone that has been able to eradicate it gives me hope, but also envy.
It appears that people with ME/CFS, and fibromyalgia, may benefit from well funded research into Alzheimer’s. E.g. anti-inflammatory drugs and tools to assess inflammation.
Interesting that Jarred Younger is using heat mapping to assess inflammation in the brain; that might help people with ME/CFS who present with autoimmune encephalitis type symptoms.
My mother was diagnosed with bulbar ALS in the summer of 2016;Her initial symptoms were quite noticeable. She first experienced weakness in her right arm and her speech and swallowing abilities were profoundly affected. She did little to seek help for this disease, as she had been her brother’s caregiver a few years earlier for the same disease.
She was able to get rid of the ideas with the help of totalcureherbsfoundation.com herbal formula that cured my Parkinson disease ,this herbal treatment helped my entire family during our worst time in life.
They exported worldwide and the herbal treatment will get to you in four days delivery to your address.
Anyone have results with Claritin®?
Jayakumar Rajadas,
(Stanford School of Medicine )
in old research article:
“”COMMON ALLERGY MEDICATION MAY BE EFFECTIVE IN STARVING AND KILLING THE BACTERIA THAT CAUSES LYME DISEASE”
https://www.bayarealyme.org/blog/common-allergy-medication-may-effective-starving-killing-bacteria-causes-lyme-disease/