

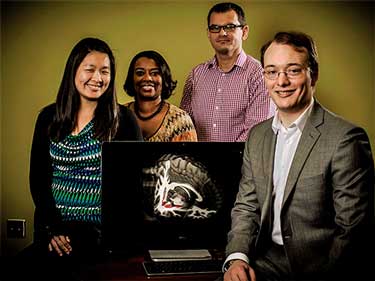
This is the last of three blogs emanating from interviews with Jarred Younger at his Neuroinflammation, Fatigue and Pain lab at the University of Alabama at Birmingham and at the 2018 Stanford Symposium
Younger wanted to know one thing from his post-doc group studying rheumatoid arthritis, osteoarthritis and fibromyalgia: which disease do you know the least about? They said “we have no idea what’s going on with fibromyalgia”. The idea of breaking new ground clearly makes Younger tick.
Big NIH Push for Better Pain Killers
Spurred by the problems caused by the opioid epidemic, the NIH is on a pain-killer drug creating push. Younger said the NIH wants no less than 15 FDA approved new drugs over the next five 5 years and is pouring money into the field like never before. Fifteen new drugs is an extraordinary goal given the difficulty of getting pain-killing drugs to market. (Two failed in phase III trials in fibromyalgia last year. )
Some of the new drugs will go to helping with opioid addiction but a big push is being made to provide new pain-killers. Among other things that push will include developing many new animal models for pain and developing a new clinical network that’s designed to speed up testing and reduce costs.
“I think all of us that are concerned about this worry sometimes that we talk about one without realizing the other requires intense attention. But what about the people with chronic pain—24 million of them—with daily pain? What are they supposed to have available? We all agree opioids are not a great solution. But what other solutions do we have for people with severe daily pain? Not nearly enough.” Francis Collins
The NIH’s big push makes it likely that over the next five years we’re going to see potentially very powerful pain-killing drugs entering the market. There’s some good news on the chronic fatigue syndrome (ME/CFS) side as well.
Younger has also noted a distinct increase in drug company interest in chronic fatigue syndrome (ME/CFS). Five small drug companies or startups that have specific compounds that are in some stage of testing have contacted him in the past year or two. Younger doesn’t sit on commercial boards but he’s happy to look over their scientific protocols and provide advice.
On The Hunt For Microglial Inhibitors
Younger’s been on the hunt – searching the medical literature – for neuroinflammation busters for FM and ME/CFS for years. He’s looking for substances to tame what he believes is at the heart of these diseases: the over-active immune cells in the brain called the microglia that are pumping out inflammatory factors and causing pain, fatigue, sensitivity to stimuli and other symptoms.
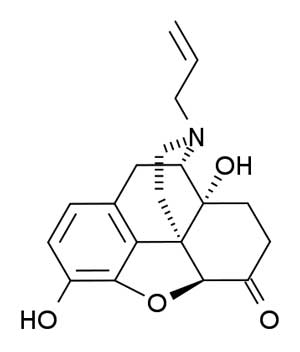
This substance has to be safe for humans, has to be able to pass the BBB and has to be available. Younger’s search has thus far spawned a bevy of clinical trials – from the breakthrough fibromyalgia low dose naltrexone trials, to the ME/CFS LDN trial, to the dextromethorphan trial that’s just getting underway, the botanicals trial that just finished up and new trial he’s trying to get underway which just might put all the others in the dust.
Low Dose Naltrexone and Beyond
The first thing I heard about LDN is that it was effective and did not produce side effects. It can be very effective but the idea that it does not produce side-effects is just not true. Both my partner and I have been unable to tolerate it and reports of side-effects can easily be found.
In Younger’s experience sleep problems (insomnia, vivid dreams) early on are common and usually work themselves out in a couple of weeks. (Taking it in the morning can help with that.) Very rarely he’s heard of people getting jittery or anxious or even having signs of mini-withdrawals (pupils bigger, sweaty, goosebumps) which he attributes to their having a super sensitive opioid system.
There may be a better way to take naltrexone, though, a much better way – one that besides being side-effect free may be much more powerful. It’s called dextro-naltrexone and Younger’s been wanting to get at it for at least five years.
Dextro-naltrexone
Younger’s studies basically started the LDN fibromyalgia craze. He gloomed onto LDN in the same way he’s did with dextromethorphan and the botanicals he’s been testing – by painstakingly searching through the medical literature to look for anything that might tamp down neuroinflammation.
Now he’s focused on a different form of naltrexone called dextro-naltrexone. (There are at least three forms of naltrexone; the higher dose form used to treat opioid addiction; the lower dose form used in FM, ME/CFS and other diseases to reduce pain and neuroinflammation and dextro-naltrexone – a different form of the drug altogether.
Both naltrexone and dextro-naltrexone block the TLR4 receptors from activating the microglia. Dextro-naltrexone probably never made to commercial development because naltrexone was first conceived as an anti-abuse opioid drug. Naltrexone’s ability to interact with the opioid receptors made it an enticing possibility for an anti-opioid drug.
When it became clear that low dose naltrexone causes an increase in an endogenous opioid called the opioid growth factor (OGF, [Met5]-enkephalin) and other parts of the opioid system the stage was set for LDN’s introduction as an anti-pain drug.
Younger always thought, though, that LDN’s usefulness in FM/ME/CFS is due to its ability to calm the microglia – not it’s interaction with the opioid receptors.
Plus LDN’s interaction with the opioid system may, however, have come with a cost. LDN”s interaction with opioid receptors may be causing side-effects and limiting the dose and therefore the effectiveness of the drug in FM and ME/CFS.
Enter dextro-naltrexone. It has the same potent microglia inhibiting properties as LDN but without the opioid hit.
Dextro-naltrexone presents the decidedly enticing possibility of being able to use a potent microglial inhibiting in far higher doses than is possible with LDN. We won’t know until the trial is finished but that should translate into more microglia suppression, greater pain suppression and more people who tolerate the drug.
Plus unlike LDN which cannot be used with opioids, dextro-naltrexone should be able to be used with them and might even – by removing the TL4R activation problem – remove the side-effects often found with opioid pain-killer’s. (Studies also suggest dextro-naltrexone might also be able to ameliorate the side-effects of stimulants.)
The problem with dextro-naltrexone, though, has been getting ahold of it. It’s not commercially available and as of 2104 Younger knew of no source that could provide it but something, it appears, has changed. Younger talked of a collaboration with Mississippi researchers to bring the drug to trial in chronic pain patients.
It’s possible that Younger’s FM LDN trials which have done so much for so many may simply set the stage for the really effective form on naltrexone….
Stopping Multiple Sclerosis in its Tracks? With LDN
Multiple sclerosis (M.S) is a neurodegenerative disease believed triggered by inflammation. Younger proposes to whack that inflammation with low dose naltrexone in people in the early stages of M.S.. If he can tame the inflammation before before it impacts the nerves he might be able to slow the progress or even stop it in its track.
Gulf War Syndrome Botanicals Trial
Younger has finished up with a novel treatment trial involving no less than 9 botanical agents that demonstrates some considerable creativity. Younger has been pushing for ways to clinical cheaply more cheaply which includes testing multiple substances in them. He believes this may be the first time so many different treatment possibilities have been assessed in one clinical trial.
The botanicals include stinging nettle, cucumin, reishi mushroom, resveratrol, luteolin and others.
Some have been well-studied studied in the lab. For example extensive lab studies show that resveratrol has neuroprotective effects and can inhibit microglia activity. Researchers even know the specific pathways (MAPKs, phosphoinositide3-kinase (PI3-K)/Akt, glycogen synthase kinase-3β (GSK-3β)) resveratrol uses to do this, yet it’s never been tested is diseases such as ME/CFS/FM or GWS, until now.
Cucurmin has been even more well-studied. Animal studies indicated that curcumin inhibits the microglia, staves off damage to the neurons, and reduces oxidative stress. One review stated
Further, the outstanding safety profile of curcumin and its… potential for neuroprotective efficacy including anti-inflammatory, antioxidant, and anti-protein-aggregate activities… make this compound a potential therapeutic agent in treating neuroinflammatory diseases.
Younger has begun to assess the data from the study.
Endotoxin Fibromyalgia Study
Younger had also just finished up his endotoxin FM study. Injecting someone with bacterial molecules which are guaranteed to illicit an immune reaction (flu-like symptoms) was not anyone’s idea of fun, and it was not easy to recruit for the study. In fact, it ended up being the longest study he’s ever done; it took a year and a half to recruit 8 FM patients and 8 healthy controls.
The study actually used a low dose of endotoxin – which the healthy controls didn’t notice but which the FM patients did react to. That suggested, as Younger had hypothesized, that their immune systems were on a knifes-edge – ready to over-react to a stimuli. Next up are the results of the immune testing. If Younger finds anything he can begin to reposition fibromyalgia more as the neuro-immune or rather immune-neuro disease he thinks it is than the neurological disease it’s mostly been characterized as.
Pioneering Researcher Making Good in ME/CFS and FM
It seems like it’s one first after another with Younger. The first LDN FM and ME/CFS studies. The first dextro-naltrexone study. The first dextromethorphan study. The first brain heat mapping study. The first study to determine if immune cells are invading the brains of ME/CFS patients. The first big multi-treatment study. The first botanicals study.
It’s good to see Younger concentrating on FM and ME/CFS and thriving doing it. Hopefully his success will spark other researchers to dive into these disorders.
Your Support Is Requested
Health Rising’s East coast trip provided a wealth of information inspiring the article you just read and the ones below. Next up on the agenda is a new treatment for fibromyalgia, an Avindra Nath interview, and – on the return home – the folks at the Bateman-Horne Center. Next up on the travel agenda is the Stanford Symposium.
Travel provides many opportunities but travel to the East Coast, in particular, is expensive for a small organization like Health Rising which is still working on recouping its trip costs. If you find conference reports and other travel related blogs helpful and want to see these in the future, please support Health Rising.
Articles From the East Coast Trip
The Jarred Younger Series
- Widespread Neuroinflammation Found in Chronic Fatigue Syndrome (ME/CFS)
- Invasion – The Source of Neuroinflammation in Chronic Fatigue Syndrome (ME/CFS)
- Jarred Younger III : Treatments – A Better LDN and the Hunt for Microglia Inhibitors
The IVIG Series
- An IVIG Chronic Fatigue Syndrome (ME/CFS) / POTS Treatment Success Story: IVIG#1
- Are Chronic Fatigue Syndrome, POTS and Fibromyalgia Autoimmune Dysautonomias? IVIG #2
- The Case for IVIG Treatment in Chronic Fatigue Syndrome (ME/CFS), Fibromyalgia, Small Fiber Neuropathy, and POTS: IVIG#3
- Winning the Lottery: “Novel” Treatments Return Severely Ill POTS Patient to Near Health: IVIG #4
Advocacy
From the Dysautonomia Conference
- 2018 Dysautonomia International Conference I: Small Fiber Neuropathy, POTS, MCAS and Vagus Nerve Stimulation
- The 2018 Dysautonomia Conference Pt. II: Could You Have a Spinal Fluid Leak? An ME/CFS, POTS, FM Perspective
- Dysautonomia International Conference Pt III: The Autoimmunity Revolution in POTS
- “Sticky Blood” – Antiphospholipid Syndrome, POTS, Chronic Fatigue Syndrome and Fibromyalgia – The Dysautonomia Conference #4
- Stagnant Hypoxia – Where Chronic Fatigue Syndrome and Hyperadrenergic POTS Meet?
- Promise Fulfilled – A New Chronic Fatigue Syndrome / Fibromyalgia Practitioner Steps Forth







He seems more focused on pain and FM. I have ME)CFS but I’ve very little to no pain. Yet, I’m severe to very severe with M.E. I wonder will any of his work help those of us without pain? Thanks Cort
Eimar, me to, allthough I have my pains (every day, it is the ME/cfs that is keeping me bedridden and incapable for much cognitive tasks, just able to eat. The last time, it looked for me as if Jarred Younger is more focussing on FM instead ME/cfs. At the conferece from Stanford? ron davis, he said he was going to do a trial on FM.
Before he said he would be doing a trial on ME. Verry confusing and I had put my hopes on it so a little bit of a heartbreaking to.
But ofcourse good for people with devistating chronic pain. Wished the NIH would be so interested in ME/cfs as well and not only the infection onset group wich I can not prove.
I had severe fatigue for 18 years. A Dr. put me on Meloxicam for a severe foot problem that almost had me in a wheelchair. I am thankful it helped with my foot pain but actually just as thankful is that within a couple of months I noticed my fatigue was so much better. I still, after 3 years cannot believe it. It makes so much sense though that a strong antinflammatory medication would help if Chronic Fatigue is caused from inflamation in your body. If I were you, I would beg my Dr. To let you try it for a few months if there are no health reasons you shouldn’t take it.
Interesting!
I think its possible it might.
If ME/CFS is caused by microglial activation then the microglial inhibitors he’s trying in FM and GWS such as dextromethorphan and the botanicals and the LDN trial he’s doing in ME/CFS could help.
Dextro-naltrexone certainly fits in this category as well. If it’s really potent as it seems it would hopefully hit any symptoms caused by the neuroinflammation.
Younger thinks small tweaks cause the microglia to produce different symptoms in different people. Hopefully a good inhibitor would those symptoms including fatigue.
Hi Cort, if i am right De Meirleir used LDN for decades in ME/CFS patiënts only a very very small group have some benefit. It is certainly not the drug to put your money on 🙁 But we need a double blind trial to know for sure.
I’ve been really keen to hear more about the botanicals study, but can’t find any preliminary info on the results etc, did jarred share any information with you on this? I’d love to read a full article on it if there’s any more information you can recall from your interview with jarred? Thanks also for all your articles, they give me hope.
Jarred had just gotten the data from the study and hadn’t processed it yet but I look forward to finding out what he found and writing about it. Stay tuned 🙂
Dextro causes massive headache in me.
Cannot sleep cannot take any neuro’s,amino’s.
Once took tryptophan in 80’s worked great, until.
HELL
Dextronaltexone isn’t dextromethorphan so your response to dextromethorphan shouldn’t really matter.
If it matters the dextromethorphan Younger is testing is low dose dextromethorphan
Ron, Interesting that the “Metabolic Trap” hypothesis of how we get stuck in sick mode has to do with exactly that – too much tryptophan. 🙁
I’m not sure how the microglia in the brain would be causing severe gastrointestinal dysfunction including mast cell disease like many of us have. Yes microglia are similar to mast cells but they are also only located in the nervous system.
The one way I can think is that the central nervous system through its regulation of the autonomic nervous system controls motility. Messing up motility can alter the gut flora.
I had such high hopes when I finally managed to get a prescription for LDN. I really tried to stay on it more than a couple weeks, but it caused POTS-like symptoms, weakness and increased tiredness, even at the lowest dose. I was SO disappointed! Glad Dr. Younger is really charging ahead with research and clinical studies on such a broad scale.
I’ve gone back to Dan Neuffer’s ANS REWIRE Program with more commitment this time, and I’m making progress. I have difficulty with the meditation, but like learning anything new, it takes practice. Thank you, as always Cort, for your great articles and Web site.
I have found curcumin useful. In particular it has allowed me to do low grade / low intensity weights training with minimal post-exertional fatigue and soreness.
@Matthias How much are you taking? And how long before you noticed an effect. I’ve been taking a small amount for some time but have noticed nothing different.
I take 2-3 capsules of Longvida curcumin per day. Each capsule is 500g. Longvida is specially designed to optimise delivery. With many curcumin products you won’t absorb much.
It’s the best supplement I have taken in terms of allowing me to do light exercise without nasty after effects. I started to see benefits after a few days of taking it.
I assume it’s powerful anti inflammatory effect reduces the muscle soreness.
Matthias, thank you for sharing that. I keep trying to do a little strength training and I keep collapsing. I recently started using D-ribose and it helps. I’m going to add curcumin.
Curcumin probably isnt going to work https://pubs.acs.org/doi/abs/10.1021/acs.jmedchem.6b00975
and can have side effects
“Turmeric/curcumin supplements are generally safe, but gastrointestinal side effects may occur with higher doses and they can cause problems for people with gallbladder disease, kidney stones, or those taking blood-thinning, blood-sugar-lowering, or immunosuppressant medications. Curcumin may also inhibit iron absorption. Be aware that black pepper extract (piperine) often added to curcumin to increase bioavailability also interacts with a number of medications. “
Quote from linked study “No double-blinded, placebo controlled clinical trial of curcumin has been successful.” That’s simply false. Here are two double-blind studies on diabetes/prediabetes.
https://pubmed.ncbi.nlm.nih.gov/22773702/
https://pubmed.ncbi.nlm.nih.gov/22930403/
Both were published years before the analysis you linked; therefore, the authors have no idea what they are talking about. That said, I’m skeptical that curcumin would do much for ME/CFS.
Cort, neither I or my sister could stay on LDN. It did help pain – but for both of us it caused severe depression. I did have the vivid dreams too.
How’s the Tramadol working for you?
Issie
Glad to hear that I am not the only one who could not tolerate ldn. It made my pain worse, among other things. I find Youngers interest in opiates/ opiod receptors interesting and I think he’s doing studies on them as well if I read correctly on his research study website. I believe that opiate withdrawal was one of my main illness triggers. And maybe related, years before I ever got sick , the first time I ever felt the dreaded “flu-like” mailaise symptoms, without actually being sick was when I was coming off of a SSRI.
This is the best day for all humans on the earth everywhere.
I don’t know what all this talk is about! I was diagnosed with CFS in 1991, and given disability. I am now 71 years old and have about a half-dozen things wrong, medically.I have been in intensive, severe pain since day one. A day I will never forget! The worst, hideous flu-like illness hit me, and never went away, only got worse! Over the years I was given almost ever drug on the market by ignorant and stupid doctors who thought I was nuts. The only thing that helped was my opioids. Now they are being taken away!! WHY?
Hopefully you’ll have some good news. Better opioid drugs are being worked on and alternatives are being developed. So while opioids are under the gun now hopefully you’ll have more and better options in the future including better opioid drugs. We shall see!
I just came across this website by accident mainly because I’ve started digging into this LDN thing. I’ve been on it since 2015 because of pelvic floor disorder. I’ve had FM for years and used to take low dose buprinorphine until I couldn’t get anyone to prescribe it after my psychiatrist closed her office.
I have had to go up to 6 mg to get any kind of relief and still ended up in the hospital where they gave me tramadol to help stop the pain. I have been stable with that therapy until I hurt my hip. DNA testing I had done showed I had to have higher doses of LDN cause of my metabolism. LDN was at the bottom of the 2nd column of drugs that would work with me. Tramadol is in the first column as the best options for me. Why isn’t a person’s DNA being taken into account? I have the information in my medical records but no one is looking at that. I pray Younger can help with dextro
Thymalin might be the answer.
As a newbie and I had sensory overload processing all the info. and comments that sent me into a Ultra flare
I realized I was way off base in left field about that biomarker as I have no proof or been tested as such. Please excuse my confusion and thank you Cort for clearing my confushion up! One of those blonde moment..lol! Sorry!
A better tolerated version of LDN will be much welcome. I have found it to be consistently disruptive of my (extremely delicate) sleep patterns, and the consensus seems to be that if you don’t take it at night, when your body is rebuilding its neural networks, its endogenous opioid pathways, etc, there’s little point in taking it at all. I can take it in the daytime with little problem other than a bit of a jittery boost when it wears off, but taking it at night is a recipe for a poor night’s sleep and a crash day afterwards. I’m thinking of trying to titrate up from even smaller doses than the prescribed starter doses and slowly let it worm its way into my sleeping pattern.
My biggest interest with LDN, aside from its neuroinflammatory indications, is its ability to increase NK cell count, which has become a bit of a holy grail for me lately. Do we know if Dextro-naltrexone possesses the same capabilites, or will this be something taken into consideration as studies move forward?
Definitely try smaller doses. I was told that taking it in daytime can have similar effects as taking it at night. I don’t know about NK cell counts.
Is dextromethorphan-naltrexone a combination of Dextromethorphan and low dose naltrexone?
I take pure dextromethorphan (obtained with Rx, at a compounding pharmacy for CRPS.) It took me awhile to titrate up to 400 mgs (four 100-mg capsules) to manage my nerve pain. But it leaves me exhausted and feeling hot, which is already an issue with me with MS.
I am interested in going on LDN for Multiple Sclerosis (which I’ve had for 30+ years).
I took LDN for my MS years ago (3.0-4.5 mgs) but stopped as it exacerbated insomnia and vivid dreams. (I never took it in the morning, as some people reportedly are having success doing.). Dextromethorphan was the first thing that helped lessen the burning pain of CRPS. I’d like to lessen the amount of dextromethorphan if LDN can be taken with it.
Well I just noticed this is an old thread, but I will comment anyway….the first time i took LDN it was at 4.5 mg and it put me in the ER the next morning…..I was so sick (this was the next morning, oddly enough) that my boss called an ambulance. The EMT that I was having a heart attack and is feeding me nitroglycerin on the way to hospital which is just a couple of blocks away…..I was NOT having a heart attack, but I was having severe nausea, etc from the LDN. I also have severe reactions to opioids and am always violently ill from anesthesia after surgery…….FAST FORWARD. Went back and tried again with a much lower dose, I think starting at .5 mg. I’ve now worked up to 4 mg. Doing it that way eliminated all side effects but the disturbed sleep, I’m still struggling with that somewhat. But I am more alert in the daytime, and while I am not well, I have more “good” days than I used to. Meaning I can tolerate being upright and/or active longer. My cognitive issues – remains to be seen. Part of my problem is I forget to take the meds at night sometimes, so I am not consistently dosing. I just recently hit 4 mg and I am hoping that when I get to 4.5 – or, based on this article, maybe up to 6mg or more….I might see continuing improvements.
So I definitely could not tolerate 4.5mg initially, but working up very very slowly (over a period of about 6 months) I am tolerating it pretty well and seeing some improvement.
Is there any update on the availability of dextro-naltrexone, I wonder? Or the dextromethorphan study?
October 2018 – “Younger has begun to assess the data from the study.”
January 2022 – No results yet.
Frustrating!
Yes, indeed. True for so many studies. In fact, I would warrant that’s true for 90% of the studies/trials out there. They all seem to take longer than expected to get done.
Do you know if the study ever started even or ran into funding problems?