

The Deconditioned ME/CFS Patient?
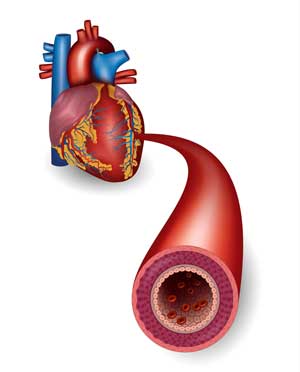
A huge (n=345) 1998 UK study set the stage. The smaller, less muscular hearts and carotid arteries found in ME/CFS made it clear – at least to those researchers – that both physical and cardiovascular deconditioning was present in ME/CFS. They recommended a graded exercise program to recondition them.

Early studies suggesting that deconditioning ran rampant in ME/CFS gave CBT/GET proponents ammunition for their conception of ME/CFS as a behavioral disorder.
That finding gave cognitive behavioral therapy/graded exercise therapy (CBT/GET) practitioners in the Netherlands, the U.K. and elsewhere a physiological basis for their hypothesis that the distress in ME/CFS was not primarily physiological in nature.
Instead, they posited that the disease was more due to a lack of activity caused by a hypervigilant state which falsely ascribed catastrophic meanings to every symptom. People with chronic fatigue syndrome (ME/CFS) were so terrified by their symptoms that they’d stopped moving and become deconditioned (and now actually did have a physiological issue to deal with). As deconditioning begot more deconditioning, they became weaker and weaker.
The hypothesis proposed that people with ME/CFS were locked in a vicious cycle of maladaptive behaviors that behavioral programs like CBT/GET could get them out of. Taking away their hypervigilance and catastrophic thinking patterns would get ME/CFS patients moving again, and once that happened, they would return to health or at least improve markedly.
UK and Dutch funders embraced the deconditioning hypothesis, funding study after study of CBT/GET. Finding that, compared to sedentary healthy controls, people with ME/CFS had reduced exercise capacity, Fulcher and White asserted that physical deconditioning helped to maintain physical disability in CFS and recommended graded exercise therapy (GET). In a 2001 Lancet article, White again highlighted the problem of deconditioning in ME/CFS.
In 2002, a Dutch team lead by HJ Timmers produced a devastating result. A tilt table test of people with chronic fatigue syndrome (ME/CFS) revealed they’d had abnormally high heart rates at baseline and low stroke volumes when tilted. The authors’ conclusion – that the ME/CFS patients were deconditioned – was not surprising: deconditioning causes exactly those symptoms.
The heart is a muscle; if it’s not used, it weakens and loses some of its ability to forcibly expel blood, resulting in reduced stroke volume. It compensates for the loss in stroke volume by beating faster. Given that, it was no great surprise that Timmer concluded that deconditioning was present and helping to perpetuate ME/CFS.
In truth, though, the deconditioning findings have never been entirely consistent.
A small Dutch maximal exercise study concluded that physical deconditioning was not perpetuating ME/CFS, and in 2005, Buchwald – a researcher not known for her embrace of physiological aspects of ME/CFS – concluded that chronic fatigue syndrome was not associated with deconditioning.
More directly, Workwell’s and Betsy Keller’s two-day exercise studies found dramatic drops in energy production on the second day of an exercise test which couldn’t be explained by deconditioning.
Despite the fact that through its funding, the UK government has promoted the idea that deconditioning is a key factor in ME/CFS, ironically it has never funded studies designed to definitively demonstrate that this is so. Instead, it has relied on indirect results with sketchy interpretations.
The costs of its mistake – decades of funding thrown down the wrong rabbit hole – may very well be too high for it to admit. The cost of maintaining its illusion, on the other hand, may be getting too great as well. If the answer to the deconditioning question wasn’t staring the CBT/GET proponents in the face before, it is now — in the form of a very large Dutch study (is that a conflicted country or what? :)) that was recently published.
The Dutch Study
The Abnormal Cardiac Index and Stroke Volume Index Changes During a Normal Tilt Table Test in ME/CFS Patients Compared to Healthy Volunteers, are Not Related to Deconditioning. Van Campen, Visser. The Journal-of-Thrombosis-and-Circulation. 7 November, 2018
The large Dutch study found no evidence that functioning in ME/CFS was associated with measures of deconditioning.
Peter Rowe, one of the reviewers of the study, said a couple of months ago it would (or should) once and for all end the myth of deconditioning as a central factor in ME/CFS.
It’s rare that we get a study big enough to compete with the several hundred person CBT/GET trials turned out by UK funders.
This 150 person study did the Timmers study one better. Timmers assumed that the higher heart rates and lower stroke volumes found in the ME/CFS patients were due to deconditioning. Using a questionnaire (SF-36) designed to assess functionality, the Dutch researchers set the stage for the study by dividing the ME/CFS participants into three groups: mild, moderate and severe functional impairments.
If deconditioning is a key feature of ME/CFS, then the markers researchers have pointed to for almost 20 years as a sign of deconditioning in ME/CFS – decreased stroke volume and cardiac output – should be lower in the most functionally disabled patients, higher in the next most functionally disabled group, and so on.
They weren’t. All the groups had essentially the same stroke volumes. The bed rest the researchers were so sure was significantly impairing the ME/CFS patients’ stroke volume – really wasn’t. Even the more conditioned ME/CFS patients had significantly reduced stroke volumes compared to the healthy controls.
Personally, this made perfect sense to me. I am not fit but I am hardly deconditioned, and yet a single maximal exercise test revealed several significant abnormalities.
Something else was going on. The authors suggested reduced blood volume and abnormal autonomic nervous system functioning – two well-documented issues in ME/CFS – may be to blame. Other possibilities include problems with venous compliance, which allow the blood to pool in the veins of the lower body, thus reducing blood flow to the heart and stroke volume. Mitochondrial problems may play a role as well.
Make no mistake: deconditioning is present in ME/CFS, and if you can recondition yourself, it’s all to the better. Deconditioning is, however, not causing ME/CFS, and if that’s true, then approaches like GET can, at worst, cause further deterioration, and, at best, tinker around the edges.
- Check out Workwell’s Letter to Healthcare Providers for a research-based assessment of GET from a group of exercise physiologists.
Yet CBT/GET studies are still being funded as if they’re going to solve something fundamental in ME/CFS. Over the past two years or so, at least four large CBT/GET studies, some containing hundreds of patients, have been published.
The real answers will come when researchers get at the physiological abnormalities that are impairing exercise in the first place in this disease.
Conclusions
A very large 1998 exercise study which concluded that deconditioning ran rampant in ME/CFS laid the groundwork for decades and millions and millions of dollars of CBT/GET studies, mostly coming from the UK and the Netherlands.
That study forgot to do one thing, though. If deconditioning is causing or contributing greatly to ME/CFS, then signs that deconditioning is present (such as stroke volume) should be more pronounced in the sicker and less pronounced in the less sick.

GET is based on the idea that deconditioning is a major contributor to ME/CFS. This study suggests otherwise. Will the CBT/GET funders listen?
Two decades later, a large Dutch study did that analysis and concluded that deconditioning was not responsible for the impaired stroke volume and other measures that were once heralded as a sign that deconditioning played a prominent role in ME/CFS patients’ disability.
Instead, issues like low blood volume, autonomic nervous system, blood vessel and/or mitochondrial problems (the options are plentiful!) are likely causing the cardiovascular abnormalities in ME/CFS – and keeping patients in bed, in the house, away from work and/or off the exercise circuit.
With the deconditioning hypothesis steadily being eroded by repeat exercise study results and studies like the Dutch one, the basis for funding the massive CBT/GET studies would, one would think, be eroded as well. Not yet, though. Four large CBT/GET studies have been published in the last couple of years.






Thank you Cort for this most recent and informative report. It suggests to me that we need to learn more about this aspect of CFS through anecdotal evidence and the observations of those outside the laboratory research paradigm. Howard Bloom, the famous publicist and writer, is a CFS victim who might wish to contribute his valuable insight to this new development in the Deconditioning hypothesis and exercise studies.
That would be great.
http://articles.latimes.com/1986-06-07/news/mn-9956_1_lake-tahoe
160 Victims at Lake Tahoe
Chronic Flu-Like Illness a Medical Mystery Story
June 07, 1986|ROBERT STEINBROOK
INCLINE VILLAGE, Nev. — Sandy Schmidt, 42, came down with the mysterious illness soon after she ran a marathon in San Francisco last July. She got better before becoming sick again this spring, forcing her to quit her job as a business office manager. Running even one mile now would “put me in bed for a day and a half,” she said.
Schmidt is among 160 residents of Lake Tahoe’s North Shore who have been diagnosed by two local physicians since the winter of 1985 as having a chronic flu-like illness in a medical puzzle that has assumed national proportions.
“The heart is a muscle; if it’s not used, it weakens and loses some of its ability to forcibly expel blood, resulting in reduced stroke volume. It compensates for the loss in stroke volume by beating faster.”
As an engineer, I know something about cavitation. That is, when pressure is to low at the low pressure side of a pump and the pump is pumping hard it does create a vacuum on the inlet side. Mind that physics says that all fluids including water cook at lower temperatures when pressure is lower and at higher temperatures when pressure is higher. An example of the first is water cooking at much lower temperatures high in the mountains due to low air pressure. An example of the later is the pressure cooker. Due to the higher pressure, the cooking temperature increases making food well done faster.
In a pump this vacuum creates tiny bubbles which are incredibly hard. That’s another thing of physics: very small droplets or bubbles are very hard. Think of the soft big drops of a rain shower versus the tiny droplets of a water saving shower that kinda hurt the skin. Those tiny bubbles destroy the steel of even a high quality pump within hours.
For the hart, evaporating part of the blood and creating a gas bubble out of blood is no good thing for sure either. In fact people have been killed by injecting them with nothing but air, causing hart failure. It’s for that reason nurses always pinch out the air of an injection needle.
Now how could we get a vacuum at the inlet of the hart? Combine narrow/constricted veins and low blood volumes. That gives only modest quantities of blood flowing back to the hart each second. If the hart would contract in a strong forceful way and too few blood flows in then at the very least a very strong pressure would be created at the hart wall, potentially causing rupture or other damage. If the expansion of the hart were fast enough a partial vacuum would form. That would be heavily damaging.
So how to reduce that risk? Only expand the hart with moderate force. That will reduce that risk a lot. As this will mean low volumes displaced per minute, higher hart rates are needed. The hart just protects itself from the poor blood flow to it due to our strongly constricted veins. Voila, no deconditioning needed.
The above is theoretical. But I do like more solid indications. I had done several small successful experiments based on this idea.
The latest simple experiment was the following. Late at night I often get my heart rate going very high but “sounding” shallow. So it often starts to beat very fast (like estimated triple the normal speed, too fast to count) but very weak.
One recent early morning I woke up laying on my side with again such fast hart beat. I was laying on the liver side (opposite side of the hart). I decided to put the idea once more to the test: Laying that way my hart was 15 to 20 cm higher then if I would lay on the other side, with the hart closer to the mattress.
If the theory was correct, turning around would improve blood flow to the hart and help stabilizing my hart rate. The results were AMAZING: within 5 to at most 10 seconds, my heart rate dropped from probably over 150 weak beats per minute to a far more stable and firm hart rate that resembled 60 beats per minute. I did not count but it was a “slow, stronger hart beat”.
That by far was the most eye dropping hart rate experiment I ever did.
The same happens to me every time. I am a severe patient and 100% bedridden. What do you make out of it? What about some kind of energy deficient state like mitochondria in the heartmuscle that are simply not functioning well. Would that not have the same result? If you put pressure on your heart by laying on your lect side, your body would simply need less energy to pump?
Hi Christoph S,
Thanks for replying! I did find such very abrupt change and normalization in hart beat a very distinct feature so I wondered if others could have the same. If so, it would IMO be that mind blowing to doctors that they could not possibly deny that this must be very clearly a biological thing rather then something in the mind.
If it were psychological it would point to “psychological superpowers” rather then to psychological weakness ;-).
I only discovered this recently.
Before I was able to normalize my hart beat by having a very forceful breathing pattern for about 5 minutes. Changes were far weaker and disappeared within 15 minutes. This one stayed. It was also quite painful to the heart and diaphragm by putting a lot of pressure on it. It could have been the pressure on the hart doing it but I rather think it was the pumping action caused by very large volume changes of the abdomen. I abandoned perfecting this method as it did not feel safe nor healthy.
Another way I can stabilize the hart rate going crazy fast is by standing up and moving. It works better and is part of my nightly improvement routine I’ll describe very soon on the forum. It takes more time to get heart rate stable then with the more violent breathing technique, which is a minus at night, but results last longer (half hour to full hour). As this should not increase pressure on the hart I believe it is the blood flow to the hart that does it.
One can say standing makes blood flow to the legs, but it also flows from the head to the hart. This supposes blood accumulates in the head at night to some extend.
Moving the legs improves results. As this activates the “leg blood pump” pumping blood back to the hart, I tend to go for this option.
As I managed to get this unstable hart rate a lot less frequent then before it’s kinda hard for me to plan testing. But if it occurs I’ll try and put my hart to rest by applying appropriate force to it while laying on the liver side (I’m in better condition then you are currently, that will probably be too much for you).
*If* you were sure the following is perfectly safe in your condition you might consider laying a sack with some stuff in on your hart side if it happens to you and lay on the liver side. The sack should be flexible enough, more like a bag of grain then a wooden board. Depending on your weight I guess 5 to 10 kg should be a good approximation. For safety, starting with 1 or 2 kg would be wise!
I’ll see if I can find a suitable bag and report if and when I have information available.
*If* you were to do something please report results. But keep safe first!!! As comments on this blog will die out someday you can contact me by using the account messaging option. My account on the forum goes by dejurgen too.
If this finding were reproduced by several of us, at least a subgroup of patients would not only get a hard to deny biological marker, but the medical community might take note as about 5% of fibrillation patients are near untreatable and that is considered a serious condition worth funding.
“If you put pressure on your heart by laying on your lect side, your body would simply need less energy to pump?”
My educated guess on physics would say that it would rather be the other way around. The hart volume (and of it’s chambers) will decrease in both compressed and expanded state, the volume difference between both extremes will be lower so lower amount pumped per beat for same effort.
Plus all cross sections will be reduced including of hart veins and arteries will be reduced increasing flow resistance.
Compression will be easier thanks to the force. But it is said that all muscles including hart muscle have more difficulty expanding then contracting. If true, expansion would be the bottleneck in low energy persons and should be hindered extra, leading to even worse hart functioning.
Still, it’s only an educated guess.
By chance I had a less clear hart beat problem this morning when waking up. It had normal rate beating plus on top of it some continuous probably twice as fast weak beating while laying on my back.
I tried to put various amounts of pressure on the hart side by applying force on it with my hands and part of my arms when laying in that position but to no avail. I did so by not elevating my arms too much in order to have less interference from additional blood from the arms flowing back to the hart due to gravity.
I then turned to lay on the hart side (no longer putting manual pressure on the hart side) and it became a clear slow hart beat in 4 seconds. But after 5 minutes it began to resemble the previous state a bit. Another 10 minutes later while still laying on the hart side it was clear and slow again and remained as such.
This sounds like it may be atrial fibrillation or some other rhythm. Have you checked this out with your Doctor?
The above gives us a potential clue to a very simple experiment helping to put that idiotic
“The hypothesis proposed that people with ME/CFS were locked in a vicious cycle of maladaptive behaviors that behavioral programs like CBT/GET could get them out of. Taking away their hypervigilance and catastrophic thinking patterns would get ME/CFS patients moving again, and once that happened, they would return to health or at least improve markedly.”
to the grave:
Have 5 groups:
* A) healthy control group
* B) ME patients group without POTS/OI (orthostatic intollerance)
* C) ME patients group with POTS/OI
* D) FM patients group without POTS/OI
* E) FM patients group with POTS/OI
* Measure their hart rate in rest (and beat strength or cardiogram if possible).
* Let them lay for (for example) 5 minutes on their right side. Measure hart rate.
* Let them lay for 5 minutes on their left side. Measure hart rate.
* Repeat a few times if needed
* Compare results; results may be sufficient to be even a simple first but incomplete diagnostic tool. Less harsh then a two day exercise test if it worked.
If the naysayers still think it is in the mind, then redo experiment with sleeping people who often roll over at night and don’t know on what side they sleep. Record simultaneously hart rate, laying position and check with brainwaves if patient actually sleeps.
The first test might even succeed with an online test setup with patients with a reliable hart beat meter and some healthy volunteers. Just needs a bit of predefined methodology to avoid bias. We can do it IMO as it’s hard to define this as a true medical experiment.
Hi. Since you’re interested in this sort of thing I wonder if you could include lying on your stomach ? Sleeping on your tummy is heavily “interpreted” by the psychs and indeed as we get older most humans find it less comfortable but in fact it takes stress off heart and increases lung perfusion.
Hi Lucy,
Thx for the suggestion. I’ll try short episodes of it when I have problems breathing or have that high pulse rate again.
It probably won’t be a good fit for me to do on a regular base as I have painful tummy due to gut problems and a stiff neck that hurts on a 90 degree bent but I’d like to see and learn what it does with breathing and hart rate. Every piece of information helps to solve the puzzle.
Problems with venous compliance is interesting. I often find my lower body is very hot whilst my upper body is very cold. So much so that on a cold night in bed I may have my legs bare and uncovered by bedclothes whilst I wear a thick fleece top, cover my torso with a thick duvet and have a hot water bottle next to my chest. I wonder if those symptoms are a good fit with venous compliance problems.
Interesting. I don’t know but problems that occur from the feet up can have to do with circulation or small nerve damage.
I am opposite to you. It is unusual for my upper body to be cold but my legs are permanently stone cold. However my feet and hands are always warm.
Go figure!
Because we know muscles exerting themselves trigger a cytokine response and phenomenal gene expression in the immune, adreneric, and sensory systems beyond healthy controls. The heart being a muscle (and lung muscles) is probably why many ME/CFS patients are constantly unwell. They are muscles unlike our normal muscles because they have to keep exerting themselves even at rest. So Perhaps ME/CFS is a constant low level of PEM caused by the heart and lungs always exerting themselves.
What an interesting idea. It sure makes sense to me. I guess the brain would be in there as well. Staci Stevens has suggested that because the small muscles that move the lungs are in constant motion problems would show up there – as you suggested.
In this sentence, “should be lower in the most functionally disabled patients, higher in the next most functionally disabled group, and so on”, I think you mean that the it should be lower in the least functionally disabled patients, higher in the next most functionally disabled group, and so on.
In response to dejurgen, when blood pressure lowers, heart rate rises to maintain stroke volume (the volume of blood pumped out of the ventricle with a contraction of the heart). So if your blood pressure drops, you want your heart rate to increase to compensate. But with ME/CFS, the autonomic nervous system is out of whack, so it’s hard to know at times why your HR is increasing.
Karen, I think Cort has it right that the stroke volume whould be lower in the most functionally disabled (not abled) group. The more dis-abled, the less stroke volume being pumped (if I’m understanding this myself…).
It’s a weird sentence I admit. I had to read it over several times but I think it’s correct – the worse off the patient the lower the stroke volume.
That is a very bad logical error in the 2002 Timmers paper to attribute high heart rate and low stroke volume on tilt to deconditioning when those could be caused by other things such as low blood volume, problems with autonomic nervous system, blood vessels, and mitochondria.
You find A. B can cause A. But C can also cause A. And D, E, F can also cause A. And things you don’t know about yet can also cause A.
So how do you conclude from A that B is causing A? You can’t. Not with the information you have. A does not tell you there is B.
It’s on the level of correlation does not imply causation.
For a whole cadre of “scientists” to follow that basic error for decades is astounding and sad. Apparently writing and defending a dissertation is far from enough to qualify scientists with basic logic and research methods.
Great point! Isn’t it something that they went right to the deconditioning angle when others were available? It was the answer others wanted to hear I guess….
It always amazes me that as debilitated as I am 99% of the time, when I absolutely have to go somewhere, even if it’s just to the mailbox to grab a package that the mailman was too lazy to bring up in an elevator , I sometimes walk just fine. But a lot of the reason I can walk Better Than I Used To is I don’t walk as often as I used to. I was retaining water and getting post exertional malaise and also experiencing horrible problems with my lymph nodes in one leg when they needed to pick up the pace on circulation. I couldn’t even go up 2 steps on my porch without my knee blowing up. it truly was much much harder to walk the same distance when I was trying to do it every day. mostly bedridden has improved my ability to get around without serious repercussion .
The rapid muscle failure & absolute weak as a limp noodle legs came on instantly with disease onset. and I have been walking all over the place for years every single day. I loved it. But just overnight I couldn’t stand up if I had squatted down to pull a weed from the flower bed. It was quite shocking! But my legs haven’t grown any weaker for needing to stay in bed so many years. It amazes me like I said earlier. Now I can’t even walk without a limp initially. That changes after I’ve been out of bed for about an hour, even if Ive been seated most of the time. Then it starts to feel like I’m walking through drying cement that is thigh deep..
Basically where I’m at with the disease and my muscles can be summed up as I walk into the doctor’s office and I limp out. That’s my limit. And I can’t do that everyday. I actually get post exertional malaise 36 hours after every doctor’s visit. But as far as muscle strength goes it’s the same now after being mostly bedridden for so long as it was when I was still up and moving and then crashing and burning. My pain levels have gone down quite a bit as well. perhaps there’s less lactic acid being pumped into my muscles? whatever the reason lying in bed seems to have benefited me in regards to how often I experienced post exertional malaise, and how much time I actually spend and what I referred to as a comatose state. I know it’s not a coma, but I would really be curious to see what the brain wave activity looks like on a sleeping me CFS patient experiencing post exertional malaise?
Long before I was ever diagnosed I had a sleep study done and they said I woke up 42 times during the night, which I did not remember at all. And my brain totally skipped over the two restorative phases of sleep. Interesting.
this muscle thing is an odd one. logic tells us that if you don’t exercise your muscles are going to get weaker. But that’s not the case in my experience with this disease. But then again exercise in general doesn’t produce the results in our physiology like it’s supposed to. I guess we shouldn’t be surprised that the mostly bedridden patient isn’t getting weaker from being mostly bedridden. It’s a very odd disease, and I think we’re at a point now where nobody should be surprised when things are opposite of how they should be with the physiology of me CFS patients.
“But as far as muscle strength goes it’s the same now after being mostly bedridden for so long as it was when I was still up and moving and then crashing and burning.”
Well resting hasn’t rehabilitated you and bed rest hasn’t worsened what was already a bad situation. Your system is just as it was…I wonder if that indicates that your muscles are beyond being deconditioned – that whatever you have is worse than being deconditioned.
Nobody here talks about nutrition and supplements rebuilding the immune system and the damage CFS has done to the body, but most keep looking for a magic pill. There is not one, at least in the near future.
I am curious if y’all have ever regularly taken supplements recommended for CFS by the late virologist Dr. Martin Lerner, MD, and many CFS specialists since then, that help cellular ATP production?
These include Magnesium, ubiquinol (CoQ10), L-carnitine, D-ribose (<a sugar), and Vit B-3.
Also the anti-virals iodine (Iodoral or Lugol's), Whole Food Vit C, zinc, and L-lysine, then some selenium (+200mcg/day) to help thyroid and adrenals recover.
Adenosylcobalamin form of B-12 is supposed to help nerves heal. I know my brain fog is reduced since I added that.
I had good luck with them in terms of upping my energy from a CFS Energy Index Point Score of 1 to a 3, and reducing FM pain along the sides of the legs. It took over a year. I still take a couple days to recover from exercise, and have setbacks, but am slowly improving.
Found that Cordyceps Mushroom capsules helped with oxygen uptake, since I often felt like my muscles were not getting enough O2. Now I can bicycle on the flat to meet my friends for coffee.
HRV also increased, which means the vagus nerve and heart is more responsive and healthy. (See EliteHRV app for info on how to measure it at home; 60 to 80 is the non-CFS rested normal on their 0-100 scale).
Cutting out gluten, dairy, and soy (mucus-causing foods) this past Fall helped get CFS Energy from a 3 to a 4, but then I overdid it and set myself back 1 level for 2-3 months.
So try the above if you aren't already on it (I assume most here already are?).
“I had good luck with them in terms of upping my energy… …It took over a year.”
Wait, are you saying you didn’t feel any noticeable difference in let’s say the first month when you took the supplements but had to take them longer to see slow improvements?
With me, no single supplement ever worked for me. But if it doesn’t work the least bit after a month I do consider it a failure and waste of money. Is that too soon?
I still do take some cheaper supplements as they are supposed to help but as I have other things like fighting food intolerances that work better I am unable to determine if these supplements do help a bit over a lot of time.
Everyone should have a Tilt test and they should follow this path in their reseach on this as explain alot as what is happening to all of us as well as elevations pressures..below sea levels as well…thanks Cort ?
I agree. I honestly think all of use have some orthostatic problems whether we meet a definition or not. A good long tilt table test that included all sorts of assessments would be very revealing.
Sorry off topic. The Younger Lab’s latest newsletter says their blood draws are showing the cause of CFS, this sounded quite a bold statement, do you know anything about this Cort?
I heard that many times before, there is not one cause for CFS, so it can’t be true. That said, Younger produces very nice colord pictures with ‘special’ MRi technigue. Her thinks it shows neuroinflamation. His findings are not accepted in neuroscience to make this statement. Only the PETscan in Japan will be accepted.
I think it’s good news. Younger is not one to overstate. My guess is that he’s getting a some proximate causes in the blood draw studies – immune abnormalities. I do think this disease is very multi-systemic and at some point someone will to piece it all together – the immune abnormalities, the blood vessel problems, the energy production problems, the brain problems – It will all fit at some point and I don’t think we have that overarching hypothesis which puts it all together. Cortene has a pretty good one though! The metabolic hypothesis is another possibility.
Cort when do we expect to hear if Cortene’s drug demonstrates efficacy in treating our blasted disease?
I so much agree with you Cort, that what we need, that has so far been elusive, is a really convincing overarching ‘theory of everything’ for ME/CFS, from its variable initial causes through its ongoing variable trajectory.
An overarching theory may be so elusive, at least in part, because, as a science writer was saying on the radio today, for 100-odd years scientific research, including medical research, has been conducted almost exclusively in the form of specialised areas of knowledge and investigation. There are no or few bona fide researchers looking for ‘unified theories’ ie how all the different areas of knowledge fit together.
In biological terms, it’s like the difference between the detailed study of individual forms of life, and the study of ecology – how multiple biological systems interact and constantly affect each other, often in unexpected and even dramatic ways.
IIRC from the radio segment, for many scientists, any attempts to develop unified theories tend to be treated with scepticism, perhaps because it’s simply too foreign to scientists trained all their lives to break everything they want to study down into its component parts, homing in on minuter and minuter detail, but rarely going the other way – panning out to see how the bit they’re studying fits together with everything else in complex ways. It seems to me there must therefore be an inadequate body of knowledge, skills, research techniques and protocols in this area of science – the very area that it seems to me is most needed for studying a complex multi-systemic disorder/pathology like ME/CFS.
I think it was in the recent OMF Symposium that Ron Davies said re the growing body of diverse hypotheses and results that researchers into different aspects of ME/CFS are at last producing, something on the lines of ‘so, we know all these different things are happening in different parts/systems of the body/brain and we know they are all communicating/interacting with each other, and thus, somehow, causing ME/CFS; we just have to work out how’.
No body system is an island, and most especially clearly is this so in ME/CFS. I believe if we are to fully solve ME/CFS (as opposed to just finding drugs that temporarily suppress/ relieve individual symptoms), we need science itself to evolve, in order to clearly and fully map the ecology of ME/CFS in all its diverse aspects, as a complex disease system with many interconnecting elements.
Since I’ve long believed a neurological dysfunction to be most likely the core originating problem from which all the other body system dysfunctions develop, I too am most encouraged and excited by the Cortene hypothesis, amongst all the other current developments in research, if it really can get to the core of the neurological issue and reset the switches, as it were, with a drug.
Although I have some criticisms of the book as a whole, I’m also very impressed by the very detailed hypothetical ‘theory of everything’ proposed by Dan Neuffer in his book ‘CFS Unravelled’, which proposes a (to me) pretty convincing sounding bio-mechanism for the whole thing, starting with an assault or constellation of assaults on the body (the triggering infection/toxic exposure and/or other stressors) that the amygdala interprets as an existential threat and which step by step, system by system, as he maps out, throws the the whole of the body’s delicate ecology out of whack.
I’m no scientist (other than as an amateur sleuth such as all of us PwME by necessity become) but it appears to me Dan’s comprehensive theory fits nicely with the (somewhat more limited, unless I’ve missed something) Cortene hypothesis. The crucial point to me, like you say, is to find something that incorporates everything – all these observable things that are going wrong with us from the mitochondria to the brain to the gut to the immune system, to the cardiovascular system, et al, and to understand once and for all, as a clear bio-mechanism, how it all links together.
Not having consistently followed your blog, Cort, I don’t know if you’ve already reviewed the Neuffer book/hypothesis, but with your brilliant ability to analyse and synthesise complex information, I’d be really, really interested in your view of how it might fit with the Cortene hypothesis, and what puzzle pieces, if any, you feel may still be missing from either or both theories. 🙂
Thanks Elizabeth. I’ve heard good things about Dan’s book and will read it and report on it. Dan is a very smart person 🙂
I had an ultrasound of my heart the result was I had dyastolic dysfunction also a Team of Cardiologists at Southampton General Hospital put Cardiac monitors on me in a standing position then after
seeing how my heart was not functioning properly they refused to let me walk on the the Treadmill saying it was to dangerous to my health I was refused anymore testing so anyone saying this illness is deconditioning
has some lose screws in their head they are Mad & totally insane. Prior to becoming Sick I was on the verge of turning a Professional Boxer I was in the best shape of my entire life pound for pound I gave beatings
I trained everyday in the last 10 years prior I never missed one day of training 7 days a week daily even Christmas day was not missed I was going places in Boxing…CBT/GET is pure complete bullshit fraud.They
will be getting Sued for damages & I will make certain a Criminal Public inquiry will be happening 100% & they will be liable for monetary damages.
Wow Aidan – you are a great example of how ME/CFS can fell even the healthiest among us. Stay tuned for the Lives Interrupted program. I hope you can get your story in there.
Anytime I read about the deconditioning scams I get really, really angry. From the onset of my M.E., I was still extremely active every single day unless I was in a really bad crash. I believed the garbage about continuing moderate exercise, even though my body was rebelling ferociously. I stayed active for 21 years. I had dogs and horses. I finally had to sell the horse farm and downsize.
Because of our family circumstances we only moved about 20 miles from the horse farm, but it was 20 miles closer to my daughter’s university.
The emotional and physical strain of that move reduced my ability from roughly 50% of a healthy person’s energy to 15% of a healthy person’s energy. Now it’s nearly 5 years later, and I have not recovered what I lost.
This isn’t quite on the same subject, but it really bothers me that we call the disease ME / CFS or just CFS. We all know this disease is profoundly more than chronic fatigue. As Cort wrote, it is a multi-symptom disease. The pain and weakness can be so intense, I curl up in a fetal position surrounded by pillows, weep and contemplate suicide. I would never take my life because I still have a lot of rescue animals, and I love my family. I’d like to see my 8 year-old grandson graduate from high school or college. I’m only 61. I might live that long if I’m extremely fortunate.
Even though the cause may not be rock-solid, isn’t there any way we can refer to the disease as myalgic encephalomyelitis? We’re all pretty certain there is neuroinflammation.
When anyone asks me what I have, that’s what I say. It sounds serious, and it is serious. If they ask what it is, I say it’s an autoimmune neuro-inflammatory disease that affects my entire body in addition to my brain, that the symptoms are profoundly serious and incapacitating.
Another term that absolutely infuriates me is post exertional malaise. It should be post exertion incapacitation, or at the very least post exertion exacerbation of symptoms. I know everybody is in a different place. Not everyone is as seriously incapacited as I am. And unfortunately there are people who are more incapacitated than I am. I just think that as long as people call it chronic fatigue syndrome, who on this freaking Earth is going to take it seriously except for a small handful of neurosurgeons and researchers??
That’s just my 2 cents worth.
Cort, thank you again and again for the work you do. It’s so vitally important, keeping all of us up-to-date on the latest research and issues. I don’t know how you do it. I couldn’t do it. Have wonderful holidays and know that what you do is crucial and appreciated.
I also want to thank all of the members of Health Rising who contribute with comments. You all share so much of your lives, the treatments you have sought over the years, and whether or not they were effective for you. I haven’t even tried. I don’t have the energy to even think about it. All I try to do is manage what I do each day. When my body says quit, I quit. I mean I mainly stay in bed and only get up to take care of my animals. And I’m not taking care of them as well as I should, but I do a much better job than most people. I know that because most of my animals were abandonded at my house.
I hope everyone manages to have some happiness throughout the holidays, even if you can’t decorate or go anywhere. I hope we can hold onto our hope that someday this disease will be properly diagnosed and treated.
CFS, both name and list of symptoms, does not even start to describe the seriousness of the disease for those patients from “moderately” (on the scale of ME, not on the scale of what means being ill for the average person) ill on.
ME or myalgic encephalomyelitis is also the term I prefer to use at it starts to indicate the seriousness of the disease. But I imagine future will tell us that even that name is a strong underestimation of both seriousness and list of symptoms as brain inflammation is only one part of the far bigger systemic or body wide disease it is.
Yet still many doctors, psychiaters and psychologists deny the disease existence as they cannot imagine a disease that devastating could exist without them having the slightest clue as to how that on earth is possible.
I believe that is the main reason of the massive denial we see in medicine, far more then it being a dominantly female disease. At least over here the majority of psychologist clearly is female and the younger generation of doctors starts to be female dominated too.
I don’t know where to begin, but the myth of deconditioning as a cause for ME is an insult to intellect and hard to believe that it is still proposed by anyone. I understand why some, mainly in UK do it, only to protect their pseudo-science that has ruined so many lives, but it is really troublesome that this even is on the agenda in 2018.
The deconditioning myth is mere politics, and has absolutely nothing to do with ME, science, it is not based on real proper curiosity, but only an attempt to derail from other and far more important issues.
Exactly, that’s what the science says – let’s hope that it catches up with the doctors, researchers, family member and particularly the funders who continue to pour huge amounts of money into these studies which could go to so much better use elsewhere.
I was born with a heart that it beats faster than normal to the extent that my mother’s obstetrician thought I was twins. This rapid heartbeat continued throughout childhood, and led to my being hospitalized when I was 14 years old.
I was born in 1961 and there wasn’t technology available to really look at the heart at that time. So after the hospitalization I was sent you Oregon Health Sciences University to a Pediatric cardiologist who explain that my x-rays showed a smaller than normal heart. they explained that my heart had to beat faster then a normal heart in order to pump enough blood. and they also said that it would wear out faster than a normal sized heart which would cause circulatory problems earlier in life then was typical and it would cut five to ten years off my life span. Since this was a long time ago I’m not sure that still applies.
All I know is I had to be put on Atenolol in my early 30s to get my heart rate to an acceptable level when for some reason I began experiencing difficulty breathing when I would be upright. all I knew was that I couldn’t catch my breath even if I was just standing still. we had to stop every one or two minutes at Family outings for Mom to being me to get off my feet and catch my breath. I went to my doctor and he reminded me that my heart used to race much higher than its already higher level heart rate, because it was in fact racing at that moment. I told him I hadn’t thought about that. and I didn’t understand why it was happening every time I was standing up. He told me next time I couldn’t breathe, take my pulse and see if my heart is racing. I’m going to go ahead and Guess That 160 BPM while standing was racing because that’s what it was when I checked it at home later. My resting heart rate was 147. my doctor decided it was time for Atenolol. I take a very low dose because it lowers my blood pressure which is already sub normal. obviously it makes me wonder if that sudden Change in the situation with my heartrate had something to do with timing of onset with me CFS. cuz it was around that time that I started experiencing rapid fatiguing of muscles that I exercised daily. Also muscle cramps that were absolutely debilitating. I also started getting these horrible headaches that also came with muscles in my jaw all the way up to my temple twitching accompanied by muscle cramps in my upper back shoulder and neck. I was extremely light and sound sensitive during these headache episodes as well as very nauseous. it would take about five days of laying in a dark room sleeping 4 everything to pass. I now wonder if that was post-exertional malaise? I also started experiencing soft tissue injury at that time as well as a severe increase in irritable bowel instances. it was absolutely debilitating. I just kind of fell apart physically for no reason. I also ripped muscles and tendons in my rib cage which resulted in about 20 years of wearing rib belts off and on. And my muscles were so weak I couldn’t even blow up a balloon and my cheeks even puffed out from the exertion of trying to blow air into a balloon. I couldn’t make them stay where they stayed all my life blowing up balloons.
One of my really painful symptoms of my me CFS cluster is hyper edema. It’s extremely painful and every time I’m up right I start collecting fluids in my lower extremities. and of course I’ve mentioned before that lymph glands swell from the effort of trying to keep up with the increase in circulation. I’ve got edema all over my body. My eyelids are so swollen it looks like they’re drooping. My face is swollen and I flush bright red from the smallest amount of exertion. definitely not a glamorous disease.
I can also remember that I was always sick what’s the age of eight rolled round and the doctor was constantly telling my mother that all of my blood work showed there was nothing wrong with me. and she was very insistent that yes there was definitely something wrong with me. I missed so much school in Junior High and High School it’s a miracle I graduated with good grades. my work history looked a lot like my school history. I was constantly sick. and to me it felt like I had the flu. but I don’t think people get the flu that often. It’s just interesting looking backwards over my life at all of the things I have been dealing with and wondering if m e CFS had something to do with what I’ve experienced for decades. the more they find out about this disease the more I feel like a poster child for it. I even push my limits on Christmas Eve because I felt strong enough and cognitively firing on all synapses so I wanted to get my living room unpacked from when I moved in over 2 years ago. I did no heavy lifting or sorting but I knew what had to be done in what order it had to be done in and I basically gave orders and was on my feet keeping an eye on what was being done to make sure the wrong things didn’t go in the trash or the trash was left in the house with nowhere to put it. by trash I mean things that I can’t use anymore and since things sat for 2 years in boxes I figured I could live without them. I now have a perfectly clean living room without a single box in it! However I am still experiencing my leg muscles trembling when I get up for the small amounts of time I used to be able to get up for. I remained on my feet that day because I was able the time and I knew that there would be repercussions as I worked myself to total exhaustion. my leg muscles at the time word violently quivering my legs were shaking like crazy. I had also used up all of my cognitive energy organizing and directing the unpacking operation. that led to me not being able to use this tablet without falling asleep within a minute up until today. which is why I’ve been so quiet. LOL! I really like having a clean living room but I hope I’m able to get out of bed and sit in it sometime! The View isn’t very good from this bed!
Happy New Year! I think it’s going to be a great year for scientific discovery in me CFS. Perhaps even adding the name to the dictionary in Android devices so that speech to text recognizes the disease when I vocalize its name and spells it correctly for me? that would be really cool for the name to be that well-known.
Check out Dr. Sarah Myhill’s CFS website, and health guru Anthony William’s 1st and 2nd books.
They provide clues as to the cause and cure of CFS.
Cort published a link awhile ago to the ‘Cincinnati EBV’ medical study (google it), published April 2018, which reflects on Anthony’s ‘theory of everything’ (various HHV virus strains plus toxins producing neurotoxins, inflammation, & chronic fatigue in almost every chronic disease) in his 1st book. Toxin-eating EBV in the organs and brain is the main culprit.
Since 99.99% of adults worldwide now carry at least one strain (out of dozens) of EBV, and various heavy metal and chemical deposits throughout their body, causing different symptoms in every person (no two are identical), modern science has yet to figure it out.