Nothing happens in your body without some of your genes going off like skyrockets. If your body is responding to something – or acting differently in some way – it should show up in a different pattern of gene expression.
If you get a virus, for instance, the virus will trigger or wake up certain immune genes which will then tell your cells to start producing cytokines or other immune factors. That unusual level of immune gene expression can then be picked up in a study.
Unusual patterns were what these researchers were looking for in this fibromyalgia gene expression study. They certainly found them, and a common theme emerged as well. The results suggest that fibromyalgia with its pain and fatigue, and chronic fatigue syndrome (ME/CFS) with its fatigue and pain, are looking more and more like sister diseases all the time.
The Study
J Pain Res. 2018 Nov 21;11:2981-2990. doi: 10.2147/JPR.S169499. eCollection 2018. A predictive algorithm to identify genes that discriminate individuals with fibromyalgia syndrome diagnosis from healthy controls. Lukkahatai N1, Walitt B2, Deandrés-Galiana EJ3, Fernández-Martínez JL3, Saligan LN
This fibromyalgia study used an algorithm from a previous study by the authors that attempted to identify which cancer patients would develop severe fatigue after radiation treatment. Just as an otherwise ordinary infection can have a debilitating effect on some people with ME/CFS, radiation has a similar, fatiguing effect on some cancer patients.
The radiation study was novel in that it assumed that a wide array of synergistically acting genes were responsible for the fatigue and so used an algorithm which looked for clusters of genes which work together to do that.
It found the fatigued group was characterized by reduced levels of gene expression; i.e. the radiation treatment had turned down the activity some of their genes off. Nancy Klimas has found a similar pattern in a network analysis of ME/CFS. In contrast to people with Gulf War Illness, the immune networks of people with ME/CFS lacked connections and were subdued. It was almost as if the immune system had, in some ways, turned itself off.
This study used the new algorithm to reanalyze the results from a prior study of women with FM. The goal was to be able to differentiate FM patients from healthy controls, and it was successful in doing that. First, studies like this typically bring up dozens or hundreds of genes. They do a pathway analysis in an attempt to determine which pathways in the patients’ bodies are most up or down-regulated.
One of the genes that best differentiated people with fibromyalgia from healthy controls plays an important role in mitochondrial energy production.
This study found that a group of 57 genes were best at discriminating people with FM from healthy controls. Those genes were associated with a number of different pathways. Two genes from that group were most highly discriminative; i.e. their expression in the fibromyalgia patients was so different from the healthy controls as to make them stand out.
The results are preliminary – the authors warned that much larger studies are needed to validate them – but are fascinating nonetheless. As with fatigued prostate cancer patients, both genes that stood out in the fibromyalgia patients were down-regulated.
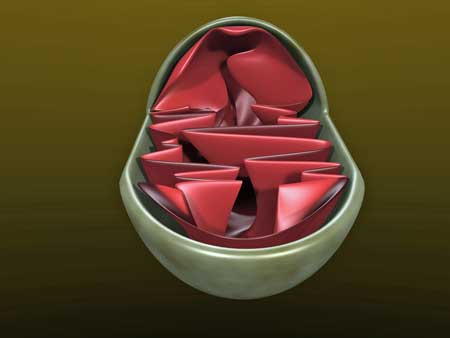
The MRPL4 (mitochondrial ribosomal protein L4) gene encodes proteins needed for the mitochondria to work properly. The down-regulation of this gene suggested reduced mitochondrial functioning may be present in FM.
This is not the first time that problems with the mitochondria – the engines of energy production in our cells – have been suspected in FM. Problems with vigorous exercise, fatigue and pain are, in fact, common in mitochondrial disorders.
A small family study suggested that a mutation in a mitochondrial gene – and the resulting increase in oxidative stress – could be playing a large role in some people with FM and suggested that future studies concentrate on people with family histories of the disease on the mother’s side.
An examination of connective tissue cells called fibroblasts found evidence of decreased mitochondrial biogenesis (fewer new mitochondria), reduced oxygen consumption, decreased antioxidant enzyme expression and mitochondrial dysfunction. Several studies of skin cells have found evidence of mitochondrial dysfunction including reduced energy production and increased oxidative stress The authors suggested that inflammation, increased oxidative stress and mitochondrial problems were responsible for the allodynia – the hypersensitivity to even light touch – often found in FM.
A 2013 review suggested that high levels of oxidative stress (damage by free radicals) are, by impairing mitochondrial function in the muscle and nervous systems of FM patients, causing widespread pain and central sensitivity. Significantly, lower levels of intramuscular ATP, phosphocreatinine (PCr) and fat content pointed to significant problems with the mitochondria in the muscles of FM patients.
That’s just in the past five years. At least five studies before that suggest mitochondrial problems are present in fibromyalgia.
The other gene that stood out was SLC38A (sodium-coupled neutral amino acid transporter), which couldn’t have been a surprise at all. This gene (like most genes) has several functions, including energy metabolism, detoxification, neurotransmitter cycling and nutrient uptake. It encodes a protein called S38A1 which plays a role in the transportation of glutamine, a precursor of the excitatory neurotransmitter glutamate, which has long been suspected of playing a role in FM and fatigue states. The down-regulation of this gene doesn’t seem to jive with the hypothesis that increased levels of central nervous system glutamate are causing pain in FM.
Glutamate is also used as a fuel in the central nervous system, however, and glutamine plays a major role in energy production. Glutamine is the precursor of α-ketoglutarate, which is oxidized to produce the substrates that ultimately produce glucose.
The under-expression of SLC38A in FM, then, if it’s validated, could have major consequences for several systems in the body.
The Hibernation Diseases?
The general pathways identified provided more evidence for the role impaired energy production may play in fibromyalgia. Genes associated with the Akt pathway, which regulates energy metabolism, were markedly down-regulated. This pathway is activated, interestingly enough, by an enzyme, PDK, which is down-regulated during hibernation in animals. PDK suppression during this time results in markedly reduced mitochondrial functioning.
This suggests that the energy metabolism system in FM may be in a state of hibernation. That, of course, sounds eerily similar to Robert Naviaux’s dauer model, which proposes that people with chronic fatigue syndrome (ME/CFS) exist in a hibernation-like state characterized by low energy metabolism.
The other highlighted pathways were involved in inflammation, which given recent findings of neuro and systemic inflammation, was no surprise.
Conclusion
The authors emphasized that no clinical conclusions could be drawn from this decidedly preliminary result and that larger follow up studies are needed.
How intriguing it is, though, to see the idea of a state of hibernation arrived at from two different starting points: from a gene expression study in fibromyalgia and from metabolomic studies in ME/CFS.
The fact that a similar constellation of factors – oxidative stress, mitochondrial dysfunction and inflammation – are showing up in both fibromyalgia and chronic fatigue syndrome is encouraging as well. Time will tell with both these diseases, but a general theme may be emerging.







Could any of this work or others point back to EDS Genes already being studied now? Most work now on EDS Hypermobility is pointing to a Protein
not properly communicating this is where there seems to be the focus now in this most common type of connective tissue issues…
genes are overrated
I have been diagnosed with EDS type 3, hyper-mobility, along with fibromyalgia at age 20. I’ve had it for 10 years now and the EDS has stayed stable while the FM has become significantly worse. So grateful to read your article. Many doctors know the diagnosis criteria but only prescribe pain medications and physical therapy and pass you off to someone who they think knows more and the cycle continues never finding a real answer. I have been told I was exaggerating or pretending and at one point had me questioning my sanity. But I know better. I remember who I used to be and what i was capable of. That has long gone but there’s still a piece if this puzzle missing
They still say there is no cure… But I know there must be something the world is missing. This article gives me hope that research and studies are coming to the beginning of an answer. For all of us who have battled this and been put down by the ignorance of the world i say please keep researching for us. Please keep fighting for us. We need your help desperately. Thank you for the information and to all of you who shared your stories.
I can see how d-ribose is suggested now for M.E. Thanks.
Not if you have undiagnosed (HFI) Hereditary Fructose Intolerance d-ribose can harm
I have FM, and tried D-Ribose. It made me sleep more than I already do…3-4 hours at a time… not for me.
“Sister diseases” is intriguing. However, is it possible Dr. Cheney’s viewpoint that FMS is the pain aspect of CFS (for those with CFS who have pain) is correct? Is FMS ever present without PEM?
I think he is right. Dr Bateman feels the two diseases are on fatigue/pain spectrum as well: on one side FM with horrendous pain problems and on the other ME/CFS with horrendous fatigue problems. Most of us meeting in the middle I think; I certainly do.
For me it was really interesting to learn that mitochondrial or energy production problems could result in pain in FM!
“For me it was really interesting to learn that mitochondrial or energy production problems could result in pain in FM!”
One of the more “effective” ways to get a very quick and strong increase in pain in my legs is to have a mental activity far exceeding the envelope. I often say mental exhaustion “sinks” to the leg.
This is an interesting and encouraging article. Regarding energy and increased pain in FM from a patient’s perspective, I have had FM for 22 years with the classic insomnia and chronic pain. I was able to work through that and be quite productive. In March 2018 I was diagnosed with ME. My pain has gone from a typical 5 out of 10 daily to a 7 or 8 out of 10 daily. I cannot push through the pain because I do not have the energy to do it. I hope that is helpful information.
Interesting Helen. Sorry you are going through this but this does suggest an energy-pain interaction is taking place; the less energy you have the more pain you’re in. It brings to mind Naviaux;s assertion that a body with low energy cannot relax!
I’m wondering where RSD/CRPS fit in with this study. Very similar symptoms.
I was accidently poisoned in utero as a fetus…i had a mass of pain as well as exhaustion was told it was growing pains…at age 9 i got masses worse was diagnosed with Fibro…i thought it was all the same thing but there are definite differences .
I think that really low energy in the mitochondria can have an expressive connection with FM. But why do the vast majority of doctors say this is not true ????? And why are so few studies conducted on this relationship ??
This is really interesting to me as well. I have FMS; my brother has CFS. I experience pain in any of my muscles whenever I use them for anything; even sitting up for too long causes a painful flare in my lower core muscles. However, I don’t feel like I experience fatigue as a symptom, except a little around the time of my period. My brother experiences extreme fatigue with any mental or physical exertion, but overall only experiences mild pain in his feet from time to time. His symptoms started with a prolonged sinus infection; mine with pain in my wrists (originally diagnosed as carpal tunnel syndrome) that subsequently “spread” to all other areas of my body. Has there been any other development along this line of inquiry since January?
It’s fascinating indeed to see what emerges as science progresses. It’s not just that others are looking at more diseases, including FM or CFS. Nor how much our capacity is growing to understand what genes do or metabolics look like for an entire organism. It’s totally intriguing, as you say, to see how many similarities are starting to emerge as we start to get a bigger picture with each of these findings. Thx for sharing!
Let’s hope it keeps up and the research cohere’s around a central or a few central themes.
We like this !
It fits so closely with all that we feel about the illness.
Very interesting article. This article, all though not conclusive sheds a light on many questions I’ve held. My Mother also had FM. Metabolism questions/answers make total sense to me. My fatigue was so severe, the Dr. placed me on Ritalin several years ago as I had been pretty much bed bound for 2 years prior.
I too have had to get prescribed Ritalin to be able to do my job. I don’t know the exact reason causing my “fog” but without the Ritalin, it became impossible to concentrate to get myself to finish a task.
I wonder if the pain literally exhausts my pain and all my energy is spent fighting the pain that it leaves no energy left for focusing.
Or I wonder if it’s the actual symptom of fibro fog that makes everything so difficult including doing things in the moment
Stimulants are very interesting really. The Synergy project tied together a stimulant with nutrient and mitochondrial factors with the idea that the cells needed the stimulation of the Ritalin to produce energy plus they needed the nutrients provided by the supplements to thrive. It’s almost as if they were using the Ritalin to break the cells out of their Dauer state (!). After a time it was hoped – and it did happen for some – that their cells were able to resume normal functioning and they could get off the Ritalin.
Ritalin seems to have something in common with lidocain and cannabis (see comment somewhere else on this blog).
When looking for “action potential” I did find fewer results. But one paper indicated a effect on K+ channels. Looking deeper I did found:
journals.plos.org/plosone/article?id=10.1371/journal.pone.0051910:
“to block voltage-activated sodium channels and therefore eliminate spontaneous action potentials at pre-synaptic terminals that would trigger glutamate releases.”
-> Ritalin too seems to be able to “calm down” the brain from firing synapses in a haywire fashion and help prevent overloading itself.
-> Lidocain and (the wright mixture and use case of) cannabis are able to do the same thing but with another mechanism.
-> While Ritalin is a stimulant, it is also a “haywire brain calming drug” or in part both stimulant and calming agent.
I used phentermine to bump start a weight loss program and also a modified keto style of eating.. and found inmediate relief for my fibro pain. Not completely gone but enough so that I can function again. And the brain fog is gone. Maybe is has something to do with the nervous system being “excited” back unti life instead of hibernation mode.
I’ve had three doctors suggest I try stimulant therapy. I’m seriously considering it. More and more of my days are spent on the couch or in bed. I have been home bound for years.
Did Ritalin help, Diana?
Thank you for another well written and encouraging article!
Thanks!
Hi Cort, thanks for the great blog once more.
Think I might have caught an error: “by an enzyme, PDK, which is down-regulated during hibernation in animals. PDK suppression during this time results in markedly reduced mitochondrial functioning.”
It didn’t made sense to me as I believed it should be up-regulated during hibernation.
PDK up-regulation acts opposite on pyruvate dehydrogenase so up-regulating PDK down-regulates PD and with it the Krebbs cycle IMO.
See also en.wikipedia.org/wiki/Pyruvate_dehydrogenase_kinase and en.wikipedia.org/wiki/Pyruvate_dehydrogenase and
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC20986/:
“Here, we report that genes for pancreatic lipase and pyruvate dehydrogenase kinase isozyme 4 are up-regulated in the heart during hibernation.”
I don’t know! You’re way more up on this stuff than I am. Here’s what the paper said:
Yesterday I was too tired to even notice you included the link to the paper ;-).
Looking into it, I saw that the paper referenced to 5 other papers concerning PDK/PD and each of them was worded in a very difficult to understand way.
Having no energy and exhaustion to spend on digging deeper into it, I believe it could well be a case of “wording creep”.
I see “wording creep” as a mechanism whereby the original of something slowly changes and shifts over time as it is interpreted, cited and recited. Consider this series:
* We have no known mechanism whereby modest exercise can cause PEM like symptoms.
* There is no known mechanism whereby exercise can cause PEM symptoms.
* There exist no mechanism for exercise to cause PEM.
* It is scientifically proven that exercise can cause no PEM.
-> The latter is far too often cited by medical professionals and plays an important role into dismissing and ridiculing our disease and patients.
-> Reality however is that this commonly beheld “truth” is more and more proven utterly wrong by recent real science.
Actually, reference 35 the paper cited and you repeated is written by: 35. Buck MJ, Squire TL, Andrews MT.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC20986/ as I cited in my original comment is written by: Matthew T. Andrews,* Teresa L. Squire, Christopher M. Bowen, and Martha B. Rollins
Basically that’s the same researchers/research group and they say
“Here, we report that genes for pancreatic lipase and pyruvate dehydrogenase kinase isozyme 4 are up-regulated in the heart during hibernation.”
-> IMO that’s the exact opposite of what is claimed by the researchers referring to this paper. However, the important thing that this gene expression down-regulates glucose metabolism is maintained correctly in both papers.
It may sound disrespectful to and trying to talk down the researchers of the gene expression study if I discuss what I believe is an ambiguity.
It is not however. One of the things I learned while doing my Msc from the professor later guiding my Phd was that reading a paper and getting what was truly said was a difficult art. At the time I did find it ridiculous.
However while doing my Phd I learned that interpreting what was truly written and more importantly what was omitted was indeed a difficult art. Even on my core domain of expertise I could miss the key point for months to years or forever.
Contrary to common believe, most top researchers do *not* wish their research to be repeated in the first two years after publication! Top science is very competitive for research grants, top publications and positions. Most ambitious researchers do wish to publish stunning results while giving away as few details as possible.
That way one keeps best funding and grants for themselves and one becomes the one and foremost known domain specific expert. Having your research only repeated after five or so years reinforces the image of how brilliant and visionary you must be. Therefor many of them master the skill actively wording research outcomes so that they can be interpreted in many different ways *and* that most competing researchers will interpret it wrong first time (nothing as efficient to delay competition as to set them on the wrong track). Completely omitting the key points leading to the discovery is also a common trick. They also mastered the skill while doing this while remaining factual correct.
So, my comment does not go against the excellent research they did. Finding gene expressions involved in FM, finding key mechanisms translating those in mitochondrial problems and coming up with a promising link between ME and FM in one research is brilliant! I would not want them to waste time to comb out all of their 39 reference but rather continue their excellent work instead!
Why do I waste energy writing this? Because I believe this “wording creep” keeps alive many firmly held wrong “truths” commonly stated troughout the very difficult and broad medical science domain.
With a disease so complex and behaving so differently compared to most diseases we cannot afford a large portion of “scientifically proven facts” to be in fact “wording creep” and closing off research to the actual core aspects of our disease because “such is impossible”.
If I have one single skill helping me to improve my health in a IMO systematical way I believe it is to see this and have high skill searching efficiently and intuitively through this pitfall.
Getting enough breakthroughs for our disease may require cleaning up this clutter and patients *feeling* this disease are so much more efficient in sensing where these roadblocks are IMO. I’d love to see that organized!
I believe both FM and ME are very high chronic body wide ROS diseases and that much of it is behaving in a slider like way. Setting the slider to more ME, get somewhat less FM and the other way around.
As I have written before such extreme ROS conditions should turn the Krebbs cycle down as much as possible.
“The other gene that stood out was SLC38A” did not say that much. You luckily worded it very clear (thanks for making us understanding it so much easier): “Glutamine is the precursor of α-ketoglutarate”. It is a key intermediate to the Krebbs cycle according to wikipedia.
That further strengthens my believe that our bodies are willfully and very determent to shut down the Krebbs cycle (and glycolysis as well) to very low values in order to save us from devastating oxidative stress.
That points to two further suspects:
* huge long term activation of the pentose phosphate pathway as medical science probably never has seen before in order to produce as much as possible NADPH and even to be a significant fall-back resource for NADH/ATP as Both Krebbs and glycolysis are very likely shut down very much in my view.
-> with it, the supposed very early shifting of aerobic energy production to anaerobic energy production in ME may be largely a very early shift towards the PPP rather then plain anaerobic energy production. A huge PPP activation can easily disguise/be mistaken for a huge anaerobic activation when one does not specifically looks for it.
* huge damage to our body wide heme both in RBC as in mitochondria; ROS can/does damage heme and damaged heme does produce copious amounts of ROS; this forms a nasty vicious circle keeping the disease entrenched; in a response the body decreases heme body wide (known response to damaged heme)
-> result: low blood volumes as reducing RBC count is a good way to reduce body heme, reduced amounts of heme in the mitochondria further crippling energy production and still copious amounts of ROS as even reduced levels of damaged heme are very good at producing ROS.
Thanks for sharing this Cort. This genetic research is getting closer to what is going on in CFS and FMS. I agree that they sister diseases where most of us fall somewhere in the middle of the spectrum. That is certainly the case for me. This theory leads me to believe that successful treatment protocols must alter the gene expressions.
I do also wonder what the link is. I find that despite having been diagnosed with fibromyalgia, I experience symptoms that are like other illnesses like ME/CFS and also actually dysautonomia. On my “good days” when I have no pain, I can be extremely fatigued, even walking up the stairs will send my heart rate through the roof. However, I suffer from a ton of dysautonomia like symptoms including heart palpitations, very (unexpectedly) high heart rate (even in resting mode), severe nausea and throwing up, extreme dehydration (which has taken me to the ER several times).
Doctors tell me it does to mimic fibro but they can’t diagnose me with anything else despite tests. However, recently after a lidocaine infusion, I found not having the “physical pain” really fixed a TON of issues from my fatigue, to my sleep issues to my stomach issues… so I don’t know exactly what it is. I can tell though that my body seems to be working so hard in “flight” mode that all these symptoms are all related!
When I take high THC cannabis for sleep it also really helps with pain. The next morning I am often drowsy but I can walk without pain! My muscle feel relaxed and good instead of constricted and painful…Pain and energy depletion go hand in hand for me.
When first reading Andrea’s comment improving on Lidocaine did sound counter-intuitive. Cort’s cannabis comment helped make it sense.
I unconsciously use tensing my muscles to reduce pain sensation to great effect. Contracting muscles to reduce pain is in fact a natural thing:
What does one do when having stomach pain? Bending over to reduce it. What does one do when having chest pain? Bending forward in such way that “chest length” is reduced.
Why? Maybe because in prehistoric times most acute pain came from wounds inflicted by animals, spears and arrows, sharp stones, thorns…
All of them bleed. Stretching the wounded site longer does open the wound gap and tears it further open increasing bleeding. Compressing local muscles does reduce the wound gap and cross section for blood loss, inhibits further wound tearing, decreases exposure of the wound to dust, dirt or an attacker and compresses local blood vessels further decreasing blood loss.
So the brain rewarding (with less pain sensation) a person feeling a strong an sharp pain if he contracts locally his muscle makes sense.
When being a combined ME/FM patient however having chronic pain spread over the body this has side effects:
* massive contracted/tense muscles (as so often observed), cost plenty of energy and increase ease of further muscle damage.
* constricted blood vessels all over the body, including both capillaries and major veins between hart and head being compressed restricting blood flow body wide.
-> Reducing pain sensation in this view reduces chronic muscle (over)constriction and it’s side effects.
-> Important IMO is to reduce side effects of medications AND to not make the mistake to forget pacing as much as before while feeling less pain.
The above felt not complete however, so I looked into lidocaine.
Lidocaine has another trick upon it’s sleeve https://en.wikipedia.org/wiki/Lidocaine: “Mechanism of action
Lidocaine alters signal conduction in neurons by prolonging the inactivation of the fast voltage-gated Na+ channels in the neuronal cell membrane responsible for action potential propagation”
-> ME (and FM?) patients are known to have brains firing all over the place for the slightest impulse. Being sensory oversensitive is closely related to it. Thoughts are hard to focus and silence and are all over the place and yielding very few results.
-> That is very ineffective. Prolonging inactivation of Na channels *seems* (ones millage may vary a lot IMO!) to be a way to “calm down” the overactive brain, saving energy and allowing it to rest and restore.
That lead to following question: does cannabis do the same thing? Answer is: THC/CBD both change action potential and activation time.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1575338/ and http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3721267/ and searching for “THC CBD cannabis channel “action potential”” all discus this effect too.
Important note: a quick overview show that different blends of cannabis subspecies and THC/CBD ratios can offer opposite effects. The same applies for sporadic versus long term (over?) use.
-> This is in line with the CBD/THC discussions on Healthrisings forum.
Hi Andrea….I had read about your fibro symptoms including the nausea, vomiting and I also get a stomach cramping in the epi gastric area. Any kind of stress brings it on…whether good stress,like having friends over to bad stress like intense pain or being too hot or cold. After much research I found all my symptoms were related to low vagus nerve function which has been weakened over many years of stressful work and lifestyle. I’m now using a tens unit to stimulate and strengthen the vagus nerve so it can calm the fight or flight response much more effectively. I hope t his info helps.
Thanks, Cort, interesting to chew on,
i hope it gets followed up.
That is the key isn’t it? I was surprised at how much evidence of mitochondrial problems already exist in FM. There’s a pretty darn good evidence base – enough I would think for a full-blown examination of that problem.
DeJurgen, in our house we say, Racing-Mind-Blank-Mind! It means what you mentioned… “Thoughts are hard to focus and silence and are all over the place and yielding very few results” in your Jan. 14 comment. Or Blank-Mind-Racing-Mind. Meanwhile, thank you, thank you so much for explaining about researchers/research papers and how they strive to actually keep key info hidden, for the sake of career competitiveness!
“explaining about researchers/research papers… …career competitiveness!”
Hi Elizabeth,
Maybe it is interesting to know that the more “honest/open” researchers do not try to misdirect other researchers.
However it near always makes sense to only release a “controlled” portion of information per research paper.
Let me explain what I did:
* On papers in top magazines of about 4 pages (certain types of publications have predetermined “typical” lengths to follow) I would explain the goal and research setup, methods and results plus go in depth on one key detail.
* Trying to explain more would just clutter a shortish paper too much making it harder to explain things well (as I desired to do, I was not into holding back information).
* As an important plus for me, it allowed me to write “follow-up” papers in sub-top magazines and do so with few effort. That gives more high quality papers (needed in research), they are easier to read and can be “cleaner” referenced to as they contain one main topic per paper making it easier to find the key information in the paper when other research references to your work.
=> So if you want to know more about a certain researched and published topic:
* Know some may try to misdirect your understanding; therefore if it’s over 5 years old try to find papers that used it as a reference: if they build upon this work they’ll often explain why the original work was so important.
* When an author is more open, try to find published follow up work of the same author; it’ll often contain important information further helping understanding what is actually in the original publication.
Great article Cort, the science is getting closer to explaining how we feel as Patients!
Hopefully, this research will take away the mystery of these conditions and patients may finally get the recognition & practical help they need, as with the treatments & support received with a Heart Disease or Cancer?
On the one hand, I am thrilled to see this article… Great job, Cort!
On the other, I’m a bit frustrated, and this is why…
My naturopathic and functional medicine doctors have already figured out I have mitochondrial issues, and are treating them, and I am making progress, but it is a totally one-off situation where I’m paying for most of the tests and treatment as this is on the “bleeding edge” of science. It’s a far cry from the “national standard of care” cancer treatment that damaged my mitochondria and triggered my ME/CFS in the first place, which my insurance happily paid for. I was stunned to find the wealth of resources in the csncer world snd the dearth of them in this one…
@Dejurgen I sure would like to know what tests you are using to test and verify all of the things you discussed. I think we ought to be discussing what tests we can do today that discover what’s going on and inform our treatment plans, so we get better and not just sit around oohing and ahing over the research. I also wish the ME/CFS clinicians would include some functional medicine (and I mean Institute for Functional Mecicine trained, not neuropsych folks who think its all in out heads) or Bastyr-trained naturopathic doctors who practice like this today who could add to what the top ME/CFS specialists are doing, because the top ME/CFS specialists (I have ond of those, too) just arent experts at this.
Tests I’ve had done that have helped uncover my mitochondrial metabolism issues and helped us develop a treatment plan include:
1) a MitoSwab test – which measures mito content and complex I-IV respiration
2) a Genova Diagnostics NutrEval – which tests Krebs cycle metabolites, including ketoglutarate, CoQ10 and antioxidant status, B vitamin, vitamin D, mineral, lipid and amino acid status and heavy metals.
3) an Oraganic Acid Test (OAT) which has some overlap with the NutrEval but is mote detailed in some areas while missing others.
4) genetic testing, of whoch there are several types, which can uncover the isdurs mentioned in the article as well as others that may exacerbate the problems
5) nitrotyrosine testing from HDRI, a marker of peroxynitrites, ehich csn damage mitochindrial membranes and impair complex I. Nitrosative stress has been noted in ME/CFS.
If you find problems, what can you do about them? Get on a mito protocol…
I found I need a lot more amino acids thsn I can eat, and unfortunately not ones in ratios found in most commercial protein powders. I need a lot of asparagine, critical to proper die off of sloppy old mitochondria, BCAAs, lysine, glycine, NAC, methionine, ornithine, citrulline, and tyrosine.
And mito supplements like NAD+, carnitine, B2, and manganese. And methylating nutrients, especially B12, which are used on the mitochondria.
To fix damaged membranes, OV phosphatidyl choline and oral NT Factor have helped.
We need to solve the problems each of us has, and not other people’s problems. I don’t have low blood volume, for instance, so following that advice is inappropriate for me. What I’m short of, you may not be, so customixing treatment to lab results is needed.
Where has this strategy gotten me? Over the past 8 months, my MitoSwab test results changed dramatically towards normal, evidence we are getting somewhere. My energy has improved, too, but the changes uncovered the next set of problems to solve, and I’m hoping thst the changes we are making now will help, along with dealing with my immune system, which I’m also doing.
My doctors are guessing, and it’s paying off, but it’s a long, slow, slog. My labs shoe the complexity of my problems and progress, but I wish it weren’t so difficult and expensive. I’ve looked across the US for a “mitochondria and metabolism specialist” but outside of a lab, they don’t seem to exist. Functional mecicine/naturopathic doctors have the best practical knowledge today, and they are scarce.
We need go be discusding how we can get from n=1 experiments in treatments to a methodology of testing and treatments that can work for us that are recognized as a standard of care. We need more doctors figuting this out and teaching each other about a much larger basket of tools.
Cool science is cool, but we need actionable information that can help cure us so we can get on with our lives…
So true, Learner1. I am often frustrated thinking this is great – we’re getting somewhere – and we are. Every step the science takes forward brings us closer. The practical, get me well side – that is much harder…
I have to watch cancer fatigue research more because I wonder if there’s enough money there for drug companies to get serious about finding solutions…
“@Dejurgen I sure would like to know what tests you are using to test and verify all of the things you discussed.”
Where I live extensive testing is hard to come by. No one at the local specialized CFS/FM center had a single clue what a food intolerance was when I asked for a food intolerance test :-(. From hearsay I learned something like food intolerances do exist and they tested 2 of them at a bigger center further away. However testing there still fell short.
Having no knowledge of many of these test at that time, to few energy to learn more of them and find out where to get tested and more importantly knowing no one who could guide me to put test results to use I abandoned that route early on. Money for tests and supplements/drugs based on them also was short.
So I largely limit myself to using my senses. Having keen senses and set up a method to better feel small differences in energy levels, “dread”, pain, GI symptoms and plain old looking down the toilet are my main “tests”.
I combine these observations with a “special intuitive and kind of pattern based searching” through available scientific information to form my ideas and “test” them by setting up small changes and see if effects are as expected and repeat themselves. Using all kind of “impossible” observations commonly stated by patients helps narrowing down the search space a lot.
Doing so, my aim is to better understand why so many things work for some but not for others or work for some time and then vanish. I believe it would be incredible if we knew roughly of half the things that worked for some patients under some circumstances how, when and why they worked.
Leveraging that knowledge would lift plenty of us out of disease I believe. I wont ever get to the above mentioned goal but I hope to get from 5% of functionality and falling to over 50% and improving in 5 to 10 years time by strengthening my bodies ability to self heal. Now I’m at 25%+ and improving in 3.5 years time.
I’m a long way from frequently being unable to recall my name or address and failing to recall it when trying, from bumping into walls when trying to pass through a door opening due to failing to realize all of my body must pass through it, from having increasing instances of short lived paralysis and having difficulties eating and swallowing food :-). Currently adding chapters to the “Me current improvement” series on the forum.
I hope to help spur this route. Imagine this route to significantly help double digit patients in a safe way to better health. Imagine it to be but one route. Imagine combining it with your route. And that of others like Issie and Phil. And adding scientific progress to it. And all of these approaches helping insight and effectiveness further of the other routes… ;-).
We sure will exchange more ideas over time. Just keep improving and sharing!
Well this is certainly fascinating, and explains my obsession with soft blankies, super-soft pajamas, and the feeling that I can’t wait to get into bed! We’re literally being programmed to want to hibernate!
Yes Ann I agree!! There is a strong pull to hibernate.
Cort; I am trying to fit these findings in with my own experience and hypotheses. If I have had these gene-related mitochondria malfunctions, I have successfully reversed them. I suggest they are not “the cause” but are part of the cascade of malfunctions in FM. Then they self-heal when the cascade is put into reverse with the right protocol.
I have some suggestions for a potential cause of these gene-related mitochondria malfunctions. 1) deconditioning as a result of exercise avoidance. 2) toxin overload from a) infections b) external poisoning c) over-production of exertion-related toxins 3) constant inappropriate muscle-fibre tension 4) excessive energy requirements for all movement due to fascia adhesiveness
Quite possibly not everyone has the genetic response that results in FM being triggered under commonly-known pre-conditions. I have become acquainted with people suffering severe stress and constant inappropriate muscle tension (to the point that it is visible at all times) who nevertheless have not contracted FM – they do not have the tender points in their muscles and they have good flexibility and range of movement!
Mitochondria being implicated in energy AND pain is interesting; but what I am most looking out for, is what causes fascia adhesiveness and the formation of intractable “clumping” in muscle tissue. I am inclined to think that the mitochondria malfunctions are downstream from this, not upstream of it.
“If I have had these gene-related mitochondria malfunctions, I have successfully reversed them.”
-> Maybe the gene expressions found in the research are mostly a plain activation of healing mechanisms. When having very few food, starvation genes get expressed. I wouldn’t consider to just knock their expression down in order to reduce symptoms of being very hungry.
If you reversed your gene expression, you may have successfully reversed some of the root causes of your disease.
“but what I am most looking out for, is what causes fascia adhesiveness and the formation of intractable “clumping” in muscle tissue.”
-> For now, I’d put my money on “stuff that helps seal off, avoid further mechanical cell damage and leakage, disinfecting or healing the plethora of microscopical wounds to your muscle cells”.
The only time I have ever felt like a human being in my life is when I was consuming some sort of stimulant. Whether it was illegal, or diet medication given to me by my doctor. My entire family on my mother’s side, including my grandma, and uncle had chronic pain. I practiced psychiatric nursing for close to 25 years. I joke that I went into the family business. I didn’t feel that I could safely care for patients any longer. I can remember feeling depressed, and being in pain when I was 9 years old. Im 57 in November. I’m in so much pain,and have so much fatigue. Is there an end to this?
Setting imagination lose, I could envision following:
Take two thick but still young adjacent branches from a willow. Cut off part of both their side so that, when tied together, the flat wounds of both branches neatly attach to each other. Leave them tied together for sufficiently long time. They will have been grown together as if they were one branch at that spot.
Now take two small muscle fibers with adjacent muscle cells wounded. Let their be no tiny fascia or a thin damaged fascia with a hole at that spot be between them. Both damaged muscle cells and hole in the thin fascia could be created at the same spot by mechanical friction between them combined with earlier cell wall weakening by strong oxidative stress.
Now let them hold positions for only a short time, like half an hour after damaging physical exertion, enough for wounds to become sticky due to healing liquids trying to seal them. Now avoid movement for half a day due to high pain levels following exertion. That may be enough to form either a direct bond of these adjacent muscle cells or create a firm collagen bond between them.
Now these two muscle fibers have no motion between them at that spot. That will create a strong tension trying to tear them apart at, near and around the bond site when moving. It also will increase tension along stressed halves of the connected muscle fiber. Trying to move them will hurt a bit along most of the fibers and greatly at the welding site.
Each painful movement creates several chances:
* disconnection of the bond, creating new and bigger wounds at the bond sites of both fibers; can slowly heal over time but also re-bond or growing scabs and creating larger surface damage due to friction of the newly formed scabs
* rip bigger holes in the already damaged fascia by dragging the connected bond site up and down; creates additional chances for muscle cells to bond
* create tension further along one of the muscle fibers that is strong enough to create tears in already ROS weakened cells at new spots over the length of the muscle fiber; can grow new connections nearby to other adjacent wounded muscle fibers
If not self healing quick enough, amount of damage and connections increases fixing growing numbers of nearby muscle fibers together. That would be the type of damage that I imagine could grow in a matter of one to two weeks when power-training muscles (and ignoring pain?) like you did.
I would imagine such hypothetical mechanism would create semi-rigid “objects” with moderate to low deform-ability. I believe such damage would tend to pack closer together at the maximum diameter section in the middle of the muscles.
The massive micro damage plus the attempts of the immune system to trim undesired connections would keep the immune system busy.
That would not exclude “fat ball” type of deform-able lumps that can be squeezed like an elastic ball and return shape when releasing them. I believe those however to pack closer together halfway between the maximum cross section of the muscles and the point of tendon-muscle attachment.
That is the place where muscles tend to be “hollow shaped” in the sense that strongly pulling fibers shortening them would tend to detach them from the rest of the muscle. That would leave gaps ready to be filled with connective tissue/collagen.
It’s highly imaginative but please say if you recognize this well. Modelling is creating plenty off options and see which one fits the situation best.
Other possibilities in highly oxidative stress diseases are calcium deposits to be formed on/in tendons and muscles. I’d imagine them to feel like sand grains embedded in tendons and muscles creating painful movement. I envision them to pack more in tendons near the bone than near the max cross section of the muscle. I don’t recall you ever mentioning something like this.
dejurgen, I marked this particular article for review, and am only now reading it and the comments, so coming late to the party. I just have to say that even though I have had to take to skimming much of it, I find your comments so in tune with my own thinking. I can’t even take the time or energy to give one example, but had to just say that! You make very much sense, and your ‘intuiting’ is in line with my own. It got me revved. (hah)
THanks Cort for all you do on this!!
Philip Hayward – I’m glad you mentioned “the formation of intractable “clumping” in muscle tissue”. That is what causes most of my pain – my muscles seizing up and not releasing; muscles pulling my spine or ribs out of place.
If this alone could be resolved, I think I could deal with the fatigue and general “all over” pain.
I have written before about my family and this disease (FM/ME/MCS) I have primarily FM type. My daughter has primarily MCS and her son (14 yrs) has primarily ME. I have always thought this cluster is basically a mitochondrial disorder. (Just look at the range of symptoms). Some studies have also linked NE (noradrenaline) excess to the illness. Excessive NE causes significant mitochondrial dysfunction and down regulates NOS (nitric oxide synthase). In addition if you have a systemic mitochondrial dysfunction you will also get some loss of erythrocyte deformability because the protein synthesis involved in erythrocyte membrane assembly is affected. I think the oxidative stress is a consequence of the mitochondrial dysfunction – as you would expect. This compounds the cellular pathology. The erythrocyte deformability is not present in all cases, but where present makes the Fibromyalgia muscle function more severe due to considerable lactate and muscle stiffness – independent of the pain levels.
I would like to know more about what rimgs one.put of the state of hibernation. How does this occur in animald? Can we reactivate the implicated genes with environmental changes (light, heat, increases in oxygen, what else?) as occurs with animals – what “causes” them to wake up. Too much focus on mechanism of disease forget focus on mechanism of health/functionality.
Could bears hold the answer to me/cfs? Wouldn’t that be something!
Very interesting article! I find it particularly interesting because I’m a fibromyalgia patient and I lost two infants 30 and 25 years ago from a mitochondrial myopathy cytochrome oxidase deficiency complex IV so I’m pretty sure that I have mitochondrial dysfunction and oxidative stress. Thank you for all of your research keep up the good work!
Very interesting article!
I find it particularly interesting because I’m a fibromyalgia patient and I lost 2 infants many years ago from mitochondrial myopathy cytochrome oxidase deficiency complex IV
I think it would be safe to say that I have mitochondrial dysfunction and oxidative stress.
Thank you for you continued research!
” Just as an otherwise ordinary infection can have a debilitating effect on some people with ME/CFS, radiation has a similar, fatiguing effect on some cancer patients. ”
This article dovetails with the CFIDS Foundation theory that CFS is a reaction to low dose radiation in some people. My Dad got symptoms identical to severe CFS during radiotherapy for cancer. In his case the rdiotherapy didn’t work and he died from the cancer. Could it be possible that radiation can cause the body to go into “hibenation” state of metabolism and that is what we have?
If the CFIDS Foundation come up with any treatment, I would consider it, even if it sounds mad.
I have thought for years that fibro could actually be treated with a stem cell transplant from a healthy donor but of course it is unattainable financially for most people, generally 10,000$. These studies all support that but I doubt insurance will ever cover it. I have only found two places performing it, where it is accessible to the general public. One in the US and one in Thailand.
Really interesting article – thanks! Although I didn’t develop ME till my mid-teens, I’ve had the FM tender points since I was a small child. I called them my ‘see-through bruises’ (I meant invisible, but I was too young to know the right word).
I’ve often wondered if it really was FM, as I had low energy but not true fatigue until the ME arrived. I haven’t done a huge amount of reading about FM, but it rarely seems to be mentioned in connection with children.
Anyhow, I’m one of those who’s convinced there’s a syndrome consisting of ME, EDS, high-functioning autism, and MCAS – or at least some of these. I won the jackpot and have all of ’em! (I still have the tender points, so I might be able to add FM to the list too.) The good news, if I’m right, is that finding a good treatment for one of them may actually help them all. Ever the optimist…
I agree on the link betwee, ME/CFS/FM and Mast Cell Activation Disorder..I have them all (though the MCAD) tests at Brigham & Women’s fell 1 point short of WHO criteria so I am “officially” in the CFS group! I now can often manage it all quite well with strict diet and making myself move but there is always SOMETHING that comes along and screws it all up..lol
Interesting.. I see I’m not the only one allergic to radiation though I don’t have cancer. I had an MRI of my head last summer after the defective automatic tail gate of our SUV (BMW no less)came down on my head as I was helping my dog into the back causing a concussion. I got what I call “pre-anaphylaxis”, I took swigs of Benadryl before it became dangerous, which was then followed by a flare of CFS that lasted for weeks. When the chiropractor I went to wanted to do an x-ray I said no and explained why. He said my explanation was similar to the description of radiation poisoning described by one of his patients who was present at Chernobyl. The future certainly gets scary when most everything the medical world offers as a treatment is a trigger for a bad CFS/FM flare.
I have in the past been diagnosed with ME/CFS & Fibro, I am now told I have EDS 3 all along. I am now waiting to be tested by a Genetic Doctor
for multiple types of EDS which is common in many also waiting to be tested for (HATS) Hereditary Alpha Tryptasemia Syndrome & the Alpha-Gal
Meat Allergy (AG) as well…My last Doctor said she wants me tested also for VEDS 4 Vascular Ehlers Danlos Syndrome. I have seen EDS3 with
VEDS 4 combined. Dr. Rodney Grahame should be on the OMF board at Stanford
this is also written in response to the persons post above about the lignocaine…..
I always considered I was lucky after I was diagnosed with FMS following a neck whiplash injury in 1998. Within 8 weeks of the accident I started developing many symptoms. (as I was diagnosed very quickly within 3 months and was sent to a world expert on FMS so was under the care of someone that understood the condition enough to have me hospitalised and managed rather quickly compared to most)
I felt like I woke up to new symptoms every day. I had 24 symptoms in the end. Pain and fatigue went hand in hand and I had both at the severe end. I was bed-bound 90% and brain fog was terrible and IBS was so bad I lost half my body weight with in 3 months. I projectile vomited most of what I ate and the bowel issues did not help. Sweating and itchiness were unbearable. The dizziness was so bad I would have to crawl around on the floor to get around the house and to water the garden many times.
I felt I was lucky because once I was hospitalised for pain management the medication I ended up on (because I could not keep anything down) helped my pain and fatigue but also the 24 other symptoms became more tolerable… some even went totally except the restless legs & the IBS. The IBS took me nearly a year to manage via a naturopath who helped me control it so at least I could eat and stop losing weight. He developed a eating program for me.
I was commenced on 50mcg Durogesic (fentanyl) patches. Now I was still bed bound all those years ago and after 6 months of being on the patches I begged to come off… only because I felt that I was not really any better and I did not want to be on narcotics for the rest of my life…
So after 6 months my GP referred me to a addiction specialist to help me come off the Durogesic in 3 days in hospital. I had no problems coming off but the problem was that within 7 days I was in agony the original symptoms were back to their fullest and it was then I realised just how much the patches were managing my FMS on the 50mcg dose after all.
I rang the doctor that got me off the Durogesic and interestingly I have never forgotten his exact words…
“I didn’t say anything to you at the time because you wanted to come off the Durogesic but in my experience with FMS patients most of you are under dosed and if you are given higher doses of pain medication I can usually get my patients managed better and more functional..”
Remember this was back in 1999…. When they couldn’t give you enough pain medication…
So he doubled my dose and explained to me that because back then I was a smoker (apparently the durogesic was metabolised faster) he told me to change the patches every 2 days instead of every 3…
I did as he directed and I could not believe the difference in the quality of my life… I was still quite disabled with FMS I struggled to attend to my activities of daily living let alone anything else but I did get a much better quality of life. I could get my shopping done most times on a better day
For the first time since I was diagnosed I could get myself washed 3 to 4 times a week. The pain level was now down to a tolerable 3-4
So being on the higher dose the other symptoms either disappeared or they became less bothersome and I was again living with pain that was bearable … I was not rolling around the lounge or bed. My fatigue matched my pain. If I was having a reasonable pain day I was having a reasonable fatigue day and the brain fog matched the pain and fatigue
Once I got to the naturopath and had a high protein diet with much less carbohydrate and get rid of as much sugar as I could plus take stomach enzymes to help metabolise the food within 2 weeks the IBS was managed … and I only had break though times if I did not stick to the diet. I still had terrible bowel pain at times but it was much better than initially.. I still maintain that diet today…
I know what will work for me may not work for you but i have been trailed on every pain management system available… over the years and again recently once all the narcotic lunacy has started… I was made to experiment with other medications… the ones that never worked previously and was told to lower my durogesic dose with the goal of coming oFF (this after 16 years of being well managed) by having to come off the Durogesic I nearly died Christmas eve 2012! Because in someones wisdom I should not be on the only medication that is helping me… The result of this experimentation was a perforated bowel and they nearly lost me that night in surgery…
By all accounts I am a classical FMS client with all the symptoms and nothing out of the ordinary…
I still think I was lucky that I did get managed on a medication that helped me so much that I did get a quality of life much better than many of the clients I was talking to ( I was a FMS advisor 20 years ago… not anymore) I considered myself lucky that at least I felt managed even though I was still quite disabled and chair bound but I did over the years manage to be able to have a life with a partner until all this narcotic scare campaign has started… now I have no life as I am not allowed to be on the dose I am properly managed on so I now have less quality of life than i used to… I am back under dosed and have lost my partner as well due to the mess…
I often wonder whether its not so much that certain medications did not work for some maybe its that the doses were not right for the person…
And for those of you that are good with the information what could be the mechanism as to why this medication would work for my FMS or FMS in general????
I just want to die