

I never would have guessed this was the solution to my ME/CFS. Jeff, on Phoenix Rising
Jeff had a typical ME/CFS onset: he was a young, healthy and active individual before being felled by a viral infection and a high temperature. The infection left him with headaches, dizziness, muscle weakness and pain, sound and light sensitivity, and a general sense of being worn down that was exacerbated by exercise – which he soon had to stop altogether. Socializing was the next activity to go as he buckled down to focus on getting through graduate school.
The best doctors, endocrinologists and other specialists could do was point him to a diagnosis of anxiety or depression (which he rejected). He eventually became bedbound where his research led him to a diagnosis of myalgic encephalomyelitis (ME) (myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS).
Confronting the fact that he now had a possibly lifelong case of a chronic illness was not a happy experience, but it did enable him to find an ME/CFS expert, Dr. David Kaufman, in the San Francisco Bay area.
Besides ME/CFS, Kaufman diagnosed him with postural orthostatic intolerance syndrome (POTS), a disorder characterized by a rapid rise in heart rate upon standing and mast cell activation syndrome (MCAS) – an immune condition.

Jeff ended up with a very severe case of ME/CFS (or so he thought.) (Taken from Jeff’s Mechanicalbasis.org website.)
Next, Jeff joined the Phoenix Rising Forums where he found many people with a similar story. Jeff’s health, though, continued to spiral downwards. Bedridden, with severe PEM, his ability to tolerate exertion essentially disappeared. Combining a shower with a 15 minute talk on the phone could leave him crashed for days.
The crashes would propel him into a world the medical community has little awareness of. Lacking the energy to chew food at times he resorted to drinking protein shakes through a straw and lost weight, becoming emaciated. He had to be wheeled into the bathroom to take a shower. He turned to earplugs for noise sensitivity and low lights for light sensitivity. At his worst, speaking or writing were beyond him.
The only way out of a crash was to stop all inputs – lie perfectly still in the dark – and hope that his body would start to revive. When it did, he poured over medical journals.
Then a breakthrough occurred – in the form of neck pain, a headache that seemed centered at the base of his skull, and a heavy-feeling head that seemed to wobble like a bobble doll when he walked.
Turning his head to the right could cause him to nearly lose consciousness. Strange and alarming symptoms – all associated with autonomic nervous system dysfunction – popped up. His dsyautonomia, formerly moderate, now spun out of control, causing his heart rate to drop as low as 30 bpm at night, causing him to stop breathing and waking him up, disoriented, gasping for air.
Losing ground, fearful he would become too debilitated to research, he redoubled his efforts, scouring medical journals for clues until one day the light bulb went on.
The condition was called craniocervical instability / atlantoaxial instability (CCI/AAI) – and it fit. (It is also called cranial-cervical syndrome, hypermobility of the cranial-cervical junction, atlanto-axial instability, atlanto-occipital instability, craniocervical instability, craniocervical injury, upper cervical instability, others.)
The strange headaches, the heavy head, the problems turning his head in one direction, the autonomic nervous system issues – they could all be explained by loosened or lax ligaments at the junction between his skull and his vertebrae which kept his head properly situated atop his body. (The atlantoaxial junction (AAI) is the most mobile joint in the body.)
With his head destabilized, his spinal column was contacting and compressing his brainstem – throwing his autonomic nervous and sensory systems out of whack. His ANS had become so disturbed that even during sleep when it theoretically should have been mostly at rest – it was oscillating up and down causing bizarre heart rates.
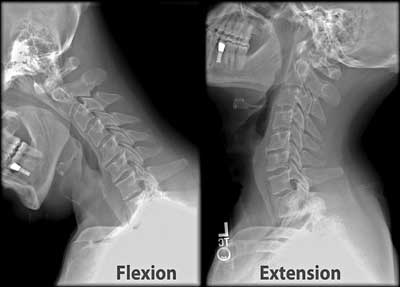
An X-ray of an neck being flexed back and forth to check for instability. (X-rays are not sufficient to test for this condition, however.)
There was no denying the validity of an CCI/AAI diagnosis – that diagnosis is well established in the medical literature. All Jeff – an immobolized patient with one suspect diagnosis (ME/CFS) and another unusual diagnosis (to most doctors – POTS) – had to do was to convince doctors that instead of a mood disorder – anxiety – he had a real (and admittedly rather unusual) neck issue.
That turned out not to be an easy task. Although CCI/AAI has been reported to occur with rheumatoid arthritis, Ehlers Danlos Syndrome (EDS), Downs Syndrome and other inflammatory conditions, unless it was the result of some trauma such as an auto accident, it is almost always dismissed as a possibility. Dr. Kaufman was a believe,r but his diagnosis wasn’t enough. A top doctor at a well-known medical clinic sneered at his self-made diagnosis – rejecting even POTS, let alone CCI/AAI as a possibility.
Jeff came to his own rescue again. After finding that pulling up his head relieved his symptoms he got a cervical collar which helped – giving him more time to, as he put it – to “find competent medical help”. Encouraged that a potential fix (fusing the top two vertebrae in his spinal column to his skull) was possible, he soldiered on.
Joining an online CCI/AAI group provided another realization: most CCI/AAI patients were in the same boat as ME/CFS patients – often waiting years for a diagnosis. Plus, there was another connection – most had been diagnosed with POTS, MCAS and Ehlers Danlos Syndrome (EDS) – three common comorbid diagnoses in ME/CFS. (About one in fifteen of people with EDS get CCI).
The EDS diagnosis was particularly intriguing. EDS occurs when the joints become hypermobile and is often diagnosed using the Beighton hypermobility self-assessment questionnaire. Like ME/CFS, MCAS and POTS, many people with EDS remain undiagnosed.
Jeff, like Jen Brea (see below), however, passed the Beighton hypermobility test . The only thing hypermobile about him, it seemed, was the junction between his head and neck plus mild hyperextensibility of his elbows and knees.
Noticing that when he pulled his head up his symptoms lessened, he bought a Philadelphia cervical collar which helped until he took it off one day, put a less rigid one on and collapsed, suffering from partial paralysis, racing heart, dizziness, etc. even after putting the stronger cervical collar on again.

A halo stabilized Jeff’s spine and improved his symptoms prior to his surgery. (Not all CCI/AAI patients require a halo) (Taken from Jeff’s Mechanicalbasis.org website.)
The ensuing ambulance ride to the hospital began a five-month hell-on-earth odyssey in the hospital that Jeff describes in riveting fashion in his blog. It ended when the Director of the Spine Center visited, ordered the correct imaging tests (dynamic CT scan w/ flexion and extension views), diagnosed him with CCI/AAI) and fitted him with a halo – a metal cage screwed into his skull to keep his head upright.
His dizziness, POTS and cognitive issues disappeared. He couldn’t believe how well he felt. He could talk fluently on the phone for hours without a relapse. He could read books again.
A spinal fusion by one of the world’s few CCI/AAI-literate neurosurgeons eliminated his symptoms, and they have remained gone. He’s now able to work out at the gym and is healthy. He also has good range of motion (after Dr. Bolognese used a new technique which maintains more range of motion.)
Despite the fact that Jeff didn’t have any overt neck symptoms until well into his illness, it appears that all the time he had craniocervical instability / atlantoaxial instability (CCI/AAI). He also had ME/CFS/MCAS/POTS, but all that was triggered by his CCI/AAI, and disappeared when his neck instability was fixed.
Another pathway to “ME/CFS” or rather ME/CFS-like symptoms has been identified.
Jen Brea’s CCI/ AAI Story
He’s not the only one. Some time last year, Jen Brea began experiencing similar symptoms. Her health had improved on Valcyte, fludrocortisone and pyridostigmine (Mestinon) but a surgery brought back symptoms she’d experienced before – at a new order of magnitude. First an airplane flight triggered a crash, flu-like symptoms and stabbing pains in her head, heart, and gut.
Next came flaccid limbs, numb, painful and weak legs, difficulty speaking and thinking. Then, one night, she stopped breathing – and couldn’t will herself to breathe again. Try as she might, she could not get herself to breathe: fifteen to 45 seconds later, though, her body’s automatic breathing response would kick in. Shifting to sleeping on her side helped.
When she realized that turning her head to her left triggered all these symptoms, something seems to have clicked. As with Jeff, a Philadelphia cervical collar which lifted her head to a better position, immediately ameliorated her symptoms.

Jen Brea and her collar (Taken from “A new diagnosis to add to the list”, https://medium.com/@jenbrea/a-new-diagnosis-to-add-to-the-list-c966145b8f0c?fbclid=IwAR1DHtlLfcnON8tDEyi9zycSUVU18yiqICw6TbCfkhwsdRKan8YIlXyun7M)
After testing demonstrated that her head/neck junction was extraordinarily lax, she was diagnosed with CCI/AAI. The diagnosis made sense of some symptoms she’d never been able to fit into ME/CFS before – why turning her head sometimes left her disoriented and why sudden jolts sometimes hurt so much.
She noticed she was unconsciously hunching her upper back and shoulders in an attempt to balance her head properly on her body. Trying to defeat that by trying to throw her shoulders back and straightening her spine resulted in crippling neurological symptoms. For the first time in her ME/CFS journey, interestingly, she’s in lot of pain. Pain, she reported, “was never really a part” of her illness, before
Jen reported that in December/January she’d three surgeries: a craniocervical fusion and two surgeries in her lumbar spine to remove a hematoma that was compressing her spinal cord (caused by a blood patch) and a tethered cord release, a condition she was probably born with.
The surgeries corrected her breathing problems, the numbness, weakness and pain in her legs. A couple of months later she’s still largely bedridden but is improving.
Because these surgeries can take from 3-12 months to take full effect even in a healthy person, there’s no way to tell yet how much impact they will have on her ME/CFS, POTS, MCAS, etc. Her surgeon warned her, however, that while the surgery could help those conditions, to not expect a resolution of them. Surgery, he emphasized, is a last resort.
- Read Jen Brea’s A New Diagnosis to Add to the List
- Update: Jen Brea’s POTS is gone!
Diagnosing CCI/AII
Symptoms
The Zebra Network and other websites report three central symptoms of craniocervical Instability (CCI):
- “Heavy” headaches (feeling like the head is too heavy for the neck) and a bobble-head feeling.
- Pressure headaches generated by things like yawning, laughing, crying, coughing, sneezing or straining.
- Symptoms of autonomic nervous system functioning problems such as tachycardia (rapid heartbeat, heat intolerance, problems standing (orthostatic intolerance), gut motility problems, thirst and chronic fatigue.
Other symptoms can include neck pain, central or mixed sleep apnea, facial pain or numbness, balance and coordination problems and vertigo, dizziness, fainting, vision issues, difficulty swallowing, choking, tinnitus, nausea, vomiting, paralysis, downward nystagmus (irregular eye movements).
Note that neck pain and neck issues are not mentioned. Jeff reported that, for most of his ME/CFS, his vague headaches and neck symptoms provided no clues that his head and neck were the cause of his ME/CFS.
Diagnosis
The results on the Phoenix Rising Forums (13 people on the Forums diagnosed with CCI/AAI thus far), while anecdotal, suggest that this condition may not be as uncommon as one might think in ME/CFS.
- Check out the Tracking CCI/AAI thread on Phoenix RIsing.
On his Mechanicalbasis website, Jeff provides advice for getting tested and a diagnosis that no-one who potentially has this condition should be without including the specific imaging needed. and how to get your scans into the right hands. Most neurosurgeons aren’t trained to recognize craniocervical instability and finding an imaging facility that does these kind of upright scans can take time.
Upright MRIs with flexion, extension, and rotational views, or supine CT scans with flexion, extension, and rotational views or 3Tesla supine MRI’s. (A patient of Dr. Kaufman’s reports that the extremely strong 3Tesla MRI’s may be the best and are more readily available. Check out the difference between the 3T and 1.5T machines).
Chiaribridges reported that “the ideal tests to diagnose CCI and AAI are an upright MRI with flexion and extension (bending one’s head forward and backward as far as one can) and a 3D CT with rotational views, respectively. Ventral brainstem compression is not always seen in traditional supine MR imaging but it usually very evident on dynamic upright imaging which has the patient flex and extend their neck.
On Phoenix Rising, Jeff reported that the dynamic imaging should also check for Chiari Malformation (which can cause similar issues), Craniocervical Instability, and tethered cord syndrome (which Health Rising will cover later).
He reported that only 3 neurosurgeons in the world can help: Dr. Henderson at the Metropolitan Neurosurgery Group in Maryland; Dr. Bolognese in at the Chiari Neurosurgical Center, New York; and Dr. Gilete in Barcelona, Spain. Dr. Faheem Sandhu in Georgetown, Washington D.C. is quickly developing competence in it. Dr. Patrick Johnson, Director of the Cedars-Sinai Institute for Spinal Disorders in Los Angeles CA, diagnosed his CCI, and knew how to fix it but is not a specialist.
Merck reported that symptom improvement during a procedure called Invasive Cervical Traction (ICT) where one’s head is pulled upward by a pulley system can help diagnose CCI/AAI. Lacking that, a doctor can simply pull the patient’s head up off the spine in the doctor’s office, and see if that helps!
Wearing a Philadelphia Cervical brace helped Jen and Jeff self-diagnose themselves. (As Jeff’s condition worsened, though, the collar didn’t help at all; i.e. it may not help everyone).
- Comorbid Diseases and ME/CFS/FM Mimics – check out the growing list here.
Treatment
Nonsurgical Procedures
Surgery was the only option for Jeff and Jen but that’s not so for others with this condition. Dr. Bolognese reports that treatment of craniocervical instability typically begins with more conservative medical management, such as neck bracing, activity limitation, physical therapy (including isometrics, sagittal balance, core strengthening and cardio), and pain management.
One of his patients diagnosed with CCI reported on the Phoenix Rising forums that manual traction (having someone pull on one’s head while lying down can help) and prescription interventions have helped quite a bit. She said it’s hard to tell what has made the ultimate difference but has had major improvements. A physical therapist showed Jeff’s family how to do manual traction properly. Some people with CCI also benefit from home neck traction devices.
Sleeping in a bed with the feet elevated and the head down in the Trendelenburg position helped Jeff.
Wayne whose believes the health issues that led to his ME/CFS started with a serious head injury/whiplash as a teenager, and who believes he probably has CCI/AAI and/or cervical stenosis, has found substantial relief from a procedure called AltasPROfilax and specialized chiropractic care. The Perrin technique is another possibility for those with neck/head issues. Find out more about Wayne’s and other’s approaches to possible CCI/AAI and other neck issues here.
Some people with ligament laxity have improved using the Cusack Protocol. Regenex is another procedure mentioned. In it, bone marrow concentrate (BMC) that contains a stem cell fraction (same-day stem cell procedure) is injected directly into the lax ligaments.
If you have EDS check out how to find the right physical therapist to help with ligament laxity.
Surgery
Surgery is considered the last option. Few neurosurgeons are competent in this surgery, travel will likely be required, and wait times to get the surgery done can be long. During craniocervical fusion the skull is pulled upward and placed into the correct position, and then the occipital bone of the skull is fused to the upper cervical vertebrae to hold the corrected position. A halo or cervical brace is worn while the bones completely fuse together.
“If you are a surgical candidate, I highly encourage you to go slow, research all the options, seek second opinions, talk to other patients, understand the risks, and to think not just about the surgery but about pain management, your personal reaction to anesthesia and medications, and your post-surgical care plan, which may require additional care-taking at home as well as a plan for physical therapy.”
Other Brainstem or Spine Compressing Conditions
Doctors regularly rule out thyroid issues, sleep apnea, etc. before diagnosing ME/CFS/SEID. They need to start ruling out these neurosurgical issues as part of their first line of investigation. Jeff
Hip, on the Phoenix Rising Forums, pointed to a number of conditions which can cause brain stem or spinal cord compression and cause symptoms similar to those found in ME/CFS/FM:
- cervical spinal stenosis — spinal canal becomes too narrow, which can put pressure on the nerves
- syringomyelia — fluid-filled cyst in the spinal cord which compresses the spinal nerves
- Chiari malformation — where brain tissue is pushed into the spinal canal due to a skull which is too small
- tethered cord — where spinal cord is “stuck” to a structure within the spine such as scar tissue
- craniocervical instability — instability of head & neck bones compressing the brain stem or upper spinal cord.
Other spinal conditions that may cause or contribute to ME/CFS/FM/POTS include cerebral spinal fluid leak and intracranial hypertension.
The growing list of potential ME/CFS/FM mimics provides more clarity but also adds complexity to an already complicated disease. Future blogs will attempt to bring some more diagnostic clarity to the structural issues that may be occurring.
Resources
Health Rising’s ME/CFS/FM Spinal Series
- Could Craniocervical Instability Be Causing ME/CFS, Fibromyalgia & POTS? The Spinal Series – Pt. I
- Jennifer Brea’s Amazing ME/CFS Recovering Story: the Spinal Series – Pt. II
- Spinal Stenosis, Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia: The Spinal Series Pt. III
Jeff’s Story and Website
- The MEchanical Basis of ME/CFS. – includes his story and resources on diagnosis and neurosurgeons
- An interview with Mattie – three months post CCI/AAI surgery
Jen Brea’s Story (Most recent to oldest)
- Health update #3: My ME is in remission
- Health update #2: My POTS is in remission (My POTS has been in remission for 21 consecutive days! — an outcome of my craniocervical fusion surgery. More on this and why I think we need to be looking at the brainstem.
- Do you have ICC-ME and other FAQs (The previous post somehow had some folks thinking I have hEDS and that I don’t have ME, even though all the previous posts have conveyed the opposite. I wrote this for all avoidance of doubt!)
- Are a subset of us members of a lost tribe? (On the possible connections between EDS and ME and the questions I wish researchers were asking.)
- Health update #1 (Feb 21) (Healing takes time)
- A new diagnosis to add to the list (I stopped breathing and was diagnosed with craniocervical instability)
CCI/ AAI Threads on the Phoenix Rising Forums
- Have you ruled out Chiari or Craniocervical Instability (CCI) as a cause of your CFS
- 20 patients now found positive for CCI / AAI, there must be many more…
- Tracking CCI / AAI MRI & Treatment outcomes
- Regenexx for craniocervical instability: my experience
- Update: CCI Surgery
- Pursuing CCI/AAI, have questions, former high jumper & figure skater
- Jeff anyone who have consulted with Dr Bolonesse … help confused!






We need to find ways to fully corroborate the efficacy and reliability of solutions which are non-surgical. I was one of the patients who was diagnosed CCI positive after suspecting ME/CFS like symptoms for a decade (via Dr Gilete + an expert radiology review by an MRI inventor / pioneer at Medserena Clinic in London).
This gave my health issues a lot of legitimacy in the eyes of my family and friends and has somewhat helped me gain a better sense of fatigue, cognition, neuro symptoms. However, a lot more needs to be done. The medical community needs to keep finding ways to support healing in a non-invasive way and, especially, we need to find ways to identify patterns and connections in a more open-minded way.
After some of the articles on Health Rising and a lot of research, I have started looking into ways to limit my exposure to radiation / electromagnetic frequencies, which most *definitely* has an influence on my fatigue and my CCI. I wake up far better in the morning (and sleep better) with my cell phone turned completely off by my bedside table. Television and laptop screens suit me poorly over short or long durations, and often to work on them for extend periods requires that I avoid them for equally extended periods.
We need to tackle our issues in a multi-faceted way, and ME/CFS et al. will remain a multi-faceted health issue until we truly understand how everything ties back together. That may not be before a good while. Detoxification + environmentally-conscious living + immunology all play a role here.
This is interesting. I have been going for NCRT for a year… neurologic centers relief technique and it decompresses the meninges. My heachaches go away with it but return when I stop therapy. I wonder, based on this article, if there is something more going on for me?
I read all I can on all associated with me/CFS. I have observed that nothing surprises me. I have had and still suffer from, every symptom others express. Including this one. Dating back to my 30’s, possibly sooner. I am now 71. One private rheumatologist dx in 2007. All others have denied it’s existence. Evidently I am psychotic in their eyes.
The news about Jen Brea is so very heartrending. There is nothing to say except to send deep respect.
I have experienced nothing comparable, but I do wonder if there could be degrees of this condition. I experience what could possibly be considered a mild, very mild version of it and I write in case my experience helps anyone else with similar mild neck issues.
A rheumatologist I consulted in the 1980s about persistent one sided neck pain pointed out to me that my joints were somewhat hyperextensive. Holding my palm vertical I can flex my figures back to 2 o’clock. Y thumbs are sufficiently floppy that I frequently drop things. And I avoid standing close to the sidewalk or platform in case I pitch forward as my ankle gives way.
I had suffiently obvious MACAs that hives would follow a finger lightly laid on my skin.. once passing through San Francisco I had three infusions of IV anti-histamines before the ‘allergy ‘ subsided, and of course fatigue etc. etc. but nothing like our brave warriors Jan.
The first suggestion this was ME came when one of my friends who didn’t think I was mad/malingering etc gave me a book published I’m 1986 by the Uk publisher Virago with an introduction by the patron, Claire Francis the first solo round the world yachtsman. Hardly malingering,
The pain she described is in exactly the same place as in this description. Claire was bedbound – but I was not.
The pain and symptoms disappeared and did not come back.i totally agree about not having chiropractic but Here’s what helped me
1 the Alexander technique- it’s a long individual therapy used by musicians and other who put great tension on their joints. It is VERY gentle- it will not jerk or jac you. It WILL NOT HARM YOU EXCEPT IN THE POCKET..
The therapist places the body joints in a position of perfect
balance; idea is that the body retains this experience. The idea is to ‘lengthen’ the spine and to lift the head as if being drawn up wards on s string while the shoulders do not hunch up. I found I did gain a sense of lengthening neck and adjusting its position relative to the spine..
2. I adopted a wierd sleeping possition which took the strain off the back. I trained myself to sleep on my back with two pillows either side of my head and a low one between the in an H pattern. The two on the sides stopped me turning or twisting my head at night. And I place pillows under each elbow to relieve putting a dragging weight on my neck. – rather anti social but what the hack.
3 I adopted a management orientation of NO lifting and a willingness to ask others to lift bags or pull doors open for me. I found most strangers on subway airport or bus very helpful.i had a wide belt and hung my groceries and so forth on it because I found that if l lifted a grocer bag for example I would throw my head back and bingo the wierd pain would zap me. Slowly slowly the pain receded
also, by the way, I stopped doing house work because you can’t when have ME – it’s a habit I have continued now i am ok.
Hello George
I am also looking into this issue and would like to get MRI at Medserena Clinic London. Have you been diagnosed by both Dr Gillete and an independent radiologist at Medserena. I would really appreciate your input. Thanks
I’ve spoken to those who found they had hidden mold exposure – and developed increased joint laxity while exposed. This laxity often got better when the person was moved from that environment.
Has there been any correlation to mold exposure and CCI?
It would make sense that if the toxins produced by mold can destroy collagen, perhaps it can repair when the triggering substance is gone. This is all theoretical and only relating to situations where the cause of excess laxity is mold.
Thanks for the outstanding blog Cort! It gives a very clear overview of the process Jeff and Jen went through.
As to Jeff and Jen: what a monumental ME/CFS/FM/POTS/CCI/AAI/… warriors they are! When knocked down to hell they fought back with barely any life left in them. And they dug deeper than what most of the medical community combined had been able to do so for them. Those are epic tales of heroic people!
On topic: Hip mentioned Jeff’s remarkable story on https://www.healthrising.org/forums/threads/is-it-a-common-symptom-to-stop-breathing.6110/#post-34716.
That’s where I saw a connection with ME: increased Cerebral Fluid Pressure. Recent research shows remarkably increased brain fluid pressure in both ME and FM patients. Until Hip’s comment, I saw it as “just” and increase by some percentage. But then I recalled a documentary on the first bunker buster bombs the Nazi’s developed and used to destroy armored bunkers that were thought to be indestructible.
Now this bunker buster bombs were “charged shapes”. Basically they were half spheres that strongly concentrated the explosive power of the charge towards one single point (near the center of what would be the full sphere). And that shows quite a bit resemblance with how the skull plus increased CBF pressure looks. If any of my physics gut feeling is wright, it should create roughly 2 main pressure hot-spots:
* The strongest one very close above the brain stem.
* Another relatively strong one close to the middle of the frontal lobe, but a bit out of the middle towards the front.
Now the brain stem and the front lobe have seen more then a bit interest in ME/CBF as particularly hard hit if I recall well. And both are 2 out of 4 brain pain hot-spots I have.
Both increased CBF pressure on top of the brain-stem or cranial deformation at the bottom of it would do to compress the brain-stem badly. They’ll probably roughly add up.
*IF* my physical intuition is close enough, an increase by “only” x% in CBF pressure could equal to a multiple of this x% increase in pressure at these hot-spots. This would “promote” this increased brain pressure seen in recent ME/FM research from a potential problem to a massive challenge to the brain. It would not only put plenty of pressure on these hot-spots, but also cause shear tension in many areas of the brain and immensely disrupt local blood flow in the brain.
Blood flow towards a particular point in the brain is for a big part determined by both blood pressure AND pressure of the brain tissue on the local capillaries. Now if that has very strong to massive local increases…
The good news: with a team of a few brain specialists and an engineer in material properties, mechanics and modeling one could build a detailed computer model to verify this hypothesis. A perfect NIH sponsored project :-).
For a more elaborated discussion, see my response to Hip on the above forum link.
Kathy Bungard also posted a very interesting link https://www.healthrising.org/forums/threads/the-link-between-idiopathic-intracranial-hypertension-fibromyalgia-and-chronic-fatigue-syndrome.6101/#post-34642
There it appears that malformation of the sines can increase brain pressure. I can see brain inflammation and swelling could increase CBF pressure too. There I also wrote about another potential cause of increased CBF pressure: poor return of blood from the brain to the hart. That should increase CBF pressure too. Potential causes of poor return of blood from the brain to the hart can be:
A) Various vascular problems like having an auto-immune reaction to blood vessel wall cells as seen in many patients according to recent research.
B) Vassoconstriction by having low NO like reported over and over in ME.
C) Tight chest shoulder and neck muscles “strangling” the major blood vessels between brain and neck.
D) The opposite of EDS/hypermobility: short muscles and hypomobility. If all muscles are too short then they will pull in different directions and the “balance of this fight” will determine the main position the head and neck is in. Likely this position will be sub-optimal and will cause both decreased blood flow and brain stem compression.
E) Personal to me: I can’t keep my eyelids sufficiently open for a long time. It’s costing me too much energy since I’ve got ME. That gave me a natural habit to put my nose and chin up when looking in front of me, giving me a very poor positioning of the head towards the neck.
=> Points C and D may be why doing neck circulation exercises !under guidance of a good Physical Therapist to decrease the risks going with it! are at the base of my first wave of improvement in plenty of symptoms.
After trying to check this idea I believe my physics intuition failed me. So near all of this post is rambling, except for Jeff and Jen being heroes.
@Cort: if you want to avoid people with ME reading this lengthy post and only then reading all of it is wrong, feel free to delete it. Dejurgen.
I thought it was, as always, very interesting!
If the spinal support structure putting pressure on the spinal cord can induce ME/CFS symptoms, then can one guess the opposite is also true? I.E. if an infection or such inflames the spinal cord and causes it to expand beyond it’s normal area, thereby also causing the same symptoms. Maybe some suffer from both.
Just an open question for those with a better understanding of human physiology than me.
Thanks to all for your efforts to share insights.
I would think so. I imagine that would show up on the right kind of imaging. It brings to mind Corinne’s problems with a spinal lesion – albeit in a different part of the spine.
I would think if the CII surgery after a time of healing fully resolved all symptoms this wasn’t a pathway into ME but a misdiagnosis of ME.
A interesting issue – which Jen devotes quite a bit of time to in her first blog. Caroline Christian struggled with this in cerebral spinal leak / EDS / ME/CFS blog. M.E. is getting more complicated all the time. I think that is going to continue!
Here’s how I see this: Jeff had ME – he met the criteria, he had the flu-like onset – he had everything a severe ME patient has – the difficulty standing, the hypersensitivity issues but he really had CCI/AAI.
That brings up a couple of questions – if Jeff so clearly met the ME criteria – M.E. can clearly be produced in several ways. That brings up the question what exactly is M.E.? Right now ME is a good descriptor for ME/CFS but my guess is that as we discover the different ways it is produced that term will decline in value.
There will be autoimmune M.E., viral ME, structural ME, etc. After Dr. Klimas found that GWI and ME/CFS look exactly the same but are vastly different physiologically I think we should prepare ourselves for a variety of “M.E.’s” including the classic – an enteroviral caused disease.
That all feels right to me too, Cort. We’ve gotten pretty good at describing a common state of being. I wonder if we’ll discover a few common ways to treat/mitigate the condition, or if every variety of etiology will require its own cure.
BTW, is it agreed that “a flu-like onset” is a requirement for an ME diagnosis? Those of us without such an onset are deemed to have “CFS” rather than “ME/CFS”? (I believe my charts just say FM/CFS, along with some neurological stuff, but I’ve been mentioning ME to my doctor lately.)
Wrong, 95% of CFS/ME patients have undiagnosed EDS types the other 5% have other connective tissue disorders this is a Quote by Dr Rodney
Grahame so do not think because a Doctor says you have ME/CFS IT IS RIGHT, IT IS NOT. I have been told I have all of them from ME/CFS to
Fibro to EDS & we are Born with EDS, then come on the complications of EDS. I even had all my bay teeth Surgically remove I even underwent an
Emergency Surgery for Appendicitis but all Pathology reports came back Negative it was not my Appendix at all the Surgeon told my Mother he
was baffled. EDS has now also been linked to (HATS) Hereditary Alpha Tryptasemia Syndrome & I also have seen Alpha Gal Meat Allergy Syndrome
(AG) positives in EDS…(AG) can cause severe drops in blood pressure & low blood pressure can also cause structural issues…Hereditary
Fructose Intolerance can also be involved in EDS as well (HFI) is a Genetic mutation one is Born with…ME/CFS is EDS
Baby teeth ‘typo’
Hi, Cort, It is great and welcome news for both Jennifer and Jeff that surgery has relieved some/ all of their symptoms, I know Jeff in particular has had a wonderful turn-around in his own dreadful illness.
I see Chiairi is mentioned in your article under the heading of other brainstem and spinal compression conditions that can cause ME-like symptoms. It is worthwhile noting I think that that in the UK ME Association’s clinical guideline (written by medical advisor Dr Charles Shepherd and consultant neurologist Dr Abijit Chaudhuri) that Chiari is a differential diagnosis, ie one of the conditions that should be ruled out before a diagnosis of ME is made. This leads me to wonder if all of these structural abnormalities/brainstem compression issues are indeed *mimicking* ME rather than actual causing ME. If one is cured after surgical intervention, is it worth considering at all that one may have been misdiagnosed?
As someone with classic enteroviral onset in 1980s, I do understand that there are subsets of ME emerging all the time, but I also think we need to be very cautious labelling Chiari, CCI etc as ME.
I would like to agree with Nasim. This means that a diagnostic test for ME is urgent.
Thank you for outlining all this Cort; I am delighted for Jeff, however, I would like to hear about Jen and how she is doing.
“This leads me to wonder if all of these structural abnormalities/brainstem compression issues are indeed *mimicking* ME rather than actual causing ME.”
Another question could be: is ME a well defined disease or more a set of disease mechanisms that are triggered by different onsets and lead to a very serious set of ME symptoms?
Could ME be both the devastating disease and a set of mechanisms transforming some challenges the body can’t cope with to a sort of common serious and hibernative ME state as a sort of last line of defense hoping to sit out the problem?
The classic postviral illness ME that I have is already well described by Melvin Ramsay. But let’s say a similar ME ‘state’, usually triggered by a viral infection, can also occasionally be triggered by other factors such as vaccinations, toxins or physical trauma. Once the abnormal neuroimmune ‘cascade’ has happened, there is still no cure, because we simply don’t know the mechanism. So we live with ME as best we can for decades, regardless of trigger.
On the other hand, if your symptoms are v similar to ME but cured by surgery, that, to my mind, means you have had a structural abnormality successfully treated, it does not mean you have been cured of ME. And why on earth would you then call CCI or Chiari ‘structural’ ME, rather than consider a misdiagnosis of ME?
The same, for example, can be said for extreme mould avoidance ‘curing’ ME. I don’t understand why neurotoxicity caused by mould (which, though, medically controversial, I fully accept as a serious illness) is called ME. Why is it not called neurotoxicity caused by mould? And also treatable/curable by extreme mould avoidance, as seems to be the case, anecdotally, at least.
But a true *ME* state caused by infections (or toxins or physical trauma) does not disappear once the trigger has gone. The abnormal state is still there. And we can’t treat or cure, because we don’t know the mechanism.
So, yes, while I can see that there could be ME different triggers, I don’t see why we are calling everything ME, I mean where do we stop?
Hope this makes sense.
I guess the real question with CCI/AAI is, if it’s not caused by a trauma, what the heck is causing it? If it is an enteroviral infection then perhaps it might fit into an ME diagnosis – if M.E. ends up being defined as a post enteroviral illness.
I think of M.E. as a kind of a broad holding term pertinent to this community. In the end CCI/AAI is the right term for what Jeff has. When the autoimmune subset in ME is identified – as everyone thinks it probably will be – a different autoimmune disease (not M.E.) will be borne and so on.
Nasim Marie Jafry – re. “But a true *ME* state caused by infections (or toxins or physical trauma) does not disappear once the trigger has gone. The abnormal state is still there.”
You raised some interesting issues. My feeling is that in these cases there is a possibility of either ME-mimicking, or ‘true’ (‘neuroimmune cascade’) ME having been at play. Maybe the parameters between these aren’t always ‘absolute’ ones, such as in instances where the latter ‘true’ ME is near recovery.
In these latter cases I think there are times when the disease process is in a less developed/entrenched state, or has reached a more responsive-potential level whereby it can be nudged into a good improvement/symptom resolution with whatever help is most relevant towards this being achieved in individual sufferers.
I’m not convinced by the appropriateness of the MEA’s (purple booklet) guide for clinician’s apparent categorisation of Chiari as a ‘differential diagnosis’ – although I’m not actually clear what this means exactly. I can appreciate the usefulness of considering this as a possible ME-mimicking condition, but not of defining it as an ME-precluding alternative if that’s what is meant, as I see no reason for it not occurring co-morbidly (perhaps significantly influencing ME symptoms) in at least a proportion of ME sufferers (and I think anecdotal reports do seem to point to this as being a particular ‘known type’ of ME comorbidity along with EDS and the other structural issues referred to in this blog).
A ‘structural ME’ label wouldn’t be something that ‘works’ for me – though I guess for differing reasons (ie, I believe the ME occurring in sufferers with multiple different triggers consists of a fundamentally like pathology, albeit in almost infinite variations within this).
dejurgen’s theorising on this chimes well with some of my formed impressions: “Could ME be both the devastating disease and a set of mechanisms transforming some challenges the body can’t cope with to a sort of common serious and hibernative ME state as a sort of last line of defense hoping to sit out the problem?”
I’m a bit confused by your question Cort, on what is causing CCI/AAI if not a trauma – as your (excellent) blog explained this didn’t it?* Or were you meaning how could this cause ME? – my brain’s interpretive functioning may have conked out too much…
(* a complication of EDS (of which there’s 13 different types) – itself a genetically inherited condition affecting the body’s connective tissues due to faulty (too soft type) collagen production. If the ligaments in the neck become too weakened by this then the cervical spine can’t support the weight of the head sufficiently, and these vertebrae can start pushing into the brain stem.)
Hi Nasim,
You certainly have a valid point.
What I meant to say is: maybe there is more then “either ME” or “mimicking ME”.
It could be that not only the symptoms are very much the same but also that many to most of the pathways in developing these symptoms are identical.
I’m not talking brain stem compression leads to these symptoms or post viral issues lead to these symptoms, but more compression of part of the brain due to either neck problems or increased CBF cause a very similar cascade of processes leading to ME symptoms or increased inflammation due to mechanical stress near the brain stem or due to an immune response in the brain cause a very similar cascade of processes leading to ME symptoms.
To me, that’s beyond mimicking. True, these are different specific diseases but they may be very close siblings both in severity, symptoms and specific pathways involved.
Keep in mind that Jeff’s case reads as a serious case of ME symptoms before this differential diagnosis. And *very* few diseases get as severe as ME. That may point to more then coincidence.
Looking at it this way, I see options beyond a differential diagnosis that can help part of the poorly diagnosed patients. It may be a window to better understanding and treating both “real” ME and mimicking ME IMO.
Hi Kate,
Thanks for mentioning the genetic factors behind EDS – I had forgotten those. So we have those. I was thinking about rheumatoid arthritis – is it the same autoimmune process found in RA that is weakening the craniocervical ligaments there? In people with ME/CFS without EDS or its genetic underpinnings, did the infection kick off an autoimmune process similar to RA, and if it does, does that mean that autoimmune drugs that help RA could help with them?
If an autoimmune process is involved is it possible that if that is stopped or reduced the ligaments could get at least partially restored?
Finally, so much CCI/AAI seems to be cropping up – 13 people diagnosed so far just on the Phoenix Rising forums -I had never suspected so many – it would be great to break down that group – how many have evidence of EDS, how many had their ME/CFS triggered by an infection, how many had head injuries, etc. It makes me wonder, too, if being bedridden increases the risk of joint laxity in that area.
“It makes me wonder, too, if being bedridden increases the risk of joint laxity in that area.”
For me, that points back to the question: how important is it to have healthy and well performing muscles to keep those more lax joints well into place?
I can’t judge this one as I do not have hyper-mobility. But having ME and being bedridden very likely will not improve control of the muscles to compensate posture for joint laxity.
I had plenty of common colds, with above average severity. The first signs of catching a new one are one of following: painful teeth (sines swelling up), headache, “raw” throat or painful/stiff cheek muscles.
If a common cold can cause muscles to stiffen up, a strong infection sure can. I forgot how that was when I got the flu.
My mono infection had the opposite effect on my muscles: no stiffness (contraction) but severe muscle weakness.
Both are probably pretty poor at supporting a “lax joint” neck skeleton if you have that. Maybe a (viral or other) infection can push somebody with pre-existing lax joints into one or two weeks of problematic neck position causing all sorts of trouble like a compressed brain-stem, poor blood flow to the brain, inflammation of parts of the neck…
I doubt those alone would get someone into a ME vicious circle, not because their impact is too small but because I feel such temporary problem should resolve itself. But that same temporary neck problem would coincide with other things like:
* a strong immune reaction to the infection
* diverting of resources away from the digestive tract to the immune system potentially giving borderline digestive tract trouble (like a starting gut overgrowth) a chance to derail
* poor back/spine and sacrum position as those joints may be lax as well and the nearby muscles will also be affected by either stiffness of weakness, leading to muscles damage and inflammation…
* thick blood due to cytokines reducing blood flow
* …
So IF lax joints require fit muscles in order to not get into trouble then lax joints may be only one of the many things being affected when a sudden strong infection pops up.
In above hypothesis we would be looking at multiple weaknesses like an over active immune system, genetic weakness to certain pathogens, faulty RBC, “defective” metabolic pathways… that all are “pushed head under water” at the same time by the “correct” pathogen trigger. Two weeks of that may be more then enough to get someone in a nasty vicious circle leading to ME.
I agree…..it is bewildering to see the lack of comment on this.
Interesting…I was recently dx with 2 herniated discs in my neck. Although that may not be the same as craniocervical instability (I’m still not certain what exactly this dx entails,) I’ve also had the bobblehead at times, and my neck discomfort does come and go. I’ve also been dx with hyper-POTS and mast cell activation syndrome.
For me, I’ve had upper body/neck/head issues since ME/CFS. It’s where most of my day to day pain is located. I don’t believe I have CCI/AAI but stretching my neck too far causes nausea and flu-like symptoms and night sweats
– something strange is going on.
It could be that (entero)viral infection –> causes typical ME symptoms + laxity –> laxity leads to CCI, causing new, more, worse ME symptoms.
Does surgery lead to complete recovery (fingers tightly crossed)? Will Jeff and/or Jen be able to go for a run and not get PEM? Or does it return them to milder ME, but without the CCI induced symptom severity?
So maybe CCI is not different from ME, but a consequence of ME?
Jeff has completely recovered. Jen’s surgeon warned her not to expect complete recovery and thus far she still has full blown ME but it will take quite some time for her to know how effective the surgery (surgeries in her case) are. So far we just have an N of 1 I’m afraid.
Since Jeff’s illness was triggered by an infection I would think your scenario would make sense. CCI is possibly just another potential outcome of an enteroviral infection which effects the ligaments which then causes brainstem compression, autonomic nervous system issues and more immune problems.
Hey Cort, one thing I can certainly say (over a ten year timeline with these illnesses) is that my CCI symptoms (ligament laxity, tendency to nausea, fatigue, post exertion malaise, anxiety, brain fog and visual issues) *did in fact* get worse after a depressive episode which I passed through towards Fall 2016.
Without overstating anything, it would seem that something about the brain chemistry or hypersensitivity, for me, did trigger a worsening of my cervical ligaments. I am convinced that there is something about brain metabolism in ME/CFS, or something about my hypersensitivity, or something else pertaining to metabolism in general, which worsens CCI and/or ME/CFS.
Or stated otherwise, brain metabolism induces, worsens, CCI (without invoking ME/CFS at all).
However, my ME/CFS began a very long time ago (a decade ago) and there were many episodes which I had to deal with which did not include any suspected neck pains, or migraines, or nausea and these are classic CCI symptoms to begin with.
I have had neck issues for a very long time, but I *still* don’t think they were at the very outset of my ME/CFS (something Jeff has dispelled or at least suggested otherwise: he would say that CCI surgery has effectively remedied or effectively abated his ME/CFS).
For me, after a sudden and strong viral onset in my first week of college (sudden-onset pneumonia), I developed what is considered now to be a very familiar ME/CFS problem (I would have maybe known this at the time except I had no concept of ME/CFS in 2007).
The symptoms were textbook ME/CFS: horrendous issues with sleep and circadian rhythm, full blown post-exertional malaise, and others I am realizing now in retrospect with the studies being published recently: issues in low-oxygen environments, issues with photosensitivity such as laptop and TV screens and issues with electromagnetic fields.
This is why I don’t think CCI is at the origin of my ME/CFS but an entirely co-morbid thing which as you mentioned, can worsen ME/CFS. That was my experience.
Yes!
Also…in some people, pre-existing CCI, and/or other consequences of underlying joint laxity, may only be revealed (or first start causing significant symptoms) when sudden (entero)viral damage causes severe weakness, even partial paralysis, of core muscles. (The latter possibility is touched upon most directly in The Polio Paradox).
If this were the case, people with underlying joint laxity could be more severely/permanently affected (particularly by ANS symptoms) than those who suffer from the same neuron-damaging (and severe weakness-inducing) viruses, but who have better inherent joint strength/integrity to better house and protect their spinal cords and brain stems.
Here’s a link to a story in the Sun – I don’t know if that’s a tabloid or not – to a person who was first diagnosed with ME, then EDS and then finally with CCI. -https://www.thesun.co.uk/fabulous/8521257/mum-condition-head-ehlers-danlos-syndrome-eds/
The Sun is a dreadful UK tabloid, for what it‘s worth.
This poor woman only finding out in 2018 she has EDS, 15 years after an ME diagnosis. And yet she must, of course, have had EDS all along, and so can we be sure ME wasn’t a misdiagnosis in 2005? She says she was visiting a lot of GPs before then.
I do though know of growing awareness of hypermobility syndromes and ME comorbidity.
I do wish this woman in article the very best, her CCI sounds terrifying.
They are both the same illness, the only difference is the Names used from ME CFS Fibro EDS just Names Labels
ME/CFS is Ehlers Danlose Syndrome types some can have a ‘crossover’ multiple types involved like EDS3 with EDS 4 or
Tenascin X or even Classic type or other connective tissue disorders, some not all even have attached ear lobes to their
face this is a sign of abnormal connective tissues…ME/CFS same illness just different names Labels
In 1990 around the time I was diagnosed with ME I was seeing a physio for twice weekly appointments to work mainly with my suboccipital muscles. This was after my GP had found some abnormality in the range of movement in my neck.
My physiotherapist, who was senior in her field, had recently returned from a conference in the UK where patients presenting with ME had been discussed. Apparently what she was seeing in me was typical for this group of patients. What she was also seeing was the problem return 100% in my neck between appointments. She still worked relentlessly on me for an hour twice a week for a year!
Recently a fibromyalgia sufferer (of 15 years) friend told me he’d regained his health. He specifically credited having learned how to work on trigger points in his suboccipital and SCM muscles.
The suboccipital muscles can be worked from the ‘reverse’ side by moving the eyes! My understanding is there is a connection with these muscles to the stability of the top two vertebrae. I think this may be a fairly recent discovery? There’s lots of info about this available on the net.
Polyvagal theory explains how tension here may fundamentally affect the nervous system keeping us in sympathetic dominance. The ANS, and quality of stage 3 sleep are affected by feedback to the brain on the state of the respiratory system – via the vagus. The eye muscles give feedback too, because of how the oldest branch of our nervous system is wired.
One helpful way to work with the suboccipitals in a way that ‘holds’ may be by releasing tension off the scalenes and the SCMs which are our secondary respiratory muscles. This can be done by trigger point release but also by re-training diaphragmatic breathing, both to take some strain off those over-stressed neck muscles and to increase vagal tone through the mechanoreceptors (pulmonary stretch receptors) in the lower lungs. That and working the eye muscles carefully. A book called Accessing the Healing Power of the Vagus details an exercise to work the eye muscles to affect a shift in the nervous system, but you can also hear the author describing the exercise in detail in various podcasts. Big tie in here with treating trauma and PTSD.
Apols for such a long comment! It’s such an interesting topic!! 🙂
Thank you, very relevant for me!
“That and working the eye muscles carefully.”
What do you think is the reason that eye muscle work helps? What do you *feel* helps when doing it?
When looking at my case, I can’t lift my eyelids (easy) enough and move my eyes to look in front of me when having my head straight. So I have to point my head a bit upwards in order to look in front of me with my eyes “falling down”.
I can imagine I move my head more then another person if I want to look left or right too, exhausting my neck muscles and compromising my head to neck position. Would that (less need to move the head when looking in different directions) relate in any kind to your experience after doing these eye muscle exercises?
Good for Jeff on his determination and health improvements.
Just some information regarding Chiari Malformation. My daughter was diagnosed 15 years ago with Chiari Malformation. Her only symptom was headaches. She had her surgery at Stanford 4 years following her diagnosis.
She wanted to continue and grasp from college prior to surgery.
The neurosurgeon told us he was surprised Malformation was as severe, once her got in there. We are grateful to have it behind us. Sometimes it just takes the right Dr. Sad for some.
Hi, my symptoms worsened after my neck was pulled up off my head, unexpectedly, during treatment. It’s been 18 months and I’m still mostly couchbound. I’ve had flexion/extension studies that show no structural instability. However, I have EDS and think the ligaments are overstretched. Where do I go for diagnosis/treatment. I feel like I have a bobble head, hard to stand up.
If I understand correctly, Jeff was doing well until January when an unexpected movement during physio damaged his fusion. All his symptoms returned with a vengeance. So please don’t try this at home (e.g. asking someone – even a doctor – to pull your head up off your neck!)
Hi, Di. This is Jeff (the same Jeff Cort is referring to in this write-up!).
I am actually doing great. The event you are referring to occurred in late 2018, when a physical therapist twisted my skull without warning or asking. This maneuver resulted in 3 (out of 6 total) of my fusion screws loosening, which brought on a return of *some* symptoms, but at a much less severe level than they were prior to surgery.
I subsequently had a revision surgery, which replaced those three loose screws, and I am back to full health once again. I am hitting the gym, pumping iron, going for long walks — all without PEM or POTS.
I am glad you drew my attention to this, as I will need to update the broader Phoenix Rising community about my revision surgery and restored health.
All the best!
– Jeff
http://www.mechanicalbasis.org
Pumping iron!!!
That is SOOOO cool, Jeff. So relieved to hear it. I’d been following your progress and can’t tell you how happy I am for you.
I love you!
Although I am sure Jen Brea has had to spend a lot of time lying down since becoming ill, I wouldn’t say from her activities that she fits the description as having been ‘largely bedridden during these last seven years’.
I removed the last part of that sentence.
Great article Cort. Thank you!
I wonder what the mechanism is by which a viral infection could later cause hyper-mobility. Two things come to mind:
-Dr Gordon Skinner writing about post-viral CFS/ME argued that a viral infection can lead to hypothyroidism at cellular level. By this he meant that the cells are not getting enough thyroid hormone despite the fact that there is enough thyroid hormone in the blood (this could be due to an issue with thyroid uptake by the cells). See his book Diagnosis and Management of Hypothyroidism.
– Dr John Lowe writing about Fibromyalgia recalls a 1975 Study that documented joint laxity in hypothyroid patients. (See Dorwart and Schumacher, 1975).
In other words: could the viral infection have impacted thyroid hormone regulation at cellular level and this in turn impacted hyper mobility?
Also:
– Golding, 1971, “ musculo-skeletal features of hypothyroidism” describes “ligament laxity” in hypothyroid patients.
Interesting blog!
I have had many people ask me if I have a sore neck because they say I turn my whole body to look at them as my neck only turns so far.
And every masseuse I’ve ever been too has said I have an unusual upper spine curvature. It’s so bad that I have to put pillows under my chest to stop pinching the nerves in my neck while laying on massage beds, as if I don’t I get pins and needles in my arms and pain in my lower neck.
But I don’t get the headache mentioned just severe ME/CFS symptoms and Orthostatic Intolerance (not POTS) for 29 long miserable years now
So is it a stiff oddly behaving spine coincidence or should I get this checked out?
Also would a chiropractor be dangerous with the CCI/AAI condition?
Interesting article. I’ve been in conversation with my doctor for years trying to find the “why” into my Intracranial Hypertension/Pseudo-tumor cerebri/ Idiopathic intracranial hypertension – *Translation for all…”We don’t know why you have elevated CSF, but lets put in a shunt for a better quality of life.” And, it helped. However, many of the symptoms noted by Jeff and Jen are spot on to my symptoms to this day (turning my head to the right makes me feel like I’m blacking out or falling, gasping in sleep, trouble swallowing, heavy head, stabbing pain in the back of my skull, etc) In a week I will be starting the process to find if CCI is the culprit. Insurance will not pay for me to get an MRI with flexion/extension, so I have to start with the flexion/extension x-rays first. Really hopeful to narrow down at least one issue to my on-going health issues with ME/CFS.
Good luck Lisa!
If you live on East coast, DR. HENDERSON is the BEST.
Collette Christianson where is Dr Henderson located?
I live in NJ.
How do you even start to get the necessary MRIs and CT scans? Do you convince your PCP? Most neurosurgeons require a referral.
I’ve been calling around with no success .
I’ve been diagnosed with POTs and cfids/ME.
Maybe show them Jeff’s and this article and ask for a neurological evaluation? Mention symptoms which could indicate CCI/AAI?
Jeff never mentioned going to a Corrective Chiropractor. All they mostly study (for more total required hours than an MD) is nerves and spine. Treatment are based on working WITH the body to free it up, and they all do the proper standing Xrays.
The head/spine issue is often a problem with babies, when drugs are used to speed up a natural birth, slamming the head into the cervix again and again. Frequent ear infections are considered one aftermath. Did Jeff have those as a child?
Adults get it usually from a fall or car accident, where the forehead hits something.
Adults are easier to adjust then a baby, or at least less nerve racking, plus they can do exercises to strengthen the supporting ligaments and neck muscles.
One easy test for neck weakness is just to lie across your bed on your back, and hang your head off. Just a little at first. Try to lift it up. Good? Try it again. Doing OK? Then on sides, stomach.
Have a friend there, in case you get dizzy or nauseous.
A good Chiropractor can save people from a lot of issues due to a pinched nerve to the lungs (asthma?), heart, guts, various organs, or limbs.
A physical, emotional, or chemical stress lowers the immune system and triggers ME/CFS; Removing that stress helps reverse it.
So fixing Jeff’s f-d up neck and then having his extreme ME/CFS also greatly reduce in severity is no coincidence, and yes, the neck was the cause, but indirectly. Childbirth, infected bug bites, some patented medications (=chemicals), or divorce can also be a cause.
Almost every adult with CFS remembers the triggering event in 20/20 hindsight.
What do synchronized swimming, karaté and Yoga/Pilates have in common ? They all need the head to be in a very specific position. All my teachers in these sports ( in my previous life…) have remarked on my neck and tried to put it in a specific position that I could never maintain. I will definitively look into this cranial thing!
Cort, this is such a valuable article. Thank you. I really think you are on to something here. And the comments thread is excellent.
I too had been struck by the ‘coincidence’ (?) that both Jen and Jeff developed CCI and AAI, despite not having hypermobility problems prior to developing ME/CFS. Jen, for example, says that she believes she still does not fulfill the diagnostic criteria for any of the 13 types of EDS. Yet the logic flow that I had seen until now indicated that CCI/AAI was as a result of a connective tissue disorder (EDS), which is a genetic disorder i.e. you either have it or you don’t.
Dom’s point though is that there might be a link between a virus causing hypothyroidism at the cellular level, which in turn might impact hypermobility [… and thereby cause ME/CFS].
I have been searching for any evidence that the connective tissue disorder could be acquired, rather than something you are born with and now this does indeed seem possible.
There is such an overlap in between symptoms cause by a spinal fluid leak or by AAI/CCI on the one side and ME/CFS, POTS and fibromyalgia on the other. Perhaps we could indeed be looking at a root cause here.
I wanted to refer two more articles that I think are relevant: Ruiz-Nunez, 2018, documents “severely depressed T3 tissue levels” in CFS patients. In other words, Independently of blood thyroid hormone levels, CFS patients had low levels of the active thyroid hormone at cellular levels. Holtorf 2014 explains the mechanism of up regulation/ down regulation of the enzymes responsible for conversion of T4 into RT3 and T3 respectively during stress or inflammation which could explain this finding. (And as mentioned above: Other studies have documented an apparent link between hypothyroidism and ligament / joint laxity). So viral infection, depressed active thyroid levels (I.e. T3) at cellular levels, and hyper mobility could be linked? The late Dr John Lowe and late Dr Gordon Skinner argued yes.
I wanted to correct my last sentence. I’m not sure that Dr Lowe and Dr Skinner argued the link between viral infection and hyper mobility. Just that: Dr Skinner explained that viral infection could trigger hypothyroidism at local cell level. And Dr Lowe argued fibromyalgia was hypothyroidism at local cell level and he referenced ligament laxity as a symptom of hypothyroidism.
Hi Dom, could you please provide links to the cellular T3 information? Thanks!
The reason why a connective tissue disorder is such an important piece of this puzzle is not just because of its linkage to CCI/AAI, but also because it is so often associated with spontaneous spinal fluid leaks. The dura tears and spinal fluid leaks out, resulting in brainstem compression. And that part of the brain is involved in controlling so many functions which are typically associated with ME/CFS symptoms.
Plus – there is this ongoing question as to how pathogens are crossing the blood/brain barrier and causing brain inflammation. One answer could be that they are getting into the spinal fluid via a tear in the dura, and from there circulating to being in very close proximity to the brain.
Again the logic flow in this subset could be:
pathogen (e.g. a virus) causes hypothyroidism at cellular level => weakens connective tissue => either CCI/AAI or spinal fluid leak => a) brainstem compression and/or b) brain inflammation due to pathogens crossing the BBB => ME/CFS, POTS, fibromyalgia symptoms.
Another subset route could then also be an injury such as whiplash, later causing a micro spur which tears the dura => brain inflammation => ME/CFS, etc.
I’m not yet convinced that pathogens leaking in the spinal fluid have *excellent* access to the brain itself, but it sure does sound like a bad thing.
You may be close to something else. Most body liquid are under pressure. When a vessel ruptures fluid leaks out of it towards the rest of the body. That’s an important function as it strongly reduces the number of pathogens entering the delicate structure.
For example: when you cut yourself at your hand blood leaks out of the veins both cleaning the wound and forcing pathogens to “swim” up against the stream of out-flowing blood, strongly reducing how much enter the veins this way.
When talking about spinal leaks, it suggest the image of spinal fluid leaking out of the spinal fluid bag into the rest of the body, again strongly reducing the number of pathogens entering this delicate structure.
But the spinal fluid bag is like a big volume at the brain itself with a very long and narrow tail running along the spine. This tail has modest volume but a fairly large surface area. Now imagine that this tail is largely “cut off” from the bigger brain bag. For example by mechanical force near the neck squeezing just a small section tight, making the brain bag and the tail nearly (and temporarily depending on head to neck position) two separate bags.
Now move the back/spine/neck/head. You’ll easily get a significant volume change of the long tail. As the flow to the big brain bag is very poor due to the “squeezing” of a passing near the neck, the liquid in the tail can’t shift quickly to the big brain bag. Pressure can rise fairly quick. In combination with poor structure like EDS/collagen problems or structural weakening due to chronic high oxidative stress it would make chances to create leaks a lot higher. That would be sort of a combination of a pre-existing weakness in combination with a trigger.
But the reverse of leaks may be the worse thing. After moving in a direction that reduces the volume, increasing pressure in the tail and allowing spinal fluid to leak out one could move the head/neck/spine in such a direction that the volume of the spinal tail bag would be expanded compared to resting position. That would create a lower pressure in the spinal bag compared to the pressure of the liquid (such as the liquid in fascia) surrounding the spinal tail. That would create an effective short lasting suction power drawing liquid in the spinal bag.
While that would restore liquid volume in the spinal tail, that would be a bad thing as it would not be spinal liquid but other liquid with very likely higher pathogen counts. And once it gets in, it’ll easily grow and or spread into the rest of the spinal fluid.
Each time you have got a “contraction/expansion cycle” spinal fluid would leak out of it and “polluted/foreign” fluid would leak into it. That sounds bad. IIRC increased cytokines have been found in the spinal fluid of ME (and FM?) patients.
Much would depend on how big the volume changes are per movement and if or how much the passages from the brain bag to the tail are blocked and how long each blocking lasts.
In effect it *could*, if this hypothetical phenom even existed, lead to the body increasing spinal fluid pressure. That would decrease changes that any section of spinal fluid ever came into a situation of under-pressure (allowing for inflow of polluted/foreign fluid in the presence of leaks).
The cost however would be chronically increased spinal fluid pressure impacting brain functioning and reducing blood flow towards the brain.
dejurgen,
I love your ability to theorize on so many diverse subjects, and so convincingly! Every time I read one of your detailed break-downs, I feel like all you need is a lab (and some major funding), and you would very likely figure this mess out for us! (Seriously.)
My best,
Martha
Thanks for the kind words MarthaLauren.
Glad to hear some people read my posts and find them useful. Wouldn’t have been able to read and understand them myself just 3 years ago :-).
I think no patient as sick as Jeff, Jen or how sick I was should have to deal with this devastating disease and try and figure out how to get out of this mess even a little bit by themselves. It may seem to come easy, but I can’t handle running my own little household without help both physical and organization wise (mental, focus). Let alone running a lab :-).
If people like Jeff and Jen and maybe one day myself can make a significant contribution to further understanding and treatment of this disease then it is first and foremost a testimony to what a healthy crew with people with diverse skill sets and the will to truly listen to patients experiences could achieve when given even moderate funding.
For a systemic disease, the lack of even considering the impact of mechanics and physics is astounding. Less then a few percent of medical research papers even mention it.
As an engineer I see nature loves to use very simple structures over and over again and build larger complex structures with it. Having knowledge of basic system design and control theory is completely lacking in medical literature. It’s totally unexplored territory. That’s why laypeople without any prior medical knowledge can achieve something in this field. It’s full of (very) low hanging fruit.
Above all I’d like the medical community to see this as a wake-up call and opening the eyes to search for other ways at looking at our disease(s) and take this job out of the hands of exhausted and physically and mentally disabled people.
ME/CFS is Ehlers Danlos Syndrome a connective Genetic tissue disorder & these above are complications of having EDS & some have ‘other’ connective tissue disorders ex: Marfans etc
I think this is the case with me. I suffered TBI 6 years ago, then diagnosed with Fibromyalgia, POTS and ME/CFS in that order. A bout of mycoplasma pneumonia two years ago seems to have teed off the ME/CFS. The TBI was the result of a closed head fall and I experienced significant cervical and lower spine injuries. The blood/brain barrier was likely breached. I’ve had bizarre symptoms of random joints “flaring” one day and be fine a few days later with inflammation, often only on one side of my body. Woke up one morning with both wrists cramped in place and they fully resolved two days later. My neck cannot support my head and I get terrible headaches in my occipital muscles into my scapula along with Trigeminal Neuralgia along one side of my face. Joint pain and pain along my entire spine is a major problem for me along with the fatigue, dizziness etc. I’ve had a hard time getting treatment and have been tossed back and forth between rheumatologist, neurologist and now back to cardiologist. Nobody knows what to do.
This is a very interesting article. Some time before I was diagnosed with fibromyalgia I had a severe painful neck problem and it was diagnosed as a degenerative disc bulge C5/C6 level causing a narrowing of the neural foramina bilaterally. Appart from that I recognised several other things that were discussed in the article,for example, stopping breathing during sleep, and breathlessness. I have found over the years that a certain neck exercise relieves the breathing problems!
And then a few years after the neck problem started I developed fibromyalgia! The article gave me food for thought that’s for sure!
Just to add yet another structural disorder that may play a factor and is not well know is Eagle’s syndrome. This is a vascular disorder where the styloid processes are abnormally elongated and impede on vascular structures in the neck leading to altered blood flow to brain. The literature states it is only noted in 4% of the population and in that group only 4-10% are symptomatic – however, in the last 2 weeks I know of 5 people in a 500 mile radius with positive documentation…..hmmmmm. I have been diagnosed with ME/CSF and a skull base CSF leaks, currently receiving surgical treatment.
You are very right about your comment Nicole on Eagle Syndrome it also can be a complication of Ehlers Danlos Syndrome & some can have the
Classic type or the Vascular type with (EG) that is why a diagnosis with proper imaging is crucial for a recovery
All this discussion is very interesting. I fall into the zebra camp with EDS and have long read about all my brethren with difficult to diagnose spinal problems (CCI, Chiari, and tethered cord etc.). There is also a high percentage of EDSers who experience CFS like symptoms (80-90%).
Also there are many who have had virtually no compromising issues with their connective tissue disorder until ‘an event’ whether it is an accident, surgery or other stressor which brings on PEM and all the other symptoms of ME/CFS with a vengeance.
Unrelenting fatigue is a very common symptom of many disorders, and I do wonder about the effort to discern the ‘true’ ME/CFS. It seems to me that there is often a confluence of factors–some more common than others.
I recently completed a MTHFR clinical trial by Dr. Klimas and about a month in I could tell I was given the placebo–my functioning had declined from bad to worse. This was later confirmed. So could similar be the problem for some of us?
I’m mentioning these things because I believe lack of energy production can be caused by so many factors and it is possible that ME/CFS is actually a severe reaction to any number of them–or a combination. Viral? ANS? CCI? Gulf War illness? Genetic? Or? I don’t know.
I suppose until the Gorgon’s Knot of causes is sorted out, the most I hope for is some kind of amelioration of my symptoms.
Any more News on where Dr Nancy Kilmas trial is Published or released? What were they using a steroid? The likely causes are (AG) Alpha Gal Meat Allergy or (HATS) Hereditary Alpha Tryptasemia Syndrome http://www.tryptasemia@genebygene.com multiple copies of the tryptase gene handed down from each Parent at Birth & yes (HATS) is in EDS
Key in tryptase on the http://www.genebygene.com website the blood test kit opens up & the cost is $169.00 requires an MD referral
the lab is in Houston, Texas & is the NIH/NIAID blood test from Dr Joshua Milner’s Team & their videos are on Youtube under
tryptase there are numerous one put out now for awareness on (HATS) Hereditary Alpha Tryptasemia Syndrome
The test above now is only being done in Batches at http://www.genebygene.com so inquire with the lab if you decide to be tested there with your Doctor for (HATS) Hereditary Alpha Tryptasemia Syndrome testing
Aidan, my study was about folate. I have a genetic mutation which means I can only absorb and use about 50% of the folate I take in via food or supplements. Folate is VERY important in a lot of body processes. MTHFR mutations, and there are several, can have different levels of impact on folate processing.
The way around this is to get methylfolate (a more useable form) into the body. I was told not to take any kind of folate for a number of months, and only use unmarked pills Dr. Klimas sent. By the end of the study I noticed that my energy had gotten so much worse and it was revealed that I had the placebo.
They took labs at the beginning and end of the study and a couple of weeks ago her team sent out the results to the participants. No word on when the actual results will be tabulated and released.
I don’t think this was about tryptase and EDS, however not too long ago there were a small group of individuals who a different group of researchers identified as having multiple copies of the variants which controlled tryptase. It certainly wasn’t a discovery that could be applied across the board.
Excuse me, students of ancient literature; it’s Gordian’s Knot.
thanks, I hope you get answers soon
Very interesting article and it reminds me of research done by the Rheumatologist Dr Andrew Holman where he thought there was a link to symptom increase in Fibromyalgia when the ligamentum flavum was irritating the spinal cord when the neck is in extension. He thought this increase sympathetic tone. His physical therapist designed exercises to stabilise the neck and body to reduce symptoms.
I’m very glad to have read this article (as well as Jeff’s and Jen’s direct accounts at the links provided).
I’ve suspected for some years that my condition had some structural component. My entire torso and neck turned into one solid mass of muscle/facia when I fell ill (typical viral onset), and I have ever since been trying to find ways to release it. It’s always felt as though my nervous system (maybe even my blood flow) was being held hostage by these strangling tissues.
But no matter how much massage, self massage, stretching, yoga, and gua sha I do, the tension always returns rapidly and with a vegence. If I do too much loosening work then whole sections of my back/neck go into many-day spasms, as if to desperately guard/stabilize the newly loosened systems underneath.
And then, if I do too much upright activity in this loosened state, or even gentle activities like yoga and stretching, my neurological symptoms and ANS imbalance becomes acute.
For years I thought of excessive movement (or exposure) of my spine to be just one other way to irritate my hyped-up nervous system. (Along with bright light, loud noises, bumpy car rides, etc.)
I had no other way of making any broader sense of this until a PT suggested that I look into EDS, as I met most of the criteria. After looking into that more with a knowledgeable practitioner it appears I fall into the newest border category of “hypermobility spectrum disorder”, and not EDS.
But as my health has improved through various other means, it’s become increasingly clear that the only sure fire way I have left of enducing the worst ANS symptoms is to be too aggressive in my structural loosening/strengthening regime. And, as I do anything to successfully bring down systemic inflammation: my spine is again left in what feels like a more vulnerable and loose state. So I have to start all physical re-hab very slow, and incrementally increase both ends of the equation (loosening and strengthening) in unison.
I have had none of the tests to diagnose specific joint hypermobility (or CCI) except an X-ray of my neck done by a chiropractor which did show instability in the first two joints of the neck: the atlas and axis. And the special (NUCCA) maneuver she did to re-set those joints did appear to be remarkably effective, particularly for my ANS symptoms and heat intolerance..but it never held.
Sorry for the long post.
I guess my point: after multiple clues and many false starts over many long years, after reading more articles like this I’m beginning to thing that my perceived spine hypo-hyper-mobility could be not just another part of all this, but a very central part. I plan to now take my instincts and interventions in this area very seriously and carefully. (And, pay most careful attention to that uppermost joint, in particular.)
Thank you to Cort for bringing attention to this subject, and to Jeff and Jen for sharing their arduous stories. Best of luck in your continued healing.
I will say this is to look into numerous other conditions with blood testing because all of these can cause serious drops in blood pressure & they go with EDS & it would not also indicate why people have
activated bacteria/virus antibodies if ones blood pressure is constantly falling even during blood draws or prior to going in for these tests…One is (HFI) Hereditary Fructose Intolerance, the other
is (HATS) Hereditary Alpha Tryptasemia Syndrome & also rule out/in the Alpha-Gal Meat Allergy( AG) Sugar Antibody from animals now being found in Humans originating from Lyme ticks…
OMG. I am literally short of breath reading this. I know it’s not the time to be speechless but after being so sick with ME, sometimes wishing for death, I saw Dr. Henderson and he concluded that I didn’t have EDS but did have some spine instability and put me in a neckbrace for a month (currently wearing). I left the office a bit disappointed-again-one more dead end rabbit hole and a heartbreaking concession that I’ll never ever get better. Despite my misgivings, I’ve been wearing the brace anyway and…I haven’t felt this good in YEARS. Two weeks later, I’ve come across your article. Jeff, Jen, Cort, I seriously love you and-now that I feel my brain working-I’d love to repay you all in someway. In Gratitude, Colette
http://www.meandcfs.com
Also-I’ll be in DC for lobbying on April 3 if anyone wants to join me:)
Brace in your neck could also be lifting your skull up more releasing pressure from bones from an Eagle Syndrome diagnosis causing vascular issues
“Well Dr., This all started after a bout with Mononucleosis and the fusion of three vertebrae…”
Amazing Blog CJ. I’ll send some money after immigration takes their cut. Nice work.
🙂 I was totally astonished as well.
Thanks!
It is so interesting to see this post.
I have had a range of symptoms, sometimes describable as some sort of CFS, fibromyalgia and sometimes describable by some sort of psych diagnosis (ADHD or Bipolar).
I had significant initial relief from Atlas Profilax, but it was not long lived (probably the result would have been more durable if I had not been chained to a desk by my work!).
The significant symptoms came on soon after a whiplash (hypomania at age 27, with no past history).
Im a health practitioner, but will probably retire as the lifestyle is not good for me. However through working with my chiropractor (also a functional neurology specialist), I encountered a book detailing the area called “The Craniocervical Syndrome and MRI”. The book is the result of a substantial collaboration between Neurosurgeons, Chiropractors and Radiologists, including Ralph Demadian, the inventor of the MRI– no lightweight.
Now a couple of things came forward for me-
1) the instability is probably driven by ruptures of one or more of the two alar ligaments and 2 transverse ligaments (responsible for stabilisation of the odontoid process of C2 on C1 and the skull).That’s a permanent injury though good physical therapy or surgical therapy can help it (surgery being the least preferable option).
2) There can be localised and specific impingements on vascular supply (my reading has found a subclinical “lateral medullary syndrome” as a likely issue. These can certainly cause symptoms of autonomic dysfunction, and it is probable that the most likely one could be hypertension. How3ever non specific dsautonomia is certainly going to hold you back.
3) However the mechanism that most attracted my interest was a functional neurological dysfunction: Namely there is no longer a clear relationship between the incoming information from the body below the entry point to the skull (the foramen magnum), and the actual position of those body parts.
Think about it- those upper joints, which contribute enormously to our perception of our body’s position, and the actual position of the body, no longer contribute information that has a one to one relationship with reality.
Our brainstem has an essential role in taking in all the body position, and movement coordinates and amalgamating them. The role of the vestibular system in this is enormous.
However the vestibular neurones are the most active cells in our body.
If there is no longer a one to one relationship between our head position relative to the body and the real relationship that is a huge problem. those neurone pools become radically over worked, and those systems collapse.
Now that, to me, sounds like a recipe for severe fatigue.
I am not trying to offer a complete solution here, ( I do not have enough training to do that), but this is interesting, it correlates closely with my own improvement (including the ups and downs) and it offers ways forwards that hopefully increase our independence.
Whiplash is estimated as a problem in 3,000,000 US citizens each year, and that does not count the borderline cases.
The reading I have done suggests that craniocervical instability and atlas subluxation as described by some chiropractors are probably the same condition.
However it looks like symptomatology is driven by a number of different mechanisms, which means that we all may be faced with a significant period of fruitless attempts to solve our problems until we find exactly the right mechanism and solution.
Thanks for another great post.
My orthostatic issues increase greatly when I look up at the ceiling, but not when I look side to side. It used to cause vertigo. (I’ve had neck pain for decades.) I wonder if CCI/AAI can manifest that way, or perhaps that’s something else. Anyone else have that experience?
I have POTS, MCAS, APS, porphyria, and a few other things. (I think I have one underlying mechanism that Western medicine only knows how to understand with these discreet diagnoses.)
Not sure if someone else already asked this question, so forgive me if it’s redundant. But I’m wondering if the axis adjustment sticks if you have hyper mobility and lax ligaments and joints? Does anyone have any ideas about that?
I dont know how they would but some people still say they have had improvement with the technique. I myself had a session where I felt better for a few days but things seemed to go back fairly quickly
This has been a common finding inner clinic for years, but we did not label it this way. The most challenging patients for us to treat are those who have had upper cervical adjustments. As some have suggested, if we take a comprehensive approach, many small improvements can add up to greater and greater independence, but it is always so tempting to go for the quick fix (which is almost universally a flash in the pan). We can identify this with functional HRV and CBVT, but that is just the beginning of the trek.
Nancy B I read one article yesterday it was a Doctor from Glasgow she had an ear infection she was given Cipro she got much worse all her MRI’s including CT’s cam back Normal readings she then had a proper CT done she
was diagnosed with Eagle Syndrome she believes the Cipro caused the calcification of her styloid process in Eagle Syndrome. I know one Guy after years of sickness he was diagnosed with Silent Migraines he
recovered 100% with diet & did not mention though which medicines he was taking…I think it is not CCI/AAI Steni=osis or Chiari or Tethered spinal cord it is likely Eagle Syndrome within some also having a Skull
based spinal fluid leaks…Eagle Syndrome can cause also Allergy nasal issues & dripping fluids. I had an abnormal Panoramic Dental x-ray showing bone on both sides, the left was worse thick long pointy right
side partial showing was very pointy…
Jen Brea’s POTS is gone! Check it out here
https://medium.com/@jenbrea/health-update-2-my-pots-is-in-remission-8fceff9c1744?_referrer=twitter
Symptoms of CCI is Ehlers Danlos Syndrome most in time get worse the gadgets they place inside cause weakness of muscle surroundings it is not any Cause it is a result of connective tissue not working it would work better if she was screened
properly for Eagle Syndrome calcification removal, ES makes the blood pressure drop it is a major cause of Syncope neurally mediated hypotension POTS like symptoms countless now are being rediagnosed & people do better with full not
partial removals through the neck or base of the back of the skull. When I saw Dr. Schondorf top Neuro in POTS in Montreal after I did Hopkins, he said the tilt table at 45% gives Syncope he said we do not walk around at 45% he does only standing
straight up table testing he uses no tilt at all he said you do not have syncope, Hopkins said I did he also said you do not have POTS either he said something structural is going on. I do know though Eagle Syndrome makes the blood pressure
drop it also plays a major role in heart rates & blood not getting to the organs…I will be screened now for (HATS), Alpha Gal Meat Allergy & Eagle Syndrome I already have an abnormal Dental Panoramic Scan put on my NHS file. Even patients told
they have Chiari they do not even meet the Chiari diagnosis they do not fit in the box. The illness goes away with 2 operations one at a time. It also explains why medicines, vitamins & quackery have never worked all these people have been
labelled with countless conditions I was told EDS 3 & partial Marfans Syndrome I just saw a top Genetic Doctor she said No I do only fit (HSD) Hypermobility Spectrum Disorder under the new criteria. Even if I have (HATS) all it means is I was
born with the condition it is something else going on that is certain & there never ever was an infection ebv cmv hsv1 hhv678 lyme are all antibodies our immune system puts out antibodies. Chronic Lyme is another hoax diagnosis so is MCAS &
Mold pure b.s. lies…They will never ever find a Cure for structural Eagle Syndrome it requires a Good skull based Surgeon in ENT & the throat operations are failures they do not take out enough bone(s). We need Surgeons, competent experienced ES ones
So in his case, at least, the viral infection caused the CCI which then caused the ME-CFS symptoms? Or are the two things unrelated coincidences?
We don’t know but it certainly seems possible.
No one knows how the 2 are related yet, but there is some literature one can find, that discusses ligament and other issues arising after infections.
Regenexx involves PRP and/or stem cell treatments targeted to damaged tranverse and alar ligaments. It is performed at the Centeno-Schultz Clinic in Colorado. Caringmedical is another clinic that treats these areas. They can also treat herniated discs. The procedure to address craniocervical junction issues is in its infancy. When treating the ligaments, they have had fairly good success. I do not believe they have treated “ME/CFS” patients yet. Regenexx’s Dr. Centeno has several informative Youtube videos on this subject.
I have treated about 30 000 people, many of them diagnosed with ME/CFS. My specialty is to put the atlas/C1 in the correct position. The first joint between occiput and Altas is an egg joint, it is bowing and side bending. In wrong position it is twisting too. (That belongs to the next joint). Then the opening in the foramen magnum gets smaller and some of the signals or the cervical fluid don’t get enough space. Then people can get different problems.
The skeleton is not standing in right angles when the atlas is out of place, and the hips get twisted to compensate. The muscles are protecting all this and the body needs a lot of energy to do so.
At once, instantly, when the atlas is adjusted (not manipulated) the body is balancing and aligning. Then you can get tired and sore in the muscles who are relaxing. You can although get some fantompain from old issues. Maybe some of you are recognizing themselves in what I am talking about.
Don’t give up.
My daughter injured her neck surfing, she had upper cervical chiropractic adjustments but still suffers and has are POTS and MCAS and EDS. Are you saying the upper cervical adjustments will make it harder to treat the CCI? Can you explain why?
thank you for this helpful info Waltraud. do you know anyone that is good at what you do in the SF bay area? thanks for the encouragement.
Great Article! Yay, Sweden!
Yep, on point! What a model !
Connecting the puzzles pieces!
Instead of surgery is why I go to Chiro. Care but it is on going and haven’t got any Dx ..just checking the boxes (areas) health history and doing what Jeff did…Det. work??You are your best Dr.?Reseacher
Hi Guys. My name is Paul from the UK. This has rung so many bells with me it’s unreal.
Background. Mid fifties at the start. Non smoker – fit – normal BP HR and Cholesterol.
My symptoms may have been coming on for over 10 years, but have only been apparent for 6/7. Started with breathless when bending over to tie my shoes, then stomach issues such as reflux and taste changes. Then more and more tirdness. Eye issues, Concentration issues, mild ED, IBS. Had to finish work.
Then the tiredness became worse to the point of passing out and then a syncope episode. Another full cardiac inspection and tests revealed nothing. Then pain in my arms and ribecage – more tests – nothing. I was even told my heart was strong ( as I believed). Then- bang – Cardiac arrest and Heart Attack. Two stents fitted. Atherslerosis blamed but no proof.
The pain got worse, tried to change my cardiac meds and no improvement. The pain then gets a source – middle of my back then upto the neck. Arthritis ruled out but a Neurosurgeon finds that there is very little fluid left in the cervicle cord. Having an op in two weeks to insert clip/wedges between 3 vertabrae.
I was involved in a bad car crash when I was 19 – I’m now 63. These last years I have felt like a basketball as I’ve been passed from one medical disipline to another.
I’ll let you know how it goes and how many issues I managed to resolve.
Tale care Guys.
Paul
What a journey you’ve been on Paul! Thanks for sharing it and good luck with operation! And please do let us know how it went.
Curious about possible connection to non-epileptic seizures. I had a reactivation of Epstein-Barr which caused a cascade of related conditions, including functional neurological disorder. Perhaps the signals are getting scrambled due to CCI. I also have hypermobile EDS, dysautonomia, and moderate ME/CFS (housebound).
Thank you for all of this information. Very valuable. I am looking for a clinic or specialist in Canada so that I can speak to someone about this. Any ideas? I have all of the symptoms that are typical to CCI. I have been thinking it could be ME/CFS. It has gotten considerably worse in the last 4 months.
It’s been almost 12 years since I was attacked during my work by a man with a dagger. He had orders to gouge out my eye with the handle of the dagger, but the arm of my glasses had moved this blow slightly downward and backward. Instead of the eye, it was the skull that had to withstand this blow given with full force, but the damage caused to the brain as well as that caused by punches and others has never really been investigated by health professionals. to this day, given that the CSST (today CNESST), i.e. the Work Accident Insurance of this Province called Quebec, after a second stabbing attack which occurred a month later (May 14, 2012) was closed, this when the two files were merged together for administrative reasons, probably by error or who knows, the file of the first incident arrived in mid-April 2012 (the one with psychological and physical damage in full beginning on June 5, 2012, keeping open only the file of the second incident with a DX of Trauma (psychological problem) and refusing since that day to take cognizance of all the physical health problems due to the first incident, which they, given this, had the complete freedom to develop and thus to develop others until this day, that is to say March 9, 2024; including chronic fatigue syndrome (ME-CFS) with all the consequences that this amalgamation of health problems could and still does not develop today.
But instead of finding help from most health professionals, even though the decline in my health has been visibly visible since 2012, I have never found one or only one of these professionals. of health. especially with regard to the ME/CFS, who said he was ready to invest time in the direction of finding solutions to the problems caused by the disease, the worst existing, even worse than cancer , what is CFS and the consequences it can have; either for lack of knowledge of the subject, but especially given the pressure that the CSST/CNESST imposes on all people, doctors, lawyers, jurists, Administrative Labor Tribunal of this Province called Quebec, located at the bottom from the east of this country called Canada.
Just to cite a few examples:
For twelve years now I have been treated as an “imaginary patient” (CNESST and family doctor and others), as an “arrogant person, who claimed that another incident had happened” (CNESST), as a “person with a tendency towards narcissism ” (the phychiatrist of a large hospital), like “someone who refused to work and live at the cost of society” (psychologist), like “actor” (internist doctor from the same hospital), like “someone that he would have to be locked up in a psychiatric asylum, given that he was becoming a danger to society (family doctor), this by yelling so loudly during a medical appointment that everyone on the floor found themselves in front of the examination room and for good reason, that I took the liberty of asking him for the third time in a row to kindly send me for a test in a sleep clinic; of a “liar”, of a ” person, who only talked bullshit”; of a person, who only invented health problems to attract attention” and much more than that.
The end result of all this is that over all these years not only has my “credibility” been reduced to nothing, my “personality” has been trampled and crushed into the mud; my “bodily functions” are deteriorating day by day, given the muscle wasting which has been destroying the bones of my skeleton for twelve years, to the point of making me more and more disabled; fatigue destroyed my entire social network; the impossibility of traveling made it impossible for me to go visit my daughters who live in Europe, this from the beginning and to get to know my three grandchildren from one of them – in all, it’s been twelve long years without any enjoyment, not even the smallest, of life.
The accidents took place in 2012, when I was not even 55 years old; This year, I will be 67 and doctors have already told me that I can be happy if I reach 75 and that in 3 or 4 years, I will no longer be able to live alone.
And all this why. Not only because of work accident insurance which has hidden for twelve years an error made during the administrative closure of the file of the first incident and which, given this, refused all follow-up of physical problems (many could have been avoided if the doctors would have had the mandate to dare to take care of them from the start; but even worse, the refusal of the doctors, lack of knowledge regarding narcolepsy and the consequences of it on the human body, to note that this disease, ME/CFS, is a chronic disease that destroys the physical human body slowly but surely and without any respite.
The only question, which has been asked every day for a long time now, is the question:
How much time remains for the inner strength within oneself to still be able to accept this irreversible situation?
This is just another story about ME/CFS and I didn’t write it to draw attention to myself, my life and what I’ve been through; or what life I live.
I’m not looking for affection, or to be taken for a poor devil or I don’t know. This stage has long passed and I no longer need it.
I rather wrote it to alarm the world or RATHER that we alarm the world, that situations like I experienced, have completely become normal in the society in which we live.
Nothing has changed or almost nothing since this illness became a physical illness and not a psychological one; and that it is finally accepted as being a PHYSICAL disease by the UN (which is not at all the case by States, Ministries of Health, Universities or Schools of Public Health, even after 40 years)
Today, all the states in the world are investing billions and billions in research into LONG COVID; but the day will come when it will decrease and that moment will be the day when truly all these STATES will realize that between LONG COVID and ME/CFS there is no BIG DIFFERENCE.
And the reason is simple:
There are more people in the WORLD who have ME/CFS for more than a HUNDRED YEARS than there are people affected by LONG COVID, but no STATE IN THIS WORLD has the financial means to take care of these millions of people who have ME/CFS…. This would exceed all the budgets of the Ministries of Health around the world.
One of my daughters, who lives in Austria, unfortunately has LONG COVID; this at 33 years old. But she too must already notice that most doctors don’t take her seriously.
I can only hope for his generation and future generations that the STATE HEALTH INSTITUTIONS, the UNIVERSITIES which train health professionals, at all levels, take seriously this disease which destroys more people, more families, plus SOCIETY; but I am afraid that this will not be the case and that situations, as I experienced them, will continue to be normal.
This is unfortunately what will happen.
Adrian
My daughter has EDS, Dysautonomia, and POTS. Fortunately we were in a support group with a girl that had several surgeries from Dr. Bolognese. She has MAST cell, Chiari, EDS, POTS, and a pacemaker for her diaphragm. We knew about upright MRIs. We went to local doctors who didn’t know upright MRIs existed. So many doctors just don’t know about how all this affects the whole body. And try to tell a doctor something they don’t know. They’re so dismissive. It’s a very long road with very little support. I’m so glad you got the care you deserve.
This is so interesting as I am six years into CFS now & I’ve realized when my neck is stretched out (aka head lifted up…or even better…Y strap!) my symptoms tend to go away for a little bit.
I think I might have an answer for the ligament issue. My illness started after I took Levaquin, which is a fluoroquinolone antibiotic, which is known for messing up connective tissue and ligaments. (I’m not a dr so Google it for specifics!) it could happen with other drugs in the class like Cipro.
I took the drug after a viral illness so still uncertain about a lot of things but now I feel like I’m not crazy for the relief via manipulation thing. Ty!
I’ve heard a lot about the fluoroquinolones – thanks for sharing that.