

Thanks to Dominic for posting his comprehensive and fascinating overview of the use of T3 in chronic fatigue syndrome (ME/CFS) and fibromyalgia (FM) Please note that Health Rising does not provide medical advice or recommend treatments and Dominic is not a doctor. Please be aware, as well, that no studies have assessed the efficacy of T3 treatments in these diseases. Because long term thyroid treatments in the absence of overt thyroid abnormalities can cause the thyroid to shut down using thyroid medications in that context is controversial.
Overview
- Introduction
- Background
- Context
- Practitioners and pure T3 treatments
- Dr John Lowe (USA): Supra-physiologic dosages of pure T3 to overcome “thyroid hormone resistance”
- Dr Gordon Skinner (UK): Treating post-viral CFS with thyroid hormones
- Dr E. Denis Wilson (USA): T3 therapy protocol to “reset” impaired T4 to T3 conversion in patients stuck in “conservation mode”
- Dr Kent Holtorf (USA): Breaking a cycle of immune, hormone and mitochondrial dysfunction in CFS and Fibromyalgia
- Dr Barry Durrant Peatfield (UK): Treating a “down-regulated” metabolic status
- Dr Sarah Myhill (UK): Kick-starting CFS/ME recovery with T3
- Dr Jacob Teitelbaum (USA): Treating inadequate T4 to T3 conversion and thyroid hormone receptor resistance
- Paul Robinson (UK): Recovery from CFS with the circadian T3 Method
- Self-treating patients: Successes and frustrations
- Conclusion
- Table: CFS/ME Practitioners and key features of their T3 treatment
- References
- Websites – Practitioners
- Websites – Patient advocates
Introduction
In my search for what could make my wife feel better, I kept coming across stories of patients’ recovery from CFS/ME and FMS involving treatment with pure T3 (i.e. liothyronine, the synthetic form of triiodothyronine). These include stories on Health Rising by Edith Bouvier Dan Burns (x2) and Joy.
In this article, I aim to provide a succinct overview of the approaches and success stories of some CFS/ME and FMS practitioners with supplementation of pure T3 specifically, documenting each practitioner’s approach. But first I will provide background on the T3 hormone, and context to explain why treatments with T3 are so contentious.
Background
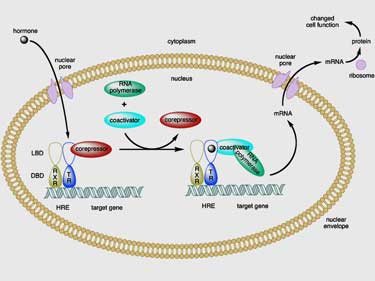
T3 is the “active” thyroid hormone, which stimulates activity in almost every cell in the body, apparently by binding to nuclear membrane receptors that control gene expression. Crucially, T3 serves to regulate the body’s metabolic rate by increasing aerobic mitochondrial function. Dr Myhill writes that if the body were a car, then the mitochondria are the “engine” and the thyroid gland is the “accelerator pedal”.
Moreover, researchers are now increasingly discovering T3’s complex role in immune responses (e.g. Jara et al. 2017).
It is important to know that while some of the body’s T3 is produced by the thyroid gland, 80% of circulating T3 is the product of “peripheral” (i.e. localized) conversion of the “less active” T4 hormone (which is produced by the thyroid gland) into T3 by deiodinase enzymes in the cells themselves (especially in the kidney and liver).
However, the story gets a bit more complicated because there are in fact three types of deiodinase enzymes that convert T4: D1 is responsible for conversion of T4 into T3 in most cells of the body, except for in the brain and the pituitary where D2 does the job (De Groot, 2015). D3 converts T4 into an inactive “reverse T3” (RT3) which (sometimes disturbingly) competes with T3 for space on the above-mentioned cells’ nuclear membrane thyroid receptors (note: D3 also converts T3 into T2; the role of this thyroid hormone is still being researched).
Critically, under certain conditions (such as inflammation, fasting or stress), D1 is downregulated and D3 is upregulated, resulting in less T3 and more RT3 at the cellular level. This can result in hypothyroid symptoms – even if the thyroid gland itself is functioning normally (Holtorf, 2014a).
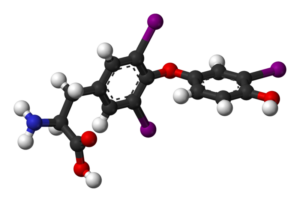
T3 – the biologically active form of thyroid
Finally, in order to understand T3 treatment, it is important to realize that thyroid hormones don’t just diffuse into cells but must be actively transported into them, and that the transport of T4 requires much more energy than the transport of T3 (Holtorf, 2014b).
In sum, T3 affects almost every physiological process in the body, and its function depends on the successful conversion of T4 into T3 by enzymes, the transport of thyroid hormones into cells, and the uptake of the hormone by nuclear membrane receptors.
Synthetically produced T3 (i.e. “liothyronine”) is generally sold under the name Cytomel in the USA (Tetroxin in Australia and Timorel in Turkey), and is used to treat hypothyroidism and myxedema coma (i.e. severe hypothyroidism). Supplemented T3 is much better absorbed through the gut than the T4 alternative (95% compared to 50% to 75%) and the “time to peak therapeutic effect” is much faster for T3 than for T4 (48 to 72 hours compared to 3 to 4 weeks).
Drugs.com explains that T3 may be preferred over T4, “when a rapid effect or rapidly reversible effect is desired, or when gastrointestinal absorption processes or peripheral conversion of T4 to T3 is impaired.” Regulating T3 dosage is more difficult, however, because of its potency, and “rapid onset of action may also produce adverse cardiac effects as a result of abrupt changes in metabolic demands” (Drugs.com). To mediate these effects somewhat, compounding pharmacies can produce “sustained-release” or “time-released” T3, which releases the hormone more slowly into the blood.
Context
The use of pure T3 as part of treatments of CFS/ME and FMS is a very contentious topic for three reasons:
Firstly, the role of “low thyroid hormone function” – i.e. cells not getting enough T3 – as an essential mechanism in CFS/ME and FMS is not widely accepted by the medical community. Indeed, only a fraction of practitioners assert that low thyroid hormone function at the cellular level plays a key role in understanding CFS/ME and FMS.
They point to the parallels between symptoms of hypothyroidism and CFS/ME and FMS, including: low basal body temperature, fatigue, muscle aches, weakness, slow reflex relaxation phase, etc. (e.g. Lowe and Yellin, 2008). A recent study that found evidence of “severely depressed tissue T3 levels” in CFS patients provides further weight to their argument (Ruiz-Núñez B, et al., 2018).
Secondly, there is also disagreement within the medical community regarding the treatment of patients with thyroid hormones when their TSH, T4 and T3 blood levels are in the “normal” range. Dr Broda Barnes, Dr Jacques Hertoghe and many others who have followed in their footsteps have had success bringing patients with hypothyroid symptoms – but normal thyroid blood levels – back to good health using thyroid hormone supplementation.
Mainstream endocrinological associations, however, maintain that standard thyroid lab tests are sufficient to assess whether a patient would benefit from thyroid therapy, and that patients with normal thyroid blood levels should not be treated with thyroid hormones irrespective of their clinical symptoms.
The many experiences of patients to the contrary has spurred the creation of patient-led advocacy groups / websites includingThyroid Patient Advocacy (UK), Thyroid UK, Stop the Thyroid Madness, Hypothyroid Mom, The Invisible Hypothyroidism, Mary Shomon and ThyroidChange as well as the publication of many books by patients and doctors alike, including the terrific titles “The Great Thyroid Scandal and How to Survive It (2002),” “Tears Behind closed doors: Failure to diagnose a thyroid condition (2002),” “What your Doctor May not tell you about Hypothyroidism (2004),” “Living Well with Hypothyroidism: What Your Doctor Doesn’t Tell You… That You Need to Know (2005)” “Why Do I Still Have Thyroid Symptoms? when My Lab Tests Are Normal (2010),” and “Stop the Thyroid Madness: A Patient Revolution Against Decades of Inferior Treatment (2011),” “Be your own Thyroid Advocate: When you’re sick and tired of being sick and tired (2018).
Finally, there is also disagreement amongst doctors on the relative effectiveness of thyroid medicines that contain T3 – such as natural (desiccated) thyroid (i.e. from pig extract), synthetic mixes of T4/T3, and pure T3 – compared to the now standard pure synthetic T4 (i.e. Levothyroxine). Indeed, the American Thyroid Association and similar endocrinological associations in other countries maintain that T4 is the best choice for treating hypothyroidism, although many doctors have found that their patients respond better to treatments which contain T3.
As further described in the next section, the fact that some patients may have difficulty converting T4 into T3, that supplemented T4 may be converted into RT3 instead of T3, and that the transport of T4 into the cells requires more energy than the transport of T3 – may explain why therapies that contain T3 have often succeeded when T4-only therapies have failed to improve symptoms. The patient advocacy groups and books cited above also denounce the continued insistence on the use of T4 by the medical establishment, counter to practitioners’ experience.
In sum: given these three ongoing disagreements, treatments for CFS/ME and FMS with pure T3 and despite (most often) normal thyroid lab results are therefore particularly controversial.
Yet still some practitioners prescribe pure T3 to treat CFS/ME and FMS – despite the sometimes great risks they may incur for providing a non-standard treatment (including sanctioning by authorities). The approaches of some of these practitioners are described in the next section.
Practitioners and pure T3 treatments
Note: For the purpose of this overview, I have picked out elements in the approaches of the various practitioners which relate to treatment with pure T3; however, their full approaches are wider in scope and more complex. Some of these practitioners (but not all) advise that T3 should be trialed only if treatments containing T4 or natural thyroid prove ineffective.
Moreover, most advise that pure T3 should be trialed only when other complementary treatments are in place, including adrenal support (e.g. in the form of hydrocortisone or adrenal extracts), and when a certain nutrient status is achieved (particularly in respect to iron and vitamin B12 levels). Finally, practitioners also advise that treatments should, of course, be performed under the supervision of knowledgeable physicians.
Dr John Lowe (USA): Supra-physiologic dosages of pure T3 to overcome “thyroid hormone resistance”
In his starkly worded short article entitled “Fibromyalgia – A Medical Mystery Solved” (2007) the late Dr John Lowe unequivocally writes: “the main underlying cause of fibromyalgia […] is too little thyroid hormone regulation of patients’ bodies.” He explains that “resistance” of patients’ cells to thyroid hormone means that these cells “need higher than ‘normal’ amounts of thyroid hormone to maintain normal metabolism.” He and Jackie Yellin explain this further in their technical article: Inadequate Thyroid Hormone Regulation as the Main Mechanism of Fibromyalgia: A Review of the Evidence (2008). Moreover, they describe the mechanisms at work and clinical trials in their gigantic book (1,260 pages!) entitled The Metabolic Treatment of Fibromyalgia (2000). According to Dr Lowe, resistance to T3 can have a number of causes, including mutations in the T3 receptors and T4 to T3 conversion problems.
Based on his team’s clinical trials (see e.g. Lowe et al., 1996), patients who had failed to recover from FMS with other treatments – including T4 and natural thyroid – and had normal thyroid hormone blood levels prior to treatment, recovered with “supra-physiologic” dosages of pure T3 (i.e. higher than physiologic dosages). His patients generally recovered from FMS with a range of 100 to 150 mcg of pure T3 per day. He argues that the fact that these patients are not overstimulated at these high dosages is further evidence that they have a form of thyroid hormone resistance.
The book he wrote with Dr. Gina Honeyman-Lowe, Your Guide to Metabolic Health (2003), describes when T3 should be trialed, how to go about it, and complementary supplements and methods to monitor progress. Many patients start on a “full replacement dose” of pure T3 (i.e. the amount a normal thyroid gland would produce per day: 20 – 30 mcg), but the starting dose depends on the patient’s health status, severity of symptoms, and other factors. Dr Lowe generally prescribed a single daily dose of pure T3 to be increased gradually by 12.5 – 25 mcg at 1 – 2 week intervals, and then more modest increases of 6.25 mcg as the patient appears to approach the “therapeutic window” (Lowe, 2008) – i.e. “a dose at which the patient has no symptoms of overstimulation, and hypothyroid-like symptoms improve or disappear altogether.”
Their methods are also described in the e-b; ook by Hugh Hamilton: Impaired Sensitivity to Thyroid Hormone (Thyroid Hormone Resistance): A Cause of Heart Disease, Cancer, Autoimmune Conditions, Women’s Health Issues, Strokes, Fibromyalgia, Depression and Other Issues (2016).
Dr John Lowe died in 2012; the many patients he helped expressed their gratitude and shared stories of recovery on Stop The Thyroid Madness and other forums.
Dr Gordon Skinner (UK): Treating post-viral CFS with thyroid hormones
The late Dr GRB Skinner was a virologist who authored nearly one hundred journal publications on herpes and other viruses. CFS/ME patients kept getting referred to him by their General Practitioners because of the belief that CFS/ME was initiated and maintained by a chronic virus infection. His insight was that the reason patients don’t recover from an infection is not because the infection becomes chronic, but because the patient becomes hypothyroid as a result of the infection. Dr Sarah Myhill credits Dr. Skinner with pioneering thyroid treatment for post-viral CFS/ME patients.
In his book Diagnosis and Management of Hypothyroidism (2003) Dr Skinner writes that viral infection, food poisoning, childbirth, physical trauma, etc. can be “precipitating causes” for hypothyroidism. He strongly believed that diagnosis of hypothyroidism should be made on clinical grounds (i.e. the patient’s history and physical symptoms) because “a ‘normal’ laboratory test doesn’t say a disease isn’t present.”
Indeed, according to Dr Skinner, the “simple-minded reliance on laboratory tests” – combined with the great diversity of clinical manifestations of hypothyroidism – has unfortunately led to a vast under-diagnosis of the illness. With reference to doctors’ manuals from an era prior to the use of thyroid blood tests (and using his warm Scottish humor), Dr Skinner spends a long chapter of his book describing the clinical features of hypothyroidism – which include lack of whole body stamina, being bed bound, loss of muscle power in arms and legs, inability to chew, cognitive difficulties, “intolerance to all things great and small,” carpal tunnel syndrome, intestinal fermentation (relating to muscle weakness of the intestinal tract), food intolerances, local tenderness in muscles, intolerance to light and other sensory disturbances, etc.
Notably, he debunks the myths that a patient who has lost, rather than gained, weight, or has diarrhea (rather than constipation) or feels hot (rather than cold), cannot be hypothyroid; in fact, that person may very well be hypothyroid.
In terms of treatment, he writes that the type of thyroid “replacement preparation, the dosage and rate of increase of a dosage for a given patient” is “almost an art form.” He used many forms of thyroid hormone, including pure T3. He writes that most patients do better on natural thyroid than T4, and that “the provision of T3 alone does not always do the job” (perhaps because the T2 in natural thyroid plays some as yet unknown important function).
Patients also responded better to thyroid hormone when taking high doses of B-12 vitamin. He found that in most cases, thyroid hormone cured low function of the adrenal glands, but sometimes he accompanied his thyroid treatments with adrenal support to allow the adrenal glands to meet the demand of improved thyroid functions (often 2.5 – 5 mg of prednisolone).
Skinner writes that non-responses to thyroid treatment often occur when prescribed thyroid hormone dosages are too low due to a “preconceived notion of a correct or safe dosage.” He surmised that initial side effects from thyroid treatment, such as palpitations, arose because thyroid receptors may have “atrophied” and the supplemented thyroid hormone gets “backed-up.” This is remedied by reducing the medication for a while and perhaps lowering the rate of increase. He wrote that it may take 1 or 2 years for patients to become well. Amazingly, he describes an international athlete whom he diagnosed with hypothyroidism and hypoadrenalism, who later self-increased his dosage of pure T3 to 400 mcg per day. He calls this self-medication “an ill-advised procedure at these levels,” but points out that “something is happening” that merits further research.
I wish Dr Skinner had entitled his book “Diagnosis and Management of post-viral CFS/ME” – I believe that would have been a more fitting title, and the book would have gotten more attention by the CFS/ME community. The UK General Medical Council opened several hearings against Dr Skinner for his stance on prescribing thyroid hormones. After his death in 2013, many of the patients whom he had helped get their lives back described their recoveries and expressed their thankfulness on healthunlocked.com (UK) and other forums.
Dr E. Denis Wilson (USA): T3 therapy protocol to “reset” impaired T4 to T3 conversion in patients stuck in “conservation mode”
Dr E. Denis Wilson writes that under conditions of severe stress, metabolism can slow down as a coping mechanism. Some patients get stuck in this “conservation mode”, even after the stress has passed, resulting in “debilitating symptoms” that will sound very familiar to CFS/ME and FMS patients. According to Dr Wilson, this “conservation mode” is characterized by low body temperature; he gave it the name “Wilson’s Temperature Syndrome”. He points to parallels in the symptoms of this condition with CFS and FMS, and writes on his website that patients diagnosed with CFS have “responded dramatically well to proper T3 therapy” and “many patients with Fibromyalgia have been completely cured” with his protocol.
Dr Wilson’s explanation for the mechanism at work is that during stress, the enzyme responsible for converting T4 into T3 (i.e. D1 enzyme) is inhibited. Instead, T4 is converted into Reverse T3 (RT3) which is inactive and blocks nuclear membrane thyroid receptors. The increased level of RT3 then further inhibits the conversion of T4 to T3, because the RT3 competes with T4 for the D1 enzyme (note: D1 can also convert RT4 into the inactive T2) causing the body to get stuck in a “vicious cycle of T4 to T3 conversion impairment.” Dr Wilson writes that “clearing out the RT3 from the tissues can serve to reset the system so that it can function normally again.”
To clear out RT3 from the tissues, Dr Wilson uses cycles of T3 supplementation which serve to halt the production of T4 by the thyroid gland (and without T4 no additional RT3 can be produced). Unlike Dr Lowe, Dr Holtorf, Dr Skinner and others, Dr Wilson generally only provides temporary T3 supplementation in order to reset “patients’ thyroid hormone pathways” and avoid later setbacks (which he suggests may be related to nuclear membrane receptors becoming desensitized with too much T3 supplementation). He likens the approach to cranking the starter cord on a lawn-mower.
The basic treatment Wilson provides (effective, he asserts, for 80% of the patients) is a starting dosage of 7.5 mcg “sustained release” T3 every 12 hours (i.e. 15 mcg per day on day 1) increased by an additional 7.5 mcg twice per day every day (i.e. after 10 days, the patient is taking 75 mcg every 12 hours; so 150 mcg per day). After just a few days on the highest dosage (max 90 mcg every 12 hours; so 180 mcg per day), the patient is weaned off T3 by subtracting 7.5 mcg off each dose every 2 or 3 days. The basic cycle, therefore, lasts about 1 month.
Patients monitor their pulse and look for palpitations (and are prescribed a little T4 to steady pulse and palpitations if needed). Wilson also provides adrenal support such as hydrocortisone or herbal supplements. After each cycle, patients measure their body temperature for a few days to determine if it is steady.
Cycles are repeated, and the maximum dosage is adjusted as needed so that the body’s system of T4 to T3 conversion re-establishes itself and the patient feels well again. Unfortunately, the longer the patient has been sick, the more difficult it is to get the natural system to establish itself again. His cycling protocol makes for fascinating reading, and is described in detail in the free e-books on his website. A journal paper from 2006 describes a successful application of the protocol with 11 CFS patients (Friedman, 2006).
The American Thyroid Association released a critical statement in 2005 aiming to debunk Wilson’s protocol (ATA website), but significantly, doesn’t challenge the “reset” mechanism behind his approach. Until recently, you could search the database of doctors that apply the protocol on Dr Wilson’s website, but it has been removed to protect their privacy.
Dr Kent Holtorf (USA): Breaking a cycle of immune, hormone and mitochondrial dysfunction in CFS and Fibromyalgia
- by reducing transportation of thyroid hormone into cells (Holtorf, 2014b),
- by downregulating the enzymes responsible for conversion of T4 to T3 (i.e. D1), and,
- by upregulating the enzymes responsible for conversion of T4 to RT3 (i.e. D3) (Holtorf, 2014a).
The resulting RT3 binds and block the T3 receptors, explaining their “decreased sensitivity” or “increased resistance” to T3. Combined with less T3 production, this leads to slowed metabolism, reduced immune responses, etc. (see also: De Groot, 2015). Critically, Dr Holtorf asserts that supplementation with T4 (including when found as part of natural thyroid) can exacerbate the problem because the T4 will be further converted into more RT3 which will block receptor sites.
Going a step beyond Dr Holtorf’s own writing, it was extremely interesting to me to learn that patients can, in fact, get stuck in a “vicious cycle” in which low thyroid function worsens oxidative stress, and the resulting inflammation in turn further depresses thyroid function at the cellular level (Mancini et al., 2016). The “reciprocal modulating relationship” between the thyroid hormones and the immune response is also further described in recent research, including: Devito et al. 2011; Jara et al. 2017 and Zhang et al. 2018.
Similar to Dr Wilson, Dr Holtorf prefers to use compounded “timed-release T3”, but just once per day. Following in Dr Lowe’s path, Dr Holtorf also advises his patients to build up to supra-physiologic dosages over time (100 mcg or more) based on clinical symptoms and an optimal RT3 to T3 ratio – as measured by blood tests. Dr Kent Holtorf’s approach to treating CFS and FMS further includes enhancing mitochondrial function, balancing other hormones, and treating infections. His approach is also explained by Cort in this article.
More information is available on the website of the National Academy for Hypothyroidism, headed by Dr Holtorf. The Holtorf Medical Group has three locations in the USA offering treatments.
Dr Barry Durrant Peatfield (UK): Treating a “down-regulated” metabolic status
In his excellent book, Your Thyroid and How to Keep It Healthy (2006), Dr Durrant Peatfield explains that in CFS/ME and FMS the “underlying problem is a down-regulation of [a patient’s] metabolic status” that most commonly originates with a viral illness, a major operation or a major life event. In viral cases, he explains, the virus inactivates a key enzyme responsible for producing eicosapentaenoic acid (EPA). Although Dr Durrant Peatfiled doesn’t explain the mechanism, he writes that this inactivation results in tissues unable to “respond properly to thyroid hormones”, in turn affecting adrenal activity.
In sum, many of the presenting symptoms of CFS/ME and FMS are a consequence of “adrenal and thyroid insufficiencies.”
A major insight I gained from Dr Durrant Peatfield’s book was the connection between the thyroid and the adrenals. Indeed, adrenal hormone status impacts T4 to T3 conversion, T3 transport into the cells and also the responsiveness of thyroid hormone receptors in the cells. Unlike Dr Skinner, Dr Durrant Peatfield makes the case that low adrenal function must be dealt with prior to thyroid hormone treatment to avoid overwhelming the body. He writes that “a failure of thyroid [treatment] to restore health may be largely down to adrenal problems.”
A further insight I gained from his book is the posited link between low thyroid function and inflammation via the gut: low thyroid function affects gut motility, leading to gut dysbiosis and fungal/candida overgrowth; this causes leaky gut which results in antigens, pathogens and toxins in the blood. This chain of events results in patients who suffer from inflammatory, auto-immune and allergic diseases.
Regarding treatments for low thyroid function, Dr Durrant Peatfield, like Dr Skinner, generally prefers treatments with natural thyroid, but indicates that “severe cases” may only respond to T3 due to problems in T4 – T3 conversion. He describes starting with 10 mcg of T3 and increasing every 5 days or so by10 mcg based on careful clinical observations (he provides no maximum dosage in his book). With time, he writes, the T4 to T3 conversion problem may subside, and it may be possible to introduce T4 for some patients. He emphasizes the importance of a flexible approach, as long as symptoms are monitored.
He prescribes adrenal glandulars or physiological levels of hydrocortisone ahead of thyroid treatments. Additional elements of his treatment protocol, described in great detail in his book, include balancing other hormones (DHEA, oestrogene and progesterone), eliminating candida, healing the gut, liver detoxification, and improving nutritional status through vitamins, minerals, and EPA (e.g. primrose oils).
Patients are instructed to monitor their progress by taking their waking and evening temperatures. With time as the “whole system revert[s] to normal on treatment” thyroid treatment may become less necessary or unnecessary altogether.
I also think that the title of Dr Durrant Peatfield’s book doesn’t do justice to the wealth of knowledge on metabolic status it contains – and therefore may have largely gone unnoticed by the CFS/ME community. Under pressure from the UK General Medical Council for offering controversial thyroid treatments – and in order to be able to continue to advise patients – Dr Durrant Peatfield voluntarily gave up his medical license in 2001.
Dr Sarah Myhill (UK): Kick-starting CFS/ME recovery with T3
Dr Sarah Myhill’s approach to treating CFS/ME is described in her book Diagnosis and Treatment of Chronic Fatigue Syndrome and Myalgic Encephalitis: It’s Mitochondria, Not Hypochondria. 2nd Edition (2018) and her website. She concentrates less on the thyroid hormone than the practitioners already cited above. Instead, she focuses on restoring the function of mitochondria, including by treating sources of inflammation (i.e. infectious, auto-immune and allergic), particularly those originating in the gut. Yet in her chapter on correcting thyroid and adrenal function, she describes that, based on her experience, “some people only feel better using pure T3”, as opposed to T4 or mixes of T4/T3.
She goes on to relate that, in addition to following a strict ketogenic diet, one of her patients required 180 mcg of T3 to “recover completely from her CFS.” Interestingly, this is the only specific example of complete recovery described in her book.
Dr Myhill’s treatment plan for T3 is a starting dose of 10 mcg split into 3 doses over the course of the day, and increased over time. She refers readers to Paul Robinson’s book for further detail on a trial with T3 (see below).
In addition to the treatment of low thyroid function as described above, Dr Myhill offers the interesting hypothesis that there may be a need to “kick-start” the brain out of “safe mode” into “normal function mode.” She cites Dr John Kaiser: “I believe it is reasonable to imagine very sick mitochondria being stuck in a dysfunctional mode similar to a heart muscle that is fibrillating,” and requiring a “kick-start” to get out of this mode.
In order to affect this “kick-start,” she proposes – as long as all other treatment options are in place – trials of pure T3 (“20 – 60 mcg, possibly more”) or natural thyroid (“1 – 3 grains, possibly more”), or alternatively Ritalin or Provigil. This allusion to “kick-starting” or moving from one metabolic state to another (or from a “vicious” to “virtuous cycle”) echoes the hypothesis of Dr Wilson.
Dr Myhill was also subject to multiple hearings by the UK General Medical Council for prescribing thyroid hormones when blood tests are normal; charges were dropped each time following strong support for her by her patients.
Dr Jacob Teitelbaum (USA): Treating inadequate T4 to T3 conversion and thyroid hormone receptor resistance
Thyroid treatment is arguably not the core of Dr Jacob Teitelbaum’s protocol for treating CFS and FMS, which is based on improving sleep, overcoming hormone deficiencies (including adrenal hormones), treating underlying infections, improving nutrition and “exercise as able” (i.e. SHINE). Yet on his website Vitality 101 with Dr T, he describes hypothalamic dysfunction, Hashimoto’s thyroiditis, as well as “inadequate conversion of T4 to T3” and “receptor resistance” as causes of “underactive thyroid hormone” in CFS and Fibromyalgia.
Dr Teitelbaum usually starts treating patients with a T4/T3 mix. Interestingly, he explicitly writes that he has found Dr Lowe’s approach of high pure T3 dosage “to be helpful in many patients.” Receptor resistance, he writes, “is often resolved in one or two years on the high-dose T3 therapy as the body heals from fibromyalgia and/or chronic fatigue syndrome.”
Paul Robinson (UK): Recovery from CFS with the circadian T3 Method
Paul Robinson describes his recovery from CFS symptoms with pure T3 after being sick for 15 years in his book Recovering with T3: My Journey from Hypothyroidism to Good Health Using the T3 Thyroid Hormone (2011). He was a hypothyroid patient taking T4 medication, but was sleeping 4 to 6 hours during the day and could hardly get up the stairs of his house. Because his thyroid blood lab results were in range, his doctor told him his hypothyroidism was “cured” and he must have CFS/ME. Interestingly, he also had a virulent case of glandular fever (Epstein Barr Virus) many years earlier when he was in his 20s.
He kept researching and found a doctor who would prescribe him T3; he improved greatly at first, but then stagnated. He didn’t feel fully recovered until he discovered that by modulating the timing of his T3 supplementation, he could affect total daily production of cortisol and other adrenal hormones, and cure his “adrenal insufficiencies”. (The hypothalamic-pituitary systems depends on T3 to start production of these hormones. ) He now uses pure T3 without complementary adrenal steroids or extracts, supplementing T3 according to the natural daily production rhythm of T3. Notably, this involves a relatively large T3 dose between 4 and 5 AM.
Robinson dubbed this protocol the “circadian T3 method” (CT3M). This method also works with T4/T3 combinations but does not work well with time-release T3. He also complements his treatment with various supplements and dietary changes. He has taken pure T3 (which he calls “T3-monotheraphy”) for over 20 years.
His own personal dosage is 60 mcg split into 4 doses. He achieved this dosage by going up in small increments of 2.5 – 5 mcg every 3 to 14 days based on observations of the effects.
Dozens of CT3M success stories are posted by patients on Paul Robinson’s website. Note that Dr Sarah Myhill refers her readers to Paul Robinson’s “excellent book” for details on trials with pure T3. I also think if he had entitled his book “Recovering from ME/CFS with T3”, his book would have gotten more attention by the CFS/ME community.
Self-treating patients: Successes and frustrations
The stories of recovery from CFS and FMS with treatments involving pure T3 (and T3 containing thyroid hormone preparations) are circulating through books, articles and patients’ forums. However, because pure T3 treatments are not recognized as a standard treatment for CFS/ME and FMS in any country, and few doctors provide them, many patients have started self-treating with T3 as is evidenced in the conversation on online forums. (c.f. healthunlocked.com, tpauk.com, www.rt3-adrenals.org, Science for ME, etc.).
Patients provide each other with advice on the form of T3 and other thyroid hormones, timing, starting dosage, rate of increase, complementary hormones and supplements, etc. Reading these forums gives a sense of the patients’ frustrations with the lack of a standard protocol and lack of support from doctors to navigate a treatment that is challenging to get right. Initial progress is also often accompanied by setbacks that patients struggle to understand.
A summary of best-practices from patients’ experiences with pure T3 is available on the website Stop The Thyroid Madness. The website also provides testimonies from patients diagnosed with Fibromyalgia and CFS that have recovered after treatment with natural thyroid or pure T3.
Conclusion
Over the past decades, there have been many positive experiences using pure T3 in treating patients diagnosed with CFS/ME and FMS. Generally, successful treatment dosages of pure T3 are much higher than the thyroid glands produce naturally, suggesting either “thyroid resistance” at the cellular level (due to T3 receptors being blocked by RT3, receptor mutations or other reasons), or T4 to T3 conversion problems.
Most practitioners emphasize starting on a low dosage and increasing incrementally based on how the patient feels. Some practitioners advise patients to wean off T3 or introduce T4 (e.g. as part of natural thyroid) once the body is again able to convert T4 into T3, in order to avoid later setbacks. Several practitioners emphasize the importance of providing adrenal supports in tandem to allow the body to cope with an increase in metabolic rate.
I am particularly intrigued by several practitioners’ hypothesis that pure T3 supplementation may serve to “kick-start” metabolic pathways (or break vicious cycles), perhaps related to T4 to T3 conversion, interactions between thyroid hormones and the immune system, mitochondrial function, or the brain. In other words, the “kick-start” model posits that thyroid supplementation could be used to break the body from a homeostasis of illness (i.e. an equilibrium state that is maintained by physiological processes) to a homeostasis of health.
However, along with these apparent commonalities, there are also many variations to the pure T3 treatments promoted by doctors and patients. Crucially, it appears that the treatment is quite sensitive: a variance in the type of T3 (i.e. time-release vs. non time-release), time of day, frequency (i.e. number of times per day), starting dosage, maximum dosage, pace of increase, cycling/weaning, complementary adrenal supports, iron status, vitamin B-12 status, etc. could make all the difference in the success or failure of the treatment.
Finally, it appears that the ideal treatment mode depends on the individual, and some patients do better on combinations of T3 and T4. This makes me wonder if perhaps CFS/ME and FMS patients who have tried T3, but for whom it has not had a positive impact, have simply not taken it according to a mode suitable for them.
In the absence of a standard protocol, patients are discussing these treatment variations in online forums. Whereas a lot of valuable information is shared, it is done in an ad-hoc and unstructured way. Moreover, I believe this information is often not accessed by CFS/ME and FMS patients because it is labeled as treatment for hypothyroidism (which they have been told they don’t have on account of normal laboratory blood results).
A comprehensive and structured place for the collection of experiences with pure T3 (and other thyroid hormone treatments) in the context of the CFS/ME and FMS community would arguably be of immense value for advancing the treatment of patients diagnosed with CFS/ME and FMS.
The Low T3 Series on Health RIsing
- The Atypical Thyroid Issues in Chronic Fatigue Syndrome (ME/CFS), Plus a New Thyroid Subset?
- Pure T3 Thyroid and Stories of Recovery from Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia: An Overview.
- The Relevance of Research on Critical Illnesses for Chronic Fatigue Syndrome ME/CFS: A vicious cycle between cytokines, oxidative stress and thyroid hormones
Table: CFS/ME Practitioners and key features of their T3 treatment
| Practitioner | Key features of the treatment | Mechanisms addressed |
| Dr John Lowe | – Supra-physiologic dosage (100 – 150 mcg of T3 per day)
– Single dose in the morning – Pure T3 (not time-release) – Starting dosage depends on health status, severity of symptoms, etc. Most patients start with “full replacement dose.” – Pace of increase is 12.5 – 25 mcg of T3 every 1 to 2 weeks. More modest increases (6.25 mcg) as patient appears to approach effective dosage. – Complementary supplements |
– Cellular “resistance” to T3 (e.g. T3 receptor mutation)
– Problems in conversion of T4 to T3 |
| Dr Gordon Skinner | – Emphasis on clinical diagnosis (not blood tests)
– Used all thyroid hormone preparations (T4, T3 and natural thyroid) – However, little detail in his book on pure T3; describes cases of T4 and natural thyroid – Sometimes provided adrenal support (prednisolone) |
– Post-viral CFS/ME leading to hypothyroidism
– Problems in conversion of T4 to T3 |
| Dr E. Denis Wilson | – “Wilson T3 Protocol”
– Uses “sustained-release T3” – Supra-physiologic dosage (up to 90 mcg twice per day; i.e. 180 mcg total per day) – Most patients start at 7.5 mcg every 12 hours and increase by an additional 7.5 mcg twice per day every day (i.e. after 10 days the patient is taking 75 mcg every 12 hours = 150 mcg per day) – After reaching the peak dose, patients wean off T3 by subtracting 7.5 mcg at each dose every 2 or 3 days – Cycle is repeated as necessary until temperature is stable and patients feel well |
– Patients being “stuck” in the conversion of T4 to RT3 following a stressor |
| Dr Kent Holtorf | – Uses time-released T3
– Supra-physiologic dosage (> 100 mcg) |
– Problems in conversion of T4 to T3
– T3 receptors being blocked by RT3 |
| Dr Barry Durrant Peatfield | – Uses natural thyroid or T3
– Emphasis on adrenal supports for thyroid treatment to work – Nutritional support and treating the gut |
– T4 to T3 Conversion block
– T3 receptor uptake resistance – Adrenal insufficiencies |
| Dr Sarah Myhill | – Correcting thyroid hormone levels, but no preference for pure T3
– Yet recognizes that some patients only feel well on pure T3 at supra-physiologic dosage (e.g. 180 mcg). – Always in combination with other treatments – Starting dosage of 10 mcg split into three doses across the day. – Refers to Paul Robinson’s book for further detail on trial with T3 – In addition: Use T3 to kick-start the brain out of “safe mode” into “normal function” mode (20 – 60 mcg of T3, possibly more) |
– T3 receptors being blocked by RT3
– Brain perceptions of imbalances in the energy equation |
| Dr Jacob Teitelbaum | – Usually starts patients on T4/T3 mix
– Has found Dr Lowe’s approach to be helpful in many patients – 1 or 2 years high dose T3 therapy to treat receptor resistance |
– Problems in conversion of T4 to T3
– T3 receptors resistance |
| Paul Robinson | – “Circadian T3 Method” – early morning dosage is key to power-up the adrenals
– T3 or T3/T4 mix – Not “time-release” – Increases / decreased in 2.5 – 5 mcg every 3 to 14 days to find optimal dosage. Slowing when close to final T3 dosage |
– Problems in conversion of T4 to T3
– Adrenal insufficiencies |
References
Broda Barnes and Lawrence Galton, 1976. Hypothyroidism: The Unsuspected Illness. (Book)
Kenneth Blanchard, 2012. Functional Approach to Hypothyroidism: Bridging Traditional and Alternative Treatment Approaches for Total Patient Wellness. (Book)
Benoît Claeys, 2015. En finir avec l’hypothyroïdie: Ce que votre médecin ne vous dit et que vous devez savoir (Book)
Leslie J DeGroot, 2015. The Non-Thyroidal Illness Syndrome. Endotext
De Vito, Paolo & Incerpi, Sandra & Pedersen, Jens & Luly, Paolo & B Davis, Faith & J Davis, Paul. (2011). Thyroid Hormones as Modulators of Immune Activities at the Cellular Level. Thyroid: official journal of the American Thyroid Association. 21. 879-90.
Barry Durrant Peatfield, 2006. Your Thyroid and How to Keep It Healthy. (Book)
Friedman M, Miranda-Massari JR, Gonzalez MJ. 2006 Supraphysiological cyclic dosing of sustained release T3 in order to reset low basal body temperature. Puerto Rico Health Science Journal. 25(1):23-9
Hugh Hamilton, 2016. Impaired Sensitivity to Thyroid Hormone (Thyroid Hormone Resistance): A Cause of Heart Disease, Cancer, Autoimmune Conditions, Women’s Health Issues, Strokes, Fibromyalgia, Depression and Other Issues. (Book)
Kent Holtorf, 2014. Peripheral Thyroid Hormone Conversion and Its Impact on TSH and Metabolic Activity. Journal of Restorative Medicine 2014; 3
Kent Holtorf, 2014. Thyroid Hormone Transport into Cellular Tissue. Journal of Restorative Medicine 2014; 3
Jara EL, Muñoz-Durango N, Llanos C, Fardella C, González PA, Bueno SM, Kalergis AM, Riedel CA. 2017. Modulating the function of the immune system by thyroid hormones and thyrotropin. Immunol Lett. 2017 Apr;184:76-83.
John C. Lowe, MA, DC, Richard L. Garrison, MD, Alan J. Reichman, MD, Jackie Yellin, BA, Mervianna Thompson, RN, MSN, APN, Daniel Kaufman, MD, 1997. Effectiveness and safety of T3 (triiodothyronine) therapy for euthyroid fibromyalgia: a double-blind placebo-controlled response-driven crossover study: Clinical Bulletin of Myofascial Therapy, 2(2/3):31-58.
John Lowe, 2000. The Metabolic Treatment of Fibromyalgia. (Book)
John Lowe and Gina Honeyman-Lower, 2003. Your Guide to Metabolic Health. (Book)
John Lowe, 2007. Fibromyalgia – A Medical Mystery Solved. Thyroid UK Website.
John Lowe and Jackie Yellin, 2008. Inadequate Thyroid Hormone Regulation as the Main Mechanism of Fibromyalgia: A Review of the Evidence. Thyroid Science 3(6): R1-14
Sarah Myhill, 2018. Diagnosis and Treatment of Chronic Fatigue Syndrome and Myalgic Encephalitis It’s Mitochondria, Not Hypochondria. , 2nd ed.: (Book)
Antonio Mancini, Chantal Di Segni, Sebastiano Raimondo, Giulio Olivieri, Andrea Silvestrini, Elisabetta Meucci, and Diego Currò, 2016. Thyroid Hormones, Oxidative Stress, and Inflammation. Mediators of Inflammation.
Ruiz-Núñez B, Tarasse R, Vogelaar EF, Janneke Dijck-Brouwer DA, Muskiet FAJ., 2018. Higher Prevalence of “Low T3 Syndrome” in Patients With Chronic Fatigue Syndrome: A Case-Control Study. Frontiers in Endocrinology (Lausanne).
Gordon Skinner, 2003. Diagnosis and Management of Hypothyroidism. (Book)
- Denis Wilson, 1996. Wilson’s Temperature Syndrome: A Reversible Low Temperature Problem. (Book)
Jingping Zhang, Jingjing Huang, Kasimujiang Aximujiang, Chenbo Xu, Abulaiti Ahemaiti, Guixia Wu, Li Zhong & Kurexi Yunusi. 2018. Thyroid Dysfunction, Neurological Disorder and Immunosuppression as the Consequences of Long-term Combined Stress. Scientific Reports volume 8, Article number: 4552
Websites – Practitioners
- Vitality 101 with Dr T (Dr Jacob Teitelbaum)
- Recovering with T3 (Paul Robinson).
- Wilsons’ Temperature Syndrome (Dr E. Denis Wilson)
- Dr Sarah Myhill
- The National Academy of Hypothyroidism
- Dr Malcom Kendrick (UK)
- Dr David Borenstein (USA)
- Dr Rind (USA)
- Dr Simone Koch (Germany)






My doctor just recently started me on T3 because blood work came back indicating T3 was well below normal. Not to help CFS but end result is T3 has helped me equivalent to D.ribose and NAC . I now have 4 hours of activity a day which is great. I so believe there is a connection between T3, CFS, and most importantly is all tied together with gut.. man, my hope is magically, it will all get tied together. I know there are a lot of great folks trying, and I am so thankful.
Good to hear Hollie. Thanks for sharing that and congrats on your progress.
Hi Dominic. I’m Edith Bouvier, the one that shared my experiences with FMS.on Health Rising, 17 YEARS UNDER THE CARE OF A NATUROPATH DOCTOR FOR FIBROMYALGIA, part 1&2.
First let me say that the love & compassion you have for your wife has touched us all very deeply. God bless you for the research you do to help improve her quality of life and also,in sharing that important information with all of us who suffer from these 2 very complicated illnesses.
I still suffer from FMS despite all the excellent care I receive from my truly amazing Naturopath Doctor. He has me well stabilized though, but I still suffer the odd set back, mainly due to new food allergies. Once I eliminate that particular food, or get treated by NAET, I resume a fairly normal life, although not cured. It is so important also when you have ME/CFS/FM to recover deep restorative sleep, otherwise it’s hard to move forward with any other treatments. I still have those sleepless nights and wake up all washed out! I have to be so careful what I eat the day before.
T3 treatment was of extreme benefit in restoring a lot of my energy. I did have another incident of my T3 dropping again and my ND told me he could not get the T3 again in Canada because of some new regulation. He did put me on another supplement that has really helped, but, I need to take it every day. The product is BMR by NaturPharma. I take 3 a day, 1, one hour after breakfast & in the evening and the third half way through the night. My ND. had me start with 1 and go up. It was easy to know when I took too much, as I felt labored, so, 3 works well for me. I can purchase this product from my ND, but I also found it on line in Canada at http://www.smithpharmacy.com.
I see that Dr. Jacob Teitelbaum’s website, http://www.endfatigue.com has a similar product as well.
After 24 years now of FMS, and almost rock bottom T3, my MD. still doesn’t believe I have a problem because my TSH is normal! Thank God for my ND!
Thanks again Dominic for sharing your research with all of us. Please let us know how your wife is doing. Blessings to you both. Edith
Thank you Edith for your kind words! I looked up the BMR by NaturPharma that your ND has advised. As far as I understand it contains bovine thyroid gland extract. (I wonder what the T3 / T4 ratio is there). On glandular extracts I found this page interesting. Dr James Wilson. Best wishes! Dominic
I had low T3 and elevated rT3 (and likely still do) and I did the T3 therapy years ago now. The T3 corrected both my T3 and rT3 levels but it had absolutely no impact on my symptoms at all.
I wonder if this is a case where the T3 may have been kind of foundational; ie your body really needs it but it needs so much more.
i admit i didnt read the whole article as its a long one, but diet makes a huge difference here as well!! a good place to read up on other approaches to this is ForeFront Health, he truly has a way of explaining the diet connection of hypothyroidism, you cant just take a pill and expect it to work if there are underlying dietary issues, like eating a diet high in polyunsaturated fats….which is one fat that can interfere with your bodies ability to convert T4 to T3, this fat is pushed as the healthy fat and its very far from that. as you pointed out , the T3 treatment may have changed the results of your bloodwork but it did nothing to relieve your symptoms, don’t give up! but also don’t expect a Dr to give you all the answers, i also didnt see any mention of high estrogen here, which in a blood test wont give you the amount of estrogen stored in your body, just whats in your blood in that one moment, estrogen blocks your bodies ability to convert T4 to T3 as well, look into Dr Broda Barns and Dr Ray Peat for more info on that. Don’t give up! i was spending most of my day on the couch and had to plan my day around one simple task only a few yrs ago,today i am not perfect but i can definitley say i dont spend my days thinking of my next nap and i enjoy a much higher level of energy….and an endocronologist tried to treat me for CFS with antidepressants!!
Thank you for the tip Troy, also on the importance of diet. Brings to mind that many of the practitioners cited above stress the importance of nutritional status. I am glad to hear you are better. Best wishes!
I would.love to know the route you chose to improve?!. Congrats by the way.
Diagnosed with Hashimoto (autoimmune hypothyroidism) a few years after post viral cfs onset.
Treated with both t4 and t3 (because t3 stayed low even when t4 was back to normal).
Only slight improvement, still housebound. T3 did mainly improve brain fog significantly.
TSH was only mildly elevated (borderline normal!), Anti TPO really high, but that’s usually not tested first.
(I’d say test TSH, FT3, FT4 and antiTPO to see if anything off with thyroid. Treatment in my experience does not result in a huge improvement energy-wise though. Extra hypothyroidism fatigue on top of the CFS exhaustion apparently doesn’t
really register :))
Thank you for sharing, Kate!
I’m glad to hear T3 has helped you, albeit only a bit. Are you getting good advice for complementary adrenal supports, vitamins, timing, dosages, etc? I think that’s the challenge for many patients.
Best wishes and courage!
Dom
No, I’m not. No advise other than “take the T4 in the morning half an hour before breakfast”. I figured I’d spread the dosages and I’m taking the T3 about half and hour before sleep.
Where can I read more about the complementary adrenal support/vitamin/minerals/timing/dosage?
Thank you!
Dear Kate, I really recommend looking at the websites of the “Patient advocates” listed at the end of the blog post: RT3-adrenals, Stop The Thyroid Madness, Thyroid Patient Advocacy UK, etc. I learnt a lot from them. And also the books — perhaps starting with Dr Durant Peatfield? Best wishes! Dominic
You really need to see where you stand with reverse T3, too. If your free T3 levels are still low & your T4 are normal, than it’s very likely that your body is converting the T4 into reverse T3, not into free T3. And, if that’s the case, giving it more T4 is only going to make the problem stay as bad or get worse. Also, taking the T3 in the morning, and/or splitting into multiple doses during the day can make a big difference.
And, the formulation of the T3 can make a big difference. You may need to try different ones. A lot of thyroid treatment is experimenting to get your individual dose, type, & time(s) of the day for taking it rt.
Could it be you need more T3 – you didn’t mention your dose.
Fascinating article. Well done to bring all that information into one place. I’ll post about it on Thyroid Uk forum so it receives a wider audience.
I take 50mcg of Tiromel, split into 2 doses, daily. I started with Paul Robinson’s excellent book.
I worked my way up to this dose very slowly. Many symptoms have resolved although some remain, though reduced,especially muscle pain. However I have suffered for decades with symptoms so I think there may be a residual tendon problem which is very hard to cure.
I think I still need to improve my vitamin levels, increase adrenal support and review the timing of my doses. Reading through has reminded me of all the salient points.
Note to Cort, the email link isn’t working. I had to come to the website to access this article. Many thanks indeed for this important overview.
Thank you!
I’m glad to hear Timorel T3 has helped you. Yes, from what I read complementary adrenal support & vitamins, as well as the timing & dosages of T3 are factors in the treatment being successful or not. Tricky!
And thanks for posting on Thyroid UK.
Best wishes!
Dom
Thanks Edward. Another ME/CFS moment (of many)..I just sent another email blast.
It does seem that these issues should be addressed in a package as Dominic notes. Here’s something from the RT3 Adrenals site
“If you are visiting this site, you have begun to address issues related to low thyroid and the things that impact its treatment. These include, most frequently, low or high cortisol, low iron and electrolyte or sex hormone imbalance. The information you will find here is an overview of the challenges you are facing and what the experiences of thousands of patients have demonstrated.”
I was taking tiromel twice daily and didn’t have much success. When I split the doses into every 3 hours (6 times a day) my temp normalized! Dr. Denis Wilson mentions this protocol must be done to the minute if not using time release T3.
Originally, due to an rT3 of 500, I was started on 50mcg T3. It was raised to 100mcg a day as I went through cancer treatment pre-ME/CFS, then lowered to 75mcg.
My TSH has been .001-.06, done a decided to try adding T4 and dropping T3 to a lower dose. I’m currently on 137mcg T4 and 62mcg T3. FT3 and FT4 are midrange and TSH is .006. I also take 20mg “replacement dose” hydrocortisone, DHEA and pregnenolone.
All of this has helped me function, but it’s not a cure for ME/CFS.
I also have high anti-thyroglobulin antibodies, which haven’t changed with changing my diet (anti-inflammatory Paleo), and taking iodine and am selenium. I did develop a 2cm thyroid nodule, which was benign.
I’m not sure what to think. The last conventional endo I saw freaked at my suppressed TSH and wanted me on 112mcg of T4 only which I couldn’t function on.
Before my biopsy, I did some resesrch and found that both EBV and HHV6 have been implicated in thyroid cancer. I’ve had both, so it’s a little worrisome.
There’s also the genetic component. Through Enlis, I was able go examine all my thyroid genes and found I have a plethora of rare SNPs and mutations on about 14 thyroid snd thyroid cancer related genes.
I think there’s a lot more to this than folloeinh any of the theories above and that thyroid treatment should be highly individualized.
The Ruiz-Núñez 2018 paper mentioned in this interesting article found that around 16% of ME/CFS patients (about 1 in 6 patients) suffer from a subclinical hypothyroidism syndrome they call “low T3 syndrome”, where triiodothyronine (T3) is low even though TSH is normal. 1 in 6 patients is a high prevalence.
This low T3 syndrome represents a subclinical hypothyroidism, which may exacerbate ME/CFS symptoms, but may not be detected by regular thyroid hormone testing, which usually only checks TSH and thyroxine (T4). So you really need a more comprehensive thyroid hormone test that includes T3.
The authors suggest that these 1 in 6 patients may benefit from T3 and iodide supplements (though they say this needs to be confirmed in trials).
I mention this, because its likely that taking T3 (in the form of the drug liothyronine) probably will not help most ME/CFS patients, but will very valuable for those 16% of patients with low T3 syndrome.
I have some confusion about this because Holtorf “seems” to use compounded T3 quite a bit. I actually don’t know how much he uses it but since he mentions it in the context of ME/CFS and FM my guess is that he does. It would be really good to get clear on that. He may have less restrictive criteria. I will try and find out.
Here’s when Holtorf recommends it:
Among patients with this type of thyroid hormone transport dysfunction (resulting in intracellular hypothyroidism) assessing the free T3/reverse T3 ratio can aid in a proper diagnosis, with a free T3/reverse T3 ratio of less than 0.2 being a marker for tissue hypothyroidism (when the free T3 is expressed in pg/mL (2.3–4.2 pg/mL) and the reverse T3 is expressed in ng/dL (8–25 ng/dL))
https://restorativemedicine.org/journal/thyroid-hormone-transport-into-cellular-tissue/
Hi Hip, I also want to jump in here just to make sure we understand Ruiz-Núñez et al. the same way:
Ruiz-Núñez 2018 writes that T3 “below the reference range” was more common in CFS patients (16 out of 98 persons). So, as you say: it is important to do the T3 blood tests.
But Ruiz-Núñez goes beyond this and writes that the CFS patients as a group had higher RT3 and RT3/TT3 ratios. Here she is no longer writing about just the 16 patients.
And Dr Holtorf’s point is that T3 supplementation will not only help the patients with low T3 levels (i.e. the 16 patients), but patients with too high RT3/T3 ratios (i.e. the whole CFS group – or rather those that have Free T3 / RT3 ratio of less than 0.2 when Free T3 is expressed I pg/mL and RT3 in ng/dL).
I reached out to Dr. Holtorf. He stated with regard to T3:
We see a good number of patients improve and with such a small amount of side effects. it is just one part of our multi system treatment program, but, no doubt, a key part. You can do everything else right, but if you don’t fix the thyroid, the patient is much less likely to respond positively.
More to this: Dr Holtorf’s colleague Dr Karen Bullington wrote: “Almost every single ME/CFS and FM patient I’m treating is on compounded T3SR capsules. Probably 90%.” [T3SR = T3 Slow Release]
I tried the Wilson Syndrome treatment 20 years ago. Titrating T3 up to try to bring up body temperature. I never could bring up my body temp. And it increased tachycardia significantly. (This was before my HyperPOTS DX.) It made me really nervous. Around the same time we also supported my adrenals with Cortef. Neither of this helped and it may have hurt. I tend to have Hyperthyroid rather than Hypo. Yet there is a T3 conversion issue. But this protocol was a bust for me. Yet my normal body temperature is between 95.6 and 96.0.
Issie
Dear Issie.
Thank you for sharing. What comes to mind in your description is that Dr Durant Peatfield writes critically about Wilson’s Protocol in his book (“I am far from convinced that his approach brings any useful advantages…”). He warns against high doses causing hyperthyroid side effects. Just to say, the practitioners described above that use T3 use it in many different ways. Unfortunately the patients are left with divergent advice that we have a hard timing making sense of! I tried to present the different practitioners’ approaches…
Hi Issie, my daughter had very low body temp for a very long time. In fact…’exercise’ made her heart rate drop and her temp drop. We speculatively took her for acupuncture….one visit. Her temp went back to normal that day. I must have taken her temp 20 times over the next week or so…out of pure ‘disbelief’.
Further treatments did not help with any other symptoms but to this day…it’s difficult to believe that we got such an immediate and permanent result.
Keep looking for answers.
Interesting. Wonder what that did? Maybe unblocked meridian and caused the electrical system to not malfunction. Since I have POTS, this is an issue.
Issie
Hi Issie,
Dr Alan Christianson has done a long video on the use of T3. Has some interesting views about the usefulness of T3 in the face of elevated rT3. And or suppressed TSH. AND Wilson’s protocol.
I suffered from q-fever fatique Syndrome, a disease Causes by the coxiella burnetii bacteria, quote simulator to me/CFs in my case except POTS. While a echo Thyroid Cancer was Discovered and to cut that story short, my Thyroid was removed in 2 Operations. Between the 1st and second Operation I got severely hypo Thyroid, the left behind half of my Thyroid didn’t functioneren at all. Because of the Quick effect of T3, I was treated with 50mcg of T3 instantly. My life changed completely in over a week. Before I was unable to come home after doing groceries and emotionally in stable, after I was able to get home after groceries easily and became emotionally calm and stable as is was Earl ier in my life. Since that time I am looking for reverse evidence, a way in which I can Provence that T3 should be considered as a treatment option for QFS, ME or CFS. In my country, the Netherlands, there is no doctor to be found that dares to experiment with t3 on a patiënt. Scientific research would cost 500.000 euro’s for this. I can only dream for my fellow patiënts that they Will get the opportunity to try if t3 can cure them <3. Thank you for your thorough research, I Hope you can help your wife soon!
Thank you Sientje for your encouraging words! I’m glad to hear you had a positive experience with T3. Best wishes!
And about my terrible experiences with T3, I was taking minuscule doses, like 1 mcg or a fraction of that amount and always got bad side effects.
For a long time I’ve wondered why I don’t make enough T3. Then I read that people who suffer from mold biotoxin illness (CIRS) can have difficulty converting T4 to T3. I’m hoping that as I get more and more clear of mold biotoxins, I’ll be able to make my own T3
Hi Rachel. A connection between CIRS / mold biotin illness -and- low T3 is really interesting. I want to read up on that! Regarding your experience of not being able to tolerate T3 — from what I’ve read that is very common and (speaking in general) is sometimes due to adrenal support & nutritional status not being in place (see the patient sites: RT3-adrenals, Stop The Thyroid Madness, Thyroid Patient Advocacy UK, etc). Best wishes!
I too was dx with mold/biotoxinillness & CIRS. And after years of suffering just received my dx of hypo thyroidism. I had chronic thyroiditis ( and two nodules to right side) and my dr is actually an endo and never started me on anything until the ER drs suggested a treatment for me after so many visits with heart issues. I just started 50mcgs of l-thyroxine but am having headaches and visual disturbances so i am experimenting with skipping a day after two. I do notice a difference in my muscle weakness and small fiber neuropathy. I pushed for more blood tests and also had a scan of my thyroid today so will find out further results next week. I hope I can advocate for t3 if needed as my cfs/me is real and i have a traditional endo (very old school.)
Glutathione/NAC can help with t3 by reducing inflammation which harms conversion of t4 to t3
Wondering if anyone has experience with micro-dosing T3, as Dr. Ken Blanchard recommends. Just learned about it and him when re-researching thyroid.
Article on and info about Blanchard & his microdosing T3:
https://www.chronicfatiguediagnosis.com/2018/05/31/1418/
Thanks for the link! I am going to add a paragraph on Dr Ken Blanchard’s approach in the blog post. Very relevant. Best wishes, Dominic
Another factor in thyroid treatment is that the fillers in various thyroid meds can also make a huge difference…..some can cause bad reactions, & can even block/counter the effects of the meds, esp in those who are chemically sensitive (which many of us are) & one filler that is commonly used in the sustained release T3 in particular actually prevents it from being absorbed well at all…..can’t remember specifically which fillers can be problematic, but I know that has been shown to be a big factor in many patients & is another reason why treating can be a process of experimenting to find what works for you.
I saw a endocrinologist, he wants me to have this test.
Interesting article about T4 vs T3! The following adds T2 and T1 into the mix as potential therapeutic agents: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6060242/
Thank you for sharing, Moira. This is a really interesting article! I understand that the T2 hormones (of which there are 3 types!) are then created from T3 or RT3 by the D1 and D2 enzymes. But the affinity of thyroid receptors to them differs… I have to study this some more. Thanks!
Hello Dominic,
Thank you for all the work you did and sharing the information with us.
Did you read about anyone who used 7- keto- DHEA, (a steroid produced by metabolism of the pro hormone DHEA) ?
It does not affect the thyroid parameters much (in healthy men )¨
“treatment of 7-oxo- dehydroepiandrosterone or 7 – keto DHEA affects the thyroid parameters only temporarily and it provides a considerable persistent amount of 7β-hydroxy- DHEA “ R. HAMPL, J. ŠULCOVÁ, R. BÍLEK, M. HILL Physiol. Res. 55: 49-54, 2006 How Short-term Transdermal Treatment of Men with 7-oxo- dehydroepiandrosterone Influences Thyroid Function
But maybe enough free T3 is not the whole story.
“experimental evidence has been reported that this steroid is a potent thermogenic agent and it could reverse the effect of thyroid hormone removal on thermogenesis (Bobyleva et al. 1997). It was even suggested for prevention of Raynaud ́s attacks (abnormal digital vasoconstriction in response to cold) (Ihler and Chami-Stemman 2003).” See ref in the article above.
I was treated for a (benign ) tumor in the thyroid with T4 supplementation some 30 years ago. Allthoug my blood values of TSH,free T4 and T3 were normal I became quite ill,:fatigue, cold feet, low early morning temperature and very painful muscles in my feet , lower legs and upper quadrant (diagnosis fibromyalgia) Later on I developed a goiter and my thyroid was removed.
I first remained on Synthroid ,but luckily I found an endocrinologist who prescribed armour thyroid (pigs) and also tried to normalize other hormones ;oestrogen,progesteron,DHEA, pregnenolone..
I stopped early on with the DHEA because of hair loss . That is why I want to try 7- keto- DHEA
I feel much better now ; less fatigue, normal temperature in the morning, no cold feet etcet but I still have the typical muscle pain with trigger points of FM. Maybe 7- keto will have some effect? Who knows?
This is an excellent article. Maybe the best I’ve read on CFS/ME and thyroid. I had a great CFS doctor in Texas who put me on a high dose of compounded T-3 and it improved my CFS significantly. Unfortunately, I moved to another state and have been unable to find a doctor willing to prescribe T-3 at higher levels. My current endocrinologist refused to even discuss the possibility with me. She explained that since she had her medical degree from Harvard and had read virtually everything on thyroid disease and treatment that she did not see the need to discuss any other types of treatment! I will be looking for another physician and taking this article with me. Thanks for the information.
Thank you Melissa for your positive comment! 🙂 Best wishes for your recovery!
Any chance you could provide that TX doctor’s info?
Thanks Cort. Name of t3 in Turkey is tiromel not timorel. Best wishes.
Thank you Dominic and Cort. Yes, I read years ago that Epstein Barr Virus can cause Thyroiditis. This was 1986 when my son was so sick following well documented EBV.
Years later I connected with a woman who had a very long, redundant colon. She had lots of abdominal pain and symptoms. She had also been diagnosed with hypothyroidism. Following colon surgery, her thyroid normalized and she no longer needed thyroid meds. Just Some anecdotal info. Thanks, again.
Thank you Merida. Yes, I think you are touching on this “reciprocal modulation relationship” between immune system (incl. sub-plots of cytokines, natural killer cells, mold biotoxins, gut inflammation…) and the function of the thyroid hormone (incl. sub-plots of conversion by enzymes into T3, T2, T1 and RT3, transport into cells, membrane receptor uptake, etc. in turn mediated by cortisol and other adrenal hormones). I really want to bring information together on this topic for a next blog post.
I’ve just seen this, a few days late, and must print it and take time to read through in segments over several days. I’m severe ME/CFS, being on here is difficult cognitively and sensorywise. I want to catch at least a few of you before comments are finished, and ask for some direction as to which part of the post I should look at, or another post, or just get your understanding of the issue we have: My 33 year old daughter and I both have ME/CFS. She had some success with T3, pure, after reduced from 7 mcg to 3.25mcg several years ago. Dr retired, and she relapsed, and was off it for three years, gained much weight too. When she was strong enough to see a new dr he started her back on 3.25 mcg T3. She reacted as she had initially with the 7 mcg dose, with severe hormonal mood shifts and could not tolerate it at all. What happened? She has mild Hashimoto’s, but all her bloodwork related to thyroid come back fairly normal. She has had PMDD (Premenstrual Dysphoric Disorder), and has PTSD as well. Anyone who understands this better than us, please feel free to make suggestions or share ideas! Thank you!!
Dear Denise, I’m sorry to hear how hard it is for you and your daughter! From what I have read, being able to tolerate treatments with T3 depends on getting cortisol levels right and then making sure iron and B-12 levels are fine. Dosage and rate of increase also seem to matter. But I can not give advice and don’t know enough. However, I think the websites Stop The Thyroid Madness (see page “NDT or T3 doesn’t work for me”) and RT3-Adrenals do a really good job explaining what is needed for NDT and T3 treatments to work based on patients’ experiences. They also have dedicated forums for posting questions / getting advice. Sites in the United Kingdom with forums are Thyroid UK and Thyroid Patient Advocacy UK . Wishing you courage! Dominic
Thank you so much, Dominic!
Many thanks for taking the time to put this together. A great starting point for researching t3 supplementation. I take NDT and at 3.5 grains still have symptoms so am considering adding/switching to a t3 regime under Dr Myhill’s guidance. It is certainly a little disconcerting the number of (somewhat contradictory) approaches but as with everything in Lyme/CFS it is a case of working out what works for you.
After 7/8 years of severe CFS (tested by Dr. Sarah Myhill) I diagnosed myself with a thyroid problem. I started taking NDT but only made a tiny improvement of dreadful symptoms.
Then I tested RT3 and it was high. I sourced T3 from abroad and started cautiously, cutting a 25 mcg pill into 6; taking a crumb, for one week; then 2 crumbs … slowly increasing.
Over the next few months energy gradually increased. I was doing things – housework, walking to a nearby shop, then moving house. It was wonderful to be able to do things again. Even though I had setbacks, they were shorter..
Now I feel I’m back living in the real world again.- not 100% maybe, but I was stuck in the pit-stop for so long, waiting to rejoin the race, I don’t mind going at half speed..
I had a very stressful time recently but recognise it, and know that I needed to cancel all appointments / outings, let things settle, rest, pamper, relax – take a week of recovery time.
I don’t want to fall back over that cliff, it’s a long, long haul back up.
I’ve spent thousands over the years trying to get well. T3 turned the corner for me, and it was the cheapest supplement I took.
I don’t yet know If I’ll need to take it always.
I’ve had no help or recognition of symptoms from any GP. If it wasn’t for on-line communities and help I would still be very ill.
Thank you..
Sandra
Congratulations Sandra and thanks for passing that along 🙂
It just shows that you never know… A very simple thing might help.
Good luck on your continued recovery.
Hello,
Since writing this blog post I came across another relevant article:
Taija Liisa Somppi, 2017. “NonThyroidal Illness Syndrome in Patients Exposed to Indoor Air Dampness Microbiota Treated Successfully with Triiodothyronine.”
The author describes successes in treating 9 patients who had been exposed to mold with pure T3 (or with combinations of T3 and T4).
Best wishes to all!
Dominic
Hi Dominic, has your wife tried T3 and if so did she get any benefit?
How can i print this article for my dr?
There is a print button on the bottom left of the article.
There is an update to Paul Robinson’s website. https://paulrobinsonthyroid.com/success-stories/
Same old story. SOme people improve some people don’t some doctors think ME/CFS is T3 hypothyroidism, some don’t believe it. Same old story. When will we ever know why one day we were normal and our thyroids were normal then the next day wehad acute onset ME/CFS or T3 Hypothyroidism? WHen will we know the answer to this question. Most GPs in ENgland don’t believe ME/CFS is a real disease. Especially since Prof Michael Sharpe’s latest paper with Greco saying CFS is an illness without disease, LOL funny life. I had post viral fatigue syndrome 28 years ago but I seemed to recover suddenly 16 years later. Now I get tremor or electricity through my body when I wake up at night sometimes. Very weird. But no more CFS.
Thanks for writing this article. These advocates and doctors are wonderful – true lifesaving heroes. The thyroid and endocrine societies that condemn these treatments should be ashamed of themselves, even criminally charged!
Beni, insani kalbi ile meme kanseri olan Kızıma Kenevir Yağı ile yardım eden Dr rick’e götüren Yüce Tanrı’ya şükürler olsun. 21 yaşındaki kızımın sağlığına kavuşması ve hayatında herhangi bir engel olmadan istediği her şeyi yapabilmesi için çok minnettarım. Dr Rick, ilacınız kanser, tümör için tek çare ve kalbimin derinliklerinden, içtenlikle en iyisisiniz ve uzun ömürlü olmanız için Tanrı’ya her zaman şükredeceğim, böylece dünyadaki daha birçok insana yardım edebilirsiniz. insanlığa tıbbi hizmetinizle. seninle şimdi kenevir Yağı’nın gerçek ve Doğru olduğuna inanıyorum, kanser ve diğer hastalıklarla ilgili sorunları olan herkes için Dr Rick ile iletişime geçmeli: ,,,,,, vb. ricksimpsoncannabisoil’e e-posta gönderebilirsiniz @ usa.com
Thank you so much for putting this together. I had read about some of these approaches in various sources, but it is so great to seem them in one place to be able to compare them. Your work is really appreciated!
Dear Evan, Thanks for your kind message and I’m very glad the post was useful to you. Best wishes! Dominic
Hello,
Thank you for publishing this. I wish there was a way to get the word out to more doctors to trust their patients. I have been blessed to find doctors who trust me and have been on sustained-release T3/T4 combo therapy for 20 years. Another 10 doctors refused to use it and as a result I could not continue to be in their care. I am astounded by how few endocrynologists are willing to trust their patients over routine blood tests. They would rather have the patient bed-ridden and on death’s doorstep with a “normal” TSH than to have a patient who is fully functional, in optimal health and feeling terrific with a TSH of 0. They ignore the science surrounding: 1) potential allergies to one’s own TSH, 2) pituitary resistance to thyroid hormone, 3) reduced end user sensitivity to thyroid hormone, 4) T3 conversion disorders and reverse T3 syndrome, 5) Sarcoidosis and other pituitary hormone blockers (tumors), 6) auto-immune diseases and post-viral syndromes that could cause a patient to feel sick until the TSH is near 0, and 7) food allergies and other allergies that interfere with thyroid function. Luckily, I found doctors who use the Free T3, Free T4 and Reverse T3 tests to guide my treatment and trust that I know based on symptoms when I am over and under-medicated.
Over-medicated thyroid patents get heart palpitations, hair loss, diahreah, nervousness, shortness of breath, menstrual irregularities, eye problems, shaking and a host of other conditions that tell the when they are overmedicated. Perhaps if they don’t have these symptoms they aren’t as overmedicated as doctors believe based on the TSH blood test.
Similarly, extreme fatigue, myalgias, feeling cold all the time, blue hands and feet, hair loss, constipation, sore throats, weight gain, brain fog, body temperature under 98 degrees and other symptoms are good indicators that we are undermedicated even if our TSH is normal. Doctors need to trust us when we say something isn’t right.
Hashimotos and other autoimmune thyroid disorders are a balancing act of adjusting up and down medication periodically (for me it is twice a year as the seasons change winter and summer). As the patient living in this body, I want a doctor who trusts me to know what over-medicated and under-medicated feels like. Luckily I almost never experience either one, as we know when the seasons change and it’s time to adjust. We are always ahead of it based on my symptoms becauaae the symptoms arrive before the blood work reflects the need for a change. Why should the patient have to become miserable for weeks with symptoms and wait for the blood work to finally indicate what the patient knew all along?
I am so blessed to have found doctors who do not fear T3 or a super low TSH in the absence of any other negative symptoms. As a result I have been able to live a normal, successful, happy, healthy life. To all the doctors I visited who were so closed-minded they couldn’t treat me outside the TSH box, please update your training. You are leaving your patients to suffer and in many cases to self-medicate with drugs they purchase online. At the very least, please consider a therapeutic trial of sustained-released T3 combo therapy since the New England Journal of Medicine has shown patient’s report feeling better on combo therapy.
Dear Amora, Thank you for your kind comment. I am glad to hear you had such positive experiences with these treatments. Best wishes! Dominic
This takes me back a bit. For the early to mid 2000’s, high dose T3 was my main treatment. I started back in ’98 with Dr Skinner. I was the classic case of normal TSH range but fairly classic Hypothyroid symptoms. I was around 20% M.E and was desperate for help. Dr Skinner put me on Armour Thyroid and within a couple of years my health had improved to around 40% where it then plateaued. After reading Dr Wilson’s theories on impaired T4 to T3 conversion I tried the timed-release T3. This had no effect on me. Further research led me to Dr Lowe, I got his books and proceeded to try the high-dose T3. My health improved to around 50-60% before again plateauing. I maintained that level for approx 2 years before I had a big M.E crash. This came after months of stress.
Although I mostly recovered from the crash, I didn’t quite return to my previous level of health. Each subsequent crash followed the same pattern, each time my post-crash level of health would be just that little bit lower. The high-dose T3 therapy just seemed to stop working, I never found out why but I eventually looked for alternative treatments.
In the early 2010’s I saw Dr Thierry Hertoghe. Although his area of interest is more to do with anti-aging, his core treatment for that is hormone treatments. I was placed on Desiccated Thyroid, Hydrocortisone, Fludrocortisone, DHEA, Testosterone and others. For a couple of years I was doing much better again but for some unknown reason, my health then started to decline again. To the point where I had no option but to discontinue this treatment as, aside from the cost, I was able now not well enough to travel to Brussels to see Dr Hertoghe.
I seem to have many adrenal related symptoms and I have wondered if the long period of high-dose T3 could have somehow permanently damaged my adrenal glands in someway. that’s probably unlikely and I’m just grasping at straws for an explanation as to why it stopped helping me.
Currently, I’m on a (comparatively) small dose Armour Thyroid, 60mg. One thing I’ve noticed is that I seem to have both under and overactive thyroid symptoms. Thyroid cellular resistance would certainly explain that. I have a similar mixed symptom pattern with both low and high cortisol symptoms. I’ve often wondered if cortisol cellular resistance is possible?
Anyway, apologies for the medical history. It was just really interesting to come across this article and I hadn’t realised that high-dose T3 therapy was still being actively pursued.
Dear Gareth, Thank you for the description of your experience with these treatments. Yes, I wonder why the thyroid hormone sometimes stops working. Do the cellular receptors or deiodinases adapt to the amount supplemented?… If interested, I’ve written two papers recently. The second relates to these treatments and is called: “Theory: Treatments for Prolonged ICU Patients May Provide New Therapeutic Avenues for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)”. Best wishes! Dominic
Gareth, there is another approach as outlined by Dr Kenneth Blanchard: microdoses. He wrote a couple of books if you are interested in learning about his approach. Some try it but adjust the ratio of T4/T3 he recommends (more T3, still microdoses).
I find that making sure I am eating enough calories, enough carbs, plenty of protein is important as thyroid ramps up metabolism. Progesterone and pregnonelone in my case.
Also, I play the never crashing game – I do not let my body go into anaerobic energy production. I sip orange juice at night when I wake up in my sleep, too.
I worked for almost a year on introducing supplemental vitamins and minerals, once my digestion improved, I am able to get most through my diet alone.
I also make sure I eat plenty of calories, of carbs and protein to meet the demands of my metabolism. A properly working thyroid (or supplemental hormones) ramps that up. You’ll just crash if you don’t eat enough. Will start catabolizing tissues again…
There is an art on how to integrate back to life once one gets metabolism going again. I’m not there yet. Others have. Perhaps there is something to learn from them. How to deal with life stressors…
Ah! do you track your temperature and pulse to see how you are responding to the medicine. And as Amora wrote, one may require adjustments according to the seasons.
gareth DId you recover from ME now? Are you still taking T3? I saw Dr Skinner too. What dose are you on?
Hi Dominic Stanculescu!
There is a third doctor that used thyroid therapy to treat ME/CFS and FMS, among others: Dr Kenneth Blanchard. His approach was a little different in that he used microdoses.
https://power-surge.co/2013/10/05/hypothyroidism-the-many-myths-by-kenneth-blanchard-m-d/
I noticed your name on recent papers with Jonas Berquist – have you teamed up?
I also heard him say on the OMF open house video that they are moving on to actually testing the approaches outlined.
Imagine the day that this will become standard of practice…
From what I understand, Dr. Roda Barnes wrote that with patients that had developed hypoglycemia, treatment with thyroid hormones became more challenging.
Mc Gregor said this on hypoglycemia in ME/CFS:
https://www.healthrising.org/blog/2019/06/15/emerging-insights-mcgregor-metabolism-chronic-fatigue-glycolysis/
Dear Meirav,
Thank you for your kind message. Yes, to make this blog more complete it should include Kenneth Blanchard and microdosing with thyroid hormones (I meant to add this in the past as someone else had commented on it, but I never got around to it). And yes, I remember also reading that blood sugar levels impact activity of thyroid hormones (perhaps it Durrant-Peatfield who wrote about the cortisol, hypoglycemia connection?).
Yes, I collaborated with Jonas Bergquist to write two papers based on my blog posts here on Health Rising — these hypothesise that mechanisms that prevent recovery in prolonged ICU patients also underlie ME/CFS. I am hoping that someone will test the hypothesis.
Since publishing these papers I’ve also been interested in the similarity between “cancer-related fatigue” and ME/CFS. See for example this excerpt from Kamath et al, 2012.
“[Cancer related fatigue, CF] represents a multifaceted, subjective, physiological state characterized by persistent, overwhelming exhaustion, and a decreased capacity for physical and mental work…. CF can be differentiated from the fatigue experienced by healthy individuals by its severity, its devastating impact on quality of life, and the fact that it is not alleviated by rest or sleep… CF is often disproportionate to the level of physical activity or exertion and interferes with usual functioning. Fatigue symptoms may persist for months or even years after completion of cancer treatment, even when the cancer is undetectable or in remission.”
Best wishes!
Dominic
Hi Dominique!
Ron Davies has spoken about using the nano needle to test existing medications, to see how the ME/CFS cell reacts, in search of a possible treatment.
I wonder what would giving the cell T3, T4/T4, progesterone, etc do?
Of course, the cells are in isolation, out of their context, not interacting with the systems and organs that make up a person. That would need to be taken into consideration, etc.
Dear Meirav,
your message makes me think of something else.
Prof Ron Davis had found that blood from ME/CFS patients affects how cells from healthy persons react to stress.
Serum from patients with non-thyroidal illness (NTIS) inhibited T4 uptake in cells.
De Groot (2015) writes: “Lim et al. and Vos et al. found that serum from patients with NTIS inhibited T4 uptake. Sera from critically ill NTIS patients caused reduced T4 uptake compared to control sera in one study, and the authors considered elevated nonesterified fatty acids (NEFA) and bilirubin and reduced albumin to play a role”
Dang! i wrote a reply but I think the recent problems with the site swollen it… Did you get to see it per chance?
there is a group in hEDS that has high bilirubin – there was a paper out on it.
I wrote more,… I can’t remember 😉
Hi Meirav,
interesting about high bilburin in some hEDS patients. (Sorry the rest of your reply was lost!). I tried to send you some additional ideas per email. Best! D
Was Looking for some advice as I just might be able (not confirmed yet) to get access to T3 on the UK NHS, I’ve been on T4 for a few years without much improvement. I want to learn more, and this blog page gave me more than that! so thank you to the person or person’s that put this in depth article together. Can’t say I understand all what’s being said, but I will continue with my research this Blog/Article has given me. I really do want to thank whoever gave their time to do this. Thank you, Del
Perhaps the mysterious factor in ME/FS blood…
and FMS
and POTS
etc
“Extracellular vesicle-based interorgan transport of mitochondria from energetically stressed adipocytes”
https://www.sciencedirect.com/science/article/abs/pii/S155041312100365X?via%3Dihub
https://www.the-scientist.com/news-opinion/fat-cells-send-mitochondrial-distress-signals-to-the-heart-69110
I am sorry that I missed reading this article in full when it came out. I will now print it all out as it is excellent!
I was diagnosed hypothyroid when I was 44 and this was 25 years ago. I began to decline in health on T4 during my menopause which began only a few years after I was settled on T4 and given my last period was at 49, it wasn’t that long after.
I didn’t think of it being anything to do with my thyroid as apparently for most of the time my blood tests were normal on my 100mcg dose of T4. When they were not, which did happen, my GP increased my T4, but slowly my health declined further. Eventually my symptoms increased and I could not longer walk a normal amount without fatigue and PEM. At this point I was diagnosed with ME/CFS.
It was 9 years ago that I began to research the thyroid and saw that some people were advocating T3 in addition to T4. I had my bloods done privately and noted a low FT3 score with a high FT4. I was very lucky that my GP supported me to see an endocrinologist in the UK, who prescribed T3 with T4 for me on the NHS, but it didn’t help me. I believe that it simply was not enough. At my request he agreed to prescribe T3 only if my GP would support me, which she did.
I cannot say it’s been a total cure, but it’s improved my quality of life for sure. I have had a huge amount of stress over the past 9 years (and before) and this constantly impacts on my recovery. And I have also been challenged by new endocrinologists to reduce my T3 drastically especially since the cost rose here in the UK. I became iller over a period of a few months, and refused to continue. Eventually I have gone back to using 50 mcg a day over 3 doses. I did have some adrenal support initially and at times since then. I am not able to walk normally without resting, but at the age of nearly 70, I have a reasonable quality of life if I am careful.
Unfortunately I am due to move house soon to another health district and I fear I will have to fight for my T3 on the NHS, but whatever happens I will continue to use it even if I have to buy it off the internet. My quality of life demands it.
I’ll add this site for additional reading. It is very strong in the science and research
https://thyroidpatients.ca/resources/our-tips-and-guides/
And just the cursory note that I self medicate with T3 only which is allowing me to continue the search for a healthier life.
I am so very grateful for the creation of this site and do wish each of you a life filled with joy even where the challenges might seem overwhelming.
Dear Dominic, I just wanted to thank you for producing this excellent article. I got used an endocrinologist in 2022 who was useless as he was using the NHS TSH scale (a word of warning to others, anyone who works for the NHS will do this even if you employ them privately).
However at the end of last year I read this article and did further extensive research, and eventually found a private endocrinologist to help me with dosing to an optimal thyroid scale using T3 which I got hold of elsewhere.
The result is that I am now on T3, and it has been a complete game changer. I have had a 15 year diagnosis of CFS which I realise for me and many others teh major problem is really a hypothyroid and or hypocortisol (both for me).
I now feel a million times better, even at a low dose. My headaches went straight away, I’m now 2 weeks in and am getting much more out of my days, sleeping much less, feeling refreshed and have not crashed in two weeks. I am early in my dosing journey but I really do feel this drug has already changed my life completely.
Thank you for writing this important article which helped me so much to find treatment for what I no longer believe is a non treatable disease, which is what I was told for 15 years.
To anyone considering this treatment and wondering. T3 is primary, do not do hydrocortisol first, T3 comes first and find yourself a decent endo before you try self treating and killl yourself. I nearly did twice. I did not know T3 should only be up dosed at 6 week intervals and many other things. I recommend Dr Frey at Country Health
https://www.countryhealth.co.uk/?fbclid=IwAR3-moHzQB5kj2ydL0EirglMpUGtc_dBOQLbb5wWk_K_Fb9Ohj8q6CnOSaM
Dear Cathy, Thanks so much for your message. I am so glad that this blog post helped you! Best wishes in your recovery! Dominic
Thanks Dominic,
Updates to my comment
For me thyroid was the primary that worked. Where I went wrong with hydrocortisone is trying the every other day treatment that is supposedly safe for someone without destroyed adrenals. It became clear I do not have healthy adrenals. People really need to be careful, though I understand not everyone can find a private endo who does not stick to the standard TSH scale, it is really worth trying and using great caution. It’s easy to get it wrong.
Final comment. It’s worked. I am now on a much higher dose of T3 and also take pregnenolone which is much safer than steroids to support my cortisol and am now in almost perfect health. I never crash and my real CFS days are nothing but a bad memory. Thanks again Dominic for your help this article was a key information source for me when I did all my research. I am healthier now than I have been in the last 30 years and really, my entire adult life. My greatest thanks, and very best wishes to you, your wife and anyone reading this article.♥️
Dear Cathy. That is great to hear! So glad you are feeling better and that his post helped you. 🙂 Best wishes! Dominic
In case anyone is reading this in 2025 and later. I believe that for the subset of patients that do not respond well to T3 therapy, extensive dry fasting will be required. This is something I have guided a few patients with, and had tremendous results. Most of this was based on my own self-experimentation that later turned into guiding a few people I was working closely with. So far, total success. The theory is that whatever affects your ME/CFS may need to be treated first. What could the problem be? Many things, but thankfully, autophagy and stem cell regeneration that you get from fasting may be able to target most of them. Some deep-seated problems may require something incredibly potent, and that’s where these really long fasts come into play. This may reset your cellular receptors/sensitivity to treatments, making T3 therapy work for everyone. Of course, fasting has a negative effect on the thyroid, which is hopefully fully reversed with T3 therapy following Wilson’s syndrome guidelines. I do believe Teitelbaum’s advice should also be heeded with an antifungal approach (200mg fluconazole) and I personally am a fan of ivermectin (daily or weekly dosing). Fenbendazole, in addition to a combo, may be even better. Ivermectin seems to work much better when thyroid hormones are regulated aka on the t3 therapy (for anyone who has had bad experiences on ivermectin, i’d like for you to consider this angle, that your t3 levels were bad and this affected many “cellular resistance” components and therefore your negative effects from things like ivermectin and possibly many other things. of course I have a few different recommendations that build on these strategies and they include peptides, thymus regeneration, and ray peat general advice.