

“…many of these people spout nonsense and then freak out when confronted with facts or details about the research that they can’t explain away.” David Tuller
David Tuller is a unique figure in the ME/CFS universe. A reporter and editor for the San Francisco Chronicle, Salon and writer for the New York Times, the policy journal Health Affairs, and other publications, Tuller became outraged at the long history of neglect and abuse directed toward ME/CFS.
Tuller has a long history of investigative journalism in health issues. (From UC Berkeley Journalism- https://journalism.berkeley.edu/person/david_tuller/)
His publications date back to 2011, when he published the long exposé, “Chronic Fatigue Syndrome and the CDC: A Long, Tangled Tale”, on the history of the CDC’s CFS program under Dr. Bill Reeves.
It was the largest (n=640) and most expensive ($8 million) clinical trial ever attempted in chronic fatigue syndrome (ME/CFS) that really got Tuller rolling. Intended to be the trial to end all trials in ME/CFS, the trial proponents hoped it would show that cognitive behavior therapy (CBT) and graded exercise therapy (GET) could get ME/CFS patients out of their doldrums and back to being productive members of society – and in a cost-effective manner – to boot.
With its $8 million price tag and hundreds of patients, the stakes were high. Lead by Peter White, Michael Sharpe and Trudie Chalder, the PACE trial featured the cream of the crop of U.K. biopsychosocial researchers, who, perhaps worried that the trial would not succeed, made a series of controversial changes to the trial protocol that ended up significantly bolstering its results.
While the results were never that great, the trial seemed to be a hit. Bolstered by the researchers’ comments to the media, the major news organizations lapped up the good news like honey: CBT/GET can help or even cure ME/CFS.
- “The Medical News Today” reported that “Fear of exercise is biggest barrier to chronic fatigue syndrome recovery“.
- “Psychotherapy Eases Chronic Fatigue Syndrome, Study Finds”— New York Times
- “Pushing limits can help chronic fatigue patients”— Reuters
- “Brain and body training treats ME, UK study says”— BBC
- “Therapy, Exercise Help Chronic Fatigue Syndrome”— WebMD
- “Helping chronic fatigue patients over fears eases symptoms”— Fox News
- “Chronic fatigue syndrome patients’ fear of exercise can hinder treatment – study”— The Guardian
- “Chronic Fatigue Treatments Lead To Recovery In Trial”— Medical News
Critiques of the trial emerged quickly from patients and patient organizations, but to no avail. Since 2011, the study, which the Lancet posted as an open access article – thus ensuring it would get maximum coverage – has been cited by other journals 675 times, and ended up playing a major role in the UK’s National Health Service, the Centers for Disease Control, the Mayo Clinic, the 2013 Dutch, and Kaiser‘s guidelines for using CBT/GET in ME/CFS. One reporter stated that, “PACE has become the paradigm for understanding a condition affecting millions of people.”
David Tuller’s 15,000 word 2015 investigative piece, “TRIAL BY ERROR: The Troubling Case of the PACE Chronic Fatigue Syndrome Study“, published on the Virology blog website, galvanized efforts to expose the trial’s shoddy methodology. Arguing that trial results were built on a house of cards, the article played perhaps the key role in lighting a fire which is still burning today.
Eight years later, the trial is shrouded in controversy. White, citing stress, has retired, Sharpe is no longer studying ME/CFS, and statisticians have trashed the Lancet for: a) publishing such a shoddy piece of work; and b) not retracting it. One hundred and fourteen academics and experts signed on to letters denouncing the methodology used in the trial. A Columbia statistician, Professor Bruce Levin, used the PACE trial as the case study in a talk last summer titled, “How NOT to Conduct a Randomized Clinical Trial,” and called it “the height of clinical trial amateurism.”
After Queen Mary College of London University’s attempt to block the release of the raw PACE data proved to be an embarrassing failure, a re-analysis of the trial, using the original protocol, demonstrated what many suspected – that the trial was largely a failure. Remarkably, every modification to the trial protocol had served to boost its results – in one case by 400%.
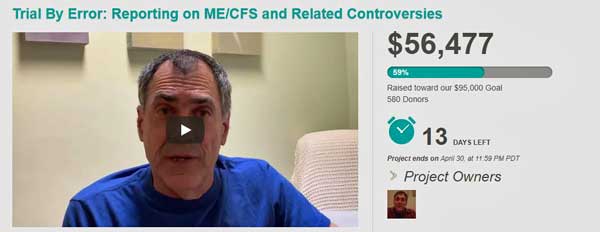
Tuller’s disgust with the PACE trial launched him on a unique, patient-supported investigative effort lasting two years, which has grown to focus on ferreting out the bad science permeating the biopsychosocial field. Tuller’s analyses of the Cochrane Report on GET in ME/CFS, the School Absence study, the Lightning Process study, and others have sparked questions and in some cases investigations.
Now, as Tuller raises money for a third year of investigative journalism, it seemed like a good time to catch up with him and his work.
David Tuller Talks
From my perspective, debunking bad research like PACE is the most effective way that I personally can improve health outcomes on a population level. David Tuller
You reported that the BMJ published an article calling you an “activist” while neglecting to include your professional credentials – you have a Doctor of Public Health degree. (The credentials of the pro-PACE commenters were all included.) That seemed intended to negate or slight your contributions. What is a Doctor of Public Health degree?
Good question! It’s a DrPH. I’d never heard of this degree before I became a public health masters student at Berkeley. In the US, many disciplines have both academic doctoral degrees — i.e., a PhD — or so called “professional” doctoral degrees. So in public health, a DrPH degree is considered interdisciplinary and geared toward problem-solving or translating research into practice.
In my case, I received my DrPH while already on the journalism faculty. I was able to continue to take courses and pursue the research for the degree as an employee benefit. I’ve never held myself out as being anything other than a social scientist in the public health field. I’m obviously not a medical doctor or a biologist or an epidemiologist or biostatistician. It’s strange to sort of be criticized for not being what I’ve never claimed to be, which is what seemed to happen in the recent Reuters piece.
With regards to the piece in the BMJ — I don’t think the writer realized, so I don’t think it was intentional. I’ve never had any contact with the journalist. I think it’s actually a bit more pernicious. He just assumed that anyone opposed to PACE was an “activist” by definition and didn’t have credentials. Fiona Godlee knows very well who I am, and so the piece was corrected pretty quickly. Of course, they added my credentials but did not remove the word “activist,” which pissed me off. I would guess the reason why is that adding something is a “clarification” while removing something is automatically a “correction.” But they have provided no explanation for why I am an “activist” for advocating my professional and academic view about this research, while those defending it are presented as just doing their academic thing.
How have the PACE trial authors responded to the many critiques of the PACE trial?
Well, yeah, they’ve “responded” many times, as they keep whining. The problem is that they keep providing non-answers. They keep repeating the same stupid things. And that essentially boils down to, ”We made changes and we think the changes we made are good, so there!” That worked for quite a few years, apparently. It’s not working too well for them anymore. The narrative has changed. They now have to portray not only patients as hysterical and oppositional, but me, my colleagues at Berkeley who use PACE as a case study of bad research, and the 100+ experts from around the world who signed that last open letter to The Lancet. It’s gotten to the point that the only way Reuters, for example, could present the side of the CBT/GET ideological brigades is to pretend only me, patients and Dr. Myhill in the UK think PACE stinks.
The Lancet PACE study was just the beginning of a series of studies that were published on the PACE trial. If the Lancet PACE trial falls, will the rest of them go as well?
Yes and no. That’s complicated. They all suffer from being open-label studies relying on subjective outcomes. That should be a non-starter in terms of relying on such studies for policy-making, but unfortunately that is not the case. PACE is also likely research misconduct on top of bad science, because of all the data manipulations and the decision to not tell readers that, for example, 13% of the participants had met the outcome thresholds for “physical function” at baseline. You can’t hide stuff like that in research. It’s wrong.
The other issue is that many of these are Oxford criteria studies, so we don’t even know who is really in the sample. Certainly, if PACE were to finally be officially recognized as garbage, that would have a big impact. But my predictions aren’t really that good — four years ago, I thought if I wrote a 15,000-word investigation and revealed what I did, the trial would not survive. Certainly if this were a trial of any other illness that people believed existed, it would have been retracted long ago, or never published.
The PACE trial has been bashed all over the place, but Richard Horton, the editor of Lancet, still seems unresponsive. What are you and others requesting that Horton do, and if he continues to be unresponsive, what, if anything, is there left to do to get him to change his mind?
I originally assumed people were thinking clearly, and that if you point out that people could be “within normal range” for physical function at baseline, and then you also point out that 13% of participants were in fact “within normal range” for physical function at baseline, there would be a response. Horton does not seem to think there is a problem with the study. I mean, among all the others. He will never change his mind. He came out swinging when patients first began criticizing PACE, and his reputation is tied to it, I’m afraid. Or at least maybe that’s how he sees it. I don’t know. It’s very bizarre. Then he runs all over the place talking about the problems with research. I want to say to him, clean up your own back yard first.
What I don’t get is what Lancet gets out of this? Having over 100 academics say a trial published in your journal is trash isn’t good, but having the American Statistical Association urge its conference participants to attend a talk on PACE to learn “how bad statistics harm patients and our profession” is beyond embarrassing.
That’s just the beginning. The Journal of Health Psychology devoted an entire issue to the PACE trial. Rebecca Goldin, a Professor of Mathematical Sciences at George Mason University, stated that the shoddy way the PACE trial and its aftermath have been handled at the Lancet (which pushed it through in 4 weeks) had “sent shockwaves through medicine.” Professor Bruce Levin has stated that the Lancet’s defense of the PACE trial had diminished the respect The Lancet is held in “worldwide”.

Richard Horton’s refusal to acknowledge the problems with the PACE trial has exposed the Lancet to ridicule. (Image from WIkimedia)
Do you have any idea why Richard Horton, the longtime editor of the journal, who, by the way, has taken the medical field to task for its often “poor methods” and misleading results and portrayed himself as a straight shooter, is willing to expose his beloved Lancet to such ridicule? At times he seems almost beside himself with anger at the “activists” who have raised questions about the trial.
I really don’t get it. I also don’t get why The Lancet fast-tracked the study to publication. My assumption, and I have no way of knowing if any of this is the case, is that he was assured it was a great trial and took these people at their word. And now he’s kind of gotten himself stuck in a place he can’t get out of. He’s defended it so many times, he’d look like an idiot to back down. But he looks like an idiot anyway because he’s defending something that objective observers know is ridiculous. Poor guy!
You’ve also criticized the Psychological Medicine PACE recovery study, where, as you noted, “the investigators weakened all four of the ’recovery‘ criteria laid out in their protocol, because, as they have explained, they determined that their initial assessment methods were too ‘stringent’ to demonstrate ‘recovery’. In other words, they were concerned that their reported ‘recovery’ rates would be too low.” The recovery criteria were so lax that 13% of the ME/CFS patients who entered the trial were already deemed recovered. What is the status of the Psychological Medicine study?
The status is the same. It’s in the literature, and so people can cite it. That study really should be retracted immediately. The single analysis is completely bogus because they weakened all the criteria, because of the overlap you mentioned, and because they do not appear to have received any oversight committee approval for these dramatic changes in the recovery definition. No study should be published with these egregious issues. The editors have behaved disgracefully — but then Sharpe is or was involved with the journal. So a lot of this, I assume, is just how they’ve always done things.
Peter White, the senior author of the PACE trial, has retired, Simon Wessely is long gone, Michael Sharpe is no longer working on ME/CFS, and the Reuters article indicated that others have left the field. A Dutch Health Council recommended against using graded exercise therapy (GET) and focusing more on biological research. The Cochrane Reviews, at least temporarily, has pulled an analysis of ME/CFS GET studies over concerns of accuracy. After the AHRQ in the US pulled its recommendations for CBT/GET, so did the Centers for Disease Control. Now NICE is reviewing its guidelines for CBT/GET. Is the biopsychosocial approach to ME/CFS, which has consumed so much UK and European funding, in decline?
It certainly looks that way from the perspective of the US, especially when it comes to ME/CFS. And that’s great. At the NIH meeting in early April, there was not an iota of skepticism expressed that this was anything other than a devastating illness and that the answer was biomedical. That’s putting aside the question of whether specific research was good or bad, or whether NIH needs to ramp up spending dramatically. On the scientific level, everyone has moved beyond that framework. Just to be clear — it will take longer for that change in attitude to spread among health care providers, so people might not feel that change immediately in their own medical care, unfortunately.
And some of these issues aren’t settled at all in Europe. We don’t know what Cochrane will ultimately do with the exercise review. We don’t know what the NICE guidance will say. In Finland, Norway, Denmark, Germany, etc., the CBT/GET ideological brigades are very strong. In the UK, they might lose some ground on ME/CFS but make it up by treating people with IBS or other illnesses falling under the category of “medically unexplained symptoms”, or MUS. Especially because they are expanding the program called Improving Access to Psychological Therapies, or IAPT — an NHS program designed to shunt people with many illnesses away from medical care and into short-term CBT and related therapies.
The National Institute for Health and Care Excellence (NICE) in the UK will publish a review of its guidelines for CBT/GET in ME/CFS next year. Do you have hope that any substantial changes will occur?
Well, I have more optimism than many in the UK who have been down this road so many times and faced such nonsense for decades. There are some smart people on the panel who have their heads on right, and then there are some biopsychosocial folks, and more of them than would appear warranted. And there are huge interests at play, and lots of money and lots of embarrassment to go around the entire UK academic and medical establishment around this whole issue. So, in some ways, how that plays out is unpredictable.
But the reason I have some optimism is that many of these people spout nonsense and then freak out when confronted with facts or details about the research that they can’t explain away. So, these folks on the panel who will be promoting CBT and GET will have to come up with some decent answers to explain their reasoning. Those answers don’t exist. Now, of course, I could be wrong, and if it comes down to a strict vote, who knows what will happen? But there are people on the panel who will be arguing very hard for what is right, and with all the facts on their side — and that’s a huge difference from the last time around.
Do you believe Dr. Sharpe and others when they say that they believe that chronic fatigue syndrome is a biological condition?
That is really sophistry. Everything is biological. Deconditioning is “biological.” I believe they believe people have real symptoms due to deconditioning. When they say they believe in “biology”, they often mean they acknowledge that it is triggered often by an infectious illness. So, in that sense, they have always believed in “biology”.
They have publicly insisted, however, that the perpetuation of the symptoms is due to deconditioning, which is due to unhelpful illness beliefs. Now, I have no idea if at this point they actually still believe that. I would actually assume no and they’re trying to massage how they talk now. However, I have never claimed that they believe it’s “all in the head” because that’s not true. They seem to believe the symptoms are very real, as I read their work. In their theory, the symptoms are the symptoms of deconditioning and accompanying disruption of circadian rhythm, muscle atrophy, etc.
What effect has the CDC’s decision to drop CBT/GET from its guidelines and pull any references to the PACE trial had?
It will ultimately have a huge impact. It’s the CDC. If they don’t believe the science holds up, people pay attention to that. But if the CDC actually behaved like a public agency, this change would already have had a much bigger impact. As soon as they dropped those from the recommendations, Dr. Unger or someone from CDC should have gone out and made a statement about it and informed Kaiser Permanente, Mayo Clinic, and so on. Even just put out an advisory or press release! Something. But they did nothing. I noticed that it had happened because someone mentioned it to me, and so it only became public when I asked the CDC about it.
Then they started making the ridiculous claim that they removed the recommendations because people misunderstood or took then the wrong way. That is really nonsense. It’s face-saving. And I find it very dispiriting to see public health professionals acting that way — since that’s what I am. As public health officials, they have an ethical and professional obligation to acknowledge that they got it wrong, that it was a mistake to be citing PACE, that everyone understood what they meant by CBT and GET, and that they are sorry about the whole mess. Of course, they haven’t done that.
In the past year you traveled to Australia, the UK and Ireland and, of course, you’re from the US. Did you find differences or similarities in how ME/CFS is viewed, studied and treated in these countries?
Well, the most striking difference is in nomenclature. In Australia, patients, clinicians, researchers all say “chronic fatigue” to mean ME, as used by people in the UK. When I was there, at first I corrected people, and then I just gave up. When I gave talks, I would say that you can’t blame others for conflating the illness and the symptom of chronic fatigue if you’re going around calling it “chronic fatigue”. And people would nod and say yes, yes, and then they’d refer again to “chronic fatigue.” So, I decided I’d either tear my hair out or just not let it bother me.
In the US, of course, no one has heard of ME. If you mention ME in the UK, people not involved say, oh, chronic fatigue syndrome, right? Or at least that’s been my impression. In the US, zero recognition of the term ME. Now, of course, in the US, the government agencies are calling it ME/CFS, but most people have no idea. So, you can’t really get around yet from referring to it often as chronic fatigue syndrome. It’s challenging to write about also because the studies all use varying terms. If a study calls itself a study of whatever in CFS, I kind of try to use CFS when writing about it.
Tuller on his Crowdfunding Effort
What’s on the tap for next year? What do you hope to see happen?
I’d like to see enough happen that maybe a year from now, I can think about, you know, something else! I’m joking, but serious also. It would be nice to feel that there’s been enough momentum and that it feels real. I still really find working on this project rewarding and fulfilling. I do feel that I need to focus more on the MUS steam engine as it picks up speed, and look more at other complex illnesses that fall under the MUS umbrella.
In the US, I’d like to focus on how care is being delivered, what care are people getting, what are the major medical centers doing now that Kaiser Permanente has at least made steps in a positive direction. I think it’s also important to keep up pressure on the NIH and the CDC to do their jobs, and that includes ensuring that case definitions are used appropriately.
I have training in public health, so while the science is very interesting to me, I tend to focus more on the impacts of things in the world. Public health is really about considering health on a population level. From my perspective, debunking bad research like PACE is the most effective way that I personally can improve health outcomes on a population level. So this is both my public health project, and it’s also my investigative journalism project. It’s kind of a perfect project for me in that way.
Help fund David Tuller in his work over the next year here. Your contributions are tax-deductible








As I told David Tuller, rather than focus on just the “mishandling” of PACE, it would have been much easier to explain that “CFS” was a ploy used by the CDC to disguise the Lake Tahoe outbreak’s evidence, and that all subsequent CFS definitions were performed by researchers who knew this, but proceeded to compound and expand upon the deception for purposes of advancing their own psychosocial agenda.
It is like trying to get a conviction for reckless driving without bothering to mention that the car was stolen.
If you know this, it is clear why they were behaving this way.
First, thank you for doing the kind of investigative journalism you do.
Second, I would like to mention a few facts:
1. Viruses are known to morph. Rapidly. In the human body and outside of it.
2. Chronic fatigue or whatever catch all term is applied, could be caused by a multitude of factors. For example, a plausible scenario could be exposure to a neuro-toxin such as pesticides, causing immediate symptoms, that lead to debilitation and impede the immune system which then cannot effectively battle an existing virus, so chronic and severe debilitation ensue.
3. EMF proximity is known to interfere with cellular health as well.
Just some things to think about.Follow the money. The medical system is controlled by those with agendas.
Thanks, Stacey and Erik.
Always follow the money trail to corporate stockholders (and the tenured chairs and pensions).
Causal multifactors also include mycotoxin exposure; of a large group of patients with ME who took the RealTime mycotoxin test (covered by Medicare), something like 80% of the group were found by a prominent physician to have significantly high levels of mold metabolites in their bodies. I trust someone will correct this figure if it is too off the mark.
and called it “the height of clinical trial amateurism.”
It could be that or it could be “the height of medical advertorials and lobbying.”
I think there was a tremendous amount at stake. That trial dwarfed others in size and cost and if it didn’t work out their careers were on the line. There must have a tremendous urge to make sure it did as well as it could. What really shocks me is that after all the shenanigans that the results STILL weren’t that good. That should say something.
There was certainly a major marketing/PR push accompanying publication, to disseminate news of the supposed success of the PACE Trial worldwide, along with its message that ME had been shown to be a deconditioning/ psychologically induced condition from which PwME could recover, or at least significantly improve, using CBT/GET.
PR/marketing professionals and/or King’s College graduates were employed specifically for this project, at least some of them working for Wessely. The daughter of my sister’s then partner was one of them, and I remember the deep distress it caused my sister (who also has ME) that as a result of their ‘biopsychosocial’ beliefs passed on to him from his daughter, her partner didn’t believe she was genuinely ill, and that going for long walks would cure her.
Elizabeth, I am so sorry to hear about your sister and the bad experience she had with her previous partner. I was actually quite shocked to read about her long walks. Thankfully my husband and children are the opposite and are all too aware of the importance of pacing correctly. So much so, that it’s Easter dad and a glorious sunny one at that, so all the family are sitting outside eating lunch that I would have previously made. Thank goodness for Marks and Spencer’s who provide a great take a way buffet! I’ve said hello to them all and given the kids their gifts and now back upstairs. I’m too poorly today to be with them, but they all understand.
Happy Easter to you and your family and let’s hope this biopysycological approach will change, but I doubt it for a very long time. Having seen a rheumatologist in January here in my home plus seen a neurologist at the end of March, both are of the belief that the trial was ‘good science ‘. I just had to take a deep breath especially when I was also diagnosed with functional neurological disorder. Mmmmm…… treatment is by a psychologist, I’ll hold my judgement until after my first visit whenever that will be!
xxx
so grateful that this change is happening, albeit slowly
disgusting that it ever occurred
hoping the funding comes together David
A lot of people contributed. I remember Julie Rehmeyer’s excellent article at the time and the work of several patients to uncover and cleverly illuminate the trial issues but I think David’s long article really sparked something – really galvanized something, brought the trials problems to attention in a new way. That was a turning point.
Thank you David for being a journalistic warrior on behalf of all ME/CFS sufferers!
Yes, yes, yes!! You’re a hero!!
Thank you, dear, sir!
Yay David! Let’s get him funded 100%!
I’ll be donating to the cause, even though I have little to give, I imagine many of us doing the same will help gain enough funding to carry on the fight
In March of 2019 the British Association for CFS/ME (Bacme) sent out the results of their survey of Specialist services serving CFS/ME patients in the UK, and the two most common treatments used by 38 out of 42 clinicians was graded exercise therapy (GET) and/or cognitive behavioral therapy (CBT). This is in spite of the clear evidence that GET has often been shown to be harmful to ME/CFS patients.
Wow…
I’d like to see a criminal investigation into the fraudulent PACE trial and its publication, not just because of the massive amount of funding they received, but because the PACE trial recommendations made many patients worse, and also enabled the medical insurance companies to avoid paying out their clients, (ME/CFS patients).
From memory I’m pretty sure Simon Wessely was also a spokesman or advisor for the medical insurance companies. Which if true could well be why he and his potentially criminal colleagues altered the PACE data to become a misleading disgraceful lie presented as fact. Which in turn stifled real biological research and prolonged the suffering of millions of patients for years if not decades.
The whole saga is perhaps the most appalling study in recent scientific history, especially for its sickening flow in effects to patients health and financial situation.
I don’t know if we’ll ever get a criminal investigation but what has happened is pretty darn amazing. Just think the trial has been used in classes as an example of how NOT to do a clinical trial. An entire issue of a Journal was devoted to it. It’s an $8 million example of how to screw up a trial! That’s amazing!
I still think it could be worth investigating the possibility of a private lawsuit though – I’m thinking, a big national or international class action, along with all the attendant publicity such an action would engender – by those who’ve been harmed by GET/CBT, as well (perhaps)as those who’ve been denied benefits/insurance payouts as a result of the false advertising/promotion of its benefits and safety.
I do think that the shock value of a successful lawsuit might be what’s needed to convince the remaining pockets of ME/CFS denial to change their minds or at least their harmful practices – and thus save countless more ME/CFS patients from the horrors of medically created long-term or permanent disability.
It would be good if we had someone who could give us pro bono legal advice on this.
Elizabeth that’s a brilliant idea, a law suit against those in the PACE trial for falsifying data while knowing it would cause worldwide malpractice and emense suffering. Plus a probe into Simon Wessely’s involument with the medical insurance industry. Did he have meetings with them? receive funding or payments from them? etc.
No matter what, it will open the world’s eyes to how badly we’ve been treated by unethical fraudulent psychiatric researchers.
We should start a ‘Give a Little’ page to raise funding for a civil lawsuit.
I’ll help where I can. The key is to promote the donation for the lawsuit as also an awareness campaign, as is a damn good story for the media to publish and follow over time. The public awareness will then attract even more research funding to the OMF and Solve ME/CFS.
My email is vespa.bw@gmail.com
I agree with you, Brendan. This has not only been bad science, but has delayed the good science. 29+ years into this, and my career as a research physicist at the Plasma Physics Lab at Princeton U. lost, I’m still angry.
The NIH is STILL promising – and not doing much of anything. Promises don’t cure diseases.
Someone needs to be held accountable – a bunch of someones who perpetrated this mess, and are invested in continuing to blame victims. It would be so good to have them brought to trial, and David has certainly documented the paper trail. Maybe some day…
“…and also enabled the medical insurance companies to avoid paying out their clients, (ME/CFS patients).”
Spot on, $ is the problem.
Americans tend to think the financial interests involved were to do with insurance companies but in the uk sickness and disability payments are not typically made through insurance companies but through government agencies, in this case the Department is called DSW. This was the major funder of the study. With the exception of a relatively small contribution from The Welcome fund ALL THE FUNDING CAME FROM THE BRITISH GOVERNMENT BECAUSE THEY HAD BEEN ASSURED THAT There were vast savings to made for the public purse by short term treatments that forced people back to work and off welfare. At the same time they set up systems for assessment for sickness and disability payments designed to do this. The ME patient groups have been struggling to deal with the consequences of this assessments system ever since.
The British government would have to undo a great part of this massive restructuring of the governments health and welfare system if they were to recognise the problems the the key research – Which they commissioned!
Many in the British government genuinely believed that these savings were going to save the Health Service NHS and the welfare state – that’s a lot to undo.
A cure for CFS would be so welcomed in my lifetime. I’ve had it and Fibromyalgia for over 30 years! Continue your conquest!!! Thank you!
The problem with the bad science by the PACE researchers and The Lancet has to do with more than ME patients being pushed to do treatments that don’t appear to work or not getting a proper medical assessment. The danger is, which this article seems to be an example of, is that people may take the opposite position for a fact: That ME in no way can be significantly improved or cured by mental techniques/therapy. All areas are worthy of scientific investigation. Especially when the scope of research into mental treatment has been so narrow up until now. So let’s remind our selves that strong positions in science is a problem no matter who is speaking, when the data to support what is stated is not there. Let’s also remind our selves that beliefs about health and disease can affect the disease state. That’s just as factual as many ME patients having abnormalities in their blood work.
There is the other side of it – that just because the PACE trail was atrociously done (and when done correctly was ineffective) and because CBT/GET are not very effective and in the case of GET can be dangerous doesn’t meant that mind/body work or that carefully done “exercise” can’t be helpful in this disease and others. They just shouldn’t be advanced as cures or as evidence that a disease is psychological.
All you have to do is read Donna Jackson Nakazawa’s account “The Last Best Cure” to get how helpful mind/body techniques can be with a serious autoimmune diseases. After a year of rigorously employing them not only did she feel much better and have better functioning but her immune results were markedly improved (!)
https://www.healthrising.org/treating-chronic-fatigue-syndrome/last-best-cure-blog-series/
It’s a good point. From personal experience I can say I was able to get great results from assiduously applying mindfulness meditation combined with a complete physical and mental/emotional ‘letting go’ technique for ‘disappearing’ deep aching limb pain and allodynia, and also completely curing my severe secondary depression and anxiety. Neither have come back; whenever there’s a hint of them I just reapply the techniques and they’re gone.
But I should add, I do also watch my nutrition and hydration, since learning from a naturopath many years ago exactly how specific food and chemical sensitivities and diet-related gut and liver issues can produce a great deal of ME-like pain and discomfort, brain fog, etc, and how to relieve them with nutritional and related therapies. I don’t believe for me, the meditation would have worked had that basic biophysical stuff not been cleared up first.
So I’d definitely agree that for some, at some point in their ME/CFS journey, some excellent symptom relief can be obtained using mental techniques. Unfortunately I haven’t found any mental technique yet for curing the Orthostatic Intolerance and cognitive issues that have been long-term symptoms since a pesticide poisoning 50 years ago, or the more recent (only 20+ years) addition of PEM/crashes, sleep issues, and severe physical and cognitive exhaustion/dysfunctions.
But it’s become increasingly clear (see the recent UK patient survey) the whole shaky concept of ‘deconditioning + exercise fear as fundamental causation, with GET/CBT as the cure’, while helping a few, has also done a tremendous amount of harm to countless patients – perhaps because it was a far too unsophisticated approach to the mind/body intersection, and was never based in any really in depth understanding or proven biomedical hypothesis of causation, but rather on a fairly random hunch fed by ‘evidence’ of false positive outcomes that were probably only achieved through its proponents’ perpetual conflation of PwME and Chronic Fatigue Syndrome with people with a single symptom, chronic fatigue.
Since 2011, the study, which the Lancet posted as an open access article – thus ensuring it would get maximum coverage – has been cited by other journals 675 times, and ended up playing a major role in the UK’s National Health Service, the Centers for Disease Control, the Mayo Clinic, and Kaiser‘s recommendations for using CBT/GET in MECFS.
The PACE-study also played a mayor role in the Dutch guideline for treating CFS and ME (2013) (https://richtlijnendatabase.nl/richtlijn/chronisch_vermoeidheidssyndroom_cvs/definitie_van_cvs.html). Therein CBT and GET are the only recommendated treatments. The Dutch general practitioner society (NHG) has removed this guideline from their guideline database, after the patiëntorganizations pointed out that it was outdated. But the NHG did not give a public explanation. (And it is no guarantee that Dutch general practitioners change their mind).The Dutch medical specialists still have not retracted the guideline.
Thanks for pointing that out. I will include it in the blog.
I’m so glad that David plans to ‘focus more on the MUS steam engine’. For those who don’t know, ME/CFS is at the heart of the MUS (medically unexplained symptoms) steam engine in the UK. The same group who have effectively deprived ME/CFS patients of good, biomedical care and research for decades have, at the same time, been working on this MUS project. In the late 1990s, Wessely, Sharpe and Chalder relayed the importance of their ME/CFS management model (CBT) for the treatment of patients with other medically unexplained illnesses.
Why does MUS matter to ME/CFS sufferers outside of the UK?
Well, firstly the aim is to sell the MUS model around the world. We’re all susceptible to other health problems and would presumably hope that they’d be properly investigated and diagnosed and not dismissed in the way that ME/CFS has been. Who’d want to see family and friends treated in the same appalling way?
Secondly, when researchers act in a certain way then it’s not unreasonable to suspect that they might act in the same way across the board, not just in one area of their research. So are there significant and potentially damaging problems to be exposed in relation to their MUS research? I strongly suspect there are.
And then there’s Michael Sharpe, poor guy, who’s seemingly been trolled out of research into chronic fatigue/CFS, but still appears to be a key player in psychosomatic medicine. Perhaps he forgot to mention to the Reuters journalist that he‘s Vice-President of the EAPM (European Association of Psychosomatic Medicine) and President-Elect of the Academy of Consultation-Liaison Psychiatry (AC-LP) which used to be the American ‘Academy of Psychosomatic Medicine’, or perhaps she forgot to report it or ran out of space. Have these organizations really removed ME/CFS from their psychosomatic portfolio? I doubt it. I’m inclined to think that rather than moving on from ME/CFS research, Sharpe has been busy branching out.
Very interesting Couch Turnip (love the title :)) I had never heard of medically unexplained symptoms (MUS) before. What a trap that is for “invisible diseases” that produce a lot of hard to explain or quantify symptoms like fatigue and pain.
Did you see that Uganda researchers tried to explain away a parasite caused disease called Nodding Syndrome (which on brain images shows clear deterioration and often results in death) as a kind of psychological disorder?
http://simmaronresearch.com/2019/04/nath-chronic-fatigue-syndrome-east-african-disease-model/
Belief systems can be astonishingly strong things.
The idea for the title came from this turnip twaddle – https://pn.bmj.com/content/17/5/417 !
I came across Nodding Syndrome a while ago and wrote to a researcher involved with it to offer some thoughts on possible non-psychological causes. It’s good news if they’ve managed to sort it out now.
Couch, I like your thoughts on MUS. I wonder what your thoughts were on FND, functional neurological disorder which I have just been diagnosed with?
I was diagnosed with ME/CFS in 2015 but privately. And despite this dr having worked with our counties consultant on CFS, he refuses to diagnose me with ME. He did however, diagnose me with fibromyalgia back in October 2012 privately.
At the beginning of my consultation with my neurologist he enlightened me that the ME/CFS consultant won’t diagnose me with ME as this consultant whom is in charge of all our counties CFS/ME services doesn’t believe that someone with fibromyalgia can also have ME at the same time. Such a shame he didn’t enlighten me himself on his visit to my home In January this year. Even more of a shame I did not ask that question myself, why won’t you diagnose me.
I digress, apologies, but FND seems a bit like MUS although there is a charity already supporting this diagnosis. It the symptoms under FND are under the symptoms of ME. So, do I have both diagnoses or just one, and if so, which one?
Got to laugh ? or I’d shoot myself with despair!
Fiona, I’m assuming that you’re in the UK?
I was told by a UK neurologist that I likely had ME/CFS, then by another that I had FND. The FND one told me to look up the neurosymptoms.org website and wrote to my GP saying that he thought I had MUS. When this happened, a few years ago, I smelled a rat and decided to look into MUS, FND, and ME/CFS for myself, and I’ve spent a considerable amount of time researching it. It’s only natural for patients to seek a diagnosis, but I suspect most people would want it to fit with their symptoms and not serve as a means of excluding them from good care.
With respect to fibromyalgia, I think it used to be thrown in the same psychosomatic bag, but I’m not entirely sure how it’s viewed now. It seems to have been removed from the IAPT category of MUS and placed with ‘long term conditions’ under ‘chronic pain’. It makes little difference though, because patients with long term conditions are being targeted to receive CBT just as MUS patients are (including patients with ME/CFS). This is being done to reduce healthcare costs by restricting referrals and investigations, so cutting the NHS’s secondary care budget by diverting patients towards cheaper ‘care in the community’ (including telephone and computer-based CBT).
With respect to FND and MUS, at least some neurologists and FND researchers seem happy to conflate the two when it suits them to. Recently the FND Action charity (is this the charity you were referring to?) tweeted that the PACE trial had ‘nothing to do’ with them – https://twitter.com/FNDAction/status/1118165287285739521 , but one of the PACE trial authors, Trudie Chalder, is on their Medical Advisory Board. She is currently in the process of completing the PRINCE trials (primary and secondary) into Persistent Physical Symptoms/’PPS’ (another name for MUS). These trials are worth keeping an eye on. NB The PRINCE secondary trial includes giving CBT to PPS neurology and fibromyalgia patients. Also on the Board are Jon Stone and Alan Carson, whose low figures for the misdiagnosis rates of FND have been touted by others as the misdiagnosis rates applicable to MUS. I’m not going to tell you not to trust these people, but I would say it’s worth casting an eye over the many papers by Stone, Carson and Michael Sharpe on MUS, FND, conversion disorders and/or hysteria to help you make your own mind up.
These papers may also be of interest –
functional symptoms and signs in neurology: assessment … – The BMJ
and
[PDF]
Functional Neurological Symptoms in North East … – FND Action
I wish you all the best.
Thanks for the information Couch Turnip. Yes, I’m in the UK.
The neurologist made a good case for FND stating that it is our central nervous system in dysfunction and the way to unscramble the nerves is through psychotherapy. So, I did smile when he said he’d refer me to a psychologist who specialises in FND as she has had some good results. I did tell him I am very sceptical but I’ll try to go to,at least one appointment. And if I get a whiff of shaming or blaming me for my illness I’ll be out of there – fast! ?
It just astounds me that our medical system, if presented with a patient whose symptoms have no medical cause from the tests they’ve run, simply can’t say say, they don’t know! Why they are continually making up terms to put us in a category so that we are given a label to appease us is beyond me.
The term MUS is laughable really. They may as well call it Mary Poppins syndrome for any good these titles have!
CBT is constantly the ‘go to’ prescription for anything medically unexplained! I wonder if the area of psychiatry is low on patient numbers or something?
I am uncertain if my referral to the psychologist is for CBT or not. I am open minded enough to agree that there may well be something going on in the brain that are causing these symptoms. But if this is a theory, which I could believe, then why isnt the scientific field analysing this theory? It seems that the psychiatry has decided for itself that they are the solution. And if they are, then why isn’t there more proof of this?
‘We’, the ME/CFS patient community are very anti CBT, but what happens if we are missing out on something here? I’m in no way, shape or form am agreeing with the PACE trial. That’s a different arena. But what if there is something wrong with our CNS? What if viruses, stress etc all the known causes of ME have triggered the CNS into some sort of shut down? I find it a reasonable hypothesis but I doubt CBT is the solution. But again, where is the science to back such theories. Why is my neurologist referring me to a psychologist when there is no scientific proof that a dysfunctional nervous system is to blame for me illness. He called it neuropsychology. Mmmmm…….well time will tell I suppose.
All I know is, that whatever is my correct label, I am becoming more ill as time goes on. More different symptoms are arising, the latest being neuralgia in the last 3 weeks. Having said that, the biggest beast is post exertional malaise as a result of expending too much energy. Is my incorrect style of pacing decreasing my quality of life long term? But remaining bed bound in order to prevent further deterioration of health is definitely not my choice of tactics!
What a minefield all this is! If the field of psychiatry are so convinced that a patients unexplained medical symptoms will be cured by CBT or any other method then let us see the evidence. If patients see reliable evidence that ‘talking therapies’ are the way to go then maybe we will be less reluctant to give them a try. But personally, I doubt it.
Apologies again Couch, as I seem to have gone down a rabbit hole from the beginning of my reply! Thanks again!
It would be more convincing if they didn’t start their research papers by saying how much these illnesses cost the NHS so implying that their treatments could save the NHS £billions. Never trust a salesman, especially not one selling snake oil.
When the neurologist I saw mentioned a ‘software’ dysfunction to me that kind of made sense, because surely the ‘software’ is the biochemistry that goes on in the body, rather than the anatomical ‘hardware’. But then it became clear to me that wasn’t what they meant at all. I wonder how much biochemistry and physiology these people know and understand. Did they just scrape through their exams at medical school?
Are you aware that Jon Stone has recently reported that there seems to be a ‘hardware’ problem too? Yet he can’t seem to bring himself to admit that he might have been wrong, and appears to me to be still clinging to the ‘software’ i.e. psych issues as being the most likely causal factor which could then cause the ‘hardware’ to change. Hmmm. https://www.youtube.com/watch?v=sloHkUy7pIs
I hope your appointment goes well. It might be worth asking them about the ‘hardware’ problem and how that fits?
David Tuller is exactly the kind of people that we need in CFS. Someone who engage in hard science without indulging in beliefs or theories. And biopsychosocial model is a belief, not a science. It may have some limited use in psychology, but some psychologists are going gung-ho with it and calling everything they can’t explain biopsychosocial.
Science is hard. I get that everyday when I try to analyze my own data. It is really no place for amateurs.
The default in the medical world IS biopsychosocial. When you have limited science and a complicated disease the default is always going to tend to that. Thankfully we have dedicated people like David who a) know what they are talking about, b) can’t be intimidated, c) basically have the facts on their side and d) are not going to stand for shoddy science.
I believe we will have more David’s helping us over time. There’s Miriam Tucker, another journalist who just penned her second excellent piece on the NIH Conference. Her articles are going straight to doctors and health professionals. They are a huge help and good on Medscape – the most trusted medical information in the world – for funding her articles.
https://www.medscape.com/viewarticle/911906
I had a very sharp decline in health from being able to walk once a day 2 km with a stop in the middle before CBT/GET “therapy” to needing a wheelchair for distances beyond 25 meters afterwards. I’d like to see justice too, but we should be careful with legal action and getting more then we wish for.
Suing for both convictions and damages may threaten many individuals and organizations (bankruptcy). Many of these individuals and leading figures in these organizations are very smart, powerful and more then willing to fight to the end to not go under. Plenty of them have decades worth of experience settling scores in a covert way.
Their combined organizations have resources and power we can only dream of. I would not like to see these “researchers”, large academic institutions and hospitals, government departments and wealthy insurers pool their resources to set up a legal and “extra-legal” defense. Giving them the impression that they have no other option then to close their lines among each other and fight or go under might just trigger that.
Just suing one party to start with would not take this fear away. A big win against a major player opens the others for follow up suits and damages.
Possible legal actions:
* endlessly delaying the lawsuit
* endlessly appealing
* claiming conflicting jurisdiction
* starting widespread legal action against doctors researching and treating ME patients based on doubtful (that these doctors would do anything wrong) claims. Regardless of value of such claims, it would make doctors and researchers even more careful, tie up their resources and further reduce ME research funding. Can be done covert too.
* “inform” the general public that a win in the case would expose insurers to such high claim that they might have to file for bankruptcy and showing emotional videos going with it how that would take away Joe the cripple’s disability benefits and make him homeless.
* “inform” the general public how much that both damage claims and the need to pay life long disability benefits to “people that could be perfectly helped by a safe, cheap and effect therapy called CBT/GET if they were only willing to do the effort” would hike their medical insurance costs.
* Seeing how divisive the medical insurance cost versus coverage topic currently is in the US (not taking any side here, just stating that it is very divisive), that would be an effective tactic to make about any jury undecided and hence dodge conviction/claims.
* “inform” the public more effective with targeted online advertisement based on personal profiles and creating a slew of “non profit patients organizations” to cause confusion much like some big internet companies recently set up “independent non profit privacy organizations” that defend anything but privacy.
* removal of doctors/hospitals that disagree from lists of refunded caregivers by major insurers
* …
I’m not against appropriate legal action. Just stating that thinking it through first, evaluating possible consequences, comparing to alternatives might be the smart thing to do. If we don’t do, the opposing site may gladly take advantage of it.
Now I need at the very least to give some “first shot” alternative.
David Tuller did and does excellent work. We own plenty to him and I hope he gets sufficient support to carry on. He exposed the claims that CBT/GET is effective to be very dubious at least and the research full of problems. That created new hope to counter the blanket use of CBT/GET. But that does not mean this is the best angle for legal action.
We need to look at our strengths and weaknesses and look at those of the defenses.
Our strengths (of use in my reasoning):
* We start to have multiple improving (under development) biological markers that can distinguish between patients and non patients; Research on them is published in absolute top journals Nature and Science.
* Some of these markers are correlating with disease severity.
Our weaknesses:
* We are depleted of both resources, energy and ability to take action.
* We depend for so much on others for survival, support and care. That would trying very hard to take away support from other people for us a prime battleground for those who wish to play it dirty and weaken our legal battle.
Their strengths:
* Vast resources including money, lawyers, very smart and strategic people, access to politics, a very large network…
* A “common cause” may unite them in “their struggle for survival” against the threat we ME patients could impose on them.
* They can play endless rounds of “responsibility is spread over many organizations”.
Their weaknesses:
* Very few of those actors would have anything to gain in such battle other then fending of big personal and financial damage.
* Many of these actors would take the first opportunity to leave the battlefield if they were convinced that they could better dodge the damage by doing so then when remaining fighting.
* Quit some of these actors would not hesitate to put the full burden on other actors and “not hindering” access to information, methods or resources that could help patient advocates to shift the blame and damage away from them to other actors.
Now let us take a look at the possible case itself:
* Going for fraud claims would be *very* hard as intent would have to be proven beyond any reasonable doubt. In many cases such can only be done by having access to written and verifiable statements that leave no doubt on the actual intent. Like mails that are guaranteed from them stating “change the data, fiddle with it, delete data that is bad to our cause, cheat and do other illegal stuff”. Having them changed protocol mid-research and every change being beneficial to them is unlikely to be considered “beyond reasonable doubt”. It could be poor judgement, an honest mistake…
Any jury or the many judges in each case and endless row of appeals might be influenced by a “think of the consequences of agreeing with the fraud claim (wouldn’t want honest disabled people to lose their benefits, would you?)” and “if they only would be willing to do the effort to try this safe and effective therapy” campaign.
* There is however a remarkably unexplored angle: the responsibility to make a medical therapy safe by having a robust system in place for checking on and following up on severe side effects.
– With any drug approval, there must be a rigorous system in place to catch any side effects and all side effects must be reported before a drug can be considered safe for use and release to the general public. Describing and using drugs that has not followed this procedure is a legal offense. Even using drugs that has been tested for all side effects can not be repurposed for other use. Think of the many cases worldwide where doctors treating ME are suspended for using drugs that are approved for disease X to treat ME.
-> We may take a page out of the same play book. If nothing in medical practice may be used that has not been proven to be effective and safe for treating that specific disease or it would be illegal practicing of medicine, then very likely some legislation on some parts of the world would make describing CBT/GET for treating ME an illegal action that could lead to suspension of doctors.
Even where it is not exactly illegal, we could argue to incorporate new legal standards to make it so for any medical treatment including CBT/GET.
If other practices like revalidation therapies and physical therapies need to undergo a safety and side effect analysis before approval just as much as drugs, we could easily argue that there is no reason for psychological research to be excluded if it involved prescribing physical revalidation therapy (GET).
Even if we can’t do that, if I recall correctly then some of the researchers claimed publicly that CBT/GET was both beneficial and HARMLESS. Public records are available on that. It may even have appeared in some papers of them, I don’t know.
Now to my knowledge there have been no fact or data based analysis nor a procedure being incorporated in the PACE trial able to prove such claims. Stating false or completely unsubstantiated or unresearched claims about safety of a medical treatment is a criminal offense as far as I know in many countries and at the very least a professional and deontologic mistake sufficient for firing the researcher in place and withdrawing the related work.
Even better, it could allow plenty of involved actors to use such conviction as a shield. Like government organizations, insurers, universities and hospitals to find their best spokesperson that can put up a straight face plus a surprising look and claim “Really, they claimed this therapy was safe without studying it or following appropriate protocols? We are shocked, utmost shocked! If only we had known, we wouldn’t have allowed us to be used (“victims”) by these fraudulent (the safe part, not the effectiveness part) claims…
While such behavior would leave a bitter taste in the mount, I’d rather have near all of them join us in our ideas of “unsafe or not proven to be safe = illegal therapy” than have them against us.
I’d prefer good insurance for all insured ME patients from now on over a few patients getting a big financial compensation (after legal fees) after a decade of legal battle and ME in large being set back due to the joint fight against patients.
Reanalysis of old research, in depth statistical relevant patient data involved in research programs or “treatment” in the past… could strengthen the “unsafe” argument. Organizations seeing our arguments about unproven safety or even proven unsafety gaining strength might switch camps and allow for scientific outsiders to put into place procedures to check the safety of their current CBT/GET programs for ME patients (in order to check if they too are the “victims” of bogus claims made by the PACE researchers and above all to avoid legal liability).
That is but one idea to make our fight more efficient: force them to prove their treatments are safe. Not being effective is apparently not sufficient reason to ban blanket treatment of ME patients with CBT/GET.
My bad,
After reading the PACE trial again, I saw they did some safety analysis and found both no more severe side effects in the groups getting CBT and GET then in the other two groups and find very few severe (side) effects in a group of about 640 patients over one years time.
Where on earth did they find this group of about 640 patients that had so few severe PEMs, severe temporal weaknesses that left them unable to stand nor walk nor speak, strong convulsions…? Did they have any ME patients at all in their groups?
I’ll stop ranting on this topic and withdraw to the reality I live in.
First, and I assume it is likely that you will read this Mr. Tuller, a big thank you for all of your investigative reporting in this often neglected area!
I am pleased to know that you are actually a kind of ‘neighbor’ as I live in Albany, just blocks away from the Berkeley boundary. Love that Berkeley spirit!
Being published in the Lancet is not unlike a celebrity sex tape that has been leaked to the media–almost impossible to eradicate as it will replicate like rabbits across social media (or in this case other medical websites).
Rather than legal action, my hope is that an accurate lab test to diagnose ME/CFS, and then perhaps more progress in verifiable treatment strategies (for various sub-groups), will be more helpful to undo the damage of the PACE study than any law suit. We need more information!
As Cort pointed out, the PACE recommendations CAN have a positive influence as the patient IS both body and mind, but to promote them as the definitive treatment is wrong. There is much in medicine that we do not understand, although it is taught as if we do. Thank you again Mr. Tuller for pointing out nature is much more nuanced than that, and for researchers not to make stuff up before the facts.
Thanks for the laugh!
“Being published in the Lancet is not unlike a celebrity sex tape that has been leaked to the media–almost impossible to eradicate as it will replicate like rabbits across social media (or in this case other medical websites).”
In my opinion the PACE recommendations can NOT have ANY positive influence.
Both good well thought out body and mind work and good well thought out exercise programs can have beneficial effects for SOME patients. But then they have to be tailored to individual patient needs and health evolution of each patient needs to be carefully monitored by a team of ME specialists.
Even for a single patient, adapting the used techniques on a time to time basis must be done to offer the best set of techniques or a temporary suspension of their use in order to cope with the very fluctuating nature of ME disease.
Both Wesley and the PACE authors are in my opinion the single biggest hindrance of better use of those techniques in ME and fibro.
They shamelessly designed their experiments around dropping patients data of those that get worse. When it was apparent that was not sufficient they shamelessly changed what they measured halfway the experiment. When that was not sufficient they shamelessly abused statistics in such a way that it is faulty in major ways as has been confirmed by the biggest statistical organization in the world.
Even then, using all these carefully designed flaws and errors, a follow up research could not demonstrate any better results compared to not having !their! (as opposed to potentially better) CBT/GET approach.
But what is far more worse is that they willfully ignored to have any mechanism to check for severe side effects. It even resembles a lot that they did design their experiments around avoiding being confronted by them. How can they not have seen patients suffering a severe decline with a sample group of thousands of patients?
Even if patients surveys are only slightly accurate, reported double digit percentages of very severe side effects like getting a very strong relapse the patient never recovers from or ending up in a wheelchair or being bed bound when one was fairly independent before the therapy are hard to ignore when one does the least bit of effort to have a working system in place to check for potential side effects.
Would one accept that a therapy for asthma puts both thousands upon thousands of individual patients in the wheelchair and leaves double digit patients far worse off then before after having a therapy where the single biggest proof of it’s efficacy is the shoddiest piece of medical research in a very long time and no single effort worldwide has been done to asses the therapies safety?
Why is it the medical community is so eager to ban homeopathy out off medicine as it is unproven where the biggest harm comes from patients not seeking better treatments while the efficacy of the PACE recommended therapy is equally unproven, guides patients away from seeking better therapies (like the opposite therapy called PACING) and the only way to not see the massive damage the therapy does to a great percentage of patients is to organize the therapy in such way that patients with averse effects drop out without leaving a single paper trail? Why is it that such therapy is not only not fought hand over fist against by the medical community but actively promoted and prescribed at a large scale?
It is the trail of massive damage that Wesley, PACE and likewise leave in their wake and the religious enforcement of their believes that is the SINGLE most hindrance of developing and using better body and mind and exercising techniques to help alleviate, not heal, ME and fibro patients suffering.
It seems like the puzzle of ME/CFS will never be solved if we keep putting all the cases in the same basket as if they were the same condition. Some cases started directly after a viral type illness; others came on slowly; some are associated with a toxic exposure; some are part of a cluster; others are individual. Some patients have reported they feel like they have been poisoned. Some became ill after surgery or other stressful event. Treatment is just as confusing. Some patients have been helped by anti-virals; others have not. Some have reported cures from yoga and mind-body work. Others not. There is, however, a relatively inexpensive way to help figure this out. The patient community could set up a registry just like our organization did for birth defects when we developed the National Birth Defect Registry. With the collaboration of seven scientists, we created a comprehensive questionnaire that collects data on line. We now have 10,000 cases. It is remarkable what you can discover collecting and then querying data in a comprehensive inter-relational data base.
Firstly, thank you to David Tuller for doing so much on our behalf, and to Cort for writing up this great interview.
Secondly, I am actually optimistic about the future of labels like MUS. We will (eventually) get to the bottom of ME, and the process of doing so will be available to assist in investigating other challenging chronic diseases. The technologies and models will readily transfer; and when new syndromes are described, people suffering from them will be able to arm themselves against unhelpful labels by reading our history.
It will be too late for some of us – I’m 61 now, and may not benefit very much from current research – but I really believe there’s every hope for younger patients.
Good point. The more that medical technology and science improves the less the MUS folks will have to chew on.
Shortly after seeing this, a link to the Lancet article showed up in my inbox – has it always been Open Source? I doubt it.
I do not know. I just discovered it was open source when I looked at it recently.
This whole thing reminds me of Andrew Wakefield’s fraudulent research when he concluded that vaccines cause autism. That was in 1998! That study was proven fraudulent but there are millions of people that still believe it. But these are doctors that know (or should know) how to conduct and analyse data from a research study. I think doctors just want to hear about treatments that are fast and easy and dismiss the patient.
The huge medical fraud that is going on in the matter of “covid19” takes bravery to report. I am always grateful for investigative journalists which are rare indeed at the time of the one media narrative( Orwellian).
https://notpublicaddress.wordpress.com/2020/10/07/a-summary-about-the-testing/
https://notpublicaddress.wordpress.com/2021/01/14/the-world-was-brought-its-knees-in-2020-by-the-banksters-global-authoritys-1st-virtual-virus-plundermic/
Sophierouse @gmail.com