

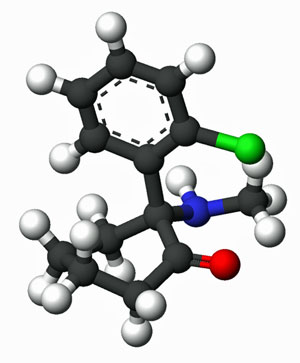
For years, ketamine was known for its use as an anesthetic or as a recreational drug. Its ability to provide quick and safe sedation saved many lives during the Vietnam war and is still the preferred anesthetic in battlefield situations. It can be used to induce a kind of trance-like state which wipes away pain, and it’s been used, in higher doses when taken orally, as a party drug (“Special K”) and hallucinogen. (It has structural similarities to PCP.)
Ketamine may turn out to be more than an anesthesia drug or an illegal means of getting high. While more research needs to be done, recent studies point to its ability to relieve treatment-resistant depression, act as an anti-suicide drug, possibly reduce pain, and even assist in PTSD.
New Approach to Depression
“In slightly more than a decade, the emergence of ketamine’s rapid antidepressant effects has been viewed by some experts in the field as arguably the most important psychiatric discovery in half a century.“ Niciu et al.
The FDA panel’s recent overwhelmingly positive (14-2) vote and the subsequent approval of a ketamine drug nasal spray called Spravato to treat treatment-resistant depression brought to market the first fundamentally new approach to depression in decades. Spravato was tested in people with severe depression who have not been amenable to other treatments. (Only people who have tried and failed two other depression drugs are eligible for Spravato.)
The need for more effective antidepressants is large. About a third of depressed patients do not get relief, and about 50% more stop their drugs because of side effects or other issues. Plus, the current crop of antidepressant drugs typically take weeks to months to take effect, and withdrawing from the drugs can produce major problems in some. (Check out this New Yorker article for more on that.) The possibility of a new, fast-acting, antidepressant drug is enticing indeed.
With the advent of Spravato, instead of paying out of pocket for IV ketamine infusions, some people with depression will be able to get their ketamine treatments reimbursed by insurance. (They will need it – the drug will reportedly cost several thousand dollars for the first month.)
Ketamine infusions certainly fit the bill for one woman with treatment-resistant depression who’d unsuccessfully tried dozens of drugs. She described the positive mind-altering changes she experienced while on ketamine:
“It feels like your body rises up, like you’re on a very peaceful roller coaster, and you’re riding a wave into a different dimension… During treatments, I feel like I learn about myself. Because I feel safe and positive, I’m able to confront things that I typically fear or that give me anxiety, like death. Because I’m able to face negative things during treatment, I’m better able to face them and cope with them outside treatment.
“After the first treatment, I felt a weight lift off me within hours. After three to four treatments, I could hear birds chirping and see vibrant colors again; I could walk out of the house without making a million excuses for why I couldn’t. I had hope again. It was the first time in 20 years that I’d felt relief. And the results just kept getting better and better with each treatment.”
Another young man’s inconsolable grief was rapidly ameliorated by ketamine. The death of his young wife left him so grief-stricken that he refused food, spoke in a tiny voice, broke out in crying spells, was borderline catatonic and ultimately ended up in the hospital.
After some brief hallucinations upon receiving ketamine, he began to communicate, was cheerful and started taking food orally. Three months later he was continuing to do well.
Studies are underway to identify how ketamine does what it does in depression. Ketamine, a glutaminergic enhancer, got its start when studies in the 1990’s began indicating that glutaminergic neurotransmission was affected in depression.

Ketamine appears to be able to restore parts of the nerves destroyed by chronic stress in depression…
Ketamine prods the brain into producing more glutamate, an excitatory neurotransmitter that several studies suggest is elevated in fibromyalgia, depression, and neurodegenerative diseases. It’s not clear why ketamine might be helpful in diseases like fibromyalgia and depression, but researchers have some ideas.
One hypothesis suggests that ketamine triggers a quick burst of glutamate which, via activation of the mTOR pathway, stimulates the formation of new synapses. Interestingly, only lower doses of the drug appear to do this.
A study recently published in Science using a new microscopic imaging technique found that ketamine infusions restored the small “dendritic spines” which allow signals to pass to and from the dendrites found on neurons in the brain. Ketamine, at least temporarily, restored the connectivity between the prefrontal cortex and other parts of the brain.
It’s interesting that dramatic oscillations in glucocorticoid levels (in particular high levels of glucocorticoids, which some believe may occur early in ME/CFS) are able to eliminate these spines, thus hampering the prefrontal cortex’s ability to communicate to other parts of the brain.
The authors noted that the loss of these spine-like projections on the dendrites – the small branches coming off the main nerve cells – may also be occurring in the hippocampus, nucleus accumbens and amygdala, all of which are possibly implicated in fibromyalgia and ME/CFS.
It’s still very early, but the ability of ketamine to increase neuroplasticity in the brain and restore broken connections suggests, as one MD on Medpage noted, that it could have wide applicability, including in diseases like Parkinson’s.
“If we are seeing these changes in neuroplasticity and these changes in the way that the neurons are talking to each other and the way the circuits in the brain are actually talking to each other, this could have wide variability.” Dr. Sanacora
The down side with ketamine infusions is that half of the new dendritic spines are immediately lost when the treatment is stopped. It’s possible, though, that once those spines are renewed, other therapies, including neurostimulatory techniques like rTMS, may be able sustain them.
The woman who got the great results from ketamine – she just keeps doing the infusions.
Ketamine, Fibromyalgia and Pain
The evidence for the use of ketamine in pain has been mixed. One large study found that half of headache participants experienced pain relief lasting weeks. A recent meta-analysis found “robust evidence” for the use of ketamine for relieving pain, but noted that results were “modest” – about a 25% reduction in pain. They suggested that ketamine was probably most useful for people who cannot use opioids or other pain medications or who need particularly rapid relief.
Ketamine use was considered in fibromyalgia as far back as 1995 when a study reported IV ketamine decreased pain intensity and increased endurance in FM patients. A 1997 study reported pain reductions in FM and a 2000 study suggested it might be getting at core issues in the disease.
A 2002 review recommended ketamine be used in combination with low-dose opioids in FM. A small 2007 fibromyalgia study found an approximately two-thirds response rate and suggested that ketamine increased blood flow to the brain. A 2011 fibromyalgia study using S(+)-ketamine found that about a third of FM patients immediately experienced a 50% reduction in pain, but the effects did not last.
Ginerva Liptan, an MD focused on fibromyalgia called IV ketamine for pain experimental but noted that “it could be big”. Dr. Podell, an ME/CFS/FM doctor, reported that ketamine reduced pain in about 50% of his fibromyalgia patients.
Ketamine was also a key component of Dr. Jay Goldstein’s (now retired) “resurrection cocktail for chronic fatigue syndrome’. (The resurrection cocktail often included ascorbate, lidocaine and thyrotropin-releasing hormone. Goldstein administered Ketamine intravenously or through a gel.
Ketamine, interestingly, also can have positive circulatory effects. Subanesthetic doses of s-ketamine actually increased cerebral blood flows in one study. Reduced cerebral blood flows appear to be universally present throughout the different kinds of orthostatic intolerance.
Check out one person diagnosed with severe back problems, fibromyalgia, chronic fatigue syndrome, chronic pain response syndrome and bi-polar depression/PTSD for whom ketamine was a godsend.
The Wild, Wild West
Because ketamine is a generic drug, its use is not well-regulated by the FDA. Over the past ten years, the number of centers using intravenous (IV) ketamine infusions to treat chronic pain and/or depression has skyrocketed. Some, like the Cleveland Clinic, Yale University, the University of California at San Diego, and the Mayo Clinic are reputable; others are not.
The kind of wild west approach to ketamine infusions prompted the American Society of Regional Anesthesia and Pain Medicine, the American Academy of Pain Medicine, and the American Society of Anesthesiologists to produce the first ever guidelines for the use of ketamine in chronic pain.
The groups concluded that, “Evidence supports the use of ketamine for chronic pain,” but described the many small, uncontrolled, unblinded (or improperly blinded) studies. A better understanding of dosing is needed. Larger, more rigorous studies (something we frequently hear) are needed.
The need for better studies is more acute in the case of ketamine because it’s being used in so many clinics, and the introduction of pill and nasal forms of the drug will undoubtedly increase its popularity.
It’s important to note that, while studies provide the more rigorous evidence for or against treatment, they’re just one part of a treatment decision-making process.
Florinef (fludrocortisone acetate) provides an excellent example. It failed in not one but two ME/CFS trials, including one 100 person, double-blinded, placebo-controlled trial which ended up being published in the prestigious JAMA journal. No doctor reading the results of those trials would ever prescribe Florinef for their ME/CFS patients.
Yet Peter Rowe, the leader of the JAMA trial, uses the drug regularly. Rowe later pointed out that the trial had a number of significant issues. The patients in the trial did not increase their sodium intake – a key part of Rowe’s protocol – and one which could have boosted the drug’s effects. The dose (0.1 mg/day) was also set low in order to ensure that the patients didn’t know if they were taking a placebo or the actual drug. Most of the patients in the study had also had ME/CFS for longer than 3 years, and Rowe apparently has found that shorter duration patients tend to do better.
The ketamine studies face similar issues. They tend to assess low amounts of the drug in single-doses. Clinics, on the other hand, often use higher doses repeated over time.
Studies can provide powerful assessments of drugs, but they often take place in a kind of artificial vacuum that does not reflect the clinical environment. They provide an important piece, but only one piece, of the puzzle regarding treatments – and can be misleading. Andrew Miller PhD, for instance, believes that ketamine may be especially useful in depressed patients with increased inflammation and that anti-inflammatory drugs may be useful in sustaining the response to ketamine. Miller also believes ketamine may be down regulating the activity of the kynurenine which some believe is upregulated in ME/CFS.
Other NMDAR-Affecting Drugs
Because the NMDAR (N-methyl-d-aspartate) receptors are involved in the transmission of sensory and pain signals, they’ve been considered possible drug targets for FM and other pain disorders. Ketamine is the strongest NMDAR receptor antagonist on the market. Two other NMDAR antagonists, memantine and dextromethorphan, have, however, been assessed in FM.
Dextromethorphan, which has milder NMDAR blocking properties (and is found in cough syrup), has shown some efficacy in a subset of FM patients. The conclusion of the 2005 study proved the point that drugs often aren’t taken in isolation and their effectiveness shouldn’t be judged solely in isolation.
“Our results provide evidence that dextromethorphan could be clinically effective for FM, particularly in combination with other agents that act peripherally to reduce sensitization of nociceptors,” Staud 2005
As with ketamine, at high doses, dextromethorphan can make one decidedly loopy (it’s another dissociative agent). Jarred Younger is currently trialing dextromethorphan – a potential microglial inhibiting agent – in fibromyalgia. Like LDN, Younger’s planning to use it in low doses (30 mg/day). Unlike LDN, dextromethorphan has the added benefit of being safe for people using opioids.
Memantine, another type of NMDAR blocker, has shown modest efficacy in FM and chronic pain.
A review of NMDAR blockers in FM concluded that, despite the role the NMDAR system appears to play, results have not been particularly good. Studies of NMDAR blockers, however, tend to be small, of short duration, and employ a limited range of doses; i.e., they’re the typical, poorly done drug trials that are common, and more work is needed to truly assess their effectiveness.
The Prefrontal Cortex Connection in Fibromyalgia and ME/CFS
Ketamine is also the first drug approved for depression that appears to be able to restore glutamate neurotransmission in the prefrontal cortex. That’s intriguing, given that the prefrontal cortex is the seat of “executive functioning“. Executive functioning refers to a wide variety of behaviors (concentration, organization, judgement, reasoning, decision-making, creativity, emotional regulation, social–relational abilities, and abstract thinking), some of which are impaired in both fibromyalgia and ME/CFS.
It’s possible that cognition is not the end of the story with the prefrontal cortex and ME/CFS and FM. The Japanese believe that damage to the prefrontal cortex in chronic fatigue syndrome is contributing to the problems with movement and exercise as well. This is because one part of the prefrontal cortex connects to and regulates parts of the brain which generate movement (premotor cortex, supplementary motor area, cerebellum, and basal ganglia.)
That’s a potentially interesting connection given that ketamine so substantially alleviated fatigue in patients with bipolar depression, that they suggested that ketamine and other glutamate affecting drugs be tried in other fatiguing disorders. They apparently suggested this because ketamine’s fatigue effects were not dependent on its ability to relieve depression.
Ketamine rapidly improved fatigue relative to placebo in a group of individuals with treatment-resistant bipolar depression. NMDAR is a glutamate receptor; hence, glutamate may represent a valuable target to study the clinical efficacy of new anti-fatigue approaches in multiple disorders.
Evolving Field
It should be emphasized that ketamine is an evolving field. While known primarily as an NMDAR antagonist, ketamine also affects other brain pathways involved in pain and mood (nicotinic and muscarinic cholinergic receptors, sodium/potassium channels, dopamine receptors, and others.)
Ketamine’s metabolites may offer more efficacy and fewer side effects and are an active area of exploration. A 2019 study found that a ketamine metabolite had superior acute and chronic pain reducing properties in laboratory animals, and a 2018 report indicated that two ketamine derivatives lasted longer, provided better effects, and produced fewer side effects than the current drug.
Conclusion
There is still much to learn about ketamine, including dosing, which patients benefit and why, and the very real concern regarding its long-term effects. As yet, the evidence for ketamine’s effectiveness is greater for depression (where ketamine appears to be able to spur the development of new synapses that counteract the effects of chronic stress) than for pain. The FDA’s recent approval of the first ketamine-derived drug, Spravato (esketamine) brings the first entirely new approach to depression in decades to the market.
In fact, given the NMDAR’s central role in regulating pain levels, why ketamine and similar drugs have not proven more effective with pain seems puzzling. Studies using single, low dose protocols that are out of sync with clinical use may (or may not) provide one answer to that question.
In the meantime, work on producing more potent forms of ketamine are underway, and several potential metabolites which may boost ketamine’s effectiveness and duration have been identified. Dextromethorphan, another NMDAR antagonist, is being tested in fibromyalgia.
- Next up – the FDA approves a new drug which may help with the consequences of having ME/CFS and FM.
Resources
- Check out Health Rising’s Fibromyalgia and ME/CFS Ketamine Resource Center for more
- Ketamine and Fibromyalgia
- The Ketamine Advocacy Network
- List of U.S. ketamine providers for depression







My niece was diagnosed many years ago with Fibromyalgia. She and her two young children also have a MTHFR genetic mutation. A couple of weeks ago her youngest child, eight years old, ended up in the emergency room to stitch up a relatively small gash in his head. The doctor gave him Ketamine so he could sedate him to put the stitches in. He stopped breathing twice and had to be resuscitated as well as having to have his throat suctioned. He’s okay but it took a long time to come out of it. He now has to wear a medic alert bracelet warning about the sedation. This may be a miracle drug for some, but it can also be deadly!
Whoa. Ketamine is actually commonly used for “Anesthesia in children, as the sole anesthetic for minor procedures” Wikipedia also states that “it’s sometimes possible to perform ketamine anesthesia without protective measures to the airways and is considered relatively safe because protective airway reflexes are preserved and it’s used as a bronchodilator in the treatment of severe asthma.”
One of Ketamine’s possible side effects, though, is…
“Airway obstruction, cessation of breathing, increased bronchial secretions, reduced effort to breathe, spasm of the vocal cords (larynx)”
Paul Cheney is currently recommending ketamine infusions in some ME/CFS patients, at least those who can afford it and are willing to experiment. I don’t recall what dose he is recommending, but I think it is lower than the dose most private clinics use for treatment-resistant depression. He has done echocardiograms on a few patients after their ketamine infusions and is finding that their cardiac output increases post-infusion from sub-normal to low-normal. One notable observation is that the improvement in cardiac output appears to be sustained even when measured while patients are upright, suggesting ketamine helps with orthostatic intolerance. I don’t think he believes ketamine will be a miracle cure, but Cheney is finding that the few patients who have tried it improve clinically at least temporarily, with the main benefit being much improved sleep. The jury is still out on whether the clinical improvement will be sustained. With ME/CFS, my guess is it won’t be.
I don’t think ketamine is ready for prime time – at least not for those who are not depressed and cannot afford the infusions – but it’s ability to help some with treatment resistant depression, activate the prefrontal cortex, reduce pain in some, perhaps even reduce fatigue, and, interestingly, increase cerebral blood flows (orthostatic intolerance) certainly make it a fascinating drug. Not many drugs can hit so many points. Ketamine affects more than glutamate – it also affects dopamine and serotonin. Something is going on there that more study will hopefully bear out.
I think Dopamine might be a dark horse factor in CFS. I remember that article you wrote on Andrew Miller and his brain scans of CFS patients that were measuring dopamine and clocking consistently low readings as opposed to controls. Andrew Miller also writes about Ketamine.
Ha! Andrew Miller – one of my favorite researchers. Thanks for the tip. Miller believes ketamine may be most effective in inflammation induced depression and that it may be dampening down the kynurenine pathway.
https://www.nature.com/articles/npp2013140#ref6
Hey mimimus – from my experience with only the maintenance dose of generic ketamine, I saw a significant improvement of all of my ME/CFS symptoms, including pain, sleep quality, fatigue, and orthostatic intolerance/POTS. The constant feeling of being “sick and tired of being sick and tired” also lifted, albeit temporarily. The effects do not last long at all. My instructions were to use it 2-3 times per week, but a daily or twice daily dose would’ve been much better. I cannot understand how infusion clinics are able to charge exorbitant costs in the thousands for such an inexpensive drug with short lasting effects.
Hi minimus – did you self-administer it? Did you have it in pill form? Are you still taking it? Sounds like it was something you tried and them stopped…Do you recall if it protected you from PEM if you had a good day and did more activity than usual? Thanks, cdax
Another great article, Cort. Thank you!
I can personally attest to the benefits of ketamine for chronic pain and fatigue. Several months ago, I finally found someone willing to prescribe a generic ketamine nasal spray to use 2-3 times per week. The effects were immediate – the pain and fatigue disappeared, and I felt an overall improved sense of well-being with no unwanted side effects other than nasal congestion due to the method of delivery. I never experienced hallucinations or dissociations, but it was truly life changing – it afforded me the ability to live a somewhat normal life again.
A little known secret is that open-minded doctors have been prescribing ketamine in the form of nasal sprays and lozenges for years. It’s a very inexpensive drug; a month’s supply costs around $40.
The problem with the FDA-approved Spravato, from my understanding, is that it’s more expensive and highly controlled and regulated – it’s kept on-site at a clinic, meaning patients twice a week must go in for an office visit where they’re monitored during use and for at least two hours after every single time – a near impossible feat for many of the folks who would benefit from the drug. Because its effects wear off quickly, you’re back to square one by the time you’re due to go into the clinic again and repeat the process. It’s a Catch-22. Prior to this, one could pick up the generic ketamine prescription at a pharmacy and use at home, just like any other medication. Now, most doctors are unwilling to prescribe the generic version given the FDA’s strict rules surrounding Spravato’s administration.
Once Spravato hit the market, my doctor refused to write another script and actually dropped me from his practice out of fear of retaliation, similar to what many of us experienced after the CDC released its opioid guidelines a couple of years ago, and this is not uncommon. I’ve not found anyone else willing to prescribe it since. In other words, the release of Spravato, along with the rise of prohibitively expensive infusion clinics, has actually limited the availability of generic ketamine for the population who benefited from it. I hope this soon changes and ketamine use becomes more mainstream and accessible. It’s a relatively inexpensive drug that offers immediate relief with no serious side effects.
Wow. It even helped with fatigue! I had no idea it was available in nasal and lozenge form at so cheap a price but on reflection, it does make sense. Because the drug has been around for decades and is a generic it makes sense that it could be produced cheaply.
What a sad outcome, though. Spravato is VERY expensive. I wonder if part of the problem is the Special K situation.
Thanks for all the info. Who would have thought that the first FDA approved ketamine drug would have negative effects?
Yes, it was immediate and life changing for me during that brief period of time that I had access to it. It was a kind of miracle drug, tackling all of my symptoms at once.
I also have MCAS and EDS, so I’m incredibly sensitive to most other medications, e.g., one dose of any SSRI/SNRI and I experience serotonin syndrome. So, I think it could be a great option for those who are suffering but cannot tolerate many drugs.
Woops, Sorry S.A. – I hadn’t seen this when I addressed questions to minimum that should have been addressed to you. This last post is extremely interesting. will look into it.. thanks for the info.
Yes, Cort, another great article. Thank you!
Hey cdax, yes, it was self-administered via nasal spray. It was used just like any other prescription nasal spray that you’d get from a pharmacy. The effects were immediate – the pain and fatigue instantly washed away to the point that I felt like getting up and getting out of the house. However, it doesn’t last very long. It would give me a few hours, at least, of semi-normalcy, but I was instructed to only use it 2-3 times per week. Had I been able to use it twice daily, I think I would’ve seen ’round the clock benefits. That’s part of my concern with Spravato’s nonsensical post-use two hour observation period – you benefit most from the drug within the first few hours. No chronically sick person wants to spend that brief window of feeling significantly better sitting in an uncomfortable chair surrounded by people in a fluorescent-lit medical waiting room.
The generic version is (or was) also available as lozenges.
The effects, for me, lasted long enough to prevent severe PEM. However, my PEM begins rather quickly, in the middle of the night after a trying day, when I was still benefiting from the drug. If my PEM was delayed a few days, like many here, I’d imagine it would’ve severely affected me, given the short lasting effects of ketamine.
It was practically a miracle drug for me, but I no longer have access to it. When Spravato was released with the FDA’s very strict guidelines on how it should be controlled and administered, my doctor feared retaliation and refused to continue the generic ketamine script and even dropped me from his practice. It was similar to how many of us were treated by doctors after the CDC released its guidelines on opioid restrictions. What a shame. I’d found an affordable miracle drug that alleviated all of my symptoms at once with no side effects, but then it was abruptly taken away, and within a few days, I returned to being just as severely ill as before. If I could’ve used it twice daily, I feel sure that I could’ve built up my strength and functioned as my normal self, pre-ME/CFS. That’s how incredible it was.
So, I hope this period of ketamine’s very strict regulation and prohibitive costs don’t last long.
While I think an immune assault triggers cfs, I have long thought that cfs is perpetuated by problems in the brain and CNS. So this is very interesting
It’s interesting that thanks to Chris’s comment I just found out that Andrew Miller – who found basal ganglia problems in ME/CFS – believes that ketamine may be most effective in those with inflammation induced depression. If you have ME/CFS/FM and depression I would suspect that inflammation may be involved.
Miller believes that ketamine’s effects may tie together or help explain how inflammation, glutamate excitotoxicity and the kynurenine pathway work together.
https://www.nature.com/articles/npp2013140#ref6
Cort, do you know if any more study results from Japan may be out this year?
I have no idea. They have published in the U.S. in the past. I believe a neuroinflammation study has been done over there but it hasn’t been published in the U.S. yet.
This sounds really hopeful. Anyone know when and if this may be prescribed by doctors in the UK?
nasal spray
https://www.depressionalliance.org/ketamine-nasal-spray/
clinics available
https://www.depressionalliance.org/ketamine-for-depression/
I had to have surgery last year and was given Ketamine. I came out from under anesthesia and starting talking a mile a minute. That lasted for at least 24 hours. Ketamine really revved me up in a good way so much so that I started researching where Ketamine infusions were being done even though I have bad veins.
Dana, I had the same experience. I have Ehlers-Danlos Syndrome in addition to ME, so most anesthetics do nothing for me. I used to ask for ketamine during surgeries. I’d always wake up walking and talking like I’d been rejuvenated. It was the ketamine. It took a while, but I finally found a doctor willing to give it a chance and wrote me a prescription for ketamine nasal spray. It’s also available in lozenge form if you can find someone still willing to prescribe the generic version. And if you do, please let me know – I’d love to have access to it again and have a much improved quality-of-life.
Much as it is tempting to try a new miracle drug for depression and fibromyalgia, it is worthwhile to thoroughly investigate the possible consequences.
“The present data indicate that the initial mitochondrial dysfunction and autophagy may be related to its inhibitory effect on the mitochondrial electron transport system, which underlies ketamine-induced neural toxicity. Higher ketamine concentration can induce ROS generation and apoptosis in human neurons.”
From:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4447382/
“Acute ketamine administration impaired the function of mitochondrial complex I leading to increased mtNOS activity, increased generation of hydrogen peroxide and NO, resulting in superoxide dismutase triggering, and improved antioxidant activity”
From:
https://www.ncbi.nlm.nih.gov/m/pubmed/25427286/
Yes, everyone should note that it’s not really clear how ketamine works and no one knows what long term effects it may have. Dosing is also a question.
It’s good to beware of the potential mitochondrial problems. That paper does refer to higher doses of ketamine. We’ve seen that dosage – perhaps particularly in the central nervous system – can make a huge difference. The effects of low does naltrexone, for instance, are far difference from normal dose naltrexone.
I’m not saying that’s happening here but it’s something to keep aware of – as are the potential risks.
The paper states that
“Third, we observed neurotoxicity of ketamine at 100 μM and higher concentrations, which is a range higher than that used in clinical practice. ”
This study suggests that with developing brains ketamine can be either neuroprotective or neurodegenerative depending on whether the infant is exposed to “noxious stimuli (!).
https://www.ncbi.nlm.nih.gov/pubmed/24275940
“Ketamine, an N-methyl-D-aspartate (NMDA) receptor antagonist, is widely used in pediatric anesthesia. Recently, a series of animal studies have shown that ketamine may have neurotoxic effects on the developing brain and that these effects can later cause neurofunctional impairment. However, other studies have also shown that ketamine protects the central nervous system by inhibiting inflammation in the developing brain. The present study offers a review of the existing preclinical and clinical studies.
We concluded that the role of ketamine varies not only on the basis of the dose and frequency of exposure but also the intensity of the noxious stimuli. Moreover, the repeated ketamine usage may be neurotoxic to immature brains in the absence of noxious stimuli, whereas it may be neuroprotective in the same brains in the presence of strong painful stimuli. Balancing the neurotoxic and neuroprotective effects of ketamine on the developing brain may be possible, but further study is required. “
Another review reports that dose is in fact determinative: high doses trigger glutamate excitotoxicity and irreversible degeneration (don’t try this at home!), taking ketamine during CNS development may be harmful, but low doses in adults are not only neuroprotective but promote neurogeneration… Our brains are really quite fascinating 🙂
https://www.jbrf.org/ketamine-clinical-trial/the-neurodegenerative-and-neuroprotective-effects-of-ketamine/
My attention was grabbed by what S.A. wrote: “The effects were immediate – the pain and fatigue disappeared, and I felt an overall improved sense of well-being with no unwanted side effects other than…”
The reason: the immediate effects. Near the onset of PEM I often first experience a rapid rise in body wide pain, and soon thereafter (if I can’t PACE rapid and sufficient enough) I start to lose strength and mental abilities very quickly. I do relate that to a sharp rise in oxidative stress.
When looking up the combination “ketamine and oxidative stress” I too, like you and Cort, do find results all over the place. Some studies declare it to be neuroprotective and able to protect against traumatic brain injury https://www.dovepress.com/ketamine-ameliorates-oxidative-stress-induced-apoptosis-in-experimenta-peer-reviewed-article-DDDT
Most studies however point to it causing plenty of additional oxidative stress and it has some nasty pathways creating plenty of malondialdehyde, aldehyde and a complex between both. That’s quite a nasty combo.
Then my eye was drawn to what Cort wrote, that it “dampens Cytochrome Complex I”. In theory, if this were the biggest source of ROS then dampening it a bit could alleviate the amount of ROS produced. But I feel that it would be very tricky to balance out, just as the other mechanisms by which ketamine could potentially modulate inflammation. They feel like to be too much of a balancing act to show good (temporary) effect in
a large subgroup of patients. And still this nasty malondialdehyde, aldehyde and a complex between both thing is adding on top of it. So I don’t feel it yet.
Then I turned my eye on “increased generation of hydrogen peroxide and NO” and reminded Cort wrote “Subanesthetic doses of s-ketamine actually increased cerebral blood flows in one study.” and, in a comment ““it’s sometimes possible to perform ketamine anesthesia without protective measures to the airways and is considered relatively safe because protective airway reflexes are preserved and it’s used as a bronchodilator in the treatment of severe asthma.””
At night my symptoms can skyrocket from time to time. I slowly developed certain techniques that can bring down a *very* fast hart rate back to normal in sometimes less then 10 seconds or can generate a feeling within seconds after a certain combination of movements of having “a fresh shot of oxygenated blood to the brains”. It’s like a small dose of heaven then. Unfortunately, it’s not that easy to get these results at wish but certain techniques start to get better and more consistent results in certain typical situations.
Those techniques all dominantly alter blood flow and I believe they work by quickly drawing pooled blood from the legs and adding it to the amount of blood in circulation. That has good abilities to quickly and temporarily improve hart prefill. Poor hart prefill is according to me a major source of my episodes of very high hart rates. Likewise but a bit different techniques may create a certain short “burst” in blood movement (refresh) in the brain I do believe. That creates this small shot of well-being I mentioned.
In the paper Cort mentioned http://anesthesiology.pubs.asahq.org/article.aspx?articleid=1942257:
“Whole brain CBF was increased by 13.7% (P = 0.035; table 2and fig. 2). Regionally, CBF increased in the anterior cingulate, insula, frontal cortex, thalamus, putamen, and cerebellum by 14.1–31.6%”
Now for anesthetic doses that would often decrease CBF rather then increase it, that’s impressive.
Why such long response when I could just have posted the previous few lines? Because I see a chanche for ketamine to both increase oxidative stress yet improve ME patients well-being and physical and mental abilities.
The drug seems (a gut feeling) to be able to increase the diameter and blood flow in the smallest capillaries in the brain and hence not only provide “fresh” blood to these regions but more importantly remove what I called more then once “stale blood”. Blood trapped in these capillaries should contain many toxins but also likely contains high amounts of ROS.
I believe that these amounts of ROS have a strong impact on mitochondria shutdown. Many mechanisms seem to point to it. Bringing in new blood that hasn’t been “stale” for a prolonged time should contain far lesser concentrations of ROS. Hence the inflow of a shot of fresh blood should dilute local ROS.
If this idea were to be wright, the speed of the mitochondria response would be amazing: a matter of seconds judging by my “shot of relieve” in 10 seconds with this technique under development. Short lasting too, so build up rate might be very high too. When thinking of it the reverse way, the very rapid (a few minutes) speed by which pain and physical and mental ability loss can conquer me does also point to a very rapid mechanism.
Now ketamine is a fast acting drug. It feels like this hypothetical “diluting of the blocked/blood pooling capillaries” effect decreases the local peak concentrations of ROS stronger then the ROS generating powers of ketamine increase it in these zones. If so, the “turning down” of mitochondria would be very much dependent of precise location and time.
While the average body wide concentration of ROS in ME would be high to very high, in this model ME would differ from other diseases with high oxidative stress due to ME having far higher peak concentrations of ROS near the most restricted (damaged?) capillaries. The combination of low blood volume, poor blood flow and high ROS would make the disease so much more debilitating.
Now what could further point to this hypothesis of having far higher peak concentrations of ROS near these most restricted capillaries then the average blood/cell ROS concentration?
Complete lack of brain coordination during “bad ME episodes”. If the turning down of brain cells was a direct function of the local amount of ROS they “saw” then the turning down of individual brain cells would be a function of how restricted/damaged the local capillaries were. That would give near each neuron a different response strength. Now in technical computer neural networks the exact strength of each neurons response is vital to the neural network to be precise and efficient in doing it’s job.
I am not very sure, but I have some insight in how they work. I do think according to my insights that individual variations in neuron strength would be far more deteriorating precision/accuracy (“brain power”) of the neural network then scaling all the cooperating neurons with the same factor. That could be easily simulated by skilled computer scientists to check that hunch of mine. Hence having strong local variation in ROS leading to strong variation in neural strength could deteriorate neural network (brain) functioning far more then the same levels of ROS could ever do when hitting the same average levels but equally spread over the brain.
Likewise, different regions of the brain would see some amount of stronger or lesser modification of the “region wide” blood flow. That would hamper communication between regions fed by a different sub-artery quite significantly. That is likewise as is seen in ME.
Now let’s look at the muscles. Of coarse poor brain (and nerve) functioning deteriorates muscle functioning. But I feel there is more to it.
If local blood flow in the smallest capillaries were varying a lot then here too there would be a double effect. Energy/food and oxygen flow would be reduced at site of the worst affected locations and on top of it these locations would have far higher concentrations of ROS that under this idea would inhibit local mitochondria functioning. (I did it mention less explicit but in the brain both effects combine too.)
Now try and move: each region in the muscle has strongly varying power/potential to engage in movement as it’s local combination of amount of energy/oxygen flow and mitochondria inhibition (both either simultaneously better or worse creating a quadratic type of response to amount of blood flow) determines the individual muscle cells strength.
That in effect would create a “sea of muscle cells” contracting at widely varying strength and amount of contraction/expansion. Nearby muscle bundles separated by the smallest fascia would likely be fed by a different “sub-artery”. That would change the contraction amplitude and strength from bundle to bundle. All of this should cause massive amounts of tension between both individual bundles and individual cells alike.
That would generate pain, damage, further restriction of certain small blood vessels making the problem worse, creating cramps (uneven contraction of zones), creating local curling up of muscles, make movements very inefficient, and reduce average range of motion of the muscles. That sounds a lot like fibromyalgia. EDS may sound to conflict with this reduced average range of motion but not all fibro is of the hypermobility type and hypermobility may be more in the connective tissue then in the muscle cells itself.
Here again, moderate-ish levels of oxidative stress with strong variation time and location wise may cause far higher disability then the average values of ROS may suggest.
In both this ME as fibro model, dysfunction could happen at far lower damage levels then what one would expect from the level of disability seen in this disease. In both cases the local big differences in combined blood flow and mitochondrial downturn would be a big part of what makes this disease so severe.
That would allow for so much disability combined with so few clear visual and observable damage seen in both ME and FM. And it would also explain why both diseases seem to be largely reversible with very few permanent damage for those few lucky to get out of it (or those having intermediate periods of near no symptoms).
Both would be very closely related in this concept too, making the main area of increased ROS concentration AND variation the differentiating factor between having ME, FM or a combination thereof.
And that leads us to two things:
– The failure of the Rituximab trial.
– The near completely ignored successful moderate scale study of IV-saline administered over longer periods of time with fairly large time intervals between them (too tired to search study)
IV saline is reported to have sometimes remarkable near instant effects in ME patients. Sometimes they turn to be nearly normal for some time but this effect unfortunately vanishes over a matter of hours. Likewise reports do exist from a sort of strong inflating pants putting pressure on the legs and increasing return of blood from the legs to the hart.
Two things are of importance here:
– Return to very few symptoms indicates some large amount of reversible damage in these patients.
– Return to it quickly does indicate to a very quick mechanism.
Now both the inflation pants and the IV saline have the power to do:
– Increase the amount of “actively used blood”. They increase apparent blood volumes by having more in the blood vessels and less pooling. As I’ve written before, blood has (due to having relatively big RBC in it) a very strong effect of reduced blood flow if vessel diameter becomes really small. More blood can “open up” blood vessels and reduce the amount of difference in blood flow between the largest vessels and the smallest vessels. Note this does again fit in the idea that strong local variation in blood flow may play a major part in both ME and FM.
– Flush out the high concentrations of ROS/toxins in the “stale blood” found in the most constricted capillaries. Note that “cleaner” saline would be good at this as it would contain non of them at start.
Now this effect may be temporary as (in those patients it works) this would initiate two things:
– The patient enjoying it too much and forget about pacing, using/creating more energy and with it more ROS.
– The concentration of ROS and toxins to rise in the “main and cleaner blood pool (compared to the stale blood in the smallest vessels)”. Over time this would help spread inflammation to other regions and decrease the “flushing out/cleaning” effect the blood from the bigger vessels has when flowing trough the smaller vessels because it’s more polluted when entering the smaller vessels. It’s like it’s more difficult to clean a car with dirty water then with clean water.
So this cleaning out may be most effective if it’s done with moderation and not for too long. It’s a bit like with IV saline and ketamine: it’s immediate effects wear off relatively fast. Under this hypothesis the “observed” period of effects may be composed of a smaller period of “cleaning the pipes” and a larger but still short-ish period of better functioning due to having cleaner pipes until they pollute again.
Having both ketamine and IV-saline in periodic and non too strong amounts in combination with as strict as ever pacing during the better period and in between treatments *might*, very strong conditional, improve disease strength over time (such as IV-saline studies suggest).
I’m too tired to work it out now, but the above shows quite some resemblance with what Ron Davis observed with “putting healthy cells in ME blood and ME cells in healthy blood”.
With the link between fail Rituximab and IV saline I meant to say:
The Rituximab study failed but in a certain way: both Rituximab administration (as a drug mixed in IV-saline IMO) and placebo (IV-saline administration), both administered at regular intervals over a longer time, had fairly good disease improvement rates.
That was interpreted as: there was such anticipation to take part of the study that there was a (very) large placebo effect but the drug failed to do anything other then being a placebo.
As I’ve written before I disagree: there are mid scale studies that point to fairly good results of IV-saline doses administered with intervals, showing improved health even long after the last administration has ended. That is a fairly strong indication that the placebo was not a placebo.
It could be a good indication that the IV-saline was (a big part of) the healing component of the Rituximab solution. I’d love to see these IV-saline studies be repeated with larger amounts of participants and methods to determine better doses and intervals if effects are positive. I see no reason to turn down on something that has potentially good effect, few side effects and is very cheap. Approval time of IV-saline treatment should be far lower then those of a completely new drug if successful as well.
Interesting, I’ve been blood letting
(Donating blood)because my ferritin was so dangerously high. It took 4 times over a period of just less than a year for the ferritin to begin to come down. It seems giving blood has helped some of my issues. Just a few days ago I had been told a startling admission from my nephrologist….he stated that the 1.5 years straight use of tetracycline at the age of 14/15 caused my me/cfs.You don’t want to know where I’ve been…I didn’t think a person could be this sick and still be alive…pretty sure I almost died.i WAS the walking dead…for years and years…,.such bad FM pain and swollen brain that I was going to go get the gun on several occasions….NOT depression but severe pain and brain swelling
One of my positive outcomes from giving blood is, my toenail had died from constantly ramming my toe into the wall, the dishwasher,has begin to grow again!
I feel much warmer overall as I’ve always had cold hands and feet….gone.so, yes I believe my issues are blood related
I suffer from fibromyalgia and – serotonin syndrome. In short: Ketamine can kill me. Fast.
Hey elvira, my serotonin levels run really high. I’ve been prescribed practically all of the SSRIs/SNRIs on the market, not because I’m depressed, but because I’m a female with a somewhat invisible illness. Even one pill made me ridiculously sick. I didn’t know what serotonin syndrome was until the first few visits to the ER after taking an anti-depressant. I understand ketamine effects our serotonin, but I’ve never experienced serotonin syndrome symptoms from ketamine.
If it’s potentially deadly for you, make sure your doctors are warned, especially before a surgery since it’s so commonly used.
I simply don’t dare taking anything affecting my serotonin level. I’ll do anything to avoid it.Had several scary episodes.For me and my family. Even food containing a lot of tryptophan knocks me off my feet. In spite what doctors say to me. I don’t want to experiment any more.I walk around with the list of drugs and foods that elevate serotonin level.
Yes, you have to obviously be very careful. This is such a complex area though. Ketamine actually increases glutamate activity – which should be be bad, bad, bad for FM – but it apparently does so in a way that is helpful.
There is so much we don’t know about the central nervous system.
While I have the highest respect for Cort and his blog, I believe, because he presents practically everything that relates to MECFS and FM, Cort needs to develop some type of hierarchy quality scoring system to help his readers focus on the more relevant potentially useful research skin to the “evidence-based-medicine“ system used in medicine.
Do you mean not such a focus on evidence based medicine which as we know is pretty darn limited in ME/CFS?
I agree with William Prigden…… this whole blog set me in a spin. As a highly sensitive long term CFS/ME person, am always on the look out for something to help, something
I can afford. I have almost given up, and remain content with what I am doing.
The articles are often too long and complex for me, but I preserver. This blog was
not helpful for me, although I know Cort has every good intention. It excited me and then scared the hell out of me.scar
It’s a fairly new product for pain and depression and while it obviously helps some people it’s hard to know what to do with it. I wish things were clearer and there was less grey area. This is true for so many things…
My post below was/is for Billie Abbott.
Cort snuck one in while a was typing
Lol
Something affordable?…you could try micro dosing magic mushrooms. They’ve helped me greatly. There is lots of info on the dosing etc. Tons of positive outcomes and not many negative. They can be purchased almost anywhere now.A good place to start research is to go online and listen to Paul Stamitts (spelling)?
I’ve been withing for Cort to blog it…maybe he has and I missed the blog🤷♂️
I haven’t – good idea! 🙂
Years ago I went into total remission.
1. at the dentist office having sedation for a tooth removal
2. an operation for which I received anesthesia
Since ketamine is a form of anesthesia,
I believe it was the ketamine which put me in remission.
I intend to visit my dr. for a prescription for the Spravato Spray
Interesting. Dental anesthesia usually makes me feel better for a couple of hours! Calmer, more energy – never thought of the possible connection! Thanks
Hey Carmel, I usually experience the same improvements after anesthesia as you’ve described.
If your doctor is willing to prescribe it, I’d suggest asking for generic ketamine in the form of nasal spray or lozenges. It’s significantly less expensive at around $50/mo, and you can pick it up at your pharmacy and use it at home like any other medication. Best of luck to you. Would love to know what you think about it.
S.A.: do you mind sharing what dosage of the nasal spray your doctor prescribed for you?
They really reset a person.and if you take more, we’ll,…. “take a trip and never leave the farm”…much like lsd but safer. I’ve gotten some for a friend’s son that suffers from depression…the dad says he’s made his bed and cleaned up his room for the first time in years.noticable difference
There’s something in this for CFS patients in serious pain, but it’s problematic. I recently underwent a round of outpatient treatment for severe polyneuropathy. My fragile condition (I am nearly bedridden with CFS) rendered the side effects—mainly profound weakness and nausea—borderline dangerous. I could only tolerate low doses and could not continue after only four infusions. More than two weeks later, I am still suffering a flare, mainly worsened pain. At the same time, an improvement in energy level leaves me a wee bit encouraged. I will try ketamine again if I can get insurance coverage for treatment in hospital.
I did Spravato for three months at my MD’s office. I have every neuroimmune issue, symptom, and diagnosis imaginable (ME/CFS/Fibro/Lyme/PANS/AE/CVID/Cell Trend+Cunningham autoimmunity/SFPN, etc., etc.).
I found ketamine (Esketamine) treatment VERY difficult, and although it briefly helped cognition while I was doing it routinely, it left me with a PERMANENT ESSENTIAL TREMOR in both hands and arms (developed while I was on the ketamine, perhaps small vessel disease related stroke or injury, nothing visible on MRI). Also, I felt worse after I stopped doing the ketamine. My Alzheimer’s-like symptoms progressed and the ketamine did nothing for my severe anhedonia.
I’ve been sick for 10 years and have tried tons of hardcore western and some experimental meds (PICC line/abx plus oral abx, antivirals, Rituxan, IgG, 100 FMTs, exosomes, etc.,etc.).
All the above mentioned meds except ketamine have helped me. Recently, Mestinon has improved my function greatly.