“The Fusion model aims to…replenish and strengthen the body so that it can” heal itself. Dr. Downing-Orr
I glommed onto this rather old book (2010) and treatment protocol with interest because it was so different. For one thing, its medical approach is centered on a drug – Nimodipine or Nimotop – I had never heard associated with ME/CFS before.
The fact that it was Dr. Kristina Downing-Orr, the author of “Beating Chronic Fatigue: Your Step-by-Step Guide to Complete Recovery”, recommending this drug seemed even more surprising. A clinical and research psychologist, neurolinguistic programming practitioner and hypnotherapist, I expected her to view ME/CFS in a biopsychosocial light but she didn’t – not at all.
It turns out she wasn’t able to. Not after two viral attacks left her bedridden with ME/CFS, migraines, restless leg syndrome, problems with fainting, food allergies and in severe pain. Dr. Downing-Orr became so weak at one point that she was unable to lift her legs, put on her shoes, or walk a step.
The biopsychosocial paradigm of someone getting ill, paying too much attention to their symptoms, becoming deconditioned and feeling worse didn’t fit her experience at all.
One wonders how many clinical psychologists would recommend their approach to ME/CFS if they’d ever experienced the disease. Dr. Downing-Orr reported that psychologists treating ME/CFS have, in confidence, told her that “the much vaunted psychological treatments were not as effective as patients were led to believe”. That lead her to ask a simple but penetrating question: if psychotherapy and antidepressants do little to help the illness, why do so many doctors assume the disease is psychological?
Yet as Downing-Orr decried the failure of health professionals to recognize the true biological nature of the illness, she, a psychologist, also reported that the psychological factors often accompanying chronic illnesses can also help perpetuate and worsen symptoms. If that sounds like a recipe for a CBT-like intervention, it is.
While the two basic treatment protocols described in the book – a medical one (more drug-based) and a nutritional one (supplement-based) – don’t involve behavioral interventions, the last section of the book describes ways to relieve the enormous mental and emotional stresses that serious illnesses like ME/CFS can produce.
Dr. Mason Brown
Dr. Downing-Orr reported that a treatment protocol program created by a U.K. doctor – which piggybacked on work by Dr. Jay Goldstein and Dr. Byron Hyde – allowed her to completely recover from a severe case of ME/CFS. Her book describes that and another protocol.
Early in her illness, she came upon the work of Dr. Mason Brown, a fellow sufferer in the U.K. Dr. Mason Brown collapsed one day while working as a junior doctor in Edinburgh. He managed to complete his schooling, and worked as a doctor for ten years, until one day in 1979 he was unable to get out of bed. He lay there for six weeks, managed to get back to work, and worked for another ten years, but then retired due to ill health in 1990.
He later reported he believed that a variety of factors including genetics, viruses, pollution, pesticide exposures, poor diet and prolonged stress precipitated his illness.
He recovered using a treatment protocol built on the work of two pioneering ME/CFS physicians – Dr. Jay Goldstein and Dr. Byron Hyde – both of whom believed poor blood flows to the brain play a significant role in this disease.
The cornerstone of Dr. Brown’s protocol was a drug called Nimodipine, which he used to increase blood flows to the brain. Like pyridostigmine bromide (Mestinon), an old drug now being used in a new way in ME/CFS and POTS, Nimodipine has been around for a long time. Patented in the late seventies, it’s been FDA approved in the U.S. for over thirty years.
Downing-Orr reports that Dr. Brown’s success rate (a complete or near complete recovery) was an astounding 80%. Downing-Orr also worked with two nutritionists (Alessandro Ferretti and Jules Cattell) who report a success rate of 85%.
(To be honest, if I was an author I might, in an effort to avoid being accused of selling snake oil, refrain from stating such miraculous success rates – but who knows?)
Causes
In her book, Downing-Orr proposes five main causes of ME/CFS – none of which will be a surprise to most of us – and most of which, ten years later, are still being explored.
- Immune issues – a malfunctioning immune system that has failed to fight off a bug properly.
- Bad gut bacteria that leads to candidiasis and poor nutrient absorption.
- Poor circulation – blood flow impairments that fail to give the cells the nutrients they need and fail to flush away toxins
- Adrenal exhaustion – overstressed adrenals that become exhausted over time – (this is a truly controversial idea; others believe that the adrenals are not exhausted but are not getting the signals they need: either way the adrenals are implicated.
- Mitochondrial dysfunction.
Downing-Orr believes – like many others – that a genetic predisposition, in combination with some stressful event or period (infection, childbirth, divorce, serious injury, exposure to the elements, toxins, etc.), causes the body to release a torrent of stress chemicals. These stress chemicals then destabilize one’s systems leading which affects the autonomic nervous system, HPA axis, and limbic, immune and gastrointestinal systems. The key player in this widespread breakdown? The hypothalamus.
A couple of years ago, in a fascinating talk Dr. Lucinda Bateman posited that hypothalamic dysfunction could play a key role in ME/CFS. She proposed that inflammation in the lower part of the brain – the limbic system – was producing a “limbic system encephalitis” which was affecting upper and lower brain (hypothalamus, thalamus, and pituitary) functioning and the autonomic nervous system.
The Medical Option

Dr. Downing-Orr reported she went from being unable to lift her leg to a complete recovery using Dr. Brown’s protocol
Dr. Downing-Orr emphasizes that if you take the medical option, you must consult with your doctor and read the entire book to make sure the treatment applies to you. That’s probably a good idea, given that if you employ the medical option, you’re probably going to feel worse before you feel better.
Downing-Orr believes that side effects often seen when taking Nimodipine and other parts of the protocol, like tiredness, achiness, swollen glands and even mood swings – are the natural outcome of a body being kickstarted into action – and releasing the toxins that have been stored in our tissues. Dr. Downing-Orr reported that while some people more or less zoom through it, she experienced severe symptoms at the beginning of the program.
She emphasizes that you should follow it exactly as it is laid out. (Please note that this short synopsis does not replace reading the book. If you decide to do this program, you should get the book.)
Step One: Improving circulation in the body and brain
Making improving circulation the first step in the protocol was intriguing given how much interest has been generated in this area since Downing-Orr’s book was published. She recommends:
- Nimodipine – brain and body circulation
- Gingko biloba – peripheral circulation
- Eight glasses of filtered or bottled water a day
- L-glutamine – digestive tract
- Evening primrose oil – relieves pain.
Nimodipine – the Cornerstone
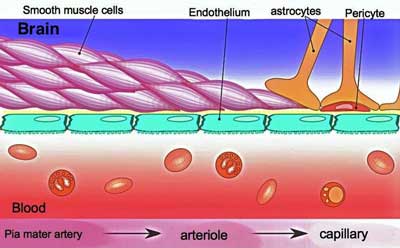
The cornerstone of Dr. Brown’s and now Dr. Downing-Orr’s approach is an unusual drug called Nimodipine which, as far as I can tell, is little used by ME/CFS experts in the U.S and Canada. A 2nd generation calcium channel blocker that was originally used for stroke, Nimodipine is used to promote blood flows to the brain in order to flush out the neurotoxins he believes have built up.
Nimodipine’s calcium channel blocking properties allow the walls of blood vessels to relax and open, allowing more blood to flow.
Because Nimodipine has a greater effect on the arteries in the brain than in the body it is unlikely to effect blood pressure. Because it may be releasing toxins, however, it may produce early side effects. Susan Parker reported that on day 4 of taking 45 mg/day she experienced “a sudden rush of foul-smelling odour in
my arm pits and felt nauseous.”. The next day, however, she felt much better.
While Nimodipine’s affects have never been assessed in a clinical trial in ME/CFS, Parker reports that in general the drug is considered safe and usually produces few side-effects.
Parker reported that 40% of Dr. Jay Goldstein’s patients improved on the drug, and Goldstein rated it the third most effective drug in his list of the 23 most effective drugs for ME/CFS. Besides Goldstein’s findings she provides many anecdotal results from doctors who have used Nimodipine in her amazingly comprehensive 34 page 2014 report.
- Dr. Jay Goldstein – the top 23 drugs for chronic fatigue syndrome (ME/CFS)
In 2004 Dr. Marilyn McNeil wrote in response to a British Medical Journal article that small doses of Nimodopine allowed her to rapidly recover from a severe 4-year case of ME/CFS which had left her bedbound. Susan Parker reported she was largely housebound before recovering 80% of her health by using the drug. Finish author and ME/CFS patient Maija Haavisto reported Nimodipine markedly improved her brainfog and puts it on her ‘definitely try’ for ME/CFS list.
Not everyone benefits from the drug. Parker reported that Dr. Brown found that “Nimodipine helps twenty percent [of ME/CFS patients] very quickly, another twenty per cent over six months, and all others to varying degrees over a period of time.”
Note that the drug can produce hypotension (lowering of blood pressure) – a possibly serious consequence for some people with ME/CFS – as well as altered heart rates, headaches; sweating, nausea and stomach problems. Dr. Shepard recommended that the drug be used with care and advises that anecdotal reports have been mixed.
- Coming up shortly – Remy takes a close look at Nimodopine
Several different protocols exist. In Downing-Orr’s “slow” protocol the dose begins very low and is raised very slowly. The drug is usually taken only for a month – and four or five months at the most. You’ll know its working when you start thinking better. Once the proper brain blood flows are re-instated, Dr. Brown believes the hypothalamus and HPA axis will begin working properly.
For more on Nimodipine check out Health Rising’s Resource below.
Step Two – Promoting Good Gut Health
Improving gut health involves another slow ramp-up with a probiotic called Prime Directive for 2-3 months which can produce fluey, etc. feelings as the bad bacteria die off. The food prescriptions are a bit dated but familiar:
- avoid refined foods, sugar, honey and syrups, soy sauce, smoked meats and fish, pickles, peanuts, mushrooms, vinegar-containing foods, dried fruits, cheeses. (This appears to be an anti-candida diet.)
- include foods such as fresh vegetables, avocados, seeds, yogurt, organic chicken, fish, olive oil, buttermilk.
Step Three – Detoxification
Many ME/CFS/FM doctors don’t include detoxification in their treatment protocols, but detoxification is a central aspect of Brown’s program. The poor circulation present in ME/CFS keeps them from being flushed out and allows them to accumulate in our tissues.
Detoxification – the process of removing toxins from your tissues and dumping them into your bloodstream – so that they can be flushed out of your system – can obviously be a delicate and tricky process.
For this reason, detoxification is only begun after signs of progress and after the gut health step is proceeding well. An antioxidant called Revenol which contains maritime pine bark is recommended. (Better antioxidants are probably available now). A key aspect of this step is how slowly this step is taken. The first dose of Revenol is just a quarter of a tablet (pill cutter required :))
Milk thistle – a liver function booster is also used.
Step Four – Replenishment
- Multivitamin supplement.
Recovery
It may be a pretty simple program but it’s not a short-term program. Expect no quick fixes. For every five years of ME/CFS, expect Dr. Downing-Orr says to expect recovery to take a year. If you’ve had it longer than five years, expect it to take two years on this program.
The Nutritional Option
For those who don’t want to take the medical approach, Downing-Orr recommends a nutritional option. That will probably be immediately recognizable to anyone who has explored nutrition, diet and supplements in connection with ME/CFS/FM.
It involves supplements like D-Ribose, acetyl L-carnitine, whey protein powder, probiotics, L Glutamine, magnesium ascorbate, NAC, Rhodiola, Gingko biloba, probiotics, CoQ10, etc.
Behavioral Aids
Despite the fact Downing-Orr firmly comes down on ME/CFS as a biological disease, she does not dismiss CBT/GET as adjunct treatments. If applied appropriately when the underlying biological problems are being addressed and one’s body is on the road to recovery, she believes these therapies can be helpful.
Why? One good reason is that no one is prepared for dealing with the kind of devastation ME/CFS often wreaks on a person’s life. People with ME/CFS, she says, have to “cope with something so extreme that at times it is beyond comprehension.” Given that, it’s no surprise to see negative thinking patterns arise.
She believes that her form of cognitive behavioral therapy (CBT) – which differs markedly from other forms of CBT – can “greatly enhance your sense of control over your health and your life”. She identifies four kinds of faulty thinking that people with chronic illnesses are prone to fall into:
- Black/White thinking – Given the activity limitations this disease often imposes, thoughts like “I am completely useless”, or “I have nothing” to offer my family”, constitute black/white thinking.
- Magnification/Minimisation – magnifying what you can’t do and comparing that to what you used to be able to do is natural, but unhelpful.
- Personalizing – given the horrific changes in our lives that often occur with ME/CFS, it’s not surprising to find “personalizing” – making the illness about us – indulging in “woe is me” conversations, blaming yourself or others, is an easy trap to get into.
- Catastrophizing – Given how poor most treatments for ME/CFS work, it’s no surprise to see that catastrophizing – seeing only gloom and doom ahead – can take hold.
These patterns come from our subconscious and Downing-Orr sets out to rewire that and ward off the negative thinking patterns with mental exercises, visualization and muscle relaxation techniques. She also provides advice on dealing with relationship issues, helping children understand your illness, caregivers support, etc.
Conclusion
It was refreshing to see a psychologist from the United Kingdom renounce a biopsychosocial interpretation of ME/CFS and embrace a biological interpretation. That decision apparently became an agonizingly easy one once Dr. Downing-Orr, herself, came down with a severe case of ME/CFS.
“Beating Chronic Fatigue” is almost ten years old and the dietary and nutritional advice is surely somewhat dated but it did focus on a drug – Nimodipine – which was new to me, and which has the potentially salient affect of increasing blood flows to the brain, and, as we’ll see in Remy’s upcoming blog, providing a variety of other possible benefits.
Dr. Downing Orr recovered from ME/CFS using Nimodipine and other treatments, and Dr Mason Brown, a recovered person with ME/CFS, and the originator of the protocol, claimed a high success rate. If you’ve tried Brown’s or Down-Orr’s protocol or Nimodipine please let us know how it went.
- Next Up – Remy Takes a Deep Dive into Nimodipine (Nimotop)







Its truly refreshing to see an English/UK (the country that “gave” us PACE) psychologist proposing such balanced view on ME and its origins!
I too believe for some time that poor (local) blood flow plays an important role in ME. I also believe that part of improving comes from slowly improving this blood flow.
Issie has improved her health too. She uses calcium channel blockers as part of her treatment. She reports other problems related to calcium.
I tried to link those two together. Our ongoing conversation is not an easy read. As it linked well to this topic and I had to rewrite an important part anyway I tried and made the last comment easier to read. It still is not an easy topic so I can do only that much.
I rewrote the 3 last comments date “june 11” today. It combines with the 2 comments I wrote before that. The order in which to read them is:
* the first “june 9” comment
* the 3 broken up “june 11” comments
* the second “june 9” comment.
The order is messed up as I had to figure out what WordPress was blocking me on; it appeared to be repeated or to many links.
@Cort: please don’t approve blocked duplicates as it would mess up structure even more.
Yes, I do believe there are issues with calcium channels. I have mutations on TRMP3. I find Tramadol and GastroCrom to be two of my best helps. Both have mild calcium channel blocker effects. They dilate vessels. I also find using a Bentyl (muscle relaxer), with them to make the combination better. I’m not healed, but this does keep me more functional. I do believe these meds have other properties that help. Tramadol works on all the neurotransmitters. Some sort of tweak there helps. (I use a quarter of RXd amount and cycle on and off this. When it stops helping, I go off a few weeks to reset a lower dose to work.) GastroCrom is also a mast cell stablizer and that helps MCAS. Also using enzymes to help blood flow and thin blood.
Issie
Issie could you tell me what mg of Tramadol you are taking. I am taking 10mg and find marginal benefits.
Thank you
Spinal Stenosis, Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia: The Spinal Series #3 – Health Rising
https://www.healthrising.org/blog/2019/05/29/spinal-stenos
Heres link to dejurgen research.
I have noticed an improvement with Beet Powder which increases nitric oxide levels thus relaxing blood vessels. As I am mildly hypertensive, this has helped there as well. I’ll share the book at some point with my N.P..
I am very, VERY skeptical about these ‘cures’.
Iv’e had docs pursue this blood flow theory in me with absolutely no benefit.
At present, it appears ME/CFS has a variety of causes, the most common being an infection with one of the herpes retroviruses.
So to hi-lite just one successful treatment is MISLEADING to most of us.
EG Jen Brea’s problem.
I too have severe spinal stenosis similar to her yet that is not the cause of my CFS as I’ve had severe spinal stenosis since 1961 yet cfs only became apparent in 2009.
It took me 3 yrs to realize that all my unresolved physical complaints
to docs were all symptoms of ME/CFS.
To hi-lite just one unusual/obscure cause is a great dis-service to the rest of us, the majority of us sufferers.
I’m glad some find relief/cures but they are a small fragment….
As someone who has tried a number of things none of which have significantly improved my illness I understand your skepticism.
If you follow or check out Health Rising’s blogs you’ll see HR covers a wide variety of treatments each of which apparently does help for the right person – but probably, I will grant you, not for most.
If you’re that person, though, how nice it must be….
I think a good chunk of people also do find some relief.
Have you checked out or tried Dr. Pridgen’s two-drug antiviral treatment? There’s plenty of information on that on this website.
Hi Martin,
I too do not believe the basis of this disease is poor blood flow.
I rather see this disease as a combination of an underlying cause and secondary factors strengthening the vicious circle.
The underlying causes could be a few different basic problems that trigger a common ME mechanism.
The secondary factors strengthening the disease seems to vary widely from patient to patient.
Impaired blood flow may be one such common occurring secondary factor. Different patients may see a different type of impact on their blood flow just like some healthy-ish people may be more prone to edema, some to low blood pressure and some to high blood pressure.
The combination of different problems (like breathing, skeletal malformation, blood flow) and the different effects of each sub-problem (like edema / blood pooling, too low blood pressure, too high blood pressure, too few or much constriction)… make a one size fits all approach (near?) impossible.
But if one finds and treats such secondary problem without extensive side effects, a significant to strong improvement could arise. If one tries however anything that worked for someone else one may expect to get (much) worse.
In order to avoid such damage I try single small changes and evaluate them with keen senses and methodology. Even then I did hit big fire-backs but health gradually improves. It remains a very difficult process not suited for many or most people so far however.
The idea behind having only a single change at once is:
* It’s hard enough to observe the effects of a single change.
* If doing multiple things at once, 3 things may be positive, 2 negative; the net effect is doing 5 things for having 1 net improvement; that makes observing it difficult and side effects varied;
* When stacking several approaches with each many positive and negative effects, it soon becomes much effort for few result and you’ll hit a ceiling quickly.
The idea behind having only small to minimal changes at once and observe their effect over a longer time:
* It reduces the chances to hit a major and irrecoverable fire-back
* I believe that with many treatments going with a low doses improves the ratio beneficial effects to side effects significantly.
The success may be due to it’s impact on bacteria — massive impact:
See http://microbiomeprescription.azurewebsites.net/Library/Modifier?mid2=829
This impact is predicted to help the bacteria associated with the following symptoms:
Post-exertional malaise: Inappropriate loss of physical and mental stamina, General: Fatigue,Neurological-Sleep: Chaotic diurnal sleep rhythms (Irratic Sleep) ,
Neurological: Impairment of concentration ,
Sleep: Unrefreshed sleep ,
General: Headaches
Neurological: Confusion
Neurological: Short-term memory issues
Autonomic Manifestations: light-headedness
Autonomic Manifestations: extreme pallor
Ken, the link you provided goes to Nimesulide, not nimodipine. However, a search (on your site) for the impact of nimodipine does also indicate a broad impact : http://microbiomeprescription.azurewebsites.net/Library/Modifier?mid2=864
Comment deleted -possible scam site.
All 8 human Herpes being a retrovirus cannot be eliminated once we are infected.
Most (like 90+%) of us have herpes 1,2 (distinguishable only by a biopsy) 3, 4, & 6 or 7……
After discussing with my knowledgeble pharmacist he said (the expensive) antivirals are available for only 1/2, 3 & possibly 5.
Yet the current culprit (according to NIH’s Pub Med) appears to be 4; also known as eptein-barr or ‘Mono’.
My pharmacist said there’s no anti viral for that….
It seems that just as 3 (chicken pox) returns as far more serious shingles, a similar thing is taking place with 4 (which ~95% of us have…)
So for the majority of us who got EM/CFS after ‘flu-like symptoms’, indicating some kind of infection, we must be patient as we suffer……………..
Cort.
Your thoughts please on my post…..
One further thought on research:
At Stanford Dr. Montoya’s team found that a thorough examination of not just a few cytokines (but all) found that they could not only predict CFS but also it’s intensity given the levels of those things in our blood.
Every one of us has degrees of impairment…..
An afterthought:
Although some may discredit him personally, his research is solid & that’s what we need to focus on…..
All of us want a cure!!!!!!
Martin,
There will never be ‘a cure’. One cure for everyone, since we all got sick in different ways, different bugs, different environmental exposures, different stresses or traumas, etc.. Almost everyone has these herpes viruses (not retroviruses, sorry) for example, yet they don’t have ME/CFS.
If only it weren’t so complicated.
Any main ingredient you would recommend to keep the Virus dormant?
Hadio, I went to that site and the response to my inquiry was classic snake oil merchant. $700 for a herbal treatment???
Thanks for checking that out. Comments like Hadio’s will no longer be allowed.
I just wonder how many GPS would prescribe Nimodipine.
I don’t know. I imagine many wouldn’t but in her superb review Susan Parker does mention doctors in the UK and elsewhere who have given it a try. https://www.actionforme.org.uk/assets/components/discuss/attachments/2/6193/nimodipine%20use%20in%20me,%20jan%202014.pdf
I’m sure mine would, but the last time I tried a calcium blocker I swelled up with oedema and we had to stop.
I just read this, Nov, 2019… . I used to absorb most research and trial protocols but now, after 30+ years following this illness I have about given up the ghost that these isolated cures’ are anything more than a casual connection to the ‘real MECFS.’
I think this book, like others who proselytize an answer to our malaise actually addresses several unique-to-the individual(s) diseases buy not common amongst the bell curve of PWCs. Maybe coincidental to a few PWCs but otherwise off the chart into possible areas involved in the manifestations of MECFS of which most of us are familiar.
Coincidentally, or not I became a patient of a bright young neurologist who knows about MECFS and shares my belief that it’s neurological in nature.
Pursuant to his treating my peripheral neuropathy which manifested
seriously this year he simultaneously began testing for tangible signs of ME ‘footprints.’
He has done all kinds of esoteric blood analysis and MRIs and genetic testing. He now wants to do brain scans and analyze the results from a lumbar puncture. Frankly, I‘m hesitant about the spinal tap due to perceived risks and concern about unknown pain. I’d be curious to know if anyone else here has undergone this procedure and what the experience was like. Any post procedure affects?
Spinal taps are generally not painful. What you have to watch out for is a possibly ferocious post spinal tap headache if you’re not careful about lying down over the next day or so. Your neurologist should be able to help you with that. The lumbar puncture could be quite enlightening.
Was it Griffin (or Griffith) University in Australia that found a problem in ME/CFS patients with Calcium channels or something to do with calcium?
If so I wonder if this is why the medicine maybe beneficial?
Yes it was, Don Staines and Sonja Marshal-Gradnisik (my spelling may be wrong) at the NCNED at Griffith university who found problems with calcium ion channels (they take these to be the central issue in cfs) and suggest calcium channel blockers (which nimodine is) may overcome the issue.
I tried nimodipine (am in UK) 13 years ago, as did a friend, as it was talked about a lot at that time as Dr Mason Brown was interviewed in a UK ME charity magazine about it. Unfortunately for me I had no benefit, my friend a tiny bit. Admittedly, didn’t do the whole protocol detailed above.
Cort,
Great reporting as always. ? for covering the fatigue conference and providing us the link to tune in for free. You are awesome brother! Regarding Dr. Downing-Orr and her insight, research, and recovery: I strongly believe she is on to something. I haven’t tried the Nimodipine but I do supplement with L-Arginine to promote NO facilitation and vacillation. It works for me but sustainability seems to be an issue.
https://www.ahajournals.org/doi/pdf/10.1161/01.STR.25.2.429
In addition, I supplement with L-Glutamine for digestive health and also incorporate fermented foods such as kimchi in my diet. I also started intermittent fasting and it seems to be helping with energy production and digestion. I may try nimodipine if the nutritional holistic approach doesn’t pan out. I have a reoccurring c diff infection that comes and goes. I see a gastroenterologist in Dallas later this month. I may opt for a second FMT transplant. I also use psyllium husk fiber each morning to soak up the excess water and mucus in my intestinal track. This fiber works wonders! It actually helps with my diarrhea believe it or not!
Anyway, I just really want to reiterate how much your blog Health Rising means to me. I am very grateful Cort. This illness sucks but your site offers data, insight, spectacular reporting, and hope.
“I also use psyllium husk fiber each morning”
I am helped with psyllium husk too. No wonders, but slow improvement of my gut.
You seem to take it in one larger dose in the morning. Does it work better then taking some with each meal? Did you try at different times and the morning turned out to be the best time to take it? Is that with breakfast or do you skip breakfast for intermittent fasting?
It helps me with alternating diarrhea and constipation. That’s even harder to treat then one of both separate. For my gut and the alternating diarrhea and constipation learning and avoiding to trigger my food intolerances works even better, but psyllium sure helps. Pre- and probiotics often make things worse.
Hi Dejurgen,
I supplement with one rounded tablespoon of psyllium husk fiber (12g) every morning on an empty stomach due to intermittent fasting. I have not experimented taking it at other times of the day yet.
I find the link that Cort provided for the Fatigue Conference very useful. I just finished watching the interview with Dr. Wahls. Fascinating approach. Any thoughts regarding what she has to convey?
I absolutely love your approach to troubleshooting chronic illness from the perspective of a structural engineer.
Please keep the feedback coming. Sometimes I find it difficult to sustain incorporating lifestyle and nutritional changes but, intuitively, I feel it is paramount to do so in a consistent and regimental fashion.
Surprisingly, subscribing to functional medicine has resulted in more positive results than prescription medication in combating my illness. Initially, I was a skeptic, however, since embarking on the principles relayed by functional medicine advocates, I am gradually improving my QOL. Goal orientation, purposeful meaning, and problem solving have become cornerstones to my combative approach. Amino acid therapy and vitamin/minerals seem to be working, slowly, but, I am seeing progress. Data sharing is pivotal and I find Health Rising instrumental when it comes to sustaining this approach. This may sound generic and counter productive but, I force myself to stay upright and mobile within my own tolerance. My grandfather once told me, “A body in motion stays in motion. A body at rest stays at rest.” I just wish I could find the keys to unlocking the mysteries to solving my mitochondrial and metabolic dysfunction. I strongly believe that gut dysbiosis triggers this as well as neurotransmitter imbalance. One day at a time right? ?
12 grams of psyllium is way over my daily dose but then again I am a “go low on dose and keep it up in the long run” type of guy.
For those considering psyllium: many products contain FOS or another type of prebiotic. For some people products with or without it can have opposite effects. My food intolerances don’t allow any FOS.
“I force myself to stay upright and mobile within my own tolerance.”
I was never fully bedridden despite being hit quite severe at worst. In fact I couldn’t remain in bed most of the day. After about 10 to 11 hours of sleep at worst my body pushed me out of bed. Nausea, trembling and confusion were getting SO extreme late morning that I HAD to leave bed. I learned that it slowly improved upon sitting upright. In the beginning I had to use an armchair or table supporting me and protecting me from falling.
Recently I learned about orthopnea or breathing getting worse a lot by lying down. I seem to fit the description very well. Lying down can cause for a limited number of patients the lungs to get filled with water, making breathing very to extremely difficult. When getting upright, the problem disappears over time making diagnosis very difficult if you don’t have a commonly known cause to it such as hart chamber problems. I believe however that an inflammatory cause creating massive NETosis (a specific type of immune response) in the lung capillaries can be a cause to. With my gut problems I may have such source of massive NETosis.
“Drowning” in my own lungs at night may have caused my extremely strong breathing (and still needing more) late night, extreme adrenaline peaks at night with extreme nightmares (more then once involving drowning or suffocation) , the feeling that as if truck had run over my chest each morning, utter exhaustion each morning…
It also could explain why I likely (tests are inaccessible but signs abundant) had low blood volume: the lungs are a major source of chemicals sending the message “reduce blood volume” (probably in order to reduce said “drowning”). Poor blood volume is a secondary problem ending up being a cause of plenty of additional nasty symptoms.
It also may well help explain why we do “hyperventilate” and have very low CO2 levels in our blood while very low CO2 levels impair oxygen uptake. Having a large part of our lungs covered with too much water would reduce the speed of oxygen uptake a lot more then it would reduce the speed of CO2 removal if I understand correct. This would result in very low levels of CO2 if we are to have enough oxygen in our blood.
Too complicate matters: I do believe that many / most / ?near all? ME patients may suffer this to some extend. The reason that many patients feel better when lying down may be because many / most / ?near all? also have some form of OI. Then both lying down or being upright makes health worse. Which of both is worse is then a question of what factor is dominant.
I improved upon the situation by evolving to an intermittent pattern of being upright and lying down. The orthopnea problem is getting worse over time so getting up partially resets the problem. Unfortunately that means getting up at night and cutting sleep into pieces too. But if it improves health and quality of life enough :-).
I’ve written more on the topic on http://www.healthrising.org/forums/threads/pacing-problem-overwhelming-urges-to-do-more-than-i-should.6181/#post-35165
I’ll have to look at Dr. Wahls website later as I missed the webminar.
Many ME/CFS have breating problems including “air hunger”, however, I have yet to read anywhere where fluid in the lungs would have been confirmed as the source of this. Breathing problems related to changes in position was one of the symptoms of Jen Brea, in fact, she had it so bad that her breathing intermittedly stopped. Jen’s problems all resolved after having a CCI surgery, which suggests that compression of the brain stem was the source of her breathing problems. I think CCI and brainstem problems could potentially be a major source behind many people’s ME/CFS.
What neurotoxins do they believe are the culprits? Having used the Cutler protocol to some effect, mercury in the brain has seemed plausible to me. Another possibility, one that has had much less attention, is magnetite nano-particles. See here:
https://www.smithsonianmag.com/smart-news/your-brain-full-magnets-and-you-might-not-reason-why-180960353/
While magnetite crystals are naturally produced in the brain — though its function is not understood — these particles, which are produced by diesel engines, might well cause inflammation and/or interference with the natural function. Around the world diesel vehicles are being moved out of cities, as quietly as possible to minimize liabilities, but this particular pollutant is still little publicized. Could Nimodipine help to flush such particles out of the brain?
The book didn’t say but with Ron Davis finding high levels of mercury and low levels of selenium in about a third of the severely ill patients in his study, detoxification may become a more important issue.
Molybdenum & selenium are low in my case.
Mercury, lead, arsenic are high.
And then there’s ammonia (from the gut?) also high. Plus kyuneric acid also high (in line w/ recent findings kyuneric pathway problems).
So: a lot of neurotoxins & little detoxifiers present.
“And then there’s ammonia (from the gut?) also high.”
I would guess ammonia comes from peak/burst consumption of amino acids. During anaerobic functioning, amino acids are consumed as energy source at a high rate. Amino acids are a source of nitrogen and leave ammonia as waste. That ammonia waste is then converted to uric acid and other less harmful products.
I guess that, if small exertion drives part of our body (brain, muscles) into anaerobic functioning often then a local peak in amino acid consumption produces ammonia at a higher rate then the body can detoxify.
Note: there are indications many patients have elevated levels of lactic acid all day round indicating that they may have anaerobic functioning in the body at times and places (the brain) they should not have. With that may come more ammonia then the body can comfortably detoxify. Ammonia in the brain for example can cause brain swelling, something which would lead to higher CBF pressure.
Here’s a case of mercury poisoning that was cured with…selenium and n-acetylcysteine:
https://www.tandfonline.com/doi/full/10.1080/24734306.2017.1392076
Also, regarding ammonia and kynurenic:
Kynurenic can be high because of insufficient niacin. The body produces kynurenic acid in the process of breaking down tryptophan to make niacin, so if one is getting enough B3, then that stops the tryptophan breakdown into kynurenic (and also quinolinic) acid.
Ammonia can come both from the gut, in response to an acidic body, in an effort to alkalize the system. But can also come from muscle breakdown, if one’s krebs cycle isn’t burning carbs and fats for fuel.
Complicated, but there are some ways to dig out of this horror.
@dejurgen … you got me thinking about possible CBF pressure & other things You wrote on this thread.
If i sleep too long my body pushes me out of bed too. Waking is sheer horror. I cannot stay in bed (like You) & need to get out.
When i sleep long hours (used to be 1,5 of sleep but now it’s ‘Comasleep’ … my eyes are very very puffy & eyelids are red.
And … my ears started ringing last year (i got worse since end 2017). Of Which i’m Sure it’s not tinnitus. Why sure? Because it Goes away sometimes & it’s more of a pulsatile noise (like bloodstream or sth).
If i don’t hear it its on the “better days”. But it can start again after doing sth that involves postural changes.
Tbh sleeping too little isn’t a good thing but i do feel better when i sleep little regarding all thes issues.
Btw: if i take a nap during the day? Sometimes i feel horrible too & the ringing starts again.
How to test for cereblal pressure though?
O, And i do have apneu & “breathing flattening” & alpha intrusions & micro-awakenings in sleeptests. The breathing issue was a bit of a mystery bc they said it was only seen in obese people (i’m slender).
Sth else: breakdown of muscle fibers. They did find fats & muscle fibers in my stool. So that cld fit too.
Your way of thinking intrigues me. A lot fits.
When Reading another post of Cort on mcgregor he thinks glycolysis is the main problem regarding kyuneric acid etc.
Keep Wondering if CCI Could possibly account for these things. Otherwise it’s Inflammation driving it all.
@Marcia … Thank You!
I’m going to start taking niacin i Think. Read it a few times the last days. Also how niacin can bypas the IDO2 issue that’s Spoken of lately. And it’s a calcium blocker it seems? (Calcium is too high in my tests)
Warning, a similar calcium blocker, amlodipine, almost killed me last year. Within 5 days it brought my RBC, hematocrit, hemoglobin and platelets down to alarm levels on a standard lab report and destroyed most of my WBCs, too. Fortunstrly, I had stopped it in my own due to severe fatigue, but if i hadn’t, I’d be dead.
Its always interesting yo hear what has helped others, but this protocol is no panacea. There is nothing to tackle infections, autoimmunity,mast cells, and hormone deregulation. And detoxing will help many of us, but taking a little milk thistle won’t do much if one is really toxic – it’s going to take a more robust approach.
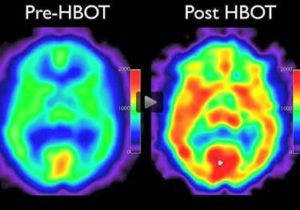
I do HBOT 2-3 times a week, which has been helpful – thanks for sharing the SPECT which illustrates why.
Whoa! Do you have any idea why that drug had such a negative effect Learner?
I, too, thought the protocol was pretty basic – the addition of Nimodipine was very interesting, though. I imagine if the protocol was created now there would be more to it.
https://www.ncbi.nlm.nih.gov/pubmed/26300312
J Chem Neuroanat. 2016 Sep;75(Pt B):43-51. doi: 10.1016/j.jchemneu.2015.08.001. Epub 2015 Aug 21.
Microwave frequency electromagnetic fields (EMFs) produce widespread neuropsychiatric effects including depression.
Pall ML1.
He talks about calcium channels that somehow are affected by electromagnetic radiation. I don’t know how much proof he has of this. Certainly the research I have seen about electromagnetic radiation before, that the policy of safety is based upon, has been really bad, with few people /mice and only short term.
Anyway, I also wondered about electricity in the completely opposite way: To use it to make the blood flow better. Here is from wikipedia: https://en.wikipedia.org/wiki/Hemoencephalography
I am just now waiting for a device I can use at home for neurofeedback, so I don’t even have to leave the house. I figured out that it also works for hot flashes, so if I can cut down on Neurontin to around one capsule daily instead of ten, I save the price of this device after one and a half year.
Neurofeedback is a lot less dangerous.
I’ve heard of people who have done well with neurofeedback – although if I remember correctly, it can be fairly intense too!
Good luck and please let us know how it goes.
A natural calcium channel blocker (full spectrum K2) along with magnesium and calcium, in theory should have the same results without the side effects of the pharmaceutical drug.
Research should definitely look at increasing ME patients blood flow to the brain.
Natural methods are the preferred way to get this result.
Very interesting story Cort. Thank you very much for sharing!
Your contributions to the ME community are greatly appreciated!
What dosage of K2, magnesium and calcium do you suggest? Are there certain proportions to be used?
I was put on nimodipine after suffering a sub-arachnoid haemorrhage and brain surgery, I can’t say I noticed any major difference but then things were a tad traumatic and I didn’t follow a slow build up or any of the other recommendations LOL, definitely one to look further into methinks
I am a psychiatrist in Texas. Many years ago, 20+, I read a letter to the editor in a medical journal about using Nimotop for Treatment Resistant Depression. I had a patient at the time who was miserably depressed and was failing to respond to all my usual treatment strategies. We elected to try Nimotop and were delightfully surprised how well it worked for his depression. He remained well for many years on it, until I finally lost contact with him. I have tried Nimotop a couple more times in other patients, but without success. It is not a mainstream treatment and does not work for everyone. But, it is nice to see that it may be beneficial for ME/CFS.
Thanks for passing that on. 🙂
Hi Thomas. Where are you in Texas and do you treat CFS in your clinic.?
Kelly, I recently closed my medical practice after 30 years. So, I’m sorry to say, no. Many of my patients suffered Chronic Fatigue Syndrome, but I was primarily treating their depression or anxiety. I also saw a lot of Fibromyalgia. I am following this website, Health Rising, because I never did find a good treatment for either one. I don’t have these conditions myself, but I have a loved one who does. I’ve tried almost everything within reason, (there is a lot that is not within reason). We are all ready to find a cure… right?
Cortef was used was small doses like 5 mg to max 10 mg daily by Dr. Beverly Pearson Murphy in Montreal for years with treatment-resistant depression & CFS patients Published as well…I know many who have great success it is the only medicine aside
from Prednisone small dose to have helped me it is a difference between night & day. Out of the 2 medicines I preferred Cortef the best…I still feel ME/CFS is Eagle
Syndrome I have seen too many people with CFS diagnosis recover with proper Surgeries removing the full bones, not partial removals…I cannot understand why more are not doing the proper CT Contrast images & 3D ones are best…There also
may be links to Poisoned by Antibiotics one Scotish Doctor wrote a letter to the Editor on the ‘The Eagle has landed’ saying her illness Eagle Syndrome was a result of being given Cipro..I have an abnormal Panoramic dental x-ray, now I am trying to
get a proper CT Scan done & it also can come with Syncope, spinal fluid leaks & increased intracranial pressure…The Vascular type can also block major Arteries & drops in blood pressure & Brain fog are common…ES is not rare it is rarely
diagnosed or even dismissed as anxiety or depression…We Need someone to do numerous patients with proper scans & good skull based Surgeons…I have also seen some who had all along another illness (HFI) Hereditary Fructose Intolerance instead
I find your comment interesting. Before Tramadol became a class rated drug, it too was used for people with resistant issues with depression. When other things didn’t work, Tramadol did. It was being used off label. Since it has properties with all the neurotransmitters and moderate NMDA channels (glutamate connections) I think this may be why it helps the high sympathetic dominance associated with Hyper POTS and high standing NE levels. It may balance that out as well as serotonin and dopamine. Keeps me much more balanced with my POTS. The Bentyl was initially given to me for IBS. But I find taking it with Tramadol makes a better combination. Helps spasms associated with FMS and EDS. Too much of it, however, will cause depression. Staying low on both things and cycling them, keep them working at very low dose. I wonder if this calcium channel blocker would be as good as my combination. Since there is now alot of frown with RXing Tramadol. Even to very Conscientious users.
ISSIE
My Medical Doctor attended a conference in the USA last year on Opiate treatments and told me that Tramadol was deemed an appropriate and safer pain reliever than the other Opiates. I’ve been on it for 20 years. I was first prescribed Tylenol #3 and then Oxycodone, but both eventually lost their effectiveness. Tramadol works the same every time without having to increase the dose. I take 50mgs every 3-4 hrs regularly so my pain doesn’t get away on me. There is a sustained release version of Tramadol, but I cannot tolerate it’s 100mg dose. I find that Tramadol gives me energy as well as pain relief.
Thanks for this, great as always Cort.
Good to see something interesting coming from the UK for a change.
Does Dr Brown still prescribe? Does anyone know if other GP’s in the UK prescribe Nimodipine?
I had a look online and couldn’t find anything.
The book, which is almost ten years old, said he had a website but I couldn’t find it. I imagine that he has been retired. Check out Susan Parker’s 34-page overview of Nimodipine and ME/CF for some GP’s who have used it
.I think of the review as “Everything you always wanted to know about Nimodipine…” – https://www.actionforme.org.uk/assets/components/discuss/attachments/2/6193/nimodipine%20use%20in%20me,%20jan%202014.pdf
What the hell ever happened to Dr Goldstein?!
Others will know better than me but it was not a happy ending. As i remember the author and pioneering physician was forced to leave his practice at some point and retired.
Check out the top 23 drugs Goldstein found helped most in ME/CFS. This was decades ago – Nimodipine was 3rd!
https://www.healthrising.org/forums/resources/dr-jay-goldsteins-top-23-drugs-for-chronic-fatigue-syndrome-me-cfs.341/
That, in itself, says a lot to me about Goldstein. I never hear of doctors in the U.S. using this drug but Goldstein, decades ago, found it quite helpful at times. A very innovative man – perhaps too innovative for his own good. Something happened to bring him down.
His Illness Turret’s forced him into Retirement Dr. Goldstein he became very ill I heard
Interesting that some of the meds he used are used for MCAS and allergies and others cause vasodilation.
I was hospitalized once for mast cell attack to heart called Kounis Syndrome. Treatment is massive antihistamines and nitroglycerin. Both which worked. They thought I was having a heart attack. But no muscle damage.
My help with GastroCrom, vasodilates and helps mast cell issues. Is also mild calcium channel blocker.
Issie
As a clinical psychologist with FM, I’ll say those CBT descriptions are the same plain vanilla CBT techniques that could help with ancillary problems of most chronic disorders. I don’t think psychology has much to add to ME or FM treatment unless you find a placebo that works or respond astoundingly well to hypnosis for pain control. I didn’t.
That’s how Dr. Downing-Orr presented them in my opinion – as general recommendations that might help with those suffering from chronic illnesses. It’s interesting that she, a hypnotherapist and NLP practitioner, didn’t, I don’t believe mention those.
An upcoming blog will feature Buddhist approaches to pain.
Nancy B, another one of my POTS friends says she felt awful with Tramadol too. Another guy tried too large a dose and slept for days and felt really drugged. When he cut way back, he said it helped him, then. I take any where from 25 to 50 mg, usually once at bed. It can be RXd up to 100 mg and is usually RXd about 4x a day. What I take is a very low dose. When it stops helping, I go off and stay off several weeks and go back on 12.5 mg to start. However low I can keep it, is where I stay. I was originally given this by a Mayo doc for FMS. Was told to take it 4 times a day. It really doesn’t seem to help completely alleviate pain, but does take the edge off.
Yes, we really are all different. What may be causing my issues will not be the same for someone else. There is no one magic pill or protocol for the masses. We have to figure out where the dysfunction is and then “fix” it. Ask WHY first and don’t just treat the symptoms as they may be trying to tell us something very important. Symptoms could be a compensatory response and the lessor of the evils. We could be undoing our body, when it is trying to save us. Maybe the approach needs to be through a different door.
Issie
When the knowledge of general internist and the knowledge of psychopharmacology expert come together in one person, powerful conclusions can be drawn, as was demonstrated by late California physician Jay Goldstein MD.
Back in the 90s, Goldstein has pioneered the treatment of what he referred to as “neurosomatic conditions” through adjusting neuro settings via art and science of neuromodulation, also commonly known as neurohacking.
In his office, Goldstein fearlessly administered various intravenous protocols and prescribed everything under the sun inspired entirely by his extensive knowledge of neurochemistry and a cowboy attitude.
Jay Goldstein had no moral dilemma about what he was doing. In his book “Tuning the Brain” he explains that by the time patients reached his office, most of them have tried everything else and were so sick that they considered suicide as their most viable option.\
Through manipulating their neuroreceptors, Goldstein claimed that he was able sooner or later to fix 90% of them, but what was really remarkable is that whenever he hit the right combination of drugs, the patients had a near immediate resolution of all the symptoms that plagued their life for years.
Because what he was doing did not abide the laws of evidence-based medicine, Jay Goldstein eventually lost his medical license, went broke and eventually ended up dying in poverty, around the same time when I discovered his book. I never got a chance to tell him that reading his book has saved my life and forever changed its trajectory (despite the fact that at the time I could only understand about 1% of it and even unrelated to my ignorance, it would be fair to describe it as one of the most incoherent books ever written).
from:chronic fatiguediagnostics.com
Really? I didn’t know it got that bad….Darn!
I do remember reading that he didn’t care about the money and his practice either made little or none.
With his books – which are still being referred to – he was clearly highly committed to figuring out this illness.
Thanks for such an interesting article, Cort..I did know about the work of Dr. Kristina Downing-Orr, and Dr. Mason, ….fascinating. However in Canada, Nimodipine is extremely expensive, and not without risk…I did do the protocol for a short while, and noticed no difference in my symptoms. If I am not mistaken, Dr. Kristina Downing-Orr died in 2014.
It’s about $1/pill at canadaprescriptionsplus or northwestpharmacy
I have tried this protocole and put a lot of energy into it after buying the book. I followed the protocol (medical) with great care but unfortunately it didn’t do a lot for me.
At first I thought it helped but as the years passed (I was on Nimotop for more almost 3 years) I kept slowly declining so I had to admit that it wasn’t helping as much as I thought. I stopped taking it a few months ago.
Thanks for providing your experience Sadie. We are a mixed lot aren’t we? Good luck with your continuing search for better health!
Yes we are a mixed lot, aren’t we? Tramadol is a nightmare for me–brings on migraines and I feel like I am swimming underwater in some kind of disassociated reality! And didn’t hardly do a damn thing for my pain–the very reason it was prescribed!
Now, regarding Nimotop and the other list of recommended medications; I ran into a small personal blog of a woman who has tried a large number of medications (including Nimotop) for her ME/CFS. I offer up that list to you all; http://www.fiikus.net/?cfstreatment
Even though it is difficult to predict what will help who, she provides some personal feedback and advice on each. As far as calcium channel blockers purported cognitive benefits, she finds that nootropics, especially Piracetam to be more helpful for her.
I suppose a multi faceted approach (diet, exercise, medication etc.) will be best adapted for many–depending. I find it interesting that Dr. Bateman emphasizes autonomic issues while Stanford seems to be focused on post viral problems. Dr. Bonilla (Stanford) didn’t seem to be interested in any of my dysautonomia. He was however, especially excited about a brain inflammation study (Yasuhito Nakatomi et al).
And regarding the comments on psyllium fiber, I do remember reading about the gut microbiome really liking vegetative fiber to stay healthy and well populated (gut brain axis and all). I do recall when I was eating pounds of farmer’s market produce that I felt much better. Now it is difficult to find the energy for all that food prep…
Cort, I once again have to compliment you on your extensive research, especially your database of past postings/information. I’m convinced that there are all kinds of sub-classes of this disorder, and so the more options that are discussed, the better for us all.
I’m slowly titrating up on my apriprazole and am noticing a small uptick in energy. But then, unfortunately, the ‘activity switch’ still gets suddenly turned off leaving me crashed out on the couch. And I still can expect to limp along after a difficult day–sigh.
Kindest wishes to everyone!
Cort. I had to chuckle at your sentence saying… if I was an author… you are an author and an excellent one at that! I know you meant book author, but wanted to affirm your talent and skill as an author and affirm your very helpful ongoing writings which by now would likely fill several books! We all benefit from all that you write which is sometimes the only ray of hope in this difficult place we find ourselves. Thank you.
When combining the ongoing discussion I have with Issie (thanks for adding the link! brainfog) on https://www.healthrising.org/blog/2019/05/29/spinal-stenos I was confused about the (amount of) opposite effects calcium blockers seem to have on cells.
Then I thought about the beginning of our discussion: calcium metabolism having near opposite effects on the arterial part versus the venous part of the blood flow.
When reading the many different outcomes from patients who have tried them it further raised my suspicion. Then I saw a patient got edema from it. That is a red flag.
So I looked up “calcium channel blockers arteries veins” and the first link was a hit:
http://www.ncbi.nlm.nih.gov/pubmed/2820194:
“it was found that nifedipine was the most potent relaxant agent in both arteries and veins, but that this drug showed no preference for any type of vessel. In contrast verapamil (10(-6) M) and (10(-5) M) diltiazem, flunarizine and lidoflazine inhibited the NA-induced contractions to a significantly greater extent in the arteries than in the veins. Comparison between diltiazem and nifedipine on contractions induced by cumulative addition to NA showed that both drugs had significantly more depressive effects on arteries than on veins if the vessels were contracted by relatively high concentrations of NA (10(-6) and 10(-5) M). The results thus confirm the clinical finding that CCBs have more pronounced effects on the arterial than on the venous side of the circulation.”
=> Now having different effects on both arterial and venous side is a MAJOR thing!!!
It means a huge difference on the impact on blood flow. In the following I assume most patients have problems on both arterial side as well as on venous side. But one problem may largely dominate over the other depending on patient characteristics.
For example one patient can have too narrow arteries as a major problem. That would impair blood flow towards the organs including the brain. Giving a (optimal dose of a) drug that improves artery dilation may help a lot.
But give that same drug to a patient with dominant problems in the veins and more blood flows toward the organs while drainage remains as poor as ever. That will cause massive and dangerous edema. This edema may even go undetected:
* the edema could be clear by swelling up in the legs, I guess that would be rare.
* the edema could increase water in the lungs a lot, which consequentially send potent chemicals in the bloodstream screaming “decrease blood volume ASAP, we’re drowning”. This may “solve” the edema at the cost of very low blood flow yielding very poor functioning of brain, muscle and all other organs. Yet the edema will be undetectable as it’s removed by decreasing blood volumes so badly.
* the problem could be “solved” by an increasing strength of the “intermediate” option: spread symptoms over reduced blood volumes and partial edema in lungs and brain. This would give plenty of (increased amounts of due to the poor choice of drug) symptoms due to decreased blood volume, increased (intermittent) problems of water in the lungs and edema (swelling, high CBF pressure and resulting decreased blood flow to the brain as high CBF counters blood flow towards the brain) of the brain.
Rather then ME causing one type of secondary problem with blood flow, it may exacerbate existing weaknesses or tendencies in patients. That would necessitate a tailored and well thought approach in order to not create havoc.
One size does NOT fits all!
Important additional note:
Calcium blockers may or may not make BOTH arterial blood flow and venous blood flow worse yet result in health improvement. Changing the balance of both is an important factor in health that *in some cases* could dominate both getting worse. On the other hand for some all could get worse… So be utmost careful and consult experienced professionals! Even if it works, dosing may be vital.
Hmmmm, when I tried a calcium channel blocker by itself, it was too much for me. I do tend to have edema and blood pooling in my feet. I blamed issues with kidney function as partially responsible.
Having high NE with my subset type of POTS, moderation completely was a disaster for me. I feel the higher levels help with me. Though very uncomfortable. If I moderate my sympathetic system, but not completely…..I’m better. Too much suppression and I’m nonfunctioning.
Issie
Hi Issie,
Your comment is cryptic so far. It seems you are still weighing factors.
I pick up these points:
* Normal doses of pure calcium blockers are having too much side effects or further dis-regulate things.
* Edema is clearly visible but only in legs (reduced compared to “typical” female leg edema).
* The kindney function you stated in previous posts is not clinical confirmed but more of a logical conclusion regarding “water household problems”.
* You “need” a certain amount of “stress” (more precisely you need elevated nor-adrenaline and adrenaline levels) to let you feel better and more energetic.
Please correct or adjust where appropriate.
=> I have the latter too but with extreme levels of adrenaline and exceptional tolerance for it’s side effects. Side effects are massive and very disturbing, but I can get adrenaline levels very high while still having a net positive effect on health.
=> Would that also mean you “cringe” when doing extensive meditation and yoga techniques making you feel extra wired (likely as a response to trying to reduce NE levels)?
Your combination of observable edema (uncommon with ME patients IMO) and overt POTS seem to be in line with my idea of having a combination of masked “critical organ (brain, lungs…) edema” that is countered by reducing blood volumes, blood flow, blood pressure, water excretion, and “conjuring up” high to very high levels of NE and epinephrine / adrenaline when you get quickly into upright activity (or any elevated exertion).
=> Would you see that description as fitting or wish to change / add to / counter it?
As to what “critical organ” is affected so much by “masked edema”, would you:
* have increasing difficulties breathing as the night progresses?
* have near daily very strong (pressure ) headaches and feel difference in it using ice packs on your head (as a sign of periodically far too high CBF pressure (or have confirmed too high CBF pressure)? If so, when do they occur during the day?
At first glance and remembering previous comments I would not rule out you have some of the first but the second seems more likely to be overt in your case. Would that be a correct guess?
Kind regards,
dejurgen
Note: if you might have GERD, you might consider “masked lung edema” as GERD is said to be able to cause lung damage and according inflamation / fluid in the lungs.
http://www.livestrong.com/article/215674-acid-reflux-and-the-lungs/
“Aspirating large amounts of gastric acid can cause a chemical burn of the airways and lungs, leading to restriction of airways, fluid retention in the lungs and a form of pneumonia known as aspiration pneumonia.”
GERD is fairly common with people with ME.
Dejurgen, I’ll try to answer some of your questions.
I had Chronic Kidney Disease level 3 and reversed it to level 1 by being a vegan for about 3 1/2 years. Still have to be careful not to have too much meat protein and very limited protein with lectin. I also intermittent fast in a.m.
I have severe feet edema, at times, and occasional legs and hands. Obvious blood pooling with purple coloring if feet are down too long or I’m having a very bad POTSie day.
I’m thinking that my high NE helps with blood flows and vasodilates. (Body compensation. ) if I suppress it too much all my issues get worse. I can lower it a certain amount. But I’m also slightly vasodilating and thinning my blood at same time. The Tramadol works on other neurotransmitters and NMDA which can cause a Hyper response. Things I use have calcium channel blocking properties. But, not to extreme amount of a true calcium channel blocker. Or at least not the one I tried that didn’t work well for me.
I’m pretty mellow personality wise. But dont do that type meditation. Studying and pondering are more my type meditation. I can sit quietly without issue. In fact, when I did some yoga, I found it very easy to go into the zen.
With HyperPOTS, we go above 600 with standing in our NE. Mine is nearly 900. This isnt the norm for most people.
I have to sleep with my head up. Alot of POTS people find this very helpful. Some have found hydrocephalus and this helps drainage. I dont know if that’s why it helps me, but maybe. I will get a bad headache flat and also feel like I cant breathe. Will send me into a stress state, create mast cell response and trigger POTS.
As far as I know, I dont have GERD. But I do have both forms of sleep apnea. Central and Obstructive. This is common with EDS.
I dont know if this calcium channel blocker would work as well as my combination, but I’d like to try it. Have a message in to my doc. We will see what she thinks.
Issie
“I had Chronic Kidney Disease level 3 and reversed it to level 1 by being a vegan for about 3 1/2 years. Still have to be careful not to have too much meat protein…”
There is a link between calcium problems and kidney disease. kidneydiseaseauthority.com/high-blood-calcium-and-kidney-disease:
“Continual high levels of calcium in your blood can damage your kidneys”
Going to a vegan diet and reducing meat protein is said to improve calcium balance and reduce bone decalcification. I read you had calcium problems in the past.
Regarding the edema – POTS relationship:
“Obvious blood pooling with purple coloring if feet are down too long or I’m having a very bad POTSie day.”
“I have to sleep with my head up. Alot of POTS people find this very helpful. Some have found hydrocephalus and this helps drainage. I dont know if that’s why it helps me, but maybe. I will get a bad headache flat and also feel like I cant breathe. Will send me into a stress state, create mast cell response and trigger POTS.”
=> It seems you describe a direct link between edema and POTS pretty well IMO. Next to the overt edema problems, it seems that the headache and breathing problem *when lying flat* could indicate a fluid accumulation aka edema problem in lungs and brain. Does it get worse if you stay lying down for a longer time?
The mast cell activation gets interesting en.wikipedia.org/wiki/Mast_cell:
“A mast cell (also known as a mastocyte or a labrocyte[1]) is a resident cell of connective tissue that contains many granules rich in histamine and heparin.”
http://www.wisegeek.com/what-is-a-mast-cell.htm
“Heparin prevents blood from clotting to allow blood to flow to the area of infection or injury”
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4701915/
“vasodilators accumulate within the tissue resulting in higher than normal blood flow for a period of time when blood flow is restored to the organ.”
Now plenty depends on *where* the mast cell activation happens. Have it in the arterial part and blood flow increases and fluids aka swelling aka edema increases. Have it in the venous part and both the anti-clothing effect of herapin plus increased drainage decrease edema.
Combining
“Obvious blood pooling with purple coloring if feet are down too long”
“herapin prevents blood clothing”
“mast cell activation when lying down”
“mast cell activation causes vasodilation”
I’m tempted to say:
When upright: excess fluid sinks to the feet
When lying down: excess fluid dis-appears from feet, has to go somewhere else.
When lying down: excess fluid goes to lungs and brain
When lying down: mast cell activation happens
=> I would like to add (speculation/educated guess):
When lying down: mast cell activation happens at places where excess fluids stack (very likely the venous part of the capillaries)
If mast cell activation happens at the venous part of the capillaries: should have a edema draining / resolving effect => reducing lung “drowning”
Similarly, in the brain glial cell activation might try and reduce brain swelling/edema and all of its side effects. (I’m guessing in the brain glial cells will take role of mast cells over, need to look into it further but ME glial cell activation is common)
=> My gut feeling says:
your POTS (reducing blood volume = less edema problems) and mast cell activation (having potential for *local, where needed the most* draining edema) seems to be (lung and brain) edema activated
As to NE and E, I may be an extreme E person and be a poor reference. Upon improving however this year levels have dropped so much that I feel like kind of ta different person but levels are still above normal.
Thanks for all the possibilities. With the complexity of our symptoms, I’m certain there can’t be a one thing fixes all. Too many variables and differences between us all. We have to figure out the WHY first. Maybe a genetic predisposition and something triggered epigenetic change. If that happened, figuring out a way to “flip the switch” to different direction. Yet, if our symptoms are compensatory – we have to make sure treating them doesn’t make things worse in long run. Our body could be trying to save us. I’m still on the Quest. I have alot of my WHYS, but figuring out what to do about it…..so much to still learn.
Issie
Hi Issie,
How do you notice, measure, observe, diagnose… mast cell response? How do you pinpoint it to a certain moment? Can you pinpoint a certain area too?
“I will get a bad headache flat and also feel like I cant breathe. Will send me into a stress state, create mast cell response”
Mast cell response can cause all types of symptoms. Redness, flushing, problems breathing……many more. It can be caused by so many things. Not a true allergy but an over response of histamine release. It can happen with exposure to something, over heating, strong emotions and stress in general. Is very unpredictable. I get numbness in my face with it. It can causes emotional liability when it happens. With me, I also get hot flashes with it. Very uncomfortable thing to deal with! I use H1 and H2 blockers daily and GastroCrom. Of recent trying out Blackseed oil. Seems to help some.
You may find this interesting. Just ran across this.
https://newatlas.com/artery-stiffening-calcium-minocycline-cambridge/60088/
Interesting that Dr. FRY uses Doxycycline along with antifungals to treat fungus found in the blood. He has found it contributes to plaque. It forms biofilms. I was on it for years, but couldn’t tell it did much for me. Maybe it was and I just didn’t know it. He told his patients that magnesium and calcium and fish oil feeds this. He didn’t want us to supplement them. He also believes in a vegan diet.
Issie
I asked my doctor to prescribe this for me so I could try it about 6 weeks ago. For me, I felt more tired than ever and strangly was smelling like a hound dog and things that others didn’t smell. The wierd part is, it is mainly in my house. My boyfriend just descovered a small AC leak in a pipe that leads to the unit inside the house. Don’t know if that is what I am smelling. Currently don’t have the money to call soneone in to replace the leaking pipe and refill the freon. Well I have the new stuff they are using that is suppose to be more environental friendly. Anyways, I stopped taking it 2 weeks ago. No improvement in 4 weeks taking 100mg 3x/day. But I am going to start taking it again cause I had this illness (CFS and Fibromyalgia) for 13 years now and know I should of taken it longer. The smell was just driving me nuts. Since I quit I still smell it but to a lesses degree. Guess it increased blood flow to the part of brain that is responsible for smelling.
Are you taking the Gingko biloba and other supplements recommended. I wonder if those could help. Good luck!
I apologize. What I am taking is Pentoxifylline 400mg 3x/day. This med also increases blood flow to the body that has low blood flow such as the brain. It obviously didn’t help my brain fog. Sorry about my 1st post. But no Cort, I am not taking those other supplements mentioned in this article. But I am going to further investigate it. Maybe that is part of my problem. I found out about pentoxiflline on my own on the internet. Although not a calcium channel blocker, SPEC scans show people who took this drug had improvement in blood flow to their brain, as hyperbaric oxygen treatments do with patients that have certain illnesses such as CHF and Fibromyalgia.
“Pentoxifylline is a prescription drug used to improve the symptoms of a certain blood flow problem in the legs/arms (intermittent claudication due to occlusive artery disease).”
There’s no mention of brain blood flow in the description at rxlist.
Nimodipine is one of the handful of many, many things that I have tried that actually produced some positive results. I tried it off and on for several months and then my insurance would no longer cover it. I did not always get consistent results and sometimes had to increase or decrease dosage. I usually did better by continuing to increase dosage. There were a few periods taking it when there were startling relief in symptoms and others when it didn’t seem to do much. If it was affordable I would definitely take it again but I wonder why it seemed so inconsistent.
Hi Cort, really excited to see you feature Nimodipine. I was surprised you hadn’t heard of it and dismayed that something anecdotally reported to help many people has slipped out of awareness and research over the years.
I started taking it a few months ago after reading Jay Goldstein’s book ‘Betrayal by the Brain’. It’s still early days (though definitely post-placebo) but I have felt what I would describe as an improvement in functionality. It’s difficult to say how much. Probably a little – 10-20%, say – but any improvement is welcome. Physically I would say I have a bit more energy but it still doesn’t take much for symptoms to worsen or PEM to be triggered. It doesn’t seem to have helped with muscle pain, nor the constant flu-like feeling of immune system deregulation. I also still suffer GI disturbance and an array of other symptoms we’re all familiar with. It might have helped improve cognitive symptoms which is possibly what in turn has given my energy levels a little boost.
I’m coming to the end of the first box of tablets and am unsure whether to continue. I had to pay for it through a private prescription as it’s not available on the NHS in the UK. I subsequently asked my registered GP about it and unsurprisingly he had no idea. He looked it up and said it had a ‘red flag’ which probably just means the NHS isn’t prepared to pay for it or that it’s repurposing for ME/CFS is way too leftfield for the mainstream medical mind.
I may press on or may take a break then reassess. I was kind of hopeful about it at first but my body seems to have fallen back into the same old (metabolic?) trap. I’ll let you know of any significant developments.
I admit I haven’t read through all of these comments, but I’d like to know if anyone has tried using nimodipine with success. I’ve tried many things that haven’t worked for me, but some have helped. My concern with trying nimodipine is that I have low blood pressure most of the time. I’m wondering if it would be likely to make my blood pressure even lower…. I guess I could ask my doctor, but I’d like to know if anyone has had experience with this drug first. Thanks.
In another disease MS with no attribution to ME/CFS, researchers have found:
Low found low blood volume in MS
BLOOD STARVED MS
https://multiple-sclerosis-research.org/2019/03/blood-starved-ms/
Nimodipine treatment can cause :
Reversible cerebral vasoconstriction syndrome (RCVS)
https://multiple-sclerosis-research.org/2015/08/neurospeak-reversible-cerebral-vasoconstriction-syndrome-and-fingolimod/
in a small number of patients
In Fecal Microbiota Tranplantation FMT
https://www.fda.gov/vaccines-blood-biologics/safety-availability-biologics/important-safety-alert-regarding-use-fecal-microbiota-transplantation-and-risk-serious-adverse
One must be responsible along with their practitioner to conduct due diligence with regards to any off label use for treatment and the potential for serious side affects.
1) You’re confusing low blood flow with low blood volume;
2) Nimodipine successfully treated the RCVS, it didn’t cause it;
3) This post isn’t about FMT.
Sorry, no points this round, Eco! But show those comments to your doctor and I’m sure he can use them to justify your rx for nimodipine (with “attribution” to cerebral blood flow deficit).
Have not been here for quite a while, but many familiar themes. What has worked for me for what it’s worth.
Chlomipramine Hcl (Anafranil) fixed most of my alternating constipation/runs. 29 years and counting. I believe the cause was low serotonin which governs gut motility.
Modafinil 15 years, helps with brain fog and mental concentration.
Melatonin less than 0.1mg helps with sleep, any more and I feel hungover for 1-2 hours
Psyllium Husk with Inulin 2-3 tsp before breakfast. Helps with constipation. The brand I use is Lifestream. Bowell Biotics Fibre + Enzymes
Colchicine- this is a gout medication but I take it for its side effects. It would give a normal person diarrhea but keeps me more or less normal, otherwise I am constipated. I take 2 with breakfast and 2 with dinner. Used to be 3 but something has changed.
I inject 1ml of Copper Chloride every 2 days as I have strange malabsorbtion problem, cannot absorb via gut- very rare. Compounding chemist makes me sterile solution. Australian soil is deficient in Copper and Selenium.
Also inject B12 once per week.
I take a bunch of other vitamins and stuff but will stop here to keep it simple. I was able to keep working after major dysfunction from about 1985 till 1990. I retired 3 years ago, probably have 70% normal function most days. Interested in reading this book as I’ve heard about the blood flow thing before, never knew there was a drug.
Hi all, not sure if this thread is still active, but is anyone out there still following the nimodipine protocol?
I read Dr Downing-Orr’s book recently and convinced my GP to prescribe it for me. I’m now four weeks into it (taking 3/4 a 30mg pill in the morning and 1/2 in the afternoon, along with the recommended supplements) but can’t honestly say I’ve noticed any improvement. I seem to be on the usual roller-coaster of good days and bad.
Although the success rates in the book seem amazing (80%), has anyone here seen any progress? If so, at what dosage? I’m loathe to keep continuing without some hope that it might be working.
I should add that I have what is probably considered mild CFS/ME & fibromyalgia. On most days I’m able to function and work (albeit in an office – currently from home), but as you all probably understand it’s had a shocking impact on my quality of life.
Some people are showing improvement while others aren’t – which is pretty typical. The 80% rate seemed too high from the beginning but the drug is definitely helping some.
Waitaminute, aren’t -pine drugs psych drugs? So we move from GET and CBT to mental drugs? Whatever happened to “cytokine fingerprint” and such?
Just a coincidence. Nimodipine is a calcium-channel blocker.
Dr Peter Novak has had some success treating patients with OCHOS with calcium-channel blockers. He hasn’t published any research on this, as far as I know, but it is mentioned in his textbook “Autonomic Testing”.
People who suspect they have OCHOS might have more success asking their doctor to try them on a more common calcium-channel blocker, such as are commonly used for high blood pressure. If that does anything beneficial, maybe the doctor will then consider nimodipine.
(Note that these drugs lower blood pressure. So if you have low blood pressure, they will be contraindicated.)
Trancranial Doppler devices, which measure cerebral blood flow velocity, are slowly making their way into hospital stroke departments. Autonomic specialists attached to such a hospital may be able to persuade the stroke unit to administer this simple test as per Dr Novak’s instructions in his textbook.
And some autonomic labs are benefiting from Dysautonomia International grants for the device with mentorship from Dr Novak. Ask your autonomic specialist whether they have one yet!
A little more information found in another paper by Dr Novak:
“Orthostatic cerebral hypoperfusion syndrome is associated with orthostatic intolerance and reduced orthostatic cerebral blood flow velocity without orthostatic hypotension, bradycardia, hypocapnia, or excessive tachycardia (Table 3).19
“This syndrome may result from abnormal cerebral vasocon- striction or abnormal venous pooling in the upright position. Our approach to therapy is the use of calcium channel blockers or angiotensin-converting enzyme blockers for patients with hypertension or prehypertension; and volume expansion with salt, fluids, fludrocortisone, or the use of pressor medications in patients with low blood pressure.”
Source: https://pubmed.ncbi.nlm.nih.gov/30308186/
(Abstract-only link)
So there are two cohorts of patients with OCHOS:
One group has hypertension and tends to respond to a vasodilator, probably because their cerebral arteries or arterioles are abnormally constricting and reducing blood flow to the head, and a vasodilator medication counters this. (Why is their body doing this to itself? Probably bad antibodies interfering with vasoconstriction/dilation mechanisms.)
The other group has hypotension and/or signs of hypovolemia and tends to respond well to the typical treatments and interventions already used successfully for those characteristics in other orthostatic syndromes. This group probably has blood pooling in the lower body/poor venous return.
I just happened to stumble across the information that calcium-channel blockers such as nimodipine (and some other classes of vasodilators used for high blood pressure) have immune-modulating properties, and I thought I would add it here.