

Remy provides the second in a series of blogs on using nimidopine – a calcium channel blocking drug – in chronic fatigue syndrome (ME/CFS) and fibromyalgia (FM). As described in Dr. Katherine Downing-Orr’s 2010 book, “Beating Chronic Fatigue Your step by step guide to complete recovery“, nimodipine, a calcium channel blocker, played a key role in Dr. Mason Brown’s protocol for chronic fatigue syndrome (ME/CFS).
Calcium Channel Blockers in ME/CFS and FM
Using calcium channel blockers (CCBs) to treat the symptoms of ME/CFS is nothing new. In reality, doctors have been using CCBs to treat the vascular symptoms of ME/CFS (like headaches) for many years. But the benefits of the CCBs as a class go far beyond the vascular system to include many other commonplace ME/CFS symptoms. Beyond that, the effects of a specific CCB, nimodipine, may provide even greater benefits for our population due to its ability to cross the blood-brain barrier.
What are calcium channels anyway?
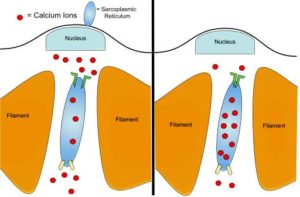
By definition, ion channels are pores in the cell membrane that allow specific ions (atoms or molecules) to pass through into the cell.
Among many other things, calcium ions also play a critical role in exercise. (from Wikimedia – https://commons.wikimedia.org/wiki/File:Anaerobic_exercise.svg)
Different types of ions use different channels to perform their intended cellular functions. Calcium ions, logically, use calcium channels and are one of the most important regulators of crucial cellular functions including muscle activity. Proper calcium functioning is vital for cell survival and disruption to these processes can be catastrophic. As a result, many degenerative diseases feature disrupted calcium homeostasis (steady state), and the importance of calcium to the proper working of the body really cannot be overemphasized.
For proper functioning, calcium levels should be higher in concentration (by about 10,000x) outside the cell in the blood and the extracellular fluid than in the cell. This concentration gradient is vital for the proper functioning of muscles, glial cells and neurotransmission. Calcium ions are further involved in the regulation of neurotransmitters and hormones, enzymes, transport, glycolysis, respiration, membrane potential and intracellular communication. Regardless of the original insult to the system, disruption in calcium channel functioning is often the final common pathway that will ultimately lead to the death of the cell.
Generally, CCBs function by reducing the crossing of calcium ions from the blood into the cells. The lowering of intracellular calcium has many important therapeutic effects, including the relaxation of blood vessels, which improves blood flow and oxygen delivery to the organs. This is the traditional reason for prescribing CCBs to patients with high blood pressure. But the main benefits in ME/CFS go well beyond the relief of hypertension.
Immune System Effects
The role CCBs play in modulating the immune system is clear. They can suppress the activation of different types of immune cells including T-cells and macrophages. The late immunologist, Dr. Robert Keller, noted CCB activity inhibits T-cell activation. Beyond that, research has demonstrated that CCBs have some systemic antiviral activity against common viral infections like influenza and all the way to HIV and hepatitis.
Researchers from Griffith University have recently shown that calcium handling is dysregulated in patients with ME/CFS. They are currently studying potential drugs that are able to activate the TRPM3 channel in similar fashion to pregnenolone, including the CCB, nifedipine.
Effects on the Mitochondria
Calcium affects mitochondrial function as well, with high intracellular calcium levels causing conformational changes which inhibit mitochondrial functioning leading to mitochondrial dysfunction. Unlike other mitochondrial issues, however, this isn’t due to genetic mitochondrial disorder, it’s simply caused by increased levels of intracellular calcium. More importantly, it can be reversed by lowering the calcium levels.
Effects on Microglial Cells
Dr Jarred Younger has studied microglial cells in patients with ME/CFS and hypothesizes that activated microglial cells in the brain could be responsible for producing some of the common symptoms of the disease. While Younger has not specifically mentioned CCBs in his work, other researchers have found that CCBs that cross the blood-brain barrier can inhibit the inflammatory activity of activated microglial cells. Nimodipine, in particular, can even promote remyelination in oligodendrocytes, which has important ramifications for multiple sclerosis (MS) sufferers.
Effects in MCAS
Mast cell activation disorder is specifically characterized by high levels of intracellular calcium and reducing this level may help improve allergic symptoms. Calcium channel blockers have also been shown to reduce the symptoms of urticaria and hives in several studies, beyond what antihistamines could do alone.
Effects on Chronic Pain
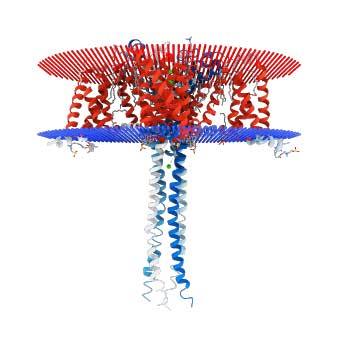
Crystalline structure of the N-type calcium channel believed involved in chronic pain. (from https://commons.wikimedia.org/wiki/File:Crystal_Structure_of_N-Type_Channel.png)
CCBs can also improve the pain of fibromyalgia. Dr. Jay Goldstein noted a decrease in the number of tender points after administration of a CCB in his practice. More current research also demonstrates how a specific type of calcium channel, the N-type, contributes to the experience of chronic pain.
N-type calcium channels have been identified as future key targets in controlling certain types of pain. Pain is a result of a cascade of signals involving the calcium channels. The influx of calcium ions triggers the release of neurotransmitters which then potentiate the pain signal to the brain where it is perceived as pain. Therefore, blocking this cascade with CCBs has the potential to dramatically improve pain levels in ME/CFS and fibromyalgia.
Beyond general, body-wide pain, CCBs are often prescribed to help control headaches, particularly migraine headaches. Migraine is thought to be initiated by cerebral vasospasm, which is then followed by vasodilation outside of the head. Cerebral blood flow has been shown in studies to be decreased, which then leads to low levels of oxygen in the brain. Calcium channel blockers can help prevent this cascade of events from happening as readily.
Other Important Benefits
Some clinicians, like Goldstein, report that CCBs may also help to increase exercise capacity in ME/CFS. CCBs have also been shown to improve vagal tone in patients following a heart attack.
Some ME/CFS specialists have noticed increases in cognition, presumably as a result of improved blood flow and increased oxygenation, as well as an improvement in mood disorders like depression and a decreased number of panic attacks.
Nimodipine vs Other Calcium Channel Blockers For ME/CFS and Fibromyalgia?
There are two common classes of CCBs, known as the dihydropyridine and the non-dihydropyridine types. Verapamil is a well-known example of the non-dihydropyridine type whereas nimodipine is a dihydropyridine type of CCB. This distinction is important because the dihydropyridine type of CCB has a greater effect on the blood vessels in the body as a whole, whereas non-dihydropyridine drugs are more targeted on the heart muscle, helping to make it easier to pump blood through the body.
The evidence for using a specific calcium channel blocker, nimodipine, may be even more robust than for calcium channel blockers as a whole. Dr. David Mason-Brown considers nimodipine (along with ginkgo biloba and other supplements) to be the most important treatment for normalizing brain circulation in ME/CFS.
Nimodipine is somewhat uniquely able to cross the blood-brain barrier and enter the cerebrospinal fluid, making it specifically suited to treating cases of reduced cerebral blood flow. In fact, the most common use for nimodipine in the US is to help increase blood flow to the brain after a stroke or cerebral aneurysm. This also means that nimodipine has less of an effect on the overall blood pressure than other CCBs, which is good for anyone suffering with low blood pressure or orthostatic hypotension.
The late Dr. Ismael Mena, one of the authors of the 2011 ME/CFS ICC criteria, used nuclear medicine imaging to measure functional brain flow in patients with brain degenerative diseases. He found that 71% of ME/CFS patients have low blood flow in the temporal lobe of the brain. After treatment with CCBs, patients showed improvements in cerebral blood flow.
Excess production of platelet activating factor increases the viscosity of the blood. Nimodipine normalizes blood flow by countering this effect.
Using Nimodipine in ME/CFS and FM
As the late Kristina Downing-Orr details in her book, Beating Chronic Fatigue, nimodipine forms the cornerstone of their medical protocol for reversing ME/CFS. Working with Dr. David Mason Brown, Downing-Orr developed a protocol for using very low doses, slowly ramped up, to increase brain circulation and remove the toxins that have built up as a result of the low circulation. This protocol starts with a very low dose of nimodipine, 7.5 mg, and then slowly ramps up over 33 weeks to a maximum of 120 mg.
Other practitioners, such as Jay Goldstein, also trialed nimodipine with patients, but if a positive response was not seen immediately, they did not continue the trial. Goldstein rated nimodipine the third best of his top 23 drugs for ME/CFS. Most practitioners now feel that either the slow-titration or slow-response protocols are more useful, however, as it may take time to observe the beneficial effects of improved brain circulation.
Because this is an off-label use of the drug, there are as many plans and protocols to dose nimodipine as there are practitioners. Some practitioners use the slow titration method Downing-Orr recommended, but others use faster protocols.
In the US, there is currently only one dose strength available, the 30 mg softgel, which complicates matters quite a lot when trying to start at the very low dose. There is a liquid form of nimodipine, designed to be used with a nasogastric tube that may be an option. It may also be possible to use a pin to open up the softgel and empty the contents into an oral syringe for dispensing that way.
Nimodipine is very expensive in the US if it is not covered by insurance. Cash prices currently are approaching $300/ 90 softgels. It may also be possible to use an online pharmacy to purchase nimodipine tablets that can be easily split as many will accept a US prescription. Typically, the cost will also be much lower as well. Pharmacychecker.com displays prices ranging from approximately $100-200/ 100 pills.
If lower dose options are not available, patients will have to start at the 30 mg dose and titrate up from there. Many practitioners, including the group that produced the Canadian Consensus document, take this approach anyway, so it’s really up to the patient and their prescriber which way to begin.
The risk of starting at a higher dose is, of course, the risk of having more side effects as brain circulation improves and toxins are released from the brain faster than the body can process them. In that case, most practitioners would recommend decreasing the dose, or skipping doses until the symptoms are manageable again.
As with any treatment, this will not work for everyone (though some estimate it will help more than 60% of patients) and some patients may get worse before they improve. This risk is always an important one to consider, as some patients may not find it an acceptable one until there are studies showing certain positive effects in our population.
Calcium channel blockers are a diverse class of medications with similar, yet also widely ranging effects. There are so many different variations of this drug that it isn’t really possible to generalize a reaction to one to a similar reaction to the entire class.
That said, nimodipine is considered a low-risk drug, and side effects are typically mild. Susan Parker reports in her very useful document, “Nimodipine Use in ME/CFS: A Comprehensive Guide”, that only 4 out of 100 patients experienced side effects with nimodipine, a rate that was less than the placebo. Parker also reports that there are no signs of drug accumulation, toxicity or liver injury, dependence, increased risk of cancer or GI bleeding as a result of nimodipine use, which is obviously in direct contrast to most pain-relieving drugs.
My Personal Experience
I started using nimodipine several months ago to try to treat vascular spasms that were causing ocular migraines and making my high pass IV ozone treatments difficult due to the reduced flow of blood during the spasm. I had no preconceived notions of benefit, other than hopefully easing my ozone treatments.
I first tried to take a small dose by freezing the softgel and cutting it into quarters, but this was mostly unsuccessful as the inside of the capsule did not freeze solid and made quite a mess. I tend not to be terribly sensitive, so I went ahead and trialed a full 30 mg capsule and immediately noticed a great reduction in the coat-hanger type pain across my shoulders that had plagued me for years.
This effect was somewhat short-lived, as nimodipine has a short half-life, but was thankfully repeated when I took another dose. Fairly quickly I worked up to 120 mg/day and have stayed there ever since.
I have POTS, though I am not currently symptomatic, but I did not notice any increase in orthostatic hypotension or a decrease in my blood pressure overall. Others have noted that nimodipine can actually increase blood pressure.
This reduction in pain has made such an enormous difference in my daily life. I never expected my fibromyalgia type pain to decrease from nimodipine, but that is exactly what happened. It works better for me than any OTC or prescription pain med ever has, and without most of the most significant side effects associated with long-term use of those drugs. Suffice it to say, I’m a fan. It hasn’t cured me, but I never expected that, and in terms of symptom relief, it is by far the best medication I have tried (and I have tried a lot!).
Most of the research I could find on nimodipine and calcium channel blockers in ME/CFS and other related conditions seems to be quite old now. Most of the resources online are out-of-date and many of the leading researchers into this treatment have now passed away or retired. But I’m hoping for a resurgence of interest in this drug and further research on how its use may benefit our population in the future.
Health Rising Resources
Susan Parker’s Comprehensive Overview (2014)
N I M O D I P I N E use in M.E. / CFS: A comprehensive guide.







Great to read your review. Would like to give it a trial and see if it would work as well as the combo I’m on.
Issie
I have been reading a lot of published studies regarding the this drug and how it alleviates the symptoms for those of us with ME/CFS. Can anyone please let me know how I go about getting a prescription? I live in South Florida.
Any doctor can write a prescription for off-label use. Then you are at the mercy of your insurance company as to whether or not it will be covered at a reasonable price.
Alternatively, you can look at some of the online pharmacies listed here: https://forums.phoenixrising.me/threads/tips-for-finding-reliable-and-trustworthy-prescription-free-online-pharmacies.8113/page-24#post-2244151
Tim, You may be able to find a practitioner who will prescribe it, but it is difficult. This will be in the alternative medicine field right now, or Dr. Charles Lapp in NC may be able to help. I am waiting to hear back from his office now. Appointments with him are expensive and the wait can be several months.
Very interesting- thank you as always for bringing new treatments and information to us. By the way, how are the ozone treatments going? Feeling any improvements?
Things are going well with ozone. I’m doing the high pass about every 12 weeks now and doing home ozone insufflations a few times a week. It’s definitely been a big part of the puzzle for me.
Does this mean people with ME/CFS should keep their calcium intake low?
No. The problem is not caused by too much calcium intake.
There is supposed to be a lot of calcium outside of the cell. The problems occur when the ion channels don’t function properly and let that calcium leak into the cell where it causes all sorts of chaos. The calcium channel blockers help to keep that from happening. So, no, dietary calcium is not the issue here.
Thanks for info both of you! That’s a relief to know!
I was given this drug by my pharmacy by mistake. It took away all of the power I had in both arms and legs and I was unable to move – I couldn’t even bend my arm or leg. I took 2 tablets, 1 per day! A few days after stopping I went back to normal.
Remy, thanks so much. Can I ask, besides pain alleviation for you personally, what symptoms do other patients on this protocol find it helps? Do many people find fatigue and brain fog reduced as well?
People have reported decreases in brain fog and fatigue as well. Beyond the pain, I found it gave me more tolerance for stimulation. For example, I was able to attend concerts where before the lights and noise would have been way too overwhelming. I also stopped needing to wear my headphones out in public.
Remy,
Thank you for such a thorough article. Nimodipine sounds very tempting to try.
Looks like there’s an oral solution which would allow people to try a smaller dose. The various generic pills contain a lot of potentially troublesome ingredients.
I am a bit leery of taking it after having another CCB, amlodipine, almost kill me last year – it rapidly destroyed my red blood cells, white blood cells, and platelets, bringing them down to alarm levels – thankfully, I stopped it due to severe fatigue before my lab results came back.
Though you were careful to note that CCBs act differently from one another, I gound this on the FDA website that looks like patients have experienced the similar problems with nimodipine:
Adverse experiences with an incidence rate less than 1% in the 90 mg q4h dose group were: itching,
gastrointestinal hemorrhage; thrombocytopenia; neurological deterioration; vomiting; diaphoresis;
congestive heart failure; hyponatremia; decreasing platelet count; disseminated intravascular
coagulation; deep vein thrombosis.
90 mg every 4 hours is a LARGE dose. I took 30 mg three times a day, but many people have found success with far less. Nimodipine is labeled for cerebral vasospasm so we also have to consider that the people typically taking it would have a lot of issues going on that (hopefully!) would not be a factor for the average person not having a brain hemorrhage.
Thanks for the clear blog and sharing your experiences Remy.
There is one point I noted. I remember having read somewhere that the Australian study reported intracellular Ca++ levels to be too low in ME patients.
That may have been Cort’s words on a previous blog on this study, I can’t find this directly back in the paper. I did however find the study tried to increase intracellular calcium, not decrease. All potential benefits mentioned in your blog discussing the benefits of trying to decrease intracellular Ca++.
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC5217865/
“Cytotoxic NK cells from CFS/ME patients may attempt to compensate for impaired TRPM3 receptors by increasing intracellular Ca2+ for sufficient NK cell activity. Increasing Ca2+ concentrations to activate the ERK signalling pathway may help to improve NK cell cytotoxicity in CFS/ME. Improvement of Ca2+‐dependent NK activity may help to improve the immune system in CFS/ME patients to facilitate a quicker response to eliminate pathogens.”
It seems the calcium channel topic is very difficult and conflicting. Things at play may be that the above was an in vitro study, not an in vivo one.
Another thing to note is that they used a series of drugs in consequence which effected both transport from the plasma to the cytostol (inside of the cell) and effected the transport between cell compartments. In case they described a drug regulating the transport of calcium between sytostol and the ER compartment.
I’m glad you bring up this study, because I’m confused by it too. It doesn’t make any sense at all to me and never has. Oxidative stress always increases intracellular calcium. I have tried to reconcile their results with everything else we know about these diseases without any luck so far. Maybe at some point we can ask them! I sure would like to understand.
I used a calcium blocker and it made me much worse. It is also very contradicted when we know that calcium is not going in to our cells propertly. When i use more calcium and vitD i feel something strange. So there could be a problem with calcium.
Has anyone tried Padma Basic?
is anyone aware of a UK doctor who wil prescriebe nimodipine please i’d like to try
Does anyone know in which of his books does dr Goldstein talk about his protocol ( the 23 most important medications he uses)?
I don’t know. I tried to read them years ago and failed utterly – they were incredibly complex. I would probably do better now..
http://www.cfstreatmentguide.com/dr-jay-goldstein-a-z-treatments.html
Which would indicate this drug is worth trying: high or low Calcium lab values?
Thanks!
Neither really, calcium channel blockers in normal doses change how calcium is managed, not the total levels systemically.
Hi – I am embarrassed to ask this but I am new to this blog and I cannot figure out what ME stands for. I have CFS/FM and SIBO for over ten years. I appreciate the information that you are providing. In March 2019, I had a stroke and now take Amodipine. I actually have noticed some positive changes in my pain and slightly less in the brain fog and fatigue. I am hopeful that I will continue to see improvements. Thank you.
Myalgic Encephalomyelitis
For everyone who would like to try Nimodipine but can’t have access to it (due to lack of prescription or cost), there is another drug that does the same thing and is much more easily accessible. It’s called Cinnarizine (Stugeron). I’m personally coming very close to remission thanks to this drug, cinnarizine, alone. It’s very cheap and the UK is even available behind the counter. Unfortunately, it’s not available in USA and Canada.
“Cinnarizine is an antihistamine and calcium channel blocker of the diphenylmethylpiperazine group.[1] It is also known to promote cerebral blood flow, and so is used to treat cerebral apoplexy, post-trauma cerebral symptoms, and cerebral arteriosclerosis.[2] However, it is more commonly prescribed for nausea and vomiting due to motion sickness[3] or other sources such as chemotherapy,[4] vertigo,[5] or Ménière’s disease.[6]”
“It primarily works on the central vestibular system to interfere with the signal transmission between vestibular apparatus of the inner ear and the vomiting centre of the hypothalamus. Cinnarizine could be also viewed as a nootropic drug because of its vasorelaxating abilities (due to calcium channel blockage), which happen mostly in brain.”
Hi, I know this is an old post but wondered if you continued to receive benefit from Stugeron? I bought some yesterday and only took half a tablet (7.5mg) and was planning the same today. Interested to understand what dosage you took and for how long.
Hi, gosh, this is a very old chapter of my life. I fully recovered eventually thanks to Stugeron. I went back to live a normal life for a few years. I’ve now developed Crohn’s disease, so things are still not easy, but at least easier than ME/CFS
For reference, I was using just 25mg a day. I continued to improve, so kept taking it for 6-8 months until I was fully recovered. Then I stopped and it was all fine.
I am very interested in using Nimodipine but have had difficulty obtaining it. I tried Strugenon and found it some help but rather soporific – it depletes dopamine and this risks sluggishness and lack of motivation.
Hi thanks for the info on your blog. I got the Dr to give nimdopine a try as I have tried everything else. I tried a quarter and have a increase in my pain should I keep trying is this normal? I have fibro chronic fatigue
Some people have to start even lower than a quarter-tablet. And some people won’t tolerate it at all. Unfortunately, it is a bit of trial and error still. You will have to decide with your doctor if you think it is a temporary flare-up or if the drug isn’t a good fit for you.
Hi Remy, I realize this is an older article but I’m hoping you can still comment on it.
From what I’ve read, Nimodipine seems to do its thing, (mainly restore intracellular calcium balance and possibly detoxify brain cells?), within 6 months. Was that your experience? Did you stop taking it after that period? And are you still in favour of it?
I’ve always felt that I have poor blood flow to my brain and would love to try this drug to see if I can get improvement.
Thanks for your efforts in researching and writing these excellent articles.
calcium deficiency treatment
Remy, I know this is an older article, but hope you see this. There have been a lot of studies recently showing reduced cerebral blood flow in ME/CFS as well as in EDS and some new autonomic syndromes. It has been measured using transcranial Doppler ultrasound.
One possible cause for reduced cerebral blood flow is abnormal vasoconstriction caused by an auto-immune problem. Calcium channel blockers and indeed any vadodilating medications can potentially help reverse some of the unwanted vasoconstriction.
See Dr Peter Novak’s article on OCHOS and various studies from van Campen, Visser, Rowe et al. Cort has some articles on this topic that helped me a lot. (I am now diagnosed with OCHOS and benefiting somewhat from a vasodilator.)
What vasodilator do you use?
I’ve tried a few classes. Unfortunately, the vasodilating part works fine but I keep having trouble with side effects, such as insomnia or reduced urine output.
Right now I am on a small dose of amlodipine and a small dose of candesartan.
(Note that I have slightly high blood pressure so taking vasodilators is okay and even recommended for me as a general treatment unrelated to my autonomic problems.)
Ideally I would like to try nimodipine as it acts selectively on the cerebral blood flow, but am yet to get hold of any.