

I listened miserably to the sounds of silence broken by my occasional exclamations: “really?”, “no kidding”, “fascinating!”. During my two long sessions with Dr. Klimas, the recorder app on my phone had decided to record only my questions – leaving silence for her replies. The few item my memory gleaned from the interview included: Dr. Klimas is investigating mold and seeing lots of mycotoxins in her patients. Sleep apnea is turning out to be surprisingly common as well, and, mentioning a recent gut finding, she said to keep a close eye on other central nervous system diseases such as Parkinson’s Disease. Findings there will help inform chronic fatigue syndrome (ME/CFS) and could even lead to treatment possibilities.
The big surprise was the news that Dr. Gordon Broderick, the originator of the computational modeling approach to ME/CFS, was now leading his own effort at the University of Rochester in New York. Travis Craddock is now in charge of Dr. Klimas’s computational biology effort at Nova – an effort that stirred so much enthusiasm in Parkinson’s disease that they tried to persuade her to devote her time and her team to that disease. Thankfully, Dr. Klimas said no, and she, Craddock and Broderick continue to work together on ME/CFS and GWI.
My interviews in shambles, there was still a lot to report from Dr. Klimas who has gone from strength to strength in her move from University of Miami to Nova Southeastern University seven or eight years ago.
Building on Success
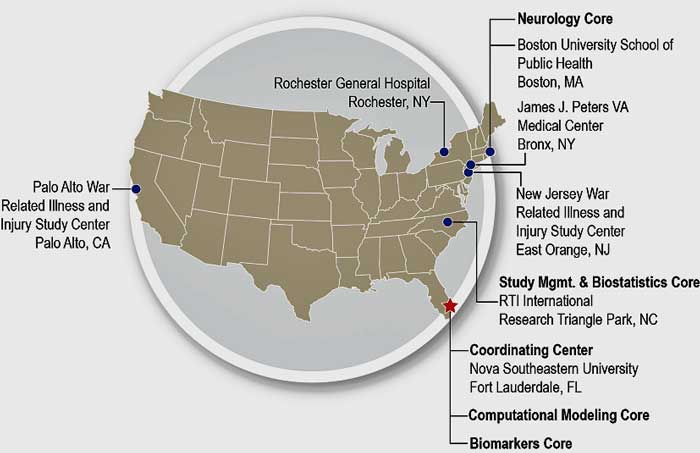
There’s nothing like success to breed success. In 2012, not so long after she arrived at Nova Southeastern University, Dr. Mariana Morris, Nancy Klimas and Gordon Broderick received a $4 million Consortium Award for the Gulf War Illness Research Program (GWIRP). The goal of Consortium awards is, as their name suggests, large awards that bring together a range of researchers to battle complex problems.
Gulf War Illness is a puzzling condition brought on by exposure to toxic elements from oil well fires, munitions, etc., vaccinations, heat, and the stress of war during the first Gulf War. It took one relatively short but intense exposure to this toxic brew of factors to irretrievably push many of these fit and mostly young warriors into a chronic illness state. Remarkably, from a quarter to a third of the servicemen and women participating in the first Gulf War have remained ill three decades later.
The really interesting thing is that despite their different trigger, they’ve looked exactly like people with chronic fatigue syndrome (ME/CFS). Their symptoms – including post-exertional malaise – are almost identical to ME/CFS. Some of them are extremely ill as well – just as some people with ME/CFS are.
Dr. Klimas’s studies have revealed, however, that despite their surface similarities, underneath the hood the two diseases are quite different. Immune networking studies indicated that the GWI patients’ immune systems have leapt to their defense and exhibit a kind of hyperactive, hyper-connected state, while the ME/CFS patients’ immune systems headed in the opposite direction; they’re characterized by eroded/impaired immune networks – they look depleted, overwhelmed and exhausted.
Klimas knew the two diseases looked the same but were actually different because the technology she used to understand ME/CFS was the same technology the first Gulf War Consortium funded helped her to develop for GWI. Now that she’s gotten another huge GW grant, we can anticipate the same result happening: she will get better at understanding GWI – and ME/CFS.
A Strategic Approach to a Disease
The feds are taking a different approach to GWI. It’s a strategic approach that’s designed to lead to clinical trials. It started in 2012. Check out what a strategic approach to a disease looks like.
Beginning in 2012, Marianna Morris, Dr. Klimas and Gordon Broderick used the a Consortium Award from the Congressionally Directed Medical Research Programs (CDMRP) to develop an animal model and to use exercise, massive data gathering efforts and computational biology to attempt to understand the processes at work in GWI and identify potential treatment targets. (Solve ME is trying get ME/CFS eligible for funding from the CDMRP).
At the same time, another winner of the 2012 Consortium Award – a the Boston group lead by Dr. Kimberly Sullivan – used the award to uncover a neuroinflammatory component and further immune disruptions in GWI illness patients. It’s been looking at a subject near and dear to ME/CFS – neuroinflammation and the microglia. Dr. Sullivan believes that continuous activation of the microglia in the brains of people with GWI is leading to a state of chronic “sickness” behavior: i.e. unrelenting states of fatigue, pain, cognitive problems, flu-like symptoms, etc. The same hypothesis has been proposed for ME/CFS.
She’s now examining markers in the blood and brain fluid (cerebrospinal fluid), doing extensive brain imaging, and studying brain cells under special microscopes.
Flexibility was built into these programs from the start.
“It is the responsibility of this Consortium to be responsive to new knowledge quickly, and not restrict the research efforts of this Consortium to the studies highlighted in this proposal. Thus, this Consortium will have a process in place to provide new research ideas with appropriate review”.
Sullivan’s 2017 Consortium award added an important piece of the infrastructure puzzle to GWI: the massive BBRAIN (Boston Biorepository, Recruitment, and Integrative Network) repository that will house just about every biological specimen you can imagine (whole blood for DNA and RNA analyses, plasma, sera, PBMCs, saliva, urine, fecal samples) as well as clinical data (cognitive data, health symptom and demographic surveys) from 500 GW Veterans. BBRAIN will also collaborate with other disease biobanks including at least one that includes people with ME/CFS.
Then, in September 2018, Dr. Klimas received a $5.3 million GWIRP Clinical Consortium Award designed to combine the expertise and knowledge gained from the two previous consortia and begin trying out a variety of treatments for GWI.
The specific goal at the start of these efforts was to “create a short list of attractive Food and Drug Administration-approved drugs that could be tested rapidly in clinical trials without requiring a drug development effort.” That effort was buttressed by the development of a “streamlined infrastructure for conducting Phase I and II clinical trials” Meanwhile, the BBRAIN repository provided an infrastructure component which allowed for a more efficient exploration of the mechanisms behind GWI, the identification of biomarkers, etc.
Basically, we have a massive and strategically coordinated effort to understand GWI and bring relief to long suffering veterans.
And here we are: using the latest Consortium funds, over the next four years, Dr. Klimas will produce no less than five Phase I or Phase II clinical trials in GWI.
They will all target similar issues to those found in ME/CFS – energy production, inflammation, and immune function – and all could ultimately apply to ME/CFS. Even though the niceties of the two diseases may be different, the core problems – neuroinflammation and HPA axis disruption – may be the same and may require similar approaches.
In short, a strategic program was created seven years ago with the intention that it would rapidly progress to clinical trials – and it has. That’s a far cry from what’s happening in ME/CFS where research is funded haphazardly – no strategic is in plan in place and no funding is available for clinical trials. (In fact, the past program announcement did not allow funding for clinical trials.)
The GWI saga demonstrates the difference between an organization (the Dept. of Defense) that has proceeded with a strategically oriented approach focused on producing data-driven clinical trials, and an organization, (the NIH), with a muddled, laissez-faire approach to ME/CFS which does not include clinical trials.
Dr. Klimas’s ME/CFS Program
At the Emerge Conference, Travis Craddock, the leader of Dr Klimas’s computational modeling effort (Gordon Broderick is now at the University of Rochester), highlighted how large Dr. Klimas’s INIM effort is. It’s made up of five cores, of which the one he leads (the clinical systems biology core) has no less than 9 members. INIM is clearly our first true ME/CFS Center of Excellence; it’s got a research and clinical team (two clinical offices, in fact) and is involved in educational efforts on the Nova Southeastern University Campus in Ft. Lauderdale, Florida.
As Broderick, Craddock and colleagues created their computational models, they tested them to see if they could reproduce known physiological processes. It’s not been easy. The female hormonal system, for instance, was so complex that it required four models simply to describe it. Once they have a model which seems to work, they perturb it to see if they can reproduce how a person might come down with ME/CFS in response to a triggering factor such as an infection, etc.
It’s worth repeating just how much data Dr. Klimas is able to throw into her computer modeling efforts. She has massive amounts of sex hormones, immune cell, cytokines, gene expression, DNA methylation, etc. data that’s been gathered 9 times before, during and after maximal exercise tests. All that is thrown into a supercomputer where it’s integrated into physiological models the team has created.
According to what I think I got from Craddock’s incredibly complex EMERGE presentation (which I can no longer find), the models suggest that the main areas of immune system interest in ME/CFS include B and T-cell receptors, TNF-a and transforming growth factor beta (TGF-b). TNF-a levels correlated most with severity scores, while TGF-b seems to be associated with pain.
Getting Stuck

Broderick’s models suggest that getting back to health requires a big push – big enough to get back over a big hill.
Gordon Broderick’s ME/CFS models very early on indicated that a strong enough stressor such as a high chemical or viral load could, under the right conditions, so destabilize a person’s system as to drop it into a suboptimal homeostatic state from which escape, even after the original stressor has been removed, was difficult or impossible. Walls had basically had been erected to keep the system in place.
The silver lining was that escape from that alternative homeostatic state was possible: the system just needed a big push to get it over the wall, so to speak, and let it slide back to normality – where, hopefully, it would stay put. Klimas’s goal has been to find the right combination of treatments to push the system back to normality. She’s been focusing on already available drugs and supplements to get the fastest relief possible to the ME/CFS and GWI communities.
Getting Unstuck
A recently published paper, authored by members of Broderick’s team at the University of Rochester and Dr. Klimas’s team at Nova Southeastern University, asserted two things:
- ME/CFS is likely so heterogeneous that one treatment cannot be expected to apply to all patients;
- ME/CFS is most likely addressed by combination therapies tailored to specific patients.
“The current literature on the treatment of ME/CFS leans strongly toward a single conclusion: that there is no single solution. The assumption that a single drug can successfully treat ME/CFS is likely incorrect. The multifaceted, complex nature of ME/CFS may instead be more effectively treated with combination therapies, tailored to the specific causes and symptoms present in each individual patient.” Richman et. al. 2019

The Klimas and Broderick groups believe a multi-treatment approach to ME/CFS and GWI is needed. Clinical trials are underway now
The breakthroughs in ME/CFS treatment, they believe, will most likely come from systems biology efforts which use a variety of “omics” data (genomics, metabolomics, proteomics, etc.) to identify the biological drivers behind the multisystemic problems found in ME/CFS. A personalized medicine approach will complement those findings. Subtyping or subsetting ME/CFS patients will be critical.
Once Klimas’s and Broderick’s team were able to produce a model which could replicate what’s happening in ME/CFS (i.e. demonstrate a infectious trigger could under the right conditions result in a steady-state condition like ME/CFS), then they were ready to perturb the virtual ME/CFS or GWI patients’ systems with treatments.
For instance, in a system characterized by the high Th1 cytokine and cortisol levels and low testosterone levels in GWI, the model indicated that a cytokine inhibitor Enbrel (etanercept) would drive the inflammation down but would not return the system to normal. Adding a glucocorticoid inhibitor (mifepristone) at a later stage, the model indicated, could return the system back to normal.
The team has uncovered other models of “stuckness” they believe are present in ME/CFS. The high Th1 cytokine/cortisol/low testosterone model applies to women not men and the Enbrel/mifepristone treatment regimen is not being proposed for men.
Gulf War Illness Studies
Two GWI studies (and one ME/CFS study) will focus on etanercept (Enbrel) and mifepristone, introduced in a staggered fashion. Two more GWI studies will focus on supplements that the group’s computer modeling suggested hit “all the right points”. One will assess the effectiveness of CoQ10 or glutathione, and then combine the best match with intranasal insulin. Another will examine the effects of a nutriceutical Bacopa, which has been shown to impact inflammation, immune function, and energy production. (Tumeric is another nutriceutical which the model predicted would hit many of the right points, but which has absorption issues.)
Focus on Bacopa
Our results strongly suggest that bacopa and its constituents are promising candidates for the development of novel therapeutics that target neuroinflammation, and have the potential for treating a wide range of CNS disorders. Nemetcheck et. Al.
Bacopa monnieri or Bacopa is a fascinating herb which, like many, is reported to have miraculous qualities :). Also called “Brahmi” or the “herb of grace”, it’s been used in Ayurvedic medicine to treat epilepsy, asthma, inflammation, ulcers, etc. and improve cognition for centuries. In Ayurevedic medicine, it’s considered a “medhya rasayana” or herb that sharpens the mind and intellect. One website reported that it was used by Hindis to help them memorize long texts.

Bacopa or water hyssop is an herb which Dr. Klimas’s computer models suggested hit “all the points”.
Also known as “water hyssop”, this pretty little water-loving plant is also found in Australia, and the United States. Many studies suggest Bacopa can cool the flames of inflammation in the body but Dr. Klimas wants to calm the fires of the central nervous system. A recent study suggests that Bacopa might do the trick. This 2017 study assessed whether a tea, infusion, and an alkaloid extract of bacopa were able to affect microglial activity in vitro – that is, in the lab. It found that the infusion extract and the highest concentration of the alkaloid extract were able to stop microglial cells from producing two powerful pro-inflammatory cytokines – TNF-a and IL6, as well as caspases 1 and 3.
Increased levels of both cytokines are associated with a variety of central nervous system disorders. Interestingly, the factor thought responsible for Bacopa’s anti-inflammatory effects, Bacoside A, actually increased inflammation. Note that this was a lab study – not a human trial – but it does suggest the potential may be there for Bacopa to cool the flames of the central nervous system. It is also being investigated as an anti-pain herb.
Assessment
Lots of testing, including going back on the bike, will be used to assess the treatment’s effects. The results will then be fed back into the modeling program. Even if the clinical trials fail, they will provide important data that will help the researchers refine their models further – and come up with better treatment candidates in the future.
The ME/CFS Field
The NIH does have a loose strategic plan for ME/CFS which includes funding several small research centers, an in-depth intramural study, and a central database – and seeing what pops up. The ME/CFS field also contains, in seed form, some of the innovative elements that are speeding up GWI illness research and treatment. Solve ME’s Patient Repository will, when it’s up and running, contain some of the features of BBRAIN. Ron Tompkins is committed to building streamlined infrastructure for the assessment of treatments at the Open Medicine Foundation’s ME/CFS Collaborative Research Center at Harvard. At Stanford, Ron Davis is dumping all his information into a publicly available database for researchers and the new Harvard ME/CFS group will do the same
All of these activities, to my knowledge, however, are privately funded and thus bear the marks of that: more funding is needed and most will probably take quite a bit of time to come to fruition (if they do). Whether the disparate and often not so cooperative elements of the ME/CFS research field will work together is unclear.
There’s no doubt that ME/CFS is more complex than GWI – an illness that was initiated by an at least somewhat homogenous set of stressors over a short period – but note how quickly the Consortia have moved from understanding GWI on a mechanistic basis to funding clinical trials. The trials may or may not be successful but even an unsuccessful trial should reap dividends as the researchers use the results to further improve their models.
Dr. Klimas has said for several years now that she’s ready to progress to Phase I clinical trials in ME/CFS now – and would have – if not for the funding barriers erected by the NIH. (A small privately funded Etanercept/mifepristone pilot trial is reportedly underway in ME/CFS.)
It’s encouraging to note, though, that despite the clear differences Dr. Klimas has found in ME/CFS and GWI, her models suggested that the same treatment, which is designed to tamp down neuroinflammation and restabilize the HPA axis, should work for both of them.
In summary, Dr. Klimas’s new infusion of money into GWI will help her assess treatments for GWI that may help for ME/CFS as well, and – more importantly – it gives her the funds she needs to continue building and refining the computational biology models that’s she’s been using to understand ME/CFS as well.
A Federally Funded Strategic Plan for ME/CFS?
This week on Sept 4th, the National Institute of Neurological Disorders and Stroke (NINDS) ME/CFS Working Group will present a plan it’s spent a year on that’s designed to move ME/CFS forward to the NANDS Study Council. This is our one big chance for immediate action. Note that this is entirely a NINDS action.
(One would have hoped that the NIH Working Group would be the one presenting a strategic plan for ME/CFS to the NIH itself but that group is continuing its almost 20 years record of disappointment.) The way out – the way to a more robust NIH effort – right now leads to NINDS, the home of Vicky Whittemore and Walter Koroshetz. The presentation is scheduled to be webcast starting around 1:30 PM EST.








This is very exciting news, Cort! Would be nice to see more trials of treatments, and especially on the west coast, where botanical treatments are more available and accepted.
The point that patients are heterogeneous and would be best served by individualized treatment plans with multiple ingredients is an important revelation, though frustrating, as it means there’s no magic bullet.
Seems the treatments being tested will be for patients with high Th1 cytokine and cortisol levels and low testosterone levels.
Researchers have found many ME/CFS patients with NR3C1 SNPs, which cause glucocorticoid resistance. Wonder if the mifepristone would backfire for these patoents, and what combo might work for patients with high Th1 cytokines, but low cortisol and other hormones, as many of us have- many og us are on glucocorticoid just to function.
Then you shared that:
”One will assess the effectiveness of CoQ10 or glutathione and then combines the best match with intranasal insulin. Another will examine the effects of a nutriceutical Bacopa which has been shown to impact inflammation, immune function, and energy production. (Tumeric is another nutriceutical which the model predicted would hit many of the right points but which has absorption issues.)”
How will patients be chosen? Will they be patients with CoQ10 deficiencies for the CoQ10 study? Depleted glutathione and high oxidative and nitrosative stress for the glutathione study? Labs and symptoms that indicate a need for bacopa? My fear is if you just give these to a bunch of random ME/CFS patients, you’ll get a mixed bag of results. And, if you don’t look at cofactors – acetyl-l-carnitine, niacin and riboflavin family, BH4 promoters, and redilucing peroxynitrites, CoQ10 may only help some patients who have deficiencies, but not others with other mitichondrial needs, it wint show enough success.
Glutathione needs can be due to lack of methylation nutrients, amino acid deficiencies (glutamine, glycine, NAC, methionine), lack of vitamin C or ALA to recycle it, infections, and/or mold or heavy metal toxicity.
Curcumin is the most useful part of turmeric. There are more bioavailable forms, like CoreCurvumin from nurish.me, CurcumEvail from Designs for Health, or IV curcumin which I’ve had and seen do amazing things for several other patients but is not currently available in the US (it was for over 5 years). It is a COX2 inhibitor, anti-inflammatory, mast cell stabilizer, broad spectrum phase 2 detoxer, and anti-cancer agent. It would be exciting to see it trailed on ME/CFS patients. It is not something to shy away from especially if its showing up in the computational biology models.
Yes, Jared Younger has finished his trials of botanicals and reportedly was analyzing the data on it. He suggested that some may be as effective as LDN.
The Enbrel/mifepristone trial is only going to be on women. (I amended the blog to clarify that) The models, if I got what she said right, do not suggest it will work on men.
I agree about tumeric and as I recall Dr. Klimas agreed on that it had possibilities as well. I had the impression that their models suggested other treatments as well – they simply chose the top ones for their trials.
Apparently Tumeric/Curcumin are better absorbed if taken with fat and black pepper (piperine)
Turmeric (or curcumin) and other natural anti inflamatories are often cited as exciting possibilities.
Ive tried them (and drug versions) and got good relief, only to find I get really bad asthma – I end up on steroids! Unfortunately, it took several tries to realise the connection. ?
Sometimes it seems there’s no real answer. I’m so grateful we have such dedicated researchers working on our behalf!
As Cort said, we are a very diverse group of patients and in the end it will probably mean individual treatment from a whole ranch of supplement and drug options.
I’m cheering on all our champions of research! ?
Thanks Cort for reporting on this even though you had the frustration of losing your recordings!
Thanks to Learner 1 for questions. Alas, as one ages with this disease, doctors become less interested in treating us since we know longer are considered useful data points in any research they are doing. Once you’ve reached 70, forget it; they just throw you out.
Oh, Cameron, it is very sad to say..I’ve been thrown out with the bathwater. Guess were suppose to just lay down and die.
Very upsetting.
I am one of those who have several homozygous SNPs and also heterozygous SNPs on NR3C1 and no way could I take a drug that lowers cortisol because I actually have to take a steroid because my adrenals cannot function on the tiny amount my own body produces.
This all goes to show how different we are and it cannot be a one size fits all so it would seem we do all need individualised treatments which makes it almost impossible for researchers to come to an agreement on what is going on in our illness.
Curcumin has been one of the best things for me. Has allowed me to do gentle exercise without awful PEM.
I tried taking one capsule of Turmeric/Curcumin once, and it dropped my blood sugar so badly that I couldn’t spoon table sugar into my mouth fast enough to stop from feeling like I was going to die. But I can eat curry no problem. So yes, we are all very different indeed.
I have suffered with fibromyalgia 10 years.
And with CFS for 5 years.
I suffer 24/7/365 with no relief in sight.
I am 78 and do not have a day without pain.
I feel like a zombie.
It has ruined our pleasure in life.
I can’t even brush my teeth without hurting my gums. I can’t swallow without pain,
I can’t walk straight from dizziness and have nightly headaches. My eyes hurt, my ears hurt. I have trouble with all my bodily functions. My jaw hurts, my wrists, y chest.
I have all the Drs. Cardiologist, ENT, Rheumatologist, dentist Eye Dr. I’ve had hundred of tests.
Always the same. No cure, just Presciptions. I take gabapentin, trazadone, lorazepam, Effexor timilol, ovantik, adderall, baby aspirin and oxycodone.
I’m miserable.
And it’s very difficult for my wife our social life is gone. My children feel terrible for me.
ID LIKE TO BE IN A CLINICAL STUDY
Gary Gordon
So sorry to hear Gary – such a difficult time. Have you tried low dose naltrexone? It’s pretty cheap and can work really well at times on pain. There’s also Cannabis – we’ll be covering strains that may helpful for pain in an upcoming blog. There’s also something called neuroplasticity. Check out the recent Moskowitz blog and his book – which we will be covering later. He says neuroplasticity exercises can work really well for FM.
@Cort Johnson LDN remarkable for pain…its been a bear for me to regulate. Year 2 only up to 2.5mg I recently had to stop it for 2 weeks (not consecutive) due to low mood) is this due to MTHFR1298c homo? Until recently, LDN allowed me to do 16000 steps. Now, after a fall, only 4-7000 if my mood allows me to go out. Any suggestions. I WONT GIVE IT UP!
Gary, I understand so much what you are pleading for. As the research grants and study formats are set up now, those of us over 70 are left out, presumably because extraneous factors due to aging come in.
I don’t think that’s any reason not to set up studies for people 70 plus, especially those of us who have had ME/CFS/FMS since we were in our late 40s or earlier. Indeed, I’d think it would be of special interest.
Just to mention, “they” are finding out now that the side effects of drugs that are listed for many common Rx’s for everything (meaning, not CFS) do not adequately reflect the reactions that the “elderly” (I think they usually define that as over 65, although I think the NIH research grants exclude people 70 or over — someone correct me please??) — anyway, the flyers that describe adverse reactions to drugs and proper dosages do not adequately reflect proper dosages for “elderly” however it is defined in the particular context.
Cort, “in all your spare time” (I know!), I think it would be very helpful to concentrate in some way on those of us who are know longer in the age group of interest to the research community.
I don’t want to say anything over dramatic, but…
Maybe someone will have some ideas. Thanks.
@ Cameron: ?????? suffering since I’m 37yo. Ldn is a miracle but difficult to regulate for my. It can destroy my mood for up to 13 days. The pain relief is amazing. Cort Johnson keep us oldies in mind. Some of us wanna LIVE.
After almost 40 years with this Ceecee, I’m with you.
Gary:
Read Anthony William’s ‘Medical Medium’ , ‘Thyroid’, and ‘Life-Changing Foods’ books, or listen to ‘Medical Medium and EBV’ (etc.) on SoundCloud if like many CFSrs, you have trouble comprehending reading (but take notes!)
AW tells how to rebuild the immune system and detox the body 100% through diet, herbs, and supplements. It is like a modern version of Chinese Medicine, with similar roots with Anthony instead of the ‘Yellow Emporer’ of 3,000 years ago.
Since you can not wait 20 years for Western Medicine to come up with a cure, it can help you somewhat now, although it may take months.
One thing AW mentions is that the underlying HHV family of virus feeds on heavy metals, toxins, and non‐natural chemicals. It was once a helpful virus, but these days it is being overfed. Patent meds (and all those ‘inert’ ingredients!) are chemicals that feed it.
Dairy and gluten are mucus causing and hide the virus from the immune system. Vaccine mfrs use eggs to quickly grow viruses, so eggs need to be eliminated, too.
Start having a lot of organic fruit, berries, and melon for breakfast and then every 1.5 to 2 hours so as to fill your body with a lot of natural nutrients and stabilize the blood sugars. A big salad of dark greens and chopped veggies for lunch with balsamic vinegrette dressing. A healthy low fat dinner with a lot of colorful steamed vegetables with cilantro or parsely and other herbs. Snack OFTEN on celery, cucumber slices, baby carrots, dates, berries, fruit slices, etc. That is key; Pre-fill little tupperwares with them. Drink lemon water, fresh vegetable huices, or herbal tea often. You should never be hungry. No alcohol for at least the first month or two; the liver needs to heal.
Try this for 2 to 3 weeks while you get and read the books. Make one of his green detox blueberry & cilantro (etc.) smoothies (from Medical Medium book #1), with added spinach, frozen banana chunks, and a few frozen asparugus stalks at least every other day.
Add supplements (like L-lysine, zinc, magnesium, folate, ALA, Vit C complex) and anti-viral teas (like Lemon Balm and/or Nettle Leaf) 3x/day.
A daily 16oz. glass of fresh organic celery juice on an empty stomach is said to speed detoxing and healing up, due to the very high electrolyte levels in celery. If a detox reaction (the runs!) results, take a day or two off, drink less (4oz 1x or 2x/day) and then build up to 16oz/day over 2‐3 weeks, or add a cucumber + red apple to the celery (nothing else) in the juicer.
With your holistically-trained doctor’s or licensed alt. Health Practioner’s help, get off all unecessary patent (chemical based) medications. Some may be supporting (feeding) the bad virus and keeping you from obtaining health. If you can not take each med and hour or two apart so they do not adversely interact with each other (read the long list of known side effects for EACH singular drug! Now imagine combining them all), you will be damaging your kidneys and liver, which are the body’s main detox system (and no wonder you feel like crap!).
Time to change it all (including your mindset) and work towards acting, feeling, and being Healthy. Your body knows how to get back to Health IF and WHEN given the right tools (natural form of the essential vitamins, minerals, microminerals, phytonutrients, anti-oxidants, and Trust in one’s inner self).
Then report back to us if you notice any positive changes after the first few weeks. If yes, keep it up! Report back again in 3 months.
The above will help until Cort’s friends come up with the Magic Pill or vaccine. It has helped thousands of others over the past 25 years, and millions worldwide over the past 5 years since the first book came out.
How ridiculous to ask a 70 ur old to eat only fruits and veg and fruits are so high in sugar and fructose. Simplistic advice for a comi ated disease.
Tumeric certainly helped rid me of pain & inflammation.
Hi Gary,
I’m sorry to hear you are suffering so badly. In addition to the LDN suggestion, I’d like to add THC/CBD products (marijuana, smoked or edibles, or tinctures, etc). It has helped others: https://www.projectcbd.org/medicine/cannabis-chronic-fatigue-syndrome
Anyone who has read Julie Rehmeyers blogs, book, or seen her videos about how she learned about mold avoidance from an Incline Village survivor & original prototype for Holmes 1988 CFS must surely know that Dr Nancy Klimas has never actually looked into “Chronic Fatigue Syndrome”
If Dr Klimas had done so, she would have known about the mold factor.
—————————————————————————————————–
http://www.washingtonpost.com/national/health-science/what-is-chronic-fatigue-syndrome-and-why-arent-we-doing-more-to-treat-the-illness/2014/10/06/4cfff312-d458-11e3-8a78-8fe50322a72c_story.html?commentID=washingtonpost.com%2FECHO%2Fitem%2F1412690684-331-594
These disputes are heartbreaking when the needs of CFS patients are so great. Even the high-quality treatment I got from Klimas helped me only slightly. A year after I saw her, I heard from some patients who had significantly recovered from CFS through assiduously avoiding exposure to mold and other environmental contaminants. Although I considered the theory wacky, I was desperate enough to experiment. And for me, it worked. Two years later, I can go running, write articles and travel with my new husband. Every time I do, it feels like a miracle.
But I don’t think it is. My recovery has almost certainly come through physiological changes in response to my avoiding mold.
Yes, of course I know this pisses people off.
Tough. Your anger, and your attacks on me
doesn’t change a thing.
So go ahead and spew your hate. It won’t do you any good.
I read Hillary Johnson’s book on the 10 year history of CFS, and although I don’t have a very good memory now, It seems like I definitely remember Nancy Klimas being in that book as one of the few who DID research ME/CFS. Isn’t she the one in Miami who actually contracted it? I could be wrong, but I thought it was her. We are talking the 1988 to 1998 period of time. The mold thing could be more recent.
Dr. Klimas started researching and treating ME/CFS back in the 80’s. Shes an immunologist who specialized in HIV/AIDS and ME/CFS treatment and eventually focused solely on ME/CFS, GWI and related diseases. I would be surprised if she was in Hillary’s book. She also ran an NIH funded ME/CFS research center for a time and oversees 2 clinics and an a research effort in southern Florida. She’s done just about everything possible in ME/CFS. We’re very lucky to have her.
Dr Klimas simply researched her own patients and called it “CFS”
But notice she never saw an outbreak.
No clusters. No contagion. No time-space spread through a community.
Obviously not the same thing as Lake Tahoe.
Nothing like what the CDC was investigating and named CFS.
Nothing annoys me more than people promoting fruit and vegetables as a cure. Read up on keto, get all of the inflammatory foods out of your diet. My stomach is so much less bloated than it used to be. Add intermittent fasting as well to give your gut a chance to heal itself. It’s not a cure but it can improve some of your symptoms. I have a lot of allergies, I would suggest getting tested. Magnesium Malate is important, vitamin c, fish oil and a multivitamin. I also take ginger and I’ve just started again Brahmi Bacopa for memory/brain fog.
I also take Gabapentin 300mg per day.
Don’t get distracted by the noise out there.
To be honest Eric this is where you lose people! You have a good message – we need to focus more on mold but stating things like this
“must surely know that Dr Nancy Klimas has never actually looked into “Chronic Fatigue Syndrome””
of a researcher and doctor who has devoted most of her career to this disease – must have made my blood pressure go up 30 points when I read it. Statements like that just bring you grief and deservedly so.
You can make your point without belittling and antagonizing others. Maybe that’s not your goal. (Most likely it’s not.)
(Why not say – Dr. Klimas helped Julie Rehmeyer a bit and that mold awareness helped her recover and congratulations to Dr. Klimas to looking more into mold and I hope she does it more or something like that?)
For me, I think Dr. Klimas is right – there are many flavors of ME/CFS of which mold is one (and only one); a variety of treatment approaches are going to be needed (of which mold avoidance for some is key) and there’s not likely to be ONE answer for any of this.
Couldn’t agree with you more, Cort.
I don’t understand the negativity that some people have towards certain researchers who are doing so very much for ME/CFS. Dr Klimas is an amazing researcher as well as human being and I am very grateful for all that she is doing for us….and GWI…and any other neuroimmune illness.
Even Ritchie Shoemaker admitted in his book that there were patients he personally treated that still had serious fatigue issues. This suggests that mold avoidance may be necessary but not sufficient for some people. For some people it may be the magic bullet but others will probably have to go beyond that.
This could be because mycotoxins create further biochemical issues in some people which then also need repaired before health can be restored. For example maybe they deplete glutathione which leads to heavy metal accumulation. The body becomes weakened to the point that it cannot remove the heavy metals even if mold avoidance is practiced. Another person may have a more robust glutathione system and heavy metals do not become an issue for them so mold avoidance is all they need to get better.
Have you watched Dr. Bruce Wauchope’s Emerge Australia talk…it was called Clinical Experience 2. He lists 17 clinical questions and mold is part of Question 9. Unfortunately he didn’t cover a lot of treatments but his approach sounds methodological.
Hi Cort.
People asked for research into CFS in the most polite, nice and diplomatic ways for 30 years.
I’ve seen every manner of request, from downright groveling supplication to firm insistence.
None of it worked.
No one ever responded.
So about 2010 I totally gave up on that approach.
Especially since I know it won’t work.
I have nothing to lose by belittling these “researchers”
They weren’t going to act like their name implies, no matter what.
If I “lose them”, then good! They can stay lost.
See my comment below. Consider that your main priority is NOT helping people understand the dangers of mold and recovering from it.
I agree.
Over and above the mold phenomenon, I feel that I am in a unique position to expose “research misconduct”
And demonstrate how it has set back science by decades and caused immense suffering and harm.
This website is about supporting research. I understand your frustration that researchers haven’t picked up on mold more but this website is emphatically not a place for people to bash well-intended researchers who are well-intended and whom you or other think are on the wrong path!
Please keeping pushing the mold idea and stop belittling or questioning the sincerity of other researchers.
Hi. One day docs may twig the one in four misdiagnosed MEs due to mould (I’m in the UK) – according to a recent report I read somewhere. Matches the one in four statistic with the genetic HLA4 (sorry – crap memory) intolerance thing. Thanks in part to you, MyHill, Paradigm Change and Dr House… I finally worked out my previous rental house was once flood damaged and something evil mould wise. Doctors think I’m crazy, not interested in the possibility and tho I was told NHS can test for mycotoxins in the blood (really?) With the urine test from Real-time Labs or whoever could give a false negative. I’m unsure how to at least prove I’m mouldy. Let alone get treated.
So to the poor chap who commented, that is suffering so badly (and anyone else) – investigate the possibility. Get away somewhere super dry for a couple of weeks and see if any dramatic improvements occur. Some of my crazy neurological symptoms vanished overnight after finally escaping. Sorry to hijack!
“You” meant Erik thanks wise.
Mould vs ME for me is probably a bit chicken and egg illness wise and may just be an extra level of immune kickings but no doubt a factor.
Yes, Adam.
Get to some place super dry and see what happens.
But don’t count on any doctors for help, understanding or belief.
They are in total denial, and remain in constant battle with those of us who have “done the experiment” and found mold avoidance to be worthy of practicing.
Respectfully, Erik, I’d disagree with the statement about not counting on any doctors for help, understanding, or belief. The International Society of Environmentally Acquired Illness (ISEAI) has some FANTASTIC, knowledgeable, and caring practitioners. Their inaugural conference in Phoenix this past May was an incredible gathering of the minds – and showed just how much knowledge there is in an admittedly small community. None of them question the fact that mold and mycotoxins can be exceedingly harmful, and, in fact, they expand on the potential damage well beyond ME/CFS. The ISEAI web site includes a resource for finding a doctor in your area, though largely U.S. You might have to travel a bit, but I’d urge anyone dealing with this type of illness to seek out one of their practitioners.
None of them question it?
Are you kidding.
Not a single ME/CFS researcher in the world has responded to “Mold at Ground Zero for CFS”
@Eric Johnson,
What steps to recovery did you for mold exposure? We have discovered high counts of water damage & mold in our house after I was diagnosed last years with CIRS (from it) We’re in the process of re-mediating…but I’m so tired of feeling tired & lack of clear thoughts like I used to have. I’m doing plant-based keto for mitochondrial health, COQ-10, Liposomal glutathione, acetyl-l-carnitine, fish oil/turmeric, binder, also Biocidin & anti-fungal currently for candida.
I have a question: HOW DOES ONE COMPLETELY AVOID MOLD EXPOSURE? Isn’t it, like, everywhere now? I live in a Senior Care Facility (I’m 64) and my refrigerator stays moldy on the rubber gasket. I noticed it and informed them, but it was so gross, I took some baking soda and peroxide and made a fizzy paste, and got most of it. They told me to just keep doing that. Really? They are supposed to do things like that. Is there a better way to kill it and keep it gone?
Thanks for the recipe! Indeed it is frustrating when people are so non responsive, but great that people like you can be so resourceful. I can use your recipe in my own kitchen. Thanks again.
Jeannie –
Yes, mold IS everywhere. No argument there.
That said, not all molds are created equal. They’re ranked as “cosmetic”, allergenic, pathogenic, and toxigenic, depending on the species. The allergenic ones, as you’d guess, trigger mainly allergic symptoms. The pathogenic ones are worse, leading to health complications in immune compromised individuals. Then, there are the toxigenic molds – Aspergillus, Penicillium, Stachybotrys, etc. – that create serious toxins. These chemicals – like ochratoxin, aflatoxin, trichothecenes, etc.- are NASTY. Among other things, they can be immune suppressive, neurotoxic, hormone disruptors, and carcinogens. These are the ones that freak out government officials, health departments, property managers, insurance companies, and health care facility operators. As you can imagine, there’s a TON of liability and money at stake, so they’d prefer we know as little as possible here.
So, where am I going with this? You need to understand that the mold on your refrigerator is quite likely just one source. There are probably others in the air system of the facility, or plumbing leaks, or condensation problems. Those molds could be producing toxins, which become airborne and spread through the facility, like smoke. That’s the real danger.
Also, as any indoor environmental professional (IEP) will tell you, killing the mold is only the start of the process. You really need to know what species you’re dealing with to understand whether they’re just “munge”, or if they’re something more dangerous. This requires special testing, typically an “ERMI” test. If toxigenic species are found, the toxins will likely have spread as microscopic particles, mainly attached to dust particles. They get everywhere, particularly into soft goods – paper, fabrics, etc. – and electronics, which can trap lots of dust.
Even if you “kill” the mold, the toxins can remain a significant health risk.
A senior care facility is NOT going to be happy about this, as it’s a giant liability risk and potentially very expensive to remediate. BUT, they need to own it. Your health – and the health of the other residents – depends on it.
I truly hope this helps.
It is inhaled airborne mold spores that one usually has to worry about, such as that in the coils of an old a/c unit, not the mold on a gasket or toilet rings. It is a trigger for CFS, just like any other physical, chemical, or emotional stress that lowers the immune system. Other infections, tick bites, divorce, surgery, and pregnancies are also CFS triggers. No one knows what their immune level is day-to-day, nor what is going to tip the scale someday.
So ANY researchers studying ANY HHV-based chronic disease are ALL taking the baby steps needed to understand chronic inflammation, pain, fatigue, and cancer someday. The issue is they need to all pool their information and resources,
since viral research aimed at curing or preventing (with inexpensive vaccines) the underlying cause of 95%(?) of chronic diseases and cancers is not supported by the current Medical Industry ‘disease care’ model.
Private funding is the only thing supporting the needed viral research. Hopefully Health Insurance companies will learn to support that research, too, and cover more non-allopathic treatments that have been proven more effective than using chemicals and radiation to improve our health.
HMOs are leading the movement, since they profit by a healthier customer base, but they let their lawyers dictate their accepted Standard of Care, and are not involved with ground-breaking research.
The Western model of health care basically only works for acute issues, not chronic issues.
Most infections are becoming antibiotic resistant (such as with Strep), so the Western model of treatment will soon totally fail with those, too.
I think Cort is one of the few who has a “Birds Eye view” of what is going on with the CFS and viral research, and he just needs to (throw more cocktail parties?) get certain key people talking to each other. Then we will get faster results!
I go to the Klimas Clinic and they do indeed know about the effects of mold and even test for it in your body fat and urine. Just to clarify that one point. My doctor there found none stored in my body but it comes and goes in my urine so she has me using charcoal to draw it out. I don’t think there is a magic bullet, as Cort makes clear. Not even mold avoidance can cure everyone.
We were concerned with mold exposure for my wife who has had ME/CFS fro 20 years. We had a professional assessment done of our home, which found only normal background levels. Can anyone recommend an authoritative test to determine if my wife has residual mold toxicity from earlier exposures? Like many suffering from this debilitating disease, we are ready to pursue all possible causes and treatments. Thank you
Urine mycotoxing testing. There are 2-3 labs that do it. Before it was only Real Time Labs. Several integrative docs recommend a glutathione challenge and/or sauna or warm bath before urine collection for better results.
Hi John,
Mast cell degranulation or mast cell attacks *may* be part of the negative health effects to mold exposure.
https://en.wikipedia.org/wiki/Immunoglobulin_G
“IgG antibodies can prevent IgE mediated anaphylaxis by intercepting a specific antigen before it binds to mast cell–associated IgE. Consequently, IgG antibodies block systemic anaphylaxis induced by small quantities of antigen but can mediate systemic anaphylaxis induced by larger quantities.”
The above means IMO, once your immunity system is chronically broken, you become so much more sensitive to any allergenic trigger. So your body can be completely “purified” from mold exposure, if your immune system did not recover you still can get a strong reaction to small doses of aggressors like mold.
Likely you’ll be and remain long after first exposure more sensitive to the original triggers by producing more IgE antigens to it too IMO, creating a double effect of sensitivity.
With this link, having chronically reduced IgG levels and strong IgE response to triggers that caused the original disease may cause a very strong reaction to minimal exposure of mold for years or decades to come. But likely there are other immune deficiencies able to get such harsh response too.
Testing for IgG levels and upping them medically could be one trick to reduce sensitivity. But it is very expensive, difficult to find a doctor to approve it and may have unexpected and undesired side effects. En plus, if there are other factors undermining the immune system then it still may be insufficient.
I believe that the difficult thing of trying to get the body to better self-heal is a very slow and tricky process towards a better immune system, better health and less sensitivity to these aggressors.
This is interesting to know. Thanks.
Pris, do they biopsy fat, then test it for mold toxins?
They do not know about the effects of mold.
Dr Klimas has been a staunch denier for 30 years, and is only recently trying to play “catch up”
Obviously without admitting to her years of denial.
Which is why she won’t tell you that she heard about “Mold at Ground Zero for CFS” personally from an Incline Village survivor & original prototype for Holmes 1988 CFS.
And that’s not good science at all.
In fact, an omission like that is more akin to “science fraud”
I know her memory is not really so bad that she might have forgotten.
(Yes. I know how much this will piss you off.
Tough. These are the facts, and your hate won’t change it)
I don’t know why I started this Eric – since there rarely seems to be any give on your side, never any recognition of the work that others are doing, or the possibility that other things might be involved in ME/CFS – just this ongoing outpouring of bitterness and self-righteous anger which has resulted in you from being banned from several sites.
If you were really committed to getting your message across, that result one might think give you pause about how you are delivering your message. Since it hasn’t given you pause, the only conclusion I can draw is that getting your message across regarding mold and helping others with it, is not your main goal
Let’s not pretend you’re on some high and mighty mission to educate and save people from mold. If that was your main priority you would have changed your ways so you could get your message out as broadly as possible. Instead you’ve kept right on doing the things that prevent you from getting your message out.
Your bigger goal appears to be getting across how you were right all the time, and how upset you are that the medical world has not laid itself at your feet, and wreaking revenge on those who have not listened to you. That’s your main agenda.
Something to think about.
Eric,
I’ve read all of your comments on mold. It is entirely unfair to dismiss all the research that is and has been done on CFS. Its complexity requires not only billions of dollars, but also dedicated reasearchers like Nancy Klimas, for instance, to continue their study of this disease. You’ve said enough. You need to look at the big picture. It’s more than annoying to read your belittling and narrow point of view
Cort. Naturally, I’ve thought about this a lot.
It has been made more than clear that the “Mighty Gods of Academia” are totally bent on wiping out me, and my evidence.
Which happens to be the evidence that started a famous syndrome.
This is not how honest researchers should behave.
Rolling over and “playing nice” is simply allowing them to have their way.
I decided not to play their game.
And let history decide who was right or wrong to do what they did.
btw.
Looking forward to seeing you and the whole gang at the OMF symposium, where we can all sit down and have a nice chat about this stuff.
Hopefully we can get Dr Davis and Dr Peterson to join in.
I do share Eriks Frustration in that almost certainly mold is a vital clue to what drives CFS. And it has not just been ignored, It’s considered a quack diagnosis by main stream. And this position is bolstered by “experts” who have ties to insurance companies and other vested interest’s who seem to cherrypick data that supports their position the connection does not exist.
I dont believe mold is the causative agent, but more of a trigger for inflammation. Those with CFS have many triggers and mold can be one of them. Im more into Dr Chias research that says an Enterovirus is the culprit. It easily explains people of all ages getting this illness as well as soldiers getting sick out in the battlefield, Contaminated water. Enterovirus is paralyzing, think of your vagus nerve, its very tough, not destroyed by heat or chlorine. Its non-cytolytic, doesnt destroy cells, it makes them sick and dysfunctional. Im one of his case studies and am tested yearly for viruses, Enterovirus is the only one I am Sky high positive for as well as friends Ive referred over to Dr chia. He has tested well over 5000 CFS patients by now and its the same virus we all have in common. The sicker the patient, the higher the PCR saturation.
Richard, I don’t think mold is the causative agent either. But like you say a trigger. I’ve seen too many people living in moldy environment’s with no adverse effects to believe it is causative. So I am open to the idea of a virus. My onset was after wholesale exposure to pesticides in a way they were not meant to be used so I am biased towards toxic exposures. That and all the the things I have been exposed to over the years both occupationally and at home. And Gulf War vet’s were exposed to all kinds of toxic material and many ended up with GWS. So I am biased towards this. But open to anything such as a virus or bacteria of some type, or protozoa. Even some type of biological weapon gone wrong.
The reason I am so frustrated with authorities ignoring the connection to mold is because if it was to be investigated scientifically and a test developed for it that would be a huge step forward not just in diagnosing but treating victims. Even without knowing what causes it or how it makes us sick.
And that would lead to insurmountable pressure to authorities to fund research into the condition.
That and it is (in my opinion) a vital clue as to what is wrong with us. And it makes no sense for this to go uninvestigated.
Exactly Robert.
Whether mold is a trigger or a cause is not the issue.
It is that researchers never made any effort to find out which it is.
As I told Dr Cheney in 1986, even if this WAS just a consequence of your “Agent X” then you would know by an explosion of mold complaints just how swiftly “Agent X” is moving through the population. So it is well worth monitoring for these complaints.
I have my 3rd appointment at the Klimas Clinic in October. Unfortunately, 2 weeks ago I had a bad crash. I need my little energy to recover and shouldn’t expend it traveling from the Midwest to FL unless they have something new to offer me right now. I had to stop the Famvir they prescribed because I had side effects and have not seen any benefit after 3 years experimenting with LDN. I already was tested for sleep apnea and mycotoxins and take charcoal. I also already take the Inosine and NAC they prescribe. Is there anything new they will do if I make the trip in Oct? I am thinking of postponing 6 months to give their good research time to result in a new treatment.
Cort, I know you get enough crap for all your hard work, but could you not use cake shots on the blog? So many of us are on really restricted diets and seeing cake is sometimes hard. 😉
🙂
I’m on a cake-free diet too!
They’ll be gone soon.
Ha Ha, Cort you had me seriously wishing, with mouthwatering, that I could eat some cake for breakfast.
Haha! You’re the best.
Plus they are not very appetizing cake shots. Thanks for taking them down. Tomatoes are in season – how about juicy tomatoes?
I think I’ll go with dark chocolate or something keto next time :).
So sorry your recorder cut out Cort, but you do seem to have a quite good memory regardless!
Of course, reading this piece gives me the nudge to try something new, Bacopa! While researching suppliers, I collided with the weird complex world of nootropics with many exotic supplements. I don’t know if Dr. Klimas is poking around there, but there certainly seems to be a lot of interested consumers buying them!
I also remember an article you wrote about a trial of NAC (to raise glutathione levels) with some success, but also that it is notoriously difficult to influence those levels directly. One needs to resort to the precursors which Learner1 pointed out, may or may not work.
Time to also report back about Stanford’s CFS Clinic treatment. I finally stopped taking Aripiprazole for a few weeks. Was forgetting everything at 2mg. per day so they had me go to 1mg. and still was falling asleep early afternoon.
Now that I was in clinic again they have corrected the dosage for everyone to .25mg. When I asked what’s next if this doesn’t work, they said Plaquenil. They also recommended an on-line self help site called http://www.cfsselfhelp.org which was partially developed by Dr. Charles Lapp. Seems as if all of us patients are part of a Stanford study. No comment except a sigh and eye roll on Dr. Montoya’s departure.
Look forward to your next report!
Thanks, Nancy B. , for opening up the field to responses about different therapies. I have to report back an extremely negative response to Mestinon, despite starting off with extremely small doses (I started with the syrup and used tiny amounts). Luckily it was possible to simply stop it short, rather than tapering down again (I tapered up to 30 mg bid). Waiting for it to wash out of my body.
Also grateful, Cort, for the info about bacopa.
PS I realize I should give more details about my negative response to Mestinon. I’d been warned about GI difficulties, which I was prepared to accept. I wasn’t prepared to accept the increased fatigue, increased muscle weakness (when I was taking it because it would increase my strength), tight muscle spasms, esp. in my legs and hips; dizziness and vertigo, and constant nausea. I stopped it 3 weeks ago and am still coming down from the side effecs.
Plaquenil is a pretty serious drug and can affect eyesight. Just saying. I think lupus doctors think of it a lot but maybe not so good for us. My opthalmologist said No to it.
I’ve had such a good response to 1800 mg of NAC daily. I used to get constant flus and colds and now I get them only occasionally and mildly.
Thanks, Cort, I’ve only just discovered your website. I’ve been sick for over 29 years, but only now am getting on the diagnosis train and into a program (have been told that could be 2 more years).
I am learning so much about this illness that I thought I had 25 years ago, but was somehow was convinced I didn’t for most of it. I know I will learn a lot from your website, and as soon as I am financially able, I would love to give some support. I’m recovering from a crash, so it may take time, but I wanted to say in the meantime, thank you for the awesome work you do!
Thanks Jane for your support and good luck with your program. I hope we hear good news from you at some point 🙂
I’m not so sure about the mold thing. I went to INIM and came back with a list of supplements I was already taking, and instructions to have my house tested for mold. My brand-new house in the desert, which I was not living in when I got sick. I’ve honestly lived in too many places in the past ten years for it to be environmental at all. The mold test they directed me to take isn’t even FDA approved. I wish they’d focus their energy on the research trials and just be honest about how little they can do for us clinically at this point.
The problem is that they have the philosophy that each treatment is additive, that if they can find thirty supplements that help a little, surely all of them would help a lot. I just don’t find that to be true, and each one comes with a cost. Those definitely are additive.
My biggest gains were when I stopped all the dang supplements and took the time and energy I was spending trying to treat the CFS and just rested instead.
Klimas’s research is world-class, though. We’re insanely lucky to have people like her. And you, Cort. Thanks as always for fighting the good fight.
Beth, my GI doctor advised me to do the same you did. He said to just drop all the supplements. I think at some point adding more just messes us up. I didn’t follow his advice to drop all of them, but I cut way back. A friend of mine divides his supplements in half, takes one or the second half every day. Gives his system some time to absorb them. Sounds smart to me. Especially in light of what the Cortene study showed, that CFS patients needed a much smaller amount of the substance Cortene was testing to have an effect. Less is more sometimes.
Interesting but my guess is that articles here run 10:1 in favor of ME research vs.
FM. What depresses me is that I know it is not Cort’s fault but rather reflects the medical indifference toward a disorder that probably affects 10 times more people than ME. Why? At 71, with 38 years of fibro, 8 with awful daily pain, it seems like understanding even at the basic level for FM is not there and will not be there in my lifetime, let alone seeing a cure. I can empathize with the other folks here getting up every day in dreadful pain. Deciding whether to continue is worth the pain is an issue I grapple with every day when I get up to virtually unbearable as opposed to just dreadful pain.
There are so many reasons for this. One, is simply that I started out in ME/CFS. More importantly the two diseases have been embraced by their communities in so different a manner.
ME/CFS has a huge advocacy presence, has several non-profit foundations devoted it, regular international conferences, several large Forums, and a community that’s very engaged in the science and advocacy. It ‘s a very vibrant space.
For some reason, none of those things have developed in the much larger FM community. I see little advocacy, few if any non-profit foundations, and no international conferences. It;s very puzzling. The FM community has the numbers – their potential is huge – but it has not engaged with its disease in the pro-active way the ME/CFS community has.
I imagine that’s just a historical accident – for some reason leaders showed up early in ME/cFS community who set the tone. It didn’t happen in FM. I sincerely hope it does – as an engaged and active FM community could do much both for them and for ME/CFS.
Maybe ME causes a stronger fight back at the disease reflex due to a stronger wired-and-tired thing?
For sure we are quite an active community despite being so badly debilitated.
Note: I have both ME and FM but I think it’s mainly the ME part giving me the fight-or-flee reflex.
My guess would be is that FM was never associated with a scary contagious outbreak.
It is the “Outbreak factor” that scared officials the most, and indeed, had it not been for the Lake Tahoe outbreak, there would be no “CFS” syndrome at all.
No Holmes investigation, no CDC committee to create it, no worldwide controversy over “What is CFS?”
I agree that FM is just as fascinating and worthy of research as ME & CFS are.
Erik, do you know what the recovery rate was at the Lake Tahoe outbreak?
In his 1999 CNN interview “Sick and Tired”, Dr Daniel Peterson responded to that question by saying “Although some have had substantial improvements, none have fully recovered”
When the interviewer expressed their surprise, “None?”, Dr Peterson repeated, “None”
Of those who have been sick five years or longer, I have also never seen a full recovery.
About 80% function was as good as it gets.
Health Rising’s recovery stories section is full of recoveries, some of which involved mold avoidance, most of which did not.
I have been taking Brahmi at night one 250 mg tablet. It calms the mind and increases speed and ability to comprehend. It also helps with multitasking. I am a CFS patient. Does Brahmi help with PEM ? well partially. If I cross the threshold by much then I still crash. So it is worth a try.
Thanks for sharing your Brahmi regime. How did you know what dose to take? and are there any negatives?
Forgot to add one more thing. Brahmi causes a 10 – 20 % increase in Free T4 level. So if you are taking thyroid medication. It is better to monitor it after you start Brahmi.
Thanks for that important information. So many of us have T3 issues
Can you provide the name or brand of the product you’re taking? I tried Bacopa a year or two ago and didn’t notice anything, but I know the right brand can make all the difference – thanks!
Re: Lost audio recording.
That sucks!! I recommend maybe having a backup from now on.
🙂
This happened with another interview as well – prompting me to buy a recorder instead of relying on an app.
Apps can “filter out” back ground noises for you. Some consider it a useful feature…
Hope the recorder will be a more faithful companion to you :-).
Thanks the Sony recorder has been a godsend (altho somehow I lost another recording (lol)
Cort,
My husband thought he’d had something similar happen while recording me ‘interviewing’ his 89 year old father about historic events that he lived through. It turns out that a recent update changed the recording behaviour on his phone so that the two ‘sides’ of the conversation were recorded on separate channels. At first he thought it had only recorded me, but finally realized that it had recorded his father on a separate channel. He finally twigged to this when he noticed his phone was displaying 2 recent recordings instead of 1.
Do you still have the original recordings? If you are technology proficient perhaps tinkering around a bit might dig up the other (very important) side of the conversation? Fingers crossed that your interviews are merely hiding – not missing.
Let’s talk about Gulf War Syndrome. The organization I direct sponsors the National Birth Defect Registry, a research project designed in collaboration with 7 prominent scientists. https://www.birthdefects.org/wp-content/uploads/2018/06/registry-doc.pdf We have health, genetic and exposure histories on the mothers and fathers of 10,000 children.
In the early 1990’s, the registry began to receive cases of birth defects in the children of Gulf War veterans. https://www.birthdefects.org/veterans-research/ In a short amount of time, we identified an increase in a rare cranial- facial birth defect in their children. Because we had a lot of national publicity for this discovery, I was invited to present our data to the Presidential Advisory Board on Gulf War Illnesses and later to the Veterans’ Administration’s Scientific Advisory Board https://www.birthdefects.org/wp-content/uploads/2014/04/VA-Presentation-GW.pd . The Department of Defense then funded a study at their research facility in San Diego. Their researcher found a tripling of the same birth defect in the Gulf War veterans’ children born in military hospitals. We had twice the cases because we also had those that had been transferred to civilian hospitals (a common occurrence in an at risk pregnancy).
Gulf War veterans were exposed to 31 categories of reproductive toxicants. In birth defect research, we know that the same exposures that can cause birth defects can also cause serious health problems in adults and older children who are exposed. Case in point, the U.S. was spared the tragedy of thalidomide because Dr. Frances Kelsey at the FDA was concerned about reports of severe peripheral neuropathy in adults who were exposed to thalidomide overseas.
One of the quickest ways to look for evidence of a toxin in the water, air or soil in a community is to monitor birth defects because they occur in 9 months or less while cancers, neurological deficits, cardiac disease, etc. can take much longer to track.
What does this have to do with ME/CFS? In contaminated communities, we frequently see a pattern of illness similar to ME/CFS before conditions with a longer time to manifest like cancer. Examples: TCE exposures in Woburn, MA; PBB exposure in the entire state of Michigan; cellusolve exposure in Silicon Valley.
Researchers we have worked with at the University of Texas have attributed Gulf War Syndrome to exposures to OP pesticides and nerve gas agents (the parents of OP pesticides). Since our birth defect registry collects data on the exposures of the Gulf War veteran fathers and mothers, we know that their uniforms were pre-treated with pesticides; their blankets, tents and other areas were sprayed with pesticides. And many veterans reported being in areas where alarms went off suggesting low level nerve gas agents.
As far as I can find out, Dr. Klimas is not looking at the dozens of extremely toxic exposures in the Gulf. And that includes the vaccinations that included everything from botulism to anthrax to plague as well as the solvents and preservatives in those vaccines.
One of the first signs of certain toxic exposures is a flu-like illness, so I have always wondered if more than 20% of ME/CFS cases began with a toxic exposure.
Betty I, I think all the man made chemicals all of us are exposed to, not only in war, but daily living, may have something to do with CFS–especially in genetically susceptible individuals. Unfortunately, with so many factors to untangle, trying to prove an association would be very, very difficult.
With the military it is even worse. One of the ‘secrets’ of Iraq and the Gulf War is that the battlefields are coated with spent uranium dust. It’s something the military doesn’t want people to know (but was revealed by an associate of mine who got multiple visits from high level military personal trying to get her to suppress it).
Just saw the 60 Minutes program about people attacked with strange sounds in Cuba and China (EFMs or something) suffering brain damage and lots of symptoms that are eerily similar to ME/CFS.
Sometimes I wonder if I shouldn’t spend a couple of weeks camping in a desert somewhere to see if I can get away from so much toxic exposure and see if I improve.
I agree we need to look at the effects on babies and also other little vulnerable creatures who are exposed to such stuff.
It’s so hard to figure out… my sympathies to everyone who is trying treatment after treatment yet still suffering…
Agree! I told Dr Klimas 10 years ago I thought ME was an environmental illness
I want to point out that Dr Klimas is actually one of the very few ME/CFS experts who is including environmental exposures into her assessment. She and others have spent considerable time at Dr. William Rea’s (now deceased) environmental illness clinic in Dallas.
And therein lies the problem.
Dr Klimas went out of her way to “Learn about mold” from somewhere OTHER than Dr Shoemaker and I.
Because that entails connecting mold and Chronic Fatigue Syndrome.
Dr Klimas is practicing “Evidence Avoidance”, otherwise known as “Willful Ignorance”, to create a false impression that she doesn’t know how toxic mold was at the very core of this famous mystery.
Eric your comments are now going to be moderated.
A – there’s no evidence that toxic mold is at the very core of this problem! There’s evidence that it’s one of many potential triggers – which only makes sense.
B – Please stop slamming our researchers and doctors and accusing them of negligence, willful denial, etc. That’s unfair to them. Please allow for the possibility that there are variety of views regarding ME/CFS and all – particularly those coming from doctors who’ve embraced this disease – are legitimate.
But Betty, why would Dr. Klimas would go to all this trouble of developing a comprehensive computational biological model of GWI and develop an animal model, and not include the effects of toxic exposures, vaccinations, etc in it? It would literally be impossible to develop an animal model with including those toxic exposures.
On another note, I have discovered a glutathione vitamin patch that delivers 500 mg. glutathione; 600 mg. NAC; 500 mg. vitamin C; 50 mg. magnesium and 1000 mg. COQ 10 and a few other things. Vitamin patches were originally developed for people who had weight loss surgery and couldn’t absorb enough oral vitamins. I have problems with almost all oral vitamins. I have “nothing” to do with this company, but if you want try the patches (they have many others) go to http://www.patchmd.com . (They have a 40% off sale today.) My daughter was having trouble sleeping and she says that wearing 2 glutathione patches at night put her right to sleep for the entire night.
Very interesting. Their Vit C “formula” looked good too, plus the Omega 3. Certainly worth trying. Thanks for the link. My gut is really tired of all the capsules!
“My daughter was having trouble sleeping and she says that wearing 2 glutathione patches at night put her right to sleep for the entire night.”
High Betty, would that be pure glutathione or patches with NAC, vitamin C and the other things as you described above?
Would there be downsides to it like allergic reactions or skin irritation? How long has she been using them?
Thanks
Cort, It doesn’t take a computational model or even the development of a new animal model to assess toxic exposures in the Gulf. We have plenty of animal models for the majority of toxins in the Gulf arena.
There are, however, better ways to determine what has happened to Gulf War veterans. Fat stored chemicals have an affinity for the brain where every neuron is encased in a fatty sheath. These chemicals also migrate to the reproductive system.
In addition to our work with GW vets, we have worked with Vietnam veterans since 1986. They have cancers, diabetes and other serious health disorders now service connected to their exposure to dioxin, the highly toxic contaminant of Agent Orange. We have found specific patterns of disabilities in their children and now it appears probable that this may continue into their grandchildren. Animal models show effects for 7 generations.
Dioxin can be measured in the veterans’ blood and seminal fluid. Research has shown that toxic chemicals like dioxin can cause epimutations of the sperm that can carry on through generations.
When we first started working with GW veterans, many reported burning seminal fluid, but no one bothered to check to see what was there or in their body fat.
What happened in Michigan in the 1970’s should have been instructive. In the civilian population, PBB, a flame retardant accidently mixed into animal feed, poisoned farm animals and farm families in the entire state of Michigan. This was discovered through testing a sample of animal fat with a gas chromatograph and a mass spectrometer. (Read, “The Poisoning of Michigan”).
When a team of specialists from the Mt.Sinai Environmental Unit came to Michigan and tested 1000 members of the farm families, the common denominator was immune system problems
In January, the CDC released this executive summary of biomonitoring of chemicals and heavy metals in the American population. https://www.cdc.gov/exposurereport/pdf/FourthReport_ExecutiveSummary.pdf If you want to read for a while, the entire 800 plus page summary is at this link. https://www.cdc.gov/exposurereport/pdf/FourthReport_UpdatedTables_Volume1_Jan2019-508.pdf
They wouldn’t be doing this monitoring if there wasn’t a concern about the effects of these toxins.
I have contacted Dr. Klimas about the birth defects we found in the children of Gulf War veterans. She never responded, so I really don’t know what she is doing to assess toxic exposures in the Gulf.
I am a co-chair of the National Institute of Environmental Health Sciences “Public Interest Partners”. Partners represent NGOs for health problems like breast cancer, autism, birth defects, autoimmune diseases, learning disabilities and lung problems. We have conference calls with NIEHS researchers several times a year and a face-to-face meeting with the director in December. I would like to see a bridge between the ME/CFS research communities and NIEHS researchers.
It’s certainly a fascinating area and I particularly feel for the poor Vietnam vets exposed to all those chemicals and as someone with MCS I can certainly relate to how impactful problems with chemicals can be. I imagine that we’re only scratching the surface.
My guess is that Dr. Klimas pouring all the research done on GWI into her models and using them to figure out what has happened and what treatments may work. She developed an animal model in order to help determine what happened when that soup of factors occurred – and importantly – to be able to first assess treatment effects. So yes, an animal model for GWI – she wishes she had one for ME/CFS – was probably very helpful.
I sincerely hope we can build a bridge between the environmental health and ME/CFS research communities. As I noted in a comment Dr. Klimas has been working with the Environmental Health Center in Dallas. I visited Dr. Rea at one point and I remember all the cases of poisoning from the farm communities in the Midwest. There’s no doubt that some cases of ME/CFS are linked to toxic exposures. I don’t know how that could not be.
Of course there can be no doubt of an environmental component.
The CDC investigation that launched CFS was into clusters of illness in Sick Buildings.
Dr Rea had nothing to do with the incident that started CFS, and he never made any effort to find out about it.
Cort, as you know, when you went to him in the 1990’s, he didn’t even mention toxic mold.
So it really makes no sense for Dr Klimas to go to Dr Rea, who didn’t know about CFS, rather than to Dr Shoemaker and a prototype for the CFS syndrome, who DO know.
Unless of course, Dr Klimas would rather not “solve CFS”
Which is what I believe to be the case, given her strange reluctance.
An honest researcher would take less than 30 seconds to go “What? An original source has information? I must look into this”
and respond appropriately.
When a researcher fails to do this, they can’t possibly be sincere.
Dejurgen, The glutathione patches have all the ingredients I listed. In ME/CFS allergic problems can always be a concern, but my daughter and I have not had any problems to date and we both have many allergies. We have been using the patches for a month.
It’s no surprise to me that immune hyperactivity feels just like exertion hyper-sensitivity: when you are inside the box, you can’t really tell the difference between the floor raised or the ceiling lowered. All you know is that you have so much less freedom. The question is whether the former is “true” CFS like the latter. In the sense that the patients recover once the underlying stressor is removed, it may not be (assuming that true CFS has no ongoing stressor). But I still think it is the same neuro-immune mechanism that is in the play, so we could learn a lot from studying it. Good luck to Dr. Klimas and her team.
Oops, this comment is posted as reply to Betty by mistake. Please read it as a stand-alone comment, not a reply..
Would love to get into one of her trials as I believe she would find so much from my body.
Mold exposure caused my ME/CFS. Were the GW soldiers exposed to mold mycotoxins in weapons? I wish someone would just up and recognize Mold mycotoxins as a cause and really try to help us. There are millions joining Toxic Mold Support Groups helping eachother, because scientists and the medical community are ignoring us. I volunteered for the ME/CFS research and no one has contacted me. I agree that there could be other causes as well, but mold makes too much sense. While you research everything but mold, families are losing their lives, health, and homes because of mold exposure every minute of every day.
Sorry to be cynical but I am not convinced. It sounds like a lot of ‘educated guesswork’ to me. I think Dr Klimas has always meant very well, but her output has in my opinion been underwhelming.
It is indeed a very complicated effort which is mostly new to the medical field – so skepticism is warranted. Given that it was good to hear that the Parkinson’s Foundation has embraced her approach.
Time will tell!
Prior to reading all these comments I didn’t realize that so many people were convinced that mold was a trigger to this disease. I was living in about as dry a climate as there is (San Diego County) when I became ill, in a fairly-new house with no known mold anywhere in my environment. Sadly I deployed to the Gulf War for 7 months and then again back to Iraq 3 more times, accumulating a total of 28 months in-country. I also was given a series of 6 anthrax vaccines and later on, booster shots. I feel that my immune system is in “overdrive” due to the fact that I almost never “get sick” with other things that those around me do. I was diagnosed with CFS but I guess I have GWI…….not that it makes any difference to me, having lost my entire life.
“The breakthroughs in ME/CFS treatment, they believe, will most likely come from systems biology efforts which use a variety of “omics” data (genomics, metabolomics, proteomics, etc.) ” Yes!!!!
Genomics, proteomics and transcriptomics show the iNOS pathway is upregulated in ME
http://followmeindenmark.blogspot.com/2019/09/genomics-proteomics-and-transcriptomics.html
AMPD3 in ME (genomics, epigenomics, transcriptomics, metabolomics)
http://followmeindenmark.blogspot.com/2019/08/ampd3-in-me.html
I have always been intrigued by Dr. Shoemaker’s treatment of toxic mold with cholestyramine. This is an older anticholesterol medicine that can also bind to certain chemicals and take them safely out of the body without having the chemicals redistribute in other tissues and organs.
Cholestyramine was used in the PBB-exposed families in Michigan and also in workers poisoning by a pesticide called Kepone made in the 1970’s.
Erik, I am also aware of the devastating effects of toxic molds. My husband was working for a foundation that was housed in an old building that had once been a metal foundry. He became suddenly and seriously ill with pericarditis (fluid around the heart). He was one of three members of the foundation’s 19 member staff to have the same unusual and serious health problem. Fortunately, all recovered.
Of course, I was worried about metal residues and that may have played a part in the illnesses. But it turned out the building was also contaminated with toxic black mold, a not uncommon event in the high humidity of Florida.
Erik Johnson has been placed on moderation and can no longer post.
If anyone is interested in his concepts, he can be found on Facebook.
https://www.facebook.com/groups/erikjohnsoneffect/
Being on moderation means exactly that – Erik’s comments will be moderated to stop his belittling comments regarding researchers and doctors from being presented. I want Eric to comment here and I don’t want comments stating the likes of Dr. Klimas is not interested in studying ME/CFS or that she’s being willfully ignorant etc. Everything else will be allowed through.
Cort, I commend you for your approach to dealing with Erik. He is a challenge. I have always been glad he regained his strength, but there is no conversation with him. I simply said adieu, in its full French meaning, when conversation on a site perhaps 20 years ago, cfs_research, stopped being conversation. He was always right or never listening. You are polite and clear, and separate the useful information from the useless insults. I think I have learned a lesson here!
Erik Johnson is right, about toxic mold exposure being the primary, and possibly the exclusive cause of ME/CFS. I have known him for 13 years, and I admire his tenacity and commitment to tell the truth, in the face of the credentialed opposition. If he were not having his posts “moderated”, he would be here, fighting the good fight.
Eric is welcome to fight the good fight here. He simply has to choose what’s more important: fighting the good fight; i.e. focusing on and informing the community about the dangers of mold or tearing down the reputations of our doctors and researchers.
Eric has chosen the second in the past and has been kicked off other Facebook. I hope he will decide that informing the ME/CFS community about mold takes priority this time.
Informing the ME/CFS community about the mold is what I have done since the day I started the CFS syndrome.
It’s kind of hard to discuss this without the implication that our “top researchers” are ignoring it, so I make no effort to cloak it.
It’s actually very easy to discuss the mold issue without hammering those who don’t agree with you. Instead of focusing on how right you are and how wrong they are you just focus on your experiences with mold.
Cort, J just want to say how much I appreciate your work. I may be a bit grump and cynical at times, for which I apologise. It’s probably because I have had my Hope’s dashed so often. But you are always amazingly patient and tolerant, and never defensive.
You give us a voice, and you present some fascinating research.
I think we all need to accept that our disease, unfortunately, is a complex one. And I’m sure all researchers are sincere and giving it their best.
So nice of you to say Matthias! We all deserve to be a little grumpy at times 🙂 I too am almost reflexively pessimistic about new treatment options. I’m very excited about the science but that next step – to treatment – is a hard one. Plus Dr. Klimas and her team are out on the skinny branches. This has never been tried to this extent in medicine so far as I know. Crossing my fingers that she, her team and Gordon Broderick are creating a new way of understanding and treating illnesses.
For whomever this might be helpful:
I was diagnosed around 8 yrs. ago with ME/CFS. This is still my diagnosis.
I am currently a patient of Dr. Mary Ackerley (mypasion4health.com).
-Never have had mold considered, by devoted practitioners for ME/CFS or by myself.
Dr. Mary is among the foremost in the mold field.
I live in Az., which is a “direct to consumer” test order state., meaning patients can self order lab. If you aren’t in such a state, you can still order lab yourself through the following 2 labs: See their websites for info on that.
I ordered both RealTime’s lab test and Great Plains Lab’s mold tests (two different methodologies).- In my case, BOTH were sky high for mycotoxins!-
Michael Schrantz (environmentalanalytics.net) travels the country, works closely with Dr. Mary.
I HIGHLY recommend his services for home mold testing. ..Not cheap but he is devoted to your welfare and is most conscientious and knowledgeable…the best!
So a mold source was found in my home- NOT visible.
I am going through the remediation process/reconstruction of my kitchen right now.
Dr. Mary was certain there had to be a home source, given my lab values- and she was sure right!
My point is that I encourage you to have your home environment PROPERLY checked for mold. Just a simple air sample is NOT sufficient- Beware! I had that done in the past. It must be a very thorough testing process.
My hunch is that this is a huge first step for me- that this will allow me to continue unpeeling the onion. I would love a magic, one-stop-shop bullet, that solves my illness. However, I am grateful as anything! that this has been found. High bodily mycotoxin is highly immunosuppressant- So to get to first base 1) the home (or work) source(s) must be found if you test high 2 ) the mycotoxins must be cleared from the body. This can take some time.
Dr. Mary considers herself a “biotoxin illness” specialist, which includes the biotoxin pathway issues: mold, Lyme/co-infections and viral activations (such as EBV, etc.)
Myself, again lots of onion-unpeeling to do but cleaning out mold is what I consider the first, critical step in my recovery. I was referred to Dr. Mary by Dr. Neil Nathan who is in N. Ca.
His book Toxic is a knowledgeable, compassionate reference…outstanding.
Blessings to each of you on your journey, Galia
Dear Mutual friends with ME/CFS, What interesting comments this evening. Thank you to all of you. About 30 years ago I began studying biochemistry 2-8 hours a day in order to figure out not only what was wrong with my own body that had seemingly betrayed me forever, but also why most of my students and colleagues were coming down with the exact same symptoms of ME/CFS. I was terrified that we had some communicable illness that was being ignored or just not recognized that was not only destroying people’s health but also their attitudes and cognitive ability. I have now spent seven years writing a book about my findings, so I just have to mention one thing about the mold issue, which I too certainly could not neglect. I contacted one of the nation’s top mycologists who stated that molds release a gas into the air which is called “1-octen-3-ol” and it is 80 times more potent than toluene in damaging the dopamine receptors of the body.This is a gas, so we cannot possibly see it.
My apartment was flooded this past winter and even though the place was more or less gutted by the construction workers, the area above my sink, in the framing of the window which had had visible pock marks of mold there, still makes my whole body shake if I even get close to it. One thing I have used to counteract that airborne effect of mold is vinegar. I just spray it into the air, and even onto my own hair and clothing. Vitamin C is also a mold fighter, so I make sure that I take plenty of that. And I try to cook with lots of garlic and sage, just to get them into the air.
Certain plants are also mold fighters. English Ivy (Hedera helix) is a known mold fighter and is an anti-inflammatory as well. It also opens up bronchial passages. So, I regularly restock my apartment with containers of living English ivy. To fight the unpleasant effects of my kitchen window still emanating mold effluvia, this fall, I gathered branches of oak leaves, which contain quercetin, and stuffed them onto the top of the curtain rod. Seems to help somewhat. Everything thing people have mentioned this evening on this site corroborate my findings also. It was a “grunt” to dig all that out. I have thousands and thousands of articles filed here on so many subjects related to this scourge. I have found short term palliative solutions but nothing that ever continues to work. I just have to believe that our collective and shared wisdom and research will find a solution to this chronic misery. Best wishes to all.
Is Dr. Klimas at the Sandford Clinic in Florida?
She’s at Novasoutheastern at the Institute for Neuroimmune Medicine.