

Pain – A Surprisingly Complex Experience
Pain seems pretty elementary – it hurts! When it really hurts, you want to throw yourself out of your skin. It’s actually not so simple. Pain is often described as a complex, “biopsychosocial phenomenon“. The International Association for the Study of Pain describes pain as an “unpleasant sensory and emotional experience”.
There’s the sensory side of pain – how the pain signals get to the brain and are processed – and the sensations they produce. We know those processes are damaged in fibromyalgia, but that’s not nearly the end of the pain situation for those with fibromyalgia or chronic pain.

Pain is more than a body sensation: it’s a complex experience put together by several different parts of the brain.
There’s also a cognitive element to pain. Triathletes, marathon runners, swimmers and other athletes, for instance, are able to push through high levels of pain partly because they know it’s going to be limited in duration; i.e. it’s controllable. Simply believing that you can control or handle or withstand your pain actually makes the pain less severe. Pain levels spike, on the other hand, in people who do not believe they can handle their pain.
That emotional aspect – the fear and other emotions associated with pain – also plays a major role in how we experience pain. Emotions and pain are necessarily hard-wired together. Pain, after all, is the stimulus our bodies use to tell us an injury has occurred. Our brain uses emotions like fear to ensure that we get the message, respond to and resolve the situation. The fear, anxiety, anger, etc. – what researchers call the “unpleasantness factor” – that pain arouses in us makes up the second major part of pain.
It turns out that pain sensations – surprise, surprise – are not necessarily unpleasant – they’re just very strong sensations. Patch them together, though, with a bunch of unpleasantness, and you get PAIN… Without that unpleasantness aspect, people with FM or ME/CFS might be distracted by the intensity or bizarreness of their sensations, but they won’t necessarily be bothered by them.
The sensation+unpleasantness=PAIN patch is usually quite effective at prodding someone to take the actions needed to relieve their pain and return to health. But what about someone sitting in a toxic stew of pain and fear for years on end. They’re certainly not experiencing an adaptive or effective pain response. They’re in the midst of a chronic pain response that has run amok, is causing pain for no good reason, and is doing no one – not the person experiencing it nor the community they live in – any good.
Finding out how all that “unpleasantness” – a typically mild scientific word for a pretty darn torturous situation – occurs, then, is a big deal. If we knew how unpleasantness got mixed in with pain, we might be able to make pain a heck of a lot easier to deal with. Earlier this year some Stanford researchers made a breakthrough in understanding this core aspect of pain.
Tracking Down the Hurt That Comes with Pain
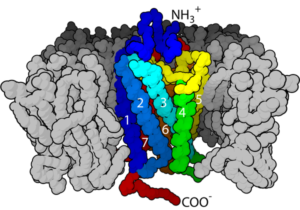
Researchers have pretty well mapped out how the sensory aspect of pain occurs. Tracking down the origins of the “unpleasantness” aspect of pain – which turns out to be buried deep in the brain – has been considerably more difficult. Some of the pathways have been mapped, but finding neurons which start the process off has proved elusive. New technology developed at Stanford, however, is tracking them down.
Science. 2019 Jan 18;363(6424):276-281. doi: 10.1126/science.aap8586. An amygdalar neural ensemble that encodes the unpleasantness of pain. Corder G1,2,3,4, Ahanonu B5,6,7, Grewe BF5,7, Wang D1, Schnitzer MJ8,6,7,9, Scherrer G10,2,3,4,11.
As reported in Science in January, Stanford researchers used a miniaturized microscope, called a “miniscope”, which is able to probe deep into the brains of mice and determine which neurons are turning themselves on in response to a painful stimuli. They charted two responses – a response when their paw was pricked with a pin and the animals’ attempts to avoid further pin-pricks or their licking the pricked paw.
The first response indicated that the pin-prick did indeed induce a pain sensation. The second response indicated that it was associated with unpleasantness. They found that repeated pin-pricks caused the animals to attempt to escape from the pin-pricks and/or lick the pricked paw. The pin-pricks were clearly unpleasant to them.

It’s the “unpleasantness” part of pain which makes pain so difficult to tolerate. Turn off the unpleasantness factor and what is experienced as pain might seem like just another body sensation.
Using what one reviewer called “some of the most advanced techniques” in neuroscience, the Stanford researchers were able to turn on and off neurons associated with pain response. Turning off one set of neurons in the basolateral amygdala (BLA) maintained the animals awareness of the sensation but left them utterly unconcerned about it. The researchers could prick the animals again and again without the animals showing any signs that it was unpleasant to them.
After reviewing the study, Benedict Kolber, Duquesne University, stated that the “full flavor” of pain had been lost. The lead author of the study, Grégory Scherrer, simply stated that the animals “essentially didn’t care about pain anymore”.
Then they exposed the mice to high levels of heat and cold. Again, the mice with the BLA neurons turned off exhibited fewer signs that the temperature changes were unpleasant compared to normal mice.
The researchers then induced a short-term course of sciatica in the mice to see if being in acute pain affected the BLA region. It didn’t – suggesting that acute pain does not, by itself, necessarily cause the amygdala to up the unpleasantness factor. Interestingly, though, light touch did increase neuronal activity – which indicates that this part of the amygdala probably plays a role in the development of allodynia and chronic pain.
They then let the mice develop a full course of allodynia. After they’d become sensitive to even the lightest of touches, the researchers turned off their BLA neurons and saw the animals’ distress levels plummet. When they did the same process with cold-induced allodynia, the animals’ aversion to cold completely disappeared.
The researchers had found a way to take the hurt out of pain.
Chronic fatigue syndrome (ME/CFS) and Fibromyalgia (FM)
While the focus on the basolateral amygdala is new, the amygdala and the limbic system have quite a history in ME/CFS and FM. Back in the 1990’s, in “The Chronic Fatigue Syndromes: A Limbic Hypothesis”, Dr. Jay Goldstein proposed that the amygdala – with its connections to the brainstem, hypothalamus and other cortical areas – was likely part of the “final common pathway”, where a damaged limbic system induced changes in ME/CFS patients’ brains.
In 2002, Ashok Gupta proposed that amygdala activation causes immune reactivation/dysfunction and chronic sympathetic nervous system stimulation, which produces mental and physical exhaustion and other symptoms. His Amygdala Retraining Program – now called Gupta Program Brain Retraining – attempts to tame a hyperactive limbic and brain through neurolinguistic reprogramming and meditative and mindfulness practices.
A recent fibromyalgia Israeli study touted the success of a neurofeedback protocol aimed at the amygdala. Another recent study suggested that when milnacipran works, it does so in part by altering activity in the amygdala. Grey matter alterations, increased glutamate, functional and structural alterations, overactivity at rest, and reduced opioid binding potentials have all been found in the amygdalas of people with fibromyalgia.
Location Matters
This study is a reminder why it’s so good to have ME/CFS researchers working at places like Stanford and Harvard. It’s no surprise that this study – which was published in the journal Science – happened at Stanford. For one, Stanford is known for its pain research. (It’s where Jarred Younger did his post-graduate explorations into pain and fibromyalgia.)
More importantly, places like Stanford and Harvard are where top scientists and their toys meet up and produce creative new studies. Reviewer after reviewer applauded the new techniques used in the study, which one said “will be very valuable to the pain field in the future”.
The study happened because Scherrer – the senior author interested in the unpleasantness aspect of pain – happened to work next door to Mark Schnitzer, the developer of the miniscope. It resulted from the “many conversations” the two next door neighbors had over the years.
Next Steps
Now that the researchers have determined where in the brain sensory sensations get turned into fear and churning, painful experiences, the next steps include better mapping of the pathways involved, one of which involves the nucleus accumbens – a part of the basal ganglia which has been highlighted in ME/CFS.
The next step is to try to isolate a receptor which a drug could attach to and shut down – and turn down the hurt in chronic pain.
Researchers also want to learn how this particular region of the amygdala gets altered in the first place, but uppermost on the Stanford researchers’ list is looking for receptors or ion channels on the BLA neurons which could be targeted with drugs – which could shut down the unpleasantness factor that makes chronic pain so very painful.
It will take time to unravel all this, but the implications of the study – to be able to turn off the hurt that comes with pain – are enormous. Kolber in The Pain Research Forum stated:
“From a therapeutic perspective, these findings could be extremely powerful, because if we could just get rid of the negative valence of pain, then even a patient with a 10 on an intensity pain scale could say it doesn’t bother them—that it’s a 1 on an unpleasantness scale—which would greatly increase their quality of life.”






If we do not experience the pain is it possible we will ignore our bodies needs and cause other damage potentially?
Such a fraught topic. Though perhaps a no-brainer (Pun intended) for those who sadly suffer constant and chronic pain.
I agree with you. In my personal case I learned over the years that very few if any pain coming from this disease was “wrong” as in not indicating something physically was wrong.
Even when pain levels went beyond extreme and it was not clear what was wrong, I later learned that they indeed indicated things went seriously wrong in my body and these underlying issues had to be resolved urgently. Unfortunately this type of pain is very very hard to interpret and near not pointing to the root causes.
In those cases that I learned more what a certain type of pain was pointing too, trying to correct the underlying issue if possible reduced pain levels a lot. Ignoring to do so for some time caused flares of that type of pain.
As to the mouse experiments: by shutting of these key neurons they learned the mouse to not respond nor perceive damaging events as being harmful. While I can see it increases their comfort, I doubt it would still do so if their paw got badly infected by “not minding” being pricked or their skin and organs damaged by cold or heat treatment. The researchers removed the hurt but also the protective function of pain IMO!
I can see that removing this hurt does not sound a bad thing if you don’t know what to do against it anyway, like in chronic FM pain, but I find it easy to see that this large amounts of pain “help” people pace or avoid exhausting their muscles even more. Take away that pain and they might be compelled to further damage their tissue to “a point of no return”.
I for example had first many years of pain at ever increasing strength but I learned to ever better deal with very high levels of pain. Pain did largely not stop me from living my life, even if levels were extreme from time to time. But I paid a heavy price for that “skill”. Utter exhaustion making me unable to further deplete and wreck my body did stop me in my tracks, and it did it “very well”.
As to the marathon runners being able to push through pain because they know it is only temporary and thus pain having quite an aspect of knowing to be able to cope with it and thus also having an emotional aspect, I see a large gap in this idea.
Just like running a marathon places physical stress on your muscles, being in intense pain places a physical stress on the brain and the pain processing pathways. Just as much as running at that pace for 3 hours isn’t exhausting the muscles as much as trying to do so for 3 weeks continuously, having intense pain for 3 hours doesn’t exhaust the brain and it’s pain processing pathways as much as having it for 3 weeks or 3 years. So again the emotional / willpower aspect is overrated in the marathon example.
There’s a difference between a pain response that works correctly and one that is pathologically disturbed as in FM and many cases of ME/CFS. The experiment was not about reducing the pain of a bad infection or acute injury (check out the sciatica section). It was about reducing the unpleasantness associated with a chronically and pathologically upregulated pain response system. The researchers actually induced that – and then took it away.
You were able to push past your pain at the cost of further exhaustion. I don’t think that’s what they’re focused on here.
Totally agree. I think the analogies and writing in this article are misleading. It makes it sound like people with CFS and Fibro have learned to mind pain more than they ought. This is what our doctor thinks is that my daughter has a perception of her pain that makes it worse than it is. BS. I’m sorry, but that just doesn’t ring true. She was always a tough kid who didn’t cry easily when hurt and I see her being incredibly tough through all kinds of pain that all people find very painful (tonsillectomy, migraine). I hate that people are going to read this and interpret it this way. More in-your-head BS.
The problem with people with FM and many people with ME/CFS is that their pain processing pathways are way overactivated. FInding a drug which calms those processes down should restore them to normal functioning not make them oblivious to all pain. Instead of feeling pain all over for no good reason you would feel normal.
I have always had a pretty high tolerance for pain (I’m a nurse and let students practice starting IVs on me) but it is at night that I realize it is bothering me and I can’t get to sleep. Must be because I am more distracted during the day. Also, post op patients get pain relief from foot massages, another pleasant distraction. I wish I had a reflexologist every night!
Distraction can be effective in relieving pain. More on this and other ways to mindfully relieve pain coming up.
The best relief from the pain of the contractions I had (for around 36 hours) when giving birth to my son, was rapidly following the patterns on the curtains surrounding my hospital bed, with my eyes. Not a long term solution obviously but it helped at the time.
Your assumption that there is no good reason is unsupported and harmful, Cort. You don’t know the pathways are overactivated. That has not been established as a fact.
Your doctor is wrong. Study after study shows that people with fibromyalgia are being pummeled with pain signals that emanate from a pathologically broken nervous system. It’s not that they are minding pain more – it’s more that pain is minding them – forcing them to experience pain. You should ask him to read the medical literature at some point!
This study reinforces that there is a physiological basis to chronic pain by the way – not the other way around.
Of course her doctor is wrong. And she feeds off articles written like this to support her incorrect thinking. You certainly don’t communicate that there is a biological cause for the pain well, Cort. Even in your comments you claim there is *no actual harm* associated with the pain. look at Ron Davis’ son and tell me there is only a problem with the perception of pain there. You promote a potentially harmful theory postulating that the pain has no true or valid function by saying there is no real biological harm present beneath, per your example, a patient’s inability to be touched without pain. We don’t now if/what harm is specifically being done but we can see very real harm.The fact that there is a pain response that can be completely normal after a tonsillectomy but is out of control the day after a massage indicates you cannot just turn the entire pain response down without also dampening its normal function. I’m all for learning as much as we can about all systems, I just don’t appreciate you pedaling the idea that ME & Fibro patients aren’t experience actual harm beneath their pain. Or wording it in a way that it is easily interpreted as a perception of pain issue. That is a recipe for abuse and potentially disastrous treatment.
I’ve been absent from this site for a few months. I wish I could reply to Holly directly, but her comments are all replies.
I continue to completely and utterly reject the notion that FM is primarily amplification of pain that would otherwise not be debilitating.
The pain is associated with obvious, palpable distortions in muscle tissue. My own successful protocol by which I have now 90% recovered from FM, has involved successfully reducing those distortions and restoring muscle tissue to normal pliability. Gaining limb range of movement, gaining function, and reducing pain have been outcomes proceeding in parallel.
I so strongly reject the “over-sensitive” hypothesis, that I believe the OPPOSITE is true. People with FM are NOT even sensing the pain they SHOULD be sensing from the severe distortions in their muscle tissue. They literally have “pinched nerves” all over the body. The pain sensing system is utterly overloaded and can’t allow the victim to feel all of it – the most painful spots tend to be the only ones “felt”. But when palpating any one of the dozens of spots that the victim is “unaware of” at the given moment, it is like palpating a raw wound! The gentlest palpation sends the pain at that spot off the charts.
The arrogance in the mainstream medical profession about these self-evident points, is disgraceful. I had one “expert” researcher tell me that palpability was “unscientific”! Presumably the palpability of a cancer lump of any kind is “unscientific” too until it is diagnosed as cancer!
Ironically, there IS scientific research finding out more and more about these distortions; their hypoxity, the altered stated of tissue, the adhesions – but the majority of “researchers” prefer to ignore this. Reading Devin Starlanyl’s book on Myofascial Pain Syndrome for the first time was a revelation to me, even though I disagree with her faith in Trigger Point Therapy. It contained so much references to research that confirms the “tissue dysfunction” hypothesis.
I will be very interested to know what happens to FM patients who have their pain artificially suppressed. I don’t believe for a moment that they will gain limb range of movement or functionality. I also strongly suspect that they will be numbed to pain signals that they actually do need to know about.
As my muscle tissue has been restored by the right mix of treatments, the hands-on therapists have noted, along with range of movement and overall functionality, the reinstatement of normal or better-than-normal tolerance to the pain of vigorous hands-on treatment. It is simply too fantastic to think that the successful protocol I have developed, somehow “dials back the pain system” as an accidental consequence, and all the restoration of normality to actual muscle tissue is misleading me to the wrong conclusions.
Thanks Phil. You know I fully agree that more focus needs to be on the muscles. As to “artificial suppression” (which IMO is not what this research is about) what about people who “artificially suppress” their pain using painkillers of all stripes, LDN, Cannabis, ketamine, kratom, baclofen, etc.?
First of all pain is mostly physical if you turn off the emotional it’s still there. Secondly these mice were tested in their reaction to cold. Cold is different than pain I sit on ice because I prefer the cold to pain. Another vs Stanford psycho study
Turn off the pain for fibromyalgia please.
That’s the goal. Note that the NIH’s Heal Initiative is pumping a whole bunch of money into understanding the cause of pain and developing new drugs. If you haven’t tried Cannabis or low dose naltrexone you might want to give those a try.
Cindy,
Turn off the PAIN ”PLEASE” !!!!! I UNDERSTAND WELL. when I die wish I could donate my body, brain ,everything to help prove there is a problem with the unknown problems so many have. It’s real and scary. I feel the brain has a lot to do with letting us know there is a problem!
Interesting study as a lady suffering chronic fatigue ,with fibromyalgia ,& autoimmune problems coeliac disease .
As a result i have been a very bad insomniac only surviving between 3 -4 hrs of broken sleep per night for over 30 yrs because of chronic pain i find it very difficult to function on a physical & mental cognitive level on a day to day basis it would be fantastic to be able to press these receptors to have reduced scale of pain & some quality of life. I so miss living my Life ! Still seeking the holy grail for chronic persistent pain
Ouch! Besides being terribly fatiguing the problem with poor sleep is that it heightens your pain levels. If you could find a way to get better sleep your pain would probably diminish to some extent.
I’ve been on ambien for at least 15 years. If I don’t take it, I don’t sleep. Maybe some of my daytime fatigue is from ambien? Had a sleep study last year. Sleep apnea. Have an apnea mouth appliance and get better sleep but still can’t get to sleep on my own. I think this is a huge part of ME and fibro.
We have a very interesting blog on sleep coming out. Be sure to check it out. Ambien it turns out does get you to sleep but it also steals deep sleep from you.
Very interesting report. I understand the points made above, but if it could be possible to read and “obey” the pain without the distress of it (which would require some responsibility, and also maybe an unhealthy amount of self-focus?) — anyway, if that were possible, maybe the Alert function of pain could continue without the distress element. Isn’t that what meditation and mindfulness at least in part tries to do? I think some of the spiritual traditions address some of this. Also, re the LD runners, aren’t they also experiencing a dopamine high that helps them push through the pain?
Yes, the idea is to reduce the distress element which is magnifying the pain for people with chronic pain down to a normal level – to a level where your body reacts properly to a painful event but is not caught in this ongoing pain trap.
Mindfulness and meditation so far as I know attempt to work on taking the unpleasantness out of pain and interacting it with it as a kind of sensation.
There’s the runners high and there’s also the potential of a reward at the end of race. Both are probably helping to dull the pain.
Sorry Cort,
I’ve tried mindfulness, meditation, ect.. Reseptors in the brain doesn’t let you get where a normal brain would respond. It just keeps working,reminding you of your pain & have to shift body around to find a confortable place. Just like sleeping. It’s not that easy to just lay down & go to sleep. the mind is still working!!
It’s not just about pain. Pain is of course a factor but we must not disguard the fundamental problem identified with the potassium ion channel receptors in every cell. The physical ability of cells to function in a normal fashion is compromised. This is the crux for everything, tinkering with anything else is akin to putting a band-aid on a gushing artery. We need a coordinated approach to every aspect, pain, energy, cognition.
Is Substance-P ever brought up in relation to pain? Im not talking just on this forum, but anywhere….
Absolutely – substance P levels are increased in fibromyalgia – check out a bunch of studies on that – https://www.ncbi.nlm.nih.gov/pubmed/?term=substance+P+fibromyalgia
Cool,
Thanks Cort!
Dan
Fascinating. Thank you.
I wonder if some of us experience the “unpleasantness” WITHOUT the pain. I have a diagnosis of FM based on my disturbed sleep patterns, sensory hyper-senstivity, brain fog, fatigue etc. (And exclusion of other explanations of my symptoms.) But I have, for the most part, very little distinct pain. Instead I have persistent “unpleasant” sensations in my body…. fragility, pressure, unease, squirminess, discomfort etc, accompanied by the flight/fight/freeze response if those sensations are intense or triggered by multiple stimuli. So perhaps that is that brain stem area activating without perceiving pain specifically…?
Jarred Younger believes the microglia in the brain can be producing all sorts of symptoms. Yours might be being tweaked in a way as to produce these strange symptoms which I think are pretty darn common in ME/CFS and FM. I certainly recognize them.
hi Rebecca,
Based on your symptoms, I wouldnt be surprised of Glutamate Excitoxicity in your situation. Have you tried cutting free-form glutamate out of your diet?
Best,
Dan
This disturbs me. As a cyclist, I was used to competing in races of 60 miles. In training, I would cycle 100+ miles a week, doing speed and endurance rides to build my stamina. I was used to pushing through the temporary pain of oxygen and energy depleted muscles filled with lactic acid, just so I could complete the race.
I developed ME on 17th August 2005 whilst on a cycling holiday around North Wales, whilst on a gentle 30 mile ride. I’ve never been able to get on my bike since.
I am in pain every day, pain that increases when I try to walk more than a few steps. It is nothing like the pain I could push through when cycling; it’s a pain that stabs my hip joints, preventing me from walking or bending. I’m on fentanyl patches, gabapentin. baclofen, paracetamol, ibuprofen and duloxetine for the pain. I still experience pain.
Last Wednesday I had one of the (thankfully rare) painful digestion incidents, where 1/2 an hour after eating, I had extreme stomach pains and my body rebelled and expelled the food I’d eaten. The pain normally goes over the next 12 hours, and I sleep. This time it didn’t, got steadily worse and on Friday I was admitted to hospital.
Without that pain, I would not have known there was something seriously wrong with me.
One of the things that is certainly wrong with fibromyalgia and presumably many people with ME/CFS is a hypersensitive pain response which is going off all the time. The fact that your pain now is different than it was when you were a cyclist suggests a different process is going on – perhaps like your brain is registering pain in places a normal brain wouldn’t. (Or maybe there is some other problem in your body which we haven’t discovered yet.)
Jarred Younger describes a situation in ME/CFS where he believes the microglial cells in the brains are pumping out pro-inflammatory cytokines that cause pain and many other symptoms at the slightest impulse and he’s found widespread neuroinflammation in ME/CFS. If he’s right then it’s your brain and nervous system which is producing your pain. In that case something which reduces a hyperactivated brain circuit which enhances “unpleasantness” might be a good idea.
Again – this is not about getting out of or ignoring acute pain – this is about getting at the chronic pain which hobbles people with fibromyalgia, ME/CFS and so many other illnesses. Researchers have shown that chronic pain is different from other kinds of pain. This finding has nothing at all to do with not being able to respond to a stomach virus or a broken leg or a wound or whatever.
The goal is simply to return the pain response to normality so that it functions properly.
This is some real “Black Mirror” shit!
The problem is we have no idea whether the procedure really ceased the sensation pain, or whether it simply led to a disconnect in the behavioural response. Which leads to human trials, which leads to…
On the topic of endurance athletes though, athletes do not ignore pain, they simply know what is normal pain and what isn’t normal pain. My father has run over 100 marathons and entered around a dozen ultraendurance 24h+ events and I can tell you, he has pulled out more than a few times because pain was telling him that something wasn’t quite right.
But fatigue and pain perception are not the same. Pain warns of damage, but perception of fatigue simply warns that there is uncertainty in the level of effort required to achieve the same level of performance. (the 2 day CPET results show reduced performance at the ventilatory threshold (gas exchange threshold) on the second day – note I am saying VT, not anerobic threshold, they are not synonymous)
There’s a difference between the pain response in a normal healthy person, and say, someone with fibromyalgia. Your fathers experience with marathons is different. When he feels pain it means “damage” (but certainly not permanent damage – I’ll bet he felt pain in every marathon he ran – but he was able to distinguish between the normal pain associated with running in a marathon and the pain which signifies a possible injury.
There’s no evidence, on the other hand, that the kind of everyday pain someone with fibromyalgia experience warns of damage. Some people with FM and ME/CFS can experience pain from the lightest of touches – but the touch is not producing damage – the pain comes from a hypersensitized pain response. It’s that aspect of pain which these researchers are trying to get at.
But a generalised hypersensitized pain response does not seem to be a sensitive factor (no where near 99% on any test) associated with either Fibromyalgia or ME/CFS.
Blood pressure cuff induced ‘allodynia’ for example has poor sensitivity in Fibromyalgia patients. (studies I have read found 29-69% sensitivity), suggesting that any increased pain sensitivity to pressure is a secondary, rather than primary factor.
But, but, but FM is basically defined by a generalized, hypersensitive pain response. (A patient satisfies diagnostic criteria for fibromyalgia if the following 3 conditions are met: 1. Widespread pain index (WPI) ≥7 and symptom severity (SS) scale score ≥5 or WPI 3 – 6 and SS scale score ≥9)
That shows up issues at the spinal cord and in various pathways in the brain. I think the big question for FM is how the body contributes or not to that central sensitization
What about ME/CFS? It’s certainly very possible that the pain and fatigue is caused by metabolic issues in the body (and brain) but there’s also evidence for a very twitchy pain response in ME/CFS. Alan Light’s studies showed that exercise prompted dramatic increases in muscle metabolite sensing receptors that code for pain and fatigue. Light believed it was this hyperactive response by the immune and nervous system that was responsible – not increased levels of muscle metabolites.
https://www.ncbi.nlm.nih.gov/pubmed/22210239
My guess is both metabolic and nervous system issues are present. Either one could be driving or acting in alignment with the other.
again, this does not ring true. My daughter has no pain when getting a massage but experiences severe pain the next day for several days from the stimulation. The experience wasn’t painful to begin with. There is something else happening and turning down the pain response will only create the unwanted side effect of being unable to feel real pain that Is vital to warning us of danger. People have become paralyzed and even died from being pushed too hard, who gave CFS. This is a fascinating thing to understand and to be able to control in specific circumstances, but it is a bandaid.
I don’t understand the resistance to a treatment option that would relieve pain. Opioids relieve pain. Cannabis relieves pain. LDN relieves pain – all these options relieve pain without these horror stories happening. Why would you think this would be different?
The last thing a researcher or drug company would want to do is to remove an appropriate pain response. An drug that did prevented people from responding to pain appropriately would quickly be ladled with lawsuits and off the market.
I’m a bit confused by this because I thought there was evidence of dysfunction in mitochondria that leads to rapid build up of lactic acid in ME/CFS . Would this not still happen even if sensory pathways turned off to unpleasant sensation and would this not lead to damage if we push on? I do also have all over body pain from fibro which I experience as something different?
I’d be interested to know what medications others use to ease pain – I’ve been offered Amitriptyline, Gabapentin, nerve block injections etc but reluctant to try. I do take a small amount of Zopiclone because I feel sleep deprivation is paramount in making symptoms worse. The reason I’m reluctant to take medication is because so many sufferers seem to be on a cocktail of drugs without finding any real benefit. I’d rather keep my nervous system free from side effects and concentrate on sleep issues and meditation. The Gupta regime helps but did not free me from ME – it really helps to calm down the nervous system though.
There is evidence of abnormal lactic acid buildup during a two-day maximal exercise test in which the participants exercised to exhaustion. I don’t believe one day maximal exercise tests showed that.
Note though that’s during an exercise test to exhaustion. Whether that finding applies to yours and my problems with walking or routine activity is another question entirely.
The mitochondrial findings are quite mixed with most tests finding normal or increased mitochondrial output. Those findings though are taken from mitochondria isolated from the blood.
Baseline tests which don’t show elevated levels of lactic acid suggest that it doesn’t.
I agree with the folks here who raise concerns about this.
Yes, it is hopeful for those in chronic pain. BUT traditional medicine has a terrible track record in terms of treating pain in the context of healing and curing. Indeed, traditional medicine today doesn’t even try in any significant way to address the holistic operation of illness, the human body or the human being.
It is a super exceptional excellent doctor (maybe 1%??) who does not just give drugs as “cures” for symptoms, to deaden symptoms, make them go away. It is not about healing the underlying condition, or supporting the body in doing so. This makes all drugs potentially destructive.
At this time in history, it is up to us as individuals to care for our body as a whole, and our being as a whole. Medicine doesn’t do it. The last 30 years of mind-body research has opened the door for us to take care of ourselves, as conventional medicine doesn’t. Awareness of this systemic problem is heightened to a ridiculous degree with CFS, in my experience.
This notion that “some pain is obviously helpful, like pain from a hot stove so you can take it off; while chronic pain from illness is not helpful” is stated as though it’s obviously true. As other people here have commented, it is not. The pain from chronic illness must be explored, regularly and carefully.
Used by a skilled doctor or a wise patient, new pain killing medication or treatment based on these studies can of course be helpful in moving towards health. “Skilled” and “wise” are definitely key. It could theoretically be helpful if a person in chronic pain who was otherwise exploring and practicing things that support health took pain killers for a while at night in order to sleep. Killing pain indiscriminately without any extensive exploration and recommendation of how to move towards health holistically will always be destructive.
Something how I wrote this blog triggered a lot of worry. Giving pain killers so that someone can sleep – one of our most basic needs – is not theoretically helpful – it is helpful.
I’ll try again! Please note that any drug which killed pain indiscriminately would ever make it to market because it would be too dangerous – so it’s not about that.
Nor is this about “killing pain indiscriminately”. It’s about fixing a brain pathology – healing a brain that is pathologically oriented to producing pain.