

A critical question at this juncture is to answer the question of whether CFS and fibromyalgia are the same or different illnesses. Benjamin Natelson
You want subsets? Benjamin Natelson wants to open up a big one. The longtime chronic fatigue syndrome (ME/CFS) and fibromyalgia (FM) researcher, neurologist and author believes fibromyalgia and ME/CFS don’t mix quite so well as many think. If fact, he believes the two diseases may be fundamentally different. If he’s right, throwing together people who have both ME/CFS and FM into an ME/CFS study is bollixing everything up. If he’s right, he’ll end up redefining both diseases and having a huge impact on ME/CFS and FM research efforts.
The symptoms in ME/CFS and FM are, of course, quite similar. In fact, the core symptoms – pain, fatigue, and sleep and cognitive problems – are dead ringers for each other. Natelson’s prior studies indicated that about a third of people with ME/CFS meet the criteria for FM.
Natelson’s studies of ME/CFS and ME/CFS plus FM patients have uncovered several differences between the two diseases. In contrast to people with ME/CFS and FM, people with ME/CFS only had altered neuropsychological dysfunction, a hyperactive brain serotonergic response, and displayed an abnormal response on a submaximal exercise test. PTSD was much less prevalent. They were also more likely to have had their illness triggered by a flu-like event and were more likely to have sleep apnea.
A 2018 study suggested that symptom similarity does not mean similar causes. Comparing balance issues in people with ME/CFS and people with ME/CFS plus FM, Natelson found significantly impaired vestibular (inner ear) functioning in the ME/CFS plus FM group but not in the ME/CFS only group. People with ME/CFS only also had problems with balance, but their vestibular functioning appeared to be intact. Instead, Natelson suggested that an as yet unknown problem with sensory integration or muscle weakness was throwing their balance off.
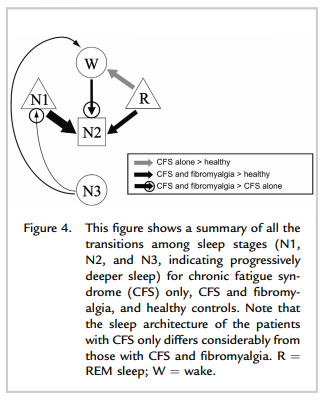
We all know sleep can be a big problem for people with either disease, but Natelson’s data suggests the sleep issues may be different. Using a new approach to assessing the transitions that occur during sleep (N1, N2 N3, Stage R), Natelson’s unpublished data suggests that people with ME/CFS plus FM are worse off.
People with ME/CFS plus FM are more likely to transition from slow wave or the deepest levels of sleep to what’s called N1 – the transition from sleep to wakefulness. This inability to maintain deeper levels of sleep produced what’s called “greater sleep pressure” or an increased need for sleep in this group. They compensated for this by having more transitions from wakefulness to the N2 stage.
The Rocking Bed Study
Now Natelson wants New Yorkers to help him get to the bottom of the possible ME/CFS and FM divide. In perhaps the most comfortable sleep study ever, he’s going to try to get those people with ME/CFS and FM some deep sleep – by rocking them in a cradle. Swiss sleep researchers devised something called a “rocking bed” which rocks back and forth like a baby cradle – sending healthy people to sleep more quickly and increasing the amount of time they spend in deep sleep. They believe interactions between the amygdala, hypothalamus and brainstem could be involved.
Natelson believes both people with ME/CFS and people with ME/CFS plus FM may benefit from being gently rocked to sleep, but the people with ME/CFS plus FM will benefit more.

Natelson’s early data suggests that people with ME/CFS plus FM have worse sleep than people with ME/CFS alone.
The requirements of this NIH-funded study are simple. (See the study here.) Be a woman between the ages of 28 and 60 without severe anxiety or depression, be off sleep meds for at least two weeks, have ME/CFS by itself or ME/CFS plus FM, and attend an evaluation and two 100-minute nap sessions at Mount Sinai’s Sleep Lab located near Union Square in New York City. Participants are paid for being in the study.
This R21 study is designed to provide pilot data for a larger grant. If Natelson sees differences in how the ME/CFS and the ME/CFS plus FM patients respond, he’ll immediately apply for a large RO1 grant which will allow him to expand the study greatly, including doing an overnight sleep study with all the bells and whistles applicable. He’ll also add fibromyalgia patients without ME/CFS.
Interested in being rocked to sleep to advance our understanding of ME/CFS and FM? If you’re in or can get to New York to take naps for two days, contact Benjamin Natelson at (212) 844-6665 or at info@painandfatigue.com. Please pass this study around on social media to get it done as quickly as possible.
(Rocking beds, can, by the way, be purchased or beds can be retrofitted so that they rock.)







Before leaping into the study, he should see if some who are dx with Fibromyalgia actually have SFPN—Oaklander has found about 40%.
I was dx with both, but now ME + SFPN. SFPN symptoms started a few months after ME.
Shelby, excuse my ignorance, but what is SFPN? TIA.
Small fiber polyneuropathy – or damage to the small nerve fibers in the skin and eyes (and perhaps more) that relay pain and sensory information to the brain. Found in both ME/CFS and FM.
I am seeing a neuromuscular specialist for this issue this month. Doctor will do EMG and hopefully order a biopsy.
Could you correct the contact phone number? There is a digit missing. Thanks.
Intriguing report. Thanks.
Thanks Cameron – fixed 🙂
I can’t make it to NY, but being rocked to sleep sounds absolutely wonderful.
I agree. I go on cruises once or twice a year. I don’t mind at all when the sea is rough because it is like being rocked to sleep.
I agree with can’t make it to NewYork. I really need a new bed, so could someone please just tell us where we can get this rocking bed? What does the bed look like?
Study is full.
I am long erm ,3 decades ill, and my sleep(patterns) together with many other symptoms changed so much as becoming 99% bedridden. the more ill, the more it changed. but research is allways good.
So we will once again come up with data relevant only to females.
Afraid so. The only light I can provide in that area is Nancy Klimas’s exercise studies for men which finished up last year. No studies published yet but it will be fascinating to see how they compare to women.
Cort and Steve, I don’t think the data will necessarily only be relevant to females. I think Natelson is very picky and tries to eliminate variables. I was rejected for participating in one of his studies in the past and understood that he is really careful about subsets and not muddying the data picture.
Hope so. I am beginning to think sex differences are very important due to different hormonal influences.
Well, for the past 70 years all medical studies were primarily male focused. I suppose it’s ok for this one to be different
I wonder if there is yet a 3rd subset. Those who have pre-existing FM and then get ME/CFS triggered by a virus superimposed over the top of the FM. I’ve had FM as long as I can remember, but had sudden onset of CFS symptoms following a virus. I’ve always felt the 2 disorders were fundamentally different. Before onset of CFS, I managed the FM beautifully with exercise. After onset of CFS, this all changed. I didn’t experience the 2 illnesses as being on the same spectrum at all.
I get the feeling from the article that his 2 groups consist of CFS alone, typically triggered by virus vs CFS mixed with FM, possibly one blurring into the other. I’m just suggesting there may be a 3rd group of people with distinct onset of the 2 very different disorders, and that this group may respond differently than those who have FM that evolves gradually into a CFS-like illness. Very interesting. So glad someone is looking at the differences. I think response to exercise alone should indicate fundamental differences between the two.
Fascinating. People with FM do seem to do better with exercise.
I wondered if the ME/CFS with FM group was actually an FM group misdiagnosed with ME/CFS.
I sent Natelson the link. I hope he checks out your idea 🙂
I don’t think so. I need exercise as it is the only way to lower the pain level but it quickly tires me. Two different beasts at war with each other I think
I know I have both FM and CFS since 1979. Exercise has always been exhausting and hard to breath. I was 33 yrs. old when i came down with this & in Nov. 2019 will be 74 yrs. old. Which makes it even harder. The brain can’t think right & the fatigue is so debilitating. With dizziness + vertigo. Getting out of bed every morning feeling drudged off balance & feeling your way just to go potty. Let alone adding the pain or headaches/migraine by then I wish God would have mercy and take me when I am really feeling sooo:( A lot of days just staying home but I make myself take my chihuahua to outside to potty, asking God to let me make my walk without falling. I have to look forward & to turn my head.
I hope Natelson can find the path to relief people with CFS and FM.This has had me for most of my life. This is not the way to living life.God Bless Everyone, including all the people doing the research…Danielle S.
I believe that I experienced the opposite situation in that my ME/CFS came on after a viral illness, then later I developed the Fibromyalgia which I suppose is the more common route. I was diagnosed with FM first, but it actually came on after ME. I found it much more difficult to express my ME/CFS symptoms verbally with my physicians, as I myself didn’t even understand fatigue as an actual symptom of illness. I only seemed able to mention all the other symptoms. I do need a new bed; who sells the ‘rocking bed’?
Interesting as my experience with onset of both diseases was the opposite. I had ME/CFS for 20 years and then developed FM. I believe the FM was brought on from a surgery I had to remove a benign tumor in my shoulder. (Just a guess.) The pain was much more severe and lasting than anything I experienced with my years with CFS. It took close to a year for a diagnosis and to get on Cymbalta, which was life changing. I also started experiencing migraines at the same time, which I never had with the CFS. They are somewhat under control with Botox and Topiramate but still very difficult to deal with.
“Those who have pre-existing FM and then get ME/CFS triggered by a virus superimposed over the top of the FM.”
This is what happened to me.
Amy, I agree. In my case, I was diagnosed with CFS first, after having Glandular Fever. However a few years later, I suffered a prolapsed disc in my back, and as I was rehabing that, I started to suffer from increased pain and was eventually diagnosed with FM. No-one has ever been able to answer my question as to whether I originally had FM which was diagnosed as CFS, whether the CFS turned into FM, or whether I have both illnesses. Due to the fact that many people with FM don’t have the dibilitating fatigue that we get with CFS, and many people with CFS don’t get all of the pain symptoms of FM, my thoughts have always been that I had two separate illnesses, triggered by different events, the CFS by a virus, and the FM by a physical trauma.
I’m really glad someone is looking at the differences too. It would be great to have an answer.
Amy, I had the same experience. I had pain for about 5 years, but was never diagnosed with FM. Then developed a virus and that was the beginning of the ME/CFS, which was diagnosed 3 years ago.
I am in the same group you are describing. Have had FM since I was a kid. Then after being in the ICU for 10 days with Covid I was diagnosed with long covid then one year later diagnosed with ME/CFS then POTS which actually may be POSH because I had earlier been diagnosed with hyperventilation syndrome at UC Davis Post Covid Clinic.
At 66 why wouldn’t my symptoms be as significant as a 60 year old? Don’t understand age limits in studies such as this.
Also do you know Cort if he’d be interested in seeing someone’s sleep study? I’m quite sure I have both CFS/Fibro and a couple years ago had 3 studies and was told I never get into deep sleep and O2 saturation was low. Seems he could learn from folks submitting any sleep studies they might have along with a symptom list and brief history. He’d get more info to work with – course I’m 66 so guess mine wouldn’t count anyway.
I don’t know why the age limit. I was age limited out of one study because thing they were studying started to physiologically change about five years earlier. Maybe sleep architecture changes around the age of sixty?
I think you are in the right track, Cort. Sleep architecture does change with age. I don’t think there’s a distinct cut-off at 60, but rather a continuum with less slow wave sleep and shorter sleep time with increasing age. He likely has to make a cut-off somewhere, depending on the study design.
Thanks VLynx. I suppose the same thing applied with the other cutoff – at 28!
Wonder where I can get a rocking bed??? Being rocked to sleep sounds wonderful.
I looked on the internet and rocking beds can be purchased or beds can be retrofitted so that they rock – https://rockingbed.com/
A hanging bed might be a more affordable option, there’s a youtube how to video here…
https://www.youtube.com/watch?v=aCZHQw-wJ_Y
I firmly believe ME and FM are two very different conditions. I developed fibro years before ME, and the latter was like being hit with a sledgehammer and caused me to no longer be able to work. I know know that fibro is not easy at all and not everyone with it is able to work, but some are. While in many both conditions are concurrent, not always, as we all know.
Gosh! 20 years ago I was telling people that I was considering inventing an adult electric cradle to rock me to sleep! Gentle rhythm, and the relief of weight on my muscles, and assisting circulation, so many benefits!
I’m amazed to find so many folks who seem to have my same sequence with first being diagnosed with fibro, then a couple of years later being slammed down with ME/CFS. I could continue working with fibro, but I was really disabled by ME/CFS.
I’m too old to be in Dr. Natelson’s study, but even if I weren’t, I wouldn’t be able to oblige, as my ability to nap went away when I came down with ME/CFS.
“My ability to nap went away” … yes, mine too. I have not had a nap for almost 20 years, no matter how tired I am. If I am feeling too awful to get through the day, I lie down for a while, but never get that drowsy feeling that was “normal” before I got ME. And never drift off. At night, I take sleep meds, and so usually sleep okay … but there is no residual effect by day. I miss being able to nap!
I have found the gentle rocking while sleeping on boat, therapeutic.
I have FMS, CFIDS/ME, & Narcolespy???!
Narcolepsy is an autoimmune disease. Could explain your symptoms of CFS.
I was diagnosed with CFS by Dr Richard Podel back in the early 1990s, when he first started helping CFS/ME patients and he accepted insurance. Can’t afford to see Dr Podell now that his a renowned CFS/ME expert, published author and saught after speaker on the subject — he no longer accepts insurance & fees are high. I’ve seen countless doctors over the years, including Infectectious Disease specialists, but no one in this NJ/NY area really understands CFS/ME like Podel & Dr Natelson. Dr Natelson has been studying this illness for many years while at Rutgers University. Thank goodness for pioneers like him! I’d love to get an updated diagnosis on my illness since my brain & body continue to change causing new symptoms to appear. Can anyone recommend a good Doctor in the NY/NJ area who accepts insurance?
Interesting Cort, thank you for the article.
I too, as Betsy, have had a sleep study and wonder if the results would be helpful to the good doctor?
Falling asleep is not an issue, staying asleep is a whole other matter.
I wonder how many people he can find that haven’t had depression with these diseases.
Natelson will do an evaluation at his office and decide about the depression. In our talk he mentioned SEVERE anxiety or depression. I’m not sure where the line is drawn but apparently there is one to be drawn.
Getting deeper into the sleep stages quickly as one falls asleep is pretty important from what I can tell. That’s one thing the bed appears to provide – a rapid and deep entry into sleep.
Natelson, by the way, recently published a study finding that should overturn any ideas that this disease is a form of depression or anxiety.
I have both CFS/M.E and Fibromyalgia. I was diagnosed with CFS/M.E first then 6 months later Fibromyalgia. I believe that the two are separate conditions.
I have tried many times over the years to exercise. Before becoming ill I visited the gym 3-4 times weekly. My pain consultant said that the only way to help Fibromyalgia is to – CBT, GRADED EXERCISE AND AMATRIPTYLINE! Maybe for Fibromyalgia patients and not for those of suffer both.
I know that being ‘rocked’ to sleep would set off vertigo.
I would like to know why is research is widely available in USA and not so much in the UK?
I would like to take part in research and studies of both CFS/M.E and Fibromyalgia.
The FM research is overflowing with exercise studies in FM. Although exercise studies suggest that impairments in exercise are present in FM, people with FM seem to do much better with exercise.
The USA is far and away the largest research funder in the world. The NIH’s budget is many times the budget of other federally funded efforts in other countries.
IDK, I have gritted my teeth with fibro pain to get through exercise for three decades. One can do it but it worsens the pain considerably, like any expenditure of energy or any movement for me.
I did that for decades too. I now wonder if it was worth it!
Interesting ideas, and thank you for reporting the story. I don’t think he’s going to get anyone with vestibular dysfunction into a rocking bed for more than two minutes, though – it would be horrific!! ? We’d need so much anti-sickness medication that we’d be knocked out for days anyway.
No one could ever pay me enough money to take a nap. I avoid them as much as I possibly can, because I feel absolutely horrid on waking, like a very bad hangover with extreme weakness. It takes hours for me to recover. Some days I am so drowsy I just can not stay awake – I feel drugged, like too much flexeril or some other anti-spasm medication.
I never had this problem until ME came along. I’ve never seen it described anywhere, but I assume there are other people who also have a bad reaction to daytime naps.
Another subset! It would be great to get you into a sleep study and see what happens. As I remember one part of the study is taking a nap.
Uggh. I had a sleep study, including the daytime nap tests, before I became near as sick as I am now. It was awful. I could hardly sleep with all the junk stuck to my head and face.
I was expected to more-or-less follow the clinic’s sleep schedule, which was basically to go to bed about 9 pm and get kicked out of bed at 6 am. I was allowed to “sleep in” only because of the daytime nap tests that followed the nighttime tests.
The results showed anomalies, but the physician had no idea what they might mean, so they were ignored. I figured out later that most sleep clinics are aimed at finding and treating sleep apnea. Pretty much anything else is beyond their competence.
jimmells – same here exactly! I’ve wanted an explanation for it so badly. I also have a very hard time coming out of anesthesia – it feels like exactly the same thing and it’s scary as heck. And waking up from a nap is exactly like waking up from anesthesia. It’s all bad. We must have trouble clearing sleep-related brain chemicals and/or something is messed up with sleep/wake homeostatis. Occasionally, this will happen with waking up in the morning, but it always happens with short sleeps – even ten minutes – and then it’s like being in a frightening non functional other worldly semi-coma for many many hours. I avoid naps like the plague, but of course, sometimes they’re involuntary.
Yes jimells and Tamara, I too feel terrible if I sleep in the day – unless I absolutely have to. It can depend on why I need to sleep.
When I was eating food I was intolerant to, such as dairy, I would fall into a sort of drugged sweaty sleep. If I ate too much fructose it was like having an anaesthetic – I could lie totally motionless for hours – until I was in pain. My breathing would be suppressed and become very slow, so that I actually had to consciously breath in and out, otherwise I didn’t breath.
I had a horrible experience in the last few years, where I’d slept for a few hours or so in the day and then felt like part of my brain hadn’t woken up. So I’ve been focussing on trying to settle my Circadian rythmn – getting up, going to bed and eating at the same time.
Actually the fructose seemed to heavily sedate me, so I wouldn’t go to sleep but I would have to lie down and would then remain completely still for hours at a time.
Also thinking about this sleep issue, I’ve always had a problem with having a lie in – just didn’t work for me – I’d feel horrible for the rest of the day. I was/am much better if I got up and got going.
For me there are unknown variables, meaning that sometimes I might benefit from a nap and other times I wouldn’t. It’s a matter of me trying to guage what’s going on and what I need. Like the food – shall I eat something or not and if I’m going to eat something what should that be? So many questions for a sluggish brain…
I’m over 30 years in with CFS/ME &FM and I avoid naps like the plague no matter how exhausted I am. Same effect from naps. Also it’s my attempt at a better night sleep, which doesn’t really help much. Just gotta laugh!??
Exactly the same with me!
I avoid naps for the same reason. I wake up feeling like I do every morning which is torture in itself. I have begun sitting up to sleep, otherwise I can’t wake up. I can hear people, but can’t physically move sometimes for more than a day and when I do get up my whole body feels knotted up, my face and eyes are swollen and my throat is so congested I can hardly breathe. I hate going to sleep at night just knowing I have to wake up! 2 of my doctors have mentioned sleep paralysis which I had already figured out from Google and are saying it’s related to Narcolepsy.
I have FM & CFS. I haven’t seen anyone else post just these 2. Am I the only 1??? I also have several other medical conditions.
I don’t nap during the day no matter how tired I am for the same reason
One of the best sleeps I have ever had was in a hammock (during the day), and after reading a Spanish study about rocking and sleep several years ago, I seriously contemplated hanging one in my bedroom. I have started going to bed at 9pm because the sleep one gets before midnight is twice as restorative as the hours after midnight.
“the sleep one gets before midnight is twice as restorative as the hours after midnight.” Do you have a study on that, Sarah, never heard it before.
Emails to Dr Natelson’s website not going through.
I’m in UK, have ME and FM. Onset was flu like virus. Don’t hit deep levels so permanently jumpy unless on 7.5mg Zopiclone which our NHS is now taking away as we’ve all been deemed as potential abusers. PJ parties? Haha. Nightmare!
But interestingly I had right vestibular hypofunction from day one so seem to fit his take on it. Any idea when results likely to be in? Looking forward to that
I’ve found that slight rocking (regular bed) back and forth, arms hugging myself, has helped distract me from pain and even sometimes helps me get to sleep. I think it harkens back to when I was a young child in a chaotic home, constantly rocking (while sucking my thumb!). I even rocked myself in the back seat of the car, which irritated my father to no end.
I have both and Fibro onset years before ME/CFS from mono. Definitely different.
The last year I’ve been taking CBD oil before sleep and I’v had the best sleep since I got sick with CFS/ME 42 years ago.
Great to hear Mary. CBD oil helps me with sleep as well.
Would you be willing to add your experience to Health Rising’s Cannabis Review program for fibromyalgia and ME/CFS?
https://www.healthrising.org/treating-chronic-fatigue-syndrome/drugs/cannabis-fibromyalgia/cannabis-fibromyalgia-chronic-fatigue-entry-form/
We have a blog coming out on helping with sleep.
I’ve been taking CBD oil before sleep and I’ve been having the best sleep since I got CFS/ME 42 years ago. Also, I take three capsules of magnesium L threonate at bedtime.
Hi Mary Jo,
I’m constantly searching for sleep aids and I’m curious about the Mag L-threonate. How does it compare to Mag bisglycinate? Is it easy to digest? (I usually get gastro sided effects from Mag supplements.) What dose do three pills add up to?
Thanks
I didn’t personally notice any difference between the two, so I use bisglycinate as it’s cheaper. However, threaonate is meant to cross the blood brain barrier more easily.
@Sarah, I actually did install a hammock in my bedroom decades ago! It was one of those huge woven Guatemalan ones where you lay crosswise rather than the fabric ones (like the kind people use in their yards) where you lay lengthwise.
I had an additional cord tethered on another spot on the wall so I could pull it to rock myself.
I got fairly good sleep excepting that it didn’t provide the kind of back support I favor. I also change positions a lot and moving on that kind of a hammock is like trying to roll over in a half filled waterbed!
I remember Cort’s ‘bed of nails’ article to help those with fibromyalgia pain. Humm, a rocking, bed of nails? 😉
Dear Cort,
Thanks again for another cathartic article!
I have moderate-severe ME/CFS, and I’ve long been frustrated by its conflation with FM. Bottom line is that people with FM only, and doctors who have only treated such patients, seldom understand the depth of our post-exertional malaise. In my experience, they tend to assume that light, low-impact exercise will almost certainly result in net gain. They don’t fully appreciate just how big a risk it is for us, in spite of our sophisticated pacing strategies.
I’ve stopped seeing many doctors for this very reason, even CFS friendly ones. One popular FM doctor just couldn’t understand my apprehension about pain treatments. He had no concept of needing to feel my body’s PEM signals. I also stopped attending a support group that consisted of majority FM sufferers. Though I certainly benefited from their fellowship, there was just too much emphasis on getting out and moving around even when you don’t feel like it. For me, on most days, that’s harmful advice.
This is not an argument for one condition being “worse” than the other. It’s just that I think the differences in symptoms alone is enough to treat them differently, apart from questions about differences in cause.
David I hear you on the PEM. As I have both CFS and FM, I have to walk a fine line between moving for the FM, and pacing for the CFS, or I end up bed ridden. I’ve found that as long as I don’t let my heart rate get too high while I’m exercising I can limit the PEM effect, so cardio is definitely limited for me. Years ago the Dr I was seeing sent me to an Exercise Physiologist. Unfortunately, that was when the whole graded exercise regime was “the thing”. Despite me telling him that if I pushed myself I’d end up in bed, he insisted on this regime and, guess what… I ended up in bed. I’ve learned to just listen to my body since then, bought a heap of books and DVDs on exercise and biology, and just do my own thing.
Yes, there seems to be a rather dramatic difference in the ability to tolerate exercise. FM patients are certainly not exercise bunnies but they tolerate it far better. The same is true for POTS by the way. People with POTS aren’t running marathons either but they do far better with exercise than people with ME/CFS. The PEM part really does seem to be what separates ME/CFS from other diseases.
We really need to get FM and POTS patients in some two-day exercise studies!
Being rocked to sleep sounds PUKE-FUL!!! I get motion sickness so bad that I cannot lay in a hammock and could barely sleep in the waterbed I had in college! Ughhhhhhhhhhhh
For a few years, I had been complaining to my general practitioner about periods of deep, deep fatigue, accompanied by bouts of fever. These bouts became longer and more frequent, to the point that it became a permanent state. My MD sent me to a rheumatologist working in a major teaching hospital, who officially diagnosed CFS AND FM.
I don’t suffer from FM. I know of people who experience that excruciating kind of pain and I don’t. To this doctor, CFS was a synonym for FM. Said rheumatologist absolutely wanted me to fit in his statistics and wrote false information in my file about my supposedly painful reactions to his digging his fingers in the pressure points. He gave me a prescription for Ritalin and Naproxen, to be renewed by my regular family doctor, and told me that he couldn’t do anything else for me. I sat in the hospital’s parking lot and cried for a long time. That was in 2003.
In 2012, I had to consult another specialist at the same hospital, for a totally unrelated condition, namely, cancer. He insisted that I suffered from FM. “No, doctor, I suffer from Chronic Fatigue Syndrome. I don’t have fibromyalgia.” He rolled his eyes as if I were a total nitwit. You know what? I decided that I would find an other oncologist, in an other hospital. I’m still around to talk about it, so I guess I received great treatment!!
This is why I’m very happy that some participants at the Montreal conference think that rheumatology is not the proper field of expertise for ME.
Good for you Genevieve, to have enough self belief to find another doctor!
So much power just isn’t handled very well by many doctors.
If I talk to people about whether a counsellor/psychotherapist might suit them, (I have a degree in counselling/psychotherapy) I say see how you feel afterwards?
Like having a haircut, some hairdresser’s/barbers will suit you and your hair and some won’t. People are sometimes intimidated by therapists and I believe that they should make a real choice as to who they see.
Health professionals can have a great deal of power over us and have an unfortunate propensity for patronising attitudes. For much of my life I was lucky enough to be able to avoid them.
My current strategy is to only approach them for what they can provide, when I absolutely have to.
And probably not the right field for fibromyalgia either! I wouldn’t be surprised if at some point FM is moved to neurology.
A cautionary tale from a former patient: When I first saw Dr. Natelson, he showed more interest in past sexual trauma than my medical history. I hadn’t experienced the trauma he was looking for, so he fabricated it. Imagine my surprise when I found it in my medical record more than two years later! He also hooked me up to a breathing monitor and insisted I wear it for the duration of every appointment. This made me very nervous, so he diagnosed me with—ta da!— anxiety hyperventilation! Eventually he prescribed Xyrem, which I could not get covered as I am not a narcolepsy patient (turns out he knew this, but whatever). It didn’t help that he couldn’t remember me from one appointment to the next. Over the year I spent in his care, I paid hundreds for each appointment, in addition to co-pays, as he collected from my insurance provider as well. A few years after leaving his practice, I started getting solicitations for donations to his Pain & Fatigue Study Center. I could go on, but you get the idea. All in all, a demoralizing experience, and a deeply discouraging setback at a time when I was new to this disease, VERY sick and frightened, and not well-equipped to question the authority of someone I took to be an expert. I learned about Natelson on this site.
I started out with FM and later developed CFS. The straw that broke the camel’s back was a mild shoulder injury. I had a sleep study many years ago and had this exact sleep pattern, sleep doctor shrugged. Went to the sleep neurologist, he said my sleep architecture was fine and they only deal with architecture issues.
Well, for the past two years I have been slowly recovering due to a new physical therapist. I have gone from mostly housebound to a 10 hour/week job. While trying to figure out what was wrong with me, she performed very similar treatments to Dr. Perrin. I only discovered him and his book a few weeks ago. His list of symptoms and theory about the posture messing up the autonomic nervous system and then causing the toxins to drain slowly does explain me and the treatments that have helped me greatly before.
About a week into rifaximin for SIBO I went from sleeping 16 hours a day to 8 hours a day, my brain fog completely went away and I was basically cured, temporarily. I have adhesions, so the SIBO, and therefore the CFS kept coming back despite multiple courses of rifaximin. I didn’t really want to just take that for life due to c. diff and other risks. The other “treatment” where I was about 80% cured was trying a new place to avoid some sort of chemical sensitivity or mold, but I didn’t have the funds to continue living there. I would guess for me at least the sleep issues that Dr. Natelson describes come from excess toxins for me.
Wow. What a great result from treating the SIBO. It’s one of the first things Dr. Chheda focuses on in ME/CFS.
Very interesting Joy. I’ve had ME/CFS and secondary FM for 24 years. I’ve been treated by top CFS docs. I recently had to change doctors because the medical board is railroading her. I’ve since been dxd with severe mold toxicity. An OAT test showed high levels of clostridia (opportunist infection) as a result of being colonized with mold. In September I went on a mold sabbatical and did feel temporarily better. Have you done a Great Plains Mycotoxin Test provoked with glutathione? Have you tested your home for mold?
Just had consult for brain study. Dr firs only televists. His reviews are not very good