

It’s the simplest of medical tests. The erythrocyte sedimentation rate (ESR or SED rate) test simply measures the rate at which the red blood cells in whole blood descend in a test tube over a period of one hour.
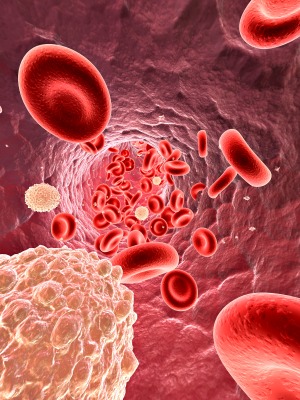
This non-specific measure of inflammation works because, during an inflammatory process, fibrinogen levels increase – causing red blood cells to stick to each other. When that happens, they form stacks called rouleaux which, being heavier, settle faster. So if an inflammatory process is going on you may very well have high ESR levels.
Healthline provides these criteria for ESR rates:
- Women under age 50 should have an ESR between 0 and 20 mm/hr.
- Men under age 50 should have an ESR between 0 and 15 mm/hr.
- Women over age 50 should have an ESR between 0 and 30 mm/hr.
- Men over age 50 should have an ESR between 0 and 20 mm/hr.
- Children should have an ESR between 0 and 10 mm/hr.
The Clumpers
Infection is the most common cause of an increased ESR rate, but moderately raised ESR rates are associated with many other conditions including pregnancy, anemia, inflammation, cancer, diabetes, heart disease and collagen vascular diseases. Very high ESR or SED rates can be found in kidney disease, cancer and collagen vascular diseases. ESR rates are often used to assess the effectiveness of anti-inflammatory or anti-pathogen therapies in people with higher ESR rates.
The Sliders
Low ESR rates, on the other hand, are mostly ignored. In fact, most labs don’t have a cutoff for a low SED rate: everything down to zero is considered normal.
Some diseases, though, (congestive heart failure, hypofibrinogenemia (low fibrinogen levels) low plasma protein in liver or kidney disease, leukocytosis (high white blood cell counts), polycythemia vera (excess red blood cells), and sickle cell anemia) are characterized by their very low ESR rates.
As an infectious disease doctor, Dr. Bela Chheda had run hundreds, probably thousands of ESR or sedimentation rate (SED) tests prior to working on ME/CFS. She ordinarily encountered increased sedimentation rates in her patients with infections, but then came ME/CFS – a disease triggered by infection which many people assume is inflammatory in nature. (ESR tests, it should be noted, do not pick up all kinds of inflammation.) The ESR or SED rates in many of her patients, though, were not just low but bottom of the barrel low (usually 2). (She thought the reason she didn’t see even lower numbers was that the test probably wasn’t sensitive enough.)
In fact, so many people with ME/CFS had very low sedimentation rates that she began to think of it as a kind of non-specific biomarker and wondered if something different might be going on in her patients with normal or higher ESR rates.
A 2011 update by Consultant360 came to the same conclusion:
Laboratory studies. These tests can be used to exclude other diseases associated with fatigue. The most consistent laboratory abnormality in patients with CFS is an extremely low erythrocyte sedimentation rate (ESR), which approaches zero. Typically, patients with CFS have an ESR of 0 to 3 mm/h. A normal ESR or one that is in the upper reference range suggests another diagnosis.
Chheda’s anecdotal reports appeared to jive with Ron Davis’s finding of reduced SED rates in his Stanford red blood cell deformability study.
For myself, I have long wondered about SED rates as it was the only consistently abnormal (or low) test result I had in a series of tests in the 1980’s. My ESR or SED rate test results have been amazingly consistent over the past three decades – always a 2. That, I thought, must mean something.
But then came, surprise, surprise, a very large British Biobank study which found normal ESR rates (median=5) in more severely ill patients and slightly increased ESR rates (median=7) in less severely ill patients.
Another seemingly consistent finding in ME/CFS went to pot! Not able to explain the differences that are showing up and still hanging on to my consistently low SED rates (they must mean something), here’s a poll with a twist to add a another slice to the data. Using Dr. Natelson’s supposition that people with ME/CFS differ from people with ME/CFS and FM, the poll will be divided up into three categories:
- people with ME/CFS only
- people with ME/CFS and FM
- people with FM only
We’ll see what we’ll see! It should be noted that ESR is too non-specific a test to be a biomarker, but low or high ESR rates could play a role in a diagnostic algorithm; i.e. a subset of patients could be characterized by low SED rate plus another finding or two. Perhaps an algorithm like that could come out of Solve ME’s international patient registry.
Please take the poll!






My ESR has also consistently been 2 every time I have been tested – so that’s going back as far as 2011 that I have records of. I also have high MCV and always assumed the two were related and tied to B12 issues?
Very low see rate is one of the parameters Dr. S. Bell mentioned in his book The doctor’s guide to chronic fatigue syndrome, in 1991.
It’s good that it is being mentioned again as it’s a simple analysis. Thanks
I haven’t gotten the diagnosis just yet but just did my sed test and my value was 2, my Dr said if he could show me a diagram of CFS my name would be at the top, I have been trying to figure out why I feel so sick and have times when I can’t get off my couch, the lightheadeness with this sucks, I hate this but am sure I will be getting my diagnosis real soon, he said he was pretty confident in diagnosing me next visit, wish there was natural ways to treat this it’s horrible
I will ask my Dr to have this test done! Thanks Cort.
Maybe there is a correction to be made here?:
‘here’s a poll with a twist add a another slice to the data.’
A little later there is a ) without a ( to close off the parentheses…
Keep up the good work, you’re contribution is very important.
THANK YOU!
Zopa
Thanks Zopa!
Hi Cort, this is great news but tell us, is this a test that is normally run or one that we have to request and we have to pay 100% of the cost. Any idea approx. what that kind of test would cost? I’m 80 now and my resources are very, very slim (can no longer see my CFS/FM specialist any more.
Don’t you think you should have added an age range to the poll?
I went looking for past ESRs and I could only find 2–both normal–for my age. As I contemplate this theory, and my other co-morbidities (many), I do wonder if you have some sort of idea about type of onset and course of disease and how it might correlate with the SED rates for ME/CFSers. Fun poll, but missing a lot of helpful information…
For the record, I’m now 67, I have Ehlers-Danlos, and relapsing iron anemia (unknown cause)–among other things. My ME/CFS onset was likely viral, and I have struggled with it for decades.
On the other hand, my normal body temperature is on the low side, 97 or so. Maybe that’s a clue too…
I was mainly concerned about the lower end of the scale but it would have been nice (and more accurate) to added an age range (and gender) but that would have required many more polls so I added a section from 20-30 that I hoped would fit women over 50.
Over the past 15 years mine is usually around 5 but it did go up to 20 in 2008 but my GP didn’t comment or inform me so I wasn’t aware. Its only now that I have online access to my blood test results that I found this out.
Will be interesting to see the results.
BTW I am 71 years old and been unwell since 1979.
My sed rate is 2, but it goes up to 10 when I’m flaring and feel like I’m dying.
Interesting! Some inflammation there that must be contributing to your flare. Yet you have ME/CFS without any sign of inflammation – at least as far as the SED rate test shows – which is not definitive for inflammation; i.e. it doesn’t always catch it.
Sounds like flare up of auto-immune disease as well.
I’m not sure if my entries worked. I tried to do it for three of us (first myself, then each of my kids), refreshing the page between each submission. We all have been diagnosed with ME/CFS. I and my oldest were 0-2, my youngest was 3-5. Although, when my oldest was at his worst, it was 0. When he was doing some better, over a year later, it was 5. I only entered his lowest score.
Thanks = it was very interesting, was it not, that the more severely ill patients in the English study had lower ESR levels than the more moderately ill patients. Maybe a bit higher is better than very low.
When i was moderately ill, my ESR was 0 for years. When I became the most severe pt we’d ever heard of (100% paralyzed, mute, locked-in), it went up. Now, 20 years later, I’m 99% bedbound (with a perfect for my age ) sed rate of 15. There’s always a monkey wrench!
Mine was always 0. but has steady gone up to 6 as I have developed rheumatic issues
I have been Dx with fibromyalgia. My ESR was 8 and then dropped to 3 over a 2 yr period. Last test I have info on was 3 years ago.
My ESR was 1 for a long time, but in recent years it has been 5. It might be that something else is now going on, or just that I’m getting older.
I have noticed that for decades, my ESR has varied between 0 and 6. Overall, it is a leading indicator of my overall health, and it is the best single indicator of my health that I know of. When it’s between 0 and 2, my health has been at its worst. It’s been 2 for the last few years. However, my most recent test showed it at 6, which seems to be the ideal value for me. Sure enough, my health has been improving recently.
It’s been my impression that there are many different subsets of ME/CFS. I think some of these subsets are connected with fluctuation in the ESR while others aren’t, which would explain the different study results.
My SED rate was 7 in 2016 when I had been fighting off Anaplasmosis/ Lyme for 6 months. After being diagnosed with Fibro/CFS in March 2018 my SED was <1, the same on 4/19. I am no longer showing symptoms of FM/CFS so will try and get another SED done soon to see if it has changed.
Congratulations on getting better. The test seems to work! Your ESR levels went up when you were fighting off an infection and they plummeted when you were not. Note that even though they went up and even though you were fighting an infection they didn’t go above normal! Then they went to almost zero – that suggests to me two things:
A) you may have had a truncated ESR response
B) I wonder if some people with ESR’s in the normal range are fighting an infection which is artificially boosting their ESR’s?
I’ve been unsuccessfully fighting a cold for nine months and my recent ESR results came back with a 2 though.
Per Dr Marty Ross “CRP & SED rate are normal in people in the middle of severe flares! Increased in arthritis and other infections but NOT Lyme!” Check his info on fighting viruses on his website, treatlyme.net. Following his protocol for 6 months is what seems to have knocked my viruses down and contributed to my CFS/FM symptoms disappearing. That and adding essential amino acids and switching from Benfotiamine to thiame and adding 200mg of riboflavin. Your article on thiamine deficiency disease started me on that path. Thank you!
It’s so interesting. ESR levels can also be low because of high levels of white or red blood cells (leukocytosis (high white blood cell counts), polycythemia vera (excess red blood cells). Sometimes my white blood cells are high. High white blood cell counts often result from infection or inflammation yet my ESR levels are consistently very low – which suggests to me that some kind of inflammation not associated with ESR may be involved.
Cort, Have you been tested for Hypofibrinogenemia? This may well be a congenital or acquired thing for the people with consistently low ESR levels. Knowing this might be a life-saver down the road for some, as illustrated below by the case with the woman with temporal arteritis.
The other thing I wanted to mention was parasites. Trichinosis can cause a low SED rate. Would other parasites have the same effect? There is dreadfully little info available. I cannot read the following article but the title alone is enough to evoke: “Low Sedimentation Rate, Hypofibrinogenemia and Restrictive Pseudo-Obstructive Pulmonary Disease Associated with Trichinosis” April 14, 1960. https://www.nejm.org/doi/full/10.1056/NEJM196004142621505
So are we “sliders” defective, not producing normal amounts? Or are we producing but showing low levels because: “Fibrin binds to the target bacteria and wraps them into a clot, killing the bacteria inside the clot.112
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4856808/#bib111
Sorry my link was wrong.
The quote was from this article:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4856808
Which referenced [112] this one:
https://www.ncbi.nlm.nih.gov/pubmed/23467586
I’ve never even heard of that before and I didn’t know that low SED’s can be caused by parasites. I will check both out -thanks!
Makes perfect sense to me, Cort. This article made me go back and check the ESR tests I had in the year after my disabling ME/CFS relapse. Rates were 2. Other inflammatory markers were normal.
At the same time, NSAIDs have always provided short-term relief not only of pain but also of fatigue and even cognitive issues. (They do not prevent PEM though.)
So some kind of inflammatory process must be contributing. But standard diagnostic tests don’t pick it up. Hence the confusion of rheumatologists.
ESR is also low in sickle cell anaemia, where rbcs are misshapen. There was info recently that they are deformed in ME also.Could this cause low ESR? I wonder if hydroxyurea would help?
Mine is always 2 or 3
Yes problems with the rbc’s can cause low SED rates. Ron Davis was not finding problems with rbc shapes but with the ability of the rbc’s to deform properly. He also found high rates of oxidative stress. The latest news though from the Symposium suggested that the deformability problems might not be working out. They said they were digging deeper.
I have fibromyalgia since 1998 – mine has gone from 25 to 14 to 6 over the last 3 years. Many years ago, in the first few years after my diagnosis, I remember it was high, over 50
Did you have an infectious onset do you remember? That was a quite high ESR level.
No, my onset was after the birth of my son.
My mom has fibromyalgia and her ESR is always low. She developed temporal arteritis, which was nearly missed because it almost always is associated with a very high ESR level. Since the sed rate was so low, her first rheumatologist didn’t believe it could be temporal arteritis. Her ophthalmologist is certain she had it, though, as she had all the classic symptoms, and even has damage to her optic nerve as a result. She could have lost her vision if she hadn’t been treated appropriately. This issue has important implications for those of us with chronically low ESR levels. CRP values need to be relied upon as measures of inflammation in situations like ours. I assume those levels aren’t impacted by ME/CFS/fibro.
Amy, What was the treatment for your mom’s temporal arteritis?
I had thought that CRP levels are not effected in ME/CFS but a recent review suggest they are higher. I think mine have been relatively normal
https://www.ncbi.nlm.nih.gov/pubmed/31465778
ESR & CRP is 150 -200+
A lot of inflammation going on there Sonia! What do your doctors say. That would call for more investigation I would think.
Five years ago I had a live cell analysis via dark field microscopy. It was enlightening! On the screen were the movements and meanderings of all kinds of stuff in a bit of my blood. It was amazing to see the many rouleaux, the rolls and stacks of RBC on their sides…So much like rolls of coins! There were few RBC moving individually. But so, so many of my RBC were sticking together edge to edge. When they are stacked and clumped, the RBC ability to deliver Oxygen to the cells is limited. More rouleaux and clumps are bad! Individual cells can deliver more O2. On the rating scale of 1 to 5(bad), I hit the jackpot, 5 for rouleaux, 4 for clumping and 4 for spicules (fibrinogen].
Over the next 6 months those numbers improved, and I was also feeling better. Unfortunately, the technician retired after my third visit. Two years later, I was tested by another technician. My numbers were still ok, but uric acid was a problem. This guy was trying too hard to sell supplements, so I never went back.
Yes, I know dark field microscopy is considered by many to be ‘junk science’. But blood tests were also ‘junk science’ eons ago. Twenty things were evaluated, including RBC shape. Some had parasites, some aging, some ravaged by free radicals, fungi, protein from leaky gut, others damaged by dehydration.
Eating better, drinking more water, being more active, adding digestive enzymes, more veggies helped. As the rouleaux and clumping decreased and my FM and CFS improved.
This past month was the first visit to a new Dr. Believing that tests are more accurate than in 1984 and 1994, I requested that he start at square 1 and retest. He missed the sed rate, will request it at next appointment…
I was diagnosed with fibromyalgia 10 years ago, symptoms already for more than 25 years (now 73 y)
Three years ago I had also a living blood examination by dark field microscopy.
It showed a high number of red blood cells en rouleaux and a lot of fibrine strands. My ESR was always around 30.After taking a mix of enzymes; (nattokinase etc) my blood looked normal after 6 months and my ESR dropped to 7.
The muscle pain didn’t change much but my shortness of breath after climbing stairs was much better.
Nah, dark field shows so much. Science just doesn’t know how to look at it in general. And I don’t think they really want to because it was popular in alternative medicine for a while.
But I think if it were studied more, I think it could be useful, especially in patients like us.
I, too, seen rouleaux improved by proteolytic enzymes. And it is just simple science. I once owned microscope with a dark field condenser. Everything is very interesting and detailed under dark field. Many things seen in dark field simply can’t be visualized in bright field, unless you use stains and other things.
I hope something interesting will come out of the research on this. My CFS doctor commented years ago to me that it was common for her CFS patients to have low sed rates. A doctor with a different specialty later commented on my low sed rate (mine has consistently been 2 also) but out of curiosity – I don’t recall what specialty she was and don’t know whether she ever took it anywhere.
I’m unable to participate in this poll because it can’t cover my experience adequately. This is how my ESR has been during the last nearly 20 years:
Pre-ME but still not well
2001 1
2004 1
On-set of ME still working until 2009
2006 1
2007 1
2007 2
Disabled by ME and onset of MCS
2009 8
2010 2
Housebound by ME and MCS
2011 5
2012 5
I may have had ESR tested since 2012 but I don’t have copies of the results. I also had a diagnosis of FM but I don’t have FM symptoms if I avoid MCAS/MCS triggers.
Should there be a category of ME/CFS or/and Fibro plus other comorbid diseases. Comorbid diseases could be the cause of inflammation rather than ME/CFS or Fibro in the SED rates.
The first blood abnormality in the 1985 Lake Tahoe Mystery Illness shows
up as being important… after all.
https://www.survivingmold.com/community/erik-johnson
Back in the late 90’s when I was having very painful FM flares, my ESR was 1. My last ESR was back in 2017 and was 10. Due to my continual trigger point therapy, I don’t have very painful flares any more though I am still extremely dysfunctional. Maybe the pain severity affects the ESR.
My ESR is always between 30 and 52. I am a woman and 60 years old.
I practically never have infections and the beginning of my CFS was probably extreme emotional stress. I believe ma mother had it too.
For the last year I have been taking about 550 mg daily of an antiflammatory (naproxen) and I am feeling very well. Not back to my old self, but with pacing, lots of salt, I manage very well. My GP sent me to a first rhumatologist who said I had nothing and refered me to a psychiatrist. My GP sent me to another one who said , gently , that I did not “belong” to the rheumatoid world. Why the anti inflammatory is working so well… I do not know. I tried half dose but I slowly regressed.
I am a psychiatrist and have been in practice for 30 years. I have found that my patients in which I suspect they have CFS/Fibromyalgia almost universally have very low ESR’s, such as 5 or less. For years I have noticed this trend and even considered it a unique finding to that group of patients. I am not a researcher, but I felt that had to be something to it. I am glad researchers are now paying attention to this odd phenomenon. Thank you.
Dr Peterson tested me four times. Twice the number was two and twice my number was three. However I was recently tested after having not been tested for two years my number was 55 which is considered high. I was actually quite surprised however since my illness has morphed into auto immunity obvious by a Cervical spinal cord lesion and I am now being treated with Remicade I thought perhaps that was the reason it had changed. Funny you wrote about this though because I was just thinking about it.
I do not know what my current, or past, SED rates were. However, I do know they were never elevated. I am due for a blood test and will request SED rate be included.
What I’m wondering is if this finding is related to the “never catch a cold or flu” phenomenon found in some of us.
I am one of those who never (1x in 40 years) seem to catch a cold or flu. Recently a very bad cold has been going around my community and I have experienced increased ME symptoms – the strange, irresistible semi-sleep, mini-coma-like hypersomnolence in the daytime, incapacitating fatigue, and aching, but no traditional cold symptoms. It seems to be abating now in a timeline very similar to the length of a bad cold.
Could it be that we do not experience these routine cold symptoms — runny nose, sneezing, coughing — because they are an inflammatory response which we cannot mount?
Further, I experienced more than a decade of repeated serious bladder infections, following ME onset, which never produced the usual burning in the urethra that would ordinarily result from inflammation. It was very difficult to explain to a new doctor that my request for urinalysis was warranted when I did not have burning, but it always was.
I wonder how Sed rates might change as ME progresses.
My ESR test history is incomplete, but the general pattern seems to be that it is lowest after initial onset and relapses, but closer to mid-range years later, even though symptom severity and disability remains unchanged.
Just had my ESR checked and it was 1. When I was first diagnosed 33 years ago it was 4. It’s always come back on the low normal side.
Most of my lab tests come back “normal.” Exceptions: C4a (very high) and tests that were part of a coagulation panel which showed a hypercoagulation state (prothrombin fragment 1+2 was 422 (H), fibrinogen activity 140 (L), T/AT complexes 5.9 (H). The interpretation of this by a researcher was that my fibrinogen was low because it was being “used up” in a process that was walling off a pathogen. This researcher and a gynecologist were studying women who had frequent miscarriages that they suspected were having coagulation problems. When the coagulation issues were treated, the miscarriages stopped.
Has anyone else had these tests done, and if so, do you know if these tests are meaningful to those of us with ME/CFS/FM? A local hematologist told me she has never seen these tests before and doesn’t know how to interpret them.
I tried Lovenox injections for a short while but couldn’t handle the pain of the injections which I had to give to myself. I tried nattokinase for a while but discontinued it because of not knowing how much to use, safety concerns, etc.
I think many had these very tests done in the past, and coagulation issues are definitely a problem in ME/CFS.
Dr. David Berg’s (Hemex) lab tested this, but it was acquired by LabCorp some years ago. He called this coagulation abnormality ISAC (Immune System Activation of Coagulation). I believe he named it this because there currently isn’t a more suitable name in medicine for the phenomenon.
It just happens that these researchers tested for many of the markers that were in the ISAC panel. And I believe these disorders of coagulation could be behind the low sed rates.
David Berg of Hemex is really someone the OMF and Simmaron Research should be contacting. The low sed rate phenomenon has been ignored for far too long!
JD, You are correct, my test was the ISAC, done through Hemex lab and David Berg. It was done 10 years ago and I’ve never been able to convince any medical professional since then that this might be a cause of my ME/CFS/FM. How do we reach out to the OMF? It seems like there would have to be a lot of patients (a subset) with these findings in order for them to take at look at this.
I have MECFS. My SED rate two months ago was 19; last year during a bad flare it was over 70, with no other abnormal results (CRP, autoimmune markers, etc.). I feel like I’m in a mild flare so I wonder if 19 is higher than my “normal”; I’m going to look at previous tests to see.
No doc has ever mentioned this test to me. I’ve had ME/CFS with fibro for 20 years. Closest I ever got was an expensive analysis of live blood by a naturopath. She showed me the slide of my magnified blood: lots of clumping, and many strangely misshapen red blood cells. The research at the time seemed to confirm that people with CFS had a high proportion of misshapen cells, making it harder for them to circulate and thus carry O2 and nutrients etc. to all cells of the body. Maybe newer research has been done on this?
Other physicians, including Dr. Alan Pocinki (Washington DC/ Bethesda, Maryland) have long recognized the low SED rate correlation to ME/CFS. Pocinki saw this pattern at least 25 years ago and it appeared fairly consistent with other ME symptoms.
My first test came in at 2, 25 years ago. Next tests sat at 3, except for one brief period where I hit a high of 17 and actually felt a bit better.
The first time I had the test done — about 10 years in to CFS — it was over 50. Two years later, at a time when my symptoms were better, it was down to 15.
This is interesting. I have both CFS and FM. I’m seeing my doctor on Wednesday, so I’ll see if I can have this test done and complete the survey. Unfortunately, all my previous tests are still packed in boxes, and I’ve changed doctors, so I don’t know if I’ve had this test done before.
Looking forward to hearing how it came out. 🙂
Okay, so just called my previous doctor, and I had an ESR test in Jan 2018 which was 2. Apparently a previous test in 2010 was also under 5. I have CFS and FM.
I had no idea what ESR was only that mine is high at 40.
I’m 44f, I’m also borderline diabetic so the ESR might be reflecting that actually. I also am homozygous for MTHFR gene (I think that’s how you say that? I have two copies of it).
I really wish someone would research this. For over 20 years, my SED rate has never been higher than 4 or 5 and is usually 0-2. CRP is always normal, too. I was diagnosed with fibromyalgia, then discoid lupus. Then told I probably have systemic lupus then Sjogren’s The latest of 5 or 6 Rheumatologists settled on a diagnosis of undifferentiated connective tissue disease. I’ve been prescribed acyclovir since 2003 to manage recurring ’mild’ viral (hsv2) meningoencephalitis (undiagnosed).
Not one doctor has been willing to discuss ME/CFS or my non-existent sed rate. My brother has the same issues. We also have high serum iron and/or ferritin off and on, (both heterozygous for hemochromatosis) and
homozygous MTFR variant.
AND, my rheumy started me on methotrexate & 1 gram folate 2 months ago.
I’m so confused. I have no idea what to do. There’s obviously something going on in my blood. Wondering if I should take methylfolate, maybe ask for a homocysteine test?
Questions:
are there any blood diseases (eg sickle cell or other) where people do not get cfs/me?
is any blood type (AB etc ) that is more or less represented?
how about Rh + or Rh – ?
anyone seen articles or research on these?
From site
http://www.medicine.mcgill.ca/physio/vlab/bloodlab/esr.htm
Some interferences which decrease ESR:
“abnormally shaped RBC (sickle cells, spherocytosis).
technical factors: short ESR tubes, low room temperature, delay in test performance (>2 hours), clotted blood sample, excess anticoagulant, bubbles in tube.“
lab samples, imo, are not tested for sed rate within two hours of collection.
Holy shit… I have low protein C and chronically low ESR (fluctuating from 2-5 since I started having symptoms in 2010), plus many SNPs for higher risk of DVT. I’m looking into this further. Thanks!
Just had bloodwork done and my ESR was 2 again. I also have had low protein C for many years. In the grand scheme of things I have a “mild” case of ME though.
Anyone know what sed rates typically are in long covid? Same as mecfs or different?
I’m me/cfs type long covid as is my teen daughter. My ESR was 5 the one time it was tested, and my daughter’s was 2.
I’m so confused. I’ve just been reading a lot about fibronolytic substances like nattokinase and serrapeptase and how they can be useful in ME/CFS and now I read this. Low ESR means low fibrinogen and little to no excess fibrin I suppose?
My sedation rate has never been over 2, and has consistently <1 for the last several years. Doctors keep telling me I should be happy because it means I have no inflammation in my body.
I m 44yo female, 165cm and 54Kg. Studied and reiki, remedial massage therapies
and nutritional medicine. I also have type3 destructive coeliac and endometriosis.
I mainly use Shoalin mindfulness and Qigong plus the Kung Fu for strength and fitness and to combat muscular spasms, hemispheric facial spasms and Neurological Migraines as I have adverse reactions to many drugs.
I have been doing physio and ligament/tendon strengthening exercises to combat all of the below things since i was in my 20s building on them as i learn.
Same as reiki, and I regularly see a psychologist to continue my journey releasing and moving through abuse and trauma.
I have been diagnosed with FM & CFS, I have ESR’s that can be 2-7, but ‘spikes’ as high as 280 when I was hospitalised, and since then it’s been spiking to 55 and taking a long time to come down below 24.
I also have CRP’s and MCV levels either borderline or outright megacell anaemia
I previously have had subacute Hyperthyroiditis with enlarged gland, thyrotoxic Free T3 & T4, and very high B12 levels and Suppressed TSH.
Was supposed to be monitored for autoimmune Graves disease.
I have found that if I mention anything about any part of my physical health I am taught about mental health and the affects of stress on my body, and persistent pain. And, pushed towards psych help or pain management clinic.
I have some minor degenerative Spondyloarthritis, i get ‘mild’ synovitis, joint effusion in hands and feet. Cervical spurring bulging slipped discs in cervical and thoraci, dome facrtal arthrosis and mild canal stenosis. Also mild Sheuermann’s disease (scoliosis) and Schmorrl’s nodes, 4 yrs ago – not informed.
I do not show signs of erosive damage or physical deformity
I was previously diagnosed with Seronegative rheumatoid and Psoriatic Spondyloarthritis and treated in clinical trials with Humira etc.
Despite all of the above since treatment was not resumed 8yrs ago. Plus now, Bilateral LL Edema and Cellulitis for 4yrs causing this time: 5mth non-healing ulcer, my GP and Vascular Surgeon all send me to Rheumatologist.
I have been told – I have no active autoimmune disease to treat – or that it is in remission as I previously never showed RF or ANCA. ANA’s, and still don’t.
It’s hard to have any trust in much anyone, is saying to me 🤣
But I will persevere on my own, as I always have I guess ✊️
Thank you for this space.
Apologies- I got the bloods mixed up : my ESR’s are generally 25-55 but come down to 2. The CRP’s have been as high as 155, and my IGE’s were above 250.
I’ve also had hepatomegaly for a couple of years with no clear cause.
Thankyou 🙏 Emily