

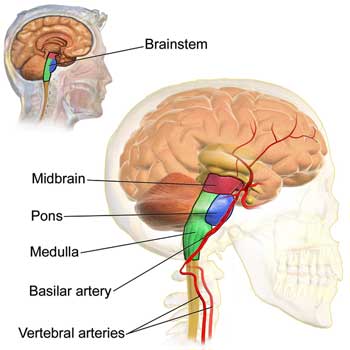
The most primitive part of the brain, the brainstem – a part of “the reptilian brain” – doesn’t get much respect in medical research. VanElzakker pointed out that most brain scan studies focus on the upper, more highly developed parts of the brain. Because brain imaging techniques can’t effectively capture the upper and lower parts of the brain, these studies often miss the brainstem.
The brainstem may be “primitive” in the sense that it was one of the earliest parts of the brain to develop, but that doesn’t mean simple, and it certainly doesn’t mean unimportant. Just the opposite, in fact. In this case, primitive means fundamentally important.
Located at the bottom of the brain where it meets the spinal cord, the brainstem is the first recipient of all the sensory and “motor” signals from the spinal cord. It regulates very basic functions – like breathing, heart rate, blood pressure, digestion, alertness, sleep – the fundamental stuff you really don’t want to go wrong.
If you want to walk or move your arm, or type on a keyboard, you need your brainstem to do that. Coordination, balance, equilibrium and muscle tone – these fine-tuned processes essential to movement – are all regulated by the brainstem. Severely damage your brainstem and you’re pretty much toast – destined to live out what’s left of your life in a care facility.
Lastly, the brainstem is densely packed with mast cells – an emerging problem in ME/CFS.
Most ME/CFS brain imaging studies have focused on the upper part of the brain, but one Australian researcher, Leigh Barnden, has been bucking the trend.
One study found neuronal damage in the brainstem which could be causing autonomic nervous system problems.
Another study which found impaired communication from ME/CFS patients’ brainstems to other parts of their brain suggested the same. Interestingly, the study also found what appeared to be a compensatory response – increased signs of myelination in the sensorimotor cortex of the brain. Barnden believed the sensorimotor region was bulking up in an attempt to understand what the wonky brainstem was telling it. Barnden suggested those hard-to-understand signals from the brainstem could explain some of the problems with movement in ME/CFS.
Barnden’s next study found inadequate communication between the brainstem and other parts of the brain (vasomotor region, hypothalamus and prefrontal cortex) that regulated autonomic nervous system functioning in ME/CFS.
The Study
Neuroimage Clin. 2019; Intra brainstem connectivity is impaired in chronic fatigue syndrome. Leighton R Barnden,a,⁎ Zack Y Shan,a,b Donald R Staines,a Sonya Marshall-Gradisnik,a Kevin Finegan,c Timothy Ireland,c and Sandeep BhutaC. 10.1016/j.nicl.2019.102045
This year, Barnden, our brainstem pioneer, is at it again. His Oct. 2019 study, “Intra brainstem connectivity is impaired in chronic fatigue syndrome“, used a functional MRI to see how areas within the brainstem and some areas outside the brainstem were communicating with each other – at rest, and during a cognitive task.
Barnden mostly examined the reticular activation system (RAS), a network of neurons that regulate wakefulness and sleep, the fight and flight response, posture, and the ability of the brain to stop paying attention to innocuous stimuli, etc. (Your brain is powerful but it can only process so much stimuli at one time and if your RAS is not doing its job you may have trouble focusing, etc.)
The bilateral medulla and cuneiform nucleus regions in the medulla and midbrain, the thalamus, the midbrain dorsal Raphe, hippocampus and left culmen, as well as the connections within the brainstem, were all tested.
The fMRI assessed brain activity levels using blood oxygen levels. The higher the blood oxygen level in a part of the brain, the better connection between parts of the brain.
Results
Very quickly, a key theme in ME/CFS research reared its head once again. At rest, everything was normal but when put under a cognitive stressor, the ME/CFS patients’ brains appeared Abby-normal indeed. Some studies which use patients at rest do show abnormalities but apparently there’s nothing like putting people ME/CFS under some sort of mental or physical stressor to produce results. This is, after all, the exertion disease.
It turned out that the people with ME/CFS demonstrated something of a “communication breakdown”. Different parts of their brainstem weren’t talking well with each other. Nor was their brainstem communicating well with other parts of the brain.
The most problematic connection for people with ME/CFS was between both parts of the medulla oblongata and the left cuneiform nucleus. While it was difficult to pin down the exact impact, Barnden reported that weakened connections between these two areas of the brain could produce such issues as maintaining movement, sleep quality, autonomic function and cortical arousal levels, which affect memory, learning and problem solving,
ME/CFS patients’ brainstems’ connection with two nuclei in the thalamus, and between the rostral medulla and hippocampus, were also impaired – suggesting that whatever damage has occurred in the brainstem is also affecting connectivity or traffic to the midbrain as well. Because the thalamus relays motor signals to the motor cortex and regulates sleep, alertness and wakefulness, a bad connection could impact all of those.
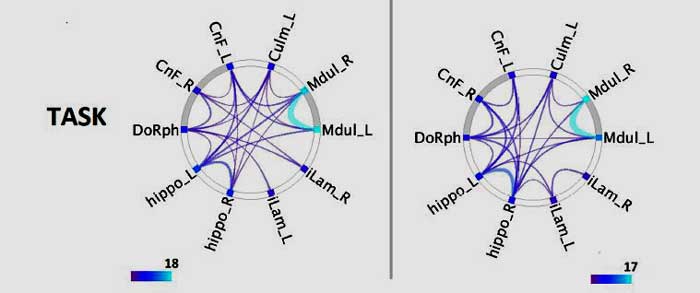
Check out the reduced connections in the ME/CFS brain on the right vs the healthy controls on the left. (from Connectogram image – study)
Barnden’s results were given an extra boost when he found that weaker connections within the brainstem and outside of it were associated with more severe symptoms.
Barnden, and Jeff’s and Jen Brea’s experiences with craniocervical instability gave us a vivid display of what a tweaked brainstem can produce. In their case – and in the cases of a surprising number of other patients – lax ligaments were allowing their skull to settle onto their brainstems. The results were severe ME/CFS-like symptoms – symptom which disappeared when surgery corrected that issue. Problems with the brainstem could conceivably, then, produce many of the symptoms – if not all the symptoms – associated with ME/CFS.
Barnden has not, to my knowledge, mentioned craniocervical instability in any of his studies. It’s not clear if it would show up in them but it seems inconceivable, on the other hand, that CCI/AAI could be responsible for all the brainstem issues he’s found in ME/CFS. If that’s true, then the brainstem in some patients is being impacted another way – perhaps by a hit-and-run virus or an inflammatory or autoimmune response.
We clearly need studies that will tease out different factors that could be impacting the brainstem. The first ME/CFS CCI/AAI paper is about to be published – and will helpfully alert more researchers and physicians to this problem. Avindra Nath’s assessment of CCI/AAI in its ME/CFS intramural study will help bring some clarity as well.
We should be hearing more about the role the brainstem – or the “reptilian brain” – and its control of basic processes plays in ME/CFS. VanElzakker is pursuing his own brainstem studies and the NIH is incorporating brain imaging into their intramural study as well.
Conclusion
With four studies under his belt, Barnden’s brainstem studies have become a model of consistency. Barnden has found evidence of damage to the brainstem (demyelination) which may have sparked a compensatory response outside the brainstem (remyelination), reduced functioning within and outside of the brainstem, and evidence that brainstem issues are associated with more symptoms.
All this suggests that this so-called primitive, but oh-so-fundamental part of the brain is not working well in ME/CFS.
Jeff and Jen Brea have shown just how devastating brainstem issues can be. Problems with the brainstem could help explain the problems with alertness, sleep, the autonomic nervous system, difficulties with focus and attention, mental fatigue and even coordination and movement. In fact, if you’re looking for one issue that could explain some of the really fundamental problems in ME/CFS, the brainstem could very well be it.
Just why brainstem problems appear to be occurring in ME/CFS is unclear but several studies underway should help to clarify the role it plays.
End of Year Fundraiser Update









I would be interested to know if lax ligaments were my issue (and this could be potentially fixed). Do you know how to have that tested for?
You need to read to article from earlier this year on craniocervical instability.
My apologies Nancy I should have included a link – here is one of the posts-
https://www.healthrising.org/blog/2019/02/27/brainstem-compression-chronic-fatigue-syndrome-me-cfs-fibromyalgia-pots-craniocervical-instability/
More on this is coming up as well.
Hi, lax ligaments may mean EDS (Ehlers Danlos syndrome).
Have a google. Comes in numerous categories. No cure but protocols to improve it are mooted. Good luck.
Yes, CCI incidence is much increased in EDS. I would be shocked if we figure out ME/CFS without finding a connective tissue connection.
@Nancy Harkness,
You need an upright MRI (not so easy to find) to get diagnosed for things like CCI and Chiari Malformation (that droopy brainstem).
I don’t believe that having something like EDS is always required for these conditions but they are certainly more common in the EDS population. Please remember that EDS runs on a continuum and people can be greater or lesser affected. The more affected individuals get the Ehlers-Danlos moniker. To find out if you may belong, it is easy to find the clinical guidelines (Beighton Scale) for assessing Hypermobile type (the most common) of EDS.
As I have EDS and usually hang out in that community, I can say from reading all the reports of people with things like CCI and Chiari, that they mostly really notice symptoms with head movement, and the symptoms can be quite severe. The ‘cure’ is often a very invasive fusion of the cervical vertebra, so I hope that most of you don’t hang your hat on having something like this!
Also what is not mentioned is that afflictions like tethered cord can produce similar symptoms. The spinal cord is designed to hang free within the spinal canal and when it doesn’t, then problems arise. Sometimes people can have ‘occult’ spina bifida too.
Thanks again Cort! I also have a (sorry, out of context) query for you. I have tried and tried to get ‘conformation’ to be on your forum, and have checked my junk and other filters, and have also written a note in the ‘contact us’ section–but alas–no response. Can you help me?
I’m a bit behind. I will get back to you on that today 🙂
An upright MRI will show craniocervical instability CCI or atlanto-axial instabilityAAI
Please give me a mail address, and I
will send a bank check.
Gladly!
Please make it out to Health Rising and send to:
Cort Johnson
2555 Hampton Rd Unit 6308
Henderson, NV 89052
Thanks!
I have Lyme, ME/CFS, Fibromyalgia, POTS, Mast cell activation, Ehlers Danlos Syndrome, etc, etc.
I’ve been sick and treating since 2011. By treating, I mean going broke seeing the experts.
Just started Brainsway Deep TMS a month ago at the local University for Depression. I am depressed due to my health battle. It is covered for treatment resistant depression by many insurers including Medicare.
Needless to say, this treatment is working wonders! It is helping my brain fog, POTS, pain, mood. It is helping everything I’ve been dealing with. It’s not a treatment that’s simply helping a psychosomatic problem, but is a top down treatment that’s making a huge difference.
The brain controls everything. More focus needs to be placed on top down (brain to body) treatments since the bottom up ones (body to brain), chasing symptoms, don’t work and leave us broke.
I am happy you got this help—from Brainsway Deep TMS! How often are your treatments and for how long each session? Thanks for sharing this hopeful experience!
Hi Cecelia,
It is 36 sessions, 5 days/week for 6 weeks then tapering down the # of sessions the final 3 weeks. 18 minutes per session.
I was so terrified before my first session, but I am so thankful I’m doing it.
Hope this helps ?
Going broke seeing the experts! Ha! Thanks so much for passing that on. TMS has become one of the most studied treatments in FM and several trials are going on right now.
I believe they had trouble before getting at the deeper parts of the brain when some of the trouble lies for FM but I believe they’re getting better at it. This is certainly an active area of research.
It’s good to hear that it works.
Angela, I am very interested to hear more about Brainsway TMS to help treat ME/cfs.
Ive tried so many things since 2003. One of my hardest symptoms is constant dizziness. Any thoughts? Is it at all invasive? Any side effects?
Thanks!
It is not invasive at all.
It scared me at first because it’s a sensation that I’ve never really felt. Kind of like a woodpecker tapping on my skull for 2 seconds every 18 seconds for 18 minutes. But you get used to it.
I have been able to take my son to the beach and go out to dinner as a family. Sounds so simple but I’ve missed out on a lot of my tween son’s childhood.
I’m not back to normal, but I’ll take these improvements after living in a 24/7 torture chamber for 8 years.
I have no idea if it helps dizziness. I feel so clear headed immediately after each treatment, though.
For years I had trouble just being able to think and form a thought. I could feel my brain struggling to think and it would scare me.
I have no idea if/or how long these positive effects will last. However, just experiencing that it’s possible is a miracle to me.
If everything goes as planned, I will be able to go see my daughter graduate from college (across the country) in 2 weeks. Fingers crossed.
There is hope. Every treatment doesn’t work for everyone. Heaven knows I’ve tried some weird treatments. But don’t give up and eventually, you might just stumble on something seemingly ridiculous that just might clear away the cloudy skies for you. Or at least let you know that the sun’s still shining behind them.
(*This is my personal experience. Of course, I’m not a Dr)
Angela, I also had 6 weeks worth of Brainsway TMS, and it helped greatly with depression and ultimately with sleep. (My brain was unable to sustain the usual 20-minute protocol, so they set up a 7-minute, theta-burst protocol for me. I liked the shorter sessions.) This has been about a year ago now. I could feel the depression slowly creeping back after a few months, and now it seems to have returned full force. However, for me, the sleep benefits remain. I can sleep longer and more deeply than I could before the treatments. If I lived in a town where TMS was available, I would consider going in for another series of them. However, in my case I had to travel 90 miles to get to the psychiatrist’s office, and then stay with family, friends or in an Airbnb because I had to be at the doctor’s office every week day. I’d come home on the weekends. Also my co-pays were $40 each, which meant a total financial outlay of about $1,200. I may repeat the process at some point, but I’ll have to be more desperate and a bit more wealthy to do it again.
A well-written article, Cort. You make it so easy to understand. Mind you, we’ve known about the locus caeruleus for many a long year but good to finally see some more exacting testing being done, especially by an Australian, my own country.
Thanks Tricia. Australia has been quite a leader hasn’t it? Particularly in brainstem research, metabolomics, NK cell functioning….Very good to see all that stuff going on down under 🙂
We may have some good research going on in Australia but it’s not reflected in our health guidelines for ME/CFS or in how doctors treat us if we have this. I have had a discectomy at C6 and spinal Cord compression at both C6 and C4. I find my symptoms are worse with head tilt down or up but have been told my neck can’t have anything to do with my symptoms.
I’ve never commented on a forum before, so here goes….
Firstly, thank you Cort for all of the information that you share and making it understandable for the foggy brain.
I’d like to share something that I have tried in the hopes that others may benefit also. I’ve had ME/CFS for fourteen years and I am now predominantly housebound. I use a wheelchair or mobility scooter to leave the house intermittently. Earlier in the year I read about craniocervical instability and Jen Brea’s story, and probably like many, I grabbed onto the hope that Jen’s remission gave me and started wondering if there was any other way to relieve pressure on the brain stem without surgery. I wasn’t well enough at the time to research whether any specialists in Australia would do the testing for craniocervical instability.
As luck would have it, my husband read about a decompression table at a local chiropractor and out of desperation I thought I’d give it a go. (I just had to lay for twenty minutes and hope I didn’t go into a crash from it).
Chiropractic is one of the things I’ve not tried in the past fourteen years. Manipulation just seems too aggressive for my body and nervous system at this point. So, with no expectations, I tried the treatment and was pleasantly surprised the next day when the crash didn’t come. (I’ve not been able to go to an appointment in the past six years without the payback. )
To make a long story short, I’ve been laying on the decompression table weekly now for the past couple of months and had my neck gently stretched for twenty minutes. For two to three days afterwards, my symptoms are a little lessened. For those few days I wake up feeling more like I’ve been hit by a mini bus rather than a semi-trailer. I know it sounds significantly small, but even a small amount of relief makes a difference in a lot of years of suffering. I’ve even been able to ride my scooter around the block for two days in a row after a treatment. Half an hour out of the four walls of my home is good for the soul.
I have no idea why this treatment helps. I just wanted to share my experience with you because it’s the first thing that has eased my symptoms (however briefly) in 14 years.
Hi Sandra,
I think any change that can be reproduced, whether positive or negative, is an indication of something and it can give us clues that we might be able to piece together.
Just having a little bit of an influence on how our body functions can be a boost ?
Great idea to try that Sandra. Manual decompression, as you know, is one of the ways doctors use to test for the possibility of CCI/AAI.
Congrats on the improvement. I hope it continues. 🙂
Yes! This gives me hope and a plan of action. Thank you Sandra for sharing this information. It is very helpful indeed.
Just recently I have been excited to hear a number of interviews and lectures by Dr. Stephen Porges on The Polyvagal Theory. I wish someone would link ME/CFS research to his work, particularly on the « freeze » or « shutdown » part of the autonomic nervous system, the aspect that we inherited from our pre-mammalian reptilian ancestor. Dr. Porges talks a lot about this aspect of the autonomic nervous system, as it has been given far less consideration in the past than the fight or flight vs parasympathetic rest and and digest aspects.
With serious hypotension, brachycardia (slow heart rate)—in fact, nearly everything slow and low in all my basic levels and function—I can see that early plant-eating reptile or amphibian in its dive to the bottom of the pond or frozen stance, attempting to hide, in the forest litter.
I am not beginning to do justice to all the details and application of Dr. Porges’s polyvagal theory and research. Hoping someone with a less shut down brain will check this out on youtube at least to see its affinity with the problems of ME/CFS
It is like your brain is in a state of underdrive, pots ME patiënts are in overdrive. Both can be due to this brainstem dysfunction. So we can explain two types of patiënts.
Yes, so often is the freeze part of fight and flight ignored. I haven’t had one for a couple of years but when I have a bad attack, my blood pressure plummets and I literally can’t move for a few hours.
My experience is that I experience subtle freezes frequently. Porges hypothesis is indeed fascinating and Tim Vaughn did dig into that a couple of years ago on Health Rising but we could use an update. (Interested in writing a blog?)
https://www.healthrising.org/blog/2014/01/02/immobilized-mecfs-fm-polyvagal-theory-movement-restriction-autonomic-nervous-system/
Thanks, Cort! I don’t feel sharp enough to research and write a whole blog. But I did add more to my comments below, Dec. 7.
I always appreciate that you are smart, motivated, caring and disciplined enough to make these research efforts for us. You do us a great service!
Thanks Cecilia. I failed to get you to write it 🙂 but it is on my list. Thanks for the reminder.
Thank you, Cort. This is really my favorite hypothesis.
Me too 🙂 It potentially ties in so much – from the autonomic nervous system problems to problems to concentrating – to movement problems – to sleep.
Time will tell but it certainly is a very intriguing area of research. Good for Barnden (and his funders) down under!
My 4 sons all have different symptoms and I keep looking for a link. One has NDPH (new daily persistent headache) with depression and anxiety, another POTS with brain fog and delayed sleep phase disorder, a third OCD and SAD, and the last one has esophageal issues and nausea. I listen to The Energy Blueprint (which every here should really investigate) podcast. There is a treatment based on Dr. Porges’s polyvagal theory, called Brain Harmony. It is owned by occupational therapists. We are going to try it out. I will let you all know in a few months if we have made progress. Wishing everyone here health and progress in their journey seeking health. The last 12 years have been hell in our house, and that’s an understatement.
Thanks.
I plan to check out the Energy Blueprint and thanks for mentioning Dr. Porges theory. Please let us know how the Brain Harmony attempt goes. Good luck!
Chiklyinstutute.com arranges amazing courses in this area for osteopaths
Thanks Cort for always posting such great articles.
I got a bit disappointed when I read some of Barndens article and discovered that he picked the ME/CFS patients using Fukuda criteria. That’s not good enough in my opinion. How can we be sure of the results if he uses such wide criteria instead of ICC? 🙁
I didn’t realize he was using Fukuda but while Fukuda may not be the best definition it was around for a long time and while it was around it was good enough to find all sorts of stuff in ME/CFS from NK cell problems to exercise issues. The only definition I would run screaming from is the Oxford.
Another reason not to worry so much about Fukuda is that Barnden is working with Griffiths which presumably has a large and well characterized group of ME/CFS patients. I would be surprised if someone who doesn’t have ME/CFS is going to get into Barnden’s studies. In a case where you have good doctors who know what ME/CFS is definitions are kind of secondary.
This may sound weird but it just occurred to me that it’s possible that in this situation – where you presumably have doctors who know what ME/CFS is and are diagnosing it properly – it might actually be better to use Fukuda.
This is because the more symptoms required for a definition – and ICC requires more symptoms than Fukuda – the more likely a subset of patients with more psychiatric illnesses (+ ME/CFS) are going to show up in a study. That suggests that a study could actually get skewed in one direction by using the ICC. (Wessely actually used the more symptoms = psychiatric syndrome – in one of his papers.)
If this is true, then if you already have a good set of ME/CFS patients then it might actually be better to use Fukuda to avoid skewing the study toward ME/CFS patients with psychiatric illnesses. I don’t know if this would pan out in real life but it seems to be theoretical possibility.
In any case, given where Barnden is and where I assume he is getting his patients from I would be surprised if they weren’t real ME/CFS patients.
How about that for an interesting twist to the criteria!
Eagles Syndrome can play major roles in the Brain Stem areas, so can Biotin Thiamine Basal Ganglia Genetic deficiencies. ES diagnosed with proper CT Contrast
so can CT Angio with Contrast then taking both Scans & put them in 3D images & never go for throat internal Surgeries always pick the external neck Surgery with
experienced ES ENT Skull Based Surgeons. I think CCI only lifts the Brain off of Eagles Syndrome & in time it will come back. One can do a Panoramic X-ray for ES
but is not diagnostic but is useful to see the styloid process. Always request measurements in the Scans results of the styloid bones each side. ES can cause
compressions of major arteries in the neck & heart veins
https://www.livingwitheagles.org
& Facebook Eagles Syndrome Group & see Wikipedia Eagles Syndrome
~Thanks Cort. This is really interesting. I wonder whether this supports Dr Raymond Perrin’s theory that ME/CFS is caused by mechanical abnormality in the spine which prevents the normal elimination of toxins (to paraphrase).
Everyone now has to wonder about mechanical issues in the spine including CCI, spinal stenosis, chiari malformation and other possibilities.
I’m surely interested in the craniocervical aspect of things but I always wonder how that could be a cause if my CFS was sudden onset? I do feel like I suffered some kind of brain damage from that “flu”. On the other hand, I also feel like I have always had skeletal issues, clumsy, confusion, etc.
Think of a virus or autoimmune response that suddenly attacked the ligaments holding our very heavy heads upright! Down the head goes onto the brainstem.
You don’t need to have an accident to have this happen. Anything that weakens the ligaments (sudden onset EDS?) could do it.
Here is a little more about Dr. Stephen Porges, which I parsed from some interviews: In the early 1990’s he became very interested in the autonomic nervous system when studying premature fetuses and early births. If their heart rates slowed, he learned, this was a sign of danger. A slow heart rate did not indicate a reduction of stress and of coping well with birth, but of the earliest, most ancient stress response coming into play. He found this was the earliest branch of the autonomic nervous system, and it was the only branch that was mature in those very pre-term babies. It was the freeze or shutdown strategy of our reptilian ancestors, but in humans, it would lead to hypoxia and death.The sympathetic branch with its activating effects was not yet mature enough in these pre-term babies to respond to the stress of birth.
He plunged into a scientific study of the autonomic nervous system, but the applications of his findings have been most employed by therapists working with trauma and autism. Still, the workings of this earliest branch of the autonomic system, the Dorsal Vagal Complex, originating in the brainstem, have many other applications. I do think that the « freeze » effect, the slowing and metabolic « retreat » involved when this earliest branch comes into play, is evident in our form of illness. Naviaux with his background in autism research saw a similarity in the metabolic slowdown of ME/CFS and described it metaphorically as a form of hibernation.
I apologize for the inexactitude of my « gleanings », but wanted to share my sense of a similar pattern between the new research showing slowing and abnormalities in the brainstem, sometimes from compression, with the effects of the earliest branch of the DVC, the Dorsal Vagal Complex, our deepest fallback system in response to « stress ».
I hope that with all the applications of polyvagal theory to work with trauma survivors, no one here will take this to mean that the implication for ME/CFS is that it is just the product of some psychological trauma, and even more so, that it is in any sense, voluntary. That is a misunderstanding of the functioning of that branch of the autonomic nervous system, which produces the involuntary effects of freezing and shutdown: bradychardia, reduction in breathing or apnea, hypoxia, metabolic slowdown, etc., as a « last ditch » attempt to save one’s life. Our reptilian and amphibious ancestors could survive with this strategy of freezing and deep shutdown—it was a successful strategy for them—but as mammals, with our larger brains and much greater need for oxygen, metabolic activity, etc., this recourse, if sustained, would kill us. So as mammals we developed two other levels of the autonomic system: the fight or flight as well as the systems of regulation when we feel safe. But the relationships and prioritization among these branches of the autonomic nervous system evolve to a great extent through experience, from physical to social, and so may not be optimal. The range of potentiality can be extended—that is some good news I found in Porges’s work. But mainly the value I see in his work is a greater understanding of all the ins and outs of the autonomic nervous system, as problems there, are so common for us.
Thanks for the start on the Porges blog :). It’s fascinating stuff and thanks for pointing out that it is NOT voluntary.
Yes, that is a non-myelinated branch of the nervous system and when it takes action, what happens is involuntary!
The fact that our HPA axis is not working properly surely would be the reason our body has to resort to the freeze function.
I was just watching the Voices from the Shadows film again because it was found that Lynn Gilderdale and Sophia Mirza (who both had severe ME) had Dorsal Root Ganglionitis.
Sophia Mirza’s spinal investigations concluded ‘Definite pathological changes are identified… in particular there is a dorsal root ganglionitis in three out of four dorsal root ganglia sampled.’
You say those who have an injured brain stem are toast and end up in care facilities but that’s exactly what we see in very severe M.E, utter incapacitation. In the very severe movement, muscle tone, swallowing and alertness can be impaired. It makes me think if we hadn’t seen the very severe ignored and focused on the walking wounded, wondering which of the Zillion possibilities was behind their chronic fatigue , we might be further forward.
M.E isn’t just another fatiguing “disorder” it’s a complex illness and potentially devastating. Reading your article that brain stem issues are hard to find via current imaging just makes it seem highly possible this is potentially the deadly mysterious source that can either be mildly impacted or majorly impacted. In the severe it’s much more issues around basic function and maintaining homeostasis than it is being tired and the being tired is usually overwhelming cognitive fogginess rather than just muscular issues, obviously there’s exceptions and probably there are different underlying causes within our community, but I think this should be a key target of research and I would love to see more.
Do I ever agree. I think the compression problems which some like Jen Brea had found and relieved, could also point to the Dorsal Vagal Complex, the top of the autonomic nervous system which is found in the brainstem. Lowering of heart rate and blood pressure, gut motility problems including gut pain, sudden motility or constipation, chronic hypoxia, mental freezes, loss of mobility to shutdown—all that to me point suspiciously to this earliest branch of the autonomic nervous system in the brainstem. I don’t know what or how this research can be best done, but it seems to me that here is one good place to look.
I agree with you and should be looked at and study! My Chiro. found my neck problem from a simple xray that my head was off my axis, the worst he had seen and no telling how long it was that way as I have had many falls from hieghts, many hits in the head in my lifetime! I also have a little curve in mid spine area which I remember my dr. telling me to get it ck. when I had an epideral with my first child 30 plus yrs. ago..never got it check ..
Show up on the xray done by Chiro. a constant problem area possible pinched just areas and methods to address the problems we are having.. to rule things out..personal choice to see a Chiro.
Well I’m very excited. Unlikely to ever get cutting edge diagnosis, but definitely going for traction and some bodywork on my short scrunched up post-injury neck to see what happens…