

A large French study finds abnormally high lactate levels in ME/CFS even at rest…sometimes.
David Systrom seemed to call it out – his invasive CPET results suggested that mitochondrial dysfunction was present in a large subset of people with chronic fatigue syndrome (ME/CFS) – and he believed their blood lactate levels were probably elevated.

Blood lactate levels were abnormally high, even at rest, for one group of patients. The higher levels occurred intermittently.
Right on the heels of that study comes a seeming stunner: a study finding elevated blood lactate levels not after exercise but at rest as well. The title of the study, “Elevated blood lactate in resting conditions correlate with post-exertional malaise severity in patients with Myalgic encephalomyelitis/Chronic fatigue syndrome”, suggested a quite troubling finding: even at rest – even when the participants’ aerobic energy production systems were not being stressed – their systems were not keeping up.
Workwell’s Staci Stevens has reported that even very light exertion causes some people with ME/CFS to exceed their aerobic capacity. If that was happening at rest in a significant proportion of patients, the French study was identifying something troubling indeed. It meant that no relief from the troubles (fatigue, pain) associated with a reliance on the toxic anaerobic energy production system was possible – even at rest.
Elevated blood lactate in resting conditions correlate with post-exertional malaise severity in patients with Myalgic encephalomyelitis/Chronic fatigue syndrome. Alaa Ghali, Carole Lacout, Maria Ghali, Aline Gury, Anne-Berengere Beucher, Pierre Lozac’h, Christian Lavigne & Geoffrey Urbanski Scientific Reports volume 9, Article number: 18817 (2019).
This very rare French ME/CFS study took place between 2011 and 2017 and grew to include 123 patients, all of whom met the International Consensus Criteria for ME.
It appears to have been very well controlled. The participants were admitted to the University hospital Angers-France the night before. Their blood was taken in the morning (following a meal after a sixteen hour fast) and then seven more times during the day. During their stay, food and activity levels were highly regulated.
The following tests were run: blood lactate, immunological assay, infectious disease screen for HIV, hepatitis B and C, Lyme disease, enterovirus, Mycoplasma pneumoniae, Chlamydia pneumoniae, serum zinc, 25-hydroxyvitamin D, plasma cortisol, testosterone, iron studies, plasma vitamin B12 and serum folate, full blood count and differential, erythrocyte sedimentation rate, electrolytes, calcium, phosphate, fasting glucose, C-reactive protein, liver function, serum protein electrophoresis, renal function, thyroid function, and creatine kinase.
The Results
Two distinct groups of ME/CFS patients were found: elevated blood lactate levels (≥2 mmol/L) were found at least once in 45% of the participants while 55% had consistently normal lactate levels (<2 mmol/L). (According to UC Davis, normal blood lactate levels at rest are 1-2 mmol/L).
A closer look at the results, though, brought some surprises. It turned out that elevated blood lactate levels at rest were not the norm at all – not even in the high lactate group. Most of the time, even their blood lactate levels were normal.
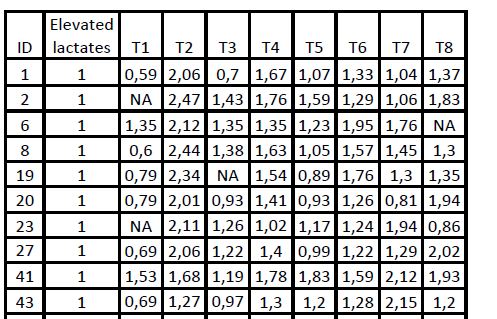
Check out the results from the first ten participants in the high lactate group. Note how much the readings jump around. High lactate levels often appear next to what appear to be abnormally low lactate levels. (Only one person in the study had abnormally high lactate levels at every time point.) While elevated lactate levels were found, normal lactate levels were the norm.
Approximately 52 of the tests showed high lactate levels but about double that number showed lactate levels that were below what is considered normal for a resting state. (Was a low lactate group present as well?)
At one time point, though – 1 hour following a meal after a 16 hour fast – blood lactate levels did appear to be consistently above normal. Something about that time point appears to have consistently tweaked a large number of people with ME/CFS.
Higher Lactate Group
There certainly was a higher lactate group. The lactate levels of the high lactate group was significantly increased at every time point relative to the normal lactate group. Even if their blood lactate levels at rest were not consistently elevated (i.e. > 2 mmol/L), they were significantly higher relative to the other group.
Plus, while the high lactate group did not experience more fatigue, they appeared to be hurting more: significantly more of the group experienced more severe PEM symptoms than in the normal lactate group.
The Blood Lactate Conundrum

With blood lactate levels being affected by several different processes, it was difficult to understand what any one measure means.
With so many questions, I turned to Mark VanNess, a Workwell exercise physiologist who has participated in many ME/CFS studies. What about all the fluctuations in lactate levels, I asked. What did it mean that lactate levels at one time point, but not others, were elevated? And what about all those low lactate readings – what did those mean?
Mark couldn’t provide the answers to those questions – it turns out that no one can, but he did explain why. It’s easy to collect and measure blood lactate but accurately interpreting them is daunting. The French paper suggested that the higher blood lactate levels might reflect a mitochondrial dysfunction but other possibilities are present.
Lactate blood levels can be affected by a number of processes:
- Lactate uptake by the muscles – Because the lactate levels found in the blood present a balance between lactate production by the muscle and lactate uptake by adjacent muscle fibers, high blood lactate levels could indicate high lactate production by the muscle or reduced lactate uptake.
- Lactate uptake by the liver and other tissues – Because the liver and other tissues also take up lactate from the blood to use to produce energy (yes, lactate is used as an energy substrate), problems with liver (or other tissue) uptake of lactate could result in increased blood lactate levels.
- Damaged slow twitch muscle fibers – Fast twitch muscle fibers produce lactate while slow twitch muscle fibers actually use lactate. It’s been hypothesized that problems with energy production in ME/CFS patients’ slow-twitch muscles could be causing them to rely more on the lactate-producing fast twitch fibers – even during lower intensity physical activity.
- Altered enzyme activity in the mitochondria – Two enzymes – lactate dehydrogenase (LDH) and pyruvate dehydrogenase (PDH) – convert pyruvate into either lactate or acetyl-CoA. If the LDH enzyme dominates in ME/CFS, as has been conjectured, then more lactate will be produced.
- Noisy variable! – Lactate levels are dependent on so many factors that interpreting single measures is a daunting task. The best lactate study would subject patients to different levels/types of activity and then compare lactate levels.
In the end, then, any number of factors (increased lactate production, decreased clearance, altered tolerance, enhanced or impaired metabolism) could be causing elevated (or reduced) blood lactate levels. In fact, it’s possible that all are happening in one subset or the other of ME/CFS patients.
A final complication concerns the inability of sedentary people to utilize lactate as efficiently as people who exercise. The sedentariness that comes with ME/CFS could be having some effect on blood lactate levels.
Conclusion
This study found that intermittently increased lactate levels (particularly at one time point) occurred in a large subset (45%) of ME/CFS patients even when they were at rest. That group also consistently had higher lactate levels than the normal lactate group. Most of their resting lactate levels were, however, in the normal range.
Unfortunately, there are no easy answers. I’ve tended to associate increased blood lactate solely with mitochondrial and energy production problems, but they could also reflect problems with liver or muscle lactate uptake or slow twitch muscle issues. More study needs to be done to unravel what, if anything, is happening with this easy-to-collect but difficult-to-understand measure in ME/CFS.
**BIG (little) Fundraising Drive Update**
Thanks to the 243 people who have contributed over 24K to HR during this drive taking us about 55% of the way to our goal.
Blood lactate, it turns out, is quite a bit more complex than it seems. Health Rising found that out when we dug deeper – which is what we do as we try to get the bottom of what is going on with ME/CFS and FM. If that kind of deep dive supports you, please consider supporting us 🙂






Cort – I sent you a message as well as an email. Can you check to see if you rec’d it. Thanks
Sorry Cort, this is off topic but interested in your views.
I have long thought the brain has a key role to play in CFS. I have been reading Adrew Miller’s work and it is both interesting and compelling.
If I have this right he believes that in some cases of depression and potentially illnesses such as CFS parts of the brain are overreacting to inflammatory cytokines. So that the cytokines are not necessarily high, it’s the reaction that is problematic.
I have read that he is undertaking a clinical trial but can’t find any detail.
Do you know of anything further?
I have a very violent reaction to D lactate if I take certain strains of good bacteria which in almost every probiotic. Still trying to find a suitable probiotic that won’t cause D or L lactate build up.
Take a look at Gutpro. I don’t understand all the ins and outs of probiotics as they are incredibly complex. But addressing lactate and acidosis issues seems to be a large part of the Gutpro formulation. I have had a couple dealings with the manufacturer and they were great.
Could lactate levels be higher after meals because of poor glucose uptake? Diabetics also have higher blood lactate levels, and most of us have problems with glucose metabolism, even if we’re not diabetic.
I have been struggling for years with trying to get energy from food, whilst attempting to avoid reactions to food that result in even less available energy.
I have found that I need to eat every few hours – animal protein and fat, olive oil, coconut oil, seeds and low carb vegetables. I react to carbohydrates, with what seems to be an inflammatory response – particularly in my brain and eye functioning.
However, I’ve only recently found an intricate path to follow to achieve a relative level of normal brain and overall activity functioning.
However the last few years have been ‘challenging’ to use the modern day euphemism!
What I believe I experienced over the last few years, was a diminishing and chronic lack of available energy, particularly to my brain. I don’t generally have muscle issues.
Having a deficit in energy required for my brain – anything that tapped into this meagre resource, diverted energy away – like eating, emotional situations and so on. I didn’t have enough energy to fuel a multitude of activities – it was a case of either activity could have a small bit of energy but not at the same time.
Jarred Younger’s work on lactate being found in the brain, made sense to me. I would relate to his idea, if I remember it correctly, that the brain (with inflammation) running low in glucose/oxygen would produce lactate, that could then be measured.
I don’t think I have a problem with oxygen but I strongly believe I have a problem primarily with getting a usable energy source to my brain.
I think that’s always been one of my issues, I just temporarily resolved that by finding I could get energy from nuts. However I then became intolerant to nuts and eating them caused huge problems. Finding a replacement, that I could tolerate, for the nuts has taken me years.
With the improvement in my sleep I can now eat some seeds, olive oil and more importantly I’m now able to tolerate coconut oil. I think the MCT oil in the coconut oil and the other fats and animal proteins are providing the vital fuel for my brain. I’ve only managed to reach this point in the last few weeks but it’s making a bit of sense to me now.
I think we’re very complex creatures that need all sorts of resources to function – we just take them for granted until they go wrong. Even when we’re ‘resting’ many unacknowledged systems in our bodies are working away, unnoticed. So I would think our bodies, including our brains, are never really resting.
Shungu has also found excess lactate in the ventricules of the brain in ME/CFS. Glad that MCT oil helps. Sleep is such a critical issue – a series on that is coming up.
I experienced a marked improvement in my energy levels when I went to a keto type high fat, low carb diet. Which seems similar to your experience with nuts, oil etc.
Yes, any carbs, even sunflower seeds, are too high in carbs. I will notice a problem with my eyes, particularly the left one – everything goes a bit blurry and my brain is affected too. I then can’t think very fast and my memory gets worse etc.
I find eggs, beef, beef liver, chicken and pork give me and my brain energy and the fattier the better. I used to be able to get energy from dairy products and nuts but I can’t tolerate them anymore – they deplete the energy available.
Your ‘not getting energy from carbohydrates’ description is in accordance with my own health situation right now.
Have you already looked into thiamin depletion?
It has been overlooked greatly in our western society nowadays.
I imagine so. Digesting meals, oddly enough, is one of the most energy consuming functions our body does. Maybe its something to do with the long fast but now that you mention it I also wonder about the composition of the breakfast….Was there something that they ate which troubled their aerobic energy production system?
Yes, I wondered that too. What was the food? There also seem to be many people around, like me, with food intolerances or difficulties digesting certain food.
If I eat food I seem to have difficulty digesting, my blood pressure and heart rate shoot up.
Also, at times I could feel the energy seemingly being drained from my brain, just after I had eaten something. Two systems competing for limited energy supplies.
I was never so dependent on regularly eating before I became unwell. I could quite easily carry on all day without eating. I actually had more energy, in the short term, if I didn’t eat. Not exactly sustainable though.
I seem to have lost the ability to maintain my brain energy automatically but I seem fine through the night and when I wake up.
I also never used to eat so much protein from meat and eggs. I was much more of a carbohydrate – meusli, wholemeal bread kind of person. Now I virtually can’t tolerate any carbohydrates.
I seem to have completely changed.
This study may be interesting to look at in relation to the above. It looks at the availability of ATP and the efficiency of oxidative phosphorylation in mitochondria in ME/CFS. It also identifies 2 groups within the ME/CFS cohort: one that is more similar to the healthy controls and the other with excess lactate production.
Mitochondrial dysfunction and the pathophysiology of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)
Norman E Booth, Sarah Myhill, and John McLaren-Howard
Int J Clin Exp Med. 2012; 5(3): 208–220.
Published online 2012 Jun 15.
PMID: 22837795
Pubmed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3403556/
Thanks – that’s a nice correlation. It also, come to think of it, fits Systrom’s findings of a significant subset of ME/CFS patients which likely mitochondrial dysfunction and others with circulatory problems. Booth’s and Myhill’s methods have, unfortunately, however, come into question 🙁
https://www.healthrising.org/blog/2019/10/06/the-myhill-mitochondrial-test-and-me-cfs-studies-take-a-hit/
Considering exercise intolerance in ME/CFS, a new article came up in my medical news feed regarding new methods of assaying exposure to BPA (and other phenols) which puts exposure much much higher than previously thought. It got me curious as to the full effect of these chemicals (besides being well known endocrine disruptors), and guess what, they are connected with many more problems than that! Lung capacity is one of them…
BPA is all around us used in everything from food storage to personal care products and more…
I have long thought that exposure to man made chemicals might be a factor in ME/CFS and think there are hints and clues in various research articles that this might be happening. Here is one article; https://www.sciencedaily.com/releases/2019/10/191001094205.htm
On a personal note, I will see my PCP tomorrow about the abnormal antibody thyroid tests. I also have achalasia of the esophagus, now thought to be an autoimmune disorder where the body slowly kills the nerves involved in peristalsis. I wonder, having that, considering my esophagus is relatively near my thyroid, if it could have some sort of (deleterious) effect?
My fatigue has really increased and am way out of breath, hair falling out, hot and cold and hot…yada, yada…
And then there is the Ehlers-Danlos too–oh my!
Toxic exposures surely play a role for some. Look at Gulf War Illness – the vets there have the same darn symptoms as people with ME/CFS. There are probably lots of roads to this condition.
Good luck with the thyroid. If you can get thyroid support that might help a lot.
I’m sorry I’m confused. Didn’t Ron Davis prove that the mitochondria of ME/CFS people were “normal” but didn’t function properly due to some abnormality in their plasma? If you take our mitochondria out and put them in normal blood they function just fine. Why aren’t there studies being directed to figure out the problem with our plasma and not just keep concentrating on “abnormal mitochondria”? While I can see this is a long term project, it’s time to start building on what we know rather than reiterating what we already know in a different way that still yields no real new information.
Great points Gregory!
Lactates presence in elevated quantities is commonly associated with sepsis and severe inflammatory response syndrome.
Chronic Inflammatory Response Syndrome (CIRS) This is the body’s “out of control” inflammatory response to a toxin (i.e. mold, Lyme, etc.) it can’t get rid of that causes a cascade of inflammatory and hormonal changes that can cause fatigue, pain, gastrointestinal and neurologic symptoms, sleep disturbances, and other damaging effects to the body.
Nine months ago, I sent the text below to Dr. Gali. I did this because I see a very clear connection between the content of fructose in my food and lactate increase. I have not received an answer.
Dear Alaa Ghali
Thank you for your kind answer to my earlier question regarding lactate levels of healthy subjects.
Now certain observations of my own lactate measurements have raised a few additional questions. And your comments would be very much appreciated:
Could the key component to explain the high, but strangely varying levels of lactate in the test subjects, be different amounts of table sugar and fructose in the meals served? The caloric content of the standardized meals is specified, but I wonder how much sucrose and fructose they contained. I hope you consider my question as a “reasonably request”. As you kindly explained, healthy subjects never had lactate levels above 1.6 in your laboratory. But could the high lactate-subjects have a dysfunction related to the metabolism of fructose? A dysfunction that could be tested for and in the future be a tool in the diagnosing of this sub-group?
My reason for asking, is my “sample of one”, namely my own experience. I have seen a very strong relationship between the content and kind of sugars in my meals. When very low in mono- and disaccharides, lactate one hour after meals were below 2. But when high, always above 2 and sometimes even 3. I discovered this when I reduced my orange juice consumption to lose weight. (BMI 26.3)
But I went further. When administering a glucose tolerance test at home, I measured blood sugar and lactate every 30 minutes. To my surprise lactate levels stayed low and relatively stable during the test. (And luckily, blood sugar ended up low too.) The next step was obviously to do the same procedure with the sugars found in orange juice. To make it easy, I drank a quantity of orange juice with the same amount of sugars as the glucose tolerance test, namely 75 g. And now lactate was indeed elevated. I reached a peak of 4.5 after 60 minutes. After 2 hours the level was down to 2.6.
So at least I know that one person, me, get high lactate from fructose. Perhaps this mechanism is so well known that standardized meals in a laboratory setting, consequently, always are low in sucrose and fructose?
Yours sincerely
Rune Nilsen
Dear Rune,
The elevated blood lactate in ME CFS, after meals may not be a big mystery.
Research studies from Henry Butt, Sheedy, Lipkin etc show higher levels of lactic acid producing bacteria in guts of ME patients (Streptococcus, Enterococcus)
These bacteria mostly convert carbs, sugars (fructose, lactose, glucose, dextrose, maldrextose or any “ose”) to lactic acid. This may be a possibility that high blood lactate levels show post meals in ME CFS, especially if high in carbs & sugars.
This may also explain why Keto helps some people with ME, because it largely eliminates carbs & sugars.
The elevated blood lactate in ME CFS, after meals may not be a big mystery.
Research studies from Henry Butt, Sheedy, Lipkin etc show higher levels of lactic acid producing bacteria in guts of ME patients (Streptococcus, Enterococcus)
These bacteria mostly convert carbs, sugars to lactic acid. This may be a possibility that high blood lactate levels show post meals in ME CFS. This may also explain why Keto helps some people with ME, because it largely eliminates carbs & sugars.
LDH is a sign of hemolysis, and hemolysis breeds fatigue, as evidenced in those with PNH, who manifest fatigue proven to be caused by hemolysis.
I’m one of those mitochondrial dysfunction POLG mutation, always high lactate folks. Ironically my variation is considered likely benign but it’s clear it’s pathogenic based on my experience. At this point chronically confused about what to do about it because the data isn’t there. I do IF and low carb, i have tried to focus on mitochondrial biogenesis and supplements. Still searching for answers.