In 2015, Dean Echenberg, MD, PhD, a former public health official and Director of Disease Control in San Francisco at the height of the HIV/AIDS epidemic, had a question. His own course of ME/CFS had been anything but smooth. Echenberg had experienced years of illness punctuated sometimes by years of complete remission. Echenberg wanted to know if others had had the same experience.
A survey indicated that he was not the exception to the rule. In fact, hundreds of people reported that they’d experienced substantial remissions and almost 50 percent reported that they’d experienced more than four remissions.
While these people by definition did not recover, something happened to them which dramatically, if temporarily, boosted their health – until ME/CFS came roaring back. Even with their impending relapse, the fact that they would able to make such inroads into this disease for a time is significant. I, for instance, have never, over four decades, found anything that significantly boosted my energy levels for a significant period of time.
With ME/CFS and FM being so stubbornly resistant to treatment, any data on anything that really substantially moves the needle on people could be helpful. With that in mind, we present two more temporary remission stories – and in an attempt to flesh out why people remit when they do – provide a poll.
A Surgical Surprise – Temporary remission story #1
She (Patient X) was 53 years old with severe chronic fatigue syndrome (ME/CFS) as well as fibromyalgia. Scoring about 20 on Sarah Myhill’s ability scale, and 15% on the AYME functional ability scale, she was getting progressively worse. She was able to sit up much of the time and could get around the house and be outside the house for an hour at a time a couple of times a week — but that was it. She met every ME/CFS criteria in the book.
Her symptoms included a horrible flu-like feeling that never went away, and an unearthly exhaustion which, as she evocatively put it, felt “as if her blood had been replaced with iron and the iron was being sucked down into the earth by a powerful magnet.”
Tests indicated she had exceptionally low NK Cell Function and a Mycoplasma pneumonaie infection that her Stanford doctor wanted to treat with antibiotics. She also tested very high for HSV-1, which will be treated with antivirals.
She believed the acute onset of her ME/CFS and fibromyalgia was probably triggered by three factors: (1) a long and difficult withdrawal from Valium (used for sleep); (2) repeated exposure to mercury vapor from poor dental work (strange neurological symptoms and paresthesia began 10 days afterwards); and (3) three concurrent sleep disorders. She was also diagnosed with attention deficit disorder (ADD).
She’d seen Dr. Kaufman at the Open Medicine Institute (to no avail), and Dr. Amity Hall, physician’s assistant to Dr. Montoya at Stanford, as well as several other doctors. She’d tried LDN, different diets, CBT, supplements, etc. Nothing had worked.
On June 29, everything changed during a 10-hour surgery during which she was given a raft of anesthetic drugs (Fentanyl, Rocuronium, Lidocaine 2%, Propofol, Cefazolin, Dexamethazone, Hydromorphone, Phenylephrine, Mannitol, Acetaminophen, Phenylephrine, Ondansetron (Zopfran)). The surgery did not correct anything possibly associated with ME/CFS or FM.
Surgeries can knock some people with ME/CFS/FM for a loop but the opposite occurred.
Upon awakening, she experienced euphoria and hypomania which transformed hours later into a state of alertness she’d never experienced before. More importantly, she had no ME/CFS symptoms and her fibromyalgia pain was gone as well.
The difference, she said, was night and day! After years of inactivity, she was, of course, deconditioned and didn’t have a lot of stamina but was able to walk regularly without discomfort. Suddenly she was able to socialize, take long walks, and check out the big box stores she used to avoid. She was like Lazarus rising from the grave.
Two weeks later – long, long after the drugs had left her system – she still had zero brain fog, was able to clearly articulate my thoughts, and was finally, for the first time in years, able to focus. After coping with ADD for years, her short-term memory was now excellent. The bone-crushing fatigue and the flu-like symptoms of ME/CFS were still gone. Her FM pain was mild and infrequent.
Instead of her usual gait problems, her legs were strong and her strides were sure, and she was taking “wonderful, effortless walks”. Instead of a “10-15” on a functional scale, she thought she was at about “70”. She said she could write pages about the difference between her condition now and pre-surgery.
Two and a half weeks after the surgery, her ME/CFS symptoms began to descend again. It took her several months to return to baseline where she has remained ever since.
As her symptoms crept back, she remained changed in some ways. Despite her cognitive shortcomings, she’d always had an insatiable curiosity. During her remission, it had became clear to her that her sharp intellect had simply been lying dormant. Knowing that left her more patient and more tolerant of her ADD issues.
The big question, of course, is what happened? How did a ten-hour surgery temporarily wipe away such a severe disability? What does the fact that it happened mean for her brand of ME/CFS?
It should be noted that studies examining the effects of anesthesiology have found only negative effects. Nothing I found described positive results from anesthesiology.
We turned to an anesthesiologist who could provide no answers except to say that she didn’t believe that Patient X’s idea that the propofolol was responsible for her remission was correct. (Patient X noted that propofolol appears to be able to aid memory retention.) The half-life of that drug is just way too short. The same was true for Ketamine which does have pain-relieving properties – which she didn’t receive anyway.
Pressure Dropping – Temporary remission story #2
Patient Y was a professional who contracted sudden onset ME 15+ years ago. Since then her functional capacity level has remained a steady 3-4/10. She’s been diagnosed with ME/CFS, FM and POTS.

Did a reduction in cerebral spinal fluid pressure relieve Patient Y’s POTS for three weeks? (Image by Jens P. Raak from Pixabay )
Her symptoms included difficulty being upright, difficulty reading for long periods, PEM, insomnia, headaches, dizziness, shortness of breath, muscle weakness and pain, and brain fog. She was also highly intolerant of and experienced sometimes paradoxical reactions to most prescription drugs, including several commonly used in ME/CFS (for instance, drugs designed to increase energy increased her exhaustion).
She’d tried many things that didn’t work out. Here is a partial list:
Creatine (to help muscles during exercise), Martin Pall protocol (ME), Cortef (energy), Florinef (POTS), Midodrine (POTS), Topiramate (POTS), Acetazolamide (POTS), Mestinon (POTS), lots of water with salt (POTS), compression stockings (POTS), LDN, glutathione, CBD oil (muscle pain, sleep), Myers cocktails (IV), Tylenol 3 with codeine (pain), carnitine (energy), biotin, inositol, magnesium carbonate, potassium bicarbonate, phosphatidyl choline, evening primrose oil, ribogen, lots of homeopathic remedies, Hawthorn, probiotics, NAC.
Her only real winner was hormone replacement therapy which put an end to the constant 10/10 migraine she’d had for over a year and which somewhat helped her brain fog. Other than that, her only other successes after 15 years of effort were sleep medications that helped her fall asleep (but did not result in refreshing sleep), magnesium, which helped somewhat with muscle pain (but not with exertion-induced muscle pain) and stretching, which mildly helped her improve muscle strength.
None of that prepared her for what happened after her spinal tap. Her spinal fluid pressure was, interestingly, not high when measured. (One study suggested that the normal spinal fluid pressure ranges may not apply to people with ME/CFS.)
Nevertheless, the change in her health was dramatic. Removing some of her spinal fluid resulted in a 3-week remission of POTS and, to lesser extent, ME/CFS.
For the first time since she became ill, she was able to clearly differentiate between her POTS and her ME/CFS symptoms. She still felt fatigue and pain after walking too much, but for the first time in years she had no need sit while at a store. The lightheadedness she often felt while standing disappeared. After having had to use a computer while lying down in bed, she could now sit up at a desk for hours. Her brain fog had substantially lifted and her mind felt clear.
The POTS and partial ME/CFS reprieve lasted three weeks and then disappeared. Noting the changes the spinal tap had evoked, her doctor tried Topamax, which produced another of her strange reactions: instead of energizing her, it put her into a coma-like state. She’s been back to 3-4/10 functionality ever since.

If you’ve experienced a dramatic (but unfortunately temporary) improvement please tell us what happened in the poll.
Your Temporary Recovery/Remission Story
Do you have your own temporary remission story that lasted two weeks or more? Total recoveries are not necessary but dramatic improvements are – say 4-5 points on the IACFS/ME’s functional scale.
If you’ve undergone dramatic improvements which temporarily dramatically improved your health, please let take the poll. We’ll put together a report which focuses on the treatments which worked, how large the remissions were, etc.
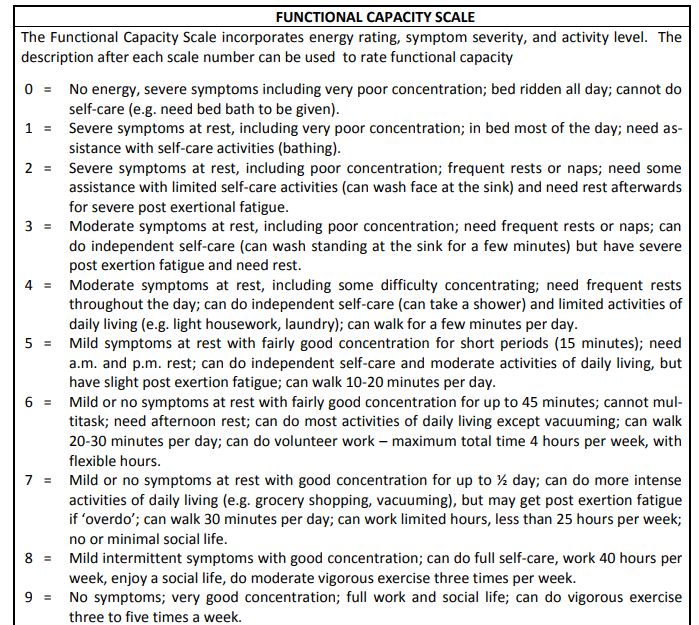
Functional capacity scale from IACFS/ME primer. Dr. Alison Bested © Dr. Lynn Marshall. May be copied for individual use.







Mine started out as Mono infection- Also I am a Dental Hygienist and came in contact at that time with Mercury on a reg basis. I developed boils under my arms and in pubic area. Pain all over and weak spells. I also notice I could not think at all or reason at all. I was also diag with CMV by an excellent dr in Atlanta who was doing research on Aids at the time. I was able to go back to work after about 6 mo part time. However the Co Bayer sold their Immune Globulin formula to another co and they changed it to Generic. It never worked for me. I took the Injections weekly. Also HydroyCobolomine B-12 injections. I have never been the same since I quit taking these meds.
There’s a scary book on generics which is on my list…
Most generic components are made in India or China with poor oversight from the FDA.
That’s my understanding.
To me- I do not feel we are going anywhere with the drugs to help us. These 2 drugs the Immune Globulin (Brand) injections changed my life in 3 weeks I started to improve. Why would it be changed when it was helping so many people? There would be a line of at least 10 people every time I went in there to get shots. This was in 1987. This means the help has gone down not up for us. I don’t get it. I am much older now and still trying. Stress knock s me out as I have no reserves.The Dr that treated me in a987 was Dr Richard DuBoise. Just wonderful. I have seen Dr Cheney when I was better. he is now retired. What is the answer? I am on a Gluten restricted diet. Sometimes helps-Sometimes doesn’t. We need more Dr in our area to help us. Love the Health Rising site. Thank you.
I have not found any doctors who treat CFS/ME in metro Orlando. My doctor gave me a referral to the Jacksonville Mayo Clinic for CFS/ME but Mayo Clinic’s facility for CFS/ME is in Rochester, Minnesota not Jacksonville, Florida.
I would recommend finding a Naturopathic Dr. They all know about ME/CFS and could help you make sure you are getting the nutrients you need to supplement your diet especially if you are restricting gluten. You can find one to interview near you here: https://naturopathic.org/search/custom.asp?id=5613
Bob Cassels, I think most would say steer clear of Mayo for ME! But Nancy Klimas’ Institute for Neuroimmune Medicine @Novasoutheastern is in Davie, Fl. They are ME specialists.
For the last couple of years I’ve been periodically experiencing boils in my pubic area. Very embarrassing. Along with the pain and weak spells and inability to reason. Had not read that this was ME/CFS related (or is it from mercury do you think)? I also have chronic mono.
No way on earth I’d try to take that constellation of symptoms to my Dr. I’m sorry you’ve experienced it, but It helps considerably to read that I’m not the only one.
Mono is the Epstein Barr virus and CMV can sometimes be with it. I do plan to see a naturopathic Dr. They cannot do RX here in Ga. but I have found one that he is in with an MD and he is supposed to be excellent.
In terms of pubic area skin issues, check out Behcet’s disease. That might be applicable.
I would be interested in volunteering in any new clinical trials, if applicable.
I did hear there was a good Dr in St Petersberg a few years ago. I do not know whether he is still practicing or not. I had thought of going there. I have property in Jax Beach. The Mayo offered me nothing there.
Dr. Daniel Dantini helped me tremendously. He practices around Ormond Beach, Florida. I traveled from out west. I went into remission after seeing him.
Dr. John Hudson in Winter Park treats CFS/ME.
Cort on the Generics- Dr will not listen when you say I cannot take them. It is getting where that is all there is and we do not know who the real mfg is or where they come from. Now my pharmacist says-” This is a good Generic formula”. Which means safe? I had also been taking Zantac for at least 3 years brand name as I had Esophageal issues . When they took it off the market saying it had ingredients that cause Cancer -I was very upset. I have had a bad Cough for at least 3 years. Well guess what folks-I have quit taking the Zantac at all and now take my cough is completely gone????? I am taking Over the counter Pepcid. I also did have Breast Cancer but it was taken care of Stage 1 with Radiation only. The Zantac issue just blows my mind. I had 3 Endoscopies as I would be choking from coughing. I am still afraid of Generics though. I do know some people that are taking Hemp oil in the Denver area that say the pain is better.
Hi Carole,
Your comment about the Zantac caught my attention. I had a look at the ingredients list and microcrystalline cellulose is on it.
I seem to remember Issie commenting on another blog (I can’t find which one) that she had some sort of a reaction to microcrystalline cellulose. It comes from trees.
I had a terrible coughing episode after eating a Rennie antacid. I seem to remember it had talc in it.
I developed asthma as part of my collection of ailments over 5 years or so ago. I don’t wheeze – my lungs clamp shut and fill with mucous. So I would be very aware of my lungs being triggered.
However, having said that, as I am seemingly managing to bring my general level of inflammation down my lungs are much better.
I have a peak flow device to check my ability to breathe out. My doctor also checked me a few months ago. I wasn’t particularly focussed on my lungs at the time but my peak flow had improved.
I am also on a CPAP- Sometimes it does help with breathing as I get Ttacycardia otherwise. But I cannot take a high pressure. All of the Dr argue I need a high pressure . They go by the standard not individual needs. I also have a elevating bed with the head up and that helps keep the tacycardia down . I do have a problem also with Antibiotics making me sick. Have a low dose is all I can take of Ampicillin (Brand). Now they have found out I have an Iron count going up?????
What about the research in Birmingham Alabama. It has been going on a few years? Dr Younger?
Younger is doing great stuff! Tackling neuroinflammation and checking out possible immune cell infiltration into the brain as well as researching botanicals and, from what I heard, a potentially much more powerful form of LDN called dextro-naltrexone. I’m sure he’s got other things going as well.
Neuroinflammation I think is the most likely explanation for CFS at present so it will be interesting to follow the research of Younger, Miller and the Japanese.
Several studies show that in CFS our cytokines are elevated early in the illness after a viral shock, but eventually return to normal (or go lower). I reckon there’s a ‘hit and run’ at play here, the high cytokines turn on a neuroinflammation switch that stays ‘on’. This means that we have higher levels of cytokines in the CNS, but not the periphery.
Cort, is Younger doing proper trials or is it just experimental?
I don’t know how extensive his trials are. He’s been testing multiple substances – I’m not sure how he’s doing that. It does seem to be a new approach, though. My guess is that these are exploratory effort intended to identify substances which can then get a more comprehensive trial.
That’s just my guess, though.
I have also heard the
re is a Orthopedic MD there that is treating some of his patients. Said he is very good.
In the Temporary Remission Story #1 I absolutely love how she describes her fatique, “as if her blood had been replaced with iron and the iron was being sucked down into the earth by a powerful magnet.” How bitter sweet the temporary remission.
I had 3 ME/CFS remissions 1) using a CPAP for sleep apnea and lasted a month 2) using LDN and lasted about 3 months 3) using low THC – CBD oil lasted a month.
Maybe the body is “shocked” and “resets” after starting a new drug, diet, hormones, surgery, etc. Although, the remission time is short lived.
Judi, I’m interested to know with the CBD oil if you’ve ever tried it again after it stopped working for you?
Some people recommend a monthly break of 3-7 days and then it begins being effective again.
Sue, I am still taking the low THC/CBD oil daily it does help with my pain. Experimenting at present with different strains of CBD and adjusting the dosage in hopes of helping the other symptoms. The biggie is PEM (will we ever find relief for that symptom?).
I’ve used it non stop for 4 years for pain and only recently had to adjust the dosage up slightly as my neuropathy gets worse. So why would you suffer for a week when you don’t need to? If it appears you are having to increase the dose a lot then yes, skip a day or two but I haven’t found it necessary
Something is happening. I used to regularly get great help from all sorts of things which would last as long as it took for me to feel really good and then my body would just fall apart. I wondered if energy production was releasing some toxin into my system.
Cort that is a good point! Just when we thought we could be onto something it brings us to our knees. Again. And then I feel very toxic, very sick when that happens!
Yes, exactly what used to happen….I would just be getting these wonderful feelings of energy and relaxed muscles and Bam! these bizarre, never experienced by me before, symptoms would start. Then it would just be a case of diminishing returns: less positive effects from the treatments and more negative ones.
Cort could be the formulation of what you are taking. Nothing with sugar or coating helps me and does just the opposite. Even cough medicine or vitamins. Also since I had the Breast Cancer -NO estrogen of any kind. it is in everything. Same with coloring.
I had the same experience of iron with the big magnet a few times. Quite powerful, very clear memory of it.
Interesting on the body being shocked and resetting. The Immune Globulin just jump started mine and kept on keeping it going. I also use a Cpap Machine. They can work great then not work at all. Great Post.
I got subcutaneous immune globulin and got very sick from it. After 3 treatments, I had to quit. I get paradoxical reactions to many of the CFS treatments. LDN almost killed me, or at least, caused so much pain, I did not want to live.
Question.. have any middle aged men with cfs found any relief with testosterone or hormone therapy?
I have heard it can help.
I Cort my body paralyzed left side can’t walk or move after so many infection and over bike riding is it happens to any one please suggest medicine I am from India
Sorry my body get totally numb weakness in nerve nueropathies or nerve dimaged can’t tell beacause no medical help do you know in India who is expert in cfs doctor
Some ME/CFS patients have found that the medication Ativan helps their extreme weakness and intermediate paralysis. Some start on a very low dose. But if you take it too often you can build up tolerance to it, and you keep needing to increase the dose. So taking it only on an “as needed” basis is best. (Note: I’m not a doctor and this is not medical advise.)
For sure some people do. Nancy Klimas’s models project testosterone as potentially very important protective agent. It wouldn’t be “the thing” but it could certainly help. My last results found low testosterone levels….
Hi Danny,
I tried and there was a temporary bump until it got worse. Once I found out the root cause was malabsorption due to pancreas damage (exocrine pancreatic insufficiency, pre-diabetes) with subsequent nutrient deficiencies and tackled that, my testosterone level more than doubled to healthy levels. Have you looked at your nutrient levels, any malabsorption issues, blood sugar control, HbA1c levels, and taken a honest, hard look at your diet?
PrimalPancras,
Can I ask how you tackled it? “malabsorption due to pancreas damage (exocrine pancreatic insufficiency, pre-diabetes) ”
I can tell that’s going on for me, but only have access to an allopathic doctor, who’ll only cover basic tests, and doesn’t really believe in this stuff. Would love to know what you did.
Hi Anne. I sent you a message and will create a post to hopefully be of help as there is a lot of info.
I am going to be check for malabsorption issue and also Pancreas issues . I am going to see a Gastro Dr. . Very interesting you hit on that. I also cannot take some of my Vitamins that used to help me. What test did they do for you to find this? Also weight loss.
Primal Pancreas do you think your pancreas is physically damaged or do you think that it is not receiving the correct signals (for example, acidic pH) required to produce the digestive enzymes? I also have pancreatic enzyme insufficiency but I am not sure if there is an underlying cause that could be addressed.
Hi Karen and Carole Rushing. Sorry, just saw your questions. I tried to send you a message through the forum. Please contact me there with any questions. I also created a thread on exocrine pancreatic insufficiency and malabsorption in case it can help you and anyone else. https://www.healthrising.org/forums/threads/malabsorption-nutrient-deficiencies-pancreas-damage-exocrine-pancreatic-insufficiency-epi.6308/
Thinking about anesthesia triggering a remission… possibly the drugs shutting down some area of the brain, like fight or flight or ? Brain no longer sending out a lay low signal to the body. ??? Prenatals and B12 shots are helpful for me, but Somatic Therapy was very powerful. My Somatic therapist moved further away. I’m thinking after reading this that I should try weekly ST. Finding a good Somatic Therapist is difficult.
This is an interesting thought. I had an anaesthetic last year to have my wisdom teeth removed, and when I awoke I remember feeling completely calm and still- without the constant anxiety I sense of dread I otherwise battle daily. It was very pleasant!
Separately, I have also suffered a bizarre remission- I have been ill my entire life (strong genetics component and everyone in the family ill unfortunately), yet after a particularly stressful time and crash at 26 years old, one day I had an odd ‘draining’ sensation from my head. While fatigue remained, for the next 12 months all other symptoms cleared up- no anxiety, no gut trouble, no trouble sleeping, no ADD symptoms, no feeling out of breath. It was like everything started working for the first time in my life, and I feel I only felt tired because my body was slowly healing from all the damage. I didn’t mind the fatigue so much without all of the other intolerable symptoms. Unfortunately it didn’t last and after 12 months the symptoms started creeping back in. It was the best 12 months of my life!
Isn’t that something! Dental anesthesia does the same for me – I feel calmer and more alert for awhile.
Doesn’t that draining maybe sound like the cerebral spinal fluid flowing normally for awhile – carrying the toxins away from your brain?
Your comment re your head “draining’ caught my attention – I haven’t ever heard anyone mention it before – I experienced the same thing! I consider myself more or less miraculously recovered from ME CFS.
After two exposures to toxic mold, I was diagnosed 2 years ago by a former CDC doctor at UCLA after I came down with mono (CMV virus) that didn’t go away. I had all the classic ME CFS symptoms and after a visit to Dr. John Chia, took Equilibrant, which helped the mono symptoms, but then became more or less bedridden with horrific PEM for months.
One morning I decided to try VSL#3, a medical grade probiotic for IBS, and I felt different within a few hours, I was able to get out of bed. By afternoon, though exhausted, I could tell my fatigue was different than before.
That evening, I too had the odd draining sensation – I remember waking up in the middle of the night and feeling like I had to sit up to let the fluid drain. That night was the first night I actually felt like I had a good night’s rest with refreshing sleep. Previously, I also had a constant pain in the right side of my neck (felt inflamed) that went away.
Over the next months, after taking anti Candida supplements and a second probiotic (PrescriptAssist), I slowly got better. At this time, I was well enough to travel to see Dr. Jose Montoya at Stanford and he prescribed antivirals, but never ended up taking them because I continued to get better with the supplements I mentioned. Today, I am not quite my old self and continue to have food intolerances, issues with vitamin/iron absorption and minor memory issues, but currently I have no problem living a normal life and going to HIIT classes at the gym.
Whoa!
You are in the gut subset for sure. Thanks for sharing that. I’ll be contacting you with a email to see if we can flesh out your story more.
Congratulations!
I have been thinking about brain congestion, like nasal congestion and so on.
If inflammation is present, which causes even a small amount of swelling, then that is likely to block fluids from passing through.
Within an inflexible structure like the adult brain, if the amount of cerebral spinal fluid increases, then something else may have to accommodate the space this extra fluid needs.
I constantly monitor my brain function myself, as it fluctuates, depending on what I am consuming – foods, medications.
I believe I have MCAS and just about every part of my body can be affected, if I trigger it.
If I get a congested brain, then my balance is affected – if I turn my head from side to side then it feels like my brain is swooshing around inside my skull. I can’t think straight, my memory’s desperate and my eyesight can become blurry and I can have difficulty focussing, particularly in my left eye.
It seems to me that the brain is sort of off limits. I like Jarred Younger’s approach – I heard him bringing the brain into the conversation – like having other inflamed parts of our bodies.
I was looking up hydrocephalus and there are all sorts of causes, including apparently infection.
This illness (these illnesses) has been so misunderstood and neglected for so long, I think that as research picks up, all kinds of symptoms will be identified.
Interesting comments Gemma and Cort.
Sorry to hear the reission didn’t last..
I don’t doubt that anxiety I experienced exacerbated symptoms and I began to notice that I felt better when I experienced periods of feeling calm.
Science tells us that when in this calm state, the body can heal, produce and store energy, the digestive system works efficiently, we achieve better quality etc.
As a practitioner, I have worked with many clients who recognise that stress exacerbates symptoms, but don’t link periods of feeling relaxed – whatever the trigger for that, with feeling better.
It may be that that is internally generated, or the result of feeling better due to some other intervention, be it supplementation, medication or other intervention.
So that may be a factor to consider.
I used to feel serenely calm and better after cranial osteopathy, acupuncture or massage for a few days, but then would slip back into bad habits of anxiety. Breaking these patterns made a profound difference.
I have had several episodes of ME/CFS, each time being a bit less able to adequately bounce back. Most involved viral onset (I think), but my unbalanced hormones seemed to be a contributing factor. I was probably a sub-clinical PCOS girl and so late in life the addition of HRT really helped put me near normal energy.
In addition to the passage of time which has helped in getting mild remissions from various episodes, eating a simple farmers market diet (mostly vegetables) and taking daily walks also helped me make noticeable improvements.
Since I have a tendency to slip into iron anemia, taking supplements for that I think has helped as well.
Lately my fatigue has gotten much worse and so I re-checked for the ‘low hanging fruit’; diabetes, anemia and thyroid.
Now, usually doctors only do a TSH for thyroid but there is a controversy about that test not being the full picture. I got a full thyroid panel recently and even though my TSH has always been in the ‘normal’ range, I discovered I had high antibodies! That triggered an ultrasound of my thyroid where it was discovered I had nodules. Technically that gives me Hashimotos. Still I test within normal for everything else excepting I have severe fatigue and hypothyroid symptoms.
Now M.D.s are of two minds about this. Most want to see your TSH out of range before they will treat. Unfortunately, your body can be attacking the thyroid for years without that happening. Functional medical doctors want to start levothyroxine as soon as they see significant antibodies with symptoms.
I have had an argument with my new endocrinologist because she did not want to treat me as my TSH was still within ‘range.’ Eventually she capitulated and gave me a tiny dose and said that it probably wouldn’t make much of a difference. After several weeks I am noticing a slight bump of energy, so time (and perhaps an increased dose) will tell.
I’m only mentioning this because a ‘normal’ TSH can fly you under the doctor’s radar. If you have some of the symptoms of thyroid issues in addition to fatigue and PEM, I would recommend that you try to get the full range of tests!!!!
Nancy B, get rid of the endo and go with the functional. Any doctor who still thinks that only total TSH needs to be tested is living in the mid-20th century.
A full panel is so much more revealing. You should also be taking T3 in addition to the T4.
I so agree with this. Lots of information regarding this on the Stop The Thyroid Madness site/book.
For many years I had adrenal insufficiency and Hashimotos but it went undetected by the NHS. However I was fortunate to find a knowledgeable private Endo who also conducted tests and said that I needed both thyroid medication and also hydrocortisone.
Turns out I am a carrier for Congenital Adrenal Hyperplasia which explains the severe adrenal issues I have had for so long but weren’t treated.
I still have ME/CFS but as long as I rest sufficiently and don’t pick up too many viruses I can have some good energy but it will always run out quickly. Everything changes though when I get a virus and then I have a very limited life again.
Traditional doctors are pretty useless about treating the thyroid in my opinion and experience.
Check out a couple of blogs on the T3 issue and another thyroid subset:
https://www.healthrising.org/blog/2019/03/07/thyroid-t3-chronic-fatigue-fibromyalgia-recovery-stories/
https://www.healthrising.org/blog/2019/03/04/hypothyroid-chronic-fatigue-syndrome-thyroid-ntis/
@Brighid and Pam C,
I am totally on board with getting a new doctor if this one doesn’t work out (that is, doesn’t increase my dose at our next meeting in about a month). I have gone on a blitz of thyroid research and am familiar with Stop the Thyroid Madness. Thank you both!
Now Pam, I think it interesting your mentioned CAH because it presents very much like PCOS. I’m assuming yours was considered ‘mild’ or ‘non-classical CAH.’ Genetically the variant for it sits on the TNXB gene right next to the place where the variant for a rarer sub-type of Ehlers-Danlos is; Tenascin-X EDS–and it is known to interact with the adrenals. Might you have signs of Hypermobility too?
@Gemma,
Regarding your experience with anesthetics, I noticed a very positive experience in PACU after the doctor used ketamine during the surgery. Some medical pioneers are experimenting with nasal ketamine for both pain and depression. Hum…
I also see I am not the only one who has progressively more severe lapses into CFS with small recoveries in between. Seems as if the immune system is struggling (and mostly failing) in some of us.
@Cort,
I think this is a brilliant question; ‘what has worked?’ Perhaps it is my imagination, but I see a very slight pattern… Thank you for all your efforts!
I absolutely agree with Brighid! Even with the correct testing I suffered for years B4 a Naturopath prescribed me T4 &T3. Made a huge difference on the same dosage. (PS Endos are useless like most conventional medicine Drs. They are trained by Big Pharma and can’t see the forest for the trees.)
I also have PCO, can You explain what.kind of.hormonal therapy you get? I think.hormones play a.huge role in my medical picture, thanks
Nancy regarding signs of hyper mobility and CAH yes I am hyper mobile with many of the symptoms of EDS but I wouldn’t consider it is full blown but more subtle in my case.
Also I was one of the CAH carriers who didn’t get symptoms till after the birth of my third child when I was around 28. It was a gradual thing but got far more dramatic after that third birth in 1979 when I actually lost 4 pints of blood immediately after childbirth during a D&C. I was never the same after that but it was 4 years later when I had 2 weeks of flu and couldn’t recover. After that the symptoms of low adrenals started with extreme vertigo attacks which went on until 2002. The vertigo attacks were accompanied by severe migraine and they completely changed my life.
Perimenopause completely finished me off and it was during this time I was given the diagnosis of ME/CFS because of all the symptoms I had. To be honest I still don’t know if its just the CAH now that causes all my issues and/or that I do have ME because I still run out of energy very quickly and have to spend much of my time horizontal. I definitely have POTS though and am helped by small amounts of Fludrocortisone on some days plus 6.5 mg Prednisolone.
My thyroid is treated with 1 1/2 grains natural desiccated thyroid plus 0.25 mag thyroxine but the NHS Endo originally said I didn’t need anything for it. Once treated I lost 2 stone in weight and have stayed slim.
Hope you do get some proper treatment to help you to feel better.
This is really interesting on the TSH test. I had taken a Thyroid compounded frm Dr Cheney years ago and it worked wonderful. He did a heavier thyroid panel then. Had really forgotten about that and also the fluid drainging from the brain and your head being stopped up. Makes sense.Dizziness?????
Thank you for that post!!!
Our daughter gave me a Fitbit for Christmas. This is a great tool for the more moderately affected patient. I learned quickly that I could walk 3000 steps in a day, but 5000 put me over the edge. Also my heart rate could swing from 58-60 at rest to 150 when walking moderately. Not sure what this means, but I think it may be important.
I just got one too. Fascinating device. Really interesting regarding the sleep stats. Some day I hope to reach 7 hours of sleep at least once 🙂
I have had several remissions and relapses from HHV-6, EBV and CFS With each recovery leading to a deeper CFS illness. Once my infections were finally cleared (prior to an understanding of the infection connection I would sleep most of my days away because there was “nothing that could be done”. This has been going on since childhood. ) I did gain energy and more of a life but the CFS has been progressive. Every relapse has set me back further. At least the infections are no longer a problem (well I do still have high titers to Varicella Zoster and HSV2) but they aren’t a driving force. During several remissions I was again able to bike ride and hike but Today I can only walk 10 minutes at a time maybe 3 times a day with housekeeping very difficult. I now consider myself completely disabled.
However, I went undiagnosed for decades and did push my exercise during those decades enjoying life and sleeping for long stretches of time until energy returned. I believe that hindered long term recovery. I feel like I’m aging very rapidly, now 59, I do less than my 89 y.o. father. During the past 1.5 years IBS has set in. I’m doing better on a FODMAP diet.
The HHV-6 was crazy making and must have been reactivated by Enteroviruses and EBV. I still have high titers to Coxsackie B4 and an echovirus strain. So I’m better -clearer head, but physically weaker.
Valganciclovir did not clear my HHV-6/EBV infections but Rituximab did. However I got too many infusions and it collapsed my immune system. It took mamy years for immune recovery and I have never been the same. For patients who can’t seem to clear infections I recommend only 2 infusions, not 4.
Acupuncture helps.
Other thing that help me are: AHCC; magnesium, doxepin, Lunesta for sleep; omega 3; red marine algae; vitamin D. I tried LDN but could not tolerate and hope to again try it now that my IBS has healed to a greater degree.
How could I forget, I also take plaquinel and colchicine daily. A severe relapse last year I contribute to stopping the cocktail because after two years I wasn’t getting incredible energy. Little did I know it was stabilizing me. But after a year on the cocktail I’m better but not as well as before the relapse.
It was surreal when my constant need to lie down went away all of sudden in 2016 after 8 years of wallowing. This was when I was spending 8 hours of my waking time lying down. I understood then why people disabled for years cry when they finally stand up on their own with help of a robotic chair.
Looking back, that was the beginning of my recovery even though the reprieve went away and I went back to the life in horizontal position within a few months. Now that I’m regularly sitting up, except when I’m having PEM, I don’t think too much about it. It’s rather anticlimactic after 12 years of drama. I still ask though: how is it even possible for someone to be so sick, so long?
About 40 years ago my doctor gave me a shot of adinosin phosphate ( spelling?) and it worked immediately and I was well for years. She also told me she could no longer get it because it was being taken off the market. Does anyone have any information about this drug and has anyone looked into getting it back for CFS patients?
https://www.webmd.com/vitamins/ai/ingredientmono-1067/adenosine. ATP is used for heart issues and that’s probably why your Dr stopped using it! Interesting that it helped you though!
It’s not anything I’ve taken but for me the only times I’ve felt the ME has gone temprarily, or at least gone into the background, is immediately after I’ve recovered from an infection. Last year I got the norovirus and the next day I woke up without the usual “flueyness” and with a lot more energy and strength. It lasted about 10 days before the ME symptoms gradually came back. I used to have the same thing on recovering from a cold (in the days when a cold used to come out as a cold when the ME was milder). Then it would only last for about a day. During the Australian conference, didn’t Ron Davis mention that his son improved for a while after having an infection? I wonder if other people have experienced this too. It does seem to point to the immune system.
Hi Nicole,
I had an interesting experience last November. I developed a cold – a proper one – with streaming nose etc, which hasn’t been happening for a good while.
I’d usually be brewing something for a week or so – but nothing would actually come out – it would just disappear.
However even though I felt miserable, I could feel that I had more energy available to me. Now I was doing a bit less because if the cold, so that could have been a factor but I just felt like a normal person with a cold. It was significantly different enough for me to notice.
I’ve been living with ME/CFS for 40 yrs and seem to be of the remission, relapse subset. Thankfully, most of those 40 yrs I was in remission with only minor relapses.
The last 16 yrs however have been worse relapses and not so good remissions. I’ve had 7 remissions since my teens, varying in length and wellness. The remissions sometimes seem unpredictable as well as the relapses.
Like Nichole, I too went through a phase of not coming down with colds etc when my husband/children had them.
But the last couple of years, I’ve caught them too. I just had a chest infection and some antibiotics which helped very quickly to clear it. Then I had a week of almost remission – I went to the hairdressers!!! Now I’m back to usual – mostly housebound.
I saw a doctor today (NHS) as I was concerned the infection had returned – I was coughing so much at night I can’t sleep and ventolin (asthma reliever) not making any difference. She confirmed my chest was clear and commented that people with ME/CFS often seem to feel better while on antibiotics and for a little while after. I’d never heard that before.
She was a locum doctor and seemed to understand that this is a real illness and not much is understood about it. It shows how we struggle with doctors’ attitudes that, although she knows little about the condition, because she affirmed it as a real, debilitating illness, I wish she was my regular doctor!
Has anyone else experienced short term improvements when taking antibioitics? I know we can’t use them much because of superbugs becoming immune to them, but it’s an interesting avenue of thought for researchers.
Also, does anyone else have asthma-like symptoms (tight chest, feeling that you can’t get enough breath inside you and coughing when lying down) that aren’t relieved by asthma inhalers? Is this to do with muscle problems – it feels like my thorax muscles are going rigid on me and squeezing me, like my clothing is too tight.
If your CFS is being caused by an undiagnosed infection (like tick born diseases) then it makes sense that you would feel better after knocking them back for a few days with ABX and once you stop they regrow and whack your immune system again. If you want to test the theory try taking the herbs Cats Claw and Otoba Bark at the same time. The combination works as well as Doxycycline on Lyme and other TBDs. If you feel worse it’s called a herx and it’s because you are killing the bugs too fast. Google treatlyme.net and herx for more info. These herbs won’t hurt you if you aren’t sick.
Thanks for the Otoba bark idea.
Hi Rose,
I developed asthma over 5 years ago – I can’t actually remember when!
I kept saying to the doctors that I was having trouble breathing. However I don’t wheeze – my upper airways are less affected. It’s lower down – my lungs felt like they were very heavy. I couldn’t lie down on my back or my side at night. I also developed a sharp little cough.
I recognised this as being similar to a cough my neighbour’s little boy had, when his asthma was triggered.
So I suggested to my doctor that I might have asthma. He gave me a Ventolin inhaler and I bought a peak flow meter. On taking the Ventolin my peak flow improved by 50 points. I was down to 325 and went up to 375. He said I was very unusual – most people wheeze – only a very small percentage don’t wheeze. I believe I was living with a continuous asthma attack for ages, which was made worse at night.
It took me years to find a preventer – corticosteroid – that helped. One of them Symbicort – has milk in it! Seriously they have no idea ? I think the Symbicort may have been making me worse.
Anyway many years later, my lungs have settled down and my peak flow had improved to 440 L/min. I rarely need to use my Ventolin now, though I do take my preventer twice a day.
I’ve also been trying to reduce my overall inflammation and not trigger my myriad of symptoms, especially my brain and heart, which I think has helped calm my lungs down.
Also one of my neighbour’s has been saying for years how she couldn’t breathe at night. She was tested for sleep apnea and had a thing to stop her lying on her back.
However recently she went to stay with a friend and it all cleared up. When she returned home, her breathing difficulties started up again. A new mattress and pillows has sorted her problem. She was reacting to her old mattress and pillows and what they contained!
T Allen – thanks, I will look into Cats Claw and Otoba Bark.
Tracey Ann – thanks for your input. My difficulty is that, although the preventer inhaler definitely reduces my asthma-like symptoms (symptoms increase if I decrease my meds) the asthma reliever inhaler doesn’t seem to have much effect. My peak flow seems to vary without any connection to using the reliever. Also, the constriction is in my throat as well as lungs.
Perhaps it’s time to talk more candidly to my asthma nurse about this. My next check up is due soon. But I get jittery about giving any more detail (especially if it’s ‘non standard’) to NHS medics. They have such rigid rules from on high about what can be prescribed for what and which symptoms you have to have to get anything. I could end up being denied the inhaler that helps! I’ve had such things happen before.
ME/CFS is a ‘non standard’ illness and we seem to exhibit a lot of ‘non standard’ symptoms. My experience is that if the symptoms don’t fit any known definition, they are ignored.
At the moment there’s a catch 22 situation. Either a doctor ‘doesn’t believe in’ ME/CFS and therefore does nothing (if you won’t have CBT, or have had it and it didn’t help). Or they do accept it as an organic disease but know there is no effective treatment (as yet) and therefore still do nothing.
I also get doctors saying, “You have ME/CFS, you have to expect to get lots of symptoms. You need to rest.” with no further exploration or testing (because it’s expensive and NHS is struggling just now.) Everything I say is put down to ME/CFS (for which nothing can be done). There may be other conditions at play, so I think this is just as dangerous as assuming it’s all psychological!
One day, I believe we will understand this illness, and there will be effective treatments, even a cure – or even prevention! It will be like the many other illnesses we’ve conquered. I await that day with great excitement! I’m praying for and cheering on the researchers every day.
Thank you Cort for this site. Thank you so much! I know you get some unappreciative or unhelpful comments sometimes, but this site is what gives me hope and keeps me praying and believing for progress! Please keep it up, it really does help.
I have had this thing of ours for almost 30 years. It waxes and wanes on its own. The people who develope a real cure for this disease will get a Nobel Prize. Until then anyone who tells you they have a cure is a quack and there are a lot of them out there. So until that Nobel prize is awarded be careful.
Your best bet is to find a doc who will listen to you, take your symptoms seriously and investigate them to make sure they are not being caused by an actual curable disease, and if they find nothing, will do their best help live with it.
So well said. Thank you. I wish I’d known that when I first came down with this in 1995.
Boy, we may not know what is going on with ME/CFS, but if there’s one thing we’ve learned over the past few years its that a good doctor who will check for everything is essential.
Cort,
Anecdotally and retrospectively I have determined Singulair MAY have provided a benefit to me for months before I stopped taking it. I started it for post nasal drip, I was able to sleep and exercise and do cognitive training apps regularly. I stopped taking it because it seemed like it wasn’t doing much and I reverted back. I only determined the POSSIBLE connection after reading a question to CFS Doctor Sue Levine and she commented about how a trial should be done with the drug. I vaguely recognized the drug name and I had been on the drug and realized it was around the time I felt better. Do you know of any connection or rumors around this drug and some people improving or any theories about how it might? Any info you may have would be appreciated
I take Singulaire for COPD (and also have ME/CFS). It has no positive effect on my ME symptoms. Probably it helps my bronchial problems a bit, but I don’t notice any real effect when I forget for a week to refill it.
Whoa! I have never even heard of that drug! Wikipedia says
” Montelukast is in the leukotriene receptor antagonist family of medications.[2] It works by blocking the action of leukotriene D4 in the lungs resulting in decreased inflammation and relaxation of smooth muscle.[2]” I can certainly see how relaxing the smooth muscles in our blood vessels might help.
There’s a mast cell connection – It may also be used as an adjunct therapy in symptomatic treatment of mastocytosis.[7]
Very interesting!
I’ve tried it twice (I have AERD, asthma, severe allergies and chronic sinusitis) and both times it made my asthma And ME worse.
(There’s just so much complexity with this illness, what helps one person harms the next and vice versa)
Like Remission Story Patient 1, I awoke from anaesthesia but after a colonoscopy, and felt like the pre ME me. For the entire day, I had pre-illness normal energy, no pain, mental acuteness, no IBS. But then, the following morning, I awoke with the regular pain.
I’d thought maybe the “remission” was due to the IV saline I’d received. A doctor of mine opined that it was the effect of the aneasthesia, which for me was very positive.
Again, it only lasted till the next day.
II think the ME activist (which is EVTREMELY important) is going in the wrong direction – ME is absolutely fatally real and concrete but the causes are many, and looking for a cure-all will not work – it can be a hidden infection, it can be hormones, it can be environmental toxins, it can be too many things (all equally non recognised by idiotic allopathic medicine).
I never see anywhere in ME groups mention of Igenex/Arminlabs that do the only remotely reliable test for Lyme and confections. Most people with ME never tested properly.
Parasites are hardly ever diagnosed, unless one seeks a veterinarian (many stories about that). It s important that ME and fibromyalgia are recognised by the system and given some necessary help, but with that approach you are never going to find a treatment.
There are plenty of treatments for most cases, you just need to look for the cause. To say like I heard several times “there is no cause” it’s just lazy.
Cort I thought there was some suggestion years back that CFS quite commonly remitted in pregnancy.
Was that a false dawn?
No I had a complete remission in both of my pregnancies. Also during lactation. There something there. Hormones maybe or immunity being suppressed. I wish I could replicate it.
Thanks. Would be good then if we could find out why! It sounds like it happens quite a lot
This article looking at pregnancy remissions in autoimmune illness suggests it’s immune factors at play rather than hormones.
Fascinating stuff, but it would be even more fascinating if it led to treatment!
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2709983/
I had relapses during both my pregnancies – another ‘applies to all’ theory bites the dust!
I know this is an older thread but I have been looking for other remission stories. I don’t know if my story can help anyone, since I can’t really explain it, but I wanted to share because the fact that I could experience this, even briefly, gives me hope that our systems are ‘turned off’ rather than broken. Thats how it felt to me, like a switch was flipped.
I have experienced a few periods of what I call remission, a couple lasting 2-3 months (typically in the fall/winter, and one long, awesome period of feeling great after coming off a 5-day 103+ fever), and others of just a couple random days here and there. But I call them all remission because of how very DISTINCTLY DIFFERENT I felt during them. The main thing was, I was able to work hard all day then go home and do chores, and at night I just felt the wonderfully satisfied tiredness that I remember from before ME/CFS. Yes, tired and muscles aching, but SO different than the fatigue feeling I have the rest of the time – it’s how one ‘should’ feel after exertion. My sleep was even better during those times, and I woke up early and refreshed. I remember remarking several times how truly NORMAL I felt. I’m a very hard worker, and I’m sure I overdid it when I felt well – but I wasn’t getting PEM so I thought it was safe, that maybe I was ‘over it’ all (I didn’t actually know what was wrong with me at the time so wasn’t using ME/CFS terms, but thats what it was). But it just wouldn’t last.
Since getting sick some years ago, I have been on a slow and steady decline in health. It always seemed to get much worse in summer, then in fall/early winter I would get a reprieve for a bit; when the cool of autumn came it felt like a huge stressor was lifted and my system bounced back. I guess the same could be said of the fever episode, it was a tremendous stressor; I sweated so much I lost 10lbs that week. Afterward I felt absolutely purified and amazing – for a few months.
Until this year, when I actually just kept getting much worse through the cold months which are usually my friend.
It finally got bad enough that I dragged myself to Workwell to find out my AT is just 81, which I exceed with any simple movement. So I am just starting medical leave to try to get a handle on pacing, with hopes that ‘aggressive rest’ will help me ‘reset’ my system so I can go back to work in some capacity – or at the very least just make some wiggle room in my AT for some kind of life.
I wish I knew what brought these remission periods on, but it wasn’t anything I specifically did or any kind of treatment; I’ve just been trying to ‘push through’ all along. But I can say when it has happened, I felt like I did before ME/CFS, so my hopes are high that this horrible disease can be figured out and this burden lifted from all of us. Keep the faith y’all.
I know of many cases where “remission” has occurred but tying down the “trigger” proves very elusive. I think it is mainly an illusion. Not the remission but the possible cause of the remission. (I am talking about remission for more than a few days) I strongly believe that most cases of ME (and FM) are cyclical. The illness goes through stages.
Over the 25 years I have had FM and the 20 years I have had ME I would say I have had 30 or more “good” times which lasted for about 1 to 2 weeks. I have also had 30 or more very bad times which lasted for about 2-3 weeks. In between I am mostly moderately affected (but everyday is not the same). Interestingly my fatigue and my pain are closely linked but I can have times where my pain is low but fatigue is quite high ( can’t climb more than four steps). Whenever my pain is high my fatigue is high (as you would expect).
Where genetics or epi-genetics of the immune system are involved illness severity is typically cyclical.
I may be an outlier but I don’t seem to cycle at all. The best I remember and I actually do remember them are a couple of times I felt good for a couple of hours. Nor have I – except for a period of time when I reacted well but temporarily to just about everything – reacted to anything thrown at me – bad or good. That’s despite the fact that my illness has mostly been moderate and doctors have thought they will have something for me. Nothing moves the needle much.
It certainly seems, though, that many who have had a temporary remission cannot identify a cause…It just seems to happen.
I haven’t really cycled much either Cort.
I was really bad first 3-4 years (high levels of fatigue, gastro issues, allergies) then I improved a significant extent up to year 7-8 – to maybe 80% of my former self – but have plateaued in all the years since (with minor ups and downs in relation to that plateau).
It does feel sometimes like there are 2-3 illnesses amongst these various experiences.
I seem to have a variety of issues that have multiplied over the last 12 years or so.
Just as I was sorting things out something else would crop up. I know I come across as an exemplary example of a serial hypochondriac.
I’m managing to add some food back in now. I generally know the reactions I could have and so I just tentatively try things that are healthy and useful and see what happens.
I don’t take medications, apart from asthma inhalers. The ones I had found useful, Ibuprofen and antihistamines, now affect my heart rhythm.
Of course local and general anaesthetics are likely to leave one feeling good- whether you have ME or not but the usual story is that it only lasted 1-2 days (as you would expect). When I had a buprenorphine patch I felt as though I was in remission for the period I was on it. It is very strong drug and used as an anaesthetic. Benzodiazapines can also be associated with brief remissions in ME. The problem with some drugs that can increase serotonin (which you would expect a remission) is their immediate side effects which confuse the issue. People who are also chemically sensitive with their ME are especially prone to these side effects – so the benefit of the increased serotonin is not appreciated.
I have gone into complete remission both times I was pregnant and while I was breastfeeding after..it has been so sweet this time but now the dreaded cfs signs are coming back one but one.. I could cry about it.
No kidding! I’ve heard the roughest time is not dealing with the illness but getting better – and then sinking back…
Doesn’t that tell us, though, how important the hormones -as Nancy Klimas’s models have been telling us – are to this disease. Couldn’t they find a way to put you and others into a state of pregnancy (without the pregnancy).
This is such a clue for a good number of people. Other people have reported the same on the poll.
See my link further up Cort, re: pregnancy and autoimmune remissions.
The research showed that it seemed to be immune system changes (self-antigens etc) rather than hormones that were mediating the remissions.
I’m looking forward to hear of more research findings on the potential autoimmune aspect of CFS. I understand some might be forthcoming this year?
doesnt the “pill” fool a womans body into being pregnant?
I am a one symptom ME type (pure PEM) whose energy levels barely vary day to day, year in, year out. I feel 80% ‘normal’ around the house and most days can walk slowly for half a mile or so over a level surface. But introduce the slightest incline and almost immediately I can feel the exhaustion set in. As I have mentioned ad nauseum (sorry) for many years (33) I had mild/moderate ME before being suddenly reduced to my present state. It happened overnight five years ago after consecutive days of too much exercise. Some governing mechanism (like the dauer response) apparently stepped in and shut my aerobic system almost completely down. I’m about to try the DNRS program to see if I can convince my limbic system to believe again.
Peter, that is about exactly how mine progressed. Too much activity, and the downslide was overnight and drastic. You would think getting much worse overnight would raise a doctors eyebrows just a teeny bit, but NO. It’s been 5 years for me also. I’ve had CFS since 95 though, but I was able to still be active until 5 years ago. Now I can only walk a block or two.
It’s amazing how some doctors can overlook this sudden dramatic fall…
When looking at patient X, I sense a signature of disturbed day/night cycle chemicals in it.
“(1) a long and difficult withdrawal from Valium (used for sleep);”
used for sleep and valium possibly interfering with day night cycle chemicals and timing
“(2) repeated exposure to mercury vapor from poor dental work (strange neurological symptoms and paresthesia began 10 days afterwards);”
Likely local anesthesia was used possibly impacting day/night chemicals and timing
“and (3) three concurrent sleep disorders. She was also diagnosed with attention deficit disorder (ADD).”
three concurrent sleep disorders: potentially disregulated day/night chemicals and timing
“10-hour surgery during which she was given a raft of anesthetic drugs (Fentanyl, Rocuronium, Lidocaine 2%, Propofol, Cefazolin, Dexamethazone, Hydromorphone, Phenylephrine, Mannitol, Acetaminophen, Phenylephrine, Ondansetron (Zopfran)).”
that could be enough to “reset” day night chemicals or at least “unbalance” the previous locked in state
It sounds a bit like an underlying metastable state that can easily topple into one or the other locked in state. Compare it to a coin standing on its side. Just a gust of wind can topple it to heads or tails. Getting it standing up its side again or flipping it to the other side is a lot more difficult.
Now take the example of a rigged dice. It’s loaded with some lead on one side so that it’s very likely to fall on number 3. A normal dice nearly at 6 but doubting between 6 and 3 would most of the times fall on 6. But a loaded dice will often fall on 3 even if it was near flat and close to falling on 6.
Now imagine the dice laying flat on 6. Someone bumps the table. That unlikely would topple a fair dice to switch to 3, but the loaded dice easily will switch to 3. So, we may be given rigged dices by nature that easily fall on the wrong side with every small disturbance.
The rigging here could be “prone to sleep disorders or day/night chemicals mess up”. Then anything sleep and sleep / anesthesia chemicals related will be a strong trigger to topple the dices here. Most of the time in the wrong direction but sometimes out of the wrong state too (if it’s already laying on 3 and gets a big swing moving it out of its position then it has to sort of do a full circle to get back on 3).
As to part remaining in submission? Compare it with playing with two rigged dices. Both topple with any same strong trigger to another state. But only one is “rigged” for sleep/awake chemicals easily being disregulated and thus easily sneaking back in. The other dice may be easier rigged to a bad locked in position in the case of a bad infection.
I started taking betablockers for anxiety for the dentist last year. My PEM has reduced significantly and my stamina increased. I’m now mildly/moderately severe in some ways, whilst still remaining severe severe in other ways. Basically it’s just easier to live with being severe more than a cure/remission. Also I can mostly stagger around the house a bit and now am not forced to crawl half way through.
I haven’t really cycled much either Cort.
I was really bad first 3-4 years (high levels of fatigue, gastro issues, allergies) then I improved a significant extent up to year 7-8 – to maybe 80% of my former self – but have plateaued in all the years since (with minor ups and downs in relation to that plateau).
It does feel sometimes like there are 2-3 illnesses amongst these various experiences.
Hi Cort my left side of body get paralyzed and severe nueropathies
I live in small town of India here no medical facility I even don’t know what I am suffering series of stomach infection since 2012 and nuerological symptoms since 2015 and severe paralyzed symptoms since2018 please help
Subhash: Have you had your vitamin B12 levels tested?
I had a chiropractor once tell me that in Germany it is standard “last resort” practice to put chronic pain patients (presumably only those in the worst way: hopefully!) into a medically induced coma in order to re-set their neurology. Like rebooting a computer. Maybe the anesthetics for a regular surgery could have a similar effect?
Oxytocin: is the pregnancy hormone that brings relief. According to pain specialist Dr. Tennant, Oxytocin is the new research area for pain relief.
I found the link on this. My doc put me on it to try. I actually had labs showing some hypothalamus issues and this is supposed to help balance it. And it does give a sense of wellbeing. Had been off it for a few months trying something else. But will get that one back out. I find I don’t need it every day. So take as needed.
https://www.practicalpainmanagement.com/treatments/oxytocin-opioid-alternative-ready-regular-clinical-use-manage-chronic-pain
Once experienced a return to “Normal” for a day after taking Homocystex Plus which is a formula by Seeking Health for MTHFR issues. I couldn’t believe how much better, like my healthy self, I felt but it didn’t last though I continue to take the same supplement for my MTHFR issues. We all need to be tested for MTHFR issues as they can make a big difference in health.
Hello Om do you have this type of symptoms I did check my vitamin b check it is super low I take vitamin supplement but no benefit now what can I do today I walk 4 km and biking 60km because I have mktg job but my nerve getting very weak day by day.
I have had ME and Fibromyalgia for around 30 years. I have fluctuated in severity and have always been a remitting/relapsing case. There has been no known cause for any of my remissions. During remissions I have mild intermittent symptoms and have to rest and sleep more than the average person. My relapses (which last months or years) can sometimes be attributed to very stressful situations (death of a close relative) and overdoing things, but mostly have no known cause. I have been getting progressively worse since my mid forties, with more severe relapses and a lower functional level during the remissions.
Hi Cheryl,
I just happened to come across this site. Your letter caught my attention, as I seem to be experiencing a similar situation to you. I seemed to first develop quite severe symptoms in 2012, and in particular fatigue and all that goes with it. I tried to continue working, I’m a teacher, but had to stop completely some months later, as I was so badly affected. I rested completely and as I got better started to gradually do things at home again and gentle exercise. I made a very good recovery and returned to part time teaching, about 2 years later, on a job sharing capacity. After about 3 years I returned to full time teaching and had been quite good, with only mild relapses, as you described, and with rest I could overcome these. I had also begun exercising again, swimming mainly a few times a week.
However I seem to have taken a down turn for a couple of months now. I am still teaching full time in the ASD Unit in school, but enjoy the work. However, I seem to have had a few viral infections, and experienced quite severe fatigue with these and have had extreme difficulty getting back on my feet. I ve spent a couple of weeks recovering from the first. Then returned to work for a couple of weeks. But the same illness returned again.
I’m going to take two more weeks out to try to recover better . Would you have any advice for me? Just wondering do you manage to work in some capacity? Is part time work more advisable with this condition. I suppose like yourself I feel more of a deterioration as time goes on. I’m 51 now, so my age may be affecting me more. Im very careful not to over do it, and rest a lot at weekends and in the evenings. However I can get stressed at times and maybe at times try to do more than someone with this condition is capable of. Just wondering if you might have any advice, as you v coped with this much longer than me I think.
Cort,
Casual reader here, retired MD motivated by the severity of my sister’s ME-CSF.
Reading your account of the 17 day apparent ME remission experienced by 53 y/o female “Patient X” following a 10 hour anesthetic, I wonder how you can possibly know the relative roles of the surgery and the anesthetic. The surgery was clearly huge. How can you isolate their relative effects?
Thanks for taking an interest David! Your sister is lucky to have an open-minded MD for a brother. The person did not wish to publicly reveal the kind of surgery done so I can’t reveal it but given what it was I can’t imagine that the surgery itself affected the results.
I definitely think mine seems to come about with infections.
My last big bedbound crash July/Aug 2020 coincided with me getting some sort of infection (blood showed this) but GP and others can’t find the cause (still keeps going up and down each month).
As soon as I started to feel not right, my GP started tracking my bloods and found my ESR and CRP and other bloods were rising weekly. GP wanted to track if was an infection. If they rise every few weeks it means that it’s probably an infection in the body. Other bloods also have been rising now for 12+ months since the date above. Some are going back to normal, which coincides with me feeling a bit better, but some still increase and decrease.
Oh and I think the very first time I got hit with this illness it was probably from gastroenteritis that maybe hadn’t healed as I had an endoscopy a few years earlier and had gastroenteritis. Since then I have had another endoscopy which showed gastritis, so I tend to get reoccurring gastritis, most probably due to intolerances rather than diet (as my diet has never really been that bad) and even on strict elimination diets, it can take me up to 7+ months to see improvements. I do notice I quite often get gastritis kind of symptoms, so yeah something is going on in the gut for me and probably causing infections, inflammation.
I have a miraculous story for you. But no one wants to listen bcos it’s to do with a street drug that destroys lives and families. I got Glandular Fever 16yrs ago and ended up in a coma-like sleep for 23hrs a day for 8 yrs. I was suicidal as my Dr kept saying it was just stress and sent me home. I was stuck and forgotten and living like I was dead. I wanted to end my torture as no one, not even my family tried to find help for me as I just kept on sleeping year after year. I started doing some research in the short periods I was AWAKE, but still very groggy. I found that stimulants helped some people but my Dr refused to give me them. He said there are no legal stims only illegal. I’m guessing the legal ones are only a copy of the real thing. But I wish Drs realised that methamphetamine is like a miracle drug for ME/CFS. I can be bed bound for months and have a smoke of meth and like a miracle my brain clears up and my energy starts surging again. It’s like watching someone with Parkinson’s smoke a joint and before your eyes like a miracle they calm down and become normal again. No one listens to me. It’s awful having this stigma of being a junky, but i am not. I can stop any time I like, but i immediately go back to being bedbound and sleeping all the time. I am ignored by every one but i at least get to function quite well on the days I have it
Everyone who has a remission always attributes it to what they were doing at the time – but then it comes back and that thing doesn’t work again the next time.
They are random and spontaneous because CFS is an autoinflammatory disorder in my opinion.
My pots cfs is in remission probably longer than it is in an active flare but at my worst I can barely stand without midodrine.