

Two ME/CFS, yes, ME/CFS low dose naltrexone papers appear, one fibromyalgia report attempts to turn dosing protocols on their head, one patient blows through normal dose levels with spectacular success, Jarred Younger hunts for a more powerful naltrexone, and then goes out on the skinny branches with the next treatments he wants to test in ME/CFS/FM…
Studies indicate that low dose naltrexone (LDN) is effective in about 60% of people with fibromyalgia but chronic fatigue syndrome (ME/CFS) is another matter. LDN was originally tried in FM because of its endorphin enhancing effects. By temporarily blocking the opioid receptors, LDN, in effect, unleashes them – causing a rebound effect and an increase in the production of the body’s endogenous opioids.
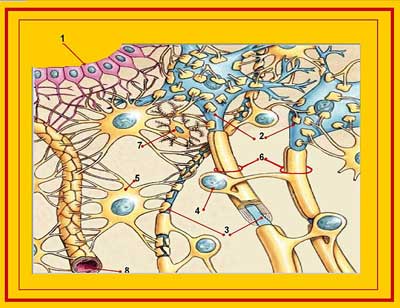
Later research, however, which found that LDN also modulates the activity of the glial cells in the brain, pointed to LDN’s potential use as an anti-inflammatory agent. Jarred Younger’s three FM studies bore this out: not only was the pain in approximately 60% of the trial subjects reduced but LDN was associated with reductions in an inflammatory marker, erythrocyte sedimentation rate (ESR), and a wide array of pro-inflammatory cytokines. None of Younger’s trials were large but they did suggest that LDN produced consistent, if moderate (@ 30%) reductions in pain as well as improvements in fatigue and sleep.
Chronic Fatigue Syndrome (ME/CFS)
“I want to make a plug for Low Dose Naltrexone” Dr. Nancy Klimas – Simmaron Roundtable Meeting
But what about ME/CFS – another apparently neuroinflammatory disease associated with extreme fatigue but less pain? The first clinical assessment of LDN’s affects on ME/CFS, “Low-dose naltrexone in the treatment of myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)”, was recently published.
Notably, it came from an unexpected source – a clinic in Finland. With this study, the recent intracranial hypertension study out of Sweden, the Norwegian Rituximab trial and the fecal transplant study under way, the Nordic countries contributions have been impressive, indeed.
The participants were given a fairly common protocol: start with 1.5 mg/day for the first week, double it the second week, and after six weeks increase it to 4.5 mg/day if they wished.
Two positive aspects of the study were the large size (218 people) and the long follow-up time – an average of almost 2 years. On the other hand, there was no placebo group, the effectiveness assessments were crude, and no validated fatigue or other symptom assessments were used.
When the patients came back into the office or needed to re-up their prescription, they were to assess things like increased alertness, improved physical performance, improved cognition, improved pain. This was a retrospective analysis based on patient charts.

Fifty percent of the participants reported an increase in alertness. (Image by Image-by-Gerhard-Gellinger-from-Pixabay)
Fifty percent of the ME/CFS patients reported improvements of at least one point in alertness/vigilance, 23% in physical performance, 21% in cognition. Surprisingly only 16% cited an improvement in pain. About half reported at least a one point improvement in two or more areas. Overall, almost 75% reported “some degree of alleviation of ME/CFS symptoms”.
While the results were moderate, the authors noted that some patients were able to return to gainful employment and that even small symptom improvements can improve quality of life.
Most patients tolerated the treatment well with most adverse side effects (insomnia, nausea, dizziness and headaches) occurring early and dropping off over time. They noted that for those who continued the treatment, “long-term adverse symptoms were practically absent.” About 8% of the patients dropped out because of side-effects.
While the most severely ill patients experienced the highest number of adverse effects, the treatment protocol – starting from a fairly high level and ramping up quickly – was pretty challenging. A less aggressive start could have benefited these patients.
The authors hoped that this preliminary study would encourage others in producing placebo-controlled studies of LDN in ME/CFS. Many ME/CFS/FM doctors, including Dr. Klimas, Dr. Liptan and Dr. Chheda, support the use of this drug for their patients.
Review
In conclusion, this study is full of holes! We don’t know if LDN was actually responsible for the symptom improvement and the lack of validated questionnaires doesn’t help. Perhaps the most positive outcome of the study that most of the people that started LDN stayed on it.
While the study protocols weren’t impressive, the study is yet another example, though, of this field lifting itself up by its bootstraps – a process that is going to be a little messy. Congratulations to the Finnish doctors for taking the time to assess and publish their results – and for being the first to get an ME/CFS study out. Congrats as well, to the patients and researchers who took the time and trouble to publish their valuable case reports.
Recent Case Reports
Then came another evidence of “bootstraping” – two patients and a researcher working together to get some case reports published. As Utah researcher Alan Light noted, case reports can be crucial in giving researchers the validation to get treatment trials underway. We have far too few of them.
Three case reports including, “Low-dose naltrexone as a treatment for chronic fatigue syndrome“, flesh out three ME/CFS patients’ experiences with LDN. As always, these case reports provide fascinating overviews of actual experiences. What they lack in statistics, they sometimes more than make up for in detail. They’re also a reminder that studies provide crucial assessments of groups of patients but don’t necessarily relate to individual patients.
PATIENT I: VIRAL MENINGITIS ONSET
One person was a healthy general practitioner until, at age 33, she developed viral meningitis and became bedbound, unable to care for herself, and experienced dizziness, widespread pain and anxiety. Over time she slowly improved and was able to return to work – only on a part-time basis – but suffered from headaches, fatigue, postexertional malaise and migraines. After extensive testing proved futile, she was diagnosed with chronic fatigue syndrome (ME/CFS) in 1989.
A stomach flu 10 years later left her bedbound again, unable to tolerate many foods, dependent on a wheelchair to get around and on caregivers for support. Various treatments provided little help.

After decades being severely disabled, one patient recovered completely – by taking very high doses of LDN!
Twenty-one years after becoming ill, she was treated with low dose naltrexone (LDN) (1.5 mg). She slowly ramped up the dose, noticed only slightly increased energy at 4.5 mg/day – but then had to cut back to 3 mg/day because of headaches. Ten months later, she made what turned out to be a momentous decision and over time successfully ramped the dose up enormously.
At 9 mg/day her abdominal pain disappeared and she was able to resume a full diet for the first time in years. She continued to experiment with dosage and for the past 8 years has taken 6mg/day two times a day — or almost three times the highest normal dose.
Remarkably, after several decades of atrocious health and a full decade of being bedbound, she’s returned to near full health and has been off disability for several years.
She wrote:
“For me, low-dose naltrexone was truly life changing. From being virtually house bound, always limited by a multitude of symptoms, pain and low energy, I found my life returning. Every treatment or therapy I had tried previously involved effort— pacing myself, training myself, coping with symptoms. With low-dose naltrexone, the improvement just happened—I didn’t have to try, I just got better.
I went for walks and started cycling again. The first time I ate out when I was no longer limited by food allergies, I could select from the whole menu—the shock of all that choice! My husband commented I was no longer a shadow of a person but a genuine companion again. From being unable to string sentences together coherently for much of my adult life, I returned to university and gained a distinction in a Master of Research degree, when aged 62!”
Treatment Takeaways
- Despite having a long and severe illness, this person completely recovered (!)
- If you have a bad reaction, don’t give up on dosing. Her body clearly needed time to adjust to the drug but once it did, she responded very positively to far larger amounts of the drug than she had been able to tolerate before.
- In the end, far higher than normal doses worked in spades for her.
Monica Bolton – one of the authors of the case study report and the patient who did so well on the higher dose – reported that her doctor, Dr. Gilhooly, told his patients to experiment with dosing, and that most of his patients ended up taking more than the 4.5 mg/day that most patients stop at.
Gilhooly was quite an advocate for LDN until the Scottish General Medical Council slapped him on the wrist. He’s no longer able to prescribe it.
PATIENT 2 – TYPICAL ONSET
Following a possible viral infection, early pregnancy and exposure to ticks, a 29-year old woman in the U.S. came down with ME/CFS, and was diagnosed two years later. Despite seeing many specialists and trying of many things including antivirals, her symptoms (pain, periodic muscle weakness, flu-like symptoms, orthostatic intolerance and unrefreshing sleep) continued unabated.
Then, 25 years after coming down with ME/CFS, she tried LDN.
Due to her immune hypersensitivity, she started at a lower dose than normal – just .25 mg/day. Even at that dose, her sleep was initially disturbed by vivid dreaming, but six months later, at 1 mg/day she began to notice some positive effects. She continued slowly ramping up the dose until she was taking 4 mg/day.
She didn’t receive the miracle outcome that the first patient did. Her pain and sleep issues improved but her functionality did not. Nevertheless, she reported:
“While the dreaming was at times disturbing, the positive changes gave me a hope for improvement I had not had in many years. The subsequent improvements have led to a much higher quality of life.”
Treatment Takeaways
- It also took this woman over 20 years to try LDN.
- Despite suffering from side effects at a very small dose, she was able to slowly increase her dose up to 4 mg/day.
- She didn’t achieve the recovery the first patient did, but she did report improved sleep and pain.
PATIENT 3 – THE MAN WITH MONO
A British man who came down with infectious mononucleosis at 10 and severe tonsillitis at 14 eventually became bed-ridden, suffering from severe fatigue, headaches, sleep issues and light and sound sensitivity. He gradually improved, though, and by using pacing and similar techniques was working in his mid-twenties at a full-time in a job with flexible hours. Still, he had trouble sleeping, recurrent colds and, particularly during those colds, suffered from depression.
Some 20 years or so after coming down with ME/CFS at age 37, he started taking LDN (1 mg/day) and slowly worked his way to 4.5 mg/day. His sleep improved, depression and anxiety lifted, and he went from a 6-7 on a functional scale to 8-9 (!).
He reported:
“Since I was 14 (when I had my first chronic fatigue episode), whenever I have had any form of illness I have suffered from depressive episodes, including needing to withdraw socially and becoming very insular. This included the period prior to any illness, where I have felt run down or could tell a cold etc was forming. I started taking low-dose naltrexone when I was 37 and for the first time in 23 years, I have not had a depressive episode linked to colds or any other illness. Low-dose naltrexone has really helped improve my quality of life and also helped in social situations where I am not withdrawing and being insular like I had been previously.”
Treatment Takeaways
- It also took this man two decades to get to LDN.
- Despite being bed-ridden initially, he improved enough to work full-time.
- This man’s functionality, while high for an ME/CFS patient, still went up about 30% on LDN; i.e. LDN can clearly help the less severely ill as well.
- The disappearance of his depressive episodes during colds indicated that the immune system can, indeed, sometimes cause depression.
- His improvement during colds suggested that LDN, as Jarred Younger suspects, is affecting the immune cells (microglia) in the brain.
Treatment Takeaways
- Finland shows up big with a big retrospective study which, while not rigorously done, nevertheless suggested that LDN had at least moderate effects on alertness and sleep in ME/CFS. Oddly, enough – not so much with pain.
- Three published case reports were highlighted by one woman who, after taking over double the suggested top dose, fully recovered from a severe case of ME/CFS. When taking the typical dose (4.5 mgs/day) her progress was minimal.
- That woman seemed to have topped out at 3 mg/day but successfully raised the dose greatly when she tried months later.
- Other case reports highlighted the fact that even patients who can tolerate only minimal amounts of the drug at first can often work their way to full doses.
- Another report out of Norway suggests that taking more LDN at first rather than less may be helpful for people having trouble taking the drug.
- Despite the fact that people with ME/CFS have no FDA approved treatment options, and LDN presents the possibility of being a cheap, readily available option, Jarred Younger’s attempt to get two naltrexone trials, an ME/CFS LDN one and a dextro-naltrexone funded at the NIH failed.
Skip Lenz, a pharmacist, suggests that if you’re not taking a lot of tramadol that you can take it with LDN.
More on LDN, ME/CFS and FM
Now For Something Completely Different (!!!)
Another group has gone even further, though. Bolton provided a pdf (see link, below) “Alternative Dose Strategy” created by Steinar Hauge of the Norweigian LDN site www.ldn.no. LDN use in Norway apparently spiked after a 2013 TV documentary was shown.
In this protocol, which Hauge asserts produces fewer side effects, patients start at 6 mg/day and then drop down to 4.5 or 3mg/day or stay at 6mg/day if they wish.
Hauge reports that “many patients with fibromyalgia (and possibly ME) … report good, and for many, immediate effects”. Hauge believes that lower doses of LDN are more immune stimulative while higher doses are more immunosuppressive.
Hauge, who is not a doctor, recommends patients try the typical dosing regimen first – starting at lower doses – but if that doesn’t work, then to try the high initial dose regimen instead.
- Check out the full protocol: 2016 06 Alternative-dose-strategy from LDN Norway group.
LDN Clinical Trials
A parallel randomized (1:1) double-blind, placebo-controlled, 100 person, Danish FM Study just got underway.
Unfortunately, Jarred Younger was unable, despite numerous attempts, to get NIH funding for an LDN ME/CFS trial. The NIH, he said, just does not fund LDN. Despite his success with FM and the lack of drug opportunities for ME/CFS – the NIH wouldn’t go for it.
Then the same thing happened with dextro-naltrexone, which Younger believes has the potential to blow the pants off LDN in terms of effectiveness. Younger reported that he was able to find the materials needed to manufacture the drug and even had the infrastructure in place for production and testing, but once again, the NIH didn’t fund it.
Because this would be such an expensive trial (>$1 million), Younger said NIH or DOD funding would probably be necessary. They’re currently looking at the HEAL (Helping to End Addition Long-Term) initiative to see if a grant there could fit. The NIH Is currently funding over 160 clinical trials and research.
Younger is still jazzed about the compound but its rarity does present real challenges.
“I still think it is the best next compound to test, but the fact that it doesn’t exist anywhere in the world currently is a huge obstacle!”
The NIH – the “Not Interested in Health” Institute was just not interested. “Not Interested in Health” is too harsh, of course, but it’s amazing how many roadblocks the huge and hugely bureaucratic National Institutes of Health puts in the way of clinical trials.
No one should confuse themselves with the idea that whatever the institute’s name is, though, that its primary focus is on improving health of this country. Its primary focus is funding research – the kind of research that enhances researcher’s career goals.
Check out the LDN situation. If any drug needs and should receive federal support it’s LDN. Because it’s compounded (and cheap) no drug company will ever fund a trial – meaning that the only available option is the feds. Studies suggest LDN works in FM and ME/CFS – two disorders that get paltry funding and lack effective treatment options.
The NIH has said ME/CFS, in particular, is a priority; yet it refused to fund a trial of a substance which could not only help ME/CFS patients but could do so cheaply -something one would hope the NIH would be interested in. It’s hard to understand.
The fact that Younger – who knows something about NIH grants – tried multiple times to get funded suggests he bent himself and his study into a pretzel in an attempt to make the NIH happy. The only conclusion Younger could draw was that the “The NIH will not fund LDN trials”. Too bad they didn’t just come out with it and tell him that at the onset.
Next Up for Younger
Younger – one of our most creative and courageous researchers – is always beating the bushes for new treatment opportunities for ME/CFS and FM. His dextromethorphan and botanicals studies have wound up or are winding up, and when that happens, he hopes to go out on the skinny branches again with trials of noninvasive vagus nerve stimulation, cannabidiol (Epidiolex), and get this, psilocybin!
Talk about rewiring the brain. Psilocybin – a mushroom extract associated with psychedelic experiences – has been going mainstream. Johns Hopkins has been assessing psilocybin’s effects in a controlled environment for decades, and the drug’s effectiveness is now being assessed in depression, anxiety, migraine, cluster headaches, early Alzheimer’s and PTSD. In 2019, psilocybin received “breakthrough therapy designation” from the FDA – which basically indicates that the FDA will do all it can on its end to support drug trials.
It should be noted that alleviating depression and anxiety may be no small matter for someone with an immune disease, as both are associated with increased pro-inflammatory cytokines. Psilocybin appears to rewire the brain by temporarily kicking it out of the rut it’s in – and allowing new neural pathways to be formed. Michael Pollan’s book, “How to Change Your Mind: What the New Science of Psychedelics Teaches Us About Consciousness, Dying, Addiction, Depression, and Transcendence“, is a good introduction to this subject.
LDN and Tramadol
LDN cannot be taken with opiates, but Skip Lenz, a pharmacist, (who does not consider tramadol an opiate), reported in “The LDN Book” by Linda Elsegood that he has not found that LDN doses in the range of 50 mg taken 2-3 times a day, cause problems.
Check out Health Rising’s Low Dose Naltrexone Resource Center for more on LDN
Conclusion
With one retrospective trial and three case reports recently hitting the medical journals, ME/CFS has finally got some LDN love. The results were not earth-shattering but they were decent, and will hopefully open the door for bigger, more rigorous studies.
Mixed in them were some real surprises, including one patient who returned to health using a dose few even dream about, and a report from Norway suggesting a different dosing regimen may help those having problems with the drug.
Plus, the case reports suggested that efforts to increase the dose can take six months or more to bear fruit, and patients who need to start very, (very) low can still work themselves up to full doses if they take the time.
The feds are just about the only group able to fund an LDN trial but the NIH, in another disappointing decision, turned down several attempts by Jarred Younger – including one that could potentially have blasted the next, more powerful iteration of LDN into existence.
Next up, Younger – a man clearly determined to turn over every stone possible – wants to assess the effects of several more potential treatments including a cannabis drug and psilocybin – a mushroom derivative and “brain rewirer extraordinaire” which is now being studied in a variety of diseases.









I had a horrible reaction to LDN, even at 0.5 mg. Agitation like I can’t even describe. I tried it twice. Took it at night, dreams were really hideous. Really scary. Took it in the mornings, and I was like a caged animal; irritable. Angry. Nothing like myself, and nothing like I have ever encountered.
I have had ME/CFS for 5 years.
Anyone else had such a reaction?
I don’t think you’re alone. Some people do have dramatic reactions to this drug – I remember that from other blogs. LDN is supposed to be pretty side-effect free but it isn’t always.
On the other hand a large survey and the study suggested that if you can lower the dose even more and stick with the drug for a couple of weeks, the side effects may very well disappear,
Hauge believes at low doses LDN is activating T-cells but not doing much immune suppression and that’s the reason for the side effects at low doses. That is speculation – we don’t know that.
I had horrible reactions to it, too, though different ones. Initially I tried it way before it was well known & was started on the 4.5…..pain improved dramatically, but heart was racing, pounding, I couldn’t see straight, was having trouble breathing, & I collapsed. We lowered the dose drastically (I don’t remember what to initially, but I continued to have many bad effects & lowered it still more. Eventually after several months, I took a break form it, & later resumed, starting at .25). I could never get above that & continued to have major side effects.
I was sleeping literally for days at a time…up to 58 hrs straight. I would wake to pee, but could barely manage to get there, stumbling, falling, bumping into walls, etc, feeling totally drugged, & barely make it back to bed in time to fall immediately back into a crazy deep sleep. I did not ever once wake up feeling refreshed, though. I did wake feeling very disoriented.
I also had horrible headaches, got vertigo & light headedness, nausea, & food starting tasting really off, my vision was doing weird things……other GI symptoms developed, etc……don’t remember all the bad affects, but there were a lot. The ones I mentioned were just the worst. And, that second time around I gave it close to a year because just the pain relief I felt initially was worth the struggle if I could eventually handle takign it. Plus, I was hearing so many positive things re its potential from the small group who was trying it at that time, & nothing whatsoever about bad results.
I did finally decide it just wasn’t worth it anymore, having given it about a year and a half total between the two trials.
That’s not to discourage anyone else, though, as many do get good results…..but it is to let those know who don’t, that yes, it CAN have bad side effects despite all the people who insist it can’t.
Everything listed i can relate to and gave experienced in 8 months – I’ve had them all. It seems to help then side effects creep up. Now I can’t tolerate even smaller doses. I think possibly we can’t clear it from our bodies the way we are supposed to. Looking at taking it 3 days a week max or quitting.
Yes, I had weird dreams and slept poorly so I had to reduce the dose and build up gradually. Start with .1mg and work up or try the advice above and start with 6mg and work down.
Great article. I’m not sure if this is related to my LDN, but I have extreme tightness in the back of my neck, which causes me to constantly. Jerk it around, trying to release the tension. Also, I wake up feeling like absolute crap every morning. I didn’t realize that, but when my last doctor took me off, I started to wake up feeling more refreshed. I don’t remember if my neck was better, but I think I’m gonna come off of it again and see if it helps. It does note in some of the side effects as snack issues, as one of them.
I noticed increased tightness/crampy pain in the neck/shoulder muscles, too. (But I took LDN only on 2 days at 0.5 mg, then stopped because the dose was too high for me).
Hi Chris, thanks for commenting on your experience. Would you mind to go into more details about your experience. Like how it’s worked for you and how it improved your condition if it did, etc. thank you
My first experience was like that, but I could tell that it was helping with inflammation and pain, so I kept at it. I have stopped and started several times. It has helped enough that I have started moving up out of the downward part of my illness cycle that I have been stuck in.
Going to a lower dose helped, and I plan to try a liquid next to see if I process that differently.
I have the same side effects. Start and give it up a few times already but the thing works for rls, so I’m back to it. Now my latest development is 2mg in enteric coated capsule I do myself. Taken at 5pm, sleep affected but all good so far unless I have a few beers. Don’t give up, work it out, maybe sublingual?
LDN has been amazing for me. It’s sad that it’s so under studied and misunderstood. The first year I was on 9mg . The second year I was on 33mg. But taken as split doses twice a day 12 hours apart. My super high immflamation is now gone, I no longer suffer fibro pain. I lost 45lbs between the various doses. And my body healed itself with LDN’s help. I am now taking between 4.5 and 9mg a day. I feel so much better than I have in years. It seems just like some people need way less, there are those of us that need way more.
I had a horrible reaction to it. My doctor started me SUPER low because I’m sensitive and terrified of getting all the bad side effects and wouldn’t you know it. -_-
It threw me into a full blown panic attack after about a week of taking it, and even when I stopped the panic attack lasted around a week. My legs wouldn’t stop twitching and kicking around, I couldn’t sleep at all, couldn’t eat, was hyperventilating, feeling like I needed to run away or die or stop existing somehow, crying constantly… It was the worst feeling I’ve had in my whole life and it was relentless. I had never done opioids or any hard drugs, do have suspected Lyme or other co-infection from tick bites, and possibly have some kind of chronic pain condition but no one can figure it out. My friend said it looked like I was in heroin withdrawal. I’m scared my neuro chemistry is ruined forever. I’m taking gaba and L-theanine and they seem to help but when I stop it starts creeping back.
I did great on 1 mg, had a few vivid colorful dreams but amazing sense of wellbeing and first restful sleep I’ve had in a decade, not necessarily long sleep, but I feel refreshed after I sleep. Also, it was like my autotomic nervous system got switched back on. I started stretching and breathing and my dream life returned after about 5 years of being a complete zombie. I was titrating up at 1 mg per week, which was too much for me. I got anxiety and irritability at 3 mgs. My pharmasist told me to go much slower. So I did, I gave myself plenty of space. I just got comfortable at 2 and my pain and sleep seem to improve over time. When it seemed to stablize, (at 3.5 months) I started 3mgs. I alternate higher and lower dosages until I feel comfortable and then I will move up to 3 mgs every day. Its going great. I had some dreams last night, but I am glad for it as I said, I had turned into a zombie. I feel alive again. I am also noticing my dry eye is also improving and immflamation going down. If i do have pain, I have a much greater tolerance. I have much more stamina throughout my day. It’s like the body gets used to surviving without endorphines and has to then adjust to having them flow again. If you think about it, the response felt is the endorphine pump that happens when the LDN is no longer present in the body. My understanding is that is no longer present in the bloodstream after 3 hours. I know I needed the endorphines. It turned some kind of switch back on.
Thanks Dana for relaying your experience 🙂
Extremely interesting. Have these results been sustained?
Many Thanks
Ed
I was on 1.5 mg but couldn’t sleep ,thus I couldn’t function and felt extremely irritable so I had to keep going down to micro doses . I’ve worked my way back up to 0.75 mg over 3 months but at this point I don’t have any relief from pain. I’d rather have the pain and have interrupted sleep than no sleep and maybe some day have relief of pain.
I am so so glad I’m not the only one! I just increased my dose from 1.5 to 3mg last week and I felt like I was losing my mind! The rage was crazy, caged animal is right. I also felt like my head was in a vice and someone was sitting on my chest. Like anxiety to the max! I almost took myself to the hospital until I realized what it was and started trying to rationalize with myself. So I rode that roller coaster for 4 days and then I just felt amped up, like ADHD, all over the place, tons of energy, sex drive super increased, so I thought the rage was gone. Now I’m on day 9 and the rage returned today. It seems to come when I’m also tired. Also, why do I need to sleep so much? It’s like I have insomnia but then if I don’t sleep enough I’m tired and cranky! I’m really wondering if I should just ride it out a bit longer or give up. I am a single mom in grad school and working, I have no room in my life for rage and focus issues. All this is making me feel crazy. The benefits on the good days are really good! Ugh.
Omg. I’m experiencing the same thing. And only on 0.5mg!!!
I also had a terrible reaction to LDN. I started at 1.5 mg but had a migraine every time after taking the medication and increasing nervous tension until my whole body was tense like a fist. Also agitation so I could never relax and focus on a task. I took a break then tried a lower dose, I had the same symptoms which were just about tolerable and I persevered for six months then decided to quit due to the absence of any benefit. That’s when the trouble started. I suddenly felt very weak and after a few days woke up completely lacking emotion. Everything felt strange and nothing gave me pleasure. It faded a bit and then a month later I suddenly was overwhelmed with terrible feelings of doom and fear and anxiety. I was on edge all the time. I was too nervous to be around people and too scared to be alone with my dark thoughts. Three years later and I’m still in the same place. It’s improved maybe 20% but I’m still overwhelmed with agitation and fear and feelings of alienation and desolation, typical of drug withdrawal. I suspect I now have a deficit of Dopamine after the upregulation which occurred while I was taking LDN. It’s made life almost unbearable and the frustrating thing is that my GP understands nothing about LDN, only the regular usage of naltrexone, so is unaware of the dopaminergic effects of a low dose. I have experienced anxiety in the past but it was related to specific issues. This feels much more profound like a chemical imbalance and is consistent with what other people experience with Dopamine Agonist Withdrawal Syndrome. I wish I’d never taken the drug as I feel it’s wrecked my brain and there’s no immediate prospect of healing it
LDN is working for me.
I’ve been on LDN a month now, near Vancouver Canada and I have less Fibromyalgia pain and stiffness, less fatigue and am able to stretch now
I was on 2.5 mg for a few days then went to 4.5mg and have had zero side effects.
My young Welsh Dr consented to prescribe me regular 50mg tablets, which dissolve wonderfully in 50ml plain tap water measured with a syringe. It’s good in the fridge for 90 days, although each tablet gives me 11 days dose at 4.5mg per day.
It’s mildly bitter, but this simple solution relieves my need of the trouble and expense of compounding.
For those people on incredibly small doses, they could just use much more water to dilute the solution.
I have reduced my dose of Lyrica, the codeine I take (rarely now) still works fine.
I’m looking forward to better days
Okay, this decides me. I’m trying it!!
I’ve been delaying on starting LDN for a couple of years now. (Afraid that my system will overreact, and also daunted about the energy needed for dealing with the compounding pharmacy. Although maybe the real cause for my aversion up to now was simply fear of being disappointed again.)
But my rheumatologist IS WILLING TO prescribe it, so I’m one of the lucky ones.
Thanks so much for this post, Cort. Now it seems more than worth it to give LDN a try.
Me too actually! I tried it a couple of years ago, kept waking up in the middle of the night and stopped it. I am going to try it again. 🙂 I have it right here!
You don’t need a compounding pharmacy. Get 50mg naltrexone tablets. Put 2 in 100 ml water and and thus you have 1mg/1ml which you can extract with a graduated syringe. There are youtube videos and its alot cheaper
You do need to keep it refrigerated and it has a shelf life of 30 days
I personally don’t reco what Chris is describing!! Even if you’re careful/know numbers there’s no way to really be precise… what if you even j mess the dose up once a month!!? Could easily defeat the whole point (esp for extra sensitive CFS pts) and do more harm than good.
Sure, you can be precise. It’s like medicating an infant with a dropper.
Thank you, Cort and all! All the Articles and inputs (comments) helps us All!??Thank you, too Jarred, Dr. Kilma and all behind the scene that is working so hard on this!??Keeping the Hope Alive for All!??
Cort
I tried LDN previously and had sleep issues. Have sleep and health neurologist who will work with me now – Is there a written patient-driven protocol that I can follow? Data to keep?Place to log results? Or perhaps I’ll just share this … just trying to save the good doc time ..
I get to sleep fine on LDN but keep waking up in the middle of the night for hours…my HR seems worse as well. The first time I tried it I gave up at this stage – about a month in. This time I need to stay at 3mg for 3 months as part of a research trial I have committed to. The NCNED took my blood before I started the LDN and will take it again once I have been on 3 mg for 3 months – then their researchers will do their clamp test magic and work out if I have benefited at the cellular level.
I have had to start and stop LDN several times because it made me irritable, but it definitely helped with inflation and pain.
This might be TMI, but I will share in case it helps others.
What I have learned is that if I’m not having bowel movements, LDN works but then over a few days or weeks I become irritable and then severely depressed. I am guessing it doesn’t clear my system fast enough. Once I get things moving 😉 then I tolerate it much better. MAKE SURE YOU ARE ELIMINATING REGULARLY 🙂
I also had to start with a lower dose than the 1.5 mg that many physicians are familiar with.
I want to try it in a liquid form next to see if that absorbs better; at least it will let me customize my dose more easily.
Finally, it felt so awkward to me, but definitely ask what it has been compounded with if you get pills. One time I was given either the time-release version or calcium carbonate filler and within days I was so depressed that I was suicidal. Fortunately, I realized what was happening and stopped the LDN for a few weeks, and picked up the correctly compounded version.
Thanks for sharing. I especially have to be careful about my bowels keeping their momentum. If I don’t it’s downhill from there so I will look out for this potential side effect.
Did you resume with liquid form & were you able to maintain?
LDN turned my life around after an all time low. I’ve been taking the 4.5 mg dose for 1.5 years after having Fibromyalgia and chronic fatigue and the numerous resulting physical and emotional problems for 10 years. It’s life changing. I emphatically recommend LDN to those with these conditions as well as individuals with arthritic pain and even cancer. I am not cured, I’m still physically challenged in many ways, but I’m able to work very long days as a business executive and sharp as a tack. I can remember a time I couldn’t do basic multiplication and I never want to return to those days. There are still mornings if I haven’t taken vitamins that I struggle with the names of some acquaintances. Nevertheless, I consider LDN a true blessing and I’m so grateful to all those who helped bring it to light! Thank you so much for the numerous articles!!! God bless you and keep you well!
Wow. That’s fantastic Renate. Isn’t this something?
It suggests that LDN is in fact getting at the neuroinflammation present. How nice it would have been to have brain scans before and after it.
Did you have any trouble getting up to the 4.5 mgs?
Yes, I had side effects for 2+ weeks (from what I can recall): besides incredibly vivid dreams, night sweats, a lot of irritation). But I pushed through because of the positive results I had read about. Other than tolerable vivid dreams now, there are zero side effects. My sleep is incredibly improved, which is why I function so well. The morning fibro fog is very slight now!!! I definitely had a ton of inflammation In my body prior to LDN that has been significantly reduced. As an example, I had chronic plantar fasciitis (on my heel), which has inflammatory cause, and I knew it was fibro-related. I have not experienced it since being on LDN. I had chronic dry eye (considered inflammatory) and had started Restasis. I stopped those eye drops shortly after taking LDN. I felt tons of nerve pricks on my skin that would make suddenly scream; gone! I also had chronic migraines whose frequency and severity have also been reduced. I no longer have constant joint pains and my muscle pains have been drastically reduced. My fibromyalgia came on as a result of post car accident trauma and inflammation to my neck and spine, so those chronic aches and pains are still there, but they are no longer periodically debilitating. I have not had a stiff neck yet. My limbs no longer feel like dead weight. Orthostatic tolerance is also 100% improved. I will still get very sore neck and shoulders if I do yard work, for instance, but my performance daily is steady; I no longer experience those ups and downs. Stressors still negatively affect me and unfortunately I’m still sensitive to gluten- no improvement there. Not sure when the positive effects will wear off. In the meantime, spread the word! There are so many doctors who have never heard of LDN. I had to bring it to my primary’s attention.
Hi Renate
I started 4.5 last week, I feel a little nausea,acid reflux,headaches, but my concern is the way body over heats when sleeping around 4am on wards.
I am thinking the dose is too high…what did you feel?
Taking mine at 12noon stopped this happening at night but i still hsve mini heatwave in the evening. I think it’s not a critical issue but could reduce a little if needed?
Same here. My body is overheated even during day time. I am on a micro dose of 0.01. Is your body heating side effect gone now?
Same here , I went up to 4.5 this week and I wake like clockwork 4 am drenched in sweat . I have no other side effects so I am sticking it out but came to tbis article to see if it was just me and apparantly its not !
Yes. I’m super super sensitive to meds and supps, even by ME standards. Need baby doses and to titrate up very very slowly. Knowing this, I wanted to give LDN a long slow trial because I’d read such good things about it.
I started on .25mg and had all the side effects, nausea, diarrhea, vivid dreams, sweats, aches and pains, sore glands, agitation, insomnia…but all of these were manageable compared with the level of side effects I’ve had from other meds. And all of these went away within about 1-2 weeks.
I left it 4-6 weeks before increasing by .25mg. Again the side effects, again they were manageable. I kept up this gradual increase until I hit 3.5gm. I felt I’d found my “sweet spot” in terms of dosage.
When I went up to 3.75, the side effects didn’t go away, particularly the agitation. I’ve been at 3.5mg for over 2 years after 15 years of ME. It’s made a noticeable difference to pain and sleep. My sleep was terrible and I had broken awful sleep for years until LDN and had to take sleeping tablets. Now I only take them once a fortnight or so.
The main thing that was astounding to me is I’d have this sickening travelling nerve pain nightly from the back to my big toe for 12 years (began at the start of pregnancy). It happened every night and meds woudn’t touch it. When I got to 2mg of LDN, it literally went away overnight. And stayed away. I’ve gone off LDN twice since then to test it and it comes back with a vengeance within 5-7 days every time.
Wow -It’s amazing how the body can adjust! Thanks for telling your story – very valuable for the rest of us.
that’s the thing Cort. Usually I would stop anything if it took this long and the side effects happened every time I would increase the dose. The weird thing about this quirky little med LDN is you can feel things happening “underneath”. That sounds weird I know, but it really did feel different than the other drugs that I’ve taken for symptom management (eg I didn’t tolerate any POTS meds like midodrine, florinef, most beta blockers, most supplements like magnesium, most pain meds esp gabapentin and neurontin). So, to not give up, meant that LDN was much more manageable. Frustratingly slow, but the side effects dissipated every time within about a week. I was lucky to have researched it for quite a long time in an LDN Facebook group so knew what I was probably in for. Most people in those groups said it was normal to have no side effects, but there were plenty who did and gave up because they thought the side effects meant it wasn’t going to help them. But it’s very true that you come to a sweet spot where it’s working for you and if you go higher it stops working for you. For some, that’s as low as 1mg, for others it’s as high as 9mg.
I am on 4.5 I only started last week on them. I feel everything you mentioned.
Just started for pain, inflammation and AS type symptoms . Ive been so ill w this post covid syndrome . Began ldn 3 days ago , like most people , with 1.5 mg . 1st day i actually felt my agonizing pain lessen markedly . But now , with days 2 & 3 , im having a paradoxic reaction where i take it and am suffering MORE pain . Im talking level 8 or 9 pain , agonizing . Help !! How to proceed ? I want and need this to work , but if the initial phase is gonna hurt like this , i cant keep on .
I had a turn with LDN. Having Ehlers-Danlos Syndrome, I have quite intense myopathic pain (joints mostly). Stanford wanted me off my low (under 20 mgs.) dose of Norco, so they put me on this insanely long titration off the opioids. It was horrible. During this time I took a lot of Tylenol–but even below the maximum dose I developed ototoxic symptoms–not good. I’m sure my liver didn’t like it either.
Finally they put me on LDN (4.5mg) and I struggled with a combo of Tylenol and LDN for pain control. It didn’t work very well. No side effects but poor pain control.
Researching LDN I discovered that it had a very short half life and realized that I COULD possibly take opioids late in the day if I took my LDN early in the morning. Naltrexone is an opioid agonist so it blocks the effects of any opioid–so you aren’t supposed to take them together.
The pain was bothering me so much that I finally resorted to kratom and found it was acceptable to take it in the A.M. and LDN late in the day. Kratom shares some of the opioid receptors with Norco but has others that are different. That combo helped with the pain. (Didn’t want to freak out my doctor so didn’t tell her… my bad).
Then I had to have a lumpectomy for DCIS and so had to go off LDN so I could take anesthesia/opioids for the surgery. What a relief–they worked so much better so I have stayed on them since.
Personally I found little side effects from LDN but little effects either. Maybe I might have benefited if I had a much larger dose–but who knows?
So Stanford’s ME/CFS clinic is doing a study on Abilify and/or LDN for fatigue. I have stopped taking Abilify since my fatigue got worse and of course they wouldn’t be prescribing me any LDN with my current Norco use.
One thing about Naltrexone is that it is water soluble and so it is easy to find on-line (a bit dodgy) and to dissolve in water to get appropriate doses. I’m not necessarily recommending this–but you know–sometimes desperation wins out.
I wish I knew where to purchase (or pick without poisoning myself) psilocybin. I know it grows locally here. I have also read that sessions with Ayahausca (hope I spelled that right) have been used successfully for psychological problems and possibly for the fatigue which can accompany them. I wonder if anybody is studying that?
Sorry this has devolved into a kind of druggy rant, but I am so tired of feeling tired I’ll look at anything. Just wanted to share my experience.
O.K. guess that’s all.
Your story is very similar to mine, Nancy. I also have EDS and my doctors recently took me off of all my narcotics. Slowly and painfully. And guess what? I’m still in pain. This low-dose naltrexone is for the birds… i’m on week 4 and I’m suffering. Legit feel like my muscles, ligaments, and tendons are tearing off of my bones. And like my back is hollow. It feels like someone has scraped out my muscles and bones and I have a gaping hole… so much pressure. That’s the only way I can describe it. I hope you’re having better luck since it’s been months since you’ve posted this.
Very evocatively put A! Sorry to hear it didn’t work out.
I am amazed at how differently it reacts to everyone. I started LDN 3 yrs ago at 1.5 mg and slowly worked up to 3 mg, then 4.5 last year. I didn’t notice a drastic change to my ME symptoms, but because I didn’t feel any negative symptoms I kept taking it. Then after a couple of years, I notice cigarettes weren’t enjoyable any longer – so that was a bonus I didn’t expect (at 3mg). Then almost a year ago I started to experience flushing from head to toe every hour. Each provider said it was hot flashes. After six months I realized the symptoms went away between the times I was filling my next script for LDN. So now I have stopped, but may try it again at a lower dose. I don’t think it CAUSED flushing, but it seemed to exaggerate the symptom, tremendously!
Have to be careful, LDN triggered an autoimmune thyroid condition in me. After reading this article, I’m wondering now if the dose was actually too low and if the higher initial dose protocol would be effective. Until there’s more info, it feels more like Russian roulette than responsible treatment. It makes me angry that as ME/CFS patients, we so often have to be the guinea pigs and rely on questionable, unproven treatments.
Agreed! How easy would it be for someone suffering from side-effects to quadruple their dose? That’s asking a lot. What would really work is a large scale trial funded by the DOD or NIH which assessed the effects of different doses of LDN on immune functioning and symptoms.
Again I assert that these are exactly the kind of the drugs trials – drugs which will never receive trials from pharma – that the NIH is morally and even pragmatically beholden to support if their mission has anything to do with improving the nation’s health.
Unfortunately, morals don’t factor in. I wonder how Francis Collins – an avowed Christian – deals with the fact that he’s running a kind of laissez-faire institution whose structure which leaves many people on the sidelines.
Agree, Cort!
And As being in the 10 % or more that always has a reaction to meds. and in recovery mode now due to most recent visit to ENT from nasal spray..
It has been touch and go as well as I approach everything with caution!
And yet, it really says something that so many people are willingly to pay to make themselves the guinea pigs even while knowing that is exactly what they are doing.
Hi Cort,
Keep up the good work. I have stopped and started LDN multiple times and cannot say whether it has had any benefit, but I have never gone over 4.5 mg (so now I have something new to try). With regard to psilocybin and other pscyhodelic meds (LSD, MDMA included), I have read multiple books including Michal Pollans and have wanted to try them. Even if they don’t actually fix the ME/CFS, it should make dealing with a chronic debilitating illness easier to cope with at least as long as the effects last.
way to look at the bright side ?
The I have had itching..
I have been on 4.5mg LDN for about 2 years now (at a slow increase initially). It got me off strong opioid medication & has relieved FM (15+ years) pain by at least 50%. Also having CFS (13 years) LDN has given me respite from a multitude of symptoms, & I can at least live fairly “normal” for half a day per week (but not able to return to paid work). I’m interested to up the dosage & see what happens!
Hi, we’re you able to take naltrexone with the opioids, as you were reducing them? I’d like to try LDN, but I’m afraid of coming down odd the opioids . If I have to come off them before trying LDN, I don’t think I could bear the pain.
I meant I live half a day per day pretty normally if I pace myself! (I live in NSW, Australia)
I recently tried a trial of LDN. If I remember correctly, I started at 1.5 with instructions to slowly increase the dose. After a week I quit. I did not have major side effects like some have described, I simply felt my fatigue getting slowly worse– exactly the opposite of the effect I was looking for. I have never yet seen anyone else describe this effect. I quit because I did not know how to respond. Lower dose? Higher dose? I did not want to risk more fatigue!!! After about a week or two off LDN, I was back to baseline.
On the other hand, after LDN I tried PEA. It has helped me to get my brain back and I am sure it has helped with neuroinflammation. Didn’t do much for fatigue or joint pain, but so happy to be able to think more clearly!
Lisa- it made my fatigue worse too. I persevered for several weeks because it really improved my sleep but had to stop taking it because the fatigue kept getting gradually worse on LDN.
LDN really calls for flexibility. My guess is that the best thing in that situation would to drop your dose – keep at it for awhile – and if you don’t have any symptoms – slowly try to raise it. It might work.
Hi Nicole, I found a new doctor who recommended retrying LDN. She also prescribed ketotifen for MCAS. In both cases she emphasized LOW AND SLOW. So I slowly worked up from a very minute dose (one prescription at a time, but I forget which I did first). I was able to work up to 4 mg (2mgx2) daily with ketotifen, and 4.5 mg (once daily) of LDN (over a period of many weeks – can’t remember exactly). I no longer feel more tired, but neither do I feel significantly less tired. The ketotifen is definitely reducing my sensitivities (slowly but surely). I decided to stay on LDN just in case it could help prevent relapses….
For me, it was SO important to work up the dose in very, very small increments over a period of time. The first time I tried LDN I started at 1.5 mg, thinking that this was a low dose. The new doc said, “Oh no – start at 0.1 mg!” (And I know someone who had to start much lower than that!)
I hope this helps, Nicole!
Hi Lisa. Thanks for your reply. Does the LDN help you with PEM? My other symptoms aren’t too bad nowadays and I sleep much better than I used to.The thing that really affects me the most is PEM.
I’m not sure, Nicole. I am doing better these days, but I have started other new interventions, too, so I cannot say which is what. I think my biggest problem has been MCAS, and reactions to environmental pollutants, molds, etc (also medications), and the ketotifen is helping to down-regulate this. So which is helping the most? Not sure….
Lisa, what is PEA, please?
PEA is a fascinating substance. We did a blog on it, jeez, over 5 years ago. Among other things it’s believed to stabilize mast cells. Younger included it in his list of possible microglial cell inhibitors to combat neuroinflammation.
https://www.healthrising.org/blog/2014/09/19/palmitoylethanolamide-pea-medical-food-fibromyalgia-chronic-fatigue-syndrome-mecfs/
It made my depression and fatigue worse at 1.5mg. Have tried it several times at a lower dose and finally got it to work. I think it was building up in me because I also have slow digestion & elimination. Once I got things moving, and tried the lower dose it really helped with inflammation. I still have to start and stop frequently.
Hi, what dose do you take? I tried a low dose and had horrible side effects now gonna try a lower dose of .2
what is PEA?
Palmitoylethanolamide (PEA) – check out this blog for more – A Medical Food for Fibromyalgia (and ME/CFS?)
Lisa, I am having the same issue. I started LDN at 1 mg 4 weeks ago. It made me feel tired so I tried taking it at night. I couldn’t sleep so went back to taking it at lunch. I have increased my dosage by 1 mg each week. I am sleeping really good, but am sleepy during the day and fall asleep at 8pm at night. I don’t know whether to stay with the 3 mg I am on or go down on my dosage. I have Lyme disease and CFS so was hoping it would help me feel less tired, but I am more tired!
Janine, check out my reply to Nicole – I had to restart at 0.1 mg and very slowly work up. I’m now at 4.5 without problems.
I started LDN three days ago 3.5 mg.
At this point it transformed my life. I wake up with no pain, energy and no brain fog. The arthritis pain in my hands has almost subsided. I also take 10 mg Adderall.
These two medications have improved my life dramatically. I pray that they will continue to give me a good life.
LDN cured my orthostatic intolerance, which was persisting even while the general CF symptoms, including exercise intolerance were gradually improving. With moderate CF, I had not tried many medications but I had bad responses to those I did and mainly I worked with supplements and meditative approaches such as letting go of any urgency. I started at 0.5mg LDN and built up to 1.5mg in a couple of weeks. I was already seeing a big improvement in my orthostatic intolerance -suddenly I could stand up to do quick kitchen tasks – so I stayed on that dose. I felt it made my sleep worse but that was so bad anyway I decided to put up with it. About 8 months later, with ongoing improvement, I felt CF was largely behind me and I went off the medication with no major return of symptoms. I stand to cook meals and chat with people in normal everyday situations, but not for prolonged periods unless I am moving about. My sleep has gradually improved over time. It changed my life.
Congratulations Linda -and orthostatic intolerance, too! I hadn’t heard of that before. Thanks for passing it on.
It greatly reduced my exertion intolerance and orthostatic problems as well.
LDN has been in my stack for almost a year.I am taking 3-3.5mg at night.In times of increased inflammation, mostly after workouts, I take it twice a day.
Not miraculous for me but it does offer observable benefits (by the way, my ESR is low, 1-2mm/h).
Slight improvement in energy and quite an improvement in brain inflammation/brain fog symptoms.I am not sure if it helped me sleep better, but my sleep is much easier to initiate now.
I believe ashwagandha, occasional sublingual melatonin and blocking blue light have made the most impact on my sleep.
It is unfortunate that the Finnish doctor who published his retrospective study concerning LDN in CFS, lost his licence to treat CFS, because his effective treatment were not according to cook book of the big boys. Finnish doctors have published their own rules of treatment, according to which LDN is not a medicine for CFS, in Finland. So LDN is a off label drug. This doctor also lost his licence to lead his own clinic because of the same reasons. He has used the best possible practise and the most recent biochemical knowledge to treat the patients with good results. But the doctor’s in Finland can’t tolerate that someone is successfull safely treating patients with off label. He is one of the best doctors in his field and most respected professional according to most CFS patients. He listens to his patients unlike many other doctors.
Just a minor mistake in your article: Finland is not part of Scandinavia. But we are part of Nordic countries. Nordic countries are Sweden, Norway, Denmark, Finland and Iceland. Scandinavia refers to a language group. Finnish language is part of totally different language group compared to other Nordic countries.
What a tragedy! And here he was actually documenting his results in a publication – trying to validate them in a scientific journal. Darn…
We more than ever need a good clinical trial.
Thanks for the explanation regarding Scandinavia. 🙂
I fully agree with Esa on the doctor who lead the LDN retrospective. He was the best doctor I ever visited, but far too good, far too independent to be tolerated by Valvira, the supervising, clueless authority. His devotion on ME/CFS patients was and is beyond comparison.
I believe he was asking for permission to commit a more comprehensive LDN study, but was turned down.
I thought Jared Younger was trying to determine which patients would benefit from LDN and which wouldn’t. I’ve tried it at least 3 times but was waking up even worse than usual at night. I was told to try taking it during the day but I haven’t worked up the nerve yet.
My problem as well. I’m going to have to bite the bullet and give it a try for a couple of weeks and hope that passes. It appears that it should.
I don’t know if that trial is underway or not.
I had problems with night waking and I know take it at 9am and it’s absolutely fine. If anything it gives me a bit more energy throughout the day.
One can only hope that courage and commitment is rewarded at some point. A good LDN trial could go a long way to doing that.
Did you try taking LDN during the day yet? I’m afraid to try again, I had horrible insomnia. If someone told me it stopped after awhile I’d be willing to try it.
I have been told that by a doctor and by Jarred Younger – FM researcher. Maybe lower the dose further and try again?
First, thanks for all your good work.
I started LDN at .5 mg and moved to 1 mg after one month.
I started having unwanted thoughts during the day that were very disturbing.
They were so disturbing that I considered going to a psychiatrist. Then I remembered these thoughts started after the LDN. I stopped it and within two days the thoughts were gone and haven’t had them since. That was about 6 months ago. My doctor who is a ME/CFS specialist said she hadn’t heard of that reaction.
I’m really glad it has helped so many people.
I had similar experience. Started at 1.5mg with declining mood. Went down to .5mg for a total of 8 weeks. I felt like I was slipping into a dark hole of depression. Prescribing doc had no answers or recommendations so I went to a psychiatrist. She ran a GeneSight genetic test which cane back that Naltrexone is under the “caution” category for me and not recommended (inability to properly metabolize for maximum affect). Also my MTHFR677T homozygous made all drugs less effective for me. High doses of methylfolate for a few months brought my mood back up.
Hey Jaci:
My reaction was not mood or depression. It was a very disturbing thought-always the same that would float into my mind many times a day. I could be thinking is something else and it would just pop up. It wasn’t about me or hurting myself.
Any way, stopping the LDN put an end to it or I would have seen a psychiatrist.
Glad to hear you went and got answers.
I also have a MTHFR mutation and had the severe reaction. I thought it was possibly building up in my system.
I have been able to use it with intermittently with good results with a lower dose among other things.
so does that mean you metabolize naltrexone faster than normal (rapid metabolizer) or
too slowly (poor metabolizer)?
I’m assuming you metabolize it too slowly and therefore were experiencing prolonged blockage at the receptors
I think this is the key to why some folks respond so differently & need vastly different amounts
Jaci, May I ask what snp or marker on the genetic testing indicated that naltrexone is in the under caution category for you?
I just started LDN also have MTHFR & have trouble detoxing in general from many things, so I’m wondering if LDN is right for me. I am on .5 and having headaches and nausea, wondering if it’s a detox thing. I would really love for LDN to work for me though …
Can you tell me more about this or reference a website…I would love to hear more. I have that genetic mutation as well & am having a negative affect so far from LDN. Thanks!
I tried LDN 2 years in total, a full Year on 4,5mg.
One side effect that never passed for me was weaker muscles. They were failing me in another way than the symptoms ME can cause. More immediately, as in trying to scratch an itch and the hand just falls limp after a few seconds…
Anyone else experienced something like this?
I have been taking LDN for 10 years. I did the usual titration. I having been taking 4.5 m.g. Between 11 p.m. and 2 p.m.
After the 4 year mark and not feeling it was doing much I went off for 6 months.
What I found is the allodynia I suffer from became out of control. I went back on LDN and it settled fairly quickly.
I do get allodynia still at times, usually during my worst flares, but the LDN helps keep most of it at bay. So just for that reason I will always take the LDN.
I now wonder if I should try a morning dose as well to see if I get more results.
I have ME/Fibromyalgia/Endometriosis/Migraines
I do not believe in LDN and I am very sceptical if doctors are thrilled. I tried LDN. It has an effect on the receptors in your intestine causing diarrhea in a dose dependent manner. I could never go over 2.5 mg, not even with Imodium. It does not seem to be a wonderpill.
In addition, increased dosage also increased symptoms in my case: foggy brain for instance and had no impact on the inflammatory markers.
It may have its place to augment various treatment modalities but nothing special.
There can be some harmful (but usually moderate) side effects for some people; yet it doesn’t mean it’s not a great medicine for many others. There’s no medication that works for all sufferers of an illness.
Again, doctors should go along the line, where there was some kind of proven success (for instance: vaccination for immune reprogramming). Another publication appeared on the ability of BCG to reverse autoimmunity and contain inflammation in Frontiers.This research says that BCG administration stimulates glycolysis (healthy energy pathway), induces apoptosis (programmed death of defective cells) in autoreactive cells and the generation of healthy immune cells.
“Since several studies have demonstrated that BCG induces TH1/TH17 responses against TB and other unrelated pathogens (62, 84, 85), its capacity to exert a regulatory effect over autoimmune diseases, such as T1D and MS is very surprising. However, there are immune-metabolic pathways involved in the activation of the immune system after BCG vaccination that may account for explanations of these observations. Indeed, the activation of innate immune cells and T cells induced by this vaccine is partly mediated by the activation of cell glycolytic pathways (86). Besides, human Treg cells are highly glycolytic (87). Based on these findings, Ristori et al. proposed in 2018 that BCG induces a tolerogenic response via enhancement of glycolysis, contributing to the reduction of inflammation in autoimmune diseases (88). Another possible mechanism through which BCG can mediate protection in the context of autoimmune diseases relays on the immune response to the infection with the mycobacterium. After infection, it has been shown that activated, but not naïve, CD4+ T cells undergo apoptosis in an IFN-γ-dependent manner (89). Thus, apoptosis of activated T cells may have as a consequence the diminution of activated autoreactive cells, improving the health condition of the individual receiving vaccination. Also, TLR-signaling stimulated by mycobacterial components induces IL-10 secretion by B cells and consequent suppression of Th1 and Th17 activities, contributing to the suppression of autoimmune reactions (90).”
I’ve used LDN for four years now and has gone from nearly bed bound to working six hours a week.
The first two years I took 1 x 3,25 mg (morning to avoid nightmares) and it helped reduce pain a tiny bit but it massively reduced PEM in both duration and in severity. But I was still struggling with lots migraine and inflammation symptoms in the head. Both with 4 mg and with 3 mg I had more pain. At 4,5 mg I had massive headache from too high dose. 3,25-3,5 mg seems optimal to my.
Then I switched to 3,25 mg x 2 a day for the next 1,5 year and now almost all migraine attacks was gone and I had tre months completely pain free. Sadly the pain returned after me trying to max test my physical ability.
For the last 0,5 year I’ve switched to alternating dose. 3,5 mg x 1 on day 1, 3,5 mg x 2 the next day, 3,5 mg the next day and so forth.
For me LDN looses it’s effect partly after 3-4 weeks of use. I first noticed this problem after the first 0,5 year of use and I need to pause the dose for 2-3 days every 3-4 weeks to regain optimal effect. The effect seems to decline pass week 4 but in a weird way making it quite difficult to notice. I often remember to pause when I’ve had to long of a PEM crash without actually doing any physical activity or if I start to get weird pain in my teeths/spinal cord when sleeping. This has become a sign of it’s time to pause LDN to regain the effect. After numerous times forgetting to pause I now try to make note in my calendar to remember to pause before I start crashing with PEM
These are all theorized mechanisms to explain the improvements in the autoimmune response that have been observed when BCG has been administered for other conditions.
While there is a trial underway for BCG and fibromyalgia, I have yet to see published results. In other words, BCG is in exactly the same place as LDN; beneficial results have been observed, case studies recorded, and possible mechanisms of action have been proposed.
Until many more studies have been conducted, there are very few proven treatment options for patients. It seems that is where we are stuck.
Are you proposing that we all wait another 50 years for the limited answers that will be provided by a system largely driven by commercial interests, instead of intentionally trying relatively safe treatments of promise because they haven’t made it out of the experimental phase, even when there is little to lose and everything to be gained?
No Cydne, because 99% of us have already tried LDN. We would know if it worked…
Yes, BCG is just another trial, but at least it is promising and is rooted in science. It still may prove false of course.
Adam, I am new to the game and found your old post interesting. Could you please give me the link to the original article you are quoting in your post ?
Thank you
I started LDN at 1.5 mg daily, then increased after 10 days to 3mg and finally 4.5 mg.
I didn’t have any negative reactions, and I am feeling much stronger. When I started LDN 6 weeks ago, I couldn’t walk to the lobby to get the mail. Now I am walking briskly for 20 minutes a day and sleeping better. I am still improving and expect to hit peak strength from LDN in about 2 months according to my doctor.
Good luckK
I would rather get Pins placed in my Ears SAAT Remmision Alpha-Gal
LDN put all of my autoimmune, and other conditions caused by a damaged immune system, into remission. Hashi’s took the longest to see changes at around 1 year, and continued to improve over a period of 3 years following. I was on 4.5 mg at night until I started split-dosing – around 2012 I think (2.5 mg at night, 2 mg in the morning). 2 weeks of that caused chronic shingles to finally stop after 7 years.
Hi Cort There is some recent research out of Griffiths University, which is one of the top universities, in Australia on LDN in Nov 2019. See https://news.griffith.edu.au/2019/11/12/researchers-discover-potential-therapeutic-approach-to-treat-me-cfs/
This is not a clinical trial, where symptom improvement and markers of patients would prove any claim.
LDN is very well know by all practitioners. There is a general consensus that imrovement is modest at best. I would like to see treatment programs, which in fact work and say that
“do not use 4.5 mg, use 9 mg. Side effects were as follows but…).
Actually, phase 1 clinical trials are not usually double-blinded. They are conducted to establish safety and efficacy of the drug. They are still a necessary and informative part of the clinical trial process.
Results might not “prove” a claim, but they establish whether further research and costs are justified.
I forgot all about that despite having written a blog on it (sigh) – http://simmaronresearch.com/2019/12/naltrexone-natural-killer-cells-chronic-fatigue-syndrome/
Does anyone know if there is research about the safety of LDN and pregnancy. I was experiencing some pain relief on 4.5mg (I know because when I came off it, my nerve pain went through the roof – weirdly in my mouth and gums), but I went off it because my doctor couldn’t assure me it would be safe to use whilst pregnant/breast feeding. He said there ‘wasn’t any research’ (though he also didn’t care to look, as far as I could tell). I went off it, and I’m not yet pregnant, and I’d really like to go back on…
I would suggest looking into Dr Phil Boyle and his fertility clinic in Ireland. He has a website and several presentations about LDN in pregnancy. He uses is to achieve and maintain pregnancy in women with endorphin deficiencies and conditions such as endometriosis, PMDD and PCOS. It actually prevents miscarriage and helps maintain healthy pregnancies as trends in his clinical experience. I would encourage you to reach out to him.
In my personal opinion ( degree in research biology but not a doctor) I would venture that if LDN provided health benefits for you while taking it, then they would likely provide systemic benefits to maintenance of a healthy pregnancy. Unbalanced endorphin levels can mean wonky reproductive hormones levels that could make conception and maintenance of a successful pregnancy more difficult than need be. I’ve been spending months looking into this for my sister who has fibromyalgia but would like to be able to start a family, as well. I’ve advised my sister (who’s just started LDN this week) that if it works well for her symptoms, then she ought to continue through conception and pregnancy, because trends in research indicate only positive, and no negative, factors in continuing. I will fight her prescribing doctor in this in future with as much evidence as I can muster, because she’s indicated she must come off LDN for pregnancy. 3 months of dedicated research from Ireland, Australia and New York do not support to idea that LDN is harmful. It shows the reverse. If I would advise it to my own dear sister, I would wish the same for you in conceiving carrying a little one.
Best of luck to you in your journey to physical comfort and having a family.
Thanks for collating all of this.
I started taking LDN about 5 weeks ago after weighing it up for the last five years.
I started at 0.5mg and really suffered with insomnia and vivid dreams. I changed my dosing time to 9am and it works much better for me. I’m currently on 1.5mg.
That ‘hit by a bus’ feeling is markedly reduced and I’ve got more stamina and I can definitely stand up for longer. PEM seems reduced. Even if I don’t get any further improvements, I’ll continue to take because it’s definitely making a difference to my overall quality of life.
I’m a moderate sufferer and have had ME/CFS/FM for over 6 years.
I started LDN at 0.5mg for about 6 months and over the next 6 months increased it slowly till I reached 4.5 mg and all of a sudden it kicked in and I began to feel better. Some days I feel very good, but I still have to pace myself.
Me too Hannah, same experience. Doesn’t help me with pain though but I would certainly say it is worth trying.
I started LDN at 4.5mg at night. I got disturbing hallucinatory dreams. After 6 weeks my pain went away. I have CFS and EDS. I dropped the dose to 3 mg but the dreaming was too disturbing. I tried it at 3mg taking it in the morning and it was no different to taking it at night.
So after 6 months all up I stopped it. That was a long enough interruption in the chronic pain for it to stay away. Then 9 months later pain returned possibly with injuries and an inflammatory response.
I felt LDN hadn’t enough research. And messing with dopamine is quite something so I wasn’t prepared to risk my mental health. Low dose hydrocortisone has been much more effective with no side effects for CFS.
I do not understand why an LDN trial would be expensive. The drug is basically free and there would be no expensive lab testing as part of a trial. Why can’t Younger get money from one of the private ME/CFS research organizations like the OMF or Solve ME/CFS?
I believe that labor is usually the biggest cost of a trial but you bring up a good point – and Younger actually specializes in doing really efficient clinical trials. I was thinking of a private donor who could throw down $1 million and get dextro-naltrexone off the ground. If LDN does as well as many of the comments indicate – how much better could dextro-naltrexone do?
Does LDN INTERFER with cannabis?
Good info, thanks Cort. Interesting to learn about all the various reactions to LDN and great to see that some people are getting relief. Stanford CFC had me try Abilify and LDN. Bad reaction to both. Abilify caused depression and LDN at .25mg made me feel like I was on a bad acid trip. Now on what I call homeopathic doses of LDN… 100ml/day (capsule powder added to water). No reaction so far either way after 45 days. Will continue especially in light of the recent research.
I tried to take LDN several times, but could not cope with it orally due to burning pain that it triggered in my upper gut. This pain has been a long term issue that I now manage by avoiding any foods/drugs that are acidic, and LDN in some way was not acceptable for my gut.
For a long while I was using the transdermal cream, but wasn’t sure it was really doing much for me, and someone who I knew online reckoned that the transdermal cream doesn’t work correctly because of the long term basis of a cream on the skin (the receptors are blocked for too long, the person thought, to work effectively). I did try the sublingual drops but got the same problem with burning pain in my stomach.
The final time I tried LDN, I had my stomach pain under good control and thought I might be able to tolerate it (I was wrong). However using it for just a few days triggered an unbearable reaction when I tried to sleep, in that I continually was jerked awake, time and time again just as I was dropping off. It was horrible! I was seriously worried on what it would do to me if I continued, but oddly, I had not had this reaction the first 2 times I tried it.
Hi,
I’m sensitive to ldn too, it just kills my GI. On and off a few times, diff.doses etc, diff. times and so on. One worked, bought enteric coated capsules and I put powdered ldn in it, 2mg at 5pm, GI all good,
cheers
Bogdan
I had the same reaction of sleep problems and i had burning in hands and feet. Did you try it again?
I have had me/cfs fibro for 30 yrs. My dr has had me try ldn several times-i think lst time was about 4mg, & last time was 1.5. Couldn’t take 1.5 so took 1/3-didn’t notice anything positive but seemed ok to take so continued. Then as his ldn he had given me was running out I switched to a good compounding pharmacy & they made .5 for me & I had the nightmares…& the drug simply was not good for me. I wonder if naltrexone can be at all different in generic meds? Not sure if I will continue if I can get the previous formulation cause I am having trouble figuring out if I get a benefit-it’s been a good 2 months & I am unsure. I am fairly stable with alternative care -acupuncture & herbs 2x’s a week, bodywork super (gentle cranioscaral 1 x week). I carefully do yoga1 time week & can do gentle 2 lb weights and tai chi, but always need to sleep daytime after exercise. No clear changes with ldn. Also take some other western & alternative meds.
I took LDN some years ago, can’t remember how many, but it was when Younger Was doing his research at Stanford. I took 4.5 mg Per day for about a year and a half. I had no side effects but also no beneficial effects. No help with sleep, pain relief, Alertness, zero. I ended up going off it because I had to have some procedures that required anesthesia, And just decided not to bother continuing. I have had lifelong fibromyalgia and even though I have sensitivity to a lot of drugs I had no issues with LDN. It honestly seemed like I wasn’t even taking it. I’m just wondering if others in this group have taken it with no effect?
Hi Billie,
After reading about all the awful side effects and the great improvements people had I thought I must have a very odd body. I took 4.5 mg of LDH for about 8 months last year and had like you absolutely no symptoms or changes . I stopped because I got tired of filling my prescription.
Was glad to read that there was at least one other person like me.
I wonder what would have happened if you had increased the dose?
Has anyone taken naltrexone (LDN) very intermittently and found that it leaves their condition better off in the long term even when not taking the drug? This has been my personal experience even though I’ve only dosed between 4 to 8 days per month for a year.
I’ve had significant results with LDN having started it one year ago at 0.25 mg (dosing in the morning). Even at just one 0.25 mg capsule, I could only take for up to 3 to 4 consecutive days before discontinuing due to side effects (severe hypoglycemia, hyper stomach acidity, a bit of irritable interior monologue, like “how dare that person cut me off on the freeway 30 minutes after it happened”, a bit of an overly wired feeling but still able to fall asleep at night ) which would lessen after discontinuance. However, all these side effects have lessened (“irritable interior monlogue” has gone as a side effect) over the months with continued use, but 4 consecutive days at 0.25 mg is still pushing it for me.
On the bright side, I received super ramped up energy while on it…more importantly even though having only dosed the drug an average 4 to 8 days out of each month, I have made significant long term improvement, (1) more energy, (2) better sleep, (3) less post exertional fatigue, (4) less sensation of tiredness and awful sensation of pain around my eyes when I’m tired, (5) more ability to concentrate for longer periods of time, and (6) better “braking system” to stimulation, i.e. my natural sedation system works better when overstimulated so that when I get tired I get a better sense of heaviness/sleepiness rather than “wired and tired” or the “agony of agitated exhaustion.” These improvements lessen slightly over weeks of non-use but they are almost always remain better off than prior to the last dose I took (even if it’s been one month since my last dose!)
And LDN is the ONLY therapy that lessens a post-exertion fatigue crash WHEN I AM EXPERIENCING IT. (I am fairly high functioning for an ME/CFS patient, but a crash from over-exertion can still knock me down pretty good so that I’m having to lay down or veg out for a huge chunk of the day…LDN during a crash picks me back up FAST…NOTHING, I MEAN NOTHING does that for me except resting for a day or two).
For the first time, I tried taking it at 0.5 mg for one day in January. I got a big bump up just from that but opted not to continue because of the potency for me.
Cort has already pretty much outlined the possible take aways from various cases. I would just like to emphasize that (1) 0.25 mg of naltrexone might be like a bazooka dose for some people, and (2) maybe there’s other patients besides myself that can gain long term improvement from the drug without daily dosing (at an average of 4 to 8 dosings a month). If you experience intolerable side effects from continued use, but you’re better off after a few days of dosing, intermittent use may be your ticket.
I don’t want to overstate this case, as I know one person who tried 0.25 mg and couldn’t sleep for two days, and she understandably won’t touch naltrexone again.
Again, it’s interesting that low dosing may have paradoxical effects compared to higher dosing (6 mgs). I look forward to hearing more on that.
I’d love to hear any feedback on this. Also, just fyi, the People’s Pharmacy chose to note, rather interestingly, LDN’s therapeutic mode of getting TRP receptors to work rather than mentioning other potential modes of therapeutic effect. Doesn’t that match up well with its potential in activating NK cells?
I too cannot take it daily, but have experienced drastic improvements in inflammation & pain levels with intermittent use.
Thanks for your feedback. That is interesting.
Stephen,
Just to see if I could do it, stopped LDN for 3 days. The pain it was suppressing came back to remind me why I was taking LDN. Didnt take long to return to LDN, and it took 2 more days to kick in again.
I did this twice more just to be sure…never again.
“LDN cannot be taken with opiates, but Skip Lenz, a pharmacist, (who does not consider tramadol an opiate), reported in ‘The LDN Book’ by Linda Elsegood that he has not found that LDN doses in the range of 50 mg taken 2-3 times a day, cause problems.”
Wow! Fifty mg 2-3 times a day doesn’t cause problems!? Maybe in a gorilla?
I tried LDN at the usual recommended starting dose for CFS/FM a few years ago. I was excited. “This is going to work!” I thought. But…I felt more tired and less able to function. Tried at even lower dosing, but still no luck. However, after reading all this, it’s apparent that either patience at building up the dose slowly, or starting right out on a higher dose might work, depending on the person.
In an interview with Jarred Younger I read some time ago, he wasn’t that concerned about being on tramadol at the same time as LDN. He did recommend spacing the LDN dose about six hours after the tramadol, however.
At 75, I think I’m tired of trying this and that over and over. I’ve gone down hill a lot lately from just several months ago. I have constant dizziness, often times more like vertigo, lightheadedness/brain fog, worsened tinnitus/POTS, sweats, etc. I’m really struggling.
I’m really sorry to hear that, Judith. Sounds like really rough going. I hope you are able to get some improvement or at least respite soon.
I’m back to comment since my March 17, 2020 comment above. I got out my original Aug 2017 LDN about three months ago. I felt over-stimulated and unwell on the recommended starting dose, so I just quit taking it back then. It was beyond the expiration date, but I kept it in a cool place. Yes, I know, not recommended. Instead of starting with the 1.5mg dose (1/2 of the 3mg tablets), I cut that dose in half, .75mg. I took it late morning with my other meds. I just kept on taking it, didn’t seem to be any side-effects, and sure enough I started to feel better. I had stamina. I started making jewelry and finally, after years of saying I was going to open an Etsy online shop, I did it! I could sit and make jewelry and still feel good. The severe middle back pain I’d normally get lessened a lot. And I started cooking! I haven’t cooked for years, mainly eat prepared frozen food. So everyday I got in the habit of making simple plant-based meals. My overall pain was reduced maybe 40-50%. My mood seemed to be better, but I’ve been on anti-depressant Cymbalta for years. But I just felt happier. Then before I ran out, I tried getting more. The same doctor would cost over $200 for the tele-medicine visit, so I found a different place. They’ve taken awhile to approve my request, and now during the bad weather (tons of snow here in NY) and an overwhelmed US Post Office, I’ve been waiting for my lower dose tablets. After awhile, I may bump my dose up, see how it goes, but I won’t go off it. After reading all this great input from these many comments, I feel I have the information I need to be able to manage my dosing. It’s just so unfortunate that the NIH wouldn’t fund Dr. Younger’s research!
Hi Judith, I’d be interested to hear of an update from you since it’s been a couple months since that last comment of yours. Are you still doing well on LDN, is it still working for you? thank you.
I am currently on 2mg of LDN mainly trying to eliminate almost daily horrible migraines with nausea and am having considerable side effects, including worse headaches, insomnia, bee sting type pain, body aches, and being down in the dumps. When reading that some people take up to six months to get over the strange side effects, I find myself questioning whether or not I can withstand six months of LDN even at this dose, when it is not helping the migraines at all. Has anyone had great success in eliminating or improving nauseating chronic migraines? If so, how long did the side effects last and how long did it take to see improvement in. the migraine intensity and frequency? I have not been on LDN very long but I am experiencing worse migraines plus all of the before-mentioned side effects. Comments would be appreciated. Claudia
Claudia, sounds like you’re starting off on a high dose of LDN. I started at 0.25mg. I had side effects at that dose, but they were manageable. I could only dose up to 3 days in a row before the side effects became too high, but I got therapeutic effect from it that persisted past the 3 days of dosing. Maybe give it a break for a few days, and then try a much lower dose than 2 mg to see if it’s manageable in terms of side effects.
Hi,
improving nauseating chronic migraines? I did, sort of, nothing 100%. Coulprit is alcohol consumption in my case. I glass of red sets nauseating. When it comes to migraines, it did go away after 6 months but you need constantly change your dose, start 1mg maybe, change the time of taking it and lastly I put my ldn in enteric coated capsule, helps GI,
cheers
Bogdan
I took ldnfor 18 years and now it’s stopped working since I got cool sculpting done on my stomach My body changed I’m thinking because of my alarm Fattic system was messed with and I don’t know what to do I’m open to find somebody that can tell me what to do to get my body to except it again I feel like I’m allergic to it help
Hi,
if stopped working I’d go and try other opioid antagonists, you need to google,
cheers
Bogdan
Can you take low dose naltrexone while on a medication like remicade or orencia? Or does one cancel out the other? I have rheumatoid arthritis and fibromyalgia and have been taking 4mg of low dose naltrexone for 2 years now. After a few months I definitely noticed a reduction in pain and increase in energy when it came to fibro symptoms.
Ive been taking LDN for about 2 years and have experienced improved mental clarity, but it has not been a total solution for CFS. I started at 1.5mg for 2 weeks, bumped up to 3mg for 2 weeks and then to 4.5mg. I am very sensitive to supplements, but I did not experience any side effects from LDN.
Before LDN, I tasted pain, touched pain, saw pain, breathed pain, and my world was literally gray with pain.
Been on LDN since 2017 (3 yrs). I mow my lawn, plant trees, garden, clean my house and perform low intensity workouts during the winter months.
Symptoms while titrating (over a 4 week period) were: vivid dreams, upset stomach (nausea), and minor weight loss. Over the course of 6 mos those symptoms slowly subsided. It eliminated the major portion of my pain however, when performing daily chores and such I still experience acute fatigue and pain and stiffness for days afterwards. Once rested I can resume my chores again.
I started on 1mg for one week, 2mg the next week and so on till maxing at 4mg. I read a couple of comments above regarding two people with MTHFR, which I have, and how this mutation can affect efficacy and elimination. It was interesting to read the experiences of the MTHFR like-afflicted. I started on LDN for headaches related to cervical spondylitis in my neck, 1st and 2nd vertebrae. I also have lumbosacral disease in my pelvis and have recently been diagnosed with Fibramyalgia so my pain was at times severe, for which I was taking cocodamol 30/500. I am unable to tolerate anything stronger and the GABA’s were basically ineffective, the side-effects intolerable. My story is, at 1mg and 2mg I started to experience bad dreams, waking at night and morning brain fog accompanied by considerable nausea. Increasing to 3mg I found that along with the previously mentioned side-effects I started to experience dizziness, irritability and extremely low mood. But I persevered up to 4mg. On doing so I became almost suicidal. Intrusive thoughts filled my day and the night-waking and vivid dreams became more frequent. Stomach pains began, first-bite syndrome appeared- intense pain in my jaw for 4 or 5 seconds with any foods. And headaches, once infrequent, became the daily norm and with the consuming nausea I constantly felt I was on the point of fainting. So four nights ago I decided to cease LDN. Last night was the first night in months that I managed a full night’s sleep, without waking and without the dreams of dread that would linger and colour my already low mood for half a day. My head is clearer, my thoughts less intrusive and already my powers of concentration are improving; previously I couldn’t read a paragraph in a book or an article online without wandering off into some intrusive, imagined existential nightmare. Taking LDN did relatively nothing for pain, yes, the headaches were slightly more tolerable but I was still experiencing the same neck, lower back pain and paraesthesia as before. I will see how I get on in the coming weeks and maybe report back to this message board. One thing I will add though is that cannabis, whether bud or hashish made all the difference to my symptoms. In March I was forced to discontinue cannabis-use after 40 years (60 now) and my symptoms rocketed. My well-being fell like a stone as the symptoms took over, thus began experimentation with the various opioids and nerve-blockers. Then LDN and all that occurred with it. I suppose I’m making a case for medical cannabis but the proof, for me, has been in the pudding. It should be available to all who need it as is my experience. Thanks to all for sharing your experiences, it has been an informative read. For me, LDN has not worked both physically and mentally. I hope for those of you who have found relief from LDN that long may it continue to provide your needs…
To be continued
Good that you have mentioned MTHFR. I attribute my intolerance to it as well. C677T (+/-).
Great to read that PATIENT I: VIRAL MENINGITIS ONSET did well at 9.0 mg LDN.
I have been taking 4.5 mg and it’s not working for my Autoimmune Disease which is sarcoidosis.
The doctor told me that he could go up to 9.0 mg LDN.
I am now increasing the amount slowly and hope that it works at that level.
Don’t understand why there is not more on the internet about doctors taking their patents to 9.0 mg and what happen afterwards.
I agree. Good luck getting that dose up!
Me (live in US): have POTS, MDDS with too many symptoms to list, it keeps me homebound/bed-ridden. Tried LDN may be 3 times: the first 2 days I did feel much better, yes, after just 2 days, then day 3 comes-zombie… I am restarting it again-1.5mg. -finally found a doctor who prescribed it. If I don’t get even smallest improvement in how I feel, I don’t know how I can continue. I already have all the side effects people describe here, without taking LDN. Not sure what is going to happen to my already horrible night time sleep, lethargy, brain fog, cognitive impairments, Cardiovascular instability, severe MDDS symptoms-rocking, bobbing, swaying….
My sister: she had severe seasonal allergy and throat “scratching” kind of cough that drove me nuts when she visited me-each day /all day. Then, I remembered unused LDN. It worked like magic-OVERNIGHT. We could not believe that it literally stopped her cough. No side effects whatsoever. We bought more through buyld and she took it home with her. That was the first year she was not hospitalized during her severe seasonal allergies. I just wish we bought one year supply. Unfortunately she can’t get it in a country where she lives.
Mom: more than 2 years ago she had extremely rare gynecological cancer and surgery to remove her uterus. We bought her LDN on buyldn dot com (unfortunately they no longer ship it) and she was taking it every day. No side effects whatsoever. She never visited her oncologist after the surgery. She had 2 strokes during 2 years, but fully recovered. I attribute all recoveries to LDN. I don’t need scientific proof. Unfortunately she just finished her last LDN pill and I am trying to figure out how and where to buy LDN to ship it to her.
Healthrising is a lifeline for me, thank you so much!! I’m on 9mg self dosing past the 4.5 prescribed for ME/CFS. I tried a second time to add an evening dose but just can’t afford all of the sleepless nights. I read that endomorphins are produced from 2-4am so why are we able to take it during the day and still benefit so much?
it is hurting. I felt going off it, the inflammation worsened (I have been on naproxen too long but can’t go off it either) but I have had a rash for months, on upper stomach and lower belly, and now can not get the covid vaccine until things clear up, I did go off it one time and seemed to feel worse (I have not yet gone up to the full amount) like with brain fog, inflammation, but this rash that they say clears up is not clearing up, after several months, and I feel this pain all over the muscles in my face and head. I am going through grief now too, it is too much right now and I have to discontinue. there could be thousands of possible treatments if there were more studies, so for now we are stuck playing guessing games, very awful. I do know my friend had very significant improvement and is becoming active again. I feel it is too much right now for me. But then I may feel worse going off it again like before. Just this rash has been for months, like hives, and so that is that
Yes, we are all playing guessing games. LDN does have some small studies but side effects are cropping up more than anticipated. Good luck!
I am wondering if this is my luck to? I suddenly since trying to use this off and on, have experienced such extreme tiredness I cant function (i have a 2 year old) and My blood pressure has increased. I have never had high blood pressure . I was being treated with LDN 1.5 for Pandas/ lymes. Im so confused. I never read anyone else having an increase in BP. My BP becasue I work out is usually 100/60 pulse 58, now its been 125/70 pulse 68. Im so confused. Also i have been to the ER 2 times for dizziness. What in the world.
Hi Robin. Are you still fairly certain there was a connection between taking LDN and having a rise in your blood pressure? I’m asking because I do occasionally hear this and I have been hesitating to take LDN because I already have high blood pressure issues. But I also want to take it to feel better. Did you figure out if there really was a connection? Thanks, Geoff
@Cort
think this might be new info on LDN research
“World-first laboratory study finds low-dose Naltrexone may improve ME/CFS symptoms”
July 14, 2021 Deborah Marshall
at site
https://news.griffith.edu.au/2021/07/14/world-first-laboratory-study-finds-low-dose-naltrexone-may-improve-me-cfs-symptoms/
Hi, has anyone found an immune challenge of some kind changed how well they were doing with LDN?
I started at a very low dose 6 months ago and would call LDN life-changing. Very quickly I got my old brain back plus saw an increase in energy and a reduction in pain and post-exertional malaise.
But following a dental infection and my first vaccine dose, LDN just seemed to stop working. I am gutted and wondering whether to experiment with a higher dose (lowering it didn’t help).
Pls. let this post dissuade you from the Covid vaccine btw, I just think perhaps it’s thrown my immune system back into a very over-activated state and maybe the LDN dose I was in isn’t enough anymore.
That was meant to be ‘please DON’T let this post dissuade you from having the Covid vaccine! Doh! You can tell I’m having a flare-up as I can’t even get my words out! 🙁
Is anyone taking a higher dose of LDN? I have increased to 14 mg because I felt lower dosages were not giving the relief from fibromyalgia I hoped for. I have days that are good and I think it’s helping, then days in a row where I feel bad and I don’t know how much of a benefit I’m getting.
Thank you all for the contributions. I am suffering since one year and diagnosed ME/CFS since one month. I am considering both LDN and Aripiprazole and am researching.
One consideration which may explain the differences:
Naltrexone half time is 4 hrs, but the metabolit 6-β-Naltrexol is also active and has half time of15 hrs (The blockage of the opioid receptors in the normal Naltrexon use is approx. 48 hrs).
Hence accumulation will occur when taken dayly. This may be an explanation, especially for on/off treatment ?
This may be of interest – it may be already on the site, but I have not seen it yet. It’s a study on 216 patients in Finland.
https://www.tandfonline.com/doi/full/10.1080/21641846.2019.1692770
Adam, I am new to the game and found your old post interesting. Could you please give me the link to the original article you are quoting in your post ?
Thank you
I’ve tried sublingual LDN several times over the last 3 years but each time have had to come off it after titrating from 0.5 to 1mg across the course of around 2-3 weeks.
I have a systemic autoimmune condition, similar to Lupus, that came on out of the blue following a coronavirus at the beginning of 2019. I’m super-sensitive to even the most gentle of meds and the LDN was prescribed to help with cytokine inflammation. Unfortunately, it caused some of my most bothersome symptoms, which are Sjogrens in nature (dry eyes, mouth, dry skin, dry organs, and so on) to worsen, as well as increasing the myoclonic jerking and muscle twitching I experience whilst trying to sleep (this gets worse when I’m having a flare), so my only conclusion is that it’s not for me! My doc said she thinks it because it’s stimulating my immune response, but I was thinking surely it would be better to take something that dampens that response, not encourages it?! As another poster states, cannabis is very good for me, but i need to find a way of taking it where it doesn’t dry my mouth out further (anyone know of any?!).
Very disappointed about the LDN for me, as I’ve read such great things and know it’s helped a lot of people. Happy to read of peoples’ success stories here – long may they continue!
LDN is an amazing drug you just have to give it time and get acclimated to right dose. I have found being constipated is a problem so just drink tons of water, take some magnesium and eat right but it’s 3 mths and I’ve never been happier. Miracle drug. I have multiple autoimmune diseases by the way.
I tried LDN first 1.5mg and then 3mg. I thought I would be tough and get through the side effects with 3mg. Most side effects went away, but insomnia never went away and only got worse over time. I endured severe insomnia for months, as a result I developed nerve pain and burning in feet; had to cut the dose down to 1.5mg after six months of being on 3mg. I sleep better, but the neuro inflammation and headaches are slowly coming back. There is no good choice for me. There is no miracle in any drug. There is no cure in any drug. It’s you body that is supposed to heal and cure itself. If a drug helps your body do that job; you are lucky, and on your way out of misery. I am going to try prolonged water only fast, trying to heal my brain naturally.
Hi,
I first tried very low dose naltrexone under 1,5 mg and build up slowly to 3 mg. I felt worse. I tried it on and of with no succes.
Then I tried 6 mg in the morning and I felt better pretty fast. I felt really good. I have never felt that goog since 15 years. But… after a few day I get irratable and anxiety. It became unbearable. So I had to stop unfortunately.
Now I know for me, there is something with ldn that could help me. It would be nice if there were more studies on higher doses. I have me/cfs for 15 years
Our teen daughter has Slipping Rib Syndrome which causes lots of nerve pain, does not have EDS but does have some hypermobility issues, POTS, possibly MALS, CRPS.
Her doc takes LDN for herself and prescribed it for our daughter. But oddly, she prescribed 2.5mg initially then bumped it to 5mg after a month.
Have not heard of anyone starting like this. I have followed LDN stories and know that lower doses and increases are the norm.
She has been on it 3 months now. Her many pains seem better and her mood seems good but she wants/needs to sleep all the time.
After reading your very helpful comments (thx!), we will try different things (under doc supervision) – dosing in morning or noon-ish, reducing dose and even skipping doses as I’ve been reading here.
Sounds like some of you have had success at much higher doses but not comfortable doing that yet.
Thoughts appreciated!
“ LDN cannot be taken with opiates, but Skip Lenz, a pharmacist, (who does not consider tramadol an opiate), reported in “The LDN Book” by Linda Elsegood that he has not found that **£LDN doses in the range of 50 mg taken 2-3 times a day***, cause problems.”
***Did you mean Tramadol?
Hi I started ldn 18 days ago 1mg fir 10 days 2 mg for 7 last night took first 3 since I ve been on ldn had epidural that didn’t work plus round od predisone I’ve been short of breath and heart papations thought it was predisone I’m waiting to hear from Dr Help
The LDN Research Trust website states that nausea as a side effect from LDN is “extremely rare”, but, judging by my search of forums, it is reasonably common. On the plus side, most people report that it subsides after a few days or weeks.
I am currently experiencing nausea from my first doses and hope it will subside so I can see what happens with any positive effects over the next few weeks and months.
Has anyone experienced night sweats? I have had a huge problem with this since starting on LDN.
My first try with LDN for ME/CFS try went haywire: Took 0.5 mg (10 drops of an 1 mg/ml LDN solution) on two consecutive days; had significant side effects, like sedation, slight speech impediment and in particular a wired/buzzing feeling in the whole body, as if the immune system revs up everywhere (it feels similar to a vaccination reaction I experienced after my Covid vaccination and another vaccination shot). This feeling is still lasting now 1.5 days after I last took LDN.
I could feel some possible benefits like less orthostatic intolerance, but I did crash hard yesterday I think mainly because the unusual sensations from LDN muddled my usual perception for pacing limits.
What is annoying is that this seems affect how other tried-and-tested medications seem to work: Nicotine patches have lately worked well for me as a crash-aid and a calming effect, and now the patch and my usual “downer” medications hardly seem to make any dent into the wired feeling and the current crash.
I called up the LDN-specialised apothecary and they recommended that I take a break and start again at a lower dose (e.g. 0.1 mg).
My tentative advice for others would be:
My ME/CFS grade is severe, and I am a person with strong chemical sensitivities and a history of reacting to medications at low doses. Don’t know if this can be predictive, but if you have similar sensitivities, maybe start at a much lower dose than 0.5 from the beginning. The apothecary said that starting at < 0.5 mg is not uncommon for ME/CFS. (Though I am curious if I could have less side effects at a much higher dose with the Norwegian backwards dosing scheme, I don't feel like risking a high dose. According to the apothecary, not everyone does well with a high dose either).
Don't start it at a time when there's lots of other things going on in your life that could be derailed by side effects.
If you have premenstrual syndrome (PMS) or pre-menopause symptoms in second half of monthly cycle, don't start it right before your period like I did ;-), but rather at the time of cycle when you feel best (otherwise PMS symptoms and side effects will overlap).