The Testing Blues Continue
We cannot get this outbreak under control until we know who is infected and have isolated them, and determined who they’ve been in contact with. Over a million test kits were reportedly on their way last week. They haven’t shown up in the stats yet. As of yesterday, the CDC reported 32,000 tests had been done. (S. Korea reportedly has the capability of testing 20,000/day.)
Diagnostic Solutions reported that after they get emergency FDA approval, they will produce mail-in kits that can be sent to homes (thanks Elena!).
Thermo-Fisher, a 25 billion dollar company, has received emergency FDA approval, but will be primarily supplying rapid testing machines and rapid throughput technology to labs and hospitals.
The UK biotech Mologic received a €1.1M grant from the UK government and The Wellcome Trust to develop a handheld diagnostic device that detects Covid-19 in 10 minutes.
The Feds
- Trump warns against gatherings of 10 or more people at one time.
- Plans to pump up to $850 billion, no make that $1 trillion (what a difference a day makes) into the economy including $500 billion in one-time cash payments by the end of April. That’s a lot of money, but consider that the estimated losses to the American economy over a 3-month span could be $10 trillion dollars.
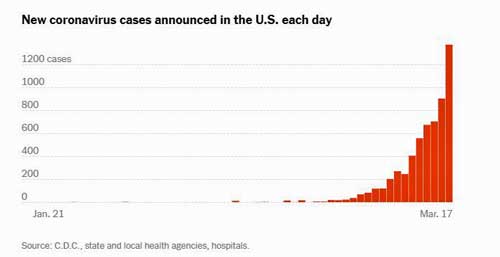
New Infections Spike
Every day we set a new record! Check out the curve. The confirmed cases in the U.S. were doubling every six days but are now doubling every two days. Increased testing is undoubtedly contributing to that, but so must be the spread of the virus.
The Next Italy? Francis Collins Suggests the U.S. May Have Eight, No Four Days…
On March 14th, NIH Director Francis Collins told the Atlantic things may get much worse soon. Note that this interview took place when the U.S. had 2,000 cases. It now has 7,324 confirmed cases (as of publishing time).
“If you look at the curve of new cases being diagnosed, we’re on an exponential curve over the course of the last month…Just look at the curve of what happened in Italy, and then look at our curve in the U.S., and you say if you go back eight days from today, they had about the same number of cases that we have today—that is, slightly over 2,000. And then if we follow that same track, then eight days from [March 22], we would be having the same kind of incredible crisis that they are facing.
If that’s true, we have only a very short period of time before this becomes an obvious national crisis with many people presenting with serious illness and hospitals quickly becoming very stressed with the ability to handle all of these sick people, especially older people who are at higher risk and who may need not just a hospital bed but even a ventilator.
Now we have a chance to change that, by applying now the most draconian measures on social distancing to try to limit the spread of coronavirus from person to person. But we will not succeed at changing the course from that exponential curve unless there is full national engagement in those commitments to try to reduce spread.
I think we’re getting there; certainly in the last few days there seems to be a lot of waking up to just how serious the threat is, but that’s obviously not universal across this large and complicated country.”
Collins warned not to expect this to be over soon:
“So anybody’s who’s imagining that this will all be over and done within a month, needs to get their mind around the fact that we’re in this, I think, for quite a long stretch of time… I think we’re facing the fact that at least until June, we all need to be in the space of taking this with the greatest seriousness—and that means every American taking responsibility about this and not coming up with reasons why it’s not necessary.”
Death Watch
The Washington Post reported that 85% of the first 100 deaths in the U.S. occurred in people over 60. Forty-five percent were older than 80 and many had underlying health conditions such as diabetes, kidney failure, hypertension or pulmonary ailments.
Politics Watch: How Not to Help Yourself
President Trump and his administration are now moving pretty rapidly, but yesterday, President Trump stepped on his experts’ words yet again stating that coronavirus was under “tremendous control”, and that his administration was doing a “great job” – right before he launched a trillion dollar, emergency effort in a last-ditch attempt to save the economy.
Yesterday, Trump also stated he “felt it was a pandemic long before anyone called it a pandemic”, which simply gave reporters the opportunity to point out all the ways that wasn’t true, including his January 22nd statement:
“We have it totally under control. It’s one person coming in from China, and we have it under control. It’s going to be just fine.”
Mixed Messaging Having an Impact

The U.S. is a very large and diverse nation. If we ever needed consistent messaging, it is now. A March 15th poll found that 80% of Democrats believe the worst is yet to come, while only 40% of Republicans do, leaving 60% of Republicans believing the worst has already happened – and presumably not practicing social distancing. Only 30 percent of Republicans said they planned to stop attending large gatherings.
The Democrats weren’t doing so well, either. At a time we all need to isolate yourself to prevent more spread of the virus, only 60% said they planned to stop attending large gatherings.
Hopefully, that number has gone down over the past couple of days. In Florida, though, Governor Santis’s refusal to close Florida beaches has led to scenes like the one above in Clearwater, Florida. We’re clearly not, as a nation, taking the disruptive actions we need to take to throttle this infection.
Singapore’s Success Story
If we’d had our act together, we might have ended up something like Singapore – which, just downwind of China – isn’t facing the health or economic catastrophe that the U.S. is. If any country was ready for COVID-19, Singapore was.
After the 2003 SARS epidemic, which didn’t kill or infect all that many people in the country (38/233 – deaths vs. infected). Singapore put a plan into place for which clinics to be used when another epidemic struck. When it did, it quickly banned travelers from China, used thermal scanners at airports, provided free testing, quickly identified everyone who was sick, traced their history, communicated about that, and produced an antibody test.
Thus far, it’s quarantined or isolated almost 5,000 people. As of today, Singapore is not on lockdown. It’s relying on a rapid identification of infected people to snuff out the epidemic. Neither is Hong Kong or Taiwan, both of which took a similar approach. They indicate that even densely populated regions can withstand the virus if they put enough resources into tracking it.
Update – Singapore reported its highest number of cases yet in one day (47), causing the government to order an immediate 14-day shutdown. Singapore has pretty effectively stifled community spread: most of the cases are now coming from people entering the country. Any Singaporean returning to the country will now face a mandatory 14-day quarantine.
The Super-Spreaders Among Us
About one in five infected people seem to be really, really good at spreading viruses around. Exactly why is not clear. They may be asymptomatic and not isolating themselves. They may have immune problems which allow the virus to replicate more. They may have lung problems which cause them to cough more. They may have a particularly contagious form of the virus.
Genetic analyses indicate that the Italy outbreak was initiated by two “super-spreaders” who spread the virus to 43 other people. A similar pattern occurred in Washington state. Super-spreading events also occur. As of March 12th, 77 of Massachusetts’ 95 coronavirus cases could be traced back to one event – a Biogen conference in late February. Large events, it turns out, are great incubating grounds for the virus.
Scary Models Pt. II
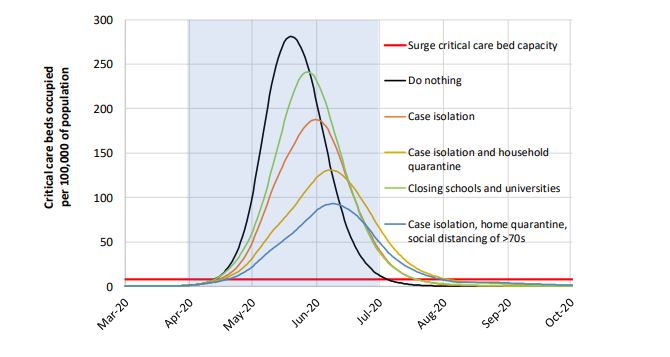
UK COVID-19 Response Team’s Scary Model to Stop “Herd Immunity” Efforts in the UK in their Tracks
The Imperial College COVID-19 Response Team delivered a sobering wakeup call to Boris Johnson’s government. Their modeling study found that the mitigation efforts Johnson was considering – to try to wall off the elderly and those at high risk from the infection – would help, but still leave hundreds of thousands dead and the healthcare system overwhelmed.
Full suppression efforts, on the other hand, which will at a minimum require social distancing of the entire population, home isolation of cases, and household quarantine of their family members, will help greatly but unfortunately, the model predicts that the die for many may already be cast.
The model shows how employing more and more extensive social distancing efforts dramatically reduces the height of the curve (number of critical care units needed), while pushing the curve to the right (giving us more time to prepare), and flattening it (so as to reduce medical resource needs at any one time).
The scary part, of the model, though, is the red line at the bottom of the graph on p.8 – the critical care bed capacity. Even in the best of scenarios, the model predicts the ICUs in the UK will become completely overwhelmed from around May 1st to August 1st. It should be noted that these models not written in stone – they’re based on best guesses. Let’s hope this one is not accurate.
Younger People Alone Might Be Able to Overwhelm the System
A table in the Imperial College’s document demonstrates why President Trump’s recent statement that most younger, healthy people will be fine is dangerous in the extreme.
Note that about 90 million people in the U.S. are between the ages of 20 and 40. Their assumed fatality rate from coronavirus ranges from .03 to .15. It appears that about 3 1/2% percent will require hospitalization and around .08% will die.
If a third of them get infected, about 1,650,000 will be hospitalized, approximately 80,000 will end up in the ICU, and 2,400 of them will die. That’s just from the healthy, relatively young adult group. The US has about 95,000 ICU units which treat about 4 million people a year, which suggests that many are probably already being used.
If large numbers of younger people become infected, they may, by themselves, have the potential to swamp the health care system. Govenor Cuomo today said that he expects that New York’s intensive care units will soon be full…
On the plus side, the Imperial College modeling showed that social distancing, plus home isolation of cases, as well as school and university closure, has the potential to “suppress transmission below the threshold of R=1 required to rapidly reduce case incidence”; i.e. to stop the epidemic.
Trevor Bedford, a Fred Hutch researcher, has a model which predicted 10-40,000 cases were present in the U.S. on March 13th. He strongly disagrees with statements that Ohio (or Arizona) already has 100,000 or so cases. He stated that exponential growth of the virus in the U.S. was beginning to occur on Friday.
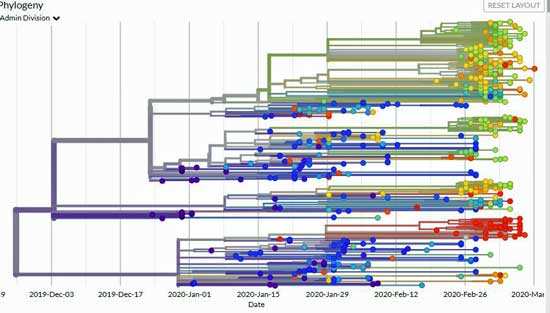
Bedford is using genetic sequences to determine where the infections may have come from.
“We can see all early samples from Wuhan are very genetically similar. Using the rate at which viruses evolve gives us a strong idea that this all came from a zoonotic event in late November to early December. After Wuhan, we see spread elsewhere in China. In February and March you can see areas like Italy and Washington state with clusters of viruses that are quite similar and suggest community transmission.”
His analyses suggest that all of the sequenced viruses in Washington came from a single introduction! That means the 1,000 confirmed cases and 50 plus deaths in Washington could have been prevented if that individual – who actually came from Wuhan – had been identified and isolated early enough. Until we’re able to do that, this scenario may play out again and again across the U.S.
“The outbreak in Washington has gotten bigger and bigger, and we’re beginning to see some sparks fly off of that. The seeming sudden appearance of outbreaks across the US are not due to a sudden influx of cases. Instead, transmission chains have been percolating for 4-8 weeks now, and we’re just now starting to see exponential growth pick up steam.”
Bedford’s model suggests that social distancing efforts will help but that “only large changes in contact rate can interrupt ongoing transmission” at this point.
The Gist
- Coronavirus cases in the U.S. spike to a new high with confirmed infections now doubling every two days instead of six.
- NIH director Frances Collins suggests that with the case numbers spiking, the U.S. may start looking like Italy, whose health care system has been overwhelmed.
- Singapore had a plan – and has kept its infections low – and the country largely open for business by relying on quick identification and isolation of those infected.
- Mixed messaging from the Trump administration and his allies has led to a sharp divide between how seriously Democrats and Republicans take the pandemic. SInce early social distancing is the key to stopping the virus’s spread, the mixed messaging could cost us dearly.
- A UK modeling effort suggests that aggressive social distancing efforts are needed to stem the virus’s spread. Even if they are implemented, the model suggests that beginning in May, the virus will overwhelm the U.K.’s medical system.
- A variety of drugs are being assessed – the most promising of which, Remdesivir, is currently being trialed in at least two places in the U.S. and in China. Other antiviral drugs may be helpful.
- No evidence of increased availability of test kits has shown up yet.
- The closure of the Pandemic office by the Trump administration in March 2018 severely handicapped the administration’s ability to deal effectively with the outbreak.
- Even if the office had been kept open, though, it’s likely that any administration would have found the virus tough going. Despite ample warning by the experts, the U.S. simply was not prepared.
Treatment Watch
Vaccines
The AP reports that dozens of research groups around the world are attempting to create a vaccine.
First attempt with a vaccine – a Seattle employee from a tech firm got the first potential coronavirus vaccine. The vaccine was developed by the NIH and the Moderna drug company.
Inovio vaccine – Another possibility by Inovio Pharmaceuticals is expected to begin its own safety study next month in the U.S., China and South Korea. Francis Collins said it will still take at least a year to get a vaccine out.
Curevac – The Coalition for Epidemic Preparedness (CEPI) and the German biotech CureVac have banded together to develop an mRNA vaccine. CureVac believes it will be able to be develop this kind of vaccine more quickly than traditional biologic based vaccines, and hopes to have the vaccine in trial by summer.
Drugs
Drugs, not vaccines, will likely be the first treatment and drug possibilities are pouring out as researchers and doctors across the world engage in an unprecedented effort to fight the virus.
On March 9th, the Bill & Melinda Gates Foundation, Wellcome, and Mastercard today committed up to $125 million in seed funding to identify and make available effective treatments. The effort – called the COVID-19 Therapeutics Accelerator – has made explicit their commitment to make the treatments developed available to all. The Accelerator aims to accelerate the evaluation of new and repurposed drugs in the immediate term, and other viral pathogens in the longer-term.
“If we want to make the world safe from outbreaks like COVID-19, particularly for those most vulnerable, then we need to find a way to make research and development move faster. That requires governments, private enterprise, and philanthropic organizations to act quickly to fund R&D.” Mark Suzman, chief executive officer of the Bill & Melinda Gates Foundation.
The clinicaltrials.gov site lists over 100 trials and studies featuring many different drugs that are underway for SARS-CoV-2. Drugs.com reported that European researchers have identified over 30 antiviral drugs that could be helpful. It will take time to determine which ones are actually helpful but the outburst in activity provides hope.
Remdesivir to the Rescue?
“We will know reasonably soon whether it (Remdesivir) works, and if it does, we will then have an effective therapy to distribute,” Anthony Fauci
Remdesivir is the top possibility right now. A broad spectrum antiviral drug developed to treat the dreaded Ebola and Marburg virus, Remdesivir has shown promise in the laboratory with a bunch of other infections (respiratory syncytial virus, Junin virus, Lassa fever virus, Nipah virus, Hendra virus) as well including possibly SARS-CoV-2 – the coronavirus sweeping the world right now – and SARS and MERS.
Francis Collins reported that, “I hope that a drug called remdesivir, which is now in clinical trials in China, Japan, South Korea, and the U.S.— will show that that particular antiviral has considerable efficacy for people who are very sick…”
Remdesivir was administered to a COVID-19 patient with pneumonia in the U.S. in late January in Washington. He improved dramatically the next day. In late January 2020, Chinese reported that of 30 drugs, remdesivir, chloroquine and lopinavir/ritonavir had “fairly good inhibitory effects” on SARS-CoV-2. On February 6, 2020, a clinical trial of remdesivir began in China.
The first Remdesivir trial in the U.S, which began on February 20th at the University of Nebraska at Omaha, included some patients from the Diamond Princess cruise ship. The trial participants will be sick indeed as they must display abnormal x-rays, require oxygen, or be in a ventilator.
That study is part of a large NIH effort expected to assess a variety of novel agents in up to 50 sites globally. It includes another Remdesivir trial currently underway at three academic centers in California. Another large Washington trial (n=400) is expected to end in May. Note that sometimes trials can be stopped early if efficacy is clearly shown. Remdesivir is not currently FDA-approved to treat any condition.
Other Drugs
Favipiravir or Avigan – A drug used in Japan to treat influenza was “clearly effective” at treating SARS-CoV-2 according to Zhang Xinmin, of China’s science and technology ministry (Thanks again, Laurie!). The drug was tested in a large trial of 340 patients in Wuhan and Shenzhen.
“It has a high degree of safety and is clearly effective in treatment,” Zhang
It took just four days for patients given the medicine to knock the virus out of their system. X-rays indicated lung improvements in the vast majority of the patients.
A Japanese health ministry official, however, said the drug was not as effective in the severely ill. The Guardian reported that a similar problem has been found with lopinavir and ritonavir, Even if that’s true the drug could help less severely ill patient pass the virus more quickly, and possibly prevent them from becoming more sick.
Chloroquine – (a cheap malarial drug) is another possibility. Chloroquine is a malaria drug with potential broad-spectrum antiviral effectiveness. A recent study “Breakthrough: Chloroquine phosphate has shown apparent efficacy in treatment of COVID-19 associated pneumonia in clinical studies” found it helpful with SARS-CoV pneumonia). One doctor speculated that chloroquine may be stopping the virus to attacking heme molecules in the blood. He also wondered whether SQ heparin might be able to inhibit or limit SARS-Cov-2 infection in the lungs, intestines and heart.
Hydroxychloroquine (Plaquenil) and Azithromycin – Professor Didier Raoult, the director of the IHU in Marseille, reports that hydroxychloroquine and Azithromycin, an antibiotic he states is effective against viruses. effectively reduced the viral load in 24 patients. The French government is now testing the drug combination on a large scale. One person reported that dozens of papers document the antiviral properties of Azithromycin. (Thanks Elena!) Medscape has a long and interesting article on this drug combination.
A recent “Communication” from China in the “Drug Discoveries and Therapeutics” journal lists some other potential options.
Antivirals – The communication titled, “Discovering drugs to treat coronavirus disease 2019 (COVID-19)“, pointed out that antiviral drugs including interferon α (IFN-α), lopinavir/ritonavir, chloroquine phosphate, ribavirin, and arbidol were included in the Guidelines for the Prevention, Diagnosis, and Treatment of Novel Coronavirus-induced Pneumonia produced by the National Health Commission (NHC) of the People’s Republic of China for tentative treatment of COVID-19. Recommended doses include:
- IFN-α – vapor inhalation at a dose of 5 million U (and 2 mL of sterile water for injection) for adults, 2 times/day (in vitro studies suggest it may be effective).
- Lopinavir/ritonavir – 400 mg/100 mg for adults, 2 times/day (in vitro studies suggest it may be effective). (A just published study suggests this drug combo is ineffective.)
- Ribavirin – via intravenous infusion: 500 mg for adults, 2 to 3 times/day in combination with IFN-α or lopinavir/ritonavir. (Shown effective in SARS study in reducing severe respiratory problems and death).
- Chloroquine phosphate – orally administered 500 mg (300 mg for chloroquine) for adults, 2 times/day.
- Arbidol is orally administered at a dose of 200 mg for adults, 3 times/day. The duration of treatment is no more than 10 days. (In vitro studies suggest it may be effective.)
Going for the Gusto – Using four drugs (Lopinavir 200mg, Ritonavir 50mg twice a day, chloroquine and oseltamivir (useful in swine flu treatment)), Indian doctors reported they cured one woman with COVID-19) (Thanks Laurie!). A February study published in Nature found that chloroquine and Remdesevir, in the lab, at least, worked effectively together to beat back the virus. (Thanks Matthias!)
Thirty Possibilities Outlined After using a drug screening in silicon and an enzyme activity test, a joint research team of the Shanghai Institute of Materia Medica and Shanghai Tech University reported 30 agents with potential antiviral activity against SARS-CoV-2. They include:
indinavir, saquinavir, lopinavir, carfilzomib, ritonavir, remdesivir, atazanavir, darunavir,tipranavir, fosamprenavir, enzaplatovir, presatovir,abacavir, bortezomib, elvitegravir, maribavir, raltegravir, montelukast, deoxyrhapontin, polydatin, chalcone, disulfiram, carmofur, shikonin, ebselen, tideglusib, PX- 12, TDZD-8, cyclosporin A, and cinanserin.
Chinese herbal medicines such as Rhizoma Polygoni Cuspidati and Radix Sophorae are also possibilities. Indian Auryvedic pracitioners recommend neem (Azadirachta Indica), Amalaki or amla (Emblica Officinalis), kutki (Picrorhiza Kurroa), guduchi/glioy (Tinospora Cordifolia), and tulsi (basil) to boost immunity.
Ibuprofen Warning! – the WHO warned individuals with symptoms of the coronavirus not to take Ibuprofen (e.g. Advil) because the drug may boost the levels of an enzyme that may worsen COVID-19 infections – and then took back the warning. (Thanks Penny!)
We Are All Responsible
This moment – the rising infection rates, the shuttered businesses, the economic carnage that is sure to come – has been roaring down the tracks at us. All we needed to know it was coming was to look at the birthplace of COVID-19 – China – two months ago. China knows flu viruses intimately. Most of our flu bugs originate there and other places in south and east Asia. Currently four influenza strains (A/H3N2, A/H1N1, and two B variants) circulate in the human population. Note that none of them are coronaviruses. The fact that a new virus, not like the others, was circulating and causing serious disease was our first warning.

No one, short of taking extraordinary measures, has ever been ever to stop a highly contagious flu virus…Why didn’t we get that and act sooner?
Our second was the huge hit that the healthcare resources in Hubei province quickly took in China. China’s healthcare resources don’t get overwhelmed because of “the flu”. China doesn’t build 16 large temporary hospitals or set up huge isolation camps, or close down 15 cities because of “the flu”.
This outbreak was different from the beginning. Somehow, we as a nation didn’t fully get that. Despite the fact that it’s been staring us in the face, we didn’t really get that there was no stopping it – not without extraordinary measures.
The coronavirus is not an Ebola virus spread by bodily fluids, or HIV spread by sexual contact, or malaria spread by mosquitos. It’s a highly contagious virus spread by little droplets in the air and on surfaces. If we’ve never been able to stop a flu virus, why would we be able to stop another contagious, respiratory virus?
The best we can do, short of taking highly unusual measures, is to blunt the flu’s impact with vaccines. Even then, the flu still kills 250,000 to 500,000 people annually worldwide. And now we’re shocked that the bug is here. It’s like we’ve woken up out of this dream world we’ve been living in. When asked about the dissolution of the Pandemic response team, Donald Trump for once, told the unvarnished truth – the truth that all of us needed to hear:
“This is something that you can never really think is going to happen.”
You never really think its going to happen, until it does. The truth is, though, that we’ve had plenty of warnings and we’ve largely chosen to ignore them. In the last 20 years, we’ve dodged two flu bullets – SARS and MERS. Both proved deadly but both lacked the crucial contagion factor that would have turned them into worldwide killers. NIH Director Francis Collins recently said:
“SARS was a terribly scary situation for the world 18 years ago, but it never reached the level of infections or deaths that we have for this coronavirus because it wasn’t as transmissible.”
A couple snips of those viruses’ gene pool, though, and we would have been looking at something far worse than COVID-19. Anthony Fauci in 2018 stated, “When you have a respiratory virus that can be spread by droplets and aerosol and there’s a degree of morbidity associated with that, you can have a catastrophe… Influenza first, or something like influenza, is the one that keeps me up at night.” Even after that, we weren’t ready.
March 10th, 2018
The closing of the Directorate for Global Security office by the Trump administration in March 2018 may, when all is said and done, end up being a key event, in the U.S.’s inept response to the virus thus far.
When the history of the COVID-19 pandemic is written, what happened on March 10th is going to go down as one of the all- time boo-boo’s.
That’s the date the National Security Council Directorate for Global Health Security and Biodefense was disbanded by the Trump administration Beth Cameron, the former leader of the unit, reported that the office was tasked with “doing everything possible within the vast powers and resources of the U.S. government to prepare for the next disease outbreak and prevent it from becoming a epidemic or pandemic.”
From monitoring foreign outbreaks, to identifying state and local needs, to clearing up testing snafus, she listed a long set of responsibilities – some of which are below:
- coordinating the efforts of multiple federal agencies
- identifying state and local needs
- backstopping testing capacity
- devising approaches to manufacture and avoid shortages of personal protective equipment (PPE)
- strengthening U.S. lab capacity (to process COVID-19 tests)
- expanding the healthcare workforce
- creating an information campaign.
Yet, when the unit was disbanded, I imagine that many of us never even knew about it. Its loss warranted one news story in the Washington Post on May 10th, 2018, which did lay out the fix we’re in today.
“Health security is very fragmented, with many different agencies. It means coordination and direction from the White House is terribly important.” J. Stephen Morrison, senior vice president at the Center for Strategic and International Studies.”
“What this all adds up to is a potentially really concerning rollback of progress on U.S. health security preparedness. It seems to actively unlearn the lessons we learned through very hard experience over the last 15 years. These moves make us materially less safe. It’s inexplicable.” Jeremy Konyndyk, senior policy fellow at the Center for Global Development.
The day before the unit was abruptly disbanded, Luciana Borio, at an event to mark the 100th anniversary of the 1918 flu pandemic which killed from 50-100 million people, declared, “The threat of pandemic flu is the number one health security concern. Are we ready to respond? I fear the answer is no.”
Despite the Cassandra-like warnings, there was no major outcry, no real effort to bring the task force back – and no attempt to really prepare this country for the likes of this flu epidemic. We, all of us, Republican, Democrat and Independent, have been a nation asleep.
Yes, a President who, while the sun was still shining, had rung the alarm instead of downplaying it, would have made a difference. An administration which went into crisis mode before the crisis appeared, which cut every bit of red tape it could to make sure we were armed with test kits, were diagnosing every person who was sick, were contacting their contacts, and made a point of warning again and again what was to come, etc. would have made a major difference.
It didn’t help that Secretary of Health Azar’s snit with the head of the FDA apparently resulted in the FDA chief from being left off the coronavirus task force. Unfortunately, the FDA is in charge of approving testing by private laboratories. As a small lab in Germany was providing the WHO with 1.4 million apparently quite effective test kits, the mighty U.S. produced a couple of thousand ones that actually worked.
It turns out there was a plan: it just didn’t get implemented because the test kits were balky. Francis Collins reported:
“There was a plan back in February to begin to sample in five cities anybody who showed up in an emergency room with a flu-like illness who tested negative for influenza—so that we could begin to find out what is the representation of coronavirus in the community. But that plan didn’t happen because the testing wasn’t working. We are now playing catch-up.”
The truth is that for all the Obama administration’s foresight in creating that task force, it probably wouldn’t have been ready for a flu pandemic then either. Nor, despite the fact that China birthed the SARS virus, was China. Maybe we should listen to our experts more.
A Slower-Moving Catastrophe – An Aside
It’s clear that if something is not happening right now, that we, as a species, have a tough time dealing with it. Right now the sun is still mostly shining – waves are not lapping at the first floors of the skyscrapers of Manhattan, Miami and San Francisco – but we might want to ask ourselves if the same thing is happening – but in slower motion and with larger consequences – with climate change.
The Coronavirus Series From Health Rising
- Coronavirus #I: Dark Sun: Reflections on the Coronavirus as it Heads For Town
- Coronavirus #2: Scary Models, 8 Reasons People with ME/CFS and Fibromyalgia Should Be Careful, How to Stop an Epidemic, Why You Should Trust No One and More
- Coronavirus #3: Is the U.S. Becoming Italy? A Singapore Success Story, More Scary Models, Remdesivir to the Rescue?
- Coronavirus #4: Lipkin Gets Hit, Testing Woes, Could the Models Be Wrong, Ikea Ventilators?, and What’s Next (???)
- Coronavirus #5: Lipkin, Bateman and Klimas Talk Plus Treatment Updates
- Coronavirus #6: Will COVID-19 Leave An Explosion of ME/CFS Cases in its Wake?
- Coronavirus #7: Records Broken, An ICU Doctor Talks, The Peak is Coming, Hot Spots, Is it in the Air? Dr. Hyams on COVID-19
- Coronavirus #8: The Grand Experiment, Starting Up? Social Distancing – For 2 Years? WHO Did It?







Thank you excellent article.
Why are you calling a flu? It is a cold virus, for all the helpful info, it puts your knowledge into doubt when you call it a flu.
You’re correct – it is not a flu virus but I haven’t called it a flu virus. Check out the first blog – https://www.healthrising.org/blog/2020/03/12/dark-sun-coronavirus-chronic-fatigue-fibromyalgia/ – for SARS CoV-2 relationships to other viruses.
I use the flu as an example because it’s the closest thing we have to what’s happening with this virus. Whether its a coronavirus or a flu virus, in some ways it’s distinction without a difference as both types of viruses act in very similar ways.
Both coronavirus and flu viruses are highly contagious respiratory viruses that tend to circulate at the same time of year. The “flu pandemic” that Anthony Fauci and others have been warning about for years is clearly the coronavirus pandemic we’re facing now.
I will make it more clear, though, that this is not a flu virus.
Chloroquine is interesting, potential interest for CFS? As it helps with autoimmune disease as well as viral. Publication in Nature journal:
https://www.nature.com/articles/s41422-020-0282-0?fbclid=IwAR2JbbZU_Hl7uLjuOTDhrNnmczzyEFvnIhY8QHv9ghY5fYBvX0IsmnhD07w
Interesting – the drugs are already popping up – a good sign.
I really do think this drug is worth looking at for CFS – has antiviral and anti-autoimmune actions. Thoughts? Any takers?
https://www.nature.com/articles/s41598-019-52085-w
Unfortunately, this drug -and others- doesn’t work as well as hoped. It is already used in Europe and have many side effects.
This is the best reporting I have seen about this and its many potential tangents, after I’ve pored over countless mainstream and other media. This should be everywhere on the web and wire services. Extremely well done – thank you!
Thanks! The coronavirus and its ability to affect so many things is disturbing and fascinating at the same time. This is something we will remember…
Well said. Thank you, Cort.
Great series, Cort!
Thank you Cort!
It is kind of ironic that I am spending the 30th anniversary of getting ME/CFS fighting off a weird cold that is probably COVID-19.
Don’t worry, I’m isolating at home.
Good luck!
Thanks!
I’m almost over it! My Enzyme Defense did not arrive in time. So the most helpful things have been my salt inhaler, Xclear nasal spray, and meditating.
Update: Lauricidin and 7 Precious Mushrooms extract have been my most important supplements. I was taking them for granted! I had been taking twice as much as usual for a week, and I felt like I was getting too inflamed, so I stopped them for a few days.
Boy do I regret that! The virus came roaring back, right as I was almost over it. It is a really stubborn illness. Really hard to kick out.
Whew! Lauricidin saved my hide again. I am better.
If you are going to try it, please remember that when it kills viruses it will increase your level of inflammation. So start it gradually and always take it with some kind of anti-inflammatory.
I use mushroom extract, but whatever your favorite anti-inflammatory thing is would probably work too. Hey, aren’t enzymes anti-inflammatory? If they are, then the perfect combination might be Lauricidin plus Enzyme Defense.
Also, please get lots of liquids, fiber, magnesium and vitamin C. That way the dead viruses will be excreted quickly. The dead viruses feel toxic.
I only had a mild case, and it lasted 14 days. It is no joke. Everyone please fight the good fight, and try to keep yourself out of the hospital!
It doesn’t appear that we would have been on top of this virus no matter what was done in 2018. Luciana Borio (whoever that is) stated the answer to being ready for a pandemic was (no) This agency had been around since 1947. Is this just another portion of our govt. that doesn’t function properly? Some learned from SARS and that was 2003, what did this dept do from 2003 to 2018? I live in Florida and I can say the Clearwater mob disturbed me (but) remember it is”Spring Break” and this is in front of the Hotels and the majority of the crowd is from (other States) and people who allowed their 18 yr old adult children to come to Florida during the pandemic and I will bet that most of them lived at home and were not supporting themselves. Our society as a whole is not taking this seriously but one cannot cause panic either.
I was astonished the read the Mayor of Miami Beach – who has tested positive – kind of pat himself on the back for closing down restaurants and bars at midnight! I know it’s a tough time to do that with Spring break at all but I would bet infected young people from Florida are going to spread the virus across the Eastern United States
Update – all restaurants and bars have been closed in Miami
Yes the White house makes recommendations and different areas make (their) rules. The governor also made recommendations after he saw Clearwater and said all bars and clubs were closed (the day before St. Patties) doesn’t look like Miami complied. I think the old adage goes you can bring a horse to water but you can’t make him drink.
Thanks for the info Cort! Helpful as always. It’s a mighty challenge to lead our country out of this challenge. Hopefully Trump will swiftly help lead us out of this abyss, and his performance can be honestly judged for all to see. The truth is hard to find these days.
https://www.washingtonpost.com/opinions/2020/03/16/no-white-house-didnt-dissolve-its-pandemic-response-office/
You beat me to it! I was going to share that same editorial. But what amazes me is that the CDC apparently never planned for a extremely contagious pandemic like this. Isn’t that their core function? They should have been much, much more prepared.
Actually the CDC did plan for this – and as the blog reported had a plan in place to start testing people early. Somehow, despite the fact that the CDC has done this before, the test failed – and they didn’t have a good backup plan.
As to that editorial – think about this. Think about all the things that Directorate was supposed to do – and all things that were done – and then see if closing it made a difference. That editorial asserts that the functions of the Directorate were simply shifted to another place – but since the functions of the Directorate were obviously not carried out – look at where we are today – whatever happened was clearly not effective.
You might also check out a piece from the Head of the Directorate, herself, on it being closed and all things it would have done if it had, in fact, been there. https://www.washingtonpost.com/outlook/nsc-pandemic-office-trump-closed/2020/03/13/a70de09c-6491-11ea-acca-80c22bbee96f_story.html
It is indeed a mighty, mighty challenge. As to that office being closed – check out a piece by the head of the office when it was closed for another opinion – https://www.washingtonpost.com/outlook/nsc-pandemic-office-trump-closed/2020/03/13/a70de09c-6491-11ea-acca-80c22bbee96f_story.html
I would be leery of azythromycin. As a longtime ME/CFS patient, I was diagnosed with bronchiectasis with suspected MAI (mycobacterium) after loss of lung function and constant coughing.
After I found a good pulmonologist, she got a sputum sample from me which tested positive for MAI.
She told me azythromycin is thought to feed MAI.
For any of us with ME/CFS things are always a toss-up, but if you can possibly find a good doc who will test you for positive MAI, and thereby exclude azythromycin from any treatment for any infection, please do.
I have not needed any antibiotics for respiratory infections since starting strict nasal passage hygeine with aerosol saline spray, and washing eyes every night. Fingers crossed.
But I know that should I need an antibiotic, azythromycin is excluded.
I hope everyone will test that out before considering the azythromycin protocol.
You know, Enzyme Defense by Enzymedica was in a study back when it was called Virastop, and it was found to be AS effective as azithromycin in treating shingles.
So I think it’s a good broad spectrum antiviral.
Cameron, Have your doctor send your next specimen to National Jewish Health if you need treatment, they are in Colorado. Previously know as National Jewish Center. It takes several weeks to grow MAI and there are different types and they test different antibiotics against the specific types. If needed sometimes there are multiple antibiotics given.
People should beware of false information being perpetuated on social media and even by some mainstream media who has intentionally made this terrible situation political. Pointing fingers doesn’t help anyone. If the medical professionals knew of a better means to address the illness, they would have made this clear to all. they are doing the best that they can.
We are in the infancy of this pandemic in the U.S. so it’s only reasonable to expect it to ramp rapidly as there is no means to isolate everyone. Testing won’t stop the spread only isolation can. We should all expect a long drawn out process as the more the healthcare professionals are able to slow the spread the longer the virus will exist. With no current vaccine we’ll need to ride out this storm using good judgment and isolation.
An excellent article – thank you Cort. Best reading since this all started.
Thanks
Nurses and docs displaying online signs asking for public to do their part by ‘staying home’ because the health care professionals are ‘doing their part’ by going to work…..risking infection….and therefore lives…..
There was a health care professional on social media early on who asked her fellow citizens to
‘stay home’ ‘do not eat out’
‘if you are healthy now, next year you can visit family’
cautioning against gatherings for new year celebrations.
I wonder if citizens from home will be called upon to try to be part of systematic alert of those who have been exposed?
For surely it must be labor-intensive to track down people —even if some might be alerted through online connections.
Still unsure of reason why Seegene—Korean company’s test kits —are not being purchased and used now in North America:
https://www.google.ca/amp/s/amp.cnn.com/cnn/2020/03/12/asia/coronavirus-south-korea-testing-intl-hnk/index.html
Hopefully, if it is true US military invested in company that has created vaccine, then perhaps this vaccine will also be fast-tracked.
Maybe why US unwilling to order tests from South Korean company Seegene
is because US invested in vaccine from plant based production technique.
https://www.defenseone.com/technology/2020/03/breaking-weve-got-vaccine-says-pentagon-funded-company/163739/
Feel that you are saving lives, Cort, by your taking the tangled ball of info and with deft manuveurs, placing a life vest into our hands.
Anyone thinking of having their family get together please read this horrific story of an Italian family which was ravaged by the virus after a family dinner – https://www.nytimes.com/2020/03/18/nyregion/new-jersey-family-coronavirus.html
Cort, the latest advice from WHO is not to avoid ibuprofen – see update to this article:
https://www.sciencealert.com/who-recommends-to-avoid-taking-ibuprofen-for-covid-19-symptoms
Thanks – I added that to the blog.
Cort – blog still says not to TAKE ibuprofen. The update says not to AVOID ibuprofen.
Updated: WHO Now Doesn’t Recommend Avoiding Ibuprofen For COVID-19 Symptoms
AFP17 MARCH 2020
Editor’s note (19 March 2020): Since the publication of this article, the World Health Organization has updated its advice on the official Twitter account: “Based on currently available information, WHO does not recommend against the use of ibuprofen.”
Excellent article Cort. Here in the UK starting soon any person aged 70 and older, pregnant women and any person with any pre existing health condition will be required to stay in isolation for up to 4 months. It’s a drastic step that I believe most people will adhere to.
Most ME / CFS patients have been living in some sort of quarantine for years or decades. People are already complaining about a few weeks in quarantine, Isn’t that ironic? And nobody didn’t care about us for all those years.
Gijs, Ronald Tompkins MD, Chief Medical Officer of the Open Medicine Foundation has sent a message out via an email from the OMF.
Amongst other things he says: ‘For those who have been dealing with ME/CFS as a disease over time, social distancing with avoidance of infections has been a way of life.’
He goes on to say: ‘Perhaps, through this crisis, others will come to understand what ME/CFS really means to one’s way of life and ultimately, we may find support to a better understanding of ME/CFS, to treatments, and possibly a cure.’
Dear Cort,
This series on COVID 19 is extremely appreciated.
I send the link around to my loved ones. One of them, who happens to be a resident in internal medicine, told me, about the first one I sent her “Dark Sun”, that it was the best, most complete vulgarisation on the subject and found it very helpful.
I’m Canadian. We try not to politicize dangers to our health, especially not in Quebec, where a never seen before solidarity between the different parties at the National Assembly has boosted individual efforts to follow Public Health’s experts’ recommendations. And, just to show how politicized we could be if we wanted to : for such a small nation, we have not two, not three but four different parties representing us. 🙂
So thank you again and know that the learning curve your hard work is creating shows an exponential propagation!!
Glad to hear the intern liked it. Thanks Genevieve.
This is pretty much an exponential learning curve for sure. 🙂
Excellent, excellent synthesis of the most salient information, thank you!
Your graphs are ones I have not seen, and very helpful.
CFS patients probably don’t have do much about the stay-at-home order that is in place for the entire CA as of today. We already stay home most of time and go out only for essential errands and short walks. We are already socially distanced, all we have to do is stay 6 feet away from other people on rare occasions that we go out. We are exemplary citizens 🙂
We won’t be the ones spreading this one around – that’s for sure. 🙂
This can’t continue, the next one is already being brewed. U.C. Berkeley published a study in late February finding that many if not most of these virus come from contact with bats because bats have a very strong immune system, thus a virus must be strong to overcome. All contact with bats must be prohibited immediately, for the good of all.
Cort: Please tone down the politics
I don’t know how you can take “politics” out of this but first a definition:
Politics: the activities associated with the governance of a country or other area, especially the debate or conflict among individuals or parties having or hoping to achieve power. (google dictionary)
Reporting: to give a spoken or written account of something that one has observed, heard, done, or investigated.
According to the definition politics involves debating which individuals or parties would be better running this country. That is not happening in this blog. This blog is reporting on what happened and why it happened. Of course in this hyper-partisan time this will seem to have political overtones.
But what is one to do? Just bury one’s head in the sand? Unless we pay attention to what happened now. Unless we have a very clear idea of what went wrong now – not later – now – so that its embedded in our brains. – history will repeat itself. If we try to cover over what happened this is going to happen again.
Instead of worrying about whether something is political or not I assert we should be taking a fine-toothed comb to everything that has happened.
The cost to this country – to our futures – probably to funding for ME/CFS and similar diseases, because we’re basically mortgaging the federal government’s future with the trillions of dollars of debt the economy will now need to survive – is simply too great to ignore.
That’s my opinion. I’m not sleeping well at night but not because I’m afraid of the virus but because I’m waking up aghast at how cavalierly this incredible threat was taken.
Cort –
I respectfully disagree with your belief that the Chinese Wuhan virus has been taken cavalierly by anyone especially the POTUS. In the U.S. president Trump was criticized for acting proactively in stopping travel from China. He was labeled a racist even though the Chinese Communist government failed to even disclose the epidemic until it had spread drastically. There is no playbook for this type of pandemic in the U.S. in modern times.
https://www.cnsnews.com/article/washington/melanie-arter/trump-nbc-called-me-racist-banning-travel-china
https://www.mrctv.org/index.php/blog/watch-trump-gives-perfect-response-after-reporter-asks-why-he-calls-coronavirus-chinese-virus
There has been a lot of political hate mongering before and during the Chinese virus pandemic. The Dems are even preventing a stimulus bill from passing that would help those of us suffering financially from this economic disaster.
Some of the Democratic governors finally admitted that the Trump admin is doing a good job.
https://www.mrctv.org/index.php/blog/some-trumps-outspoken-critics-are-praising-his-actions-coronavirus
Most of the liberal U.S. media has been promoting political divisiveness instead of unity. Little has been done to scrutinize China’s damage to human life world wide.
https://www.newsbusters.org/blogs/nb/rich-noyes/2020/03/23/study-china-escapes-scrutiny-tvs-coronavirus-coverage
I’m not sleeping well not knowing if I will have a job, can pay the rent or buy food. That’s a lot more important to me than maligning the POTUS and his admin for doing the best they can in a pandemic. Hindsight is always 20-20 and if people want to find fault they will even when their attacks are meritless. Maybe people should take a deep breath and stop the politics and work towards uniting our country and mitigating the China virus as best we can.
But Jorg, I say the US treated the coronavirus cavalierly in the beginning and in response to that you cited the travel ban – which I noted did occur – then veer off to a racial issue, and then take up the present stimulus issue – which didn’t have anything to do with the question whether the US treated the epidemic cavalierly at first.
You’re right that I need, for myself and others :), to stop relitigating the past. So here’s my last take on it:
In Wuhan city was shut down in January every infectious disease expert knew we were going to get hit. if we’d had that pandemic office, if we had been warned then, if our leadership had made that a point in late February, if the virus had not been compared to the flu, or the media coverage called a Democratic hoax – lulling tens of millions of people into a sense of false security, if we had begun to stockpile the needed supplies (cotton swabs, reagents, personal protective equipment) early, if the FDA had been pushed to approve private tests early, etc. – maybe we could have had a chance at snuffing this out as it showed up, instead of holding our breath, watching it wash over us, and watching our economy go down the tubes.
To be fair only 3 or 4 countries got it right. We are not alone at all.
Nor is it all Trump’s fault. We clearly weren’t prepared in ways he didn’t have anything to do with. The CDC wasn’t prepared for problems with their test, the FDA lagged along for far too long. We didn’t have the stockpiles we need.
Any administration – Democrat or Republican – would have been hit hard but to have President Trump got out again and again, contradicting the experts -saying this is under control – when it was like a tsunami barreling towards us. That’s hard in hindsight to take. The National Security guys have apparently been sounding the alarm to the White House since January.
Thankfully Trump has seen the light. He declared a National Emergency, emphasized social distancing, etc. History will judge if he’s done enough.
Now he’s going to have to make some really tough decisions. Do we keep the social distancing up and watch the economy tank or do we relax, restore the economy and then watch some people. My guess is that he’s going to do the later and that’s an understandable decision.
Cort,
You are being duped by the unscrupulous Liberal media who’s goal is to prevent Trump from being re-elected in 2020. This is irrefutable but I’ll prove it to you. It’s also worth noting that I did not vote for Trump in 2016…
Trump did not create the Wuhan virus nor is he responsible for it spreading. That would be exclusively China’s fault. Neither the U.S. nor anyone else would have expected China to hide a contagious virus for a month or more while it spread out of control. The removal of a CDC position in China occured months before the China virus happened. Again the Libs are desperately seeking to make Trump wrong for this by their smear campaign.
The media didn’t have much to report about the Chinese doctor who disclosed the epidemic and later died from it after China censured him for reporting it, did they? Why was this not front page news for weeks? Why has China not come under intense scrutiny for their incomprehensible murder of innocent people world wide? Do you see the media’s agenda?
https://www.usatoday.com/story/news/world/2020/02/06/doctor-coronavirus-death-epidemic-wuhan-china-spread/4678344002/
Trump has tried to prevent public panic while the Liberal media conspired to create it. Trump stated his beliefs that the Wuhan virus was similar to the flu because that was his understanding in the beginning. He was not downplaying it he was activating all of the medical resources.
There were in fact some test kits that were incomplete as well as some incorrect. Trump did not produce the kits so how could he be responsible when he had the medical experts handling this aspect? The reason for delaying private local labs developing test kits was because they needed proper guidance as to the appropriate test procedures.
Testing will not stop the spread of the virus. Isolation will not stop the spread of the virus forever as eventually people will have to leave their homes. Testing and isolation will SLOW the spread, not stop it. Again the U.S. has never had to address a pandemic in our lifetime so there is no playbook. Finding fault is easy in a crisis but it’s counterproductive and futile. It doesn’t make anything better it just divides the country.
There was no 3 out of 4 countries that got it right AFAIK. The only country that even came close to “getting it right” as you say would be Taiwan due to their past experience with SARS. Taiwan is a very small country compared to the EU or U.S. with a population of less than 24 million.
https://foreignpolicy.com/2020/03/16/taiwan-china-fear-coronavirus-success/
It was perfectly fine for all of the media to refer to the China virus as the Wuhan (China) virus for weeks until Trump referred to it as the Chinese virus. The POTUS specifically referred to it as the Chinese virus AFTER Communist China propagandists alleged that a U.S. soldier brought the Wuhan virus to China which is absolutely false.
That is why Trump started and continues to make it crystal clear that the Communist propaganda is a lie, much as the Liberal media claims are a lie because they both have an agenda to disparage the POTUS and U.S. for personal gain.
Watch the video which is all before Trump properly labeled the Wuhan virus the Chinese virus and count the number of times the Liberal media called it the Wuhan virus which now is unacceptable so the media claims. There is no racism involved at all because China is a country not a race and Asian is a race not a country. This should be obvious.
https://thefederalist.com/2020/03/13/woke-media-calls-term-wuhan-virus-racist-after-using-term-wuhan-virus/
In regards to the “hoax” once again we find the Liberal media lying. FACT checkers have stated in no uncertain terms that Trump did NOT call the Chinese virus a hoax. The POTUS stated that the Dems and unethical media were using the Wuhan virus as a hoax against his administration. I’m pretty sure anyone who understands the English language knows the difference yet the evil lib media continues to perpetuate the “hoax” lie which is why they are now being sued because they know it’s a lie yet they continue to spew hate.
https://www.politico.com/news/2020/02/28/trump-south-carolina-rally-coronavirus-118269
https://www.factcheck.org/2020/03/trump-and-the-new-hoax/
Trump has used a measured response as the pandemic has spread because the U.S. has seen how badly the situation is going in Italy and they don’t want the U.S. to suffer such devastating results. At no time in our lifetime has the U.S. had to deal with a pandemic of this magnitude with no vaccines or means to stop the spread.
There are NO good options on how to proceed. Locking down the country can only slow the China virus. Unless a vaccine is developed it is likely that everyone will get the virus eventually. All we can do is protect ourselves, use the brain we have been given and stop believing the lies and fake news perpetuated for personal gain. The lnks about illustrate the lies have been fact checked and proven to be false allegations perpetuated by evil people with an agenda. Don’t be gullible.