

The Grand Experiment: California vs Kansas, South Dakota and Sweden
Across the world a grand experiment is taking place between countries and states which have employed aggressive social distancing measures versus those which have employed less restrictive ones. The more aggressive social distancing measures produce more economic costs, but will hopefully reduce infections, deaths and the time the economy needs to be partially shut down. Less aggressive social distancing efforts may reduce economic costs, at least in the short term, but may produce more infections over the longer term.
Three states in the U.S. exemplify these differing approaches: California, Kansas and South Dakota. The goal of social distancing is to “flatten the curve”; i.e. reduce the number of infections so that the infection dies out more quickly and with fewer deaths, and possibly less economic pain. Let’s see if it’s working.
California Surprises
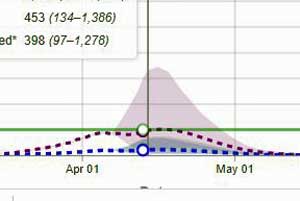
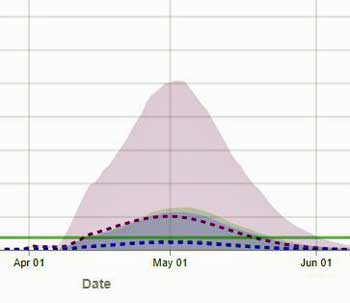
The IHME model for California (https://covid19.healthdata.org/united-states-of-america/california) shows the lowest, flattest and shortest curves – suggesting that the state should be able to get back to business earlier.
By all rights, California should be a basket case right now. The most populous state in the nation, it’s the main entry point for people coming from China and they have been coming – in the tens of thousands over the past month or so. Yet California is doing well.
Gov. Newsom’s March 19th, stay-at-home order, which also closed educational services and non-essential services, basically shut the state down.
(Contrast that with the federal government’s more moderate March 16th recommendations to not gather in groups larger than ten and to avoid bars, restaurants, etc.)
The Institute for Health Metrics and Evalation (IHME) April 13th model projects that California hospitals will meet their peak resource use tomorrow, and that California is well-prepared. The model also projects a remarkably small and shortened curve: i.e. it appears that by acting quickly, big, heterogeneous, busy California has dramatically “flattened the curve” and will be able to open for business earlier than other states.
Kansas
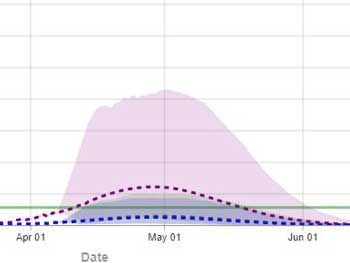
The IHME model for Kansas shows a broader curve, stretching into early June, suggesting more viral activity over time.
Kansas closed its schools before California (March 17th) but didn’t implement a stay-at-home order until March 30th, and never closed non-essential services.
The IHME model predicts that Kansas will reach its resource peak two weeks later than California (Apr. 29th) and has a significantly higher and longer coronavirus “curve” than California; i.e. it’s projected that the virus will be present and placing a significant strain on hospital resources much longer than in California.
South Dakota
South Dakota closed its schools even earlier than Kansas (on March 16th), but never implemented a stay-at-home order or closed non-essential services.
The IHME model projects that those decisions may cost the “Mount Rushmore” state. The projected curve of increased hospital needs will be more intense and be present longer than either California or Kansas – lasting well into June.
Sweden
According to the IHME, Sweden hasn’t implemented any of the four major social distancing measures: it hasn’t produced a stay at home order, it hasn’t closed non-essential services,and it hasn’t closed schools or severely restricted travel.
Sweden has become a kind of icon for a less top-down approach to the virus which emphasizes individual responsibility.
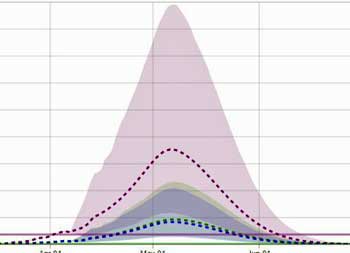
The IHME ((https://covid19.healthdata.org/sweden) predicts Sweden’s approach will cause it to be hit harder and longer, and that its hospitals will be overwhelmed for almost two months.
The IHME, though, predicts that Swedish health system will soon get overwhelmed and stay that way for almost two months.
Time will tell if the models are correct. There will also surely be an accounting of economic costs vs lives saved.
The Midwest Advantage
Some Midwestern states have taken advantage of their geographical isolation from the coasts, and the time that has afforded them, to implement contact tracing and may not need to shut down their economies.
A robust testing and contact tracing scheme is the best of both worlds: infections are quickly identified and walled off while the economy mostly hums along. The failure of the U.S. and other countries to institute robust testing and contact tracing protocols is one reason so many nations have been hit so hard – both economically and medically.
As the infections drop, the U.S. will have another chance at instituting a rigorous and thorough testing and contact tracing regimen.
The Next Steps
To say restarting the economy is difficult during a pandemic is to understate matters.
The number of new, confirmed cases daily has leveled off in the low 30,000’s and begun to drop. The number of tests being done every day (135,000) has also leveled off, making it a bit more difficult to say that the rate of infections is increasing.

As the virus recedes it will leave many, many, (many) potential victims behind should it re-emerge again.
The problem is that even after all these infections and deaths, and even as social distancing tamps down on the virus, and even as the curve flattens and falls, the vast majority of the population will still remain at risk from the virus – giving it plenty of “ammo” to rise up again. The U.S., after all, has about 600,000 confirmed infections. If ten times that number are infected or have been infected, that still leaves 320 million potential victims.
Dramatic times call for dramatic actions. We got through the 2008 financial crisis only because the FED and the Dept. of Treasury threw out the rule book and embraced every opportunity – even those which went against their belief systems – to save the economy.
Bill Gates in 2015
The next outbreak? We’re not ready | Bill Gates.
Can the U.S. do it? Bill Gates doesn’t think so. Gates, who’s been warning about a pandemic for years, and who’s been funding the organization – the IHME – whose models many have been using, said he believes that the federal government is still focusing on the wrong thing.
Coronavirus in the U.S. he said, is “still completely mis-prioritized. The natural thing would be to do like South Korea did, and create a unified system — that we haven’t gotten any interest from the federal level.”
Any test results, Gates asserted, have to come quickly enough for someone to isolate themselves before infecting someone else.
Testing Woefully Inadequate For the Next Step?
In order to safely prevent that from happening, the U.S. has to be able to quickly identify the infected – particularly the asymptomatic people – whom many believe are inadvertently driving the infection. That will require enormous amounts of testing – far more than the U.S., even with its dramatic ramp-up in testing over the past month, has been able to achieve thus far.
We shouldn’t pat ourselves on the back too much regarding testing. Germany, a much smaller country, is able to produce almost as many tests a day (120,000 – 135,000) while many places in the U.S. are still missing the reagants, swabs, etc. needed to do testing.
Does the U.S. really need to do millions of tests a day – and if it does, could it find a way to do that? (Image by Gerd Altman from Pixabay.)
Estimates suggest that from 750,000 to millions of tests a day may be needed for the U.S. to be confident that it can identify those who are ill, quarantine them, and reopen its economy. One researcher wants the U.S. to test 25-35 million people a day and to continue doing that for several months. In a phone call, Ron Davis said he thought hundreds of millions of tests would be needed over time.
Doing something like that would probably require the U.S. essentially going into war status, and having the federal government use all its powers to implement the testing – something the Trump administration has been leery of doing.
An international team of researchers, however, has recently formulated a genetic test using barcodes which they say could easily be mass produced and provide millions of tests per day. Fifteen years ago, Ron Davis tried to get a grant from the CDC to produce a $1/test kit that could have been used for this very situation. (More on that later).
Dramatic Undercount of COVID-19 Deaths Expected
The 20,000 or so people who have died in the U.S. from COVID-19 is almost surely an undercount – a significant undercount. It has to be. Until recently, COVID-19 testing has been so pitiful that it wasn’t possible to test many people who died and their deaths were listed as heart attacks or pneumonia or other illnesses. All you have to do is track overall death rates to understand that our COVID-19 death rate is likely way off.
Cardiac arrest calls resulting in a death in a home jumped fivefold in New York City in the last half of March. A New Orleans doctor, Geraline Menard, reported: “When I was working before we had testing, we had a ton of patients with pneumonia. I remember thinking it was weird.”
This week, the CDC reported that the percentage of death attributed to flu and pneumonia is 10% – above the epidemic rate of 7.0%. The CDC stated: “The increase is due to an increase in pneumonia deaths rather than influenza deaths and likely reflects COVID-19 activity.”
Social Distancing For Two Years?
“Under current critical care capacities, however, the overall duration of the SARS-CoV-2 epidemic could last into 2022, requiring social distancing measures to be in place between 25% (for wintertime R0 = 2 and seasonality; fig. S11A) and 75% (for wintertime R0 = 2.6 and no seasonality; fig. S9C) of that time.” Kissler et al. 2020
A Harvard study published in Science that modeled the coronavirus infection over five years smashed any ideas that the SARS CoV-2 coronavirus will be a “one-and-done” thing. The models predicted that unless we want to see hospitals overwhelmed by virus victims, some form of social distancing will likely be necessary, at least on and off, for a couple of years.
Vaccines and herd immunity are what we count on to stop contagious viruses but we don’t know whether either will be effective. The problem with a vaccine is that coronaviruses, like all viruses, mutate. Mutation is only a problem if it occurs in the parts of the virus (its antigens) the immune system uses to recognize it and respond to it. The measles virus mutates so little in that part of the virus that a vaccine developed in the 1950’s is as effective today as it was then.
Coronaviruses, though, are cold viruses. Researchers have found 11 places it’s mutating – one of which allows the virus to attach to lung tissue. Thus far, little change has been seen in that part of the virus, but that could change as the virus starts to tangle with the immune systems of those who have become immune to it. Once that kind of evolutionary pressure comes to bear, the virus could start altering that area, rendering the vaccine less effective or ineffective.
Herd immunity, on the other hand, will help – but studies suggest that some recovered patients are not mounting a strong antibody response; i.e. they could quickly be re-infected again – and so will not contribute strongly to herd immunity.

Will we be practicing social distancing on and off for the next couple of years? (Image by Omni Matryx from Pixabay)
Herd immunity is also likely not a great long-term option for SARS-CoV-2 because, if it’s like other coronaviruses, immunity will be short-lived – leaving those who recovered from it susceptible again a year or two later. (They tend to have less severe infections, though.) That suggests surges of the virus could happen every couple of years.
On the plus side, it’s possible, but not known, that people exposed to other coronaviruses via the common cold may have some immunity to SARS-CoV-2. If that’s true, SARS-CoV-2 infections could dramatically fade, and then once that immunity lapses, surge again in a couple of years.
While it’s not clear how effective a vaccine will be, a vaccine will certainly help. Developing treatments to blunt the severity of the infection will be crucial. Building out more intensive care units may be needed. It sounds like regular testing may be in our future for some time to come as well.
Clearly we’re in a great battle and the scientific community, at least, is rising to the challenge – creating collaborations and devoting resources that have never been brought to bear on a pathogen before. New tracking tools are being developed. Hundreds of clinical trials are underway. Automatic intelligence is being brought to bear. The amount of sophisticated technology being brought to bear on this virus is incredible.
If we can just get along and work together, maybe we can beat this thing more quickly than we think. Speaking of that…
WHO Did It?
The race is on to understand how the best prepared country in the world for a pandemic (remember that?) ended up leading the world in confirmed infections (now over 630,000) and deaths (26,213). Unfortunately, it looks like innocent lives are going to get ground up in the battle to lay blame.
Putting forth the argument that it was ‘them”: it was the World Health Organization (WHO) that essentially crippled the U.S.’s response, and so the Trump administration cut off funding to the biggest international health organization for 60-90 days. President Trump accused the WHO of “severely mismanaging and covering up” the coronavirus outbreak and said:
“Had the WHO done its job to get medical experts into China to objectively assess the situation on the ground and to call out China’s lack of transparency, the outbreak could have been contained at its source with very little death.”
There’s little doubt that the WHO could have acted more quickly, but the organization’s unique constraints should be noted. In order retain access to countries, the WHO rarely directly criticizes sometimes touchy government officials. During the Ebola virus epidemic, the WHO was similarly critiqued for not declaring a state of emergency earlier. It apparently held off doing that in order to keep access to the countries.
The funding stop – the U.S. funds a third of the WHO’s activities – won’t hurt the U.S. in the short run but it’s hard to believe that it won’t hurt many of the most needy at the time they will most need it. The developed world is getting hit harder right now because it’s more connected, but given the many densely packed cities with poor resources in the developing world, the toll there will likely be magnitudes greater. The International Crisis Group has warned of dire health and economic impacts that may de-stabilize nations, providing the opportunity for terrorist groups to flourish.
Besides its work on malaria, tuberculosis, polio, genital mutilation, etc., the WHO’s country-level teams are tasked with developing COVID‑19 Country Preparedness and Response Plans (CPRP) across the developing world. These plans identify gaps in each country’s preparedness and suggest ways to fill them. The plans – and the ability to implement them – will clearly be critical for many countries. Ironically, the Trump administration’s Pandemic Plan called for increasing funding for the WHO.
Since the outbreak began, the WHO has produced and sent millions of test kits to 126 countries – and was at one time offering them to the U.S. It has also shipped protective equipment to health workers in 133 countries. Bill Gates, who knows international organizations and global health like few others, warned:
“Halting funding for the World Health Organization during a world health crisis is as dangerous as it sounds. Their work is slowing the spread of COVID-19 and if that work is stopped no other organization can replace them. The world needs @WHO now more than ever.”
A Timeline of WHO and U.S. Events
January 9th – WHO warning that a new coronavirus had been found in China alerted health departments around the world to start tracking it.
Mid-January
- WHO’s attempt to get a team into China is rebuffed.
- The National Security Council knows the virus has probably escaped China, and warns President Trump not to trust China’s assessments. On January 24th, President Trump tweeted:
“China has been working very hard to contain the Coronavirus. The United States greatly appreciates their efforts and transparency. It will all work out well. In particular, on behalf of the American People, I want to thank President Xi!”
Jan 27th – Feb. 27 the Technical Situation Report from the WHO stated that it did not recommend travel restrictions.
January 30th – WHO calls the coronavirus a “public health emergency of international concern”, thus triggering the development of country-level plans and directives. It warns:
“The whole world needs to be on alert now. The whole world needs to take action and be ready for any cases that come from the epicenter or other epicenter that becomes established.”
February 11th – WHO Director-General Tedros Adhanom Ghebreyesus, reportedly frustrated at the paltry responses from many countries, states:
“To be honest, a virus is more powerful in creating political, economic and social upheaval than any terrorist attack. A virus can have more powerful consequences than any terrorist action, and that’s true. If the world doesn’t want to wake up and consider this enemy virus as Public Enemy Number 1, I don’t think we will learn our lessons.”
Mid-February – After reviewing the “Crimson Contagion” model in mid-February, the administration’s coronavirus task force determines that “aggressive social distancing” will be needed.
February 24th – President Trump tweets:
“When you have 15 people, and the 15 within a couple of days is going to be down to close to zero, that’s a pretty good job we’ve done.” “CDC & World Health have been working hard and very smart.”
March 13th – The WHO again states that it doesn’t believe that travel restrictions are effective stating “Countries may gain time in the short-term as they limit travel to fight the new coronavirus pandemic, but the World Health Organization thinks overall that “it doesn’t help to restrict movement”. The organization asserts that the key to stopping the spread of the virus is not stopping travel, but vigorous “testing, testing, testing” and contact tracing .”
March 16th – the Trump administration issues recommendations that Americans employ moderate social distancing measures (including not meeting in groups greater than 10 people, avoiding drinking at bars, going to restaurants). The next day, President Trump said he: “felt it was a pandemic long before it was called a pandemic.”
April 7th – President Trump stated the WHO “could have called it months earlier.” – well before before the first cases in China had been reported – and suggests “They probably did know” about the outbreak.
April 14th – President Trump suspends WHO funding as confirmed cases in the U.S. reach over 600,000.
Coronavirus Central – Resources From Health Rising
- Tracking – check out the multiplicity of ways the virus is being tracked: its spread, its infectious rate, the deaths it’s causing, efforts to model its effects.
- Advice From ME/CFS/FM Doctors and Researchers – ME/CFS/FM doctors and researchers give advice.
- Staying Safe – how to stay safe: including hand washing, nasal irrigation, disinfecting, making a mask, plus – is the virus being aerosolized? How long is the virus alive on different surfaces, and does the amount of virus present matter?
- Treatments – Check out the astonishing number of COVID-19 treatment trials underway.
- Apps – be part of the solution; use apps that help us understand the spread of the virus; plus, use apps that can warn you if you’ve been in contact with someone who is infected.
The Coronavirus Series From Health Rising
- Coronavirus #I: Dark Sun: Reflections on the Coronavirus as it Heads For Town
- Coronavirus #2: Scary Models, 8 Reasons People with ME/CFS and Fibromyalgia Should Be Careful, How to Stop an Epidemic, Why You Should Trust No One and More
- Coronavirus #3: Is the U.S. Becoming Italy? A Singapore Success Story, More Scary Models, Remdesivir to the Rescue?
- Coronavirus #4: Lipkin Gets Hit, Testing Woes, Could the Models Be Wrong, Ikea Ventilators?, and What’s Next (???)
- Coronavirus #5: Lipkin, Bateman and Klimas Talk Plus Treatment Updates
- Coronavirus #6: Will COVID-19 Leave An Explosion of ME/CFS Cases in its Wake?
- Coronavirus #7: Records Broken, An ICU Doctor Talks, The Peak is Coming, Hot Spots, Is it in the Air? Dr. Hyams on COVID-19
- Coronavirus #8: The Grand Experiment, Starting Up? Social Distancing – For 2 Years? WHO Did It?








A superb analysis! Thanks for pulling it all together so comprehensively.
I’ll second that. Thanks Cort!
The timeline…
In 2012 Texas was the first state that got surprisingly close to breaking away from the union @.gov
https://abcnews.go.com/Politics/texas-petition-secede-reaches-threshold-obama-comment/story?id=17701519
Around that same time there were other things happening that need questioned like around the same year of 2012 bitcoin would first be hitting the public after it’s anonymous founders had used it for years to cover black ops payments encrypted outside of government ledgers..
Fast forward a couple years.. pneumonia deaths begin to spike around Texas and surrounding states…
https://www.cdc.gov/nchs/pressroom/sosmap/flu_pneumonia_mortality/flu_pneumonia.htm
In 2015 them pneumonia deaths growing throughout the United States just happens to line up with 2015 jade helm states and near major international airports…
In 2015 I lived in Colorado Springs the summer i got sick and lost all motivation to even get out of bed.. this was the very summer jade helm cia experiment started as a known military operation in public environments…
My story started in 2015 however in no way am I claiming to be the first person effected…
I believe this started in Texas in 2014…
https://duckduckgo.com/?q=jade+helm+states&t=brave&iax=images&ia=images
Now before I continue with my story let’s get back to bitcoin…
https://thenextweb.com/news/satoshi-nakamoto-left-bitcoin-because-of-the-cia-theory-cryptocurrency
The founders of bitcoin have remained anonymous since 2009 and have passed ownership many times to avoid being identified…
https://slate.com/business/2019/10/andrew-yang-automation-unemployment-freedom-dividend.html
I believe there have been closed door meetings about covid spreading for years…
I believe the cia was behind the planning and or suggesting of the jade helm experiment and the cia downplayed it most as well as leadership in the cia has changed over this same timeline of events
https://archive.thinkprogress.org/russian-bots-amplified-jade-helm-conspiracies-6caa41073c08/
https://dissidentvoice.org/2020/05/the-covid-19-manhattan-project-and-its-ties-to-the-cia/
32 minutes into the way I see it it’s clearly marked that Obamas photographer was coming to work with walking pneumonia the same timeline when this started for me
https://www.peacocktv.com/watch-online/movies/documentary/the-way-i-see-it/3aa22d3e-a9a3-38e5-bfdc-6605632d365f
I’ve messaged everyone from the white house to major news to world health organization and more.. the cdc nih cnn msnbdc rueters fox spectrum and more..
It’s getting to the point where I don’t know who really will dig for the truth or try to prove my story wrong and nobody has pressed back all the way to the white house…
People around me had been getting pneumonia since as far back as before I left Colorado Springs… recently I tried to contact the first person who got pneumonia after being around me and two days ago I learned she died on June 8 2018… at my last job 2 other people died…
My fight is not really for me it’s for everyone because we all deserve the truth especially those who died before 2019 from this and their deaths are being covered up.. they and their families deserve someone to fight until the truth is told…
Compare 2015 jade helm map to 2015 cdc chart of pneumonia deaths… and think about where the major international airports are from there on how the spread began…
2016 was nearly as bad as 2019 and by then the government was desperate for someone else to blame and along comes china the country that holds most our debts…
History repeats.. this isn’t the templars who everyone owed money until they were destroyed..
This is not the Spanish flu all over again…
This isn’t weapons of mass distraction all over again…
We have the chance to stop the cycle of insanity and tell the truth for those who wrongly died..
If my country cannot tell the truth then maybe we don’t deserve this country or its governance…
The truth is all I’ll have when I die and today it matters more than ever..
Do you have the courage to find it?
One day one of your networks has to have the courage to speak the truth and of all the networks I’ve messaged it seems yours is the last one I can rely on for a somewhat non bias honest source of news.. however on this story it seems nobody has the courage to report the truth or dig for it..
They cannot hide the covid deaths pre 2019 forever and it’s going to take more than me to fight for this truth
Yes quite thorough.
But I live in British Columbia, Canada & Dr Bonnie Henry has (although slower than I’d liked) enacted protocols resulting in B.C. being perhaps the safest province in Canada. Countries rushing to ‘open their economy’ (such as Trump & others in other countries) are going to pay a huge price.
Sadly, many of those protestors ignoring ‘social distancing’ & ‘stay home’ will be among the dead….SO short sighted!!!
A further (but morbid) thought, let them protest in tight groups (as they’re doing) spreading the virus among themselves & then they’ll be in no position to protest…..
So you’re saying a significant number of protesters are elderly or have heart disease, AIDS, diabetes, lung disease, are on dialysis, or have cancer. Because these are the people that are dying.
If anyone thinks Trump could have shut down business the way the States have you need to read the Constitution. He can’t shut down the economy anymore than he can force businesses to open back up. His control was limited to Interstate business, not what goey on inside any State’s own borders. Under Article 10 public health measures, the same as with policing, are left to the States.
Also, Dr Fauci on Jan 21 said this is not a problem for the US; on Feb 29 he stated there was no need yet to change social habits. He even continued to claim the 1st week of March that, except for the elderly, especially those with pre-existing conditions, cruises were A-OK. Also had a CDC/FDA tagteam turf war against research by outside institutions.
I’m far from Trump’s biggest fan, but he was I’ll served. Y those who should have known better.
Actually only President Trump has had the idea that he can shut down and open things as he will. 🙂
Be that as it may, President Trump does have a huge bully pulpit. Republicans who step out of line have a history of being squashed like little bugs – so they all watch him very carefully. More than most Presidents he does set the tone for the party, and affect what it does.
So does he actually close businesses by order? No but does what he does impact whether business will close or how Republican governors in particular or the citizens of this country will act- of course, he does. He has a huge impact – he’s the President.. As soon as the Trump administration announced new guidelines things changed in the states.
I agree that Trump didn’t have CDC and FDA chiefs that rose to the occasion – far from it. He and the country were ill-served by them. On the other hand he is not a hapless victim. He is the Chief Executive; he is their boss.
I’m not the biggest Fauci fan but much of what he said early on was predicated by the fact that he presumed we would have ample testing to screen and catch infected people coming into the U.S. He was also not aware that asymptomatic transmission was fueling the outbreaks. In fact that is a very unusual thing to have happen.
As we learned more Fauci obviously quickly changed his tune.
You people need to stop with your propaganda against President Trump…. you’re so divisive and wrong…. I’m a Democrat’, but I’m not blind to my own party’s lies.
Stop being political and open your minds to seeing the truth!. Follow the time line. The Chinese Government hide the outbreak of the virus from the USA and the world. Trump put a travel band in place while my democrats friends were trying to impeach him and called him a racist for starting the travel band. That travel band saved many us lives. The WHO is corrupt and lied to us, they still are lying to us The us DOJ has now found proof that the virus started in a Biolab in Wuhan China.
I’ve Had ME for over10 years.
I wish you people would stop hating Trump so much that you miss an opportunity that just maybe he’d be willing to listen and help us find some solutions.!
Hi, Mary, I didn’t intend the WHO part of the blog to become a referendum on the Trump administration. There are some many ideas and conclusions running around – not all of which are based on facts – that I wanted to present a kind of fact-based timeline. If any of them are wrong or I’ve missed something – please let me know.
As to your other points – shame on any Democrats who called the Travel restrictions “racist”. That was uncalled for, petty and not helpful.
After some epidemiologists cast doubt on the effectiveness of the restrictions I was leery of them, but in retrospect I think its very clear that they must have helped and probably significantly particularly since we know that asymptomatic people are driving the spread of the virus. I don’t believe we knew that then.
As to the biolab escape idea you might want to know that Joint Chiefs Chairman Gen. Mark Milley recently stated (https://www.defenseone.com/threats/2020/04/coronavirus-escaped-chinese-bioweapon-heres-what-pentagon-says/164612/ ) that the Pentagon had taken a “hard look” at that and concluded that they didn’t know but that”the weight of evidence seems to indicate natural”.
As to the WHO lying to the U.S. my question, again, I go to the motivation of the organization. What would the WHO get out of protecting a small donor like China and then lying to a huge donor like the U.S. – particularly lying about something so deadly?
The WHO’s leader’s chief task is not to work on health. His main job is to keep the money flowing in so that the WHO can work on health. So why would he would take the risk of losing the WHO’s cash cow – and if he isn’t doing that then what other explanations are possible?
Newsflash: He’s the reason the US has the highest number of cases in the world, no one else. He’s the one — as Cort has pointed out — that repeatedly, REPEATEDLY — downplayed it.
Now of course he’s trying to blame the World Health Organization. That’s what he always does, pass the buck.
It is worth mentioning that China has developed Ethiopia as a client State and chose the head of WHO from there. It is also worth mentioning that Taiwan’s warnings to the WHO were ignored due to the absurd one China policy.
No mention of China’s global purchasing of PPE while maintaining there was no person to person transmission and of travel restrictions preventing any domestic travel from Wuhan province to other areas of China while continuing to allow folks from Wuhan to travel all over the world.
No government is particularly efficient or effective by nature, and I cannot see material differences had we a different administration. We were certainly not prepared for a pandemic, but neither was any prior administration.
The Chinese Communist Party knew they would take a further economic hit, and not wanting to fall behind the rest of the world, allowed international flights to seed the virus globally. Odd that the bat species in question is not found anywhere near Wuhan and was never sold in the market, but was in fact being studied in the lab there. Had China immediately shut down all international flights, how much of this might have been mitigated?
China will bear the biggest burden of all when all is said and done. The whole thing could have easily been stopped there.
This blog was not about China, though. It was about the current situation in the U.S.
With regard to China and the WHO,though, consider this – the US gives the WHO almost $900 million a year. China gives it about $80 million a year. Now what country would you guess the WHO is more beholden to? If you were the leader of that organization who would you be more worried about offending? The country that gives you a third of your funding or the country that gives you 3% of your funding?
The idea that the WHO is somehow in lockstep with China to go after the US and that the WHO KNEW about the virus and refused to tell the world about is just doesn’t make sense to me. I can’t see how it does the WHO any good to whack the economy of their biggest donor.
A far simpler explanation for the WHO’s actions is that this is just how they operates: they are in countries at the behest of the country, they do everything they can not to offend them, and that leaves them behind the ball at times. (This time they were about a week behind.) That makes more sense to me at least than some grand China/WHO conspiracy.
Blame is different from seeking accountability…we are holding them accountable for their actions as we should accept and learn from our shortcomings. Assuming that different leadership here would have made a tangible difference is a bit naive in my opinion.
I’m just saying this blog was not about China. If it was it would have been really ugly (lol). China kept the wet markets open after SARS, China refused both the WHO and CDC teams entry into the country to get samples of the virus, the Chinese authoritarian system stymies reporting of bad news from the local level, encourages lying and incompetence. You’ve pointed out more things.
I’m not saying that the Trump administration is good or bad but I do assert that leaders and their teams – even in this situation would make a big difference. Take the approach between Herbert Hoover and Franklin Roosevelt in the great Depression They both had similar situations and similar limitations yet one prevailed and one did not.
Here’s an interesting question. If the U.S. is going to need to do millions of tests a day how in the world are we going to get that done? It doesn’t appear we can rely on the states or private industry to do it. And how about contact tracing? One estimate suggests 300,000 people are needed. How are we going to ramp up to do that? There are big challenges ahead. I sincerely hope we can rise to them.
“The Chinese Communist Party knew they would take a further economic hit, and not wanting to fall behind the rest of the world, allowed international flights to seed the virus globally.” If either this is true, or if the virus was released as a bio weapon with the Chinese willing to write off many of their citizens (they have a lot to waste) to economically cripple the U.S., one could regard that as an act of war. My guess is that we may never know if either is true because the implications are too dire in terms of decision-making.
To bring the discussion closer to home, IMO this puts the final nail into any of us Boomers, already prime meat for Covid-19 LOL, getting any relief from fibromyalgia and probably a lot of other diseases. We are entering a recession, maybe even the Greatest Depression, and medical research funding for many things is not going to be at the top of any playbook of those in power. Trying to keep the country from sinking into various forms of depression, hyperinflation, etc., will be Job 1 for them as well as massive funding for our War Machine, the Pentagon. I always somehow hoped that some small improvement for my pain would be found but the virus is going to be game changer.
But look at where China is now, Steve. They’re by far the most indebted country in the world and have taken a tremendous economic hit – and who do they depend on to drive their economy? American, European, Australian, etc. consumers. And what has happened to them now that everyone;s economy is shut down? No consuming…..
China can’t even open its economy until America opens theirs. I wouldn’t be surprised if the Chinese economy goes into a freefall because of this. It was too fragile an economy to begin with – way too far in debt, far more convoluted, far more pieced together with sticks and strings than the U.S.’s is.
New York has already said they will be cutting $2 billion in public services – that’s New York City – not New York state. The economic costs of this virus and the debt we’re incurring will likely take decades to pay off. It’s a harsh lesson indeed.
My hope is that more study into viruses, neuroninflammation and post-infective illness will pay off for both ME/CFS and FM.
Hi Cort,
I dont know where you got your facts about Sweden? The fact is that we are implementing social distansing on a volontary basis, which works quite well! Our goverment has strongly recomended us, to stay at home! Work from home, all those who can. And people do! Our universities and high schools are closed and have home studies. All people who find them selfs having the slightest cold are told to stay at home until well +2days. The state pays for your sickleave. Its prohibited to visit home for elderly. Sadly staff has probably in some cases brought covid 19 into these homes, so quite a few old people have died. Not all other countries count these deaths as covid 19. All holiday travels within the country are banned, for easter for exemple, if not nessesary! All ski resorts closed down before easter to stop the spread. All domestic flights are basically down exept for absolute necessary transports. The borders are basically closed! Don’t think we are doing things so much different from other countries, just more of own responsibility. We do not live crowded here except for the big cities like Stockholm, Malmö and Gothenburg, so keeping distance is not a big problem…. Hope you all keep well all over the world!
Thanks for providing a fuller picture Mary! All I had to go on was the IHME report which you can find here – https://covid19.healthdata.org/sweden – which just lists whether or not a country or state has applied 4 major social distancing measures. Glad to hear Sweden is taking so many other measures. Good luck to Sweden – and to all of us.
Institute for Health Metrics and Evaluation, that is what IHME stands for. I guess I am not keeping up, not to know that. The Institute is at the University of Washington (state), which is how I recollect news folks naming this source.
That is a good set of comparisons and it is good to read that California is expected to hit its peak so soon. Per the New York Times tally, California has lost 971 people, or 2 per 100,000 population, to covid-19. With such a large population, it might have been worse. In my own field of transportation planning (well, when I was able to work), New York metro area has been hit so hard because of its urban density, jobs per acre, people per acre, and thus more close contact in elevators up to jobs and so on. Average state population density does not matter for spread of the virus. In urban planning, New York City and its metro area are in a class alone, no other place in the US is like it. Thanks for your good work.
As to our president and WHO, Gordon Brown of the UK says other world leaders must persuade him to change his mind. Interview I heard this morning on BBC world news.
https://www.bbc.com/news/av/world-52308372/brown-halting-who-funding-is-act-of-self-harm-by-us
Yes, indeed. The Big Apple far outstrips San Francisco in population density when compared to the cities themselves (28,000/sq mile vs 18,000 per sq. mile) as does the New York Metropolitan area (5500/sq mile vs 1100 sz. mile). Plus the New York Metropolitan area is so large – 20 million people (vs 7.7 million SF Bay area) Contagious viruses, of course, love congested areas. New York City will always be at the greatest risk when something like this happens.
By the way, you might want to check out the IHME came about – it’s a fascinating story of one man’s attempt to accurately assess the world’s health needs – https://www.healthrising.org/blog/2017/01/11/epic-measures-chronic-fatigue-fibromyalgia/. He actually bumped up hard against the bureauracy of the WHO and then convinced Bill Gates to write a very, very large check.
I agree with Mary above. Sweden has done more than you write Cort. I agree that it is not a total lockdown here, but many are deeply affected by our restriction and our social distancing. Though some people foes not follow restrictions, many, many do.
As proof you only have to check how many that has lost their jobs, how many jobs that actually gets economic support etcetera.
As I can see your graphs are from models? Some news from Sweden fresh from today tells us that we still have unused capacity for intensive care, about 20% more “beds” than are already used. Which is hopeful. Even better, “the curve” is now thought to go down/stabilize. And that is from fact checked sources.
Why do I react so fiercly? Well, I’m a health care worked even if I’m not working now. So I can validate the data we get, because I know how their are produced. And I’m very upset by all misinformation that are spread on this subject.
True. Haven’t read your entire post, so maybe I rant for nothing. But I know how this virus is spread, and the most effective way to combat it is by washing your hands with soap (destroys the virus) an water – often. Stay at home if you are sick (whether you trransmit while not having symtoms. Yes maybe, but even more when you have symtoms). And most transmitting occurs in close relationships, by family or friends/collegues so keep distance! Meet outside, at a broomsticks length. So that iswhat we do here in Sweden really!
Fact check on https://www.folkhalsomyndigheten.se/the-public-health-agency-of-sweden/communicable-disease-control/covid-19/
Thanks Kajsa – I can well understand your upset – and thanks for clarifying what is going on in Sweden. One of the important outcomes of all of this will be understanding which models are accurate or not. It’s clear they are varying dramatically. Let’s hope Sweden’s is the correct one.
I do think that there will be alot of evaluation from many different sources(?) afterwards on what was right … 😉
I also think that there is no RIGHT WAY, that is every society have to take different measures. Say to tell someone who lives alone, and with a distance of several miles to their closest neighbour it is quite ridicolous to ask them to stay indoors … Or if you live in Calcutta how do you really keep distance. If you are short of water should you use the little you have to wash your hands or to food?
In most areas here it is very accomplishable(?) to keep a distance to other people on the street as long as you are not in the subway, on the bus or in shops at rush hour. Though there is no rush now … and both restaurant owners and shops are told to minimize customers so that proper distance can be held. Of course not everyone follow these rules, or as called in official language – advise (that is almost a law in Sweden), but alot of people do.
As for travelling, during easter travelling from Stockholm went down with 96% or there about compared with last year. People are recommended to NOT take commuter trains, subways nor busses. There is ONE aircraft supporting our whole country! All other flights are grounded, domestic ones.
Yes we go to our work if we cannot work from home, keeping society running – haltingly. You are supposed to stay home if sick, and get financial support to do that! School are closed, but not for the younger ones, because we cannot close tgat down, then we would not have anyone that could do those things that still have to get done. Studies have also shown that that is not what is driving the spreading. But our officials will, if nessesary close them too. But at the moment that would do more harm.
On the surface, yes it might seem that we don’t do much. But we do, really.
And also again, it is so important what is done where, and also when and how. I think. Well we do not know yet, maybe we wont ever even, and there is probably no single truth.
It is an interesting time to live in indeed, even if I very much had appriciated if this hadn’t happened. With all data collected, with todays analytic force and possibilities to communicate and everything there will be so much to research on. We will learn heaps!
Sorry again!
Thank you Cort, for this other comprehensive and well documented article.
I’m not an American, but I did not read any political attack in your chronological report of U.S.A. leader’s shifts of position towards COVID-19. One can approve or disapprove of the President’s comments and attitudes, but one HAS to know what was and is being said and decided. It’s not a matter or hatred, it’s a matter of practicality. If citing a politician is a twarted political manoeuvre, on what else are citizens going to evaluate their choice when the time comes to vote? Looks?
Why should a citizen have to choose to BE Democrat or Republican? The people we elect to represent us are so much more than their party. Forget the colour and take a long, lucid look at how each of the person(s) you want to put or maintain in office actually contributes to their communities, the large and the small, in a period of crisis.
I would also like to thank Mary for her comment on Sweden; I’ve heard pretty much the same from different Swedish sources. In Quebec, where I live, when our political and health officials explained the measures we were going to take in order the “flatten” the curve, a few journalists asked why we wouldn’t follow the Swedish model. Sweden is so very often cited as having the best models to imitate, whether it’s education, health, social benefits, etc. It can be unnerving for leaders of other countries who do not have to deal with the same realities : larger population, bigger cities, different cultures, etc.
I think that what is important, is that measures adopted to counter this pandemic are coherent within a given country. It’s the only way we are able to get realistic and meaningful numbers, to adjust ourselves accordingly and avoid a second wave.
I understand that it is close to impossible to apply sea to sea prevention strategies in the United States, but each state who has reached a good balance between the number of cases and the pressure felt by it’s health care system will not want to jeopardize their hard earned gains on the virus by opening itself to the rest of the country for “national” economy purposes.
Be safe.
Amen! Well put!
It’s all a grand experiment isn’t it? It’s actually good that countries and states are taking different approaches as they will allow us to assess which works the best in which situations. Epidemiologists will be teasing out which factors which best in which places for years.
@Cort, The list of facts at the end making Trump appear to make poor decisions and making WHO look like they were making good decisions is quite shocking. I saw WHO’s reaction when Trump implemented the China travel ban on Jan. 31 and they were absolutely not in support of it. I just think the way the facts are listed as such are if not inaccurate give an inaccurate narrative by what is left in and what is left out.
I was looking at my notes from the WHO website which makes their documents public. I wrote some notes about two weeks ago.
I wrote down that on Feb. 27 the Technical Situation Report stated that there were no travel restrictions. NONE. It looked something like this: “WHO does not recommend any specific health measures for travellers. It is generally considered that entry screening offers little benefit, while requiring considerable resources. In case of symptoms suggestive to respiratory illness before, during or after travel, the travellers are encouraged to seek medical attention and share travel history with their health care provider. WHO advises against the application of any travel or trade restrictions on China based on the information currently available on this event.”
Today that report is simply gone. It says it has been superseded by the one the 29th I think…. I wrote down Jan.23, 24, 31 Feb. 1, 2, 3 and did not note stronger travel advice until Feb. 28. Today many of these reports look different to include stuff about Taiwan which most definitely was not in there before.
I just want to say to everyone use some common sense. I get it you hate and distrust Trump but please don’t mistake that for believing what the WHO and China are shoveling. There is a lot of rot at the WHO and it is quite scary how history is being rewritten in real time.
Here is a link to an article on Feb. 3 from Reuters in which they quote WHO Chief talking about Trump’s China travel ban that was announced on Jan. 31. WHO was not happy about. https://www.reuters.com/article/us-china-health-who-idUSKBN1ZX1H3
Well Tina, those were all facts and you can interpret them as you will. Yes the WHO disagreed with the travel restrictions at the time. I have noted that and I will add that fact to the list, and I just added a March statement from the WHO which disagrees with travel restrictions. The fact is that the WHO does not believe travel restrictions – whether from China, Europe, Mexico or wherever -really helps. That’s their opinion. It doesn’t mean they’re in bed with China. Instead the WHO has been pushing countries to focus on testing and contact tracing.
I would be wary of being fixated on any one event when assessing how well a country or institution is doing. Common sense would dictate, I think, that we assess the events and actions that occurred over time – particularly in a novel situation like this.
I think the facts indicate that while the WHO disagreed about travel bans they consistently attempted to warn the world that the virus was coming.
The travel “ban” – we shouldn’t call it a ban since it did allow many people travelling from China into the US over the next months – so the “travel restriction” probably did buy us some time. Note, though, that epicenter of the epidemic in the U.S. – New York City – got walloped by infections coming from Europe which got there well before the European travel ban.
All any travel restrictions were going to do was buy us some time. Whether the virus came from China or Europe or Japan or Australia this virus was coming.
Given that the next question that might be asked is how well did we use that time to prepare? With the U.S. having more than double the number of confirmed infections and more deaths than any other country, my guess is the answer is not a good one.
That has nothing to do with whether I like or don’t like Donald Trump. The facts indicate that as a country we obviously haven’t done very well.
I would also be wary of trying to put the responsibility for that on others. Once the virus reached our shores, neither the WHO or China nor the UK nor Germany or whoever had anything to do with how we responded.
The fact that the WHO’s dissension regarding travel restrictions was NOT listened to by the U.S. (and dozens of other countries before us) – means it’s disagreement regarding travel had no effect at all on what has happened in the U.S. Yet here we are, essentially crippling the funding of the only world-wide health organization dealing with the coronavirus. It’s the poor people in the developing world – people who have nothing to do with this controversy – that will pay the price of that. That’s my main concern.
I can’t comprehend the logistics of testing. Someone could be cleared one day and become infected the next, unless the cleared ones are isolated. With millions of people? OK all of you over hear. How about a button that lights up when one become infected? The whole thing is just a knight mare.
The experts say this is just a warning.
“True wisdom comes to each of us when we realize how little we understand about life, ourselves, and the world around us.” – Socrates
Great question Ron – the answer from what I’ve read is repeated testing – testing again and again and again. For first line workers – a test with rapid results – every day. They are isolated for the time it takes to recover from the virus – and we move on. Nobody to my knowledge has done that but if anyone can and should do that – we would. It would be the quickest way out.
The funny thing is is that if I understood Ron Davis’s purposed test right – the test would light – and the test result would be delivered within something like 20 minutes. He proposed that 15 years ago.
It would surely be the quickest way to limit the economic damage and the fewest people would get sick over time.
With the administration leaving testing to the states, though, it’s probably not going to happen.
Cort there is a test out there now how accurate..I dont know..within that time frame but the problem is the duration on the recovery as well as re infection exposure..not known as each person system is different in the healing mode as well as their health histories and physical/mental-stress level state..very univerisal (a perfect storm senario Situation) MPO..(my personal observations..
I do agree with you on/about this Virus happening that this will help all believe and know that FMS/ME/CFS is real and it will help us all in the generations to come in the science/medical fields.
I have Faith, Hope and Believe..? this
Stay well and Strong All!
Just out:
https://www.washingtonpost.com/opinions/2020/04/17/trump-tells-damnable-murderous-lie/
My husband’s cardiologist told us 10 days ago that we should plan to “enjoy the summer in our own back yard with all of our current safeguards still in place. No visitors, no going out, no social contact.” At that point he’ll let us know what to do for the fall and the winter.