

Still at the Beginning?
A recent review “Current and Emerging Pharmacotherapy for Fibromyalgia” examined the state of drug therapy for FM. It was a bluntly honest review. The news on the drug side has not been, after all, all that good in FM. A large study found that only a minority of people with FM continue taking the three FDA-approved drugs for the condition (pregabalin, duloxetine, and milnacipran) or other drugs for more than a short period of time. The language they used – “rather modest rates of success” and “strikingly modest progress” – stood out in a scientific literature which, if anything, tends to overstate gains.
Why has FM been such a tough customer? The authors of the current review believes it’s not just FM – the “great complexity” of the central nervous system mechanisms that cause chronic pain make it, to put it bluntly, a bitch to treat. Add in the special extras that FM brings – the fatigue, sleep, cognitive and stimuli problems – and you’ve got a real challenge. The recent findings indicating the neuroinflammation in FM is far more widespread than in your garden variety chronic pain suggest FM is going to be harder to get at.
The authors really lay it on when they state that despite all the progress made in understanding the neuroscience of pain, “we are yet at the beginning” with FM. “Much greater insights will be necessary before a truly rational and effective pharmacological solution for fibromyalgia (and similar conditions) will be at hand.”
That wasn’t easy to hear, but progress always starts with speaking the truth. It’s not that some progress hasn’t been made. All the 14 drugs the authors listed are effective for some people. They’re not as effective and not effective in as many people as we would want, though.
| Amitriptyline | Tricyclic antidepressant | Improvement in pain, fatigue, and sleep abnormalities. | Several randomized controlled trials, guideline recommended [8–10] |
| Duloxetine | Serotonin-noradrenaline reuptake inhibitor | Improvement in pain and depression. | Several randomized controlled trials, meta-analysis [11, 12] |
| Milnacipran | Serotonin-noradrenaline reuptake inhibitor | Improvement in pain and fatigue. | Several randomized controlled trials, meta-analysis [11, 12] |
| Reboxetine | Selective noradrenaline reuptake inhibitor | Improvement in pain. | Mostly case reports [13] |
| Esreboxetine | Selective noradrenaline reuptake inhibitor | Improvement in pain and fatigue. | Randomized controlled trial [14] |
| Citalopram, escitalopram, fluoxetine, paroxetine | Selective serotonin reuptake inhibitors | Improvement in pain and depression. | Randomized controlled trials, meta-analysis, guideline recommended [8–10, 12, 15, 16] |
| Cyclobenzaprine | 5-HT2 receptor blocker | Moderately improves sleep, mild improvement in pain. Development stopped due to low efficacy. | Randomized controlled trial [17–19] |
| Pregabalin, gabapentin | Gabapentinoid | Improvement in pain, fatigue, and sleep abnormalities. | Randomized controlled trials, guideline recommended [8–10, 15, 20–22] |
| Lacosamide | Gabapentinoid | Effective in animal models. No clear evidence in FMS. | Randomized controlled trial [23] |
| Naltrexone | Opioid receptor antagonist, TLR-4 antagonist | Improvement in pain in depression. | Randomized controlled trial [24, 25] |
| Tramadol | Opioid with SNRI activity | Improvement in pain. Mostly for severe symptoms and short duration, see text. | Guideline recommended [6] |
| Nabilone | Cannabinoid | Improvement in pain and anxiety. Conflicting results, see text. | Randomized controlled trials, meta-analysis [26–28] |
| Dronabinol | Cannabinoid | Improvement in pain and depression. Conflicting results, see text. | Randomized controlled trials, meta-analysis [29] |
| Ketamine | NMDA antagonist | Improvement in referred pain. | Clinical trial, animal models [30] |
| Memantine | NMDA antagonist |
The general paradigm regarding FM is that nervous system hypersensitivity or “central sensitization” causes the nervous systems of people with FM to interpret benign stimuli as painful. One’s body hurts despite the fact that there’s nothing physically wrong with one’s body. In the central sensitization paradigm, increased levels of neurotransmitters such as serotonin and noradrenaline tweak the nerves causing them to become twitchy and respond to all sorts of stimuli.
Hence the serotonin reuptake inhibitors (SRI’s – citalopram, duloxetine) and serotonin and noradrenaline reuptake inhibitors (SNRI’s – duloxetine, milnacipran) that litter the list of FM drugs.
Because other neurotransmitters (GABA – Lyrica, gabapentin; cannabinoid receptors – Nabilone, substance P, NGF, and opioid receptors – tramadol, naltrexone) may also contribute to central sensitization, drugs affecting them are used as well.
New Approach Needed
“Thus, future breakthrough in the field of FMS will clearly necessitate a truly eclectic and multidisciplinary approach.” The authors
The authors believe, though, that new approaches are needed. The major pathways drug manufacturers have concentrated on thus far- serotonin, noradrenaline and the anticonvulsants (gabapenten, Lyrica) – have been mostly tapped out and will likely produce only “incremental progress” in the future.
So where are the breakthroughs likely to come from? The nature of a real breakthrough, of course, is that it often comes from an unexpected place, but the authors had some ideas.
Cannabinoid Drugs
The first drug arena the authors pointed to was the cannabinoids. Cannabinoids are a fascinating possibility given the abundance of cannabinoid receptors in sensory pathways of the central nervous system, and the ability of THC, in particular, to reduce pain and inflammation. One study suggested that FM is a disease of reduced endocannabinoid (the cannabinoids produced by the body) activity. One proponent of the endocannabinoid deficiency hypothesis believes that it also applies to migraine, irritable bowel syndrome, and other treatment resistant syndromes. Another suggested something whacky was going on with the endocannabinoids in FM.
Numerous reviews have suggested that cannabinoids may be helpful in inflammatory and neuropathic pain, but all descry the limited research and clinical data available.
The drugs that have been tested thus far unfortunately can’t tell us much about the promise the cannabinoids present. The cannabinoids work best in conjunction with each other, and with the terpenes and other chemicals found in other parts of the Cannabis plant. The current man-made Cannabis drugs such as nabilone and dronabinal can’t match the therapeutic richness of Cannabis plants or tinctures. These drugs have produced just moderate results in FM studies.
A large prospective study, on the other hand, emanating from a specialized medical Cannabis clinic, showed a strong drop in pain intensity scales from an almost intolerable 9.0 (out of ten) to 5.0 and adherence rates (71% after six months) that blew the FDA-approved drugs out of the water. The study also indicated that sleep disturbances and mood were also improved.
Given the vast reach of the endocannabinoid system in the central nervous system, it’s not surprising to find that efforts are underway to attempt to tweak it, not by ingesting Cannabis, but by altering the enzymes that metabolize endocannabinoids. If fibromyalgia truly is a disease of reduced endocannabinoids, this approach could reap dividends.
The authors called the endocannabinoid system “a vastly understudied area, which would appear to hold great promise regarding the treatment of FMS”. The authors looked forward to the “development of high-quality medications”. That, of course, will take much more research – and the U.S. government fully removing its decades long restrictions on Cannabis research.
Turning Down the Fire – the Glutamate Inhibitors
Glutamate is the most abundant excitatory neurotransmitter in the central nervous system. Increased glutamate levels have been found in the insula – a major pain-regulating area of the brain – and other areas of FM brains. Given the hyperexcitable pain transmission pathways in FM, inhibiting the main excitatory neurotransmitter in the brain surely makes sense.
Plus, the N-methyl-D-aspartate (NMDA) receptors in the glutamatergic system are activated by substance P – a pain producing neuropeptide shown to be increased in FM. One of the earliest responders to stressful situations, Substance P, is also, interestingly enough, given the recent vasodilation hypothesis by Wirth and Scheibenbogen for chronic fatigue syndrome (ME/CFS), a potent vasodilator and a potent pain producer. Theoharides has also speculated that mast cells may be increasing substance P levels in FM.
NMDA antagonists which reduced substance P and glutamate might have a good shot, therefore, at taking FM patient’s pain response systems off the knife’s edge they’re on.
Ketamine
Ketamine, is an NMDA antagonist which has been shown to reduce pain and depression, and a ketamine nasal spray has been FDA approved for treatment resistant depression. Memantine is another NMDA receptor antagonist that’s shown promise in two FM studies, including a 2019 one which tracked brain metabolites.
Whether Ketamine is ever going to go mainstream is a good question but a 70-person “Ambulatory Infusions of Lidocaine and Ketamine for Management of Chronic Pain” trial is starting at the end of this year and ending at the end of next year.
Check out more on ketamine in fibromyalgia below.
Emerging Possibilities
Neuroplasticity Enabler? NYX-2925
There’s a new NMDA receptor modulator in town, though. Called NYX-2925 ((2S,3R)-3-hydroxy-2-((R)-5-isobutyryl-1-oxo-2,5-diazaspiro[3,4]octan-2-yl)butanamide), it’s been effective in rat models of neuropathic pain and may, in contrast to ketamine, which appears to whack sleep, to be able to improve sleep.
The drug has come quite a ways. Using brain imaging, Aptinyx, the drug manufacturer, found that symptom improvements were correlated with reductions in glutamate levels (glutamate/glutamine (Glx)) in two key pain processing areas in the brain (insula, anterior cingulate). (People with ME/CFS should note that studies have highlighted those brain areas in ME/CFS as well.) NYX-2925 is also intriguing in that it apparently provides a kind of neuroplastic boost by enhancing synaptic plasticity. (Might it enable the neuroplastic approaches to pain relief found in the DNRS, Gupta’s Amygdala Retraining Syndrome, Moskowitz’s imaging protocols.)
NYX-2925 passed its phase II clinical trial test of safety and efficacy for FM last year, and a phase III trial was set to go in the fall of last year.
Aptinyx appears to be quite high on the drug and expects it to be helpful in other chronic pain conditions characterized by central sensitization. (That would, of course, include ME/CFS).
“We believe the therapeutic profile of NYX-2925 will allow us to expand the development of this molecule into multiple other chronic pain conditions.” Aptinyx
Neuroinflammation Reducers
Neuroinflammation reducing drugs were only mentioned in passing in the review, but they provide possibly the most creative new way to treat FM and ME/CFS and other central nervous system diseases. New, and hopefully more effective, kinds of antioxidants are being developed and used to cool the fires in our brains.
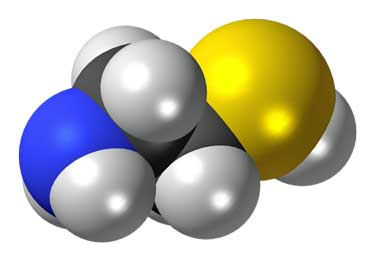
Cysteamine, a derivative of the amino acid cysteine, and cystamine, an oxidized derivative of cysteamine are two of them. Cysteamine (Cystagon) is FDA approved to treat cystinosis. Cysteine is a major component of the master antioxidant in the body – glutathione.
In a review paper, “Therapeutic Applications of Cysteamine and Cystamine in Neurodegenerative and Neuropsychiatric Disease“, Bindu Paul and Solomon Snyder of Johns Hopkins proposed using cysteamine and cystamineto to treat not fibromyalgia or ME/CFS but neurodegenerative diseases such as Alzheimer’s, Parkinson’s and Huntington’s Diseases as well as autism.
The general goals behind such treatment approaches, though – reduced oxidative stress, increased mitochondrial functioning, reduced microglial activation, neuroprotection and immunomodulation – appear to make sense for FM and/or ME/CFS.
(People with high cortisol levels might want to note that cysteamine was also able to reduce anxiety, and depression-like behaviors in a mouse model of anxiety/depression induced by chronic glucocorticoid exposure.)
Cysteamine and cystamine function as antioxidants and are very potent antioxidant boosters. Cysteamine, In fact, is three times more powerful a cysteine booster than N-acetylcysteine (NAC) – the supplement which Shungu proposed to treat the glutathione deficiencies he found in the brains of people with ME/CFS. Cysteamine’s ability to cross the blood-brain barrier means it could potentially get at the neuroinflammation in the brain.
The authors propose that cysteamine/cystamine be added to the mix of drugs used to treat central nervous system diseases. Clinical trials will likely begin in one or other of the neurodegenerative diseases. If they’re successful, a new way of tamping down the oxidative stress and neuroinflammation in the brain may have been found – one that could apply to FM and ME/CFS.
In a serendipitous note, one of the two authors, Bindu Paul, has a Solve ME/CFS Initiative grant to study ME/CFS.
A Multiple Sclerosis Drug To the Fore?
The authors missed this drug as well. One nice thing about dimethyl fumarate, though, is that it, like cysteamine, is already FDA approved to treat a disease (multiple sclerosis). Dimethyl fumarate, like cysteamine, is a powerful antioxidant.
The Pain Research Forum reported that researchers at the University of Texas attempted to use dimethyl fumarate’s antioxidant capabilities to clean out the free radicals and restore the oxidative balance in lab animals with neuropathic pain.
It worked – not only were the animal’s pain behaviors (including allodynia) decreased, but the drug increased levels of the master antioxidant in the body (glutathione), reversed the damage caused by the oxidative stress, and increased oxygen consumption (i.e. mitochondrial functioning.) In one fell swoop, dimethyl fumarate hit something of a trifecta.
It did this by activating a core transcription factor called NFE2L2 which is responsible for turning on over 200 antioxidant-related genes. Interestingly, the DRG neurons examined in the study have been proposed to play a role in both fibromyalgia and chronic fatigue syndrome (ME/CFS).
The authors hoped to start clinical trials in humans soon. While the study focused on neuropathic pain, the authors also believe that dimethyl fumarate could work in other pain types.
“We also want to investigate whether dimethyl fumarate can be used to treat oxidative stress in other chronic pain models.” Grace
Fracktaline Inhibiting Drugs
Fracktalkine inhibiting drugs were not mentioned either, but fractalkine (CX3CL1) – an immune factor found elevated in FM – may be a key player in the production of chronic pain. One review suggested it might even be the central nerve factor that turns on the microglia – the key player in neuroinflammation. If that’s true, it’s a biggie.
If fractalkine turns out to be a big deal in FM, the potential good news for FM patients is that several fractalkine inhibiting drugs are being assessed in various diseases.
Others
More drug possibilities not reviewed by the authors exist. The big Phase III clinical trial for TNX-102, Tonix’s drug began in November 2019; it’s not clear, however, how it’s been affected by COVID-19. If it’s successful, though, it could help with both sleep and pain in FM.
Dr. Pridgen, the creator of an antiviral approach to FM, and Innovative Med Concepts, his startup, reported that he’s recruited a new, experienced Executive team (CEO, CFO, and COO) in preparation for going public. They are likely moving forward with an IPO near the end of the year with a large trial soon to follow.
Jarred Younger tried, without success, to get NIH funding to assess a possibly more powerful form of dextro-naltrexone. Younger is also assessing the effect of dextromethorphan, a microglial inhibitor for FM.
The new class of migraine drugs could help with FM as well and a trial is underway, “Anti-CGRP for Inflammation and Pain Modulation in Small Fiber Neuropathy/Fibromyalgia”,featuring Galcanezumab.
Check out more FM trials that were or are slated to be underway in the blog below.
Unforeseen Possibilities
The truth is we don’t know what will pop up and one reason for that is the NIH’s Heal Initiative. The opioid epidemic demonstrates what a dead end we’re at with regard to treating pain. Opioids certainly have their place but the fact that they still occupy such a dominant place in pain treatments indicates how stagnant the field has become.
To that end, the NIH’s Heal Initiative is pouring money into pain research and development with the hopes of triggering the development of no less than 15 new pain drugs over the next couple of years.
Check out some treatment options your doctor may not know about:








Thanks, Cort, great review, and finally something on FM (thoughI know you look for them, they just aren’t there). I thought I knew about and had tried just about everything but you had some new ones to me there. The lack of research and plethora of retooled meds is depressing, though, and with America beyond broke and now Covid, I look forward to more years of suffering no doubt due to lack of interest/funding in FM. I found this amusing:
Tramadol Opioid with SNRI activity Improvement in pain. Mostly for severe symptoms and short duration, see text.
Short duration…I’ve been on this crap for five years at the maximum dose, with several profound side effects. It helps only 10% but if your pain is at 7 or 8, you grab 10%. I wonder how many of the meds they’re looking at also have such significant side effects coupled with marginal response such that only the desperate like me will use them. I have been experimenting with ULDN, benign at least, for eight months with no effect. Keep up the good work, wear a mask, carry a hydrogen peroxide sprayer everywhere like I do.
Thanks Steve,
Have you tried any cannabis products? When I use one for sleep the first thing I notice is the pain just disappearing.
https://www.healthrising.org/treating-chronic-fatigue-syndrome/drugs/cannabis-fibromyalgia/cannabis-fibromyalgia-chronic-fatigue-reviews/
Hey Cort,
I didn’t see any mention of PALMITOYLETHANOLAMIDE (PEA) in the article linked and it is something that my pain specialist went from telling me not to bother with 2 years ago to trying to push this year. Have you heard much about it and it’s use as a treatment for FM? I’ve gone through all of the medications listed with no affect except opiods, which they obviously don’t want to use, and during ketamine infusions there was 1 hour my pain went down to a 2 out of 10 but that was at the maximum dose and they said they couldn’t go any higher and an hour wasn’t good enough to try investigating it further.
hi steve. i’ve had FM for over 20 years. sounds like we have both been cycled through the same list of ineffective drugs – none of which worked for me. i started taking LDN about 4 years ago. it’s the cornerstone of my medication -it really helps me reduce pain and improve sleep. i’d say it’s a 30-50 per cent reduction. it also has the advantage of being cheap and having relatively benign side affects. with LDN it’s important that you start low and build up slowly and fine the right dose. i’d be very happy to pick this conversation up directly if Cort wants to pass you my contact email.
best
peter
Opiodes work, with long term issues. Many years ago I tried Tramadol, and others with little effect. Low dose Naltrexone did not seem to do much after about six months (although now I see that results may not show for at least this time – so, maybe I didn’t try long enoug).
Duloxetine and gabapentin worked for FM and pain from neuropathy, etc but only with side effects which caused me to discontinue them, twice! Starting is easy but stopping requires so much time to titrate doses.
At least physicians are more responsive and receptive today to even acknowledge this is real. Thanks for your continued assistance and promotion of the issues.
I have suffered from fibromyalgia since my 30s. I am now 72. I also have lichen sclerosis on my scalp and lichen planus in my mouth. A hospital dentist prescribed BETATHASONE to alleviate the soreness. I was to use this as a mouthwash 4 times a day, but not swallow it. Because of covoid19 I couldn’t return to the hospital and phoned my GP the get a further supply of this drug. It is a corterosteroid. She had never heard of it and was unwilling to put it on a repeat prescription. However when I got the box she DID prescribe it said the tiny pills should be dissolved in plenty of water and swallowed!
I have been experimenting. I now use the mouthwash and then swallow it once a day.
I do feel the anti-inflammatory effects are helping my general pain levels. However I have also managed to lose 2 stone and to walk about 10000 steps a day. That might have something to do with it
I should be most interested if research could be done in this drug for fun to sufferers
Fm for 15yrs tried lots some drugs everything holistic .just come across the low oxygen saturation link due to buting a oxyimeter in case got covid .i have low oxygen and never knew .looked up and there is a link with fm .i never knew .
How about that. There is a hyperbaric oxygen study going on or about to go on in Isreal. The last one was successful.
Just saw this today on the Pain News Network site about a peptide which is showing great promise in pain control–in rats. Researchers think that it will work in homo sapiens too and clinical trials are in the works;
https://www.painnewsnetwork.org/stories/category/Pain+Research
Regarding various gases, I also read that nitrous oxide seems to be lethal to the Covid virus. Imagine that! Getting high to eradicate it in one’s lungs. Much better than bleach I think!
Oops! It’s nitric oxide, not nitrous oxide! Sorry. Here’s the link; https://gizmodo.com/scientists-are-testing-nitric-oxide-to-treat-coronaviru-1842642935
Still better than bleach!
A better pain killer without the side effects would be a help. However more analgesics, fancy analgesics are not going to fix the problem. Pain is so idiosyncratic (idiopathic), it is also a function of many other pathologies. I do not believe the hypothesis of central sensitization. There is clearly a sensitization or a lower threshold for pain but the hypothesis that it is purely central is not strong. More research is needed to identify the source of the pathology, such as at the nociceptors, the role of the immune system, such as the role of the IGg auto-antibodies. FM has all the hallmarks of an auto-immune disease. The gut disturbances, the balance and gait problems, the weakness, the fatigue and the great variation in pain – are not “central” sensitization.
The Norwegians are reporting promising Phase II trial results with cyclophosphamide.
Note, however, there was no placebo control. interestingly, positive outcomes were double the frequency in patients with specific Human Leukocyte Antigen (HLA) alleles.
Again, this is suggestive of an autoimmune subgroup infectious onset?), who may be major beneficiaries from this type of treatment.
Wow! Are they? I know they are investigating cyclophosphamide for ME/CFS along with work done by James Baraniuk. I cannot see why they would be doing this for FM though. FM has a different autoimmune profile.
Sorry, my comment was in reference to ME/CFS, I should have made that clear.
I just wanted to get it out in this forum, and bring it to Cort’s attention 🙂
Eww… Interesting – thanks for pointing that out. I didn’t know that connection was being made.
I’m hoping for others’ sake we move away from SNRIs as a ‘treatment’. My fibromylagia onset was 12 months into venlafaxine use and, this is anecdotal of course, I hear a lot about widespread body pain and cognitive ‘fog’ issues in other SNRI users which, encouragingly, reduces as dose is lowered (and the sometimes debilitating withdrawal symptoms eventually subside). ‘
I think the research world, at least, recognizes that we’ve gone about as far as we can go with these kinds of drugs.
How do I put my name forward for a trial?
I am new to fibromyalgia I got diagnosed last year in November however it’s taken about 3 years to diagnose me, I also suffer cluster headaches which I have oxygen at home which does help abit, I also suffer IBS, Fatigue, Brain Fog along with Slurred Speach, TMJ, Tinnitus, Sciatica and so on.
I have been on alot of different tablets which none really work I am praying for a miracle as I am young and would love my life back.
Hi Rachel, stay tuned to Health Rising – we will have a way for you to easily find trials in your area.
New to this site. Been suffering with FM for over 12 YRS. I’m completely miserable and fed up. All I have been finding are Dr’s who want to push you off to another Dr. I’m on lyrica and cymbalta. Nothing has worked well enough to where I can function. Brain fog is the worst, the flare ups last for weeks. I’m hoping for better treatments.
Denise, there is so much research going on right now. Hang in there and there will be a better treatment in future. It is hard waiting but if you are able, focus on the things you can control and the things that make your life richer. Take care x
I have had chronic fatigue and fibromyalgia for 20+ years. My rheumatologist believes they are on the same spectrum, but I see that a few people here see them as distinct conditions.
I have found Endep (amitriptyline) to be the most effective treatment but I still feel I could have a much fuller life if I could find a better treatment. Endep takes the edge off the pain/ muscle spasms and helps me get more restful sleep and think more clearly as a result. I also find saunas and yoga really helpful.
I have tried a few other treatments to no real benefit and in some cases (particularly Lyrica), to my detriment. Lyrica is a powerful drug which took away all my pain but made me crazy (anger/ hostility – and I am a very gentle and calm person usually). These side effects stuck with me for years afterwards. As a result, I am wary of trying Cymbalta, which my doctor recommends.
I am interested in the literature on neuro-inflammation and wonder about trying low dose naltrexone (LDN) or CBD. I’d be interested to hear if anyone has been down a similar path and can compare Endep to LDN or CBD/ another treatment. Thank you!
I also wanted to mention the research in Calcium ion channels for FMS and CFS, which is interesting. I hold a lot of hope that this will lead to some more effective treatments.
https://www.abc.net.au/triplej/programs/hack/breakthrough-in-diagnosis-of-chronic-fatigue-syndrome/10188210
https://www.healthrising.org/blog/2019/06/12/nimodipine-calcium-channel-blocker-fibromyalgia-chronic-fatigue-pt-ii/