

“I have sympathy for people with chronic fatigue syndrome now, and I believe this disease fast-tracks you into experiencing these symptoms.” Paul Garner – Infectious Diseases Specialist
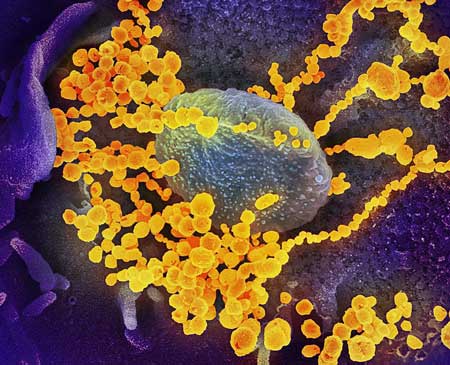
A lot of infections can trigger chronic fatigue syndrome (ME/CFS) but in some ways SARS-CoV-2 is different in ways that reminds one of ME/CFS. For one, it’s causing weird symptoms (loss of smell and taste, buzzing, electric, vibrating sensations, red/purple faces, purple toes, pink eye, digestive issues, nausea, dizziness, cognitive issues) that aren’t usually associated with a virus.
The director of infection prevention and control at Mount Sinai Hospital attributed the weird fizzing-type sensations to the immune system acting up:
“Our immune cells get activated so a lot of chemicals get released throughout our body and that can present or feel like there’s some fizzing. When our immune response is acting up, people can feel different sensations… I have heard of similar experiences in the past with other illnesses”.
Post COVID-19 Cohort Showing up in the Media
It’s early yet, but thus far, the post-COVID-19 ME/CFS-like cohort appears to be showing up as predicted, and when it does it’s freaking people out.
Paul Garner, an infectious disease professor, and Director of the Centre for Evidence Synthesis in Global Health, and Co-ordinating Editor of the Cochrane Infectious Diseases Group, knows infections on both a personal and professional level . During his tropical infectious disease research, he came down with malaria and dengue fever, but nothing he’s encountered has compared to his bout with COVID-19.
Given the fizzled attempt of the UK’s NHS to introduce a little CBT into the coronavirus discussion, Garner’s post on his unrecovery from COVID-19 couldn’t have landed in a better place – the opinion section of the British Medical Journal. Garner, called post COVID-19 a: “a roller coaster of ill health, extreme emotions and utter exhaustion.”
Garner doesn’t appear to be describing post-COVID-19 illness so much as he’s describing a descent into ME/CFS. All the hallmarks are there – the post-exertional “malaise”, the delayed and mind-boggling symptom flares after little exertion, the inability to understand his limits, Garner talked about the “apparition”, a semblance of improved health that kept getting smashed as he innocently overreached.
“People who have a more protracted illness need help to understand and cope with the constantly shifting, bizarre symptoms and their unpredictable course.”
While Garner specifically mentioned ME/CFS in his piece, a recent New York Times piece, “Surviving Covid-19 May Not Feel Like Recovery for Some”, did not but you could replace every mention of COVID-19 with ME/CFS and not skip a beat. We could be watching a slow-motion epidemic of ME/CFS unravel before our eyes.
“Some of the longest-suffering Italians are finding themselves in physical and financial uncertainty, unable to shake sickness and fatigue and get back to work.”
“We have seen many cases in which people take a long, long time to recover. It’s not the sickness that lasts for 60 days, it is the convalescence. It’s a very long convalescence.” Alessandro Venturi, director of the San Matteo hospital, Pavia, Italy.”
“It leaves something inside you – and you never go back the way you were before.”
Another doctor noted that after all the different, initial symptoms were gone, it was the fatigue that remained. That rang bells. Early studies of the ME/CFS outbreaks came to the same conclusion: the early symptoms were often different but the fatiguing state that ultimately remained was quite consistent.
The medical profession generally treats acute cases of infections and then drops out. Dr. Bateman noted in “ME/CFS Diagnoses Could Rise After Coronavirus, Researchers Suggest”:
“Because we generally, in the past, haven’t taken viruses seriously, we simply tell patients to ‘go home and rest up’. The significant fraction (which might be as high as 1-10%) of patients who do not recover normally after infection have often been marginalized and forgotten.”
This time there may simply be too many unrecovered patients for the NIH and other medical funders to ignore. After Fiona Lowenstein opened a Facebook site for people struggling to recover from COVID-19, it was flooded with thousands of members.
“I thought I had fully recovered a couple of weeks ago, then I relapsed into some old symptoms, chills and sweats. And this intense feeling of fatigue. It almost feels like I’ve been hit by a truck at 4:00pm each day.” Fiona Lowenstein
The Special COVID-19 ME/CFS Cohort
Picking the right cohort to study will be important. People who land in intensive care, and on ventilators, for instance, are often going to have trouble recovering, not necessarily because of ME/CFS, but because of the damage to their lungs and other organs that has occurred. The long-term effects of having “acute respiratory distress syndrome” are well known.
These more complicated patients, many of whom are older and have risk factors such as diabetes, heart conditions, lung conditions, liver disease, etc. don’t readily fit an ME/CFS profile. A recent case series study that tracked the course of disease in 5,700 patients in 12 different New York City hospitals found that the median age of the hospitalized patients was 63, and that the vast majority of the patients (88%) had two or more dangerous co-morbidities.
It certainly doesn’t usually take a hospital stay to cause ME/CFS. Simply a nasty cold is all that’s needed to set one up for decades of illness. Healthy people with zero risk factors who weren’t hospitalized – but who haven’t been able to recover – are the group we need to focus on. The illness in any other group could be too easily tied to lung damage or some other issue associated with severe illness.
The non-ICU group is also the group – people in the prime of their lives who become chronically ill – that we, as a society, should be most focused on. This group is starting to showing up as well.
“But there is another unexpected element: a growing number of reports that even people with mild illness, who didn’t go to hospital, are experiencing long-lasting symptoms. Some people infected in February or March are still being ambushed by extreme fatigue, headaches, sudden breathlessness and problems concentrating or doing even light exercise.”
Many will probably recover, but if COVID-19 patients go the way of past Ross River virus, Coxsackie B, Giardia and SARS patients and others, a subset will remain quite ill.
Not Seizing the Moment …Yet.
The NIH is not yet attempting to understand the long-term effects of COVID-19. A variety of searches (post COVID-10, COVID-19 sequelae, COVID-19 recovery) of the NIH Project reporter site found just one study that might be helpful.
To some extent, that’s understandable. COVID-19 has presented the NIH with a once-in-a-lifetime (hopefully) all-hands-on-deck, find-answers-now kind of crisis. They are not looking to the future: they’re just trying to get through the present.
One group, thankfully, is definitely seizing the moment.
Seizing the Moment: Open Medicine Foundation Launches International ME/CFS COVID-19 Study
We may never have a bigger moment, a more ripe opportunity to get at chronic fatigue syndrome (ME/CFS), or a greater chance to get on a bigger stage.
Being able to definitively show that large numbers of formerly productive, healthy people have been unable to recover from COVID-19 would put us quite a ways down the road to definitively erasing the stigma associated with ME/CFS. Being able to uncover how that happens molecularly could, of course, give us the answer or answers to this disease. Plus, bringing the new ME/CFS patients into the community’s fold could provide a rocket boost to our fundraising and advocacy.
That’s why the Open Medicine Foundation (OMF) and Ron Davis’s decision to seize the moment and produce an international effort to understand how COVID-19 turns into ME/CFS is so welcome. The OMF’s four-site COVID-19 study (Stanford, Harvard, Canada, Sweden) will collect body fluids, do continuous health monitoring using wearables, and collect symptom data over two years. Its genomic, metabolic, and proteomic analysis will attempt at the molecular roots of ME/CFS as it occurs.
We’ve had research efforts examine post-infective fatigue states before but never with the tools available now.
Whitney Dafoe Urges Support of the Study
Whitney Dafoe, Ron Davis and Janet Dafoe’s severely ill son, is so ill that he rarely makes statements, but with this study looming, he did. He made clear why everyone, healthy or ill should support it.
“My name is Whitney Dafoe and I have severe ME/CFS. I have had symptoms for 15 years but have slowly gotten worse because of a lack of beneficial treatments.
I am only able to communicate by taking a drug called Ativan which temporarily alleviates some of my sensitivity to contact with others. It takes hours to communicate these posts and makes me worse, but I do it anyways because most people with severe ME/CFS simply disappear into dark rooms never to be seen or heard from again and someone has to tell our story. We exist.
ME/CFS is an extremely devastating illness that takes and takes and takes until there is nothing left but flesh and bone. I’ve lost my friends, my career, my hobbies, everything that brought meaning to my life and all sense of humanity.
Right now, a viral pandemic has spread throughout the world.
Everyone reading this should be worried not just of catching/surviving this viral pandemic but what might happen to their life even if they catch it and survive. Because one of the known triggers for ME/CFS is a viral illness. A huge population of ME/CFS patients got the virus Mono and never fully recovered, instead they wound up with ME/CFS.”
Should the expected explosion of problematic COVID-19 recoveries or non-recoveries occur, the data collected during this study by ME/CFS experts will only grow more and more valuable over time. Perhaps this time we’ll have the NIH knocking on our door.
Health Rising, as a rule, does not directly endorse fundraising efforts, but in this case, it’s making an exception. I’m supporting this effort. I hope you will as well. You can support it here.
Other Studies
Other post COVID-19 efforts/ studies that could help are underway.
The Solve ME/CFS Initiative – The Solve ME/CFS Initiative is also working on a group of COVID-19 projects. Health Rising will report on them as they become more fleshed out.
Leonard Jason of DePaul University – Leonard Jason quickly applied for and got a university grant to assess COVID-19 in the almost 5,000 college students he’s been tracking after they come down with infectious mononucleosis. So far, he reports that about 5% of the college students he’s contacted have come down with COVID-19. Jason, then, is in the unique position of possibly have two post-infectious cohorts to study. He’s been trying to get funding to assess his infectious mononucleosis samples. Now he’s going to try to get NIH funding for the COVID-19 patients as well.
Year-long Australian Study Underway – The nice thing about the year-long study at St. Vincent’s Hospital in Sydney, Australia is how quickly ME/CFS got into the discussion. Lead by Greg Dore, an infectious diseases expert, the study, which will look at “any effects” of COVID-19, is not focused on people with very severe pneumonia or organ damage. It’s interested in every possible long-term effect of the virus.
“We’re interested in even the milder cases, whether there is an ongoing effect on people’s health, what we call a post viral fatigue; effects on people’s exercise tolerance, on neuro-cognitive function, so ability to concentrate.”
Dore clearly knows of the groundbreaking ME/CFS Dubbo studies which took place in Australia.
“We know that you can get post viral fatigue with other viruses and glandular fever is probably the classic one, but Ross River fever and other viral illnesses are well known to cause viral fatigue.”
UCSF COVID-19 Follow-up Study
The University of California at San Francisco’s (UCSF) long-term, longitudinal study is not designed to investigate post-infectious illness but it will include a wide spectrum of SARS-CoV-2 infection severity, and will collect large volumes of peripheral blood and saliva during frequent intervals for two years. Among other things, they will dig deep into the immune response to COVID-19, focusing on T cells, and define the long-term kinetics of the antibody response.
Update – As of June 5th, four major media outlet articles, three of which have mentioned ME/CFS, have highlighted the difficulty some people have recovering from COVID-19.
Conclusion
This is an opportunity not to be missed.






It is like wthney says: Because ONE of the known triggers for ME/CFS is a viral illness. i am glad what omf is doing with covid and other researchers! but before covid, I experience (might be wrong, very ill) that the focus allready was on post viral fatigue.Or better said post viral me/cfs. When will there be attention to other causes with the same devistating effects? in my case it was a mix from everything over 3 decades that made me severelly ill. infectious ofcorce but also just even for excample a stupid to hot summer, a fall or just no reason… I would wish they looked into other causes to and not only the infectious one
Good to hear from you Konjin. It’s been awhile! As someone with a non-viral trigger I understand your concern. I think focusing on the infectious onset – as Avindra Nath is doing at the NIH – is probably the fastest route for all of us.
My guess is that if researchers can get at the core of the patients with one kind of trigger that will illuminate what’s going on with the rest of us. Our symptoms, after all, are so similar and the stress response apparently responds in similar ways to all sorts of different stressors.
How many ways can post-exertional malaise be caused? Let’s hope not too many!
Why does Dr byron Hyde of Nightingale Foundation say true ME can only be caused by an enterovirus infection yet others say mono, Q FEVER, ross river and now covid19 can cause it. Is ME and CFS the same illness if you have a different virus? Why would an enterovirus be any different to catch although I gather they used to cause poliomyelitis.
I think he’s wrong about that. Certainly the weight of evidence and that includes some really good studies, indicates that a variety of pathogens can trigger ME/CFS. It appears that any bug with causes a strong illness can do the trick. There’s no physiological difference that I know of between people who caught it because of one virus vs another.
I understand your comments and they are relevant. However a patient with typical ME/CFS may very well have had a virus infection as a trigger with no symptoms of the virus infection at the time when it began. Coming from pediatrics/ neurology that is extremely likely in other assumed post-viral diseases (acute cerebellar ataxia etc). Virus infections with serious consequences may very well themselves to under the radar.
Kristian Sommerfelt, professor pediatric neurologist, Univ of Bergen, Norway.
Interesting! Given my onset I wonder if that could have happened to me.
A truly remarkable quote by Dr. Paul Garner: “I have sympathy for people with chronic fatigue syndrome now.”
I never thought I’d see it – I hope this really is our moment.
yes, truly remarkeble… What must happen to us before they see us???
The “now” shows how much embedded contempt he had for patients…
I think his sister has M.E. and she’s been helping him. I don’t know what their relationship was like before but he seems on board now
Fairly typical of doctors to dismiss things they can’t diagnose with one test, or the usual/common tests they think they have. Some just can’t think outside the box. And for other people – if it doesn’t affect them personally, they don’t care; don’t take the time to understand it; or worse yet, dismiss it outright. It’s only after he, himself, is coming down with some post infectious fatigue that he “believes”. Sad.
I saw a video where Dr. Oz interviewed Ian Lipkin, where they were talking about the Coronavirus. As many of us know, Dr. Lipkin contracted Covid and during this interview, he mentioned how he’s having a problem getting over the fatigue. He also mentioned ME/CFS.
I’ve been wondering about him. Was that recent video? Of all the people I hope he fully recovers.
I was thinking the same as I was reading this article. I was curious to know how Dr. Lipkin was doing post-virus and if he was going to provide any updates to anyone in the ME/CFS community. Cort, do you know if he ever provides interviews?
He can be quite available. I’m leery right now of trying given all the COVID work he is probably engaged in but will try at some point.
This will sound horrible, but if anyone HAS to get ME/CFS from COVID, of all people, I’d hope he (or someone who can make a huge difference in CFS research & funding) gets it. Self-interest is most powerful motivator to find a cure.
I can not remember how many decades ago, there where more the 300 kinds of reuma. ME/ cfs is so heterogenous. Even the many definitions. I can not understand that they where talking befor covid, about precicion medicine and precicion therapeutics where needed and I thought even precicion tests. TO SOLVE ME/cfs. and now covid comes and all the rest is gone…
I don’t think so Konijn – there seem to be many people becoming interested in ME/CFS. Covid’s glare might be blinding us to what else is going on.
Anyway good to see you’re still hanging in there! I was getting concerned as you hadn’t commented for ages. I was wondering what, hopefully, might bring you out? ?
Sweet of you of thinking of me! do you really think they are looking as hard at other causes of me/ cfs or the 25% severely ill ones and the different reasons for declining as for pôst viral or other post infectious desease that leads to me/CFS? I thought there are only a few studys for for excample the 25% group.
You did not read anymore from me because declining and I alomost can no longer read the post.
But really sweet of you!!!
Hopefully this is the opportunity for more precision medicine. Ron Davis wants to get at the molecular heart of this disease. If he and the other Centers can pin down the molecular changes as formerly healthy people come down with ME/CFS then they can a) hopefully find ways to reverse them and b) see if they apply to other kinds of ME/CFS patients.
My guess is that there are similar core disruptions. They may be coming from different directions; i.e. an infection is causing it in one person, a toxin in another, and an accumulation of things in another. For me, I have no idea what the trigger was.
The post-exertion problem seems so distinct or rather so heightened in ME/CFS that I’m hopeful that there is one similar cause for that – some core damage that is consistent across all of us.
I hope you are right about the possibility of being core disruptions. My adult daughter has had symptoms of ME/CFS prior to 3 yrs old. Eventually she was Dx with its common comorbid illnesses, POTS and EDS. Not until she was out of high school and in college did she receive her ME/CFS diagnosis. We know of no known triggers and since I also suffer from very similar symptoms but much less severe I don’t think this could be virally triggered in our case, or could it have and I passed on the virus. Sorry to get off point but I was hoping to use the opportunity of this discussion to get some opinions. I feel like my daughter, Konijn, Cort and myself are all stumpified as to our triggers.
Ron Davis has always been looking at the possibility of any cause he can find. His group has delved into several and has plans to look at more, with more funding.
Ron Davis is so tireless in his work. I can’t imagine how weary he might get at times. Thank you Dr Davis, for all your hard work and to you Janet for the Huge part you must play in it all. Thank you Whitney for hanging in there and encouraging those with me/cfs, all over the world. The me/cfs community cannot thank you enough. I’m sorry Whitney, that you are so sick with this illness. I cannot believe it has taken a pandemic for us to possibly get the help we need. It’s so double edged. Were we not worthy of such research and medical care. Now the well and able bodied are affected we may get the medical help we so desperately need. In Dr David Tuller’s words, I cannot believe people can be so sick and so debilitated and governments and health care systems everywhere have abandoned them, leaving them to fend for themselves. It is so negligent and criminal. Let’s hope the funding for research and improved understanding is the Covid19 silver lining.
The ME/CFS community cannot say enough about what an amazingly brilliant minded scientists Ron Davis is! The level of devastation, and suffering that ME/CFS inflict on its victims, and their families is Immeasurable!
This disease has caused untold losses to millions around the world. On top of struggling with a horrible disease the fact that this patient population has faced unprecedented discrimination, gaslighting, biases and marginalization for 30 plus years is beyond inhumane! This is evident by the very high rate of suicide as cause of death from ME sufferers.
Ron Davis has been our saving grace and only source of hope and light in a very dark place. His commitment to finding answers in unrelentingly! He is an incredible human being that has taken the tragedy of his own sons very serious battle with ME and turned it into his personal mission to bring treatment and hopefully cure to millions worldwide. He is truly one of the greatest human beings and scientists we could ever hope for!
Donating to his efforts to tackle this extremely complicated monster ME and possibly stopping millions of people from suffering for decades is the most righteous cause anyone can donate to!
So give freely knowing you played a small part in relieving untold amounts of human suffering of millions!
Thank you to Ron Davis his amazing wife Janet Defoe who also does lots of advocacy and reaches out to personally encourage ME sufferers and their care givers. And of course Whitney Defoe who continues to also inspire ME community even though he is probably the most severe case.
This is a tip for everyone who has me/cfs/fibromyalgia. I got a severe viral infection in Nov. 1997 while on a 3 week work trip to London. I am actually sure that it was communicated by a passenger in the plane sittting next to me. After 3 weeks lying in bed with my throat so swollen I could not talk I finally made it to one sales meeting. At that time I was the lead network engineer for the company. I felt better when I got home but never recovered. I was able to work for 4.5 years following but it was a downhill spiral all the way. My doctor then ordered me to quit working because if I continued it would kill me. He was not wrong. July 2002 I was fully disabled. In the interim I was diagnosed with hypogonadism (no testosterone) and began weekly intramuscular injections. .An infectious disease doctor diagnosed “CFS” and said no treatment and nothing he could do … basically dont bother coming back. My GP then told me he did not believe in CFS. He had referred me earlier to a Rhumatologist who diagnosed Fibromyalgia but but GP never informed me of this dagnosis. Those were the days, sick as hell and nobody believes anything you say. I was increasingly having Migraine headaches. By 2004 I was in a wheel chair (electric, no way I couls push myself in a manual chair). That was the beginning of a 14 year wheelchair bound stint. I caught a break when a close friend (a pediactric gastroenterologist) suggested that my muscular symptoms were similiar to an inborn condition sometimes seen in newborns (ie DNA problem) in carnitine metabolism. My neurologist first suggested that there was a blood test fot that and when it was positive he researched treatment and then put me on about 3 grams of pharmaceutical Levocarnitine a day. Two weeks later I was migraiin free and have not had another one in the past 16 years..
My lesson was these viral illnesses are really nasty, they can even mess up your DNA!
I have made more progress, I found out about a Co-Q10 substitute through Cort Johnson, and was able to enroll in a small double blind study back in December 2015. I had the placebo first but when I started on the real thing I immediately knew something was different. That was in the beginning of 2016. I also met a physical therapist who is amazing at Myofascial release massage and started a weekly regime. In October 2018 I was finally able to begin walking again without the wheelchair! WoW.
Now with this Covid-19 epidemic, well I got it. Just 2 weeks in and so far it has not been too bad. My daughter, however, has been struggling with it for 9 weeks. About 3 weeks ago she was in the ER and her lungs were OK but she had a d-dimmer test (blood clotting factor) that was off the charts high. Since then that test normalized and she was able to get through 3 days without a fever but she has been fatigued and occassionaly still gets a fever in the evening. It appears she is having Post Covid-19 fatigue.
As for me, well I am hopeful tihs will be a mild case and I will be back wherver I was before this episode began. I have been following a Facebook group for Covid-19 suvivors and a lot of people are having problems.
I hope this is legible… and Carpe Diem I guess..
Cort, thank you for everything you do. You are amazing as always
Greg
Glad for your improvement Greg, out of the wheelchair.
Wondering if you feel up to posting what lab did carnitine test and name of test(s) to check for it?
if not, no worries, just get the rest you need please.
What a fascinating story Greg and how interesting that such a variety of treatments – testosterone, Levocarnitine, a kind of CoQ10 and myofascial release massage turned out to help.
— What were the muscle symptoms you were having?
— Did your muscle knots eventually go away?
— What test did you do to check for carnitine dysfunction?
Greg,
See if your daughter’s physician will check her EBV VCA IgM levels. I’ve already had one (possibly two) post-Covid patients whose secondary prolonged symptoms were (probably) from activated EBV. Especially if her prolonged symptoms dont involve pulmonary issues and are more fatigue,myalgias, and malaise.
I think this is how the developing CFS/ME patients will present post Covid. Hopefully not, due to what that might mean long term, but it may be worth checking to help decide how to treat her symptoms now.
Greg, ME/CFS has also given me very low testosterone too, my go says he usually doesn’t send people for treatment for this but mine was so low he suggested that I should. I have ignored it so far. Did treating it improve your symptoms in any way?
TY for relating this to us Cort. I think there may be real diagnosis and treatment possibilities in the presumption that viral stresses (perhaps in concert with a genetic predisposition) may cause CFS and/or Fibromyalgia.
However, this does not mean that viruses are necessarily the only stressors that can trigger these chronic symptoms. Personally, I strongly suspect that Mast Cell Activation Syndrome (or MCAS) is implicated – often, if not always. Mast cells are the first cells to activate the immune system (and the inflammation that attends it). If the mast cells are triggered but remain chronically over-activated, it can cause smoldering inflammation and no end of secondary symptoms throughout the body (with fatigue being the most prevalent). If this interests you, and you don’t mind reading, I have provided a link below to some well-documented medical information on MCAS. This information fit and explained my symptom profile and history – perfectly, and, may fit yours. This information does not contradict or de-value the information, insights or opportunities presented by the article above. Rather, it complements and expands upon it. Hope you enjoy, and good luck on your journey. P.S. You may want to skip past the long early section on MCAS history.
https://www.jillcarnahan.com/downloads/MCAS-Afrin.pdf
This is true. But we do need the H2R (Receptor) and H3R to stay turned on and not blocked as they regulate the immune system. What turns them on is histamine. And it comes from degranulation of mast cells on/by H1R activation. We need the histamine to do many things and turn on what helps with our T cell response.
I do have MCAS and very severely. (Hospitalized in ICU one night.) So trying to moderate receptors and not take antihistamines has been a risky undertaking. But I am having some success. If I don’t get on top of a MCAS “attack” fast enough, and dont get my H2R turned on and moderating the release, I will resort to a sip of Children’s Allegra or GastroCrom. One is a mast cell stablizer, the other stops H1R receptors and calms down the degranulation.
There also was a paper linked by Bayard showing that an H1R antihistamine could calm down the degranulation and cytokine response and inflammation chemicals in the COVID19 virus. (Mast cells play a part in our immune function and are being researched in regard to this virus.) But it says nothing of blocking H2R or H3R, as they help with these immune responses too. So a little bit to activate them is desired. Also, histamine is now being given for Alzheimer’s, Parkinson’s, MS, Narcolepsy as a help in these illnesses.
https://www.researchgate.net/publication/340815617_Pathogen_Stimulated_Histamine_Production_and_Release_by_Neutrophils_as_a_Potential_Therapeutic_Target_in_Preventing_Progression_of_COVID-19
So if we had our receptors working as they should, this release of histamine would be a type compensation and a good thing. Where the problem lies, is not having them come on and moderate that response properly.
There is a thread on this on the Health Rising forum, also started by Bayard. I’ll try to get that link too.
I was just sent this interesting paper on MS and them finding histadine is low and they think causing fatigue. Histadine is precursor to histamine. Giving it is upping histamine in the brain.
Interesting as I just added a new supplement a few weeks ago to add more histadine and another thing. (Part of an ongoing experiment. )
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7241417/
https://www.ncbi.nlm.nih.gov/books/NBK28245/
Here is a link to an article and how histamine can actually be a benefit to the body and brain function. Just needs to be moderated and H2R turned on, by histamine, moderates it.
Thanks Dave.
I’m curious if there are hypotheses why MCAS got started in the first place? It appears that a virus could trigger it, and if, so the OMF’s study would hopefully pick that up (???)
I had one of my patients test positive for Covid 19 around 6 weeks ago with symptoms of fever, chills, and SOB/Cough. She recovered without going into the severe “cytochrome storm” phase, but then started feeling worse again a couple if weeks ago. Except, this time, she had symptoms of severe fatigue, myalgia, and malaise without fever or pulmonary symptoms. Today her labs returned with a positive EBV IgM titre and elevated sedrate of 50, and we discussed that she was likely developing post-viral CFS/ME.
I’m interested to see if anyone else has noted this, or whether they are testing for secondary viral infections rather than presuming that symptoms are just a prolongation of Covid 19?
Isn’t that something! Is EBV reactivation after a (different) viral trigger a or even the pathway into ME/CFS? That’s the kind of fascinating possibility that this study could show. Does an severe infection trigger EBV reactivation in some people who remain ill?
I’m crossing my fingers for this study…
This is for Bryan Evans as well… If I am understanding Dr. Robert Naviaux’s and Dr. Bupesh Prusty’s most recent paper correctly, they’re investigating reactivated HHV-6. I was exposed to HHV-6 as a child, but I did not get ill with ME/CFS until I was exposed to EBV about 45 years later. I’ll put a link to their paper at the end of this comment.
I, too, have prayers said and fingers crossed that Dr. Ron Davis’ Covid-19 study will find a silver lining to this very, very dark cloud. I’ll be 63 in a couple of months, sick for 12 1/2 years. While I’m trying to stay cautiously optimistic, I have gotten my hopes up to only have them dashed again too many times. That roller-coaster is far too costly.
https://www.immunohorizons.org/content/4/4/201
Dear Bryan,
Please check to see if your patient is living in a home with a mold issue.
My EBV reactivated because of living in a moldy apartment building. It’s an environmental factor that can hobble someone’s immune system.
If she was living in a moldy home and could get out, then you could try Dr. Brewer’s protocol on her and see if you can nip the ME/CFS in the bud.
It is pretty sad to hear about someone looking like they are getting ME/CFS.
I feel like ME is initiated by exposure to some chronic virus along with a period of high stress on the system, whether that is mental or physical. No mold in her case, but she was under extreme mental stress to return to work as she wasn’t allowed testing(early in outbreak)
BTW, her employer required her to return early eventually infecting two others in a food-handling service restaurant.
Wow, that is really tough.
I put the wrong link on that though you can get to the article that way, but here is Bayard thread on histamine and the virus.
https://www.healthrising.org/forums/threads/mast-cell-histamine-immunotherapy-with-histamine.6233/#post-36599
https://www.healthrising.org/forums/threads/pathogen-stimulated-histamine-production-and-release-by-neutrophils-as-a-potential-therapeutic-target-in-preventing-progression-of-covid-19.6353/
Here’s the link to the thread on Healthrising to COVID and histamine.
Yeah, when this Covid thing started I was thinking, here comes a huge new batch of ME/CFS. Well, along the way I got a ‘something’ in mid February and Stanford has since found that the virus had already been circulating in my area for at least a month earlier. Finally, today I got granted a serology test and will know in a couple of days whether I actually had the virus. And yes, my ‘something’ waxed and waned for quite a few weeks and even now, I still feel the fatigue–a kind of double dose of ME/CFS.
@Greg, I admire all your efforts! Persistence does pay off!
Sure hope the shear volume of post viral fatigue inspires more research!!!
It is too early to diagnose ME / CFS. The COVID patients who still have complaints after 2 months can still recover within this year. If this does not happen and the complaints get worse and the lungs are recovered and there is no other medical explanation for their complaints, then we can speak about ME / CFS. But it looks like this will be the case for some COVID patiënts.
As I remember the past studies show the percentage of those still ill dropping all the way to at least a year out . Even after six months some people do recover.
Thank you. I’m 66 days into Covid and debilitating fatigue; praying that it doesn’t turn chronic.
Yes, and no or? The good thing is that it is a long term study over two years. Then after that you will have data on both those who recover and those that maybe not recover. Anyway, it will collect data that might explain post-viral fatigue, and that is VERY important as there really is so much we do not know yet.
There is alot of research on fatigue from several angles and I think that that is good to, also for ME/CFS.
It is very funny that mold is not mentioned in any comments because it is MOLD that started CFS in the first place. This viral illness is secondary to the effects that it has on the system. Get away from mold and get better!
Yes! ME/CFS – is the world’s biggest infectious outbreak ever!!! and the best kept _SECRET_…why? Reading a book by Neenyah Ostrom called “America’s Biggest Coverup”…not just America coverup anymore either. The theory put forth is that HHV6 (possibly another name for African Swine Fever virus- that would explain the secrecy)…..HHV6 causing ME/CFS and AIDS, as well as several other diseases. What ever happened to Ampligen, it worked didn’t it? There are also other treatments for HHV6 but we don’t hear anything about them. So many people infected worldwide since at least the 1980’s, some a lot earlier, and still we have nothing: no test, no treatment. Why not? At least we don’t have toxic AZT! It has been so long now that people new to the disease don’t even know about the past and there is quite a past! Why do most doctors still not know anything about ME/CFS? Why is it not on everyone’s radar as it spreads like a pandemic, all in silence. Enough already!!! If not now, When?
P.S. Low NK cells seem to be a common sign of ME/CFS and HHV6 Infections.
Thanks Cort for all this writing and research you do to keep us updated.
Much appreciation.
And great appreciation to OMF and Ron Davis and his team, for research that keeps us hoping. and OMF for the much needed fundraising.
and Solve for the research and awesome Congressional work
MEAction for giving us a place to advocate effectively.
and others, the scientists across the globe working hard now.
I am hopeful again.
Good to see an OMF attempt to track a new post-viral condition. But it’s not unique, this reminds me of another recent post-viral study. The 2018 study that followed a group of teenage EBV patients to collect data as some developed CFS. The researchers tracked a few immune parameters but did not learn much. Slight differences in CRP and B12, so a little more inflammation and those with lower B12 had more fatigue. All other findings were just differences in symptoms. I hope this time we can learn more, sounds like researchers will be collecting more data than the 2018 EBV study, so here’s hoping…
In case anyone is interested:
https://www.sciencedirect.com/science/article/pii/S0889159118306251
I agree that past studies like this haven’t been nearly as illuminating as one might have hoped. Hopefully Ron Davis and colleagues can get enough funding to do a really deep dive.
Very interesting , first time reading this blog. I got chronic fatigue after returning from Paris with a virus three years ago. I am fortunate it is mild, need to have a long nap after lunch and go to bed early. At first I thought it was from aging since I was in my early seventies but now accept it is CFS. One of my doctors agrees with me because her husband had it, but my internist is not very interested.