

The neuroinflammation findings in chronic fatigue syndrome (ME/CFS) and fibromyalagia (FM), while restricted to a few studies, are still pretty compelling. We know that many, if not all of the symptoms associated with ME/CFS and FM such as fatigue, pain, cognitive problems, and mood issues can be produced by the brain.
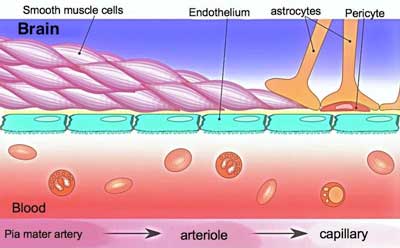
But how to treat the brain? Getting compounds into the brain is not easy. For one thing, when taken orally they must enter into the general circulation, get broken down by the liver, and then surmount the blood-brain barrier (BBB) – a circuitous route.
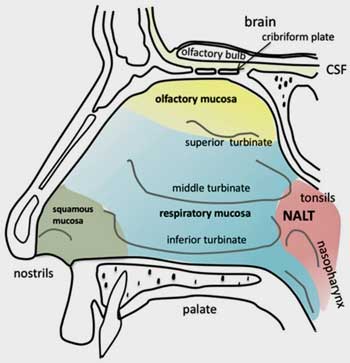
The nose provides quick entry to the brain. Could intranasal delivery represent the future for ME/CFS and FM?
There may be an easier route. The brain’s only direct contact with the outside world comes through the nose. There’s no blood-brain barrier to worry about. Anyone with a bloody nose has direct experience of how well vascularized the nose is. Plus, stimuli from the nose don’t go through a peripheral nerve intermediary as do all other stimuli – they shoot straight into the brain.
Intranasal.net reports that absorption rates through the nose are similar to those achieved during intravenous infusions. It asserts that atomized pumps provide better delivery systems than nose drops, plastic bottle nebulizer and pressurized aerosols.
Given the more direct drug delivery route, intranasally delivered drugs have the potential to be more potent, work more quickly, be better targeted, produce less side effects and be more effective overall.
One review of the field stated that “intranasal drug delivery has emerged as a reliable method to bypass the BBB and treat neurological diseases.”
It’s not a done deal, though. Anything which irritates the mucosal lining of the nose wouldn’t be tolerated, congested nasal passages could inhibit delivery, and it’s not clear how far or where into the brain the substances might reach. If intranasal administration works, though, it might just be the ticket for cooling the fires in the brain.
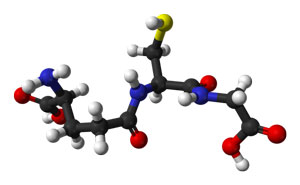
In ME/CFS, cooling the fires of the brain means upping the levels of the master antioxidant of the body – glutathione.
The Master Antioxidant – Glutathione (GSH)
Shungu’s findings suggest that high levels of reactive oxygen species (ROS) and low levels of antioxidants (glutathione) are part of the neuroinflammatory mix in the brain in ME/CFS. If that’s true, then ME/CFS is not alone – low levels of glutathione have been implicated in many central nervous system diseases (multiple sclerosis, autism, Alzheimer’s disease, Parkinson’s disease, schizophrenia, and bipolar disease) as well.
Glutathione – the “master antioxidant” – scavenges or neutralizes reactive oxygen species such as the hydroxyl radical (*OH) in central nervous system cells, and plays a role in detoxification and other functions. If not enough glutathione is being produced relative to the oxidative or free radical load present, then the free radicals, seeking balance, will rip holes in the neighboring cells and neuroinflammation will occur.
But how to tamp down those fires? Taking glutathione in orally will not do it – its bioavailability is too low. Liposomal and sublingual forms and creams have more availability and N-Acetylcysteine (NAC), a precursor, can cross the blood brain barrier, although it has to go through the general circulation first. Infusions of NAC can, however, increase brain GSH levels dramatically.
With its ease of use, intranasal glutathione could be the best option.
Intranasal Glutathione
According to one report, intranasal delivery of glutathione in aerosolized form is believed to have begun in 2003 when a compounding pharmacy in Florida began providing it to people with multiple chemical sensitivity (MCS). The pharmacy later provided it to people with Parkinson’s disease, Huntington disease, chronic sinusitis, Down syndrome, and autism. (Intranasal glutathione is compounded.)
A survey suggested it was well tolerated. The most frequently reported benefits across a variety of diseases included improvement in disease symptoms (45.5%), improved sense of well-being (28.8%), decreased frequency of sinus infections (27.3%), and improved energy (24.2%).
Intranasal GSH has been formally studied only in Parkinson’s disease (PD), a disease characterized by early glutathione depletion. Stymied by the low amount of GSH reaching the brain when given orally, researchers turned to intranasal administration. A 2016 study confirmed that when taken intranasally, compounded GSH does indeed increase brain glutathione levels. A 2017 Phase 2 trial, did not, however, find that intranasal GSH was more effective than placebo. (The authors noted that the placebo response was, however, especially strong.)
Theresa Dowell DNP, who has ME/CFS, reported, however, that both she and Dr. Klimas have found that intranasal glutathione helps in about 80 – 90% of their patients – producing about a 20% improvement in fatigue and cognition. Most patients notice improvement in 6-8 weeks but a three-month trial is called for.
She prescribes compounded intranasal glutathione, 250 mg/ml, two sprays in each nostril three times per day. (Dr. Klimas uses the Key Compounding Pharmacy in Seattle). For patients who have trouble breaking down sulfur metabolites, Theresa starts them on a very low dose and slowly work up to 200 mg per day – about a third of the dose used in the Parkinson’s study.
Clinicaltrials.gov lists just three intranasal glutathione trials – all in Parkinson’s Disease – and all completed. Despite the anecdotal evidence, the medical world is not rushing to assess intranasal glutathione. It’s much more interested in a different intranasal – intranasal insulin.
Intranasal Insulin
Insulin Resistance in the Body
Insulin regulates blood sugar (glucose) levels in the body. While insulin resistance per se – which allows glucose levels in the blood to rise to dangerous levels – hasn’t been found in chronic fatigue syndrome (ME/CFS), an exercise-related insulin resistance which was ameliorated by metformin did show up in cultured muscle cells from ME/CFS patients. Metformin also improved mitochondrial functioning (AMPK) in fibromyalgia muscle cells.
Several studies suggest that insulin resistance may play a significant role in fibromyalgia including one which associated it with memory issues. Metabolic syndrome, which is associated with insulin resistance, has also been found at various times in both FM and ME/CFS.
Insulin Resistance in the Brain?
While we’re more used to hearing about insulin’s effects on the body, researchers are learning that insulin plays a major role in memory formation as well as protein, lipid, and carbohydrate metabolism in the brain.
In “The High Costs of Low-Grade Inflammation“, Dantzer points out that during chronic inflammation, insulin resistance in the brain decreases glucose and protein metabolism in the astrocytes, forcing the neurons to rely more heavily on the less efficient process of lipid metabolism for energy.
A recent study found reduced glucose metabolism exactly where one would expect – in the thalamo-limbic-brainstem regions in women with “functional somatic syndrome” – a category used by some to describe ME/CFS and similar diseases. The authors asserted the women were suffering from “cerebral hypometabolism”.
Reduced levels of insulin in the brain also contribute to the deposition of some really nasty substances (amyloid proteins, neurofibrillary tangles and tau proteins) and neurodegeneration. Central nervous system insulin issues have been linked to Alzheimer’s, and type 2 diabetes.
Intranasal Insulin Field Taking Off
Insulin’s broad effects in the brain have lead intranasal insulin studies being attempted in a wide variety of diseases and conditions including Alzheimer’s, type 2 diabetes, addiction, epilepsy, depression, and to reduce anxiety and fear. Clinicaltrials.gov lists 28 intranasal insulin studies underway or soon to begin recruiting.
Mouse and human studies have found that intranasal insulin reduces central nervous system inflammation and improves cognition by reducing proinflammatory cytokine levels and oxidative stress, and boosting antioxidant levels and mitochondrial functioning.
Dr. Klimas’s modeling studies suggest that intranasal insulin should work in Gulf War Illness – which suggests it would likely work in ME/CFS/FM as well. She will reportedly combine an antioxidant with intranasal insulin in a Gulf War Illness trial. If it works there that would likely open the door to a trial in ME/CFS.
The Future
While ME/CFS and FM might get lucky with a new drug (such as Cortene), the most likely quick advance in treatment, given the poor funding the field receives, will come from other diseases which share issues. The good news is that neuroinflammation is a big deal in central nervous system diseases, and benefits from fighting it in those diseases may very well accrue to people with ME/CFS and FM.
Intranasal administration of treatments is nothing if not a growth field. Glutathione and insulin are just two of the many intranasal compounds Parkinson’s and Alzheimer’s researchers are checking out. Both groups appear to be throwing just about every compound they can think of up the noses of their laboratory rodent models, and some compounds are making it to human trials as well. Anything, it seems, to get a drug or compound past the blood brain barrier to the heart of the problem.
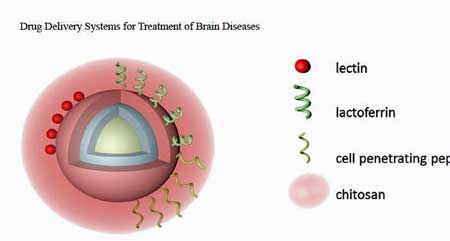
A variety of drug delivery systems are being explored. (From Updated Progress of Nanocarrier-Based
Intranasal Drug Delivery Systems for
Treatment
of Brain Diseases – Fan, 2018)
Nanoparticle formulations of the Parkinson’s drug, selegiline, resulted in 12-20 fold increases in brain concentrations in laboratory animals compared to delivering the drug orally. The drug also significantly increased dopamine, catalase activity, and glutathione content in the brain. (Selegiline is also used in major depressive disorder and ADHD.)
Treatment Takeaways
- Intranasal delivery potentially represents a faster, more effective and safer way to get drugs and supplements to the brain.
- Intranasal preparations of glutathione appear to be safe and well tolerated and have been used by some compounding pharmacies to treat a variety of nervous system diseases for over 15 years.
- Three intranasal glutathione Parkinson’s studies have been done – two with good results and one which showed no significant difference was made.
- Dr. Klimas and Theresa Dowell RN report that intranasal glutathione is typically helpful in ME/CFS when used for three months.
- Intranasal insulin has the potential to improve metabolism, reduce inflammation and improve memory.
- With 28 intranasal insulin studies underway in a variety of central nervous system diseases, intranasal insulin has become a hot topic.
- Many other intranasal preparations using specialized delivery systems involving nanoparticles are being assessed in laboratory – and sometimes human – trials across a range of diseases. These systems can deliver far more of a drug to the brain than the aerosolized or atomized solutions currently available.
- While significant obstacles remain, successful attempts to reduce neuroinflammation could provide a boon for ME/CFS and FM.
The attempts go far beyond aerosolizing a substance in a nebulizer and giving the nose a good squirt. Parkinson’s, Alzheimer’s and other researchers are embedding nanoparticles of drugs in a substance called chitosan (a biodegradable, biocompatible polymer) which can adhere to mucous membranes in the nose and release much more of the drug much deeper into the brain than aerosolized preparations do. Plus, they have a longer half-life and are less prone to bacterial contamination.
The many types of intranasal nanoparticles being developed (polymeric, solid lipid, microemulsions and nanoemulsions, polymeric micelles, nanonstructured lipid carriers, polymer-lipid hybrid, chitosan and PGLA nanoparticles) speak to the richness of this drug delivery field.
Other intranasal preparations being explored in Parkinson’s include dopamine, one using gene therapy, a vitamin E loaded naringenin, stem cells, glial cell-derived neurotrophic factor (GDNF), carnosine, BDNF, intranasal insulin, rotigotine, and estradiol.
For their part, Alzheimer’s researchers are assessing intranasal preparations of galantamine, deferoxamine, tacrine, tarenflurbil, rivastigmine, risperidone, curcumin, quercetin, piperine, and insulin. Other fields exploring intranasal drug delivery include epilepsy, brain tumors and multiple sclerosis.
Almost all of the above cited studies have appeared in the past five years, with the majority published in the last two. Intranasal drug delivery is clearly a hot topic in brain research.
Still, significant hurdles remain. While a few human trials have occurred, most studies involve laboratory animals. Time will tell how this all works out but future opportunities for other central nervous system diseases including chronic fatigue syndrome (ME/CFS) and fibromyalgia (FM) seem clear.
With Travis Craddock and Nancy Klimas uncovering evidence of a possible genetic vulnerability in the mucous membranes of the nose which could potentially explain much in ME/CFS, the nose is becoming an ever more interesting place (blog coming up.)
If you’ve tried intranasal preparations of glutathione, insulin or another substance, please let us know how it went.






I tried intranasal glutathione several years ago, but couldn’t tolerate it. It felt like it was burning off my nasal lining! And yes, it was compounded specifically for intranasal use.
Finding a way to deliver drugs through the mucous membranes of the nose without irritating them is one of the challenges of intranasal drug delivery. Other challenges include finding a way for the drug to attach to the membranes and slowly diffuse across them. If your mucous membranes are already in an irritated state, as well, they might be more sensitive.
I imagine the delivery methods are
I liked the effects but it blocked up my nose dramatically over time. I stuck with it for 9 months but it was tough to administer with my nose so blocked. I might have put up with it anyway if the positive effects had held up more strongly.
The pharmacy said it was likely a sensitivity to the pH, which they try to address in compounding. Not well enough for my nose, sadly.
There is a simple way of doing that: liposomal delivery. And liposomal gluthatione is available (although expensive).
I tried it too. It smelled bad and then it had to be refrigerated so spraying it into my nose wasn’t pleasant.
Other than your nose pain, did it help with the Fibro and CFS?
Hi Andrea – did it help? is it available? no matter how painful it does not matter. I found my 15 yr old daughter been searching the web to commit a suicide. she says I will not be there for her graduation, wedding, you will never see my kids
jade- I hope your daughter is doing ok. Do you know about ketamine for acutely suicidal patients? It can also reduce the physical symptoms of ME/CFS. It’s a very powerful anti-inflammatory and anti-depressant. If she’s still going through this, ad if you haven’t tried it yet, I strongly urge you to look into it. It could save her life. Best of luck to you.
Wow! What a fascinating area of research – right up my street. My most enduring and debilitating issue is with my brain.
Interestingly and something that I find encouraging is that my brain problems are flexible – my brain can function fairly well or abysmally, depending on what I eat or don’t eat.
When I wake up in the morning my brain is just fine – it’s when I eat that the problems kick off. Even if I eat food that I seem to be able to tolerate, I’ll still have what I feel is a drop in available glucose to my brain – not in my body – a few hours later. I have a blood glucose monitor and I’m not regarded as being diabetic.
I have often wondered whether some sort of inflammation in my brain (gut/brain connection?) is causing insulin resistance specifically in my brain?
This kind of research gives me great hope ?
Just have to educate the medical profession ?
Same here. Whenever I eat grain my gut tolerates it well. I even feel somewhat positive effects on my body’s energy. But it slows down my cognitive function so much after a few hours. This effects lasts for a day, sometimes longer, when I feel an inflammation is going on.
Check for POTS and MCAS. After eating, POTS makes all the blood move to your gut. It often makes a “shut down” extra sleepy feeling.
Dear cort,
thank you for the in previous post nice words of reading something from me.
I do not understand that nancy klimas is promissing for years for excampple thhe combo trial (forgot the names of medications) in me/CFS. Now she is talking of other studies in gwi that would help me/CFS to. i have been waiting so long for the combo trial. Do you know why there is nothing happening for me/CFS? On her site it is almost all GWI… and the combo trial seems to me (maybe I am wrong) is not happening. Greatings!
Hi Konjin,
You really disappeared there for awhile! I too was starting to get worried.
I have no idea why it’s taking so long for those trials. The only thing I can come up with is that everything seems to take much longer than expected and clinical trials are the worst. I expected them to be done quite some time ago.
In the spirit of transparency, I joined the INIM webinar Dr. Klimas’s team held two weeks ago. I asked if there were any updates on the etanercept & mifepristone ME/CFS trials that have been reported to be underway this year at Nova on the webinar.
This was Dr. Klimas’s response to me, if this helps shed any light on the situation:
“We had a delay in start up due to some IRB (human safety review ) delays then the COVID-19 epidemic, we were just about to start the first subjects the week that everything shut down. We anticipate a restart in the month of July we will be recruiting
men and postmenopausal women into this open label study. This is a pilot funded by private donations, we are also applying to the NIH next week for sufficient funding to move the project along and expand to the other subgroups”
Hi cort, thanks for your kind words!!!! feeling desapearing again. get worse and worse with sometimes a better moment. Can almost not read the most of the time. So I am no longer up to date…
She certainly talks a good talk. Frankly, not good on the delivery.
Sorry, bit harsh, but she’s talked up lots of things over the years…so I’ve tuned out on her. I don’t have much patience for false hope.
I hope she proves you wrong Matthias!
Rituximab/Cyclophosphamide trial hasn’t been published either. We know the end result of the former drug but no details.
In one of Nancy Kilmas’s videos I was watching, she said GWI is getting much more funding from the government, than ME/CFS, so that is why GWI is getting so much more accomplished. She seemed very sad about it.
Yes, Nancy has gotten much more funding for GWI than ME/CFS and the federal group – which is not the NIH – funding GWI is much more willing to fund clinical trials and several federally funded clinical trials are underway. The feds have funded several very large integrated efforts in GWI. Thankfully, Nancy been able to use that funding to better understand ME/CFS.
Check out this blog for more – https://www.healthrising.org/blog/2019/09/01/klimas-chronic-fatigue-syndrome-guld-war-bacopa-etanercept/
amazing article! I definitely think intranasal medicine is going to be huge for a lot of different diseases!
@Dakota
Thanks for your information and proposing the questions to them??
@Cort
Very interesting and hopeful article of traveling in the right direction, Cort!??
Really loved you including the RPN story in this as well!??
It sounds remarkable, as much as I could understand with the brain I have. I take
compounded Glutathione orally, and now, what to do….. I suppose it is for the future,
mine future is diminishing after 22 years of this wretched illness… not many years left.
So for some it is hope, and I am happy for them, for others, like me, it is just another headline that may offer hope, but eventually doesn’t. The way of things. Maybe I’ll have to start snorting all my compounding ($$$$$) supplements?
Billie,
Your comment made me laugh at the end but I do get your despondency too. I can swing from hope, to acceptance, to fury, to frustration and sometimes to despair.
I am better off myself, if I can, to stay in the hope mode – however deluded that may be… ?
Realistically, I think this illness/these llnesses will be better understood in the future but that isn’t fast enough for all those who are suffering now and barely hanging on.
I send you good wishes and thanks for your sense of humour! Am just going to see if I can find some reasonably priced NAC to add to my supplement arsenal.
It took me ages to try CoQ10 and only tried it because I got it half price, as it was near it’s use by date. I think it may have made a positive difference and I still take it.
Will also make tentative enquiries regarding intranasal medications.
I feel the same way you and Billie do and thank you Billie I needed that lol today to hold back tears!
Had a rough day yesterday..???
To both Tracey Anne and Laura, So relieved someone got what I was talking about, thankyou to both of you. Thank you for your good wishes and appreciation of my
strange sense of humour, can’t always rally that…… and Laura, those rough days
come round far too often, I know, and understand. I’m in Australia where some of
this stuff is not available, and wyes, Tracey Anne, it feels like an arsenal, and I can’t
always think it is worthwhile, except when I realise how many are totally bedridden.
Love to you both, Billie
True Billie and you’re right, I am very grateful that I have managed to cobble together a much higher level of functioning and can therefore participate in life, where many others, like Konijn and Whitney, cannot.
The fear that I experienced when, a few years ago, I was completely out of control and spiralling downwards at an alarming rate is now calming.
I sometimes feel like I’m a conductor of an orchestra, trying to bring out the best in my body – constantly adjusting and trying to sense where things are going.
I’ve made good progress and that fires me on to try and figure out more.
But I do remain grateful for the health I do have and just try and endure the episodes where it all goes wrong and my brain and heart seem to go into meltdown.
Tracey Anne, it is so alarming at times, and I am so glad you have come up
from that terrible place. I find for me, now, after all these years, that
events in life which are distressing for healthy folks, just throw me
completely down in the depths, and that’s what I fear the most at the
moment. Just don’t have that fortitude any more, and certainly had it
many years ago. I wish you well in conducting that body of yours, and
hope that the orchestra plays the most beautiful symphony most of the
days.
Yes, I could be extremely vulnerable too Billie and lost a level of emotional resilience, I used to have.
For a while, I had to literally block potentially negative people/situations out of my life (given the lack of understanding of my particular situation that meant most people) because I didn’t have the capacity to manage them effectively.
If something stressful happened I would be triggered and not to a good place and it felt like my last drops of energy would be sucked out of me – I felt an emotional instability that was unfamiliar.
So what I did was, I created a reinforced clearing within my mind and I lived in and through that.
Your comments have sparked off a whole load of thoughts, in a positive way.
You got me thinking, that maybe if I can consistently keep what I believe is brain inflammation to a minimum, then I may be able to strengthen the more helpful, moderating elements, within my brain, over time.
It’s been really good to exchange thoughts – like no one I know would understand this experience.
The great thing about this website is that it brings together people who might…
Tracey ?
Tracey, you sound like underneath a very strong woman to be able to create that
space in your mind, don’t know if I could manage that. Have an out of control mind.
It is lovely to know that what we shared has sparked of positive thoughts for you, and
you have a feeling of healing within your brain, by a process you can manage. I am
not able to do things like that, I guess we all find our own way: but how lovely that
we could reach out to each other, who knows how many miles away, and share our
suffering and our pain, and be able to say it without shame or paranoia. Not many
understand, one of the cruel side effect of this condition. My circumstances are
pretty difficult, so I think I manage as best I can. I would thank you for all the
contact, and what that I have felt recognised by your contact, just the fact that you
got me in the first post was amazing. Sending love……and wishes for the healing of
that fine brain you have.
I send love back to you Billie ♥️
I’m in the South West of Ireland. Even though we are geographically and physically distant (very important these days ?) we are connected in spirit and through the words that we use to express our thoughts and feelings.
I was thinking after our last exchange that I’m so grateful to be able to communicate, through Health Rising and the wonders of the internet.
I’m so sorry your circumstances are pretty difficult and you’re right, all we can do is the best we can. No one really knows what other people are going through…
Tracey, it makes sense….. you come from Ireland!!!!!! I have Irish blood in my veins
from my Mother’s side: (McCann and Darby) I don’t know where from, as haven’t done ancestry because of CFS/ME. But I am drawn to Ireland. I felt the connection as well, may a combination of shared suffering, and and Irish souls was what bought us together. I thank you for all that you have
given me, just by understanding, and coming together.
May the road rose up to meet you,
May the wind be ever at your back…….
Love Billie❤️
Does anyone know where to purchase intranasal gLutothione? finding oral sprays only.
I tried the intranasal glutathione for awhile but had a problem with one nares & med would not stay in. Saw ENT & had to have surgery. Now that is done, I want to give it another try. I will say that even though only one nares was absorbing it, I still did improve somewhat. I am anxious to see what it will do with both nostrils working!!! Thanks for the reminder that we do have hope. Theresa Dowell is the one who prescribed it for me, as well as LDN, which I still take. I am so thankful to find her as she is the closest practitioner to me who will see ME/CFS clients.
I wonder if this might help my constant head pressure? Cort, is there a doctor in Las Vegas who might prescribe this?
Not that I know of but we will be presenting something soon that might help with that. If you can get to Flagstaff Theresa Dowell is there!
The results of my liver function tests have shown over many years : “Low glutathionation”. Is this a problem with the liver not producing enough glutathione, or are we producing so many free radicals that our glutathionation can’t keep up with them?
Interresting study, I wonder is there some information somewhere that , for example liposomal glutathion which passes the BBB, has a major effect on ME/CVS?
I wish there were studies on this. One would certainly think it has the potential of helping. I don’t have any data – anecdotal or otherwise on it.
Carnosine has been of help to me on so many levels. It is mentioned in Corts article here. It can up the glutathione levels in the brain as it will cross the BBB. It helps with reperfusion issues, can take down acetaldehyde, and help tamper down ROS.
https://www.ahajournals.org/doi/full/10.1161/STROKEAHA.107.488502
Our results show that carnosine not only preserved brain levels of the reduced form of glutathione, a crucial endogenous antioxidant, but also significantly reduced the number of ROS-positive cells in the infarct area. Preservation of glutathione levels by carnosine might be due to a reduced oxidation of glutathione in response to the carnosine-induced decrease in free radicals or to an increased expression of its synthesizing enzymes. As a whole, these data suggest that the neuroprotective effects of carnosine after focal ischemia may be mediated in part through its known antioxidant properties.
Thank you Issie. You always have great suggestions.
https://www.healthrising.org/forums/threads/mast-cell-histamine-immunotherapy-with-histamine.6233/page-2
I just added some more info to another blog on carnosine. You may find it of interest too.
Gracias Cort y Health Rising por publicar los tan interesantes estudios que nos ayudan a llevarlo mejor y un abrazo para l@s comentaristas que aún estando mal tienen un ratito para comentar y para esbozar una sonrisa
One person emailed in:
“Just wanted to say that years ago my daughter found she felt better nebulizing glutathione. She overdid it and started reacting to it so that she could not continue taking it. maybe it was an allergy. i recommend people watch the doses of glutathione they take or they may not be able to take it at all after a while.”
Maybe not intranasal, because chemical intolerance is a significant part of CFS.
Intranasal collodial silver and EDTA has successfully treated chronic sinus problems I have had. It is compounded by Hopkinton Drugs but you need a script. google.com/search?q=hopkinton+drug+now+has+edta%2Fsilver+nasal+spray&rlz=1C1CHBF_enUS819US819&oq=Hop&aqs=chrome.1.69i57j35i39l2j0j69i60j69i65l3.8332j0j7&sourceid=chrome&ie=UTF-8
We are discussing intranasal glutathione with our PCP, and she is open-minded about considering it. When I called Key Pharmacy, I found a very patient and helpful pharmacist who described several of the various forms and strengths that they regularly compound. Since our PCP has never prescribed intranasaI glutathione, is there any more specificity you can provide as to the actual prescription that Dr. Klimas has found effective? They have various strengths and delivery mechanisms. It would be most helpful to know what we are specifically requesting our PCP to consider. Lastly, does Dr. Klimas start a patient off at full dosage or ramp it up over time. Anything that can improve cognition and energy by 20% sounds miraculous to my wife who has tried so many things over 20 years.
Hi John,
Here is what I got from Theresa Dowell. (Contacting the Key Compounding Pharmacy in Seattle and asking them might work too.) I don’t know how low of a dose Theresa starts at.
She prescribes compounded intranasal glutathione, 250 mg/ml, two sprays in each nostril three times per day. (Dr. Klimas uses the Key Compounding Pharmacy in Seattle). For patients who have trouble breaking down sulfur metabolites, Theresa starts them on a very low dose and slowly work up to 200 mg per day – about a third of the dose used in the Parkinson’s study.
My doc prescribed intranasal glutathione and I used it for several months without any noticeable benefit. Compounded meds can get so expensive & I just didn’t want to keep spending the $$. BTW- it REEKS of rotten eggs and will just about make you gag. Just be forewarned if you try it.
Soooooooooooooooo many USA doctors trying to cure ME/CFS. Has anyone actually recovered and if so, was it due to them or just that your body recovered? I am sure if a sick person with ME/CFS could be treated with a drug, they would instantly feel much better. I tried IV glutathione once but I have no idea if it did anything. How could I possibly calculate what an antioxidant is doing? Remember, so far, no one in the world knows what causes ME/CFS to carry on and on and on and on.
Actually quite a few recovery stories exist. While they’re not that common people recovery in all sorts of ways. I have, I think, about 7 or 8 stories that have come in in the past half year or so that I need to add to the recovery stories part of the website –
https://www.healthrising.org/forums/resources/categories/recovery-recovering-stories-click-to-see-categories.123/
Martin, I appreciated your comment. Yes, even though I don’t like pharmaceutical
drugs, I would take it if it cured me afater 22 years of CFS/ME. The mystery illness
that is brutal with some, and a little kinder to others. I am in Australia and checked
on the availability of intranasal glutathione (I take compounded capsules$$$$), and
it was way out of my range, and required doctor’s script. I don’t know a doc who
would know what it was about, or be willing to know, so your words helped.
I almost got better in 2003, then there things happened to my body, and I “crashed”.
The doc at that time had it at the time herself, but as she said not with the head
problems, which I had big time. She put me on on Rivotril a drug for epileptics to
was the short circuits I was having in my brain (inflammation on the nerve endings of the brain)… it slowly helped, and I have been taking it for more than a decade in
small doses, only pharmaceutical I take. She also treated me with homeopathic and
a huge list of natural supplements. Then I couldn’t afford to see her. Now I am on compounded natural supplements for the methylation cycle of the brain, (zinc/copper balance) and I think this has helped me through, but, in saying so, it all depends on what happens in your life, emotionally, financially, physically (accidental injury – any extra stress on the body, and you are gone again. On and on and On, a great way of expressing it….. mine is one step forward, three steps back. Maybe we should become CFS/ME song writers. Wishing you some relief and a miracle. Billie
i test low on glutathione. I have tried it in different forms and have not tolerated it-that is the problem with raising it.
Jeanne, perhaps the precursors of glutathione would be better for you….NAC, GLYCINE AND GLUTAMINE. Someone would have to prescribe dosages. Oh, plus some Vit C
Good luck
I take reduced Glutathione and tolerate it just fine. No adverse side effects that Im aware of. I take it along with ALA first thing in the morning and an hour before I start “popping” my 16 other pills (mostly methylated B vitamins, l-carnitine, quercetin, turmeric, fish oil, and Parasym Plus (PP). The L-carnitine and PP supplement has the biggest effect on my cognitive functioning, fatigue and muscle functioning. I’d like to try the Carnosine but it’s already tough just getting through all these pills every morning.
https://www.sciencedirect.com/science/article/pii/S2352340919314490?via%3Dihub
I guess intranasal glutathione is intolerable for a lot of people or it would have caught on more. The price is also prohibitive.
~
If BBB permeability is an issue in ME/CFS, then perhaps getting drugs past the BBB is not as much of a difficulty?
~
GlyNAC seems to raise glutathione in trials with healthy participants – though I would caution that glycine can be excitotoxic in some contexts (high homocysteine)& oral glycine can spike CSF glycine in some people. Serine might have different kinetics – as with everything else, there needs to be more research.
Intranasal treatment for brain fog