

Dominic reports on the new Phelix bacteriophage Lyme test his wife with ME/CFS tested positive on.
Possible new “break-through” blood test for Lyme and other tick-borne diseases
Summary:
- A new type of blood test for tick-borne bacterial infections became available in September 2019: the Phelix Phage Test.
- The test looks for “phages” to confirm the presence of host borrelia infections that are otherwise invisible to antibody or PCR tests.
- Test results validated treating a long-term, very severe ME/CFS patient for a tick-borne bacterial infection.
My wife has been ill for over seven years. She has done countless urine, feces, blood, breath, hair and saliva tests – effectively every available type of laboratory test across two continents. This included tests for Lyme and other tick-borne diseases with a specialist laboratory in the United States (ELISA, Western Blot, PCR, etc.).
Her test results have shown some abnormalities (e.g., gut dysbiosis, abnormal metabolites, poor mitochondrial function, adrenal insufficiency, impaired T4 to T3 conversion, etc.), but never a pathogen. Like so many people with ME/CFS, she has a complex illness without a clear origin – if only she had an identifiable “bad bug” to explain it all!
In March, my wife tried a newly developed blood test for bacteria of the borellia genus by Phelix. The result was *positive* for Borrellia miyamotoi (one of many “cousins” of Borellia burgdorfi, the well-known bacteria that causes Lyme disease).
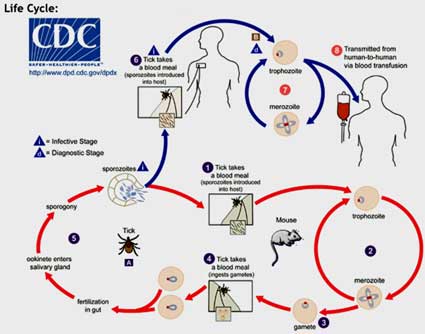
Borrelia life cycle (from the CDC).
B. miyamotoi was first identified in Japan in 1994, and is now known to be present in ticks with ranges across Russia, Europe, and the west and east coasts and the midwestern U.S.
It’s spread by the same ticks (blacklegged or “deer” tick (Ixodes scapularis), Western blacklegged tick (Ixodes pacificus)) as B. burgdorfii, but is more closely related to to the bacteria that cause tickborne relapsing fever (TBRF). It rarely causes the distinctive erythema migrans or bulls eye rash that sometimes occurs in Lyme disease. Both bacteria typically produce fever, chills, headache, fatigue, body and joint pain, nausea etc.
Her doctor indicated that this pathogen could explain her very severe ME/CFS symptoms. We could hardly believe it!
The symptoms caused by tick-borne bacteria are varied: they “mimic” other diseases and can resemble ME/CFS or fibromyalgia — leading to questions over whether they are (at least in part) the same.
Since receiving the results, I’ve been reading about tick-borne diseases and the unfortunate experiences of patients trying to get diagnosed and treated. I have learned that the new blood test is a break-through for the tick-borne illness community – and may also be a break-through for some ME/CFS patients.
Why is this new blood test possibly a break-through?
Blood tests for tick-borne bacteria were (until now) unreliable. Indeed, conventional tests for tick-borne diseases – based on serological antibody measurements – may fail for patients who not produce detectable levels of antibodies in response to the infection. In addition, tests relying on the detection of bacterial DNA (i.e., PCR tests), may also return “negative” results because the bacterial DNA is not always present in blood samples. In sum: the previously existing tests have a high rate of “false negatives.”
Consequently, patients who have a tick-borne bacterial infection may not be diagnosed or get treatment. The US Department of Health and Human Services’ own Report to Congress from November 2018 serves as federally mandated “wake-up” call to the problem of vastly under-reported tick-borne diseases in the United States.

Phelix labs in France developed the test.
Moreover, those patients who were “lucky” enough to be diagnosed and treated for a tick-borne illness are sometimes (mistakenly) pronounced “pathogen free” based on “negative” post-treatment blood tests — despite still presenting symptoms. The medical community has been perplexed by the persistence of symptoms even after weeks of antibiotic treatment in a subset of patients – termed “Post-Treatment Lyme Disease Syndrome (PTLDS).”
“Lyme Literate Medical Doctors” (LLMDs) have for years been arguing that PTLDS patients are likely not pathogen free, but rather that blood tests fail to record “persistent” pathogens (see the book by Dr Richard Horowitz). Recent research on mice has indeed found evidence that tick-borne bacteria can persist even after weeks of heavy antibiotic treatment because they are protected by impenetrable “biofilms” and “cyst” formations. The new blood tests may prove the LLMDs right and validate continued antibiotic treatment of PTLDS patients.
So how does the new blood test work?
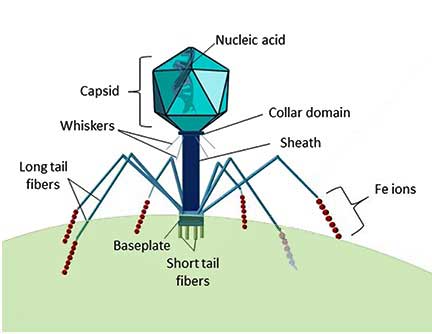
The structure of a Myoviridae bacteriophage.
The new blood test does not test for the DNA of the tick-borne bacteria (which is not always present or very diluted in blood and thus easy to miss), but rather for the DNA of “phages”, which are simple life forms that live off of bacteria. Importantly, phages are tens to hundreds of times more common than the host bacteria and are specific to their hosts – which means that the presence of a certain type of phage DNA in your blood sample tells you which bacteria you have!
Another significant advantage to testing for phages (as opposed to antibodies) is that the presence of phages confirms that the bacteria are still present – antibodies don’t distinguish between current or past infection.
The phage-based test can currently only detect bacteria of the genus borellia. Its originators – researchers at Phelix R&D and the University of Leicester – are now busy expanding the test to other tick-borne bacterial genuses (e.g., babesia and bartonella). Phelix asserts their new phage-based PCR test is 50% more sensitive than other tests used.
Unfortunately, it is very difficult to rid a body of tick-borne bacteria: patients describe months and years of grueling IV and oral antibiotic treatments. Yet we are encouraged by recent trials that have had positive results on defeating “persistent” bacteria based on off-label uses of existing drugs (c.f. dapsone and disulfiram).
After years of searching, I am hopeful that this is a big step towards understanding and solving my wife’s very severe ME/CFS. I suspect that phage-based tests may also reveal hidden pathogens in many other ME/CFS patients.
Stay safe!






Been tested positive for lyme a couple years ago in a private clinic. Test from Germany. Chronic -got bit 35 years ago. I have ME/CFS and POTS. antivirals used for Lyme made me worse. Cleared mold first. Nothing has helped. Now what?
Stay tuned and check out this blog – http://simmaronresearch.com/2019/10/better-lyme-diagnostic-nih-strategic-plan/
It looks like the NIH – thanks to strong advocacy efforts – is finally going to spend some real money on Lyme.
Try Supportive Oligonucleutide Therapy. Or a Doug Coil Machine ir Disulfiram or azoillicin
How will this be treated any differently? Millions of people have been treated with all kinds of drugs to “ kill” off the bad bacteria. When the medical community understands it’s the host terrain that’s damaged and opportunistic pathogens are over taking the immune system. Until we have proven medical procedures that detoxify environmental toxins and support cell regeneration, all these chronic illnesses will continue to exist. It’s not working the way conventional medicine approaches these types of illnesses.
Have you considered disulfiram? Lots of Lyme patients are finding success on it. Not necessarily an easy treatment, but it can be very effective and lead to people getting their lives back. There is a FB group called Disulfiram for Lyme.
Lyme isn’t a virus, it’s bacterial, so needs antibiotics….
Thanks for sharing! Has your wife tried antibiotic therapy already? I tried for one year month working with two Lyme literate doctors, and all that resulted was to be made me more sick than before, plus I gained 35 pounds because one of the antibiotics required high fat intake. It was also hell, as I couldn’t tell herxing from side effects.
I do so hope this test allows your wife to be healed, and better treatment developed. At present, I’m loathe to lose another year of my life to antibiotics. But I wish you success.
We definitely need better treatments and more clarity on testing. According to this website -https://www.lymedisease.org/the-fda-and-lyme-disease-testing-fda-is-listening-but-does-it-matter/ there are no FDA approved tests. Hopefully new funding for Lyme disease at the NIH will help. I don’t know much about them but there’s also some talk of using bacteriophages as treatments. Hopefully someone will know more.
Hi Cort, have you seen this information from the Netherlands? Amsterdam UMC https://www.amc.nl//web/mijn-afspraak/mijn-afspraak-in-het-amc/b.-miyamotoi-en-de-fagentest-.htm
Yes, I agree antibiotics will never fix these chronic infections. Only rebuilding the immune system and supporting the body will help heal.
Hello. Yes, I read that Antibiotics have often not (sufficiently) helped in recovery from tick-borne illnesses. The bacteria persist. We are hoping that Disulfiram will root out the borellia (after an initial antibiotic treatment to bring the Bacterial load down). Disulfiram is an enzyme inhibitor (not an antibiotic). That’s what the Dr told us anyway!
There’s a team studying the application of Disulfiram for Lyme disease at Columbia University. Best wishes! D
I am a retired RN who has had FMS/CFS for 40 years. My own theory about the disease is that antibiotics contribute to the disease by altering the gut biome, which in turn alters the brain. This certainly ties in with Cort’s recent article about hypothalamus dysfunction. I theorize that fecal transplants from healthy people might end up being a cure, once necessary antibiotic treatment was finished.
Fecal transplants are soooo interesting. A Norwegian group, I think it is, is examining them now, and a UK study went well.
https://www.healthrising.org/blog/2019/08/24/chronic-fatigue-fecal-transplant-study-positive-results/
If you need support while she is on disulfiram, you might join the FB group Disulfiram for Lyme. There is a lot of helpful information in the files on supplements and diet, as well as some interesting threads on dosages and herxes. There are other FB groups, too.
Thank you Marguerite. She has not started treatment yet. We are also nervous about the antibiotics… Best wishes! Dominic
I took the phage borrelia test last year after 15 years of ME. It was positive for borrelia but I chose to treat with ozone rather than antibiotics. I am much improved thanks to this test.
Would you share which route of administration of ozone helped you improve
10 pass ozone therapy weekly with Frank Shallenberger md.
Yes it cannot multiple in a high oxygen environment. Hyperbaric oxygen fixed limes in my daughter but the sooner the treatment is used the better. She had hyperbaric every day for two weeks in the mornings followed by IV vit C to treat the free radicals this created. Worked for her
I have been begging for this treatment as my wbc count, sed, crp eludes them. My spouse read the description from a punk rocker and turned to me and said you have had Lyme for 20 years! We were avid campers and hikers.
Phillida, I’m so happy to see someone else who witnessed success with hyperbaric oxygen therapy.
I had great success with it after having Me/cfs for twenty years.
I had seen doctors and tried so many things, always with such a lack of support from family or the medical community. I logged 90 hours of oxygen therapy and was amazed how much better I was!
I’m 70 years old now and housebound by this illness, but hyperbaric oxygen therapy helped so much! If it had not broken my bank account I would have continued as needed.
Something to think about.
Why did it help so much?
Interesting. thank you for the info, Carol. Best wishes! Dominic
Hello Carol Perry is it possible that we exchange the test outside of PR I am not used to PR, by email is it possible?
This is exciting information. I’d love to take this test. Does anyone know of U.S. doctors who will request the lab for it?
Hi. I suggest to call the lab in Nevada – they should be able to tell you who prescribes the test. I also heard you don’t need a prescription to do it. Best wishes! D
Thank you for the article Dominic! I hope your wife finds answers & wellness in her medical journey. I know Lyme and tick-borne diseases have long been suspected in a subset of ME/CFS sufferers.
One question: “her doctor indicated that this pathogen could explain her very severe ME/CFS symptoms” – do you mind if I ask if your wife sees an one of the handful ME/CFS specialists in the country? Just was curious.
Hi Dakota. I sent you a PM with the Dr’s name. Best wishes! Dominic
GREAT!!!!! Glad science is starting to be able to detect more. I sure hope this works for her. I had a LLD doc who is a bioscientist and who could recognize symptoms even with negetative results. He was of the opinion that there are many things that can’t be detected by science just yet. But if symptoms fit, see if the “fix” makes a difference. But I came back positive with coinfections of other pathogens and had the red ring rash. But despite years of low dose antibiotics and many other herbal treatments, it still seems present with flares at times. What they call Post Lyme disease. I’m using an antiviral for this now, called Lomatium. It has helped somewhat in getting over this. I’m supposed to use it for 18 months. It’s been about 6 now. I stopped to just see what would happen, and it’s still there.
Also there is a fungus gotten from mosquitoes that can mimic Lyme and sets up biofilms and gets into blood and organs. It can form tumors too. It’s called Funneliformis mosseae. Unfortunately, I have both. And the treatment for that is different.
https://www.sciencedirect.com/science/article/pii/S2452231718300083
The most frequently observed eukaryotic DNA was for Funneliformis mosseae, an arbuscular mycorrhizal fungus, which was in both ME/CFS and normal control samples.
Herbals worked better for me than the antibiotics. (Though we did those first.) I found Coptis to be helpful and Serrapeptase. Green leaf stevia is said to help too. We mostly used herbs that Buhner protocol recommended. But have since learned that those doing the kits from Cowden seem to have better, long lasting response. He has several packages and it goes in steps. I know a guy who thought he had ME and he got treated in Mexico with a retreat atmosphere and heat treatments and then went on the Cowden protocol and is doing much better. Saunas are helpful too.
Dear Issie. Thanks for all the info. Also on the herbals… I will look into this more too. Best wishes! Dominic
I would like to know the name and location of the treatment center in Mexico. Could you mention that here please. Thanks!
Issie – seriously! I asked multiple ID doctors if I could have anything from the
mosquitos after living in the everglades for
3 years!
answer — NOPE!
and no tests just unbelievable
If this test really was a possible new “break-through” then the article would refer to scientific papers demonstrating its accuracy. Instead, it links to the website of a commercial lab that has sold unreliable tests before.
With all the respect to the author of this article but I don’t think this is the way forward. ME/CFS patients don’t need unvalidated tests or speculative diagnoses, but more and better science.
Thanks for writng this! It put things in perspectif for me. I looked it up: redlabs 🙁 I know it to well! unlucky me and the treatment to… in 2001. indeed no solid tests and big big scandal years and years later in my country!!!
every patient with every desease diserves reliable approved tests! and even those can have fals positivs or negativs. But at least you get the best chance.
it says Phelix and university of Leicester developed the test. Redlabs was chosen by them to use it. So it’s not a ‘redlabs test’ if I understand correctly.
Bacteriophages have been known in Russia & ‘behind the (former) iron curtain’ for decades to treat disease bc of lack of ABx. It makes sense to go look for the phages instead of their targeted Borrelia‘s which hide in biofilms and tissue.
Phage testing is not ‘new’ if you read the literature (veterinary sources too). The difficulty of phage tests is mainly linking which phage targets which bacteria, since there is an abundance of bacteria to look for and so an abundance of phages that are linked to these specific bacteria.
Finding which phage to look for is the reason why they call it a ‘new test’. They found the phages for a limited amount of Borrelia species.
Ps: miyamotoi is called a ‘Borrelia’ but resembles much more a relapsing fever spirochetes.
It does not belong to the Borrelia sensu lato family. It gives a flulike illness & differs from ‘Lyme disease’ as most know it.
Me too, I was first cautious when I first heard about this test and after reading some bad press I found about RED Labs on the Internet. So I ran my own investigations. I found that the bad press was linked to RED Labs planning to propose a test to detect a XMRV virus following the publication of scientific paper in one of most prestigious journals – NATURE. However it turned out that the reported “findings” in that paper were actually just an artefact. Also as a consequence of this “affair” the complete staff and management have changed.
I have also contacted the Chief Science Officer at RED and Phelix requesting scientific evidence backing up the Phage Test. I have been told that as it is ongoing a patent application, they cannot publish scientific articles at the same time. They will do so when the patent is granted.
So I decided to trust them. My family (My autistic child, my wife and I) took the Phage Test as well as some others. We managed to diagnosed for all of us an active Borrelia Miyamotoi infection, an intestinal dysbiosis, gastrointestinal permeability, and a lot of immune disorders including a dysregulated serotonin pathway.
We are now undergoing the right treatments which have a great impact, especially for my daughter. Believe it or not but a lot of her autistic symptoms are improving.
Dear Ghostseb. I am glad to hear that your family members are experiencing improvements. You are a few steps ahead of us (my wife has not started the treatment for borrelia miyamotoi yet). I am curious to know what treatments your daughter is undergoing. Best wishes! Dominic
@ghostseb, what are you doing for it? And how is the serotonin pathway affected? Downregulated or upregulated???? Throwing balance off????
The test has not been validated in a scientific journal and I was concerned about this as well. Martynas asked some Johns Hopkins researchers about it, though, and they thought it made sense and had promise.
Hi Michiel, a disappointment again for all the patients Amsterdam UMC https://www.amc.nl//web/mijn-afspraak/mijn-afspraak-in-het-amc/b.-miyamotoi-en-de-fagentest-.htm
Is anyone with positive antibodies for tbd also on IGg infusions? I have been tested by igenex, which was very expensive, and shows I am positive for some tickborne disease. However, I know these results can be effected by my Igg infusions I have been on for six years. Also, I am negative for all tbd when I have taken all other blood testS besides Igenex.
@Jessica, since no one is answering….I can’t speak personally, but I have a POTS friend who kept testing for Lyme before IVIG and was always negative. Then after awhile on IVIG, she showed up positive. There is debate as to whether Lyme can be passed with blood, or other bodily fluids. Also question if it could be in antibodies as that is from 100s of people. The question is, was it already there and then with better autoimmune response it starts to show up. Or was it gotten from IVIG and others mixed antibodies? (IVIG carries the same warnings as a blood transfusion. ) My friend thinks it was there and the more antibodies made it present itself. But I tend to lean the other way. So it still needs to be determined, as far as I’m concerned. (Just my opinion. And though I qualify for IVIG, as I have Hypogammaglobulinemia, I chose to not take that chance.) So far, I’m still okay and have not regretted my decision. (Though Mayo made me sign a paper that they had told me pneumonia likely would kill me and they had warned me and I refused IVIG.) And if I can make it to age 60 and still have a bit of quality to life…..that’s pretty good, I think.
Thanks for responding I’m just seeing this. You can’t get lymes from infusions or Epstein bar or any of those other viruses. You can only get the antibodies which means you when you test your immune system against any of the viruses it’s hard to know if they are your own. The only way really know is to stop the infusions for four months and then test but I can’t risk it. My infusions have not helped with fatigue or pain put has helped prevent me from getting infections greatly! The blood is screened for all bacteria and viruses these days so you should never get an infection from igg only antibodies.
Been tested and they fois Bartolena cells. Took antibiotics ext’rememy strong which caused me a huge herpes crisis in the mouth and outside, took 2 months to comme back with a healthY mouth. Plus, I should have taken the antibiotics for 5 weeks and I took it only 4 weeks, the doctor didn’t advise me for the 5 weeks. I might have to redo the trAitment. Plus, an internist-rhymatologist found me a collageneous illness but because of the Coviv I couldn’t pass my blood tests, which would have indicated from which one I’m suffering. Now, I have to take amphetamines if I want to get out of bed and do things. But, I still have big crashes the day after because I do to much on amphetamine. I’m really fed up, only on amphetamine I can feel in a beTter mood.
Dear Agnes. Yes. We are also concerned about the antibiotics to treat the borellia… not sure what to do. Best wishes! Dominic
I am so sorry Agnes. Our bodies eventually become so worn down from this complicated and extremely complex disease.
I’ve found little to help except with hyperbaric oxygen and that was for symptoms only. I too take methylphenidate, to allow me to get out of bed.
Do not loose hope my dear, there are so many brilliant researchers and biochemists searching for answers.
When I’m low on hope I read the articles that Cort has applied his editing expertise to bring to this website he created.
Cort you are a hero to many of us, I find hours of exciting articles leading to more articles to expand my knowledge.
Thank you immensely.
Best wishes to all of you searching for treatments, Dominic best of luck with your wife’s illness!
Will Medicare pay for this test? I’ve been told I’m negative for Lyme disease but I’ve been bitten by ticks three times in different states. I would love to have this test
The test is not coverage by insurance and is 360.00 USD .You do not need a doctor to order the test, just contact Redlabs.
Thank you Cort for keeping us apprised. We never know what might be the helpful link for improvement. Everyone responds differently. Both myself and my daughter share very similar traits in our illnesses (POTS,EDS, ME/CFS) but she is much worse off than I am. Makes me think there is a genetic factor for us or the possibility that I passed it on to her via blood, etc. I have never found much about this in my years of searching. Does anyone think it is possible to pass on a tick-borne disease? We both had parallel symptoms when we were adolescents so perhaps passed on by mother or we just inherited weak systems that are triggered easily for these illnesses. I would love to hear opinions.
I’ve never heard that tick-borne illnesses can be passed on by casual contact. I think they have to be passed via the blood. Is it possible, though, that you were both bitten by ticks?
I found this interview. I had read that Lyme could be passed from mother to unborn child. There was also question of breast milk. And they have found it in vaginal fluid and male fluids too, so they question if sex can pass it.
https://www.gordonmedical.com/pregnancy-and-human-transmission-of-lyme-disease/
Most of the more current info I looked at feels there needs to be an open cut for it to be passed. But, back when I first learned it was an issue for me…..they thought it could be passed.
Those of us with wonky autoimmune systems, seem to be the ones that it will hide from. As it can morph into 3 stages and lie dormant and then reemerge if conditions are right for it. It and its coinfection are hard to get rid of.
There are only two small studies from the 90s (as far as I know) which found that Borrelia went through Placenta in 40% of cases when there was an active infection during pregnancy.
Does anyone know if Myamotoi is also involved in the Alpha-Gal Meat Allergy & if Yes have they tried the SAAT Alpha-Gal Remission methods yet used by this Facebook
Group? I just shared this post on the Group on Facebook to see their response. I know the SAAT procedure only costs $250.00 to have the items put in the ears & are putting
people into complete remissions without drugs a lot have their lives back now & also back to eating foods with no bad reactions or allergies
@Chfrazzle, it is in my family too. My maternal grandmother had POTS and EDS, my mom had MCAS, my sister has OI and CFS, her twins have POTS, daughter EDS, I have ME, POTS, EDS, MCAS and more. So yes it can definitely be in the genetics. And my sister and I was in the family genetic study with the Lights in Utah. We both have genetic mutations that can play into ME/CFS, and these other illnesses. My Mitochondria was not functioning properly on any of the 5 Factors checked.
As for Lyme and coinfection and possibly this other fungus, I have been told it can be passed in pregnancy. But they could not prove that it was passed later on. (At least that is what my doc said, especially for the fungus. He checked spouses of those with it and found a few with it, but no symptoms. But mostly found them without it.) So a lot depends on the immune system and how well it works.
But genetically, the dysfunction in families can be passed on. And the future generations possibly worse. I have had most of this as a child. And both my sister and my ME/CFS, started after a vaccine and horrible illness that followed, when I was around 8 years old. So this has been a lifelong journey for us. Still around and actually making some improvements.
My Lyme was not treated until years later and that’s probably why I fall into the Post Lyme catagory. Early treatment has better outcome.
There is also CIRS in our family and that has a genetic component too.
Thank you very much for the info about your family. At least I feel some confirmation and have something of substance for my theory. Don’t know how it’s helpful at this point. Do you know if any of the test results were published?
They didn’t publish our patient results, but confirmed what they were looking into with mitrochondria and also some genetics in families. Dr. LIGHT did a speech about the results. But we were given numbers. We however, did get our own results. It was really enlightening. I’ll look for the link when he spoke at Stanford.
https://www.youtube.com/watch?v=xDQL7v4XlRU
This study was on ME/CFS in families. Looking for genetic components and mitrochondria issues.
Hi Issie. I agree with Chris and want to thank you for your ongoing generosity in sharing information with your fellow patients. Gosh 52 years of ME/CFS is a long time to be sick. I first got sick at 18 after a glandular fever type virus and have been sick for 26 years now but often wonder if it is genetic and if I have actually been sick my whole life. I was fit as a child as I did gymnastics but I did get sick a lot with anything going and was allergic to basically everything on the RAST test. Like you I share symptoms of hyperadrenergic POTS and MCAS but those issues are more mild for me than the PEM. Maybe this is just chance but some members of my family also have signs of EDS (including freaky knees that go backwards) and a friend of mine with EDS has a father with ME/CFS. I also appear to have some methylation issues but have never been genetically tested. Fingers crossed for answers one day and, Dominic, good luck to your wife. All the best
Thank you Debsw!
@debsw, I hope what I share helps. Also hope we find more of our WHYs.
I’m encouraged of my progress over the last year. Dejurgen and I are making discoveries and finding some things to do about it. I hope others are seeing what he is sharing, as we are starting to bring more out. We are still experimenting on ourselves. But I’m really encouraged. We are in search for our “purple bandaids”.
It is a long time to be living in such a dysfunctional body. But I have learned so much from observing it. I hope it will one day benefit others.
And yes, I feel much of what we face has a genetic component and a dysfunctional autoimmune systems and inflammation.
I have some really wonky methylation mutations. 23&me is one good place to have genetics checked. I just recently signed up with Selfhacked and put my 23&me in. I am getting so much from what I’m learning there. I’m really glad I did it. He has a genetic test too and it is supposed to give more snps. But I already had 23&me, and am getting good info from it.
One huge word of advice is……find an hour of joy every day. If nothing more than staring out the window making animal shapes from the clouds. Or watch the butterflies flutter, or listen to the birds singing. Surround yourself with nature and let it embrace you. But find that hour of joy. And if you get more…..yayyyyyy! Good going! Hang in there ALL……we are finding “purple bandaids”!
Will Medicare pay for this test? If not what is the cost? I’ve been told I’m negative for Lyme disease but I’ve been bitten by ticks three times in different states. I’ve also suffered from CFS and fibromyalgia. I’ve had recurring infections of pseudomonas staph strep stenotrophomonas e-coli c-diff etc etc. I would love to have this test my mom. I’ve been waiting for it to come to the US. Does anyone know who’s doing this testing in the United States?
Jane, get back to me , please…I am from Stamford and remember you…I , also. may be able to help you with this ironically…
This is not my area as I don’t think I have Lyme disease but I’ve been interested in Jay Davidson’s ideas over the years and wondered whether others are aware of his work?
His wife was very unwell too.
Dear Tracey. I don’t know about Jay Davidson’s work. I just now read up online about his 5 Steps to Restoring Health Protocol. But there’s not much information on the specifics. I might get his book on audible… Best wishes! Dominic
Hello. If people do not have an infection or anemia, is ME just misdiagnosed hypothyroidism? The TSH tests could be a load of hogwash see according to the late Dr Skinner but the college of endocrinologists told him to get lost.
Have any bedbound CFS peeps taken thyroxine in a great anough amount for a long enough time?
Hello Martin, Thanks for your comment. I think you might be interested in a previous post as well: Pure T3 Thyroid and Stories of recovery from ME/CFS and FMS.
I have found out that it is a T4 to T3 conversion problem which is why the TSH in ME/CFS is always in the normal range. Dr SKinner was telling everyone with ME/CFS about this years ago but the endocrinologists just told him to shut the F up.
Hello Martin, Thanks for your comment. I think you might be interested in a previous post as well: Pure T3 Thyroid and Stories of recovery from ME/CFS and FMS.. Best wishes! Dominic
I had/have this issue. They call it Wilson Syndrome. About 20 years ago I did the protocol to try to reset that. It did not work. I never could get my body temperature up to the desired temperature. And the medicine is really hard on you as it increases heart rate considerably and caused a lot of anxiety. You titrate T3 up trying to increase body temperature. I couldn’t get it to work. It’s a problem with Reverse T3.
Wow – this is good news. I’ve beed tested many times for Lyme but not with this test, and of course there were no positives. I’ve often wondered if Hisoplasmosis could have caused problems for me. I had it really bad many years ago and I was never the same after that. I got RA, fibro and ME/CFS after being very healthy. I haven’t run across any doctors who will even think about my question. Anybody here ever heard anything like this?
Would this test detect any strain of Lyme?
https://biologixcenter.com/phages/new-lyme-phage-treatment-may-eliminate-borrelia-in-two-weeks/
Dear Dr Hooper, Thank you for the info on the “Induced Native Phage Therapy (INPT).” First I heard of it and sounds very interesting! Do you know of anyone offering this treatment in Europe? Thanks and best! Dominic
So interesting and I appreciate this article. I just came across it, surprisingly. I have been suffering with ME/CFS for 16+ years. This March I was confirmed to have B.Miyamotoi via the phage testing. Looking into this bacteria, many of my neurological symptoms now make sense. This is a very aggressive bacteria. As my symptoms are increasing, I’m looking into many treatment options. I just wish testing and treatment was more affordable, easier to access, and that it actually worked. Thank you, Dominic, for writing this article.
Thank you Lisa! We’re in the same place: researching about treatment and wishing it would be accessible and work! Good luck! Best wishes! D
Hi Dominic, how is your wife doing? Have you seen this information? Amsterdam UMC https://www.amc.nl//web/mijn-afspraak/mijn-afspraak-in-het-amc/b.-miyamotoi-en-de-fagentest-.htm
Dominic can I get you contact details please.
Regards
Jan
It’s been three years since this was published here….can anyone give an update about this test? Is it valid? Worth the expense?
Haven’t heard a thing unfortunately.
Hi i am from, Stamford CT originally any way to contact you? Long history