

The Scheibenbogen Effect
With the studies pouring out, it’s getting hard to keep up with Carmen Scheibenbogen and friends in Germany. Scheibenbogen has co-authored no less than five papers on chronic fatigue syndrome (ME/CFS) in 2020. With Klaus Wirth coming on board, the autoantibody testing lab there, and Scheibenbogen and company in a publishing frenzy, Germany – out of which virtually nothing on ME/CFS came for decades – has become quite a research hub.
The one constant in all of this appears to be Scheibenbogen, who has co-authored 17 papers on ME/CFS since she appeared on the scene in 2014. Such is the impact one dynamic researcher can have.
The hunt seems to be circling mainly around two factors: autoimmunity and the blood vessels. This study tackles one of the most intriguing possibilities in ME/CFS – impaired circulation. ME/CFS has been thought of as an immune disease, a hormonal disease, and a metabolic disorder, and indeed it seems to have aspects of all of these, but what about ME/CFS as a cardiovascular disorder? What quicker way to impair energy than to inhibit the flow of oxygen-rich blood through the small blood vessels?
The Study
ESC Heart Fail. 2020 Jun;7(3):1064-1071. doi: 10.1002/ehf2.12633. Epub 2020 Mar 10. Peripheral Endothelial Dysfunction in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. Nadja Scherbakov 1 2 3 4, Marvin Szklarski 5, Jelka Hartwig 5, Franziska Sotzny 5, Sebastian Lorenz 5, Antje Meyer 1 3 4, Patricia Grabowski 5, Wolfram Doehner 1 2 3 4, Carmen Scheibenbogen 1 5
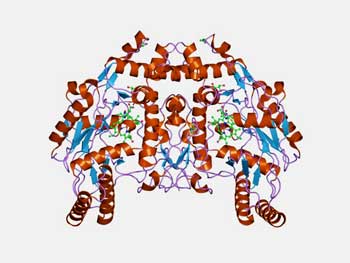
In this study, lead author Nadia Scherbakov, senior author Carmen Scheibenbogen, and other researchers focused on the thin line of endothelial cells that line the blood vessels and help to control whether they are open or constricted. They also produce immune and blood clotting factors.
First, they used a non-invasive technique called “Peripheral Arterial Tonometry (PAT)” to measure changes in the “vascular tone”. During the test a blood pressure cuff reduces blood flows to the hand for five minutes. After the cuff is opened the amount of blood flowing to the fingers is measured.
The EndoPat test, which can be done in a doctor’s office, can be used to quickly assess risk factors for cardiovascular diseases such as heart failure, stroke, and pulmonary arterial hypertension.
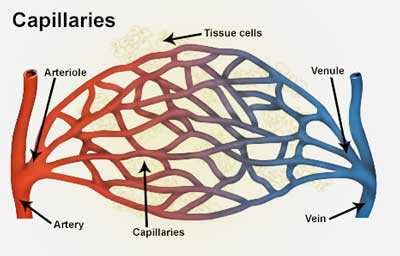
In contrast to other cardiovascular tests, PAT assesses microvascular functioning; i.e. the functioning of the peripheral arterioles found just before the capillaries. These arterioles, which are lined with smooth muscles, are where most of the blood flow regulation occurs. If not enough nitric oxide (NO), a vasodilatory substance, is produced, the arterioles will not be able to dilate enough to let sufficient amounts of blood through to the capillaries that transmit nutrients to the tissues.
The German researchers assessed something called reactive hyperemia, which occurs when the flow of blood through the veins gets blocked, lowering oxygen levels (producing ischemia) and causing a buildup of metabolic waste. The doctor in the video below reports that a result above 2.0 is normal.
The Gist
- Using a non-invasive approach (Endo-Pat) featuring a blood pressure cuff and a finger monitor, German researchers assessed the functioning of the small blood vessels called arterioles.
- The arterioles, which are located between the arteries and the capillaries, regulate blood flows by producing nitric oxide, a blood vessel dilator.
- The study assessed something called a “reactive hyperemia index” (RHI). An RHI below 2 is considered a cause for concern. It suggests that damage to the endothelial lining to the blood vessels has occurred, which is blocking the flow of blood. Endothelial dysfunction is often the first sign of cardiovascular disease.
- The small study found that about 50% of people with ME/CFS had low RHI’s. Attempts to find a metabolic or immune cause including B2 adrenergic antibodies were unsuccessful, however.
- A small substudy involving 6 patients with increased levels of B2 adrenergic antibodies, however, did find that immunoadsorption resolved the small blood vessel issues in 5 of them.
- Dr. Scheibenbogen reported that another small follow-up immunoadsorption study has produced similar results to the first one. (The first one produced excellent results in a subset of patients.)
- Three studies using the Endo-Pat technology have been done in ME/CFS – two have found endothelial dysfunction and one has not.
- Larger studies are needed to validate this study’s intriguing finding indicating that narrowed small blood vessels in large subset of people with ME/CFS may be reducing blood flows to the tissues.
- Other studies, but not all, have found reduced blood flows to the brain and/or muscles in ME/CFS. David Systrom’s large studies indicate that reduced oxygen delivery (i.e. energy) to the muscles is present in this disease.
- Systrom believes three factors – one of which involves the microcirculation – may be causing the oxygen delivery problem.
- As endothelial dysfunction is found in many diseases, it cannot by itself explain what’s causing the fatigue and exertion problems in ME/CFS. Wirth and Scheibenbogen have proposed impaired blood vessel functioning that results in dramatic increases in pain and fatigue producing vasodilators is present in ME/CFS. They are working on a second hypothesis they believe may explain the energetic problems in ME/CFS.
Results
The study, which used 35 people with ME/CFS and 20 (age and BMI-matched but not sedentary) healthy controls, found evidence of peripheral endothelial dysfunction in 51% of the ME/CFS patients. The endothelially challenged ME/CFS patients were functionally more limited and had more severe fatigue-related and immune-related symptoms (sore throat, painful lymph nodes) than the patients without apparent endothelial issues.
The researchers appear to have identified a sicker group with more endothelial issues. They were, unable, however – at least with regards to the lab tests – to determine why. Given the beta-adrenegic antibodies Scheibenbogen has found in other studies, one might have expected elevations to be present, but they weren’t. (Dr. Scheibenbogen suspects these antibodies only play a role in a subset of patients and other factors are likely also responsible for blood flow issues.)
None of the immune or metabolic markers (C‐reactive protein, albumin, hemoglobin, creatinine, aspartate transaminase, alanine transaminase, gamma-glutymytransferase, hemoglobin A1c, basal thyrotropin, immunoglobin A, G, M, IL-8, sIL-2, soluble V and ICAM, β2‐adrenergic receptor antibody, M3 acetylcholine receptor antibody) were either elevated or reduced in the patients with endothelial dysfunction.
But then came a clue. An immunoadsorption trial that attempted to rebalance their immune systems caused the endothelial problems to disappear in five of the six sicker patients.
Similar to plasmaphoresis, immunoadsorption is a blood purification technique which removes IgG autoantibodies and other pathogenic substances from the blood. It’s an expensive treatment (about $20,000) sometimes used in multiple sclerosis and other autoimmune diseases.
Every one of the six patients getting immunoadsorption had elevated levels of antibodies to the beta-adrenergic receptors found on the blood vessels (these receptors also play a key role in vasodilating the blood vessels). The immunoadsorption appeared to open their blood vessels – allowing blood to reach their tissues – and presumably reducing the hypoxia and metabolic wastes that were building up.
The authors didn’t say how much the health of these patients improved, but a study on the effects of immunoadsorption on ten ME/CFS patients found that 7 rapidly approved and three had moderate to marked improvements lasting 6-12 months. Much larger studies are needed, but the increase in endothelial functioning was promising, and the trial’s success suggested that a focus on the immune/cardiovascular interface made sense.
Conclusion
The idea of ME/CFS being a kind of cardiovascular disease affecting the small blood vessels seems to make perfect sense but has been surprisingly little explored. This appears to be the third time that PAT has been used in chronic fatigue syndrome (ME/CFS). Back in 2012, Newton did find evidence of endothelial dysfunction in ME/CFS, but in 2018, the Moneghetti /Montoya study, which matched ME/CFS patients to healthy sedentary controls, did not.
In contrast to the Montoya study, which used sedentary controls – and did not find diminished endothelial functioning in ME/CFS – this study did not use sedentary controls. The Scheibenbogen study did, however, appear to have a more endothelially challenged group, and perhaps a sicker group as well, as over 50% of their patients had a low reactive hyperemia index (RHI) (<1.81).
Montoya’s ME/CFS group, on the other hand, had a much higher average RHI of either 2.21 or 2.44 (the paper did not indicate which number referred to which group.) Montoya’s ME/CFS patients also had similar exercise results as the healthy controls.
While few studies have actually studied endothelial dysfunction in ME/CFS and FM, the idea that it may be present appears to fit well with what we know. Shungu’s brain lactate, Scheibenbogen’s mRNA findings, several, (but not all), brain blood studies suggest something may be wrong with blood delivery in ME/CFS.
Several, but not all, studies suggest that oxygen delivery to the muscles may also be impaired in ME/CFS. After earlier exercise studies suggested oxygen delivery issues were impairing energy production during exercise, Systrom’s more recent, and much larger, invasive exercise studies seem to have settled that issue: oxygen delivery is indeed an issue for a large subset of patients.
Similarly, Staud’s finding that greater cerebral blood flows and higher heart rate variability levels (lower sympathetic nervous system (SNS) activity) were associated with reduced fatigue in ME/CFS made perfect sense given the role the SNS plays in squeezing the blood vessels. Dr. Natelson has proposed that some of the cognitive symptoms in ME/CFS derive from an “episodic cerebral hypoxia“; i.e. episodic declines of blood delivery to the brain.
The possible presence of stagnant hypoxia in ME/CFS and POTS provides yet another clue that oxygen delivery in ME/CFS and related diseases may be a problem. Stagnant hypoxia occurs when the oxygen content of the blood is normal, but the blood is moving too slowly to deliver sufficient amounts of blood to the tissues.
Arterial stiffness – an expected outcome of endothelial dysfunction – was found in one ME/CFS study, but not in a pediatric one.
Finally, Wirth and Scheibenbogen’s recent hypothesis – that a breakdown between vasoconstrictor and vasodilator forces in the blood vessels results in a massive upregulation in pain-producing vasodilating substances – puts a new twist on the blood delivery issue in ME/CFS.
It’s not just ME/CFS, though. At least as early as 2006, researchers were suggesting that muscle ischemia caused by low blood flows could be contributing to the pain fibromyalgia (FM) patients experience. They asserted that next step was to determine what happens to capillary blood flows (i.e. the microcirculation) in FM during exercise.
While most studies are small, the possibility that small blood vessel oxygen delivery problems to the muscles and brains of people could be causing or contributing to ME/CFS, and perhaps FM, appears to be growing.
Cause?
What might be causing it is another matter. Factors like high blood pressure and high blood glucose have not been found in ME/CFS. High levels of lipoproteins, oxidative stress and inactivity have been.
Nitric oxide synthase – the study suggested that the small blood vessels in a significant subset of ME/CFS patients may not be producing enough NO.
Systrom proposed the oxygen delivery problem could be caused by mitochondrial issues, hyperventilation, and problems with the oxyhemoglobin dissociation curve – and/or microcirculatory problems. This small German study suggests microcirculatory problems and reduced nitric oxide production by the endothelial lining of small blood vessels (arterioles) may contribute to fatigue and other symptoms in about half of the ME/CFS study group.
Because endothelial dysfunction can occur in many diseases, if it’s present in ME/CFS other factors must come into play that produce fatigue, post-exertional problems, etc. (The “Blood Vessel Crunch” describes a blood vessel hypothesis that is unique to ME/CFS. The authors, Wirth and Scheibenbogen, are working on the second part of that hypothesis which seeks to explain the energy production problems in this disease.)
While the lab results couldn’t uncover why the small blood vessel shutdown was occurring, a small immunoadsorption trial that reversed the small blood vessel problems, suggested that the problem could lie in the immune system, and possibly in antibodies that affect the beta-adrenergic receptors found on the small blood vessels. Much larger studies, of course, are needed to validate their findings, and it should be noted that Montoya’s study did not find evidence of endothelial dysfunction. Dr. Scheibenbogen reported that a small, second as yet unpublished immunoabsorption ME/CFS study had results similar to the first one.
The study did not report on natural NO boosters but several natural substances (L-Citrulline, L-arginine, niacin) are reportedly able to increase nitric oxide levels. I have no idea if they would work in ME/CFS or not but at least with me, niacin (Vit B-3) can temporarily provide small boosts to cognition and oddly enough, given its rather stimulating properties, be relaxing.
Lastly, the EndoPat is typically used to assess the risk of cardiovascular disease. The study results suggested that half the study group might be at increased risk. While no studies have verified that this is so, the combination of arterial stiffness, low-grade inflammation, and high levels of oxidative stress has been hypothesized to put people with ME/CFS at increased risk of cardiovascular diseases.







Maybe no connection, but I got Pericarditis when I was 26, and CFS was ushered in right after that.
Has to be a connection there. I was never well after that .
I’ve got a pericarditis and CFS afterwards with 26 as well. ?
Got exactly the same test and had (or have) endothelial dysfunction.
My doc said it can be everything from smoking to anorexia to Burnout.
And he is actually right:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2860445/
… Fatigue is thought to induce endothelial dysfunction and may be linked to the occurrence of CCVD…
Erm..Jen Brea was supposed to have had severe ME and then suddenly recovered after thyroid surgery and thyroidectomy which means she is on thyroid meds.
Thyroid surely regulates vasodilation?
Oh, I thought she “recovered” after some spinal neck surgery. Now it’s thyroidectomy? Lol, what a scam artist
Jen LeBrea is NOT a scam . Quite the opposite, a pioneer in ME/CFS research. A brave intelligent strong Woman!
please read her full history of illnesses and diagnosises and what she is doing now. Thanks
Jen Brea was truly sick and got truly well.
Jennifer Brea never said she recovered after thyroid surgery. She said that the operation made it obvious that she has intracranial hypertension, which again led to a diagnosis of CCI. Hypoxia was definitely a part of the picture for her.
Jen Brea got much worse after thyroidectomy, likely because the strain on the neck during intubation and the extended neck position required during thryoidectomy, which worsened her underlying issue of weakness of the craniocervical ligaments, increasing brainstem compression. This led to a diagnosis of craniocervical instability CCI), thanks to new symptoms pointing to this (severe central sleep apnea for one). The treatment for CCI is craniocervical fusion, which she underwent for the CCI-related life-threatening symptoms. Subsequently and unexpectedly, her ME/CFS symptoms were nearly eliminated. Jeff Woods had a similar experience, which you can read about on his page The MEchanical Basis of CFS (MEchanicalbasis.org).
The rumor trail is a fascinating monster. Some people with ME/CFS appear to be displeased with the idea that a structural problem could underlie the illness, one that may require a major and majorly expensive operation to address. This response is understandable to an extent, because if CCI is the underlying cause of ME/CFS (it’s not thought at present that all cases are caused by this) then the treatment is out-of-reach for a large portion of patients, because of cost, the need for travel, or unwillingness or inability to undergo surgery. However, the backlash against the suggestion that CCI is a cause of ME/CFS has led to a bizarre backlash against those who have benefitted from this diagnosis. Jen Brea is the most salient and so now some are tarnishing her name because they’ve heard something negative, even if they don’t know what it is!
This understandable phenomenon of social psychology is truly unfortunate. Even if CCI is not the answer for everyone, surely there are clues there. If brainstem compression (the result of CCI) can cause ME/CFS, then researchers should be looking hard at the brainstem in ME/CFS, with or without mechanical compression. For example, the endothelial dysfunction here could be caused by brainstem dysfunction, as the brainstem control the autonomic nervous system which in turn controls blood vessel dilation and contraction and endothelial activity. Conversely, poor blood flow to the brain caused by narrowing of the arteries to the brainstem could cause low oxygen to this critical area with a similar result. Thus, those who fear that the buzz about CCI will lead researchers to abandon research on other possible causes (thinking or hoping that CCI could not possibly be their personal cause) should instead feel encouraged about this enormous clue that has been revealed.
As for “knowing one doesn’t have CCI”; I don’t think that’s possible either. I had very little suspicion of it for myself, but was blown away to find that my cervical MRI taken a few years ago for an unrelated reason, showed significant evidence of CCI. Please, we cannot afford to close our minds or speak ill of each other.
Health Rising has Jen’s story here – https://www.healthrising.org/blog/2019/05/21/jennifer-brea-chronic-fatigue-mecfs-recovering-story/
And she’s been updating it regularly on Medium.
If I remember correctly the thyroid surgery caused her then unknown case of CCI to get much, much worse.
Jen Brea tells her full story here:
https://medium.com/@jenbrea
Vlynx, you make excellent points. The other possibility for everyone to be aware of is that it may not be the CCI that caused the ME/CFS. It could be the other way around – maybe ME/CFS, which affects every other system in the body, also affects connective tissues. Other syndromes associated with CCI as a causal factor include connective tissue disorders like EDS (which also has a lot of other symptoms!)
Maybe ME/CFS is another risk factor for CCI. Who knows. I find the idea that a surgery – no matter how scary – could possibly give some of us our lives back – that’s a beacon of hope and progress.
It was the spinal surgery that caused Jen to recover. Even after an extensive and in some ways horrifying surgery that took her a long time to recover from she immediately realized it had been successful.
If I am remembering correctly, it was the thyroid surgery that revealed the structural problems in Jen Brea’s case.
Whatever made Jennifer Brea better it helped and I am very happy for her. But in all the discussions afterwards I never saw people talk about this and I always wondered : what medications did she receive after the operation ? I mean I know nothing about it but I just can’ t believe they would sow you up after such a serious operation and that’s it. Special preventative antibiotics / medication ? Could that also have done something good ? I am not saying it has anything to do with it but… know what I mean ?
Cort, where can we find out more about Jen’s surgery and recovery? Thks
Martin, Just to clarify, Jen’s health problems worsened after thyroid surgery and only got better after her tethered cord surgery and CCI surgery.
Another interesting Article, Cort!
Happy to see the puzzle pieces coming together! I sure can relate to that squeezing feeling in my legs and pins and needles ..
Pain is so extreme..
I agree with the flow of blood is constricted which in turns does do damage …
Thanks for sharing! Hopefully Drs. they will use this as Dx test tool as it should be a routine on a visit anyhow..???
Erm, you post the same thing in every comment section despite me replying to you and correcting your misinformation. Did you actually read her blog? Because she clearly states she got worse after thyroid surgery. She recovered after CCI surgery which itself disrupts blood flow to the brain.
SORRY BUT YOUR INFORMATION IS INCORRECT. JEN BREA HAD SEVERAL VERY DIFFICULT SURGERIES ON CCI CRANIOCERVICAL INSTABILITY AND TETHERRED CORD SYNDROME. SHE ALSO HAD EDS AND FOUND THIS ALL OUT BY HAVING CANCER AND HAVING THYROID SURGERY. YOU CAN READ ALL ABOUT CRANIOCERVICAL INSTABILITY BEING THE CAUSE OF ME/CFS AND I THINK FOR SOME PEOPLE IT IS THE CAUSE. OTHERS IT HAS TO DO WITH A VIRAL INFECTION AND A GENEDIC DEFECT WHICH CAUSES CERTAIN PEOPLE TO HAVE WHAT THEY CALL POST VIRAL SYNDROME. STANFORD HAS ALOT OF INFORMATION ON THE STUIDIES THEY ARE DOING RIGHT NOW. DR RON DAVIS HAS MANY POSTS ON YOU TUBE AND HE IS FINDING SOME VERY EXCITING NEWS ABOUT WHAT MAY CAUSE ME/CFS. IT IS VERY COMPLEX SO WATCHING AND HAVING HIM EXPLAIN HELP. WE ARE SO BLESSED TO HAVE DR RON DAVIS WORKING SO HARD TO SOLVE WHAT IS WRONG. HE HAS A SON THAT HAS SEVERE ME/CFS.
Being a person with Ehlers-Danlos and ME/CFS, I just received a new EDS book called ‘Disjointed’ (available on Amazon, pricey but substantial at almost 700 pages). I have just begun to study the book, but there is a huge section on dysautonomia which is a very common problem with EDSers, especially those with POTS, hyperadrenergic POTS and other related forms.
Although I haven’t read everything, there are discussions of dysautonomia influencers such as Mast Cell Activation Syndrome, triggering infections, endocrine issues, autoimmunity, gastrointestinal problems, and more. It sure is sounding a lot like all the areas ME/CFS researching are visiting–and with similar results!
Some of you might recognize me as reporting on Stanford’s Chronic Fatigue Clinic. I go fairly infrequently as that’s the way they manage patients, but the last time I was there (pre-pandemic) they told me they were going to pivot their focus more to EDS caused fatigue (rather than the post viral theory that Montoya was more focused on) since a large portion of their patients had EDS. I think that Dr. Bonilla is still continuing his focus on neuroinflammation too.
That’s not to say that everyone who has ME/CFS also has EDS, but there sure are a lot of similarities. I’m going to study my new book and if I stumble on something noteworthy, I’ll report back.
It is refreshing to see a book with so many of the docs leading the way in this area. I was dx by Dr. Atwal last year. That diagnosis led to me finally being able to have my spinal instability addressed. The list of comorbidities that go with EDS can be so long that docs fail to take us seriously because it seems impossible that one patient can have so many issues from a condition that they barely had any education on in med school. Thank you for mentioning this book.
Can you tell me where the Dr is that diagnosed you? How did you find someone trained in this unique area of medicine? Thks
Good pivot for Stanford – and good luck with that 700 page book! You can find it here – https://smile.amazon.com/gp/product/1734794909/ref=smi_www_rco2_go_smi_4368549507?_encoding=UTF8&camp=1789&creative=9325&creativeASIN=1734794909&ie=UTF8&linkCode=as2&linkId=b219c5a69620b2edd19a6da66197778c&tag=edaw-20
It’s getting great reviews.
Definitely seems connection ,I was told years before diagnosis I had blood flow murmur ?♀️Years later after diagnosis I have also developed what looks like reynauds syndrome aswel burst veins ,& also been told my blood clotting levels are higher
Wow. If I’ve understood correctly, the possibility that small blood vessels are not dilating sufficiently seems completely opposite to the theory that for some of us with PoTS and M.E., our autonomic nervous system fails to constrict the blood vessels that aid the venous return to the heart? Indeed, many of us, are being prescribed Midodrine based on the latter theory. The findings here lead me to wonder, are those of us on Midodrine dealing with a double – or even triple – whammy here? If the small blood vessels are failing to constrict adequately, could Midodrine be making our bodies work even harder? Or is one theory looking at delivery to the brain, muscles, tissues etc, and the other looking at venous return away from them – back to the heart? Sorry if I’ve got the wrong end of the stick – but it’s all very interesting, and your updates are really appreciated, Cort.
I don’t know if they are in conflict or not. It’s a very complicated subject. This study focused on the arterioles that send blood to capillaries. After the capillaries provide blood to the tissues it and the waste products from the tissues are directed to the venoules I think and then the veins. It did not assess the venous system.
Wikipedia reports, though, that Midrodrine works “by activation of the alpha-adrenergic receptors of the arteriolar and venous vasculature, producing an increase in vascular tone and elevation of blood pressure.” The alpha adrenergic receptors are different from the beta adrenergic but yes they do stimulate the sympathetic nervous system on both sides.
Systrom has found reduced preload; i.e. reduced venous return to the heart during exercise in ME/CFS.
The really strange thing is that hypadrenergic POTS is characterized by an overactive sympathetic nervous system yet Midodrone, a SNS enhancer, is prescribed for it and it apparently works.
We’re obviously missing something! Maybe Issie can chime in here.
Thanks Cort. The blood vessel discussion is super interesting but also disorienting. I developed POTS much later than ME, and with it came a new sensitivity to anything that increased blood-flow (e.g. vasodialating and/or blood-thinning). This includes supplements that I previously found helpful for ME (e.g. Devil’s Claw tuber).
Question: Even if they’re not in theoretical conflict, do you think it’s possible that treatments for a supposed arteriole cause could exacerbate POTS? For example, I tried a two-week trial of PEMF therapy (pulsed electromagnetic field therapy), which allegedly improves microcirculation. I was skeptical and expected it to have no effects. To my surprise, it made an impact: my POTS got worse!
@David, Devils claw can have a pretty strong detox affect as can Cats Claw and Boswellia. It may be you went into a bit of a herx.
First time I took Boswellia I had the most severe spinal pain I can remember. Couldnt sit, couldn’t lay. They thought I had a ruptured disk and sent me to a spine doc who did xrays. I have spinal stenosis, but that wasn’t the cause. The spinal doc also has POTS and with lots of questioning and sorting, we determined it was a herx pulling out toxins and hitting my spine where I had an old injury as a child. It can work as a sort of antibiotic and with Lyme and coinfection and certain fungus, it can cause that type herx. As can the others I listed.
Also, as things are detoxed and pulled out of tissues, organs etc. They have to be eliminated. If one is not using binders and the detox channels are not working well, we recirculate those toxins. That can also include heavy metals.
Electromagnetic pulse……heavy metals. Pulling out toxins, increasing circulation and maybe not detoxing properly……
And pulling out toxins and recirculating forming more ROS and inflammation and just the stress of the body in an overload condition…..yes, POTS can get worse! I have done this to myself and POTS will go wild. Along with MCAS.
Hmmmmmm, what do you think?
Not all of us need to vasoconstrict with POTS.
I’m HyperPOTS and taking that drug was one of the worst things I ever attempted. I need to vasodilate. Thankfully now, some POTS docs are recognizing that there are some of us POTS people in a whole other subset. What works for the “majority”, will not work for my subset type.
I have reasons for needing to vasodilate. One is too thick blood. There are several things that can cause this.
I do have Ehlers Danlos, and most Ehlers Danlos people will say, they need to constrict because of lax veins. That is not true in my case. I have had Lyme and coinfection and also a type fungus that is in the blood and organs that causes biofilms. Those biofilms attach to the vein walls and they can narrow them and cause dysfunction with proper mechanisms of function.
However, that being said, I have to be careful how much I dilate or POTS will be worse. I use an enzyme to thin my blood and it also takes down these biofilms. I’m using Serrapeptase. Lumberkinase is said to be better, but is more expensive and Serrapeptase seems to work for me.
I do also have low blood volume and have a huge need for my veins to carry both blood and oxygen to my heart and brain. So increasing volumes is a good idea. BUT, not with salt for me. I have kidney dysfunction and one of the POTS medicines increases sodium to make you hold onto water for fluid. I have questioned this “forever”. That medicine is a synthetic aldosterone. Of which I have very, very little of. I also have low renin. Both of these are associated with the kidneys. What is the treatment for this? According to a highly esteemed Nephrologist at Mayo…… diuretics. Well, that won’t work with POTS and low blood volume. So therefore my holding onto salt more with a “traditional POTS medicine”…….all wrong. And he also said there was no way for me to treat this with my POTS. (But, I’ve recently found another way to work around this and am in trial with it now. It should improve blood volume and help oxygenation and clean up acetaldehyde and help muscle strength and connective tissue. Not ready to talk about it yet. Need more observations. )
Sooooooo, to answer your question on this medicine…….not all POTS people are the same. Some of us Do NOT need the same medicines. We need to get to the core of the issues. Some things we think of as “symptoms of illness” are in fact compensations. They are the lessor of the two evils and our bodies way of trying to correct the worse wrong. Even though some of those symptoms make us miserable……it may be the desired response to “Save” us.
I was having similar thoughts about whether or not all the extra salt I consume to counter my POTS symptoms is making my body work harder than it needs to, too.
We are not usually deficient in salt. Salt is corrosive. What, long term is that doing??????? I have been a bit of a “rebel” when it comes to how POTS is treated. I don’t think the “core” is being addressed. And long term, I worry of consequences of masking symptoms.
Especially when those “symptoms” appear to be compensatory and trying to correct a worse issue.
I totally agree with your view, Issie, of trying to work out what your body is trying to do.
I believe our bodies are highly sophisticated and despite what we might feel, at times, they are trying their best to do what they can to help us survive.
Our challenge is to try and work out – what’s going on, why that might be happening and what we can do about it…
So true @Tracey Anne. Ask the question of WHY…….find that answer and don’t go into something blindly or just because someone else says so…….
We are all different and our bodies are created with intelligence. We have to question what it tries to tell us and not react to symptoms as disease……it could be the answer to WHY!
Yeah, I’m a bit of a “rebel”, I want to see the other side of the coin and while I’m at it, what is in the middle too. LOL 🙂
I try and do “circulation exercises”. That are very short sessions of gentle exercises aimed at improving circulation.
Note I use improving, not increasing. When doing them, they remove excess stalled blood and improve lymph flow a bit.
Their main strength IMO however is that they help to make tissue a bit more flexible by not only removing excess waste a bit, but just by the gentle bending and relaxing.
I believe they help both relax muscles and blood vessels. Having your muscles cramping or stiff is one way to constrict blood vessels. A bit of low grade gentle movement can help remove small debris in blood vessels too. When exerting “a lot” of force, your muscles and blood vessel walls might be damaged by semi hard debris. When doing tiny series of low grade gentle movements now and then, each time tiny amounts may grind off.
As such, the quality of the tissue improves and blood flow can better ADAPT to what is needed for each time and activity of the day. Increasing or decreasing all blood flow all day long with medications can never mimic good adaptation I believe.
Doing neck circulation exercises is not to be overlooked. But be careful: doing them wrong can do more harm then good!
Therefore I am NOT going to try and explain what to do. They are simple, but I cannot explain safely for all to read on how to do it. I advice to take a few session (with enough time in between to practice) with a good physical therapist. I did and it was worth every single penny!
For those having few money to spare a free one: when getting out off bed, I first sit for a minute on the side of the bed. Then I slowly get up. Getting up straight from the bed is soooo much more harsh on my blood flow. That makes blood flow and with it oxygenation poorly regulated for a few minutes and likely makes a shower with hormones like nor-adrenaline necessary. That will come at a cost.
Since doing so I slowly lost the moments lasting up to 10 minutes of “walking folded double” with very weak legs too. Those were harsh on my leg muscles!
As a last one, learning to diaphragm breath helped me a lot too. It might seem unrelated to blood flow, but having an extra option to breath better allows my body to better regulate both oxygenation and optimal CO2 content at the same time. Having additional breathing techniques should further help but I still lack the muscle strength for good chest breathing.
Here again: don’t try and learn it from a book or video if you can afford a series of sessions with a good physical therapist. I tried to learn it from a book and did a lot more damage then good to my health. The therapist on the other hand, who is very good at her job, helped me so much. You’ll need more session for it then for the circulation exercises to learn it well.
So, helping your body to be able to better ADJUST blood flow itself according to the needs is a valuable option rarely discussed.
Both the circulation exercises and the breathing exercises could be considered “exercising at a fraction of the physical effort with far more of the good effects of exercising and far fewer of the bad effects of exercising”.
And while doing so, without a single endurance or strength training my endurance and strength increased. How? By improving tissue quality!
It even has a clearly lower bar of entrance for the severely ill then “real” exercising. What’s not to like save the need to find a good and affordable physical therapist?
I wake up with the feeling that a truck run me over and soreness in my muscles [PEM?].
I drag myself to the pool, even if it feels really hard to do, because once in, I start moving around and I wake up and my muscles stop hurting. I just move inside the water, in which ever way I can that day. I feel better afterwards .
Also, liquid vitamin c ‘wakes’ me up like no amount of caffeine does.
Someone with EDS wrote about working on her breathing, how it improved her ability to do so much more, with this tool https://www.pnmedical.com/product/the-breather/
I am wondering if 1) Wim Hof method of breathing exercises, which apparently “shape up” the vascular system could be helpful, and 2) Bemer medical device, which improves local blood flow could be useful interventions. Bemer devices are expensive, but much less than $20k to remove IGG autoantibodies (and which may need to be regularly repeated).
I did try front-loading with citrulline and CoQ-10 prior to exercising, but it did not help with PEM….the only thing that does is keeping my heart rate below 105bpm.
Cort, as always this is a genius piece of work. Every ME-CFS patient should take a PAT assessment. Thank you from the bottom of my heart.
Hi Maria,
If not for a neck problem I would be doing Wim Hoff regularly as I found I was able to exercise at least for a little while afterwards with no after-effects after doing his breathing exercises. They are not for everyone – they can be rough but some people have done well with them. An ME/CFS Wim Hoff Facebook group was started by someone who recovered using his technique.
It makes me wonder about other breathing techniques as well.
I’m looking into breathing exercises and also using mouth tape at night when I sleep. Yes, tape your lips with a criss cross at the nose area. It makes you aware it’s there and you keep your mouth closed and breathe through your nose. It has greatly increased my oxygen, I sleep deeper and longer. And I don’t snore or seem to have apena any more. It’s a keeper.
Dejurgen beat me on telling of the body movements during the day and when awakening. That has helped a lot.
And @Cort, I have had some really bad issues with my neck. I didn’t realize how stiff I was holding it through the day. These gentle neck exercises, that Dejurgen speaks of, has helped my neck sooooooo much. I still have a bit of creaking in it, but nothing like it was. And I had a shoulder injury that hurt all the time. I don’t notice it near as much now.
And if a POTS person, like me, can do these…..anyone can. You do them sitting in a chair. Build up slowly.
If Issie with her high EDS hypermobility had a really stiff neck but didn’t realize it, then a few more of us may have so ;-).
But as said: doing these neck (and other) exercises wrong and you may create a lot of extra damage! They may look simple, but simple things can be surprisingly hard to do well!!!
Even a year or so before I finally fell ill ( but was already low-level ill without me knowing it) I already started to have a stiff neck. I started to have difficulties parking a car going backwards because I could not turn my head around enough to see.
This stiff neck problem has been mentioned before by people with ME / CFS and is absolutely one other very typical symptom with it.
New article just sent to me on nasal breathing vs. Mouth breathing in COVID. Importance of NO in nose and lungs.
https://www.sciencedirect.com/science/article/pii/S1286457920300800
I… thought my ‘stiff’ neck was from poor muscle tone/endurance. Last night I had a front-row seat to some interesting sensations. I was working at my desk on the computer, the tightness creeping in over neck and shoulders, feeling sleepy. I lay down on a mat, to get the blood flow back into my head. Swoosh! I could feel my heart beat all over the blood flow in the area and the base of my head. I get this with my legs when I sit after walking. And then came the dripping – CSF?
The neck stiffness can be low blood flow to the brain (CCI, Chiari, POTS, a rose by any other name…). Coathanger pain is it called?
So what did she have this Jen Brea then? ME or Cranial problem? She was saying for two years she had severe ME. Now she is a director of ME Action I see. Well why does she need to do that if she did not have ME? Am I confused or what lol? SHe makes this film documentary, comes over here to the UK and talks on Breakfast TV about her ordeal with ME, then suddenly two years later………….woosh……….oh it’s not ME it’s cranial surgery with a spanner in the works called thyroid cancer LOL. AMAZING!!!!!!!!!!! Hey let’s all go and Cranial cervical surgery CCI. Yehhhhhhhh
I agree that it’s confusing but getting the time line right should help. Jen Brea fit all the criteria for severe ME/CFS when she created “Unrest”, did her TED Talk and created ME Action.
It was well after that that she, after learning about CCI from another former ME/CFS patient, was diagnosed with CCI, had the surgery done and basically fully recovered from ME/CFS.
As an interesting side-note neither she nor Jeff – patient zero in the ME/CFS community for CCI – had typical cases of CCI/AAI. The ME/CFS symptoms they exhibited are unusual for people with CCI/AAI; ie. – they seemed to have a kind of ME/CFS presentation of CCI.
SInce then, she has, thankfully, continued to advocate for ME/CFS. Through her story many people with ME/CFS have had their spinal conditions diagnosed. Both her and Jeff are also providing a real service by highlighting connective tissue problems like EDS which have been overlooked in ME/CFS.
you can say it somuch better then me CORT!
A bit off topic but It is interesting, Cort. I can remember getting a severe stiff neck Suddenly some time before all my current symptoms developed. It went away then came back at some point and went away again but I never thought twice About it until I contacted a rheumatologist in Wa state who found disproportionate amount of fibromyalgia patients had positional cervical cord compression syndrome pc3. With his guidance I received a special MRI and he confirmed the diagnosis. My question is I wonder if there are more people with neck symptoms and CFS than we know. Not everyone is able to get such imaging And lack of symptoms don’t tell the whole story but I wonder if a survey or poll has ever been done asking about neck symptoms and if it might be beneficial for one to be done to see how many may have some sort of overt symptoms? Just a thought.
Hi Michael –
I’m starting to suspect that my neck is driving my dysautonomia disfunction and PEM. I have already worked on my MCAS, and gotten better in that respect, yet the HR/BP problems persist and getting worse this summer.
I have the symptoms that go along with CCI. Comes and goes.
I’m paying more attention and trying to be more aware of what is going on with my body. For example, when I sleep on my side, I flex my neck. I’m trying to reposition it to be straighter. Etc.
Did you do something to address your neck problem?
Pillows make a huge difference. I find the microbead pillows very helpful. And there is an anti snore collar that can stablize the neck with sleep.
Meirav,
I Sadly did not. The rheumatologist I consulted by email directed me to a specific Physical Therapist in Wa state and said just a few relatively easy exercises to train to balance the skull differently and help increase spinal canal space helps a lot. He Also said a few medications such as low doses of Klonopin (I believe) help reduce the spinal cord irritation. He said it is very treatable with the right PT. I stopped traveling to WA and I was unable to reach the experienced physical therapist he recommended. I was unable to find anyone local to me to help. I have now found physicians interested in possible spinal issues in CFS at Mass General/Harvard in Boston and they are sending me for an updated MRI since my WA MRI Showing spinal stenosis was about 6 years ago. It is unknown what they might recommend. I too have found to have dysautonomia. I had an Invasive Cardiopulmonary Exercise Test from Dr. Systrom at Brigham in Boston and found to have preload failure. Tried Mestinon for a year without benefit and am now trialing Florinef. However, I like you, wonder if there could be cervical issues causing some or all of my symptoms and why some treatments others have found useful have not worked for me yet.
Please Martin, read all her posts and articles about her illness and her advocacy before making such statements. She has summarized much of her experience in the online magazine Medium. As a community we need to reject charlatans, but not lash out at people who have suffered for years from ME/CFS and from medical abuse & who continue fighting for our cause.
Thanks for writing about this Cort. I started a drug, Kuvan, in late February, that’s dramatically and positively changed my ability to exercise. It used to be a supplement, tetrahydrobiopterin, or BH4, before BioMarin made it into an orphan drug for children with PKU. It has many other uses, though.
BH4 is needed for the body to make NO from arginine. And BH4 is needed in Martin Pall’s treatment theory for reducing oxidative and nitrosative stress in ME/CFS, along with folate, B12, and C. So, BH4 is useful in creating NO, and reducing peroxynitrites,which impair mitochondrial function and damage mitochondrial membranes.
In addition, I got some nitric oxide test strips, and found I had very little nitric oxide. I was able to increase it using a product from Berkeley Life, which contains vitamin C, thiamin, folate, B12, calcium, potassium, green coffee being extract, and a Nox: BP complex, with beet and pomegranate.
The help that I’ve gotten from these interventions is on top of the autoimmune POTS treatment that I’ve been doing, which is a beta blocker and Huperzine A (this is instead of Meztinon, as Mestinon contains allergens).
I hope the scientists can look into tetrahydrobiopterin and nitric oxide supplements.
s if I understand it correct, tetrahydrobiopterin, or BH4, is no longer available as a supplement? Sorry to ask but verry verry ill.
Where you for decades bedridden if I may ask?
Even though I have mutations in MTHFR pathways, including BH4, I have found addressing some of those mutations to not be very helpful. In fact, some I just don’t tolerate and it sends things off in a unwanted direction.
Building up certain things can cause more free radicals and more toxic issues if things are not in place to “clean up”, what may happen. On paper a lot of times it looks like…..I need this, I know there is a problem here. But it just might not work as desired.
Just be cautious with supplements. We may “fix” one thing but create other issues.
BH4 also plays a big role in development of neurotransmitters. And Huperzine A increase choline in the brain. Both are important and can help with brain fog, memory issues, muscle dysfunctions. But as Dejurgen posted on a previous thread, too much and improper detox of those neurotransmitters, can lead to more disastrous chemicals and if not properly “cleaned up” worse consequences for us.
Think of all supplements as a medicine. Our body has to process them. Can it? And will it do it in the desired way?
I prefer herbals and supplements over synthetic medicines. But I do realize it becomes a very potent medicine when it is refined and standardized. And the liver, kidneys etc. Has to process it all. We have to know what we do and WHY, before we attempt it.
Yes Di I have read some of her story on her website. But I contacted our ME Association today to ask the Dr’s opinion about Jen Brea’s recovery and he wrote back and said they do not recommend CCI for ME/CFS patients and it is doubtful whether a neurosurgeon would undertake such a procedure for ME/CFS patients in the UK. He then said that he knows of one ME sufferer who went abroad at great cost to have CCI surgery but there were no benefits at all after surgery. Therefore he does not recommend it as a treatment currently for ME.
Also as I mentioned, Jen Brea had thyroid surgery so she may have recovered if it was her thyroid causing her ME. SOrry to be a spanner in the works here. Please just wait for coxsackie antivirals from Belgium soon as this may cure a lot of ME sufferers. I smell a rat with Jen Brea and it is the Hollywood multi million dollar film industry. Sorry I am a spanner.
Enough Martin! Please keep your whatever you think you “smell” out of this blog, Martin, stick to the facts, and stop with the character assassination. No more on Jen Brea.
CCI surgery, by the way, is not done for ME/CFS – it’s done for people with documented spinal problems. Of course a surgery like that would not be recommended for ME/CFS population as a whole. .
And I have/had two POTS with EDS friends who had this surgery. One is no longer with us as it went horribly wrong for her. With multiple corrective surgeries, that didn’t work. The other one is not recovering well either (and it has been years) and is having to use a Walker to walk. Neither got a better life from that surgery. At least the one girl, no longer is in the pain she was in.
My son has been taking nifedipine / nimodipine for 12 months and there has been a gradual but significant improvement in his 8 year ME journey. Does nifedipine (supposed to increase cerebral blood flow) tie into the German study of blood flow and narrowed small blood vessels? His pain has significantly reduced but fatigue issues still there…..
I looked this medicine up and it is a calcium channel blocker. It does vasodilate and slows down the heart rate.
There seems to be some connection with ME/CFS and FMS with calcium channels playing a part. There is a study out of Australia called the Griffith study and they associated it with some mutations on the TRMP genes with calcium channels. Of the 5 they associate with these illnesses, I have all 5 as predisposing me to these issues.
I also have found very, very mild calcium channel blocking activity associated with GastroCrom (a mast cell stablizer) and Tramadol (works on all neurotransmitters, including glutamate and opioid receptors.) And both have been a big help with me over the years. BUT, have to be extremely low, low amounts and cycled on and off to be effective.
treatments for ME in America are like the goodies in Charlie and the Chocolate Factory. Also Mestinon (Pyridostigmine Bromide) was trialled here in the UK years ago but I think it failed to show benefits yet this Jen Brea said it helped. Amazing. Still, only small trials have been carried out really on anything.
ALso if CCI is the cure for ME due to the ligaments being attacked as US scientists say, then we need not go any further. Get the papparazzi round. EVeryone stop reading. THE CURE HAS BEEN FOUND. What are you waiting for? You all have medical insurance there. Go get the neck surgery and report back. Yes,Di andrick, if you are so sure CCI is the answer, why have you not had the surgery then? LOL
Nobody but you is claiming that CCI surgery or any other treatment for that matter is “the cure” for ME/CFS. Here’s an idea – go to a Forums or a place with recovery stories (Health Rising has one) – and see the many different ways people recover when they do – and then come back and try to make the argument that any one thing is the cure for ME/CFS.
I’m getting increasingly frustrated with some of these studies. I understand the need to investigate from every possible angle, but researchers often can’t see the wood for the trees. All we know is a lot about nothing. Small fiber issues are a symptom, not a cause. It is a manifestation of the hypometabolic state. The cell danger response can cause this to happen! I fear that we are just going to end up with another mountain of farmaceutical products aimed at ameliorating symptoms, while ignoring the cause.
I can see your argument, about lots of studies all finding different interesting theories, but not seeming to actually get us any further.
However I wonder sometimes if the problem is that that banner of ME/CFS is covering too broad an array of conditions. There are perhaps a lot of us with similar and overlapping symptoms, but brought on by different initial causes. But these various conditions all happen to end up with similar symptoms.
There is deffenitly a problem with bloodflow and oxygen in ME and POTS patiënts.
It also could explain the UBO’s found by MRI studies in these patiënts. Also the higher microglia cells and other anomalies found in the brain. I would like to see more studies about the red bloodcells. The blood is sticky and the shape of the redbloodcells are different. So they can’t go in the cells to give oxygen. Then the ANS kicks in to compensate the lack of oxygen. So the fight mechanism kicks in to survive. Now the loop is complete.
Very interesting.
I can’t help thinking, though, that for some of us low NO is something our bodies do very deliberately to preserve core blood flow in the presence of low blood volume. If I take anything that dilates blood vessels my BP drops dramatically. The price for the body’s natural response is small fiber neuropathy, numbness and further problems with circulation leading to gastoparesis etc., but it happens for a very good reason. MCAS is a possible driver of low blood volume/high adrenaline.
I also wonder if the researchers here were considering antiphospolipid syndrome?
To answer your question on APS, yes I was positive with one of my checks and also on 2 other markers for too thick blood. So that is on the radar too. Too thick blood can definitely slow blood flow.
Yes. Delivery of oxygen, and possibly the pickup of the carbon dioxide waste product, is the problem. And the feedback loop to get more oxygen to the cells, makes the problem worse for us. Anything that calms the brain, relaxes the feedback loop, and makes us a little better, but does not correct the original problem.
The delivery of oxygen by red blood cells seems to be pretty fragile chemistry – a lot of places things could easily be off, not just in the red blood cells themselves.
(Comment edited – out of existence actually.
Note: Disrespectful and mean-spirited comments just don’t fit here. Fact based comments do. Martin’s comments are now being moderated. Cort)
I have a small question that is not yet really clear to me : If someone with POTS and ME / CFS improves their illness, or it gets better over time, do the POTS symptoms also get less, are they intimately connected in general ? It did exactly that with me but I would like to know.
For me they are connected – less ME leads to less POTS. Quickly, even.
My POTS symptoms are getting better. Still there, but better.
I’m don’t have a medical background. But as far as I know, their underlying connection is as mysterious as their underlying causes. I know people who were diagnosed with POTS well before ME, whereas my POTS-distinctive symptoms didn’t begin until years into ME, after a relapse left me chronically deconditioned.
Regarding how improvement in one might improve the other, here’s a few basic points:
1) POTS makes your heart-rate go higher than what moderate-severe ME sufferers can tolerate. If your POTS got better, then you should be able to handle more upright activity without crashing, which could benefit your ME itself in all kinds of ways (e.g. less deconditioning, better sleep, better self-care, etc.)
2) ME’s most distinctive symptom is PEM, especially an unusually harsh reaction to exercise. If your ME got better, then you’d be in a much better position to employ one of the best natural treatments for POTS: core and lower-body exercises. And if that fails, well, at least you wouldn’t have to risk crashing from the application of those godforsaken compression socks!
3) An improvement in one might benefit the other if it eliminates medication interactions, contraindications, etc. For example, before I had POTS the most effective medication for my ME was low-dose Trazodone for sleep. Now that I have POTS, I can’t handle an effective Trazodone dose without lowering my morning blood pressure, which exacerbates my tachycardia. Conversely, while my POTS responds immediately to Mestinon, this drug seems to cause restlessness and reduced sleep over time, which I doubt would happen if it weren’t for my ME drug sensitivities.
Many people have relapsing remitting ME like I do. This time the relapse is not that bad however. So I suspect Jen Brea may relapse in future too. Watch this s pace. Yes my OI went away when I went into remission. It has not come back with this relapse.
Do you know how regulate this pathology : « Narrowed Small Blood Vessels »
Do it exist dietary complement, alternative medecine or other things ?
I dont know about any off-label drugs to use for this. A few months ago I invested in a $200 sauna blanket to help with my microcirculation, which I know for me, is part of what is the source of many of my issues. After using it regularly for a few weeks my cuticles miraculously appeared and my skin cleared up. I know these are surface-level observations but I hope this is reflective of similar changes inside. At the very least I figure this gives my tissues increased access to oxygen for a short time, and allows for metabolic waste removal. Hasn’t been a cure-all, but it has helped slightly energy-wise and cleared up my head some. Am sleeping better too. I do hope this triggers an increase in blood volume with longer-term use.
A vegetable-heavy Keto diet has been my mainstay. Any time I try anything else I have major setbacks. Im still working with a functional MD to get other supplements and medications figured out. Im not “recovered” by any means, but have figured out that I have more energy when I do these things.
As for my hEDS, from what Ive read, my theory is that it is a symptom of the body compensating for other core issues such as increased lactic acid. The body takes proteins (or something) from the connective tissue to neutralize the acid (or other toxic byproducts). I think the body sees the connective tissue as more disposable than other available tissues and mines what it needs from there, to survive.
Thank you for your good advises… perhaps for your hEDS you can try collagen ?
Obvious that Bartonella is a small blood vessel disease is at work here. They should screen how many are cat owners?
I’m curious about your comment? I have Bartonella H. and would love to hear why it is obvious to you. Ps I also have a cat. 🙂
Hello
After reading earlier articles on the “oxygen crunch” in FM/CFS and then reading about the micro circulation and endothelial dysfunction in the latest post to HR, I’d like to ask if there have been studies on or patient experiences with PEMF devices.
PEMF reportedly supports healthy micro circulation. Any info on the use of PEMF for CFS in particular?
Nicole
I remember from a past article that low dose propranolol helps with fatigue in POTS patients but not high dose. Low dose propranolol causes a release of NO in the brain but high doses do not.
https://www.frontiersin.org/articles/10.3389/fnins.2019.00033/full
Nicole,
Great question. I’d like to see Cort do a post dedicated to this if he hasn’t already. There are many references to PEMF on ME forums and there’s a post by Cort on a device that may do similar things (https://www.healthrising.org/blog/2019/01/29/hummingbird-fibromyalgia-pots-chronic-fatigue-syndrome/).
See also my response to the POTS convo started by Angela above. In sum, I had to quit my PEMF trial after 1.5 weeks of multiple times per day because my POTS got dramatically worse.
It’s possible that it may have helped my ME if I tried it for longer. But my advice for ME patients who also have POTS: be cautious about messing around with blood flow.
See my response above to @David above……may be more issues involved.
Many thanks. Would ALSO like to see more on micro circulation, ME, and PEMF
NICOLE
This POTS specialist recommends NO enhancers.
https://franklincardiovascular.com/nitric-oxide-in-promoting-healthy-autonomic-function/
People with low blood pressure need to be careful with NO and vasodilating. It can lower the blood pressure even more.
Even though I need to vasodilate (to a degree), I didn’t do well with things that increased NO a whole lot. I found other ways to vasodilate to be more “gentle” with me. It was a bit too stimulating and too dilating. We are all so different.
NO is not a stable molecule but a radical. It lacks enough oxygen to be stable.
As such, it IMO reacts very quickly with oxidative stress. That reduces the amount of free NO available for dilating veins. NO however doesn’t convert to something harmless when reacting with ROS, but is very likely to create even more reactive radicals: RNS.
Where ROS stands for reactive oxidative stress, RNS stands for reactive nitrosative stress. That is a bad thing too. Adding NO to a system with plenty of ROS risks to add plenty of RNS.
The subject is complex however, but it’s IMO not as simple as just adding more NO is always good if it is short.
Perhaps these autoantibodies are the missing link in Ron Davis (Stanford) where he put ME/CFS blood cells in healthy plasma and they worked correctly. When he reversed the scenario, the healthy blood cells placed in ME/CFS plasma acting sick, unhealthy. So what was in the plasma of sick patients causing the problem? Was it these autoantibodies against beta-adrenergic cells. Also I understood the researcher in Sweden, Dr. Bergquist, found elevated levels of these same autoantibodies. Intriguing!
That would be our dream scenario! Let’s hope! Whatever happens good news that Bergquist has apparently replicated the findings. 🙂
This research in this article is not new. The idea that there is hypoperfusion going on has been thought about a long time ago. Some researchers in Australia I think found there was not a deformability problem but Ron DAvid said there was. My hands and feet have never felt or looked cold in 28 years. Whether hypoperfusion causes brain fog or not though I have no idea. I wish I knew the answer to this question. Many things can cause brain fog though. WHat I would like to know is do hypothyroid people experience post exertional malaise? Seems logical to me. If you exercise and need more energy and aren’t getting it delivered to the tissues, then this could cause a problem but would it cause PEM in hypothyroidism I wonder.
I think it’s interesting that there seems to be more awareness of the hyperadrenergic mechanism in POTS in this community of patients than the EDS one.
The literature says this mechanism is seen in a smaller subset of people.
I asked in an international (h)EDS forum who has hyperPOTS. About 30 answered.
Someone else posted focusing on just the symptoms – too much ‘adrenaline’ – and over 300 comments in a few hours.
The literature in fibromyalgia describes over-activation of the sympathetic system. A rose by any other name…
+ How small is this hyperpots subgroup, really?
Is it really rare, or under-diagnosed and under-recognized, even by doctors themselves. (The EDS doctors around these lands don’t recognize that POTS can present with orthostatic hypertension, for example…)
And also, it is interesting to note what is the autonomic system doing while SUPINE. My HR and BP seem to go down too much, and then a wave of something (nor-epinephere?) rushes in to pick things up, eventually settling in at normal rates. Also, how is pulse pressure changing before, during and after.
The supine response seems to be more dramatic when I am experiencing more autonomic instability while upright. Or when I first come to being supine after being upright. Like the systems is settling itself. OR the liquids in my brain. Who knows?
There are different mechanisms that drive POTS, that have been identified for now. One can have more than one mechanism present. Where is the good paper that explains those mechanism? I need to dig it up 🙂
Both in the medical population and community groups, they make note of how difficult it is to treat the hyperadrenergic subgroup. Non-pharmacological and pharmacological interventions that work for the other types, don’t work. A lot of trial and error to get the right combination of medicines, etc. Ivabradine is reported to work well, which interestingly, is also reported to work for same heart problems in MCAS. Dr Weinstock uses Ivig with his more extreme patients that don’t respond to prescribed MCAS treatment, I gathered from one of his patients.
Informally, what I am gathering from other people, is that addressing MCAS and/or homocystinurias-related gene defects manages the hyperPOTS too.
Ah this… thing about veins being too stretchy and hence causing all the problems… It’s a theory with no legit studies nor research looking into. Probably it started with one or a few doctors saying this is what they were thinking is going, I can picture it during a Q+A session after a presentation, and then everyone started repeating it as gospel and became ‘fact’.
@Meirav, for them to truly call you as having the subset type of POTS as Hyper, right now the criteria is a suge of norepinephrine above 600 from Laying to standing. They don’t base it on blood pressure. All people blood pressure goes up slightly when they stand, as does the heart rate. But then it settles down. With POTS, the heart rate climbs. And that is with just standing still and no movement. If it goes 30 points above laying heart rate or above 120, they say you have POTS.
With many, not all, HyperPOTS, many of us have higher blood pressures. There is still the Orthostatic drops that causes feelings of dizziness and fainting. But it is from a higher level more down into a more normalize level. Still same affect. Still a need to get seated and feet up. I usually have enough warning signs and can get seated before I faint. (Thankfully fainted only 3 times, in a lifetime of having it.)
As stated above…..I’m a bit of a “rebel” when it comes to just accepting what is said or even written. I dont agree with a lot of it. I do my own research and have very keen self awareness and observation.
There is a strong connection with MCAS and POTS. It does help my POTS to have MCAS better managed. I also have EDS. So am aware of that too.
Many things thought of as “symptoms” of illness is compensation of the body trying to right itself and is the lesser of two evils.
I’ve written a good bit on Cort Healthrising forum and also the DINET forum (years ago, but it can be looked up under my profile). But you will find, what I say to be a good bit different than the majority. But now, many of my hypothesis are becoming more mainstream and finally becoming known.
How you treat a HyperPOTS with higher BP and the more common forms IS different. We can NOT be treated the same.
I’ve been addressing MCAS and I’m so much better, haven’t been in the hyper-reactive mode for a while. My POTS hasn’t improved at all. If anything, it’s the worst ever this summer. I’m begin to wonder if CFS leaks / CCI are driving it [I do have symptoms of it.].
Also, responds to methylfolate.
Trying to figure out the next step, what and how to address.
POTS happens when standing. POTS has a strong connection to poorly regulated blood flow.
When standing, blood in the legs easily accumulates and has more difficulty returning to the heart. It also needs to be pumped at higher pressure to the head. If the vascular system is damaged, that may be tricky.
With mechanical pumps however, the low pressure side is often the bottleneck. The fluid has to find its way to the pump entrance by nothing but air pressure. With the human heart, the fluid has to find its way back by the pressure of the skin and the pressure provided by movement.
The blood returning from the head? Easy as gravity pulls on it.
When laying down however things change. Blood now far more easily returns from the legs to the heart as it hasn’t to overcome the forces of gravity. The often forgotten part however is that blood from the brain isn’t helped by the pull of gravity. For people with supposedly constricted veins and capillaries, that is very likely a problem.
It almost naturally results in a decrease in return of blood from the brain to the heart. If the blood pressure would remain constant, even more blood would reach the brain as once again that part doesn’t need to overcome gravity when laying down.
When there is a driving force for more inflow of blood to the brain and reduced outflow, the arteries and veins have to adapt in order to not let too much fluid pile up in the brain.
When fluid piles up in the brain then brain or CBF pressure naturally will build up until a new balance is found. It is, physically spoken, one of the natural ways to reduce inflow and increase outflow. So IMO in *any* disease with increased CBF pressure one may question the return side of the blood flow in the brain being sufficient. To me that is what physics says.
=> As our arteries and veins likely are already quit constricted, regulation range for blood flow to the brain by modulating them is limited. In plain speak: it’s hard to squeeze a tube even further if it’s already squeezed to the max. How to further reduce inflow that way?
Doing, under guidance at first, some neck and shoulder circulation exercises eases a single bottleneck of blood return from the brain to the heart a bit (by not allowing tight neck and shoulder muscles to further squeeze those big arteries and veins to and from the head).
It’s not much but any bit helps. Shaving off the worst 5% of the problem often shaves off quite a bit more then 5% of the dysfunction and that shaves off quite a bit more then 5% of the poor quality of life.
The third mechanism to better balance brain blood inflow and outflow is reducing heart pressure.
=> That leaves the body the option to reducing blood pressure when laying down a bit more then what is needed with healthy people as a good option. Now if you just stand up from laying down and start to walk away from the bed, your blood pressure *has* to race up.
Allowing it some time to gradually adapt is the easy way to reduce the problem. Using that leg blood pump a bit while still seated helps getting sufficient blood to the head too.
Any bit of less nor-adrenaline needed by doing this IMO will have small benefits for way longer then the next 5 to 10 minutes and they’ll accumulate over time.
=> The remainder that can’t be compensated? Much risks to end up in increased brain pressure. Trying to get brain inflammation bit by bit down is part of the challenge here I believe.
reminds me of this
https://www.theilcfoundation.org/wp-content/uploads/2012/04/Driscoll_Theory_EDS_-_Online3.pdf
That drug was a real disaster for me. It is a sulfur and sent my kidneys off in a bad direction. Is also a diuretic.
Sleeping with head elevated, is a must for me. Having my feet a bit lower than my heart and not bending too much at the waist.
And always sitting with my legs up. I love a big bouncy exercise ball for my legs. I can fidget a lot and get a little exercise in with it. And it’s easy to roll up to a chair or away from one. My best leg rest ever.
Just note as to stabilization surgeries, not all have had a good response with that. I lost a dear, wonderful friend to that and other girl, is soooooo not good either. I have some bad issues with my neck and full spine because of EDS. But surgery is not even on my radar. Other things to try and that would be my last resort. And I do now have some spinal cord compression from it.
But the spinal fluid leak, for sure needs addressing. That can explain all sorts of symptoms. Just had a friend undergo that surgery too. Jury still out. Recovery is up to 6 months.
Look at the information Bayard has on MCAS. Whole new way of looking at histamine and how to manage it. It too may be a much needed compensation.
I agree!
Just a little sidewalk: Maybe this curcumin is a component when it comes to endothelial function and muscle oxygen saturation? Combined with slow breathing, meditation, short walks it ha made a difference for me with ME.
https://clinicaltrials.gov/ct2/show/NCT04119752
Issie, that’s because stabilisation surgery is nothing to do with ME/CFS. She had thyroid cancer and so that was her ME/CFS. In fact the thyroid or hormones have got everything to do with ME/CFS. It’s an environmental illness afterall.
@Martin, Brain stem compression can affect the nerves going to the body and also the autonomic nervous system. With EDS, there can be not only brain stem compression, but the whole bottom part of the brain can drop down into a V shaped canal and compress that part of the brain (called cerebral tonsils). Jt most definitely could cause issues with not only POTS but ME/CFS. Those labels could be the symptoms of structural issues. And with brain compression, who knows what all else could be affected. Even issues with proper brain detox. Tumors in the brain, just that small interference, can cause all sorts of problems.
Treating thyroid issues, has not made my other things any better either. So may be one piece of the puzzle…. but that is only one piece.
Cort,
Do you think plasmapheresis or plasma donation would benefit mecfs patients based on this research?
Immunoadsorption is similar but different. It removes antibodies- leaving the good ones (hopefully) behind while plasmaphoresis adds antibodies – hoping I suppose to swamp the bad ones. Both appear to be seeking to alter the antibody status of the body.
https://www.sciencedirect.com/topics/immunology-and-microbiology/immunoadsorption#:~:text=Immunoadsorption%20is%20a%20selective%20apheresis,not%20in%20the%20United%20States.
One would think plasma donation could have similar effects and IVIG sometimes helps.
@issie There is no evidence at all that I have ever heard in 28 years that ME patients have got brain stem compression. A neurologist would surely be able to tell if ME patients had that. And lots of patients have consulted with neurologists. People also get better from ME/CFS for no reason at all. Mine went into complete remission for thirteen years. So it is I would think impossible for those people who go into remission to have brain stem compression. Sorry but I don’t believe it is the cause of most viral onset ME/CFS. I am from the UK though so you might know something else.
It could be true for a few. All these things are labels for symptoms. If we get the label because the symptom fits, then we search for the WHY. And there may be many reasons and the answers to WHY, having many different answers.
NEVER say NEVER, and Never discount what may be true for someone else. We are all complex, complicated and different.
I have POTS……how many subsets are there. That is based on symptoms which subset I get put in.
There are at least 8 known forms of Ehlers Danlos. Most can be checked with genetics. But there is at least one form that cannot. Yet they still say it is Ehlers Danlos. We all have similar symptoms. But we present differently.
There can be structural issues causing symptoms of ME/CFS. If those structural issues get corrected…..it could correct and change the DX that was given that person. But until that WHY is fully explored and determined……they are stuck with the knowledge they have at the time and the label given them.
That’s NOT to say all ME/CFS people have EDS or structural issues. But neither does all POTS people have EDS and MCAS. But many of us have all of these. Now to determine the WHYS. And then to find our own personal, fix it the best we can, “purple bandaid”.
There can be, ARE, probably, most likely more puzzle pieces to all these complex illnesses. And if we can get enough of the pieces and connect the dots…..we just might get some RELIEF. And if some find their relief……have a party and celebrate them finding their long lost life. Yayyyyy for them!
Most people’s symptoms start after a viral infection. Perhaps people who get ME/CFS in a car crash or head injury might suffer CCI. In almost all cases, viral onset ME/CFS I would highly doubt is anything to do with CCI. That’s why I don’t understand Jen brea. I think she had hypothyroidism. SOrry but that is my opinion.
And, she has EDS. If you go on sites and read symptoms of EDS, you will notice many of the same symptoms connected to ME/CFS.
I didn’t get DX with EDS until in my early 40s. And have had it my entire life. It was sooooooo obvious and no one told me that I had it as a child. As that would had explained an awful lot. Why I got sooooo nearsighted as I was growing. Why I was double jointed and could do strange tricks with contortions. Why, I was a bit clumsy and always spraining my ankles. Why I had pain as a child and had to be careful how I moved, slept or things went out of place. Why, I easily bruised. It was always there, just unrecognized. Now I have a WHY.
We have to sort our WHYs. The clues are there. We have to observe them, connect them and work with them. Our body tells us what to observe. And it tries to right the wrongs with “compensations”. We mistakenly sometimes think these “compensations” are symptoms of illness……when they are not.
I have all those “labels”. Those labels just connect me to a list of symptoms associated with them. That does NOT give me my WHYs! I want to go deeper than symptoms….I want the “core” reasons. I want the WHYs. On the search for more “purple bandaids”. And I am getting some!
I have a whole lot of my WHYs! Doesn’t mean the answers can change the “core” problem and actually completely solve it. But what it does mean is I can work with what I know and cover over the booboo a bit and not notice it so much.
For those that don’t know why I call it a “purple bandaid”. This phrase is my own creation. Purple is said to be a very healing color, and periwinkle purple is my favorite color. So what better choice to have…. my favorite color and its healing. 🙂
Issie
Does anyone have any thoughts/knowledge/experience on whether plain beet supplements with nitric oxide are helpful for people with ME/CFS? Or if they can be harmful? I’ve searched but not easy to find. Appreciate the post that mentioned a supplement which contained beets appeared to be helpful, not harmful.
PS, to clarify – or rather, plain beet supplements that encourage NO production. Sometimes these things are counterintuitive, in that if your body can’t handle/utilize something that would normally be good for it, it may be bad. Will give it a try but again wondering about personal experiences.
Beets, I read recently, are also rich in potassium. Which the balance of that with sodium is wonky in my system, and I think many of us – right?
Hi @Linda Rouleau
Since reading this article I have been using a combination that has worked extremely well for me – my post exertion malaise and general health has significantly improved over the last few months since starting a combination with beetroot and other things
1) a variation of hydrogen rich water (HRW – which is basically h2 gas in water). One brand I had a slightly negative reaction, one brand a limited positive reaction, and on the Mercola brand I have been doing very well (said to be up to 8ppm).
For the first week I had a strong detox reaction in spite of my liver being in a relatively good shape (much better than a year ago), I am on a detox programme.
I had various issues that seemed to relate to microcirculation and also use a combination of:
2) Beetroot (for nitric oxide NO to improve circulation),
3) Vit B3,
4) L-Arginine (important to circulation) and L-Lysine (to balance out the Arginine which can create a good atmosphere for chronic infections to thrive), and
5) Citrulline malate;
6) and also regular electrolytes (cheap local sports drink brand).
When I tried to stop some of these supplements things deteriorated so I seem to need the combination, the one I seem to need least so far is the B3.
@issie Well it seems like your have EDS then but…..I do NOT have EDS. There was nothing wrong with me as a child, I am not double jointed and do not bruise.
WHat you have to do is ask yourself how your ME/CFS started. Was it after a viral infection? If not, then what happened to you to get ME/CFS? Most people get it after a viral infection. Some people get it after poisoning (organophosphate poisoning for example). Jen Brea had a viral infection she wrote and did not get over it so hers has nothing to do with EDS even though she has EDS.
[This is continuing a prior set of comments/replies; was getting narrow, the paragraphs, so I started a new one]
[1]
I’ve read in a few journals calling for more awareness and research into orthostatic hypertension, and it is recognized to be connected to hyperadrenergic POTS (and a few other conditions). Not necessarily true in the other direction [If A, then B but not if B, then A]
While there are some changes in blood pressure to compensate for the action of gravity on the cardiovascular system experienced in all bodies, when that response :
– decrease in systolic blood pressure of at least 20 mm Hg or diastolic blood pressure of at least 10 mm Hg = Orthostatic Hypotension
– no official definition YET, some propose at least 20 mm Hg, others 10 for systolic, 5 or 10 mm Hg for diastolic. You get the idea. this is work in progress = orthostatic Hypertension
(which if yours goes up 50 mm Hg, that difference between 10 and 20 is irrelevant)
Now, if your blood pressure does both, I’m not sure that it is technically one or the other. I also seem to experience bradycardia, not only tachycardia. I think instead of getting all these different labels/diagnoses it would be _____ to describe what is happening by means of really thorough testing and/or acute observation powers by a very knowledgeable and astute doctor with experience in the field.
[2]
From what I understand, there are a series of mechanisms going on in Hyperadrenergic POTS, in addition to the elevated levels of nor-epinephrine.
https://www.vumc.org/adc/38938
[3]
POTS can also be ‘seen’ during the valsalva maneuver – by exaggerated responses in phase 2 and 4 [https://www.vumc.org/adc/38918]
– – -> As I write this, it reminded me: so I have hypertonicity – in only some muscles or all, this I do not know yet. What I learned doing biofeedback, is that when the muscle goes from contraction to relaxation – it takes a longer time than usual. And that is one of the things to work on. When I do contract the muscle, I cannot keep it contracted for long [low endurance, i.e. weak].
I wonder, if, then: could this also be happening at the level of smooth muscle? If they are ‘slow to react’, if the veins need to dilate as instructed by the vagus nerve/brain, etc, and they do that slowly, and how that may be influencing feedback to the autonomic system. If the veins dilate slowly, if they cannot keep contractions for long, if their normal ‘resting’ tone is somewhat tense (hypertonicity of the veins. Could that actually be a thing?) – maybe that is why my autonomic system is so unstable and has a hard time reaching balance. Maybe the problem is the veins and all the wonkiness is the autonomic system responding to that, trying to get things working. This sounds logical – we know so little about the body, and what is unknown doesn’t work logically, because we don’t know it yet. So this could all be way off… Observations –> hypothesis —-> testing —> observations, etc. This is to say = I know very little.
There are just thoughts.
[4]
I also have been thinking how this may affect my breathing. My exhalations seem to be… long. If that’s when the diaphragm is relaxing, and if mine is hypertonic, it makes sense.
So working on breathing, works to correct whatever is off with the respiratory muscles, and yes, resulting better oxygen in the body.
[5]
It works the other way as well, those with hypotonia would have the opposite problem.
[6]
Fun fact: when I take a methylfolate, spasms stop, stiffness releases, heart rate and blood pressure stabilize, and I feel like I can finally breathe. Within 30 minutes of taking if not less.
[7]
Now, I wonder if a few – more than few – of you here.. have some degree of hypertonia… hypermobilty?
I say this
because
In my family, my sister had a diagnosis of EDS at an early age
A hundred years later of weirdness and all sorts of symptoms and conditions, I finally get diagnosed also.
The thing is – she is on the hypotonia side of things. She ‘looks’ bendy. I do not.
She looks like the typical classical EDS (even though is is hEDS). I think marfanoid habitus is also more prominent in those with hypotonia, at least when I look at my extended family.
I never thought I had it because I didn’t ‘look’ like her, did not do that weird thing with my fingers, etc. I thought I was rather not flexible – which turns out to be true, because that is a property of muscles. And mine are hypertonic.
When the PT measured the range of motion in my joints – sure enough, hyperlaxity.
My joints seems fine, seem to function fine – the moment forces come into play (gravity, trying to open something with fingers), the instability is obvious.
So maybe those on the hypotonic side of things, get more easily recognized as having hEDS/hypermobility.
I must also point out: as I have gotten older, the stiffness has gotten worse and reduced range of motion. If I had been tested even just five years ago – there would have been a very big difference. Imagine as a child, etc.
Also, people with hypotonia can have stiffness in some parts of the body. They are not mutually exclusive. In my father, the osteoarthritis plus stiffness also limits movement. He hyperextends a lot less than in his youth – yet, it still is more than a young non-hypermobile individual (he was on the hypotonia side when younger).
And interestingly, in the homocystinurias, even in the same gene mutation, it presents both as hypotonia in some and hypertonia in others.
I thought this was interesting, given I hear more and more of people with mutations in these genes.
The hypotonia seems to becomes less ‘visible’ with time in some of my family members.
It’s not… full-blown. If the hypertonia were so incredibly bad, one would know already [that when you fall, you fall as a log, for example] Same for the hypotonia. We probably fall not so much on the extremes. That’s why it goes ‘undetected’ for so long.
hEDS / Hypermobilty Spectrum Disorder / Unrecognized Homocystinurias/Unknown defects along the homocystinuria-related genes / a collection of gene defects that together give rise to these conditions
This doesn’t have a name yet – maybe.
I can’t wait for the day studies shed light on this.
As for vasodilation:
last summer, I tried bilberry. I was looking for something to help with the POTS, and this was something that turned up when I was searching herbs not for POTS per se, for blood pooling maybe> ? Can’t remember these things anymore…
It seemed to help. How can I know?
Because I ran out and the POTS got worse.
I was going to order more and then temperatures went down, POTS got better, and then I forgot about it.
I read another person improving POTS symptoms with tart cherry. When I looked up what that contains – it’s the same compound, anthocyanins.
It’s interesting, as I read now the other effects it has been studied for:
lowering glucose and lipids, lowering oxidative stress – which are things that are also wonky around here, yes?
https://www.ncbi.nlm.nih.gov/books/NBK92770/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5613902/
@Meirav, thanks for all the ideas! Worth exploring. EDS is in my family too, on both sides.
I used to take Bilberry too. I stopped for whatever reason. But it helps your eyes if you have poor night vision. They used to give it to pilots to improve their night vision. And it did improve my vision. Thanks for the reminder. Good to know it helps your POTS too! Maybe should try that again. Though my POTS is better these days. Still there, but better.
As for the testing on all the above things you mentioned. A lot of them are done at Mayo in Arizona. They test all sorts of things. But have really good insurance and know you will meet your out of pocket. Because it really expenses. They are good to diagnosis but not for treatment so much. They prefer you find a doc close to you for that. But you get a lot of WHYs.
https://www.imet.ie/imet_documents/BYRON_HYDE_little_red_book.pdf
@issie Please see little red book about ME. It is nothing to do with EDS/CCI Jen Brea was not cured of ME by CCI. THanks
Thing is @Martin, you missed my point……we get labels based on our symptoms. If we have symptoms that fit, they hand us a label. It may or may not be a correct label. But we have to proceed with assuming the label we get is accurate, until proven otherwise. It doesn’t matter if she did or did not have ME. What matters is she got a “Cure” for what made her so dysfunctional for so many years.
The poor woman had a whole lot happen to her. A lot going on. She had mold exposure and found out she had CIRS, I don’t recall about Lyme…..but, I’d guess she checked for it. She found out she had EDS, had to have serious thyroid surgery removal. (That alone can damage vocal cords and do damage to the neck.) She had serious spinal surgery with grueling recovery. She lived in a wheelchair for many, many years and lost a very successful career due to her illness. Look at what all she has gone through, yet she still searched for answers and tried to spread awareness for what she “thought” was “THE” Cause. Now whether it was or not……AGAIN……does NOT matter. What matters is she has her LIFE back. Isn’t that what we all want……to “HAVE A LIFE”?
And despite that, she still tries to spread awareness for something she now says she no longer has symptoms of. Celebrate her life, give her a That-a-Girl! She found what we all search for. I’m soooooo glad she found her “purple bandaid”. And I hope it keeps covering over the booboo.
I’m done now, @Martin…… let you and I go on to find our own “bandaids” and find those WHYs, then WE will celebrate even more so with her!
@issie I feel sorry for Jen Brea but a lot of what you say is whataboutery.
If she had neck problems after thyroid surgery which required CCI surgery then that is nothing to do with her previous ME. I spoke to out ME Association here in the UK about it and they did not really want to comment about Jen Brea I felt but when I pushed them, they wrote back and said in their limited experience, having CCI surgery for ME in the patient(s) they know about, did NOT cure their illness. I believe my ME Association. As I said, you keep talking whataboutery. Jen Brea has damaged the cause of ME now in falsely claiming she was cured of ME by CCI surgery. This is impossible since it is not what the cause of ME is.
Automated Motion Tracking and Data Extraction for Red Blood Cell Biomechanics
https://currentprotocols.onlinelibrary.wiley.com/doi/full/10.1002/cpcy.75
Ron Davis e.a.
Very interesting Cort!!!
http://www.softcellbio.com/about-us/
Soft Cell Biological has developed a patent-pending protocol to culture
and examine hidden bacteria in the circulatory system. Our ultimate goal
is to reveal the link between these bacteria, autoimmune disorders, and
recurrent infection. Preliminary testing reveals that donors suffering
from chronic fatigue, fibromyalgia, arthritis, and anemia carry high
concentrations of L-form bacteria in their blood. Despite the medical
community’s recognition that bodies attack themselves, the source of
this process is mysterious-a source we have potentially discovered. In
lacking cell walls, these bacteria are able to invade red blood cells,
traveling freely throughout the body and eventually taking any cell
within as a host. The ability to culture L-form bacteria from two drops
of blood reveals new avenues toward solving these problems.
(c) 2020 SoftCell Biologicals
This sounds really interesting. However, I can also see some dangers in practical use. Suppose my local surgery got this equipment and started testing people with risk factors for heart problems. People with this subset of ME would come up with a low reading and would be diagnosed as potential risk for heart attack (seeing most GPs would not have the knowledge to realise that people with ME are in a different situation) and would be put on statins!!! Have I understood that correctly? Is there any way for this equipment to differentiate?
Impaired blood rheology has been known for 35 years and discussed between scientists a lot. It is all documented in the book Ramsey’s Disease. Also ME is a specific illness with muscle fatiguability taking days to recover and it runs a chronic course. CFS does not have such a profound if at all muscle fatigability which is why it is pointless calling ME , ME/CFS and likewise CFS ME. The debate has been rearisen about blood flow again after 35 years.= of debate. Perhaps just ME has this phenomenon and CFS is just something else.
So if ME is impaired blood flow through various capillaries giving diverse symptoms in each person, why were we normal once? If we have anatomically smaller capillaries than normal people, why were we normal once? Did the red blood cells just get bigger and less deformable after a viral infection or something?
Or did we have normal diameter capillaries but they got smaller after a viral infection (and red blood cells got bigger) Perhaps this is an interpretation of severity in ME? If only one happens you don’t get so severe as when both happen perhaps?
It sounds plausible. Anyone got any thoughts on whether or not the virus that often leads to M.E causes the vessels to narrow or if we’re born with narrow vessels what triggers the M.E. Also why this would affect more women than men.
In the case of my daughter, narrow vessels run existed beforehand .
A bike courier friend who rides 80 -100km per day put me on to Citrulline Malate. The biking community take it for recovery, I ( 8 1/2 yr ME/CFS sufferer) found it really helps to give a lift and better daily energy; it’s not a fix but due to increasing nitric oxide (NO) it really helps.
Another very interesting reading from this study is that it might confirm the lactic acidosis vicious cycle which it is suspected to be behind many of the symptoms in ME/CFS and the diagnosis of POTS. Mitochondria dysfunction (btw not only in our cells but hypothetically in the microbiom also) leads to this scenario. Hence the blood vessel unification hypothesis is not going to fly as the endothelial dysfunction is just another consequence, not a root cause.
Thanks Hugo. Time will tell. Systrom has found what he believes to be a mitochondrial dysfunction subset.
Is anyone aware of studies or anecdotal evidence of taking isosorbide mononitrate to enhance nitric oxide production in vascular tissue? Isosorbide is vasodialator and used to improve blood flow and often used to “relax” coronary arteries. Many factors contribute to vascular constriction but the results of constriction in heart patients are similar to symptoms of CFS. I only found one reference to use for ME/CFS patients (http://waleshealthcare.com/wp-content/uploads/2017/05/wpr32-2017-mecfs.pdf).
I have had ME/CFS since 2009 after the swinefluepidemic. This spring 2022 did I get microvaskular angina (after covidinfection). The cardiologist gave me Imdur 30 mg and then later 60 mg this fall. I had sudden relief, not only of anginapains, but also in especially my thighs function and endurance. The endurence increased at least by 3-4 times almost over one night, but the pain in my legs are almost the same. I also have shorter period of tiredness after physical activation. Before 3-5 days and now 1-2 days. Even it is not so fun to have angina I´m actually glad to have so I did get this medication. So nitric oxide/endothelium hypothesis can actually be something to follow up for the scientist!