Media Barrage
A veritable avalanche of stories – the C19Recovery Awareness website provides a link to approximately 50 articles since June 1st – have highlighted the problems that many people have had recovering from the coronavirus. With eight stories published in the past four days, they’re still coming at a good clip.
That is all good news. These media reports – some pitched by organizations like Solve ME/CFS and ME Action – are crucial in getting us more support. The U.S., inadvertently, is helping a great deal to keep the story in the news. Six months into the coronavirus pandemic, infections have slowed down markedly in Europe, Asia and Australia but have picked up steam in the U.S., South America and other countries.
The U.S.’s inability to get its act together, as tragic as it is, does present a silver lining: the more people that get infected, the more people will likely have difficulty recovering, and the more people will come down with an ME/CFS-like condition. That’s bad news for them, but it’s good news for everyone saddled with a post-viral illness.
Plus it could be argued that the more people that get sick, the more chance we have of getting the resources to develop treatments that will help them and others get well.
This isn’t, after all, just about Covid-19 or chronic fatigue syndrome (ME/CFS). The insights learned from this research may be able to be applied to every disease that can be triggered by an infection including fibromyalgia, POTS and autoimmune diseases. Potentially millions of people could be helped.
The media is playing a crucial role in getting the COVID-19/ME/CFS link out, but some media stories are better than others. It’s crucial that a link be made between ME/CFS and problems recovering from the virus. The best media stories for us involve people who look like ME/CFS patients; i.e. they are healthy younger or middle-aged people who were never hospitalized and who remain ill several months later. The worst news stories focus on hospitalized patients, who often have underlying conditions and never mention ME/CFS.
A recent New York Times article, “Here’s What Recovery From Covid-19 Looks Like for Many Survivors“, is a case in point. This article focused entirely on people who have been hospitalized and were often frail or sick beforehand. It indirectly implied that only people who have been hospitalized will have trouble recovering from the illness.
Thankfully, most media stories have been much better. Yesterday’s Business Insider story, “Meet the ‘long-haulers’: A growing chorus of coronavirus patients have had symptoms for more than 100 days”, noted that many “long-haulers” are younger and were never hospitalized. Normal blood tests, and tests indicating that they’ve cleared the infection, have left them medical mysteries to the medical profession. While the story does mention infectious mononucleosis, it does not mention ME/CFS.
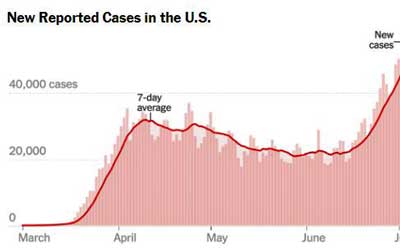
The ever increasing rates of confirmed coronavirus infections in the U.S. have produced a strange silver lining – lots of opportunity for better understanding how postviral illnesses occur.
A recent San Jose Mercury News story, “Living with COVID-19 When It Won’t Go Away“, however, hit all the points. It featured formerly healthy, younger people, mentions chronic fatigue syndrome (“The devastating Chronic Fatigue Syndrome”, in fact), notes that all sorts of people are being affected, and even emphasizes that supremely healthy people have been getting knocked for a loop. It quotes one doctor: “We have people who were world-class athletes who are really incapacitated now compared to what they were before COVID”.
An Atlantic article, “Covid-19 Can Last for Months“, by Ed Yong was near perfect. First it laid to rest the mistaken view that only elderly people or people with preexisting health problems, who ended up requiring oxygen or a ventilator, were having trouble recovering.
Yong focused on the thousands of younger, formerly healthy people flooding Facebook and Slack COVID-19 groups, and noted the similar circumstances that people with ME/CFS/FM and/or POTS had found themselves in. Yong reported how many people have ME/CFS, stated that most are undiagnosed, quoted Jen Brea, and devoted the last half of the article to ME/CFS. He even referred to Dubbo studies.
Our cause is greatly helped when medical professionals and academics speak out, and some are. Many people know about Paul Garner, the infectious disease researcher, who has never been hospitalized, but has been documenting his non-recovery in vivid terms in a blog in the British Medical Journal.
Garner (https://twitter.com/paulgarnerwoof?lang=en) was reluctant at first to say he had an ME/CFS-like condition (he thought he was perhaps still coping with COVID-19) but after several months, this formerly robust academic, runner, and ex-military man acknowledged he has ME/CFS – and even blasted the UK for not updating its NICE guidelines on ME/CFS for 13 years. It was unsettling, but also validating, to see this respected professional describe his difficulty pacing amid the shifting sands and new symptoms showing up in his perplexing illness.
Dr. Scott Krakauer, a psychiatrist, recently described his long trial with COVID-19 three days ago on Today. His doctor believes Krakauer is suffering from an ongoing immune response. He noted the many symptoms he’s seen from his many COVID-19 patients who remain unwell and even mentioned post-exertional malaise. He also highlighted ME/CFS.
A news story on Yahoo from “The Mighty Staff”, “COVID-19 May Cause Hallmark ME/CFS Post-Exertional Malaise“, explicitly linked the PEM in COVID-19 to ME/CFS and then followed that up with a nice description:
“This fatigue I’m talking about, which isn’t just feeling tired or sleepy, but like there’s no bones in my body and gravity is pushing down extra hard on me, to the point that I can’t lift my arms above my head.” — Heather Hogan
Other themes familiar to people with ME/CFS are cropping in: the dismissal by doctors, the psychologizing, the suggestions to exercise more. Because of its multi-faceted presentation, ME/CFS has been called the disease of a thousand faces. Recently, post-COVID-19 was referred to in a similar manner.
“This disease, it has many faces, and we’re just starting to scratch the surface of what convalescence is like,” Dr. Reynold Panettieri Jr., a pulmonary critical care physician and director of the Rutgers Institute for Translational Medicine and Science reported in a story four days ago in the Chicago Tribune. Panettieiri reported that many people having trouble recovering are younger, some are athletes, and major underlying medical conditions can’t explain their illness.
Major Health Organizations Not Getting It Yet
With all this media coverage, it’s somewhat surprising (or is it?) that the really big health organizations have uttered nary a word about problematic recoveries. The only “long-haulers” the CDC appears to provide support for on their website are truck drivers.
So far as I could tell, neither the CDC nor the World Health Organization (WHO) websites mention the problem of long-term recoveries or chronic illnesses on their websites. The most Dr. Maria Van Kerkhove, the technical lead for the WHO’s pandemic response, could muster up during a press call last week was: “They may feel quite fatigued for some time”.
Fatigue, though, can hardly describe the utter exhaustion that many feel. Three months after one 27-year-old became ill, she reported that just in the past couple of weeks has she been able to get from her bedroom to the living room.
Another fit, healthy 32-year-old, reported: “I’ve been reduced to not being able to stand up in the shower without feeling fatigued. I’ve tried going to the supermarket and I’m in bed for days afterwards.”
Why Anthony Fauci is not using the threat of long COVID-19 recovery times to get younger people to practice more social distancing and mask wearing is a mystery to me.
Update 7/9/2020 – A couple of days later at a news conference organized by the International AIDS Society Anthony Fauci did indeed refer to both a post-COVID post-viral syndrome, and to myalgic encephalomyelitis.
“There may well be a post-viral syndrome associated with Covid-19, If you look anecdotally, there is no question that there are a considerable number of individuals who have a post-viral syndrome that in many respects incapacitates them for weeks and weeks following so-called recovery. There are chat groups that you just click on and see people who recovered that really do not get back to normal,”
Fauci also reportedly said the symptoms (brain fog, difficulty concentrating and fatigue) resemble those seen in patients with myalgic encephalomyelitis, or ME, once known as chronic fatigue syndrome.
And what about Francis Collins? Now referred to as “Anthony Fauci’s boss” Collins just participated in an excellent and lengthy interview on the coronavirus in the New York Magazine. His thoughts on the vaccine situation were fascinating. A public statement on the “long-hauler” situation, though, would be helpful.
Familiar Hypotheses Popping Up
Several hypotheses that have been put forward to explain why ME/CFS and fibromyalgia (immune activation, dysautonomia, small nerve fiber problems) are starting to show up for COVID-19 survivors.
Some believe the virus may still be present but is undetectable. Others believe the virus has unleashed a devastating immune response or has discombobulated the immune system in some way. My favorite is that the virus has damaged the autonomic nervous system.
Dr. Putrino of the Mount Sinai Health Center believes 5% to 15% of all COVID-19 patients may suffer from dysautonomia. Serena S. Spudich, chief of neuroinfectious diseases at Yale, believes the small nerve fibers in the skin and elsewhere, that relay sensory and autonomic signals, have been affected in somme people. She’s launching a long-term study that’s following COVID-19 patients with neurological problems.
Post COVID-19 Studies
“The more we learn about coronavirus, the weirder it gets” Tim Spector – COVID Symptom Study Lead
A major stumbling block for us right now is the lack of hard data. We’re swimming in anecdotal stories with little hard data available on prevalence, illness state, etc. Some major studies are underway, though.
The COVID Symptom Study, created by Harvard, Kings College and Stanford researchers, which is following 4 million people, reported that ten percent of people with COVID-19 are still sick three weeks later. They reported that “people with mild cases of the disease are more likely to have a variety of strange symptoms that come and go over a more extended period. The Symptom Study lead, Professor Tim Spector of Kings College, stated that: “the more we learn about coronavirus, the weirder it gets”.
Two Large NIH Studies Provide Hope

The LIINC study has already collected 1000’s of samples. It’s early findings are not unlike those found in ME/CFS.
Two major studies following the trajectories of COVID-19 patients are thankfully underway. While they don’t include ME/CFS, they are big well-funded studies at reputable institutions. Dramatic increases in understanding what happens to turn an infection into a chronic illness should be expected.
The Longitudinal Immunological Impact study taking place at the University of California San Francisco is taking a deep dive into the immune systems of COVID-19 patients. The Mercury News reported that the two-year study has already banked thousands of vials of immune cells, plasma serum and saliva specimens and shared them with 12 different research teams.
Thus far, the 2-year T-cell and immune study is producing findings that generally align with what we suspect in ME/CFS: T-cell depletion, signs of immune exhaustion and increased levels of pro-inflammatory cytokines. The researchers appear to be well acquainted with ME/CFS.
Huge NIH Immune Study Underway – A National Institutes of Allergy and Infectious Diseases (NIAID) study that will track at least 1,000 COVID-19 patients will assess their immune responses, their viral loads and do a variety of multi-omic assessments. They hope to provide “deep insights into how infection by SARS-CoV-2” produces disease-perturbed networks”. This study will establish high quality biorepositories and is projected to end in 2022.
We need more – we need studies that assess brain functioning, autonomic nervous system functioning and exercise capacity.

The fact that the NIH has funded Nath’s Covid-19 study appears to suggests this ME/CFS study has gone well.
Avindra Nath’s Intensive COVID-19 NIH Study while small – just 40 people, is going to partially fill that bill. Nath’s small study is intriguing in a couple of ways. For one, the week long intensive study is going to piggyback on what’s he’s learned during his even more intensive two-week long ME/CFS intramural study.
We haven’t heard much about what Nath’s found in the ME/CFS study, but since he had to use the results from that study to get the NIH to fund the COVID-19 study, he’s clearly found enough to get the NIH interested in doing a similar COVID-19 study. That intensive study was projected to provide a kind of Rosetta stone for future work on ME/CFS at the NIH. Perhaps it’s working out…
Five Year NIH Study – Although I couldn’t find it in the NIH Reporter site, the NIH is reportedly launching a platform to collect COVID-19 patient data “including demographics, symptoms, medications, lab test results, and outcome data over a five-year period.”
Open Medicine Funded Stanford/Harvard COVID-19 studies – will seek to get at the molecular changes underpinning the shift that occurs as COVID-19 patients fail to recover.
Uppsala COVID-19 Center Study – Jonas Bergquist of the Uppsala ME/CFS Research Center is engaged in a long-term effort to monitor the sickest COVID-19 patients “who require(d) the most advanced intensive care” from neurointensive care units. It should be noted that people this sick – people who may have organ damage or terribly low oxygen levels or who have been on ventilators – start off their COVID recovery periods with problems which few people with ME/CFS have. Studies show, for instance, that people put on ventilators often have long-term health problems. Since the researchers are looking for the same neuroinflammatory markers and nerve cell markers they’ve found in ME/CFS, though, finding those in these very sick patients could be significant indeed.
Huge U.K.COVID-19 Followup Study Will Likely Not Help – The U.K. kind of stuck its head in the sand when it decided that its 10,000 person Post-Hospitalisation COVID-19 Study (PHOSP-COVID) will only study hospitalized patients. Applauding the creation of the study Health Minister Matt Hancock stated “we should also look at how COVID-19 impacts on the health of people after they have recovered from the immediate disease”. Let’s hope he means what he says, and the U.K. will follow up with another study of non-hospitalized patients.
COVID-19 Tracking Studies and Patient Registries – Our Tickets to Better Funding?
A hugely promising development concerns the appearance of COVID-19 registries that will track patients over time. If this all works out we should have mountains of data on the prevalence of post-viral illnesses after COVID-19.
More importantly for us, if the coronavirus pandemic does create a large cohort of people with an ME/CFS/FM-like illness, these registries could be invaluable in helping us validate the need for more funding. After all, after six months, many of these patients will presumably fit the criteria for ME/CFS. Researchers, the medical profession and the public will know that post-infectious ME/CFS is a serious illness.
Solve ME/CFS Patient Registry – has integrated a COVID-19 questionnaire to track the impact of COVID-19 on the health of people with pre-existing ME/CFS. Solve ME/CFS has also initiated partnerships with established COVID-19 registries and apps to include questions that ask participants whether they have developed post-viral ME/CFS-like symptoms. If they answer yes, they will be referred to You + M.E. so they can provide more comprehensive information.
HERO ( Healthcare Worker Exposure Response & Outcomes) – Duke University is following 15,000 health care workers (600 have died of the virus). The goal is to follow 100,000 people and the projected duration of the study is, get this, up to 79 years :). Does it get any better than having health care workers – so often our bane – validate the seriousness of post-viral illnesses (i.e. ME/CFS). (And what better allies to have?)
Stanford COVID-19 Registry – is open to people who have tested positive or negative for COVID-19, people who may have or had COVID-19, people who do not have or never had symptoms of COVID-19: i.e. it’s open to just about everyone!
The Center for Post-Covid Care – the Mount Sinai Health System in New York City is monitoring about 1,000 post COVID-19 patients who had mild to moderate initial symptoms.
Others
- American Heart Association – COVID-19 Registry – focused on heart issues in COVID-19 patients
- COVID-19 Registry
- American Society for Microbiology Registry
- ACR Covid-19 Brain Imaging Registry
Resources
- The Center for Post-Covid Care – the first Center devoted entirely to post Covid-19 patients has opened at the Mount Sinai Health System in New York City. Hopefully we will see more Centers opening up.
- COVID-19 Recovery Awareness – provides regular updates on media articles
- Body Politic – COVID-19 Support Group
Conclusion
The media interest is there – and a follow up blog will show that it’s producing results for us. Two big longitudinal immune-based and “omics” NIH studies, and a smaller but intensive study featuring Avindra Nath, plus the OMF-funded Stanford and Harvard “omics” studies provide cause to hope that we may finally be able to catch ME/CFS in the act during that crucial period when an infection somehow devolves into a life-long illness.
They are a good start. We need more and we will hopefully get them as some of the 25 CMDRP grant applications get funded and as more NIH grants get funded as well. One would hope and expect that a well-funded Request for Applications (RFA) grant opportunity to study the long-term affects of COVID-19 will pop up soon at the NIH.
The birth of numerous COVID-19 registries and tracking efforts provides hope that the extent and seriousness of post-viral illnesses such as ME/CFS will finally hit home in the medical community. It’ll be interesting to see if, after six months, the still ill post-COVID-19 patients are given an ME/CFS diagnosis.
Plus, the post COVID-19 issues are already opening new doors in one area that could benefit us greatly – in Congress. A blog on that is coming up shortly.







I’ve had ME/CFS + POTS for 23 years and Fibro thru my lifetime (65 years), which has been life changing. But it’s been getting dx. with a “mild” case of probable covid-19 back in March with no end in sight that has been really horrible. Never went to ER as I didn’t need to be vented. But it’s been hell. I am a member of the Facebook’s Long Haulers group and the posts there are so much like what we all see in the ME/CFS groups. I can’t quite finish reading this article nor finish posting this. My body is done, my brain is done, my lungs are done. Make lots of noise 4 me cause I can’t.
So sorry to hear Donna that COVID-19 has made things so much worse. Thanks for relaying what’s been happening in those groups. I haven’t gotten on one yet.
Hang in there. Let’s hope that the work on COVID-19 opens new insights (I would be shocked if it didn’t) and new treatment possibilities. Its a shame that so many people have to get sick for the medical community to take note but hopefully this is the darkness before the dawn.
I think you’ll be happy at all the noise that’s being made. I’ll cover that in the next blog.
Take care.
I wonder are these post Covid patients that have been cleared of lung damage yet say they are short of breath actually do have ME/CFS and are experiencing ‘air hunger’ that many of us ME/CFS patients have? I hope that the Covid researchers realise air hunger and shortness of breath are a symptom of ME/CFS as i imagine many will dismiss it, and assume its some sort of lung damage that can’t be seen or tested for.
The problem is many Covid patients will have lung damage and the reporting by patients of air hunger will automatically put them in the lung damage category. Which will be disastrous if they actually have ME/CFS Instead because I bet the therapy for repairing the lungs will involve a lot of exercises. Which will worsen the condition of the ME/CFS group. Avoiding misdiagnosis here will be crucial
Good point!!!
Interesting. I don’t know if it is documented or not but I have fibromyalgia and for years I’ve had issues with breathlessness as well. I feel my doctors dismiss many of the symptoms I have and this us one of them. Maybe I have a milder form if chronic fatigue as well? Or is it definitely a symptom of fibromyalgia as well.
Just so tired of doctors dismissing all of a patients symptoms, which could by a big part of solving some of the mysteries of fibromyalgia and finding a cure or answers.
Sincerely
M.Y.
I think that’s a very interesting and possibly fruitful intersection and a reason it’s very good that the two Ron’s – Ron Davis and Ron Tompkins – are leading their own COVID-19 studies. For me it presents the possibility of finally understanding what’s producing the air hunger in ME/CFS. Air hunger in COVID-19 is interesting as it doesn’t always manifest when blood oxygen levels are low. On the other hand it appears to be present in ME/CFS without low blood oxygen levels. It’s certainly a good reason for ME/CFS experts to be in touch with these studies. I had the impression, but am not sure, that the LINC study researchers were quite acquainted with ME/CFS.
I’m 3 months past the 4 weeks of what I’m supposing was the active infection phase of covid-19, based on the symptoms before versus after. I was never hospitalised and didn’t even have as bad symptoms as some others who resolve at home, but I’m still having brain fog, fatigue and mood swings that have prevented me from working from home yet, as well as some phenomena that are clearly related but not causing impairment or bothering me much. Even though I still have the mild burning, itching and aching sensations I’d never experienced prior to covid-19, deep in my chest for minutes at a time on an almost daily basis, I’m only having air hunger or shortness of breath beyond what is typical of my asthma during the occasional heatwave-induced flare ups of the cough and varied and distinctive other symptoms that I had in those first 4 weeks (the debilitating hypoxic, top of a mountain feeling, very different to air hunger or dizziness/fainting from other causes, has never returned, thankfully). The rest of the time it feels like all sorts of strange things are happening in my lungs but with little or no breathing impairment that I notice – though of course I’m getting very little exercise and not even talking much so I don’t test my lung capacity much. My best guess has been that those sensations are caused by minor scar tissue being reacted to by my immune system. I’ve stopped worrying that I’m infectious again every time it happens, but the reactivation theory has me concerned I need to stop having visitors every time this happens.
Governments in the US and the UK are more concerned about restarting the economy than they are about how many people get the virus. People are not going to go out and spend money if they realise just how sick they may get, therefore it’s something no-one wants to talk about.
Many people want to “get back to normal” and dont want to hear about the risks. The young always think it wont happen to them and in America anyone who is white wants to think it only happens to people of colour.
The rich think they can avoid the virus while sending the poorer people out to make money for them. They forget that their lives actually require people to collect their garbage, bring their food and so on. Also that if they allow their medical staff to die and their hospitals to be overwhelmed there is no-one to treat them when they get sick from something else.
I want our economy to pick up too – but I’m not willing to lie to people about the risks to get there. Everyone needs to be doing anything they can to keep the risks down because the more the virus is allowed to run riot the more people will stop spending.
I know this is highly political in America – but in a pandemic you need health care available for everyone and you need people to be able to stay home when sick, whatever you do the rest of the time. You didnt need a president who tried to dismiss the whole thing.
For anyone who has not got one – get an oximeter. This virus produces “happy hypnoxics” – people who dont realise how bad their oxygen levels are and that they should be in ER. If possible you avoid ventilation but you may need oxygen delivered in a less invasive way.
“They may feel quite fatigued for some time”. The CDC and WHO officials should stop using the word “fatigue” when referring to post-exertional malaise. It’s not “fatigue” if it’s a life-long condition. It’s not fatigue if it’s ME/CFS.
I have been part of the UK Covid 19 study for about 5 weeks now and report daily. Within a day of reporting any symptom like a sore throat and extra fatigue I will get a request to have a test and then once this has been done I report the date of the test and the result via my phone.
Because of this I have had 2 tests and both as I had expected were negative. I think in both cases I had another short-lived virus which at the time made me feel terrible but it is a comfort to know that I will definitely be tested.
It’s an excellent way to document people’s symptoms on a daily basis and so easy to do. There are many explanatory videos to update the group’s findings so I thoroughly recommend doing this especially for people with ME/CFS.
Nice! Good for the UK COVID-19 study. We don’t know what you had but how strange it is that a) we don’t know the false negative rate for tests in the U.S. anyway and b) that from what I hear it’s quite high…How this has not been fixed I don’t know.
For any UK readers who still don’t know about it, this is the Covid-19 Symptom Tracker study using a smartphone app to report symptoms daily, with around 4 million people now signed up — but still lacking participants in the 65+ age group, ie those most vulnerable to infection by reason of age.
The study is headed and run by a health science company ZOEglobal, set up by Prof Tim Spector of University College London (UCL), where he is Professor of global epidemiology (in the UK, a professor is a very senior, tenured academic — usually heads of department who rank above lecturers and senior lecturers who in the US are referred to as “professors”).
I started to report daily from early April but got very fed up with the difficulty of slotting into a badly drafted questionnaire which had no response in between the two options of “mildly fatigued” and “exhausted”. This failed to recognise that for anyone with ME/CFS/FM the norm was likely to be “exhausted”, or “more exhausted than usual”.
As I am 78 & have CFS/FM for 18 years, the daily struggle over how to answer this git too much forme after a couple of weeks, and I stopped reporting — despite the acute shortage of respondents in the 70-80 age group.
But I was interested to notice that my temperature was consistently below –or very below — normal, just it had been 17 years ago when I kept a Barnes Thyroid Temperature chart (given to me by a chiropractor) for a year: and my basal temperature reached normal only once, on the hottest day of the year.
NHS doctors routinely rejected the Barnes chart and any suggestion I might be hypothyroid, despite my having all the clinical symptoms except weight gain: their cheap and misleading TSH blood test trumped any clinical signs and, because flouting British Medical Association Guidelines meant malpractice hearings and being struck off the medical register, I got no treatment — as I couldn’t afford private treatment by GPs more willing to take a risk.
I read a long time ago that 40% of ME/CFS/FMS patients are hypothyroid but usually undiagnosed — in the UK at least. Regardless, the low metabolic rate fits the “hibernation” model I read about in the HealthRising blog some time ago now. My chiropractor also told me that dysfunction in any one endocrine organ generally meant disruption of the whole endocrine system: and I later read about disruption of Hypothalamic-Pituitary-Adrenal (HPA) axis as being typical of chronic insomnia, as another characteristic symptom of ME/CFS/FMS. So stress would appear to play a significant part in overall muscle tension and pain, leading to central sensitisation to pain.
There is also convincing evidence (assembled by Martin Pall) of head and neck trauma as the “trigger” most often associated with the onset of FMS as a diagnosis distinct from ME or CFS as conditions with almost entirely overlapping symptoms. And in my case, I would say there is a strong element of PTSD — starting with a road accident aged four that damaged my left foot, apparently leading to a host of musculoskeletal imbalances underlying muscular tension caused by the unremitting stress of being brought up by two narcissistic parents.
So viral infection — starting with “rheumatic fever” / Chorea aged nine or ten — might just have thrown in damage to my immune system too: it’s popularly called “St Vitus Dance” due to involuntary muscular tics — which can be huge spasms and jerks.
I find that the better I get at relaxing (an extremely difficult task, from a rigid numbed-out state) the more violently varous bits of me flail around, at first always involving my left ankle, and with progressive left-side involvement. Apart from my right arm and shoulder.
So I regard my own FMS as having a variety of interlocking causes, with different treatments appropriate to each. For the PTSD components (including other scenarios later in life) I am hoping that EFT — Emotional Freedom Technique — will be fairly transformative: and Alexander Technique has been so far the best re-education of my unbalanced, stress-laden muscular habits.
There are other things too: I am electrosensitive. That means no more wifi, only wired connections — and, if I can manage it, giving up my mobile phone. After recently switching off my wifi router and using a new air purifier and ioniser, I had a single exhilarating day of extraordinary energy followed by no sleep, and the predictable crash, with zero energy since. But then I discovered the ioniser was completely DAB radio signals: so I’ve had to switch that off too.
PS meant to say I found the ioniser was completely blocking DAB radio signals — so I had to switch off the ioniser too, as an extra source of radiation.
Funny about the dexamethasone in the video. Accidentally, I had dex shot for rhinitis in the States when I had ME ongoing symptoms and it produced a severe fatigue on me for 6 weeks. Then years later after I had recovered mostly from ME, I had another dex shot for rhinitis again but that time I did not have a set back of fatigue. Why that is for both times I have no idea but it is interesting.
Our family of three are in a fix. My 27 year old son has had severe ME/CFS, needing care for 4 years. My husband and I had probable COVID-19 in early March and we are definitely long haulers. Even small exertions knock us right off our feet again. Our symptoms are very similar to our son’s although we do have more energy than he does. Boom and bust is a thing, and we are pacing very carefully. I was interested in the air hungry ness as I hadn’t heard of that. I think I have it, although I didn’t have trouble breathing during the intitial bout of COVID. We have tested negative a couple of months after the initial infection…on one of the occasions when it came back like being hit by a train. My son also has had COVID I think, and he is a step down from where he was. He could occasionally enjoy a board game or sit in a cafe (if driven there’s. He is housebound now and cannot manage social interaction. My husband and I are also filling in the COVID UK study daily, so we hope to add to those statistics which will push on ME/CFS research. The fact that we all have fatigue now does Indicate genetics as a factor. Please excuse the long ramble. Thank you very much Cort, for these links
I’m so sorry to hear about your tough situation, Nicky.
Has anyone listened to the interview with Professor Danny Altman, professor of immunology? It makes me so sad as nearly everything he says in the interview in the U.K. Guardian on ‘Covod19 Why are people suffering long term symptoms’ sounds just like us. What makes me sad is it takes a whole pandemic to get more interest and also that he has to say this is a real thing. And yet I am hopeful that maybe, as your article suggests, there might finally be some leap of progress in medical understanding and even treatment for us as a community as well as increased medical literacy amongst more doctors
@Alison The reason why people are suffering long term symptoms after COVID19 is that their HPA axis is hit. Viruses can knock the thyroid or HPA axis back and this is what causes fatigue in ME/CFS. I had a shot of dexamethasone then I had ME/CFS bad and it made an incredibly awful fatigue for six months. However, after I had recovered from ME/CFS, I had another dexamsthasone shot for rhinitis again and that time I did NOT suffer a relapse. So I have proven that fatigue in ME/CFS is caused by hypersuppression of the HPA axis. This is what is happening in COVID19.
I have just read in “Regenerate” by Sayer Ji (who set up GreenMedInfo.com) that corticosteroid inhalants for asthma (caused by allergic rhinitis) hit the adrenals — so it’s odd that your second dexamethasone shot didn’t have the same effect as the first, re link between HPA axis and chronic fatigue.
Dexamethasone is a steroid to reduce inflammation. I think steroids are given to people who get bad cases of mono as well. Wonder if the steroid I received for mono helped push me into cfs.
Thank you, Cort as always for an interesting and informative Article on the happenings going on! As I am still am here watching ..
Seems Leronlimab and Lenzilumab is on Center Stage in quelling the Cytokines Storms..so watching and keeping all the hope that it just might be help for us soon as well..if..Research paths similaries wil/should or maybe be combined and used soon! At very least a peek at it.. Fingers crossed as well as toes..Ouch..lol! THAT IS A Big, If!
I think our chance is that post-covid patients are mostly middle-aged men (versus female teenagers developing ME/CFS after mono). The default mindset is that men are to be believed when they describe their symptoms whereas females are easily labelled as neurotic, hysteric, etc. Perhaps progress will be made.
And then a part of me believes that many post-covid patients will be sent to infectious diseases specialists who always refused to hear anything about ME/CFS, who will google ‘CFS’ and who will read about the PACE trial… And then here we go again with Groundhog Day…
Cort, you might be interested in this article: https://www.theguardian.com/world/2020/jul/08/warning-of-serious-brain-disorders-in-people-with-mild-covid-symptoms
Kind regards,
Thanks!
Here’s another article on LongCOVID – https://sszeemedia.com/2020/07/12/the-long-and-difficult-road-to-recovery-why-coronavirus-isnt-always-over-in-a-fortnight/
prusty posted this in twitter
https://www.neurologyadvisor.com/topics/general-neurology/chronic-fatigue-syndrome-viruses-and-the-innate-immune-system/
Wow, that was interesting. Thanks, Linda!
I’m in the Covid Long Haulers Slack group. I have been sick since March 13. I live in NYC so I was unable to get tested when I was initially sick. I tried repeatedly. Now I test negative for antibodies (the antibody tests are not accurate), many of the Covid long haulers are I the same predicament as me. Without a positive test or a positive antibody test I cannot go to the Mount Sinai Center and my doctors have not taken me seriously. I am one of the many who have been told that it’s all in my head or chalked up to psychological issues. I have pre existing medical conditions so the doctors also like to blame everything on these conditions, despite that the symptoms were all new. It’s a baffling and horrible sickness. Also like many in the group, all the tests my doctors have done have not found anything. I too have SOB but without any depletion to my oxygen levels and without any lung damage.
Women are often ignored and dismissed in a medical system whose illness models and test subjects are overwhelmingly male. You might bring to the attention of your dismissive doctors a report just published in the UK called “First Do No Harm”, the findings of a committee headed by Baroness Julia Cumberlege, concerning the routine dismissal of suffering by women from vaginal mesh implants, and birth defects, autism and epilepsy caused by a hormone pregnancy test known to cause harm yet still prescribed without informing women of its dangers. This has provoked outrage — and apologies from the Secretary of State for Health & Social Care, and from the National Health Service, with undertakings that women MUST be listened to and taken seriously.
I’m so sorry to hear what you are going through, Emily.
Poor Richard Quest, the CNN reporter, has not been able to get well from COVID-19, either.
https://www.cnn.com/2020/07/07/health/richard-quest-covid-wellness-intl/index.html