

Using magnetic fields to treat the brain sounds more than a bit woo-woo. The brain, though, is an electrical organ. Our central nervous system uses tiny bits of electricity – electrons – to send signals whizzing around the brain, and electrons in turn create magnetic fields, which in turn, can alter electrical currents.
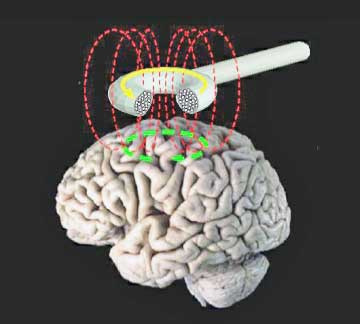
Transcranial magnetic stimulation (TMS or repetitive magnetic stimulation – rTMS) produces brief magnetic pulses which alter the electrical currents in the brain. At first TMS was used in behavioral disorders like depression, but over time it’s come to be used in other central nervous system disorders.
TMS has been used to reduce depression and fatigue in multiple sclerosis and TMS significantly reduced episodes of “freezing” in which people with Parkinson’s Disease find them themselves unable to move. TMS appeared to be able to do this by increasing connectivity between the supplementary motor (e.g. movement) area and other parts of the brain.
Studies suggest that increased activity in the dorsolateral prefrontal cortex and orbitofrontal cortices is associated with increased pain. As the prefrontal cortex is a higher brain organ and is the seat of executive functioning (i.e. rational thought, planning, creativity, working memory, etc.), it seems surprising that increased activity there would result in more rather than less pain.
The brain is a complex organ, however, and the dorsolateral prefrontal cortex (DLPFC) is not only involved in pain control but also pain detection. Activity in the left side of the DLPFC has been associated with increased sensations of the unpleasantness side of pain. (The sensation of pain unpleasantness is distinct from the sensation of pain.) Increased DLFPC activity has also been associated with allodynia – a common problem in FM.
It’s possible that both pain activation and pain inhibition are regulated by the DLPFC. Activating one DLPFC circuit appears to result in increased pain catastrophizing and an intensification of pain, while activating another circuit results in increased pain control and reduced pain.
The Fibromyalgia TMS Study
Repetitive transcranial magnetic stimulation of the prefrontal cortex for fibromyalgia syndrome: a randomised controlled trial with 6-months follow up Suman Tanwar, DOI: 10.1186/s42358-020-00135-7
Low or high frequency TMS can be used. While low frequency TMS generally results in reduced brain activity, high frequency TMS produces increased brain activity.
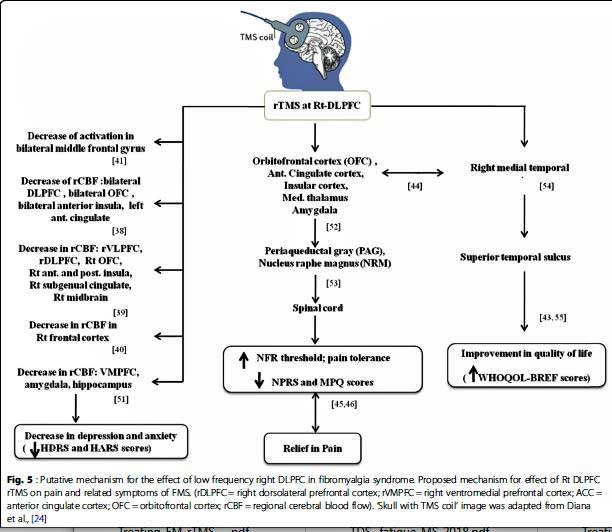
Figuring that the DLPFC in FM patients’ brains were already too active, this fibromyalgia study used low frequency TMS. It was hoped that calming the fires in the DLPFC would translate into reduced activity in other brain organs involved in pain production including the thalamus, brainstem, insular and cingulate cortices.
TMS was delivered over the right DLPFC of 45 FM patients for 27 minutes a day for 5 consecutive days/weekly for 4 weeks. (A sham TMS protocol was delivered to 45 more FM patients.) The patients were followed for a full six months – an exceptionally long time for a study like this – to see if the effects were long lasting.
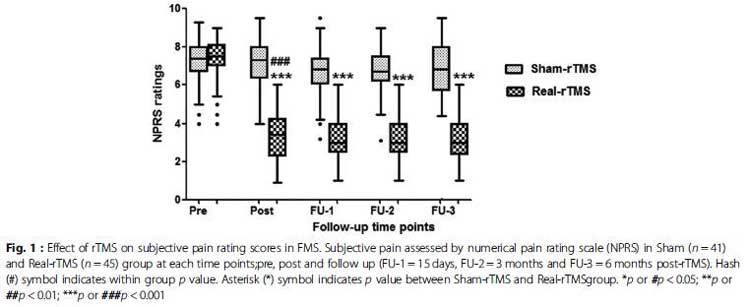
The primary outcome of the study was something called the Numerical Pain Rating Scale (NPRS) which assesses pain on a 1-10 scale (1=no pain; 10=worst possible pain).
Results
Using a magnet to calm the electrical signals in the DLPFC worked. The FM patients getting the electrical signals in their brains gently rearranged received quite significant pain benefits.
At the beginning of the study, both the sham TMS and the real TMS participants rated their pain at about a dauntingly high 7.5/10. From there the pain levels of the two groups diverged markedly. Those given the real TMS rated their pain at approximately a 3/10 while those given the sham TMS dropped a bit but still remained high (@ 7/10). Remarkably, the pain levels of those given the real TMS treatment remained low six months after the treatments had ended.
Pain-related depression and anxiety were also significantly reduced in those given the real TMS treatments.
Objective Evidence of Reduced Pain Sensitivity
The researchers also provided an objective assessment of pain using something called the nociceptive flexion response (NFR). There’s no other way to objectively assess pain without causing it, and that’s just what they did.
NFR is assessed by electrically stimulating a nerve in the biceps femoris muscle in the thigh. The test assessed the degree to which that muscle jumps in response to the painful stimulation. The magnitude of the reflex is related to the intensity of the pain evoked.
The researchers only did this test once 15 days after the TMS sessions had concluded. The biceps muscle of those getting the real TMS treatment was much less sensitive to the electrical stimulation (i.e. jumped at a higher level of stimulation.)
Treatment Takeaways
- Transcranial magnetic stimulation (TMS or rTMS) is a way of using a magnetic coil to alter the electrical impulses – aka the activity of the brain.
- TMS was first attempted in depression, but is now being tried in a variety of other illnesses including chronic pain states such as neuropathic pain, migraine and fibromyalgia as well as multiple sclerosis and Parkinson’s disease.
- This study used low frequency TMS to calm down the activity of the right dorsolateral prefrontal cortex – an area of the brain which has been associated with chronic pain.
- They hoped that calming down this area of the brain would calm down pain producing areas of the brain known to be upregulated in FM such as the insula and anterior cingulate cortex.
- Half of the participants received TMS five days a week for a month for about 30 minutes at a time. The other half of the participants received a sham treatment. They were then tracked for an unusually long period of time – six months.
- The study found that the FM patients getting the TMS treatment were in significantly less pain – dropping from about 7.5 on a pain scale to about a 3.5 throughout the six month study period. They also reported less depression and anxiety. Those getting the sham treatment remained about the same.
- The study also used an objective test using electrical currents to show that the FM patient’s pain producing system had calmed down.
- TMS results in FM have been mixed, with more studies showing positive effects. The variety of approaches the studies have used (low vs high frequency, aiming the TMS at different parts of the brain) have made it difficult to derive conclusions regarding the treatment’s effectiveness.
- A recent overview, however, stated there was probable efficacy for using high frequency rTMS on the left M1 (motor cortex) or left DLPFC in fibromyalgia. (This study used low frequency on the right DLPFC).
- Insurance reportedly does not cover TMS for fibromyalgia.
- Next up – could TMS help with the fatigue in FM or ME/CFS?
Nobody is exactly sure how TMS does what it does, but the authors believed the stimulation probably reduced blood flows between regions of the brain involved in producing pain. Several studies have found increased connectivity between the pain producing regions of the brain in FM.
According to Clinicaltrials.gov, eight studies assessing the effectiveness of TMS in FM are underway: four in Brazil (!), two in Spain and Israel, and one in the U.S., in Charleston, Mass.
Unfortunately, while TMS Advantage website recommends TMS for FM, it states that insurance does not cover TMS for fibromyalgia.
This study was noteworthy because it suggested that the effects of TMS, if done intensively over a month or so, may be long lasting – something the insurance companies might find helpful.
Field in Flux
Of the 10 TMS randomized control trials in FM (including this latest one), seven have had positive results. A 2017 meta-analysis, however, did not find that rTMS produced clinically meaningful reductions in pain. A 2016 meta-analysis found significant improvements in quality of life and a trend toward reducing pain. That review highlighted a key issue: the need to determine “optimal treatment protocols.”
The field is plagued by an abundance of variability. Studies have not consistently used the same frequency or aimed at the same areas of the brain. In contrast to this recent study, most studies have used high-frequency or stimulating TMS aimed at different areas of the brain such as the motor cortex or the left dorsolateral prefrontal cortex (DLPFC) (three studies).
The last FM study to employ the kind of low frequency stimulation used in this current study occurred in 2013. It produced significant reduction in pain thresholds, increased ability to perform daily activities, decreased perceived chronic pain and increased sleep quality.
Another approach concerns the use of multi-coil (as opposed to single-coil) magnetic stimulation to reach the deeper parts of the brain. A 2013 study found this approach significantly reduced pain for at least four weeks following the 20 rTMS sessions.
A European Commission recently published “Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS)” on a variety of conditions. They concluded that there was Level B evidence (of probable efficacy) for using high frequency rTMS on the left M1 (motor cortex) or DLPFC in fibromyalgia.
It should be noted that rTMS or TMS is just one of several non-invasive stimulatory techniques being attempted. Others include transcutaneous electrical nerve stimulation (TENS), transcranial direct current stimulation (tDCS), remote electrical neuromodulation (REN) and vagus nerve stimulation (VNS).
With brain stimulation techniques becoming more refined, and with the NIH’s SPARC initiative (Stimulating Peripheral Activity to Relieve Conditions) taking a deep dive into the nerves in the bod, it’s possible that over time we will see more and more effective ways of non-invasively and safely modulating the bodies electrical fields for better health.
This study suggested that TMS can significantly reduce pain as well as anxiety and depression – but what about fatigue? If TMS can reduce pain in some people, could it also affect the fatigue in ME/CFS and other diseases? A blog on that is coming up shortly.
Health Rising is a Community Supported Website
Your Support Keeps HR on the Web






Quite a number of chemicals can occupy receptors for far too long. Quinolinic acid for example can stick far too long to the NMDA receptors before releasing. That over-stimulates the brain on a near chronic base. Too much quinolinic acid is said to trigger a self reinforcing effect of producing more quinolinic acid entrenching the problem.
Now if a comparable chemical would stick far too long to a certain receptor AND be magnetic or charged or polarized to some extend, strong enough magnetic pulses could kick them away from occupying that position and restoring normal function for quite some time.
Ions (charged molecules) sticking to receptors or polarized molecules sticking to receptors might play an important role in our diseases if that were at play. Maybe even unstable metal chelators could do the trick as they work by charge too. That might narrow the hunt.
I had TMS 6 or 7 yrs ago for almost 2 months and it did NOTHING for me. Don’t know if it was high or low frequency. Afterwards they told me “it doesn’t work in the type of depression you have.” WHY didn’t they figure that out ahead of time and save me all the traveling back and forth and pain? YES, the procedure IS painful, which they did NOT tell me ahead of time. They did talk therapy during it which was actually rather helpful. I was severely depressed and had just been hospitalized for suicidal ideation. That’s when I first learned about cognitive behavior therapy and dialectical behavior therapy. I did a long course in CBT (group therapy, which I really don’t care for much.) I have a real hard time hearing other’s problems. I can only handle so much…
And yes, it was covered by our insurance. I wasn’t monitoring my pain levels, but my constant achiness is NOT too bad unless I overdo. I’m sure I would have noticed if it made a significant effect, as we moved a couple months later, and it’s impossible to do that without overdoing!
I wonder if the TMS of 6 or 7 years ago is different from the TMS of today. While you can never guarantee the efficacy of a treatment – even in treatments that work for others – hopefully the TMS they’re doing today is better.
I’m a full fledged woo skeptic and .. a family member suffered from severe depression for almost 20 years and 3 months of TMS treatment returned them to their pre-depression self. I hadn’t thought of TMS for ME pain (headaches, malaise) and fatigue but it may be worth a try. BTW, insurance does cover TMS for depression.
That is impressive!
My understanding that insurance does cover TMS for depression – but perhaps only for treatment resistant depression – not sure.
Here’s a link to one hospital with some videos, case studies and FAQ.
https://www.mcleanhospital.org/treatment/tms-service
You’re right Cort. It looks like TR depression is covered by insurance. This seems to be a carefully calibrated medical process so I’m not sure about DIY at home methods.
Hi
I’m lucky, I’ve been having RTMS for a few years now. It really helps with pain and eases my symptoms. I’ve been having it on the left side of my brain, which is the side they use for depression, but I’m not depressed. They use it for so many conditions including anxiety, which they treat on the right. When the clinic opens up again I’ll ask about the different sides and why I’m treated on the left.
Good to hear. How often do you have it done? Most studies seem to focus on the left DFLPC not the right. Not sure why this study did it on the right but it seemed to work.
Interesting. My TMS fo TR MDD was focused on my right side. ? Why the difference? I don’t recall if they said anything about individual differences. My migraines are focused on the right side and my mother has them on the left side, so maybe?
Thanks Cort,
Is there any info available re where to find these devices for home use, and/or what specs to be looking for? (What numbers correspond to ‘high’ and ‘low’, etc)?
Related: Are you aware of any studies of trans-cranial brain photo-bio-modulation for CFS/FM? (I got one of these brain PBM devices- it hasn’t helped my (non-FM) pain, but I’ve been having really good results w fatigue. (Seems worth mentioning, even though I’m not sure if my version of fatigue is typical CFS. The “Vielight” device I got is pricy, but there is a 6 month return period!)
I’m afraid I have no idea if these can be purchased or not or how to set them.
if this is the same thing there has been one study which combined exercise and photobiomodulation and got good results.
https://pubmed.ncbi.nlm.nih.gov/29170901/
I have had TMS for depression twice. Once years prior to my ME and one after. First time it made a big difference for me.
Struggled th hrough the second time. I believe they were doing high frequency. Made my tinnitis wirse and gave me headaches. My anxiety would spike at times. It did lift th ed depression for less than a minth.
Unfortunately, it’s not something you can purchase and do at home. There are small devices on the internet that you can purchase for home use, but they are NOT the same thing. The TMS that actually works for major depressive do (MDD) and that is being studied for other health problems, like FM, are only available for use by healthcare professionals, such as psychiatrists. It’s complex and there are risks involved, so only trained personnel can administer the treatment. I can tell you from personal experience with TMS, for a 23 yr history of treatment resistant MDD, is that it is INTENSE. The treatment is also highly individual. First, they must ensure that they are targeting the correct part of your brain. This is done by meticulously measuring the placement of a helmet. Next, your seizure threshold must be determined and that can vary from day to day (caused by a multitude of variables), so your treatment may also vary. It was my psychiatrist who determined my treatment (strength of the magnetic pulses, etc.) and continued to oversee the process. BTW, it was amazingly effective for me!
There is an audio visual entrainment device (David Delight Plus) by a Candadian company, Mind Alive, that can help, but results, at least for me, took a long time to notice and were not as dramatic as Magnetic Resonance Therapy at the Brain Treatment Center in Newport Beach, Calif. That worked like the TMS study results. I was at the center for 3 weeks in 2014 and the very first session reduced the FMS pain to nil and it hasn’t come back. Recently, I started neuro-feedback sessions for PTSD from childhood trauma, and that is helping everything else (IBS gone after 25 years of nothing else helping, anxiety greatly improved, etc.). So, I am a big fan of brain “woo woo.”
That’s amazing news Linda and Wendy. It’s shocking to think that a series of treatments like this can have long lasting effects. Obviously we need more studies that determine the best approach but hopefully that will be worked out and TMS will become more available over time.
An organized approach that elucidated the best TMS protocols would be so helpful. Unfortunately we rare see that in medical research.
I was diagnosed with multiple sclerosis in 2014 but had my first symptoms in 2012. both my legs were spasming mostly at night which made sleeping difficult. I tried Copaxone for about 5 years or so. The Copaxone causes joint pain, I have tried several types of medications but all made me sick. In 2019 I went to a care facility, life was too difficult at home for my husband and family. I was advised by one of the nurse at the care facility to try natural treatments, She introduced me to Mayaka Herbal Clinic, spoke to my husband about it and he went online to research, My husband read positive reviews from other people who used the product from Mayaka Clinic, We decided to start me on the treatment. Its been 7 months since I completed the treatment, It has made a tremendous difference for me. all my symptoms including poor vision, pain, fatigue, and other symptoms stopped Visit their website ww w . mayakaherbalclinic .com
hi michelle, i could not find anyrhink under the link you gave. Also not with surching in mayaka clinic. has the name changed? how did you know wich treatment you ha to follow? Can i do this from in bed from europe? Is it also for me/CFS? thanks!
I was able to find it by searching Mayaka Herbal Clinic. It is on South Africa. They use herbal remedies for various diseases/ conditions. ME/CFS is not listed. They have online chat if you want to ask about treatments for ME/CFS. Fibromyalgia is listed as something they treat. I hope this is helpful.
Hi Cort, this topic is intriguing. I am unable to wear any magnetic jewellery because I end up with RSI like pains and aches. For example magnetic bracelets make my arm feel like it weighs a ton and that’s not because the bracelet is heavy. I know it sounds abracadabra and I thought I was imagining things but, as per your article, there is more and more evidence that magnetism does affect the body. I now wonder if the reverse will also work for me such as wearing a magnetic necklace to ease pain in my neck and shoulders (??) Not sure Looking forward to your next blog about this topic!
Wow, a fibro study finally and a positive one. Thanks for your diligent research into this, Cort, I got excited reading it. However, when I read the original study I found it was limited to women and under 50, excluded those on tramadol and other seizure threshold lowering meds, and excluded those with tinnitus. Aside from that Mrs. Lincoln…
IMO that means a pretty good number of us were not seen as suitable for the treatment for a variety of reasons we can suspect. They used a frequency of 1 hz and pretty specific location. I have a PEMF generator from Micropulse.com that puts out some low frequency TMS as one option and will consider having a doctor friend help me find the precise area to zap. I can probably hold my tramadol for a dose without going into withdrawal but I’d like to know why they excluded tinnitus. I was encouraged that so many fellow fibies are also at 7.5 pain, sadistic as that sounds but makes me feel like the hell I go through every minute is not unusual. Bad enough so
i will pursue doing this to myself if frequency of my device seems in ballpark.
While the research on TMS for FM is limited, it shows promise and therefore warrants continued research. If more studies provide evidence of efficacy, larger studies are warranted. Personally, I am encouraged by the fact that a study focused on women. Women are under studied in general and we are finding more and more that women tend to respond differently to medications, treatments, etc. Certainly not all research is high quality, but it is these small, preliminary studies that provide that basis from which to learn from and expand upon.
I would be interested in whether or not the small, low frequency devices for home use can be helpful. I’m also curious if there is risk for seizures with the lower frequencies. Anyway, it’s exciting to see much needed and promising research for some relief for FM sufferers!
Women understudied?! Virtually every FM study is done with middle-women, often overweight. That’s the modal profile of patients with this disorder. FM is probably the most female study inclusive of any research…check the studies.
This is a bit long, but I have personal experience with TMS and hopefully may be of interest. Here goes.
A few years ago, I had TMS treatment for 23 years of treatment resistant major depressive disorder (MDD). It wasn’t until the last 1-2 weeks of my 6 weeks of treatment that I suddenly felt better – like I no longer had MDD! Three years later, I am still free from s/s of MDD. An important note here is that there is a big difference between MDD and situational depression. MDD can strike when everything in your life is going great and you have no reason to be depressed, which strongly suggests that it is primarily related to a brain that is just not working right.
It just so happens that I had also recently been diagnosed with system exertion intolerance disease, or SEID (I prefer SEID over ME/CFS as the diagnostic terminology…..) that started 1-2 yrs prior and had been gradually making itself apparent. At first, TMS treatment seemed to worsen my symptoms of SEID, which I attributed to the physical stress of it all. However, TMS can just really take it out of you – independent of SEID. A couple weeks after I had completed treatment, I felt quite a bit better from an SEID standpoint. Unfortunately, the severe moral and emotional stress that I was experiencing at work continued to escalate and my symptoms returned and got worse. About a yr later, I went through the entire TMS treatment again in hopes that I might again realize some improvement. This was not the case. Of course this is an “n of 1” scenario and there were numerous complicating factors, such as the fact that my SEID was worse and I was much further in the progression of the illness. My treatment was also designed for treatment resistant MDD, not SEID. With the monumental losses I have had due to SEID, I often have significant situational depression. If I still had MDD on top of it, I’m not completely confident that I would still be here today. It is my understanding that TMS has been widely efficacious for MDD sufferers. The TMS studied for FM is very different and probably would be for SEID, too. It is my hope and dream that the right TMS treatment could also produce such positive outcomes for SEID – and SOON!
A bit off topic, but a friend of mine just forwarded me this article which basically says that Anthony Fauchi has recognized and commented on the similarity of post Covid symptoms and ME/CFS.
Finally, some real recognition in high places about our plight!
https://www.statnews.com/2020/07/21/chronic-fatigue-syndrome-keys-understanding-post-covid-syndrome/
Maybe that will mean the money (and more research) will follow!!!
I am referring to health research in general, not just FM, that has historically assumed that study results for men could be applied to women equally. I do not pretend to know about all the research w FM as I do not suffer from it. As a healthcare professional w training and experience with health research, I do have a fairly good handle on all the different facets of it. I suspect that so much of the FM research focused on females b/c there is greater prevalence in women. But, just as men cannot be applied to women, the opposite is also true. absolutely I agree that, unless a health problem solely affects one gender (such cervical and ovarian CA or prostate CA), both need to be studied, both separately and combined.
Yes!! And the exciting thing for CFS research is that there is a large coalition that has formed for the sole purpose of studying onset of CFS s/p COVID infection. (This is according to my Dr at the Bateman Horne Center). CFS so often isn’t recognized and properly dx until the sufferer (like in my case) is already pretty far along in the course of their disease. This is an opportunity to catch it early on and not only try to understand what is really happening, but also in hope of being able to help people with early interventions!
Yes, great news about Fauci. I have some COVID studies listed here – https://www.healthrising.org/blog/2020/07/05/long-haulers-media-covid-19-chronic-fatigue-syndrome/ and have a blog coming up on COVID-19/ME/CFS shortly. Big opportunities for us and for the long haulers.
Thanks Nancy,
What a great article by David Tuller and Steven Lubet. I think it’s a brilliant round up of where we are, how we’ve got here and the current danger of following the inappropriate ‘treatment’ (CBT and GET) that has been dished out to vulnerable people over the years, which results in the cementing of their symptoms and not their alleviation.
Thank you for the feedback and for bringing awareness and attention to the vulnerability of many in our community – too often overlooked but of such significance and great importance. <3
Just an FYI, the biceps femoris is one of the hamstring muscles. ?
No kidding! (lol) Thanks
I consider myself very fortunate that I am generally not in any pain and don’t have FM, even though my mother does.
I’m really looking forward to the blog on TMS and fatigue because though I have reached a good level of functioning – I still haven’t completely figured out the energy depletion, which I find very frustrating. I am trying to resist the temptation to keep pushing on in the hope I’ll break through to a place of boundless energy. I can now get through to the afternoon, mostly feeling good, but if I keep going I end up feeling like a dredger heaving itself through the sediment. I’m not very good at recognising or accepting that I’m fatigued! Tired just isn’t the right word… This is all occurring in my brain and I seem to have reached a certain level and seem a bit stuck – maybe that’s just impatience.
I live on the Central Coast of California. Does anyone know of a facility that does TMS treatments within a hundred mile radius of San Luis Obispo, CA? Thank you.
BTW, I have had fibromyalgia for thirty years and both of my daughters have it. I would love to find not only hope for myself but hope for my daughters.
Karen, a quick google maps search turned up these San Luis Obispo TMS options:
https://www.greenbrooktms.com/covid-19-resource-center
https://www.slopsych.com/
Hope these help if you haven’t already found something.