

In “Key Milestones Contributing to the Understanding of the Mechanisms Underlying Fibromyalgia“, two Australian researchers give a fascinating overview of what they consider to be the breakthrough findings in FM.
There’s a lot going on in FM patients’ brains. But could the brain account for all the problems in FM? (Image by Oberholster Venita from Pixabay)
Tellingly, they quickly highlight neuroinflammation. In one of the first sections, “Neuroinflammation as a Peripheral Pain Mechanism”, they assert that neuroinflammation “likely contributes to many of fibromyalgia’s clinical features” … and may even produce the small nerve fiber neuropathy and found in the skin and corneas of many FM patients.
Not only that, but they lump FM’s allies (irritable bladder syndrome, migraine, restless legs syndrome (RLS), multiple chemical sensitivity (MCS)) in the same basket. (Why they didn’t include chronic fatigue syndrome (ME/CFS), I don’t know, but it would surely fit for them.)
The Nervous Nerves in Fibromyalgia
The good news is that if neuroinflammation is the cause of the multiple problems in FM, then at least we’ve defined a central cause. It’s an interesting one because back in the 1990’s, when central sensitization was first uncovered in FM, it was believed caused by the hyped-up activity of pain nerves – specifically the A-delta nociceptors connect to the dorsal horn of the spinal cord – and leading to the brain.
After repeated stimulation some pain producing nerves in FM get “wound up” = ready to send out pain signals at the slightest stimuli. (Image by PublicDomainPictures from Pixabay)
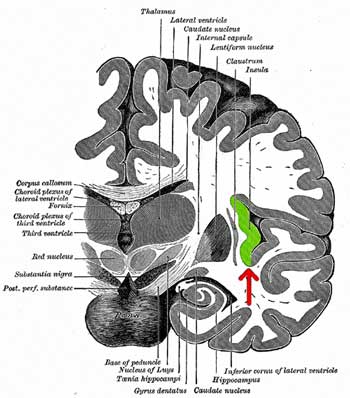
The dorsal horn of the spinal cord is going to be mentioned several times. It carries sensory signals from the peripheral nervous system to the central nervous system,
Next, researchers showed that in a process called “windup”, that if they repeatedly stimulated C-nociceptive (pain transmitting) nerves, those nerves would stay activated far longer in FM patients than in healthy controls. In healthy controls, the pain nerves quickly calmed down, but those nerves in FM got “wound up”.
Plus, they were able to show the nerves in FM patients were primed to act more quickly – they seemed to spontaneously erupt into action more. Those twitchy nerves affected the muscles as well. It takes less stimulation to produce a pain-evoked muscle response in FM than in healthy controls.
FM researchers next added yet another nerve to the FM hit list. Peripheral A-beta nerve fibers function as relays to the dorsal horn of the spinal cord from deeply embedded mechanoreceptors that respond to pressure. Some believe a sensitized pathway from the mechanoreceptors to the dorsal horn is producing the pain FM patients feel while bending, moving, etc. – anything that puts pressure on those mechanoreceptors.
The mechanoreceptor issue may have special relevance for the upper body, neck and head pain often seen in FM as the mechanoreceptors are particularly deeply embedded in and around the spinal column. That’s interesting given that recent study suggested that a type of connective tissue massage on the neck significantly reduced pain, muscle fatigue, and feelings of tension and anxiety.
Note that no mention has been made of the brain yet. Despite all the nerve issues found, the authors don’t believe they can explain the constant pain FM patients are in. The brain, they assert, must be involved. So how could the brain affect the activity of pain nerves in the body?
The Brain
Neurotransmitters
There’s a lot going on in the brains of FM patients. Take the two neurotransmitters primarily involved in the pain response – substance P and glutamate. Both these neurotransmitters turn on the N-methyl-D-aspartate (NMDA) receptors that increase the pain response – and both are increased in FM.
Substance P can do everything from sensitive nerves outside the spinal cord to enhancing the activity of pain processing regions in FM: it’s elevated in FM.
Substance P is a neuropeptide that is released from sensory nerves which can travel the length of the spinal cord. It by itself is able to sensitize the nerves in the dorsal horn of the spinal cord mentioned earlier. It’s also abundant in the emotional and pain centers of the brain. People with FM have been shown to have up to three times the normal levels of substance P in their brains.
Glutamate is the main excitatory neurotransmitter in the brain, but high glutamate levels can burn out nerves and activate the microglia. Studies suggest the neurons in FM patients’ brains are just itching to produce glutamate.
While not all the findings below have been validated, it’s possible that many other neurotransmitters may be altered in FM (calcitonin gene-related peptide, brain-derived neurotrophic factors, corticotrophin-releasing hormone, hemokinen-1, neurokinin A, neurokinin B, adrenomedullin, vasoactive intestinal peptide, neuropeptide Y, and gastrin-releasing peptide.)
Reduced Pain Inhibition
But how are these problems affecting the pain signals coming up from the body? There are pain producing pathways that ascend to the brain and there are pain inhibiting pathways that descend from the brain to the spinal cord. One might think the ascending pain pathways are the problem, but no – it’s the poor performance of the descending inhibitor pain pathways that many FM researchers believe is really ramping up the pain in FM.
The recognition that inhibitory pain pathways descending from the brain play a major role in how much pain we experience sparked a revolution in our understanding of pain. Prior to that understanding, it was believed that pain signals were simply sent straight to the brain and that was it.
Now we know that how much pain we feel is, to a good extent, controlled by the brain. During times of danger, for instance, the brain may temporarily completely inhibit pain signals from the body. In the case of fibromyalgia, the opposite appears to be happening – the brain’s weak inhibitory pain pathways are believed to be allowing too many pain signals through.
It’s important to note that pain and sensory signals to the brain are always modulated. The brain can’t function if it’s exposed to every bit of sensory input the body is experiencing. It weeds out innocuous signals so that the more important signals can get through.
Ascending pain signals are believed to go through a series of checkpoints, or gates, which determine if they should continue on their journey. If those gates are stuck open – causing a cascade of signals to hit the brain – they could very well produce something like FM.
Problems with descending inhibitory pain pathways in FM and other chronic pain states are demonstrated by an interesting test. The arm is laid in cold water (causing pain) and then the pain sensitivity of another area of the body is tested.
Through a phenomenon called “controlled pain modulation”, causing pain in one area of the body causes other areas of our body to become less sensitive to pain. Animal studies show that the controlled pain modulation process is initiated in the brain and is believed to cause an increase in the activity of descending pain inhibitory pathways. Studies indicate that the activity of the pain processing regions of the brains of healthy controls actually declines when they undergo this test. This process is not working well in FM, though, and in some cases is not present at all.
There is a catch, though, to this descending pain inhibition hypothesis. It’s possible that the descending inhibitory pain pathways are working just as hard as they can in FM, but their inhibitory signals are simply being overwhelmed by a barrage of pain signals emanating from the damaged nerves in the body.
Plus, not all FM patients display problems with descending pain inhibition – for a substantial number of patients, their problems lie elsewhere. In fact, some researchers believe the cold pressor or thumbnail pain test could help doctors better treat their FM patients. One study, for instance, suggested that diabetes patients with descending pain inhibition problems do better with duloxetine that those who do not have this problem.
Autonomic Nervous System
The authors mostly ignore the autonomic nervous system, but studies have shown that reduced pain inhibition pathways are associated with low heart rate variability (HRV) in chronic pain. Low HRV refers to an inability of the parasympathetic nervous system (rest and digest) to control the sympathetic nervous system (fight or flight); in other words, another modulating process has gone awry in FM.
But what is the connection between the autonomic nervous system (ANS) and pain modulation? The ANS is one of the two main stress response systems in the body and pain has been shown to increase sympathetic nervous system activity. It’s possible that the reduced pain inhibition processes are also failing to activate that other notable modulator and calmer – the rest and digest, or parasympathetic nervous system, in the body – leaving one not only in pain, but edgy and having trouble sleeping as well.
That suggests that FM doctors should also consider assessing autonomic nervous system functioning. Mestinon (pyridostigmine bromide), an ANS regulator, has been helpful for some people with ME/CFS, who tend to have similar problems. The Open Medicine Foundation is funding the first ever Mestinon study in ME/CFS.
Brain Scans
The Gist
- Three nerves that transmit pain signals to the spinal cord have been found to be overactive in FM.
- Nerves should calm down and adjust to repeated stimulation, but in a process called windup the pain nerves that get activated in FM stay activated. They also respond more quickly to a stimulus and are apt to fire off spontaneously more.
- Twitchy nerves leading from deeply embedded mechanoreceptors around the spinal column could explain some of the upper body pain common in FM and the problems with bending, moving etc.
- Two neurotransmitters associated with pain, substance P and glutamate, have been found elevated in FM patients’ brains.
- The brain exerts enormous influence over the amount of pain we feel through a pain inhibition process which can reach all the way down the spinal cord to the spinal cord’s dorsal horns.
- When one part of the body is exposed to pain, our sensitivity to pain in other parts of the body actually reduces. This process – called controlled pain modulation – is due to a pain inhibition process which begins in the brain.
- This process has been shown many times not to be working well in many, but not all, people with FM. Interestingly, although it’s not clear why, the low heart rate variability (HRV) found in FM is associated with reduced pain inhibition. Mestinon is one drug that has proved helpful for some people with ME/CFS.
- Pain signals are believed to need to pass through a series of checkpoints or gates in order to make it to the brain. Those gates are believed to be opened wider than usual in FM.
- Some researchers, though, think that the pain inhibition process in FM is working just fine. They believe its signals are being overridden by a constant stream of pain signals emanating from the body.
- Brain scans show more problems. Blood flows to various parts of the brain are altered. The pain processing areas of the brain are hyperactive. Even when the brain is resting, it still maintains its tight connection to those areas.
- The authors believe that widespread neuroinflammation could explain all the symptoms in FM.
- With so many validated issues in just the brain and nervous systems of FM patients, it seems incredible that any doctor worth his or her salt could dismiss this disease.
Brain scans find yet more evidence of brain problems. SPECT scans have found altered blood flows in numerous parts of the brain (prefrontal cortex, thalamus, insula, somatosensory cortex, amygdala, caudate nucleus, inferior pontine tegmentum, parietal cortex, and the gyrus rectus).
Functional MRI (fMRI) studies indicate that the pain processing areas of the brain are more quickly activated than usual to painful stimuli. Even in its resting state, the fibromyalgia patient’s brain shows greater connectivity to the pain processing regions of the brain (insula and others) than usual.
At the end of the brain section, the authors return to neuroinflammation – perhaps the central process responsible for the symptoms found in FM. The evidence for neuroinflammation in FM is climbing. High levels of the pro-inflammatory cytokine IL-8 in the spinal fluid, evidence of brain glial cell activation, and high levels of metabolites associated with inflammation suggest that neuroinflammation may be widespread.
Conclusion
This brief nervous system primer on FM shows how much has gone awry. It’s no wonder that FM has been called the “quintessential pain syndrome”.
From a bevy of hyperactive nerves in the periphery, to the possible loss of gating mechanisms, to high levels of pain enhancing neurotransmitters, to problems with the pain inhibiting pathways, to increased activation of the brain’s pain producing organs, to evidence of neuroinflammation, it seems that virtually every aspect of pain production process in the brain and nervous system is out of kilter in some way.
The fact that the brain can reach down into the spinal cord (and into the peripheral nerves?) and turn off pain signals is remarkable indeed. The brain’s amazing reach can be demonstrated by the role the insula – a small organ located in the middle of the brain – may be playing in FM. A recent review suggests that besides pain, problems in the insula could be contributing to the “heart rate and blood pressure, bladder and bowel symptoms, and anxiety and sleep disturbances” found in FM.
The central role the brain may play in FM suggests that rewiring the brain using drugs, neuroplastic approaches, magnetic stimulation, or other techniques could produce dividends. It also helps to explain why some drugs work when they do. Lyrica has been shown to reduce glutamate levels in the insula. Duloxetine may work better in FM patients who have controlled pain modulation (CPM) issues. The fact that many patients don’t benefit from these drugs is not surprising. More and more evidence suggests that FM is a quite heterogeneous condition.
While the authors believe the brain is producing all the symptoms in FM, a minority view believes it’s possible that the opposite is happening: that hyperactive nerves in the periphery flooding the spinal cord with pain signals and overriding the brain’s natural pain inhibitory signals.
Some anecdotal reports suggest that things like vagus nerve stimulation (of a balky parasympathetic nervous system) can be quite helpful in the right patient. With that in mind, we should keep a close eye on the NIH’s SPARC Initiative, which is dedicated to find ways to tweak the peripheral nerves, including the vagus nerve, for better health. Even if peripheral nerve problems turn out not to be the biggest drivers of pain in FM and similar diseases, they are clearly contributing to the problem.
Could the upper body pain in FM be caused by twitchy nerves communicating signals from the deeply buried mechanoreceptors? (Was the success of the (small) FM connective tissue neck massage study do to its ability to take pressure off the deeply embedded mechanoreceptors and their nerve pathways?)
The recognition that neuroinflammation, on the other hand, may be driving the pain in FM opens up an intriguing new target that could reap dividends given the intense interest given neuroinflammation in much better funded diseases. Many treatments are currently being assessed.
Whatever is happening, the many documented problems in the brain and nervous system in FM make it incredible that any doctor could believe this disease is not very, very real. They also may hint at why FM is so difficult to treat – the entire pain producing process has been affected.
One last note: given that a significant subset of FM patients do report an infectious trigger it’ll be very interesting to see how many cases of FM show up in the long haulers. Hopefully long hauler studies will help what’s happened in both ME/CFS and FM.







Excellent article….I learned a lot!
Me too! A lot going in there! (lol)
Something I’ve been wondering is – why do some people develop FM and some don’t?
Like me, I don’t have FM and don’t want it (!) but considering I have many other issues, which seem to include brain inflammation, what or where is the difference?
I know this may seem to be a bit of a stupid question!
Not a stupid question at all. Jarred Younger has an idea – he believes that because microglia can produce so many different inflammatory substances that it just takes a small change in how they are provoked to produce either ME/CFS or FM or ME/CFS plus FM.
Hi Cort! First I apologize that what I am about to share is about Covid long haulers, not fibromyalgia patients. I’m doing it this way because I’m not sure you or others actually go back and read later posts on some of your blogs.
This, IMO, is a ‘must read’ about Covid long haulers and ME/CFS. It covers a lot of ground including how both are under recognized and under researched. I know it is a topic close to your heart as this Covid problem might lead to more focus on ME/CFS.
https://www.theatlantic.com/health/archive/2020/08/long-haulers-covid-19-recognition-support-groups-symptoms/615382/
I hope you can glean something helpful from reading it.
Thank you for posting this link. Helpful.
Please Nancy never apologize for posting something on the long haulers – not on this blog. 🙂 Thanks very much for pointing out another Ed Yong blog – perhaps the most astute COVID-19 writer writing today.
He’s even got HR 7057 – the Raskin bill for ME/CFS – in there! What an ally he is!
Check out this from the article:
Is that your and my story to a tee? This is really happening…Wow..
Cort it’s my story too. To a CAPITOL T !!!!! I was a super health conscious woman and now I can’t move without pain. I can’t stay still without pain. I was super fit and now I just have super fits of disabling symptoms that cover a whole spectrum of every system in my body.
By the way this article on Health Rising is so very very informative ! The connection between extreme emotional pain sensitivity and FM really caught my attention! Thank you ! So interesting!
I have been diagnosed with Fibromyalgia and i have been telling my doctor that I believe it is in my brain, spinal column and affecting everything mentioned in the article. I have saved it so I can email it across to him. The missed opportunity here was the chronic fatigue, impacting so much of our lives to 10 to 20 minute windows of activity. It would have been interesting to see the findings had it been included. Insightful and reading it gives me hope that we are finally on the right path. I can physically feel the inflammation inside of.me.pulsing around my body and head, it has a sound, like a whirling noise and i feel the energy of it. Glad to have been diagnosed as i have discovered a world of information and this has been the best so far.
Cold water dipping has helped me
Thank you for this information, it was detailed and very helpful in understanding FM.
Outstanding article and finally gives me some hope for the future. I would like to add that I was put on high doses Cetirizine for possible eosinophilic esophagitis and much to my surprise most of my FM symptoms simply vanished for several months, I did a bunch of digging and discovered histamine intolerance and have been treating myself for this and I have had wonderful success. I have been able to re-introduce a number of foods that I had not been able to tolerate for quite some time. The mucus in my bowels has vanished after a good 20-25yrs and that is truly remarkable. Histamine levels affect inflammation so it all makes wonderful sense to me.
Very interesting! I’ve never heard of Cetirizine….Thanks!
I believe it is Zyrtec
Buen dato sobre la cetirizina. Me pregunto, eso sí, en el Sindrome de piernas inquietas, se describe sd de agravamiento con el uso de antihistamínicos, y muchos pacientes tienen estos cuadros asociados FN, piernas inquietas e intolerancia a histamina (incluyéndome). Qué opinan de eso?
Cort, has there been any reports of FM being autoimmune? Thought I’d seen something,
but can’t find it again.
All i need to do is run my razor over the back of neck
(Male) , an hr or so later I get hundreds of bumps about 1/2 inch in size.
When I was sent to Calgary alberta,Canada I was receiving iv vitamins, minerals.they added a trace mineral molybdenum…soon after I had hives the size of baseballs all over the front of my trunk.
it seems I have trouble with my lymph.
Years later I bought Raymond Perrins 1st book and found my perrin point to be very tender. I, at the time had lumps under my skin ranging from 1 inch to 2 inches.
I began his skin brushing exercises…not much happened until about the 2 month mark, then, one morning my lumps, astonishly were half the size.
I should add that at the age of 14 I took tetracycline for acne for 1.5 yrs non stop. I’m adding this tetracycline story because I have this gut feeling that it really messed up my guts years later. I continue to be “allergic” to many many foods and dust mites etc.
And yes, I too had the cytokine storm so bad and so much pain I was going to go get the gun and do it. I am like whiteny dafoe….sometimes I think I was worse than him but who really knows.all I do know is , I was very near death. They at one time were going to place me on baby pablum as I couldn’t digest anything. To me, this all seems like a detox shut down.🤷♂️
Has high lipids have a baring on FM.