

One of the great questions facing chronic fatigue syndrome (ME/CFS) is whether many COVID-19 long haulers will come down with an ME/CFS-like condition. Anecdotally, it appears likely that they will. A few, isolated studies are beginning to suggest the same. Recently, a case report “Post COVID-19 syndrome associated with orthostatic cerebral hypoperfusion syndrome, small fiber neuropathy and benefit of immunotherapy: a case report” suggested that not only will COVID-19 at times turn into ME/CFS, but into orthostatic intolerance and small fiber neuropathy as well.
In “Post COVID-19 syndrome associated with orthostatic cerebral hypoperfusion syndrome, small fiber neuropathy and benefit of immunotherapy: a case report”, Novak reported on the case of a 64 year-old-woman who presented with a cough and shortness of breath.
The First Post-Infectious Illness
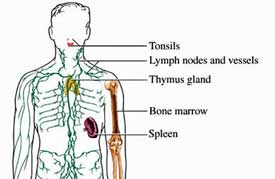
The woman had apparently been healthy until 4 years prior when a tick bite produced a bulls-eye rash, arthritis-like symptoms and swollen lymph nodes. She was quickly treated with antibiotics, but several months later relapsed, leaving her with headaches, severe pain, disabling fatigue, dizziness, brain fog, mood swings, and burning sensations in her arms and legs.
She was lucky in that she saw Peter Novak MD, PHD – the Chief of the Division of Autonomic Neurology and Director of the Autonomic Laboratory at Brigham and Women’s Hospital (Harvard). Novak had recently uncovered a new kind of orthostatic intolerance and he put her through an autonomic nervous system workup.
Various autonomic nervous system tests (tilt table, Valsalva maneuver) indicated she had a mild parasympathetic impairment, no evidence of postural orthostatic tachycardia syndrome (POTS – increased heart rate when standing) or orthostatic hypotension (reduced blood pressure upon standing).
The blood flows to her brain, though, declined dramatically upon standing, indicating that she had orthostatic hypoperfusion syndrome (OCHOS) – which Visser, Rowe and Van Campen have recently reported in ME/CFS.
She also tested positive for small fiber neuropathy (SFN), which appeared to be causing the burning sensations. She next got the full antibiotic treatment (rifampin, ceftin, cefdinir).
In short, she looked very much like an ME/CFS/FM patient. Despite the fact that several months had elapsed between her original infection and her relapse, she clearly had a post-infectious disease and was diagnosed with Post Treatment Lyme Disease Syndrome (PTLDS).
Over the next year, she apparently improved substantially. One year later, Novak simply reported she had moderate headaches, which occurred about twice a week.
Post-Infectious Illness #2 – COVID-19
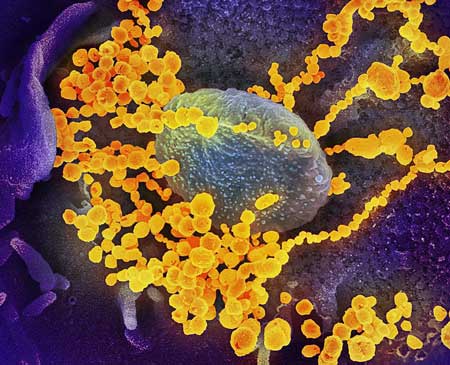
Then she got COVID-19. First she experienced shortness of breath and cough. Several days later, after both of those worsened and she developed a fever, an x-ray indicated she had viral pneumonia, and she tested positive for SARS-CoV-2. She was treated with hydroxychloroquine and azithromycin and responded well to both: within a week, she was close to baseline.
Then it got really interesting. Once again, she responded to therapy and appeared fine but then two weeks later, she experienced severe leg pain, burning sensations on her feet and hands (probably from small fiber neuropathy), strange sensations (twitching and vibration feelings at her face), blurred vision, headaches, brain fog, forgetfulness, chronic fatigue, orthostatic dizziness and urinary incontinence. Repeated tests for the SARS Cov-2 virus were negative – she had fought off the virus: something else was causing her symptoms.
She was suspected of having an autoimmune reaction and intravenous immunoglobulins (IVIG) was prescribed (2 g/kg monthly for 2 months, decreased to 1 g/kg monthly due to the IVIG-induced headaches). Her leg pain, brain fog, urinary problems and blurred vision completely resolved and her headaches and fatigue improved by 50%.
Check out an overview of IVIG effectiveness in these diseases.
Infections are often cited as triggering events for autoimmunity, and Novak attributed this woman’s continuing post-COVID-19 issues to a “postinfectious autonomic syndrome likely due to autoimmune process”, and noted that other post-infectious syndromes and conditions that have been associated with COVID-19 (Guillain-Barre syndrome (GBS), acute disseminated encephalomyelitis, postinfectious brainstem encephalitis, necrotizing autoimmune myositis). (A Colombian researcher cited even more autoimmune conditions (systemic lupus erythematosus, autoimmune hemolytic anemia, autoimmune thrombocytopenia, multiple sclerosis) that COVID-19 appears to have triggered.)
(Another case report “Dysautonomia: An Overlooked Neurological Manifestation in a Critically ill COVID-19 Patient” also focused on dysautonomia in COVID-19.)
The Wall Street Journal just reported the majority of the more than 300 long-Covid patients being seen at the Mount Sinai Health System in New York City have “developed a dysautonomia-like condition” and that 90% of patients report experience exercise intolerance, fatigue and elevated heartbeats and 40% to 50% experience gastrointestinal issues, headaches and shortness of breath.
Note how similar this woman’s post-COVID symptoms (severe fatigue, dizziness, brain fog, burning sensations, etc.) were to her post-Lyme symptoms. It appears that despite the difference in the pathogens, one a bacteria and the other a virus, both infections triggered a similar response. That’s what the Dubbo studies found with a variety of pathogens in ME/CFS – and that’s good news for everyone hoping that COVID-19 long haulers will help reveal what’s happening with ME/CFS.
Novak noted that both the reduced blood flows to the brain (OCHOS) and small fiber neuropathy (SFN) this woman experienced twice may have immune roots, and that “theoretically both may respond to immunotherapy.” That’s a more than an intriguing notion given that both OCHOS and SFN appear to be pretty common in ME/CFS, FM and POTS.
The emerging focus on autoimmunity in COVID-19 highlights yet another potential silver lining from the pandemic: to understand better how an infection turns into an autoimmune disease. It could even help uncover autoimmune processes that may be at work in ME/CFS, FM and POTS.
The Autoimmune Question in COVID-19…and ME/CFS?
“It appears, therefore, that neurological manifestations of COVID-19 are not caused by direct cytopathic effects but indirect immune-mediated mechanisms targeting various unknown elements of the nervous system.” Lucchese
Just this week, the New York Times reported that:
“An autoimmune response “may also explain why so-called “long haulers” have lingering problems months after their initial illness has resolved and the virus is gone from their bodies.”
One study found high rates of “autoreactive” cells in patients with severe COVID-19. Another study found high levels of autoantibodies, “mainly against unknown autoantigens in the brain”, in the cerebrospinal fluid (CSF) of patients with COVID-19 with neurological symptoms. One more study – done by “researchers…known for their careful, meticulous work” also found high levels of autoreactive antibodies. Some of the autoantibodies being found also affect blood flows – a possibly key topic in ME/CFS and POTS.
Dr. Akiko Iwasaki, an immunologist at Yale University was not surprised:
“I’m not surprised, but it’s interesting to see that it’s really happening,” and then leveled the kicker: “It’s possible that even moderate to mild disease may induce this kind of antibody response.”
Is it possible that infections often produce autoantibodies which no one has thought to look for? Despite extensive testing, there’s almost no evidence of SARS CoV-2 being present in the CSF. Nor have pathogens been found in CSF testing in ME/CFS. If the brain is being affected, it’s more likely due to some sort of immune response.
The presence of numerous autoantibodies that are targeting as yet unknown brain tissues opens up another possibly fruitful area of inquiry for COVID-19 and for ME/CFS – two diseases loaded with neurological issues.
If there’s an autoimmune subset in ME/CFS, the first task may be finding the autoantibodies and determining what they’re affecting. Time will tell, but COVID-19 studies could conceivably help with that,
A chronically deranged immune response could certainly explain how an infection gets turned into a long-lasting illness, but we’re still in very early days with COVID-19. At this point, autoimmunity is just one possible explanation of the long-hauler phenomenon.







I look forward to the day Dr. Novak’s workup on his patient becomes standard.
No kidding! The placement of an autonomic workup as a standard workup in COVID-19 and other post-infectious illnesses is another potential silver lining. What a breakthrough that will be.
I. Have fibromyalgia and severe cervical deterioration. Can you recommend a stem cell physician? I live near San Francisco area and can travel to Mexico. Thanks.
I’m afraid I know nothing about the efficacy of stem cells. Sorry!
You may want to check out Dr. Neil Riordan’s clinic in Panama. I haven’t been there but would very much like to get evaluated by him. It’s very expensive but he’s made significant inroads into the use of stem cell treatments for several conditions. Dr. Riordan (a phd) is the head of the Stem Cell Institute and employs several medical doctors in his clinic. There are multiple videos on YouTube about his work.
My doctor Dr. Erik Spayde in Thousand Oaks, CA is using stem cells in both cervical spine and low spine. He fixed my cervical spine several years ago and I have been doing great ever since. I just attended a webinar where he discussed using stem cells in the low spine. He went to Harvard Medical School and specializes in orthopedics (just the spine). His phone number is 1-805-379-2322.
Hoping people will actually cite ME/CFS in these comments and discussions, so perhaps the long-haulers will receive our same diagnosis code of “post-viral FS” G93.3 so the Long Term Care insurance companies will recognize it as a serious condition, not in our imagination.
Now I see another code of R53.82 became effective Oct 2020 and wonder if that would work better by Assisted Living facilities.
I have paid premiums for 25 yrs and am now told my illness unfortunately does not qualify.
Hi Cort,
You mention IVIG in the title, but I didn’t find it in the article. Is there more you can share on that potential treatment? Or for that matter, is anyone exploring plasmapheresis, which seems like a natural thing to try considering the studies about the “something” in our blood that makes good cells go bad…..along with anectodal reports of patients going overseas for these treatments and being helped by them (to the extent they can pay out of pocket).
Cort wrote:
“She was suspected of having an autoimmune reaction and intravenous immunoglobulins (IVIG) was prescribed (2 g/kg monthly for 2 months, decreased to 1 g/kg monthly due to the IVIG-induced headaches). Her leg pain, brain fog, urinary problems and blurred vision completely resolved and her headaches and fatigue improved by 50%.”
I had herpes viruses and not COVID, but this is the approach my ME/CFS specialist used with me, finding infections, finding autoimmune antibodies and POTS, then prescribing IVIG at .75g/kg WITH support medications to reduce side effects like brain swelling (benadryl, SoluMedrol, ketorolac, etc.) It has greatly helped me.
Unfortunately, I know a patient of the same doctor mentioned in this article who got the exact protocol described. He had brain swelling and was given no support meds, either by the doctor, who refused to help, or 2 major Boston hospitals. This patient now has serious permanent neurological damage, verified by two outside specialists that originated with the treatment and its mismanagement.
The strategy can be an excellent and effective one, it’s just that it is a big gun to use, and does have the potential for significant side effects, and should be used with careful management and plenty of support medicines, including steroids, antiinflammatories, and Benadryl. And there is a range of IVIG dosing for autoimmunity, from .75g to 2g/kg body weight (.4g/kg is used for immunodeficiciency).
The other lesson is that going to an emergency room with side effects is not always the best strategy – though I have and have gotten appropriate help, it all depends on the staff and their knowledge of IVIG side effects in delicate patients, and knowing the appropriate thing to do.
I remember u telling me this Learner. I got approved for IVIG still deciding on taking it or not.
I was in a trial of IVIG for ME/CFS patients 30 years ago. The side effects were dreadful for many and the trial was found not to be helpful.
Hi Learner1,
If you don’t mind sharing, which CFS/ME specialist do you see? I’m in desperate need of one. Thanks
I started receiving Ivig last year ( only for immune low platelets by my hematologist) and what a difference in my chronic fatigue, dizzy fog, migraines, fibromyalgia. Unfortunately the immune system takes back over in about 2 1/2 wks & Ivig very expensive (about 12K) per treatment. They will have to figure out lower cost, longer term effective treatments
Same here Brenda. I have seen much improvement since I started IgG, except in my cognitive issues. It took a while, changing medicine 3 times and then increasing the dosage from 3g to 6g. I have been doing it subcutaneously (versus IV) and at home myself for 3 years. The cost is fairly prohibitive though, they definitely need to work on that. My insurance paid 100% the first 2 years but this year (and probably next) I have a 20% co-pay. This was $800+/month so I asked my doctor about either reducing the dosage or frequency. He didn’t want to reduce dosage, too hard to get insurance approval to increase again if needed, so he did agree to reduce it to bi-weekly, which is still costly but I just give up other things in life. About the 2 1/2 weeks though. I have found the same in trying to stretch mine out. If I go more than 3 days past the 2 weeks, I start getting sick again. I thought it was just me!
I was also unfamiliar with what IVIG is exactly. This was helpful to read:
https://www.webmd.com/a-to-z-guides/immunoglobulin-therapy#1
Hi Cort,
if you quote a medical professional at lenght, you should put the sorce in the body of the text. Not because you are not reliable, this is an excellent page. At the same time, if a medical professional reads this page, it seems to be built on stories rather than facts. If there was a successful treatment with IvIG, some documentary evidence, summary would be necessary… It is essential to show that this disease is real, proposed treatments, examinations are rooted in science.
I should do it for patients too! I mean too – but forgot. Thankfully, when I do this people usually notice and support me in getting the source in there. I just put it in there -thanks for making the blog better.
Here’s the link – https://pubmed.ncbi.nlm.nih.gov/32984564/
Thanks Cort, this is what I was looking for !
Thanks Learner1 for writing about your experience with IVIG but also about the serious pitfalls if given by less knowledgeable doctors than the one you had.
Here in the UK I just cannot imagine ME/CFS being treated in this way as the majority of doctors don’t even know what POTS stands for? That is according to my GP btw.
All that Cort has written about above fits with my own presentation of ME/CFS. It all started with 2 weeks of flu from which I couldn’t seem to recover. Two weeks later severe vertigo attacks followed that were disabling and left me partly bedridden for a time plus severe migraines started at that time too.
But it wasn’t till 10 years later that adrenergic symptoms of POTS started to develop slowly and got a lot worse a few years later which meant I could no longer carry on working as a teacher.
It’s interesting though that many patients with ME/CFS say they don’t suffer with OI or POTS. I would love to get tested for the antibodies that have been found in POTS, just to have it confirmed. There couldn’t then be any stigma attached to my own illness.
I have thought that it’s been pretty obvious for quite a while that CFS is an autoimmune illness.
Too many diversions away on fanciful theories.
I have to agree with Matthias: I thought ME/CFS being a mixed up autoimmune response-among other things-was a given. Cort, I too have a doc who has given me a ‘cocktail’ of various supplements that he claims are akin to getting IVIG, but w/o the huge costs and insurance denials. I have been on this regimen for 2 years and have never felt stronger in my 11 years of ME/CFS. How I wish others could afford treatments like these. And learn basic lifestyle changes-like ‘pacing’. These 2 things-new doc w/ immunoglobulin therapy thinking AND pacing-have been a HUGE game changer!!
Hi Linda,
#MEAction have a #StopRestPace campaign. I think pacing can seem a bit passive and just an absence of doing things. However I think I’ve been able to make some of my greatest gains by pacing – staying within my energy budget and by getting more restorative sleep. I feel by adopting a regular lifestyle, calming down, resting when I needed to, sleeping better my body could organise itself and make better use of what I ate and the supplements I took etc
Would you mind sharing more about this cocktail akin to IVIG?
What was the ‘cocktail’ of supplements Linda?
I don’t know if this is what Linda is on. But many have been on what is called a mito cocktail. Here is what is in it.
https://www.mitoaction.org/diagnosis/mito-cocktail-coq-10/
Agreed, I believe it definitely is from much personal and family evidence
Yes. And lots of things like how CFS often improves during pregnancy, which occurs with other autoimmune illnesses.
And the common infectious trigger.
I find this article quite interesting as I’m an ivig patient for a rare neuromuscular disease called stiffperson syndrome. Sps manifests as autoimmune disorder and symptoms vary in each patient. I first heard of the antibodies found in covid-19 patients and was curious to learn if the antibodies present in sps patients could have any immunity to covid-19. I raised these questions to my specialist and although he was quite intrigued, he suggested at the time there was no relation as the antibodies associated with sps (GAD65) were not the same as in covid recovered patients. I receive 60g of ivig 2 days a month, I have been exposed to multiple covid positive people including family members and every covid test I took came back negative and I have yet to even present symptoms. I really believe my ivig treatments for my sps is acting as a barrier to fend of the virus from entering my body. Id be interested to see if these studies start to find a connection as it would be a major breakthrough in finding a cure for this virus and bring an end to this pandemic. I hope this doctor continues his research and it becomes more public. I also receive i.v. medications (benadryl, Phenergan, Ativan and tylenol) during ivig to reduce the side-effects of ivig treatments as this medicine is extremely hard on vital organs.
* when I first heard of the antibodies back around May*
hi cort,
do you maybe know if OMF is further working (more patients) on the study you wrote about with autoimmune anti boddys with carmen scheibenbogen (germany)?
They had some succes in me/CFS patients if i remember well but the study was small. scheibenbogen only takes patients from berlin and one place next berlin. Glad you where one of the few that was helped!
i knew me/ cfs patients who where given IVIG and nothing…
It is all so complex, only the immune and auto-immune system and all the other things in me/CFS; you where verry lucky!
I would like to see MS coming (more) into these discussions. Much rarer than CFS, there are many similarities. The emergence of my MS symptoms 20 years ago coincided with 2 episodes of Optic Neuritis (ON) in the same year, one in late spring (March) and the second early in October. On each occasion, within 3-4 weeks of the onset (a clear and definable symptom), I developed a heavy cold. My conclusion back then still stands: that the cold-causing virus triggered the ON. After the second episode, I rapidly went on to develop other MS symptoms, becoming so tired that I could sleep more than 10 hours a day (note: I could be up all night and asleep all day!). Subsequent research further cemented my postulation about the viral trigger. It was a strikingly similar experience to some of the reports I’ve read regarding long-Covid and CFS.
My treatment was self-prescribed: high dose nutritional supplements, as many as it took to alleviate my symptoms (I had nothing to lose!), the theory being that if your nutritional status is low or borderline (no matter how fit you think you are!) when the immune system is activated, you can readily fall into a state of mild to severe deficiency. This can reveal hitherto unknown health issues, just we’ve been hearing about with Covid.
Needless to say I’m making sure I’m topped up with all my supplements for when Covid strikes! I’m 58 years of age and can still walk, though not very far. I’d very much like to keep it that way.
It’s great to see this view emerging (as well as treatments that are helpful, at least for some and so glad it was helpful for you Cort!)
In my 20 years of examining the research in chronic illness I’ve found that infections of different kinds are triggers for all kinds of chronic illnesses. Interestingly, and similar to UC San Diego Robert Naviaux’s theory on the cell danger response in ME/CFS, there can be all kinds of different onset triggers for all of these diseases as well. http://www.ncbi.nlm.nih.gov/pubmed/27573827
Naviaux has proposed that the altered immune and nervous system responses that lead to altered metabolic function represent unresolved threat responses. And that the reason some of us get sick when others do not after similar exposures, is that our threat responses were initiated earlier in life and strengthened or stimulated over time from other forms of relative threat (other infections, exposure to toxins or mold, as well as exposure to adversity).
When I looked it up a month or two ago, I started finding reports in the literature of new onset of other autoimmune diseases post covid as well (I looked up Type 1 Diabetes and Rheumatoid Arthritis).
Do you have the reference or name of the “Columbian researcher” ? re:
“(A Colombian researcher cited even more autoimmune conditions (systemic lupus erythematosus, autoimmune hemolytic anemia, autoimmune thrombocytopenia, multiple sclerosis) that COVID-19 appears to have triggered.)
Does anyone know if patients with autoimmune presentation always have postive ANA results? My experience has been that many in the ME/CFS, Fibro, POTS, & SFN communities test negative for ANAs, and therefore, autoimmune etiology is ruled out. That’s part of the reason IVIG is not pursued.
I know they don’t. Lauren Stiles did numerous autoimmune tests but only a biopsy for Sjogren’s Syndrome indicated what she had.
Seemingly healthy people can have a positive ANA, and people who are quite ill with an auto-immune disease can have a negative ANA.
Also, you may see people with auto-immune diagnoses described as “seronegative”. That means that they tested negative for antibodies usually found with that disease, but were diagnosed anyway, based on overwhelming evidence from symptoms, family history, biopsy, scans, etc.
I have heard it said that antibody testing is not yet very good for many diseases.
What antibodies are they testing for and finding? I’ve had numerous tests for auto-antibodies and they’ve all come back normal.
I’m not sure which ones are consistently tested for or consistently found in patients although I have seen and heard of a few but I don’t want to give wrong info So I will let others who are more sure answer. I personally have increasingly Found autoimmunity signs in the course of my illness. I began years ago with EBV which I have heard has some associations with autoimmunity. I had a very high RNASE-L Several years after known infection which I understand works to lower viral loads but I tested positive for ANA pretty early on and have on and off for 20 years. Some as high as 1:3200. I showed positive for tissue transglutiminase antibodies years ago then Celiac Disease. A gluten free diet lowered those antibodies but I showed positive Parietal antibodies in 2018 which attack the lining of the stomach. Starting at a low level These are now in the thousands. I also was found to have ca6 IGG a novel/experimental Sjögren antibody that attacks the salivary glands With at least association to Sjogrens.. I also a few months ago have shown positive for Myelin IGG IFA antibodies attacking the myelin of the nervous system and been found my EBV has gone from latent to active. This coupled with a muscle biopsy in 2012 that shows small fiber Neuropathy and an EMG in 2018 showing axonal degeneration progressing at four limbs and motor sensorineuropathy has me thinking seriously if IVIG May be an option for me to consider with so much research pointing to autoimmunity and Neuropathy being involved and IVIG being beneficial in both conditions. I have been told I should try it by an extremely prominent Neurologist who has written several studies about it and knows it very well, a pulmonologist who suggested it might be a good idea in the same network and another prominent Immunologist in a separate city. I just can’t help but worry about the severe complications that can arise though with IVIG. It seems like these complications could be especially likely in people such as myself whom can’t exercise, have high cholesterol and whose other organ systems might not be running as efficiently as people in their 20’s. I also likely would be using a hodge pudge of providers to get it. Is it best to risk the treatment or the progressing Disease? Any thoughts?
I was diagnosed 35 yrs ago with CFS after two bouts of Epstein Barr virus and in March I was diagnosed with low IGG. It had never been looked at before but I wonder if it’s related to my chronic illness (my mecfs is moderate now) IBGG is not low enough for IVIG treatment just another odd piece to the puzzle of my health that my docs don’t understand or treat. Unfortunately I do not have a MECFS doctor to help sort this all out
Search out an Immunologist. They usually fall under “Allergy & Immunology”. Unfortunately, like many doctors, it took a bit to find one that understood my needs via Immunology. Others only wanted to do expensive Allergy testing before they would consider anything to do with Immunity. I do IgG treatments at home myself subcutaneous rather than IV, for 3 years now. They have helped tremendously.
yep i have to say i was coming to the this conclusion prior to covid – everything i have done to heal myself from CFS (i am 95% better these days )has been based around calming down the vegus nerve/ hpa axis etc – I first got ill in a hotel in Los angeles and everything my body now reacts to points back to then – mold issues – hotel had a leak n the roof! , pollution, hotel was on sunset blvd (one of the most polluted places in the USA), im allergic to nuts, bread (gluten) sunflower oil and (all found in things I was eating from the hotel mini bar) – I have always believed that ME is the body mistakingly believing everything is the enemy and overreacting and going off the scale , including exersise and overdoing it and producing some kind of chemical- im sure this is why we always feel like we are coming down with flu ..
I agree with you Michelle – my immune system is hyper vigilant and over reactive. My main trigger is food. And again, I feel that calming my stress response and then getting better sleep has been a large proportion of my improvement – which may seem unrelated but for me it has been central.
I have been using IVIG for the last 8 yrs for Autoimmune Autonomic Neuropathy with Paraneoplastic Antibodies. I was due for infusion on a Thurs. On the following Sat after infusion, I developed a headache that wouldn’t go away. On Sun, I got a call that I was exposed to COVID-19 on that Tues/Wed before Infusion. I went and got tested! Positive!! Scared to say the least for my underlying condition, took extreme doses of vitamins, protein shakes, etc. I ran fever 1 day and slept for 2 days. Then back to normal. My Drs. Believe my infusion came at the perfect time stopping me from getting worse. My friend who I was exposed to ended up in hospital on oxygen for 2 weeks.
It took 10 years from when Dr Susan Levine first wanted me to get IVIG to this year when I finally got it. Hematologist and Insurance company had to wait until IGG went under 600. I have been doing it monthly since February (with a 3 month break to see if I could maintain higher levels as per insurance) and have not had any negative side effects. I get Zyrtec and Tylenol prior to IVIG. Mostly, I feel less “flu-like”, my allergies clear up a bit and terrible mouth sores go away. I don’t have more energy per se but actually do because I don’t always feel like I’m coming down with something. Not having the mouth sores for 3 weeks out of 4 is worth the $500/mo copay since the meds don’t work anymore. I also do feel as if my immune system is getting a boost during the pandemic. I am very careful but am also very susceptible.
Just a note. Most infusion centers in the US have very highly trained personnel who look for issues patients might be having and respond to them immediately. That has been my experience at least. I am impressed. I would not go to a hospital infusion center as the costs are much higher.
I have lived with ME/CFS for 38 years. It has not been easy. I have been dismissed and ignored by many doctors, particularly neurologists. Fortunately I have also had caring G.P. doctors. But they say they know nothing about ME/CFS. I would like to contribute to the study of the connection between long-haulers and ME/CFS. I have been a professor and writer all these years, with family, colleague and student support. How can I be helpful?
Because I have ME/CFS will the vaccines, soon to be available, trigger a more difficult, even more sustained severe ME/CFS reaction, e.g. set me back to incapacity to do anything for six months or even permanently?
Are there any people with MECFS who have had an FDG PET Scan that showed hypometabolism in the cerebellum, brainstem and occipital lobe?
I have OCHOS, although I don’t have any of the other conditions that the patient in this case study had. I’m assuming she must have been very unwell to receive IVIg. My OCHOS definitely has an autoimmune cause, but I’m only sick enough to get hydroxychloroquine so far. Can’t tell whether it’s working yet.