

This blog is one of a continuing series of blogs that are attempting to peer into the future and see what treatments possibly await us. This blog provides an overview on CoQ10 – what forms work best and how to take it – and then takes a look at the next generation of more powerful CoQ10 supplements we may see.
- Are Intranasal Drugs the Future for ME/CFS and Fibromyalgia?
- Glial Cell Inhibitors: The Next Sleep Drugs for Fibromyalgia and Chronic Fatigue Syndrome (ME/CFS)?
- Cooling the Flames: Possible Approaches to Reducing Neuroinflammation in Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia
- Future Drugs for Fibromyalgia and Chronic Fatigue Syndrome (ME/CFS)? A Clinical Trials Survey
- Could Fibromyalgia Patients Linalool Their Pain Away (Someday)?
CoQ10
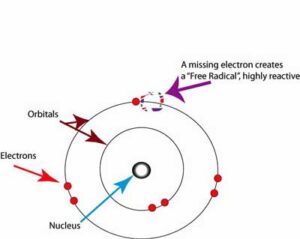
Free radicals are produced en masse during ATP production. Unless they are mopped up by antioxidants like CoQ10, they will snatch electrons from cellular membranes, causing havoc.
Coenzyme Q10 (CoQ10) is best known as an antioxidant – a scavenger of the free radicals that knock holes in the lipid membranes protecting our cells – sometimes setting off a free radical chain reaction. CoQ10 also mops up free radicals produced during energy production inside the cell and is an ATP production enhancer. If “dirty” energy production is occurring – as has been suggested in ME/CFS – CoQ10 might provide a way to clean up the mess and increase energy.
One of the most well-known and broadly used supplements, CoQ10 has been prescribed and/or studied in a surprising array of diseases including cardiovascular disease, diabetes, viral hepatitis, Parkinson’s disease, periodontal disease, and migraine, as well as fibromyalgia (FM) and chronic fatigue syndrome (ME/CFS).
Given that many of these factors have been implicated at one time or the other in both fibromyalgia and chronic fatigue syndrome (ME/CFS), CoQ10 looks like it might be a good deal for both diseases.
Fibromyalgia
Spanish researchers have done the bulk of the investigations into CoQ10 and fibromyalgia. The most recent FM study – a small placebo-controlled crossover trial – found that adding CoQ10 to Lyrica (pregabalin) (300 mg/d (Mega Life Sciences – Thailand) further reduced pain, anxiety, mitochondrial induced oxidative stress and inflammation, while increasing the levels to two important antioxidants (reduced glutathione, superoxide dismutase).
A small (n=20) 2017 placebo-controlled study found that 300 mg/day (divided into 3 doses per day) of CoQ10 from Pharma Nord, Vejle, Denmark resulted in clinically significant improvement in depression, anxiety, and hostility, and was of moderate statistical significance in reducing somatization, and obsessive–compulsiveness. That finding, of course, suggested that those behavioral characteristics derive from high levels of oxidative stress and inflammation.
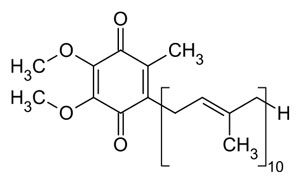
CoQ10 is a multipurpose molecule. Not only is it one of the most powerful antioxidants, but it also plays a role in energy production.
Apparently, the same trial (but another study) also found that CoQ10 produced significant reductions in fibromyalgia impact scores with reductions in pain, fatigue and morning tiredness most prominently occurring. Physiologically, reductions in inflammation, increases in antioxidant levels, mitochondrial biogenesis and AMPK gene expression were found.
Another small study from the same group found that CoQ10 increased serotonin levels and reduced depression in fibromyalgia. In 2012, Spanish researchers found that CoQ10 restored catalase and ATP levels in FM patients and significantly improved symptoms, including headache.
While the study results suggest CoQ10 may be helpful, a recent Spanish study did not find (probably to their surprise) that FM patients’ CoQ10 status was helpful in differentiating them from healthy controls. Thus, while CoQ10 supplementation was shown to be helpful in this small trial, problems with CoQ10 did not appear to be core to the disease.
It should be noted that CoQ10 assists ATP production in two of the five mitochondrial complexes (II. III.). Mitochondrial problems that do not affect those complexes probably won’t be helped by CoQ10. (The study did find mitochondrial issues with the FM patients appeared to have more mitochondrial degradation).
Chronic Fatigue Syndrome (ME/CFS)
In 2016, the Watanabe group’s small (n=43) placebo-controlled, double-blinded study from Japan found that 150 mg/day of ubiquinol-10 (the reduced form of CoQ10) for 12 weeks improved autonomic nervous system and cognitive functioning.
A larger (n=80) randomized, controlled, double-blinded Spanish trial found that a CoQ10/NADH mixture (50 mg CoQ10, 5 mg NADH, 40 mg Vit. C, 20 mg phosphatidylserine, 40 mg of vitamin C) taken 4 times/day found a trend (not statistically significant) towards a reduction in fatigue and no effect on pain levels or sleep. A similar CoQ10/NADH trial found a significant reduction in fatigue.
In 2005, Maes found very low plasma CoQ10 levels in ME/CFS.
Conclusion
On the plus side, most of the studies are placebo controlled and the results are mostly encouraging. On the downside, the studies tended to be quite small and many of them came from one research group.
Since the mitochondrial problems, if indeed they are present in FM and ME/CFS, are not clear – it’s not clear that taking CoQ10 will assist them. Fisher’s recent study, for instance, found problems in complex V of the mitochondria in ME/CFS, which is not one of the complexes affected by CoQ10.
There is another way that CoQ10 might be helpful, though – as an antioxidant. Increased levels of reactive oxygen species (free radicals) are one of the most consistent findings in ME/CFS and FM.
Better Blood Flows?
Kaneka Nutrients recently reported that healthy people with dyslipidemia – high rates of lipids in their blood – who took 100/200 mg/day of ubiquinone significantly increased their blood flows and reduced their levels of LDL oxidation.
(Lipid peroxidation/oxidation occurs when free radicals, in an attempt to achieve balance, rip electrons out of cellular membranes – often producing a free radical chain reaction.)
That’s an interesting finding, given the possibly reduced blood flows in ME/CFS, and the no less than five studies since 2001 which have found increased levels of lipid oxidation and/or free radicals in the blood of people with ME/CFS. Findings like those generally set people up for increased risk of cardiovascular illness. With virtually all ME/CFS patients, in particular, being unable to engage in strenuous exercise, anything to clean out the blood vessels may be a good idea.
Using CoQ10
The Two Forms of CoQ10
- Conventional CoQ10 or Ubiquinone – is the oxidized form of CoQ10, this form is more stable but has to be transformed into ubiquinol first. As we age, we become less able to convert CoQ10 to its usable form. Some people, particularly of Hispanic or Chinese descent, may also lack the enzyme to transform ubiquinone. Eating green, leafy vegetables may help.
- Ubiquinol – is more “hydrophilic” (i.e. it is absorbed better) and is the form of CoQ10 which scavenges free radicals in the mitochondria and cellular membranes, and it increases energy output. Our mitochondria naturally produce enormous amounts of free radicals which need to be mopped up.
Life Extension reported that one study showed that it took just 150 mg of ubiquinol to produce the same CoQ10 blood levels (3.96 mcg/ml) as 1,200 mg of CoQ10 (ubiquinone) over four weeks. Mice aging studies suggest that ubiquinol may be far superior for older patients. In low CoQ10 disorders – which both ME/CFS and FM may be – the goal is generally to get CoQ10 levels above 3.5 mcg/ml).
Dose
Life Extensions recommends 100-150 mg of ubiquinol daily for adults over the age of 30. It recommends 200-300 mgs of ubiquinol a day for those attempting to receive its “anti-aging” benefits. They noted that large doses (150-300 mg) result in an “exponential increase in blood CoQ10 levels”, which is sustained longer.
Dr. Mercola recommends starting with 200 to 300 mg per day, and then ramping down to 100 mg/day after three weeks when your CoQ10 plasma levels plateau. If you experience a lot of stress, though, 200-300 mg/day Is recommended. Other reports, though, suggest that it may take up to four weeks for the CoQ10 levels in your blood to reach their maximum levels.
The Future CoQ10
The CoQ10 of the future may be quite different from the formulations available today. A Spanish group recently produced a broad overview of the field “Coenzyme Q10: Novel Formulations and Medical Trends“- with a focus on CoQ10 future prospects.

Much work has gone into developing a better CoQ10.
CoQ10 has a lot of potential but there is a catch – low bioavailability. CoQ10 is a large molecule that doesn’t disperse well across gastrointestinal barriers; i.e. if you take CoQ10 orally, the intestinal absorption is poor. In fact, rat studies indicate that only about 3% of the orally ingested Coq10 is absorbed. The authors noted that CoQ10’s low bioavailability means it’s often not prescribed for conditions it could conceivably help.
The traditional way to improve CoQ10 bioavailability has simply been to pack it in oils. People taking CoQ10 should note that it’s practically insoluble in water and should be taken with high fat meals. The oil formulations increase drug solubility in the gut and enhance drug transport via the lymphatic system. Negative factors, though, such as the poor dispersion rate of the supplement in the gut, its not so stellar mixing ability, and the large particles that are still present, inhibit its bioavailability.
The desire to get more CoQ10 to the tissues has resulted in a surprisingly fertile field of experimentation with many approaches being tried. Several attempts (oil solution and suspension, lipid and surfactant-based emulsion, solid dispersion system) have been made to increase CoQ10’s bioavailability, but the authors reported that the bioavailability remained low.
Researchers have not given up, though, and recent efforts have been more successful.
- Nano-liposomes – Freeze-dried nano-liposomes with “long circulating elements” that improve the stability, and prolong circulation times, appear to increase bioavailability.
- SEDDS – Lipid-free self-emulsifying drug delivery systems (SEDDS) which feature surfactants that reduce the surface tension of CoQ10 – allowing it to be more easily absorbed through the gut wall – appear to be effective.
- SNEDDS “Self-nanoemulsifying” CoQ drug delivery systems or SNEDDS have been developed to increase CoQ10’s delivery across the gastrointestinal membranes. These delivery systems use oils, surfactants and a drug to produce a product which, when subject to the kind of agitation found in the intestinal tract, produces droplets small enough to ooze through the gut wall into the blood. Early results suggest this approach may work with much lower levels of CoQ10 able to be used.
- Lipid Free Nanoparticles – the goal – to take the fat and its problems with dispersion, emulsification, etc. out of the equation. In this approach, nanoparticles of CoQ10 are modified with surfactants using a hot, high pressure system. The surfactants allow CoQ10 to ooze through the cell membrane and slip between the tight junctions present. Animal studies suggest the process works and bioavailability is significantly enhanced.
- Oleogels – solubilized CoQ10 – “emulsions where CoQ10 is dissolved in an oil-dispersed phase” – have increased bioavailability. Solubilized formulations of CoQ10 do appear to be available.
- Water-based CoQ10 solutions – The authors reported that a water soluble version (Q10Vital) has been produced which is as effective – if not more effective- than oil-based preparations. Qunol has a liquid from of CoQ10 which they say is both water and oil soluble.
Creating forms of higher bioavailable CoQ10 is clearly a growth field. Just in the last two months, two new formulations were published in the scientific literature.
This is not to suggest that ubiquinol in its present form cannot be successful. Studies show that taking it in sufficient amounts for 4 weeks or so results in increased levels in the bloodstream. Better, more effective forms in the future are likely, however.
Note that if you’re buying through Amazon, be sure to purchase supplements from a reputable retailer based in the U.S. (Even then, counterfeit pages identical to the retailers’ pages can be made.) A 2017 Forbes article indicated that the Chinese have flooded Amazon with counterfeit products, and Amazon has done little to combat that. It stated that 25% of Amazon’s vendors are Chinese. Jill Carnahan recommends avoiding Amazon and buying direct from the manufacturer, if possible.
Conclusions
CoQ10 is a mighty antioxidant and plays a key role in ATP production as well. Fibromyalgia and ME/CFS studies, while small, do suggest that CoQ10 might be helpful with pain, cognition, mood and other symptoms.
It’s not clear that CoQ10 will help mitochondrial functioning in FM or ME/CFS, but it should help clean up the free radicals that studies indicate are present.
CoQ10 is best used in its ubiquinol form, which is better absorbed and has more potent antioxidant properties. Older people, in particular, are advised to use ubiquinol.
Suggested doses for healthy people appear to be around 100 mg/day. For those under stress and those wishing to receive CoQ10’s possible anti-aging properties, the suggested dose is 200-300 mg/day. The study parameters suggest that four weeks should be allowed for CoQ10 (ubiquinol) to reach its maximum levels in the bloodstream.
Because ubiquinol is fat soluble, it should always be taken with high-fat meals.
CoQ10 has been prescribed for many diseases but the authors of a recent overview suggest that its uses have been limited by the difficulty it has making its way through the gut wall into the blood.
A surprising number of different formulations have been created, with several showing promise. One form – solubilized CoQ10 – does appear to be available. Expect more effective forms of CoQ10 to show up in the future.






I have me/cfs and have tried taking CoQ10 in various forms quite a few times. I usually initially get a slight boost in energy, but then unfortunately experience flu-like symptoms, so have to discontinue (even with low doses – I think I was only taking 30 mg once or twice a day). I have read that this is a possible side-effect, but wonder what is causing it.
This actually happens to me frequently with things that help. I get an energy boost and then fall apart…So strange.
It hasn’t happened with B3 – which does help – which is interesting.
Cort, is it possible that the flu like symptoms may be the body going into a Herxheimer reaction? Just a thought.
Thanks, Cort, I might give B3 another try. I already take a Vit B complex supplement, but perhaps I might try adding in some more B3. (I think when I tried taking it alone in the past, I had a weird side-effect – my stool became lighter [sorry for the gross detail 😉 ] – which was perhaps suggestive of an effect on the liver, which I read could be a side-effect of B3).
Very interesting that you and lots of people in the posts below are reporting similar side-effects for COQ10 and other supplements. Susan Sikes – I don’t think it is a Herxheimer reaction – about a decade ago, I tried taking COQ10 for at least a couple of months, and the side-effects didn’t subside – in fact, I wondered whether I had caught mononucleosis. I don’t think a Herx reaction could last that long.
I suspect that the CoQ10 gives an initial boost to the given energy pathways, but this puts added strain on other components and aspects of the pathways – which may also be depleted/disturbed in me/cfs sufferers – and so the sufferer feels worse or crashes.
Excellent work as always. I too have found that almost anything that helps, nimodipine, taurine, various high dose antioxidants, stops working. I wonder if what is happening is that the core metabolic “bottleneck” is still there so increasing the function of any pathway just causes metabolites to accumulate upstream which eventually causes problems. I’m highly skeptical of the supposed “herxheimer reaction”.
Core metabolic “bottleneck” – great term! I will remember that. It’s amazing how things work and then poop out…
George and Cort,
Have you considered that once you begin taking Co Enzyme Q10 at 100 or 200mg, once your body adjusts to it, that you might need to INCREASE the mg again to get sustained benefit? In the big picture if our health, 200mg is a very small amount of CoQ10 to take.
If you do additional research into CoQ10, it is possible to take up to 1000mg a day without negative side affects.
Thanks for mentioning that Dian. As I’m 6’6″ I imagine that my dose should be higher anyway. If I’m doing OK at 2-300 mg. I will go up and see how it goes. If anything – just cleaning the junk (free radicals) out of my bloodstream would be a bonus.
Right, same experience, I do well on B2 (handle stress better) but feel bad in the evening. B3, which I always just thought of a useful distraction, seems to have about a 2 week efficacy life span, then I stop for a few days. I get “waves” (5 hrs) of depression and it does seem to help with this.
Interesting given that B3 is a blood vessel dilator – https://healthfully.com/supplements-dilate-blood-vessels-6615780.html
Vitamine B3 also increases the NAD+ and NADH pool (as it is a building block for NAD+/NADH). So it helps to “boost the mitochondria”. As explained below, boosting the mitochondria is like increasing the speed of the conveyor belt.
However, “the mitochondria” is not a single thing working in unison. Speeding up one or several parts while other are bottlenecked is like speeding up all of the conveyor belt while some some workers on it can’t follow the speed.
When this happens on a car building conveyor belt then you get things like parts pilling up on the conveyor belt and tumbling of it or doors attached to only one hinge rather then two. Neither are very good.
In the case of having a bigger pool of NAD+/NADH and too few oxygen, more NAD+ will convert to NADH and hence more NADH will pile up. This in turn risks to create more, not less, ROS if you increase vitamin B3.
Note: Increasing it and being actually able to produce more ATP can be a good thing even in partial hypoxia *IF* your cells can use enough of the extra produced ATP for recycling glutathione for scooping up the extra ROS and have some spare energy left.
IF is the big thing here, with IMO bigger chance in the less severly ill and some less oxygen starved subgroups.
Could be with the extra energy boost you exert more and trigger PEM?
It’s very strange. It comes immediately after I experience energy and feelings of real health. My muscles feel relaxed and supple – and then it comes – these flu-like feelings, joints sometimes start popping and this incredible lethargy….
All those are different from my normal PEM symptoms (tight contracted hot feeling muscles, racing heart, dizziness)
I have taken ubiquinol for years, and recently added a product called mitoQ (mitoquinol mesylate). Any research available on this? Does it fit into any of these future categories?
Hi Andrea, I was checking to see whether Terry Wahls mentions CoQ10 and found this interview she did with William Stow from MitoQ – Breakthroughs in Targeting Mitochondrial Dysfunction with CoQ10
https://terrywahls.com/targeting-mitochondrial-dysfunction/
Apparently some CoQ10 is too large to get through the mitochondrial wall, so MitoQ is designed, according to William Stow, to be ‘a shortened version of CoQ10 given a positive charge to enable it to be drawn inside the body of the positively charged mitochondria.’
Try taking it 100mg at a time.get used to it and then increase to 200mg after 4 weeks…then wait a month and go up to 3. Sometimes taking such a high dose in the beginning leads to flu like symptoms. Your body must get used to it.
Thank you for bringing this up! If you didn’t, I would. When I take CoQ10, I feel so much better for a couple of hours. Then, after four or five hours, I have tremendous pain and muscle cramping. This also happens to me with other things that are supposed to give people energy and relieve pain — Alpha Lipoic Acid, Tumeric, etc.
You, Tamesin and Ryan M report clear side effect. Issie did too if I remember correctly. I had no response good nor bad with it.
I think the cause of potential trouble is this:
“CoQ10… …is an ATP production enhancer” and “It should be noted that CoQ10 assists ATP production in two of the five mitochondrial complexes (II. III.)”
are IMO wrong or at least cutting corners too much.
CoQ10 as far as I understand improves NADH and FADH2 production. From NADH and FADH2 the ATP synthase, a key part of the mitochondrial membrane, can make ATP *IF* nothing goes wrong AND the mitochondria have sufficient access to oxygen.
=> When (enough of) our cells have sufficiently good access to oxygen (during most of the time) then CoQ10 can improve ATP production and recude oxidative stress.
=> When increasing NADH and FADH2 production (by adding q-CoQ10) while having frequent bad bouds of local hypoxia (during and after too strong effort) you build a surplus of NADH and FADH2. That does two things:
* deplete NAD+ for glycolysis (hampering anaeorbic energy production you badly need during hypoxia)
* create plenty of EXTRA ROS as NADH and FADH2 are unstable high energy carriers that dump their energy to form dangerous ROS when piling up too high.
=> IMO the better your oxygenation, pacing and the fewer you exhaust till PEM, the more chance coQ10 could benefit you. The worse your oxygenation, pacing and the more frequent you hit PEM the higher the risks are IMO that it will backfire.
Can you please explain that in English ?
The mitochondria produce energy by breaking down fuel, like pyruvate derived from sugar, step by step. The end result of all these little steps, if all goes well, is providing us with ATP. It’s like an episode of the TV show “How do they do it?” You start with raw pyruvate at the beging of the conveyor belt and end up with ATP at the end of the conveyor belt.
CoQ10 does help produce two chemicals called NADH and FADH2. Those two things will help the mitochondria produce the desired ATP. They are essential as an intermediate step in that long conveyor belt.
Producing more of these NADH and FADH2 intermediates does help produce more ATP at the end of that conveyor belt. The problem however is that the mitochondria simply can’t convert NADH and FADH2 to ATP if they don’t have enough access to oxygen. Let the mitochondria having poor access to oxygen now be a problem in ME (and FM?).
If the mitochondria produce plenty of NADH and FADH2 but have too few access to oxygen, then they start to produce MORE ROS, a lot more ROS. That may seem incredible, but the mitochondria produce too much ROS at two conditions: too few oxygen and too much oxygen.
Producing more NADH and FADH2 then there is oxygen available to convert them to ATP is a (or THE) major reason why the mitochondria produce ROS at too low oxygen conditions.
Compare it a bit with driving a car in the peaks of the high Andes mountain range. It will have plenty of trouble producing enough power to ride up the steep slopes. In order to be able to make it despite the engine stuttering, you can push harder on the gas pedal. The problem however is not a shortage of gas but a shortage of oxygen.
Increasing the amount of gas going to the engine can work just well enough to push the car over the mountains, but much of the fuel will leave the engine poorly burned. It will leave a thick black and toxic smoke through the exhaust. The engine will make all sorts of weird noises. Just increasing the gas input during this lack of sufficient oxygen is rather damaging to the car engine.
Requiring less power from the engine, by shifting to a lower gear and driving slower, or adapting the engine to get more oxygen would be the better option here.
Requiring less power and let the engine time to rest is the equivallent of pacing. Adapting the engine to get more oxygen would be the equivallent of doing exercises to improve blood flow, do breathing exercises and try to get the Red Blood Cells in better shape.
Taking supplements in order to produce more NADH and FADH2 therefore is hoping that oxygen supply to the mitochondria isn’t too crippled because if it is, you can expect things to fire back.
It can work and even be beneficial as long as the oxygen supply problems aren’t too bad, but if they are you can expect this hack to fire back quickly.
Is that clear enough? I had to get the science right in the first comment, but I agree it’s really complex. I needed a rest after verifying and writting that first one too ;-).
That is so darn clear and thanks for explaining how oxygen is vital to pathway. I had no idea that mitochondria absent enough oxygen = lots of ROS. I am copying this to One Note….thanks for the primer, DeJurgen 🙂
I started to take the co q 10… my first negative reaction was a headache in the left front part of my head, so…
I took a couple of days off, then started again, no headache this time no head aches since just helps with my nerves in my legs and a general feeling of being 30 ears younger
IN CONCLUSION,
co q 10 works very fast, and coq10 works in blood circulation, coq10 must have been trying to clear a blocked blood vessel in my head, after the blockage was cleared and repaired, my headaches never returned
Great explanation. What does ROS stand for? Thanks.
Reactive oxygen species – a prominent kind of free radical.
Yes, thank you for explaining it a little better 🙂
After reading some of the comments (as I can’t read too much info without it overtaxing my brain) it made me realize not only how complex this disease is, but also just how complex and wonderfully made the human body is – everything is so finely tuned to work perfectly as it was meant to, but because of imperfection it takes only one small thing to throw the whole thing out and stop it working as it should. It’s how Albert Einstein explained it – the more I learn the more I realize how much I don’t know!
Hi, it is really a fantastic blog. I just want to know your source or lad address in Denmark, Sweden, Japan Or any Other labs from whom you have taken data. We are having naturally derived highly stable Water soluble form of Coenzyme. But struggling to get laboratory trials in India. Can you please send coordinate at following correspondence:
Email-nilesh2.84@gmail.com,
phone- +919904233104.
Interesting, I have pretty severe ME/ CFS, MCS and lupus ( or something similar).So take hydroxychloroquine.
I took ubiquitol for the first time, 100mg, and a few hours later felt sick, shaky, dizzy, hot and cold ( basically M.E fluey). Took HQL and an hour later am ok, sort of.
Forgotten to take it and vitamins last few days, and noticed this happen before, but so close to the ubiquitol, I feel maybe a rapid detox perhaps?
I’ve ME/CFS and is using 400 mg daily for the last 4-5 years. I’ve tried several brands but the only one working is the one from Pharma Nord with oil capsules. I take 200 mg twice at day (morning + evening) to get a 24 hour effect
https://www.jala-helsekost.dk/pharma-nord-bio-quinone-q10-180-kap.html?gclid=CjwKCAiA7939BRBMEiwA-hX5J5SdyGypgtQUuFCyC7YBQyBSRufXDO6NaDoO8SgN8ZGzdpEY0yvizxoCcWUQAvD_BwE
I haven’t yet read your full article due to fatigue, but if it’s not mentioned readers may be interested and amazed that we produce CoQ10 naturally after eating green vegetables and then sitting in the sun,
Because the Chlorophyll in our bloodstream after eating greens may react with wavelengths of sunlight that penetrate through our skin to reactivate the antioxidant Coenzyme Q10 (ubiquinol).
Here’s a Short 6 min video on the interesting phenomenon
How to Regenerate Coenzyme Q10 (CoQ10) Naturally | NutritionFacts
https://nutritionfacts.org/video/how-to-regenerate-coenzyme-q10-coq10-naturally/
Great article – thanks again!
Just wondering if anyone else is highly sensitive to CoQ10?
Even the smallest amount seems to overstimulate me. A few MG in the morning and I can’t sleep that night.
I’m 10+ years into CFS, for reference.
I have been taking CoQ10 for years. I buy the liquid Qunol brand at Costco where they frequently have sales. After reading your blog, I now realize I am not taking nearly enough and should probably switch to Ubiquinol.
I think the recommended dosage of many supplements is often too low for people like us who have problems. I am now going to up my dose. I’m taking half the ME/CFS amount–and mostly because of cost. All these supplements can get very expensive!
Now on to a different subject. I just listened to a lecture about chronic sinus problems in people with EDS. I know there are a number of people here who have both EDS and ME/CFS, myself included. Anyway, embedded in this lecture is a theory that the disorganized collagen fibers inhibit white blood cells from fully migrating through tissue in order to find and dispense infections, both viral and bacterial. Chronic infections, over time, can develop strong biofilms which further inhibit healing. What this doctor is hypothesizing is that the fatigue which is so common in EDS may be from the body continuously fighting low level internal infections–but not quite having the strength to completely eradicate them. Even antibiotics have trouble with biofilms. There may be some evidence that an overstressed immune system may eventually flip into an autoimmune problem.
I was quite intrigued with this idea and thought I’d share, although not sure how this might apply to people without EDS. I do however, remember sinusitis being mentioned here before. I won’t post the link (unless somebody really wants it) as it is mostly about sinuses, but the doctor is Dr. Subinoy Das and he might have more to say about this someplace else (but I haven’t yet looked).
Nancy, I would very much like to have the link to Dr. Das’ lecture regarding sinusitis. I’ve had sinus issues all my life…ME/CFS for 13. I’m now 63. It seems the past couple of years have been the worst ever. When my sinuses act up, my ME symptoms exacerbate. I’m not sure about any EDS, but do have a knee that tends to go backwards on me, and have been intrigued by the possible connection. I’ll see my PCP in January, so this may possibly give me more avenues to investigate. Thank you!
@Bottsie;
Here is the link to the webinar on sinuses; https://www.youtube.com/watch?v=vWIGPylrGgg
I have to warn you it is 1 and 1/2 hours long with introductory comments at the beginning, sinuses basics and then at about 20-30 minutes in they get to the good stuff. Towards the end there are some technical issues, but generally there is a lot of useful information–plus that interesting theory I described.
Do hope you get something from it!
increasing oxygen could be achieved through light excercise or other mofalities like ozone therapy.
This reminds me of the Klimas/Broderick CoQ10 study with Gulf War Veterans and ME/CFS patients you wrote about in September of last year. I’ve been taking the ubiquinol form of CoQ10 for a number of years, starting out at 100 mg. three times daily and now 100 mg once daily. Not sure it’s made a tremendous amount of difference but know it helps overall so will continue taking it. Also, a cardiologist said he thinks it’s imperative for anyone taking a statin drug to also be taking Ubiquinol CoQ10 so people might want to ask their cardiologists about that.
Ubiquinol works for me. I also take it in conjuction with a product from Enada called Co-Enzyme-1sublingual. Its the anti oxident form of B3. It does help on days when I need extra mental clarity and need stamina.
I only take a single supplement for my 12 year ME/CFS: 150mg/d of CoQ10 (Ubidecarenone). I’ve tried all manner of supplements over the years and this has been a godsend for me. I’d estimate it grants me an extra 1 hour of energy a day, and I need 1 less hour of sleep a night, giving me a huge bonus of two hours every day.
I get the “Healthy Care” brand which is quite cheap in Australia.
Thanks for this article Cort. I have been taking 150mg of the conventional form of co q10 but haven’t noticed any improvement…so will now be switching to the other form to see if it helps.
Good luck! I too have changed from CoQ10 to ubiquinol.
I took 800 mg daily a year ago after some obscure study suggested decrease in fibro pain. Nope. Some brand I don’t remember. There is another study mentioned on examine.com that used 100 mg t.i.d. for fibro pain so I have been doing that for a month, too tired now to get bottle in another room but is a standard brand with white plastic and green lettering selling lots of supplements on Amazon. Once again, zero effect.
I have found my fibro pain to be remarkably homeostatic in the sense that many things…travel, meds, supplements, etc. might work for a day or two and then my system reverts back to the default awful fibro pain. I accompanied someone to a small town in Mexico a year ago as a gift and had two pretty fun days there with minimal pain, on my usual useless tramadol/acetaminophen combo. The third day,
I woke up in the middle of the…fibro pain returns with a vengeance, and I wS miserable for the few remaining days. I think HPM axis is so involved in so many regulatory function that damage…physical, psychological, viral, toxic, etc….can reset the default to hell.
I have tried CoQ10 on a number of occasions and every time had a bad reaction to it. Can’t remember now the exact effect it had on me but remember feeling very unwell at the time. I also get the energy boost then deterioration when I have tried Acetyl L Carnatine Feel great at first then very unwell. Very mixed reactions to anything I take in the way of supplements but never found anything that I feel really helps. Also very drug intolerant now. M.E. does such strange things to our bodies and it seems very hard to try to work out how to deal with it. Seems a lot of things will have great effects for some but make others unwell.
CoQ10 helps converting more glucose/pyruvate to energy.
Acetyl L Carnitine helps bringing in more fatty acids in the mitochondria for conversion to energy.
For many ME patients, both of these give first a quick burst of extra energy and then fire back.
That may be another illustration that producing enough energy may not be the first problem in (a large amount of cases of) ME, but producing enough energy without too much damaging side effects. It seems that in a large subgroup of ME patients the body wilfully and decisively shuts down the energy production in order to prevent this damage.
When we find new tricks to work around this safety mechanism, the body is taken by surprise and we are more energetic for some time untill the body adapts and finds a way to shut down our attempt at cheating. Then we are left with less energy then before because we created extra damage and the body has to do extra effort to block our cheating hack.
For those who’s body shuts down their mitochondria because high energy production is too damaging, it very likely is better to find ways to reduce the damage produced by energy production rather then finding ways to override the bodie’s safety mechanisms.
This was interesting. I had not thought that perhaps my mitochondria when pushed are producing too many free radicals. CoQ10 might help with that…hmmm. That is actually the first possible explanation that anyone has ever provided.
I am in the energy produces side-effects category. I had to quickly stop taking the oral rehydration solution because it was improving my health.
I had plenty of experiences of drugs or supplements before working for one or two days and done then too.
Even more weird, I had several times I take a new drug and I feel clearly better for a few days. I keep taking it, nothing or just the side effects. I stop taking it (always be carefull building real drugs down, sometimes stopping quickly can be really dangerous; experienced that too) and I feel clearly better for like a day too and then things go back to normal.
@Cort: can you explain what you mean with “I had to quickly stop taking the oral rehydration solution because it was improving my health.”? It sounds interesting but I fail to read what you mean to say.
I’ve had ME/CFS for 28 years, and over the years have tried just about everything. This is a great article, Cort and it reminds that both COQ 10 and NADH did help with my energy level. I’m not sure why I quit taking it, but pretty sure it was because of the cost. I’m ordering both tonight from Pro Health because I think they have the highest quality products. Could someone please tell me how much B3 I should take?
Many Thanks!
@dejurgen, I really relate to what you’re saying about high energy production being too damaging, and thanks for your car and conveyor belt analogies, they convey the concept well.
I’ve always been baffled that I can have a sort of “hyper-overdrive energy” — like an excited/nervous energy — when I was actually utterly fatigued and would inevitably collapse afterwards in a puddle of increased symptoms for days. I half-jokingly called it “over-draft energy”, which carries steep interest charges. After getting too far into “energy debt” I started having to borrow “loan shark energy”, and as we all know from the movies, those guys just make sure you’re always in debt… and never mind interest, they shoot your knee caps!
I love what you say about it being better to find ways to reduce damage than to just override safety mechanisms. I strongly feel this should be mainstream advice and practice, rather than the ironically self-defeating “productivity über alles” mindset that our modern society is so caught up in.
@Cort, you make me laugh with your “I had to quickly stop taking the oral rehydration solution because it was improving my health.”
But I relate, it’s like some parts of your body can’t keep up with the state of health other parts are in. Dejurgen’s sped-up conveyor belt meets Brian’s bottleneck…
I just been taking 100milgram CQ10 just for 3 weeks my polimialger has so improved able to excercise again it may be a little soon but l carnt think any think else l am takeing can it give you polpertations ?
Hello – not quite on coQ10…
because dyslipidemia is mentioned:
I’ve been reading this blog:
https://chronicallycaroline.com/2019/06/02/keto-and-me-part-i-an-elevated-heart-rate/
and
https://chronicallycaroline.com/2019/12/18/10-tips-for-getting-started-on-a-ketogenic-diet-with-me-cfs/
She has superb research and writing skills – really good at communicating and presenting how things connect.
Even if one’s particular brand of dysfunction doesn’t fit with hers, there’s lots to learn that may still apply, or can help figure out how to go on about adjusting one’s diet.
Figuring out how to allocate activity/rest and food to support our energy production
– alongside the nutraceuticals.
can go longer ways, as I see it.
Approaches are going to be a little bit different for each one of us, depending on how our bodies adapt at meeting the meatbolic hiccup. Studying your individual biochemistry may help (the use of plasma amino acids has been useful for me). There’s probably subgroups, so when you find someone with your same profile, and they found strategies that are working – something to take note of.
I’m supposed to be taking a break myself! to change life-long habits of energy usage…
wanted to share this resource
Thank you for sharing it. I think everyone would be well served by subscribing to Caroline’s blog.
Thanks Meirav, I’ve signed up for Caroline’s blog – I had a quick look, as I’m fairly tired at the moment – she looks right up my street.
Interesting that this blog should pop up just as I have run out of CoQ10 and wondered whether I needed to get any more. I started taking CoQ10, in March/April 2019, because I kept hearing about it from Dr Nancy Klimas, Dan Neuffer and Terry Wahls M.D. I saw some half price in the health food shop and decided I didn’t mind trying it out at 15 euro for 30 capsules. Now, it may or may not have had a small effect on my stamina because as Dejurgen says in his three part series – don’t try 3 things at once because you won’t know which things help. The other two changes I had made was to try and calm down and get better sleep.
I might leave the CoQ10 out for a bit and then re-introduce it and see what happens. I always look to see whether I can find the same nutrients in food and so I do eat things that apparently supply CoQ10.
I also read somewhere that Magnesium is needed for the mitochondria to be able to make ATP. I remember from previous discussions that some people may have a problem with Magnesium.
I didn’t have any issues taking CoQ10 and I thought it might have been helping – hard to say. I still take Magnesium and a load of other things I’ve tentatively built up over the last few years.
In the last week or so, I’ve just started feeling fairly normal – in energy terms. I’ve been working at it for years – trying to very slowly to achieve small improvements. I see it as sort of going backwards to come forwards. So to rest and pace as much a possible. Not to push forward but to hang back.
I’ve also been trying to engage in some sort of dialogue with my ancient brain, which has been convinced my life is a major catastrophe. I’ve been trying to communicate that, despite some evidence to the contrary, my life’s not too bad. Ancient brain does not have a window seat and only knows what’s going on from what it picks up from me and my reactions. Living in constant flight/fight/freeze is an exceptional drain on my energy supplies and I found it was unsustainable.
I still have immune issues – there’s no dialogue possible with General Immune. As a dictator, what they say goes – I’ve learnt that the hard way!
Got to do a blog on magnesium and my experience is similar
It’s gotta be a huge drain….It’s not that everyone – healthy or not – doesn’t do this – it’s that consequences are so much worse, I believe, if you have energy production problems.
Keep conversing with your ancient brain 🙂
What I wonder about:
if ATP is leaking out of the cell when it is stressed –
would producing more ATP
lead to more of it leaking out
and increase signaling activity to neighboring cells to go into ‘protection’ mode?
and hence the slowing of metabolism
that produces the aggravation of symptoms (PEM/crashes).
This in turn reduces ATP production
and less of it becomes available to leak out as well.
We start to feel a little better, expend more energy again
and the cycle repeats over and over again
The greater the imbalance,
the deeper the state/severity of ME/CFS,
the longer (and longer) the stays in PEM are
{per Cell Danger Response theory, as it is proposed}
– – – – – – – – – – – – – – – –
There is mitochondrial stress and there is cellular stress.
Are they one and the same? not sure – need to read more.
https://febs.onlinelibrary.wiley.com/doi/pdfdirect/10.1016/j.febslet.2007.07.001
Lack of oxygen can be one source.
Another is calorie restriction – in ME/CFS, that takes the form of drops in blood glucose (hypoglycemia episodes) because of the energetic dysfunction
(easier to control during the day. at night, during sleep…)
There is osmotic stress, aldehyde stress…
What else is there? Which ones are at play for us?
The implication being that we may not necessarily want to focus on making more ATP
– instead, focus in reducing cell stress, in the different ways in can be provoked and reducing the ‘toxic’ substances produced.
Support the way your particular metabolism adapts to the glitch in ME/CFS energy production in ways that produce less byproducts that may build up to higher than normal levels. And address reducing those high levels as well.
Then we can make better use of ATP,
hopefully less of it leaking out –
May we perhaps even heal 🙂 ?
This opens up different avenues for therapeutic interventions – there’s PLENTY to work with here.
Since it’s easier for our system to get out of balance
to have a more pronounced response to even insignificant stimuli,
to take longer to come back to baseline
– building islands of stability in our day-to-day life.
Which is the same thing that Dejurgen is saying, I think.
– – – – – – – – – – – – – – – –
What about approaches targeting antioxidants?
And look how interesting, some are studying mitochondria in anxiety and neurotransmitter business:
https://www.quantamagazine.org/mitochondria-may-hold-keys-to-anxiety-and-mental-health-20200810/
https://www.epfl.ch/labs/lgc/
I think it’s possible
why supplementing with amino acids that one is low in can be tricky:
The body may desperately need them
– may ‘suck it up’ like a desert absorbs water from the rain –
it goes towards where it has been sorely missing
but quickly feeds into the dysfunction
and the by-products it produces take a while to build up to levels that are detrimental
That’s the delay in feeling ill effects – the time it takes to reach ‘toxic’ levels.
– there is a reason they are low to begin with…
I have wondered if tiny tiny amounts will do the trick…
enough for the good effects, not enough to build up by-products.
I have better experiences with end products…
This is what happened with me Meirav, over the last few years, in brief. I had been becoming more and more intolerant to different foods. By 2017, I was thin (fab!) but I was also pale and barely ticking over. Then I discovered that my reaction to eating chocolate was that I became fat (!), rosy cheeked and my blood pressure soared. From teetering through my day, I was now fired up and flying through my day. At first I thought this was great but it had consequences. So in November 2018, I had to go to the hospital to have a small procedure. On the Monday, I could feel my brain running out of energy, so my blurry brain said go to the supermarket and buy some chocolate. Now I had been having reactions to it, where I felt very nauseous, but I had sort of forgotten that and put it aside. I ate half of the 60% dark choc bar 125g on that Monday and half on the Tuesday. By Wednesday I was feeling unwell and then on the Thursday I had to fast and go to the hospital. I felt really horrible.
As the nurse was taking my blood pressure, I could see the large screen on a wheeled pedestal. I was scanning the numbers and said what’s the 168? She replied that’s your blood pressure. What! It immediately went up to 198! So all day, as I lay on the bed, quietly reading my book, feeling fairly relaxed, my blood pressure kept spiking. They were contemplating whether to let me have the procedure. Anyway it went ahead and even though I was unconscious, my blood pressure went up to 178. Also when they took a urine sample, it was the colour of mahogany wood – clear but dark brown. The nurse did ask whether I’d had a problem with my liver? No, I said. All I wanted to do, by that stage was get the procedure done and get out of there. Beam me up Scotty!
But I did have Glandular fever/Mono, at 17 and that I believe effects the liver. I also developed a massive problem with fructose, in 2007, when all this started after massive stress/flu and fructose is processed by the liver.
So, what I’m trying to say is – that when I was running on nervous energy, not sleeping properly or for that long – I was wired – and that for me seemed to mean that I couldn’t process food properly and that then had a domino effect around my body.
Now that I’m much calmer, not wired, sleeping much better, staying within my natural energy limits, I can eat the exact same chocolate – without that reaction, I describe above. I do find however, if I eat too much on consecutive days, it sets off my immune system. So I’m going to try just having some every 3 days or so and see what happens.
Did you ever notice ammnonia exuding from your skin, maybe with sweat, during that period, and also when you lost weight and experienced worse health?
Or stronger smelling urine?
It sure is good you are finding your way to better health!
I liked your sentence re: ‘closing the door and shutting the world out to decamp to bed and slumber’.
I like conjuring this image
I’m attempting a vacation from the world of ill health myself… 😉
Yes I too have bad side effects from most “boosting” supplements… Coq10 in most forms, ALA, amino acids and everything thing in that vein. I believe our bodies are down regulating for a “reason” for sure!
Also, our metabolism is often turning to catabolism to make up for the energy glitch at the entrance of the Krebb’s cycle, it seems. This is the breaking down of amino acids to produce ATP/energy and it releases nitrogen byproducts, which may be building up to higher than normal levels in ME/CFS then.
This is one of the areas the Australian research team is investigating.
https://www.omf.ngo/2020/10/12/nitrogen-metabolism-and-testing-nitrogen-hypothesis-in-me-cfs/
Constant accumulation of ammonia in the blood can lead to effects of ill health,
both from the high levels and from ‘taxing’ organs involved in elimination mechanisms, perhaps.
“When excessive amounts of ammonia enter the central nervous system, the brain’s defences are severely challenged. – A complex molecular chain reaction is triggered when the brain is exposed to excessive levels of ammonia. We have found that ammonia short-circuits the transport of potassium into the brain’s glial cells”
“Your body treats ammonia as a waste product, and gets rid of it through the liver. It can be added to other chemicals to form an amino acid called glutamine. It can also be used to form a chemical compound called urea. Your bloodstream moves the urea to your kidneys, where it is eliminated in your urine.”
A primer on ammonia
https://www.ncbi.nlm.nih.gov/books/NBK541039/
Ammonia inhibits mitochondria respiration, alters energy and amino acid metabolism, produces ROS in cells of the central nervous system
(what about in other cells, outside the brain?)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7657470
it would be interesting to compare the tables on this study to the ones from ME/CFS meat-a-bolomics.
It can affect muscles as well.
https://www.journal-of-hepatology.eu/article/S0168-8278(16)30474-3/pdf
Intracranial hypertension?
– – – – – – – – – – – – – – – – – – – – – – – – – – – – –
Some of the symptoms of hyperammonemia and Reye’s Syndrome are similar to ME/CFS – being very clear that it is not those conditions.
I do wonder if there is a small percentage of the ME/CFS population that is indeed not getting recognition for their inherited metabolic disorder. When I hear of someone severely ill, with seizures – my mind wonders: have they had a thorough workup for metabolic disorder and ruled it out before arriving at the clinical diagnoses of ME/CFS?
Even if it is one out thousands of patients – that is one person too many not receiving the care they need and a chance at life.
There are also nitrogen byproducts I have yet to read up on.
– – – – – – – – – – – – – – – – – – – – – – – – – – – – – –
This was all to say that perhaps some of these supplements are fueling a catabolic state,
and as such – will lead to higher productions of nitrogen byproducts. It may take a few hours, a few days, or weeks until they accumulate and show up as symptoms. Perhaps.
Fluge and Mella, in their 2015 meatabolomic study , divided amino acids into three categories by where in the Krebb’s cycle they participate and discern which processes are being affected.
https://www.meaction.net/2016/12/23/fluge-mella-and-armstrong-more-support-for-disordered-metabolism-in-me-patients/
If you have plasma amino acid results and do the same and compare, you may be able to discern how your particular biochemistry is responding to meet energy needs / ATP production.
I have a few areas that stand in stark contrast to those results – some amino acids that are not affected in the study, are for me and vice-versa. Bigger studies would maybe reveal my sub-group.
You don’t need to do this to get better 🙂
Trying to shift metabolism towards anabolism more often is a potential approach – a slow one at that. Otherwise you overburden your body and can get into REAL trouble. Your cells will suddenly have an abundance of nutrients and substances that they didn’t for a long time, and it may not be prepared to deal with that, potentially leading to more cellular stress.
Muscle-builders take glutamine to prevent catabolism and stimulate anabolism.
Heidi Collins – the one hEDS doctor that dares talk nutrition – has mentioned her patients tend to do well on glutamine.
Not sure how it jives with ammonia… per this:
Glutamine as a Mediator of Ammonia Neurotoxicity
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4714775/pdf/nihms-228735.pdf
Trying to get ATP to leak less out of the cell could also help.
When it completely stops leaking – my guess is those are that experience ‘spontaneous’ recovery.
Thanks Meirav. Fascinating stuff! Ammonia…who would have thought? I hope to interview Chris Armstrong about this.
Ammonia has been a long time research topic for Issie too. As I learned to trust on her “science intuition” often being right if she keeps on banging on the same nail, I had to look into that one too.
She is working on workarounds for the last half year. More to be read on https://www.healthrising.org/blog/2020/06/05/fight-flight-neuroinflammation-fibromyalgia-chronic-fatigue-syndrome/
With quotes such as:
“There is another thing I use to take ammonia and acetaldehyde down, it is a combo product of bee propolis/bee pollen and royal jelly. I sometimes interchange it with Yucca. It also is a good help for MCAS issues. I do have a CBS mutation. (Issues with sulfur pathways, and that forms more ammonia.)”
She and I are also trying to work on improving urea excretion through the gut. Urea gets excreted not only through urine but also through sweat (a minor route) and the gut (a major route). Trying to get on top of potential ammonia problems requires a good knowledge on how to reduce reabsorption of that urea from the gut.
(Ammonia) Reabsorption by the gut, or taking up the urea and ammonia again and again, is a problem when you have poor gut flora. We discussed that topic spread over HR too. Wish we had time to bundle all that info in a clear way :-).
On https://www.healthrising.org/blog/2020/05/27/neuroinflammatory-paradigm-chronic-fatigue-me-cfs/ we describe things like:
“Things like excessive extracellular glutamate, another key part in our hypothesis, are heavily modified by hypoxia. Excess glutamate decreases firing threshold and increases firing rate. ROS is a known inhibitor of the mitochondria. That decreases the firing strength and potential of the neurons. Excess ammonia, potentially formed by fast amino acid consumption during hypoxia as an alternate route to counter the dangers of brain hypoxia, is both excitatory and has a potential to inhibit the mitochondria. So this is a complex one.”
Ammonia acts just like glutamate (another nail Issie is “pioneer banging on it” a long time) to trigger the NMDA receptor. That increases excitation feelings and sleepliness.
Warning about increasing glutamate and glutamine intake: the research Meirav linked is about hEDS. There are many long standing discussions about glutamate potentially harming ME, FM and POTS patients.
Several of us had a discussion back in 2013 on high glutamate to GABA ratios and how it affected us.
https://www.dinet.org/forums/topic/23706-pots-excitotoxicity/
Many of us had those high ratios.
One of “smart pioneer” woman Looneymom who discussed this bad high (excitatory) glutamine (and glycine) versus low (calming) GABA ratio seen by several patients with exciety problems. She was in a desperate search to help her son with POTS. Those were her numbers she posted:
“Gaba 2.7 Low 3.9-7.9
Glycine 1963.8 High 441-1258
Glutamate 81.2 High 13.5-36.8”
We felt that the sympathetic system seemed fueled and overly stimulated by glutamate and not enough GABA for a more desired parasympathetic response. But many of us when trying to up our GABA had an opposite reaction or paradox response. (We had that happen with many experiments and we all shared what we tried and if it worked or backfired.)
Many of us tried GABA and precursor to it like glycine and glutamine and even glutathione trying to up our GABA, but had quite the opposite outcome and upped our glutamate even more. (In one of the links, I’ll list below, there is a link showing why this paradox may happen.)
Cort also wrote on too much glutamate potentially causing small fiber neuropathy by burning down small nerve fibers.
https://www.healthrising.org/blog/2019/08/12/brain-small-fiber-neuropathy-fibromyalgia-chronic-fatigue/
In 2018 Cort wrote an article on Simmaron that sparked a discussion about the risks of high glutamate in the comments. This is rather lengthy with really good comments and lots of additional research linked in those comments. (This is one with link to possible reason for paradox with glutathione.)
http://simmaronresearch.com/2018/08/system-reset-chronic-fatigue-syndrome-mecfs/
I was trying to get my fatigued head around the section on mitochondria maladies in your next article discussing research that indicates that complex I may be upregulated in people with me/cfs, whereas complex V, downstream, is inefficient. Since the reaction catalysed by complex I is NADH + H+ + CoQ + 4H+in→ NAD+ + CoQH2 + 4H+out (Wikipedia)), might supplementing with coq10 further upregulate this reaction leading to overburdening of the underperforming complex V downstream? (or have I misunderstood this system?). Might that be an explanation (or partial explanation) for why some people with me/cfs have a negative reaction to COQ10?
Good remark!
I had to look for a good quality picture and found one in https://www.biologydiscussion.com/respiration/electron-transport-system-and-oxidative-phosphorylation-in-mitochondria/23316
The first picture in it shows how these complexes cooperate. You’ll see that there are two parallel steps that make UbiQuinone (UQ), a substance that is needed in the Electron Transport Chain to convert things like NADH and succinate (an important intermediate in the Citric Acid or Krebbs cycle, another key part of how mitochondria work) into usable ATP.
That UbiQuinone is then fed further down the chain (like on a production line with work stations in sequence) into complex III and that makes stuff that is further fed into complex IV. Complex V finally makes ATP out of what complex IV (and also a bit out of what other complexes) produce.
Now when complex I works faster, then the parallel conversion step used to convert succinate to fumarate *has* to slow down if the other complexes would still work at the same speed as before. It even gets worse: if nothing but complex V is slowed down quite a bit, stations like complex III and IV have to slow down or “stuff” would be pilling up along the production line.
So, the combination of complex I being sped up and complex IV being slowed down slows down the conversion of succinate to fumarate *a whole lot*.
=> That is nothing but slowing down the entire Krebbs cycle a whole lot, as the conversion of succinate to fumarate is a necessary step in the conversion of pyruvate and acetyl-Coa in the Krebbs cycle. If the conversion of both pyruvate and acetyl-Coa is slowed down in the Krebbs cycle, then the use of both carbs (glucose), fats and even ketones is slowed down (to a trickle) in the mitochondria. No wonder we produce few ATP (at peak capacity).
That exact step, the conversion of succinate to fumarate, is slowed down a whole lot and it indicates *a lot* that the body is trying to reduce excess ROS production because fumarate pilling up too high is a well studied major source of excessive ROS creation. It seems to be a protective measure. Trying to force those complexes “to work correctly” seems very close to trying to override essential safeties to me.
Thanks, dejurgen 🙂 . I’ll read through this post and the linked article carefully and digest when I have a bit more time and energy.
I have chronic fatigue and likely mitochondrial dysfunction. my bloodwork showed very low CoQ10 so My doctor put me on a liquid CoQ10, and I believe it’s making my fatigue worse. Why? If I need it why would my body not except it? Is there a genetic implication? ideas? i’m Tired of being tired