

This is the first part in a series on mitochondrial enhancers for chronic fatigue syndrome (ME/CFS), fibromyalgia (FM), and long COVID series. The series uses the book “Mitochondria and the Future of Medicine”, by Lee Know, a former naturopathic doctor in Canada, as a starting point, and includes insights from ME/CFS/FM practitioners.
- Pt I: D-Ribose, CoQ10 and PQQ
- Pt II: L-carnitine and Acetylcarnitine
- Pt. III: Magnesium
- Pt IV: N-acetyl cysteine (NAC)
- Pt V: Oxaloacetate
- Pt. VI: Niacin, Niacinamide and Nicotinic Riboside
Mitochondrial Enhancement
Is more energy the cure-all for chronic fatigue syndrome (ME/CFS) and fibromyalgia? Dr. Lerner observed years ago that symptoms in ME/CFS/FM tend to go up when energy levels go down and decline when energy levels go up. Even at rest, our muscles are affected by low energy levels. Because it takes more energy to relax a muscle than contract it, the muscle tension and pain many of us feel could be due to low energy levels in the muscles.
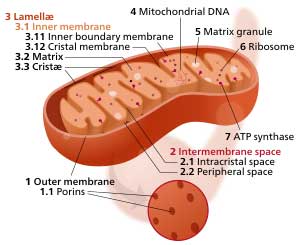
The low energy situation in ME/CFS/FM makes one think immediately of the main energy producers in the body – the mitochondria. Of course, it’s not as easy as that: it never is.
Problems with the mitochondria have been found, but the results overall have been inconsistent.
Two recent reviews of the mitochondrial findings in ME/CFS noted that significant problems with the mitochondria have been found, but the results have been inconsistent. A recent review of mitochondrial studies found that alterations of mitochondrial structure, DNA/RNA, respiratory function, metabolites, and coenzymes have been reported, but it highlighted the inconsistent results. Three New Zealand researchers proposed that doctors and researchers should focus on the mitochondria when treating and studying the COVID-19 long haulers, but they too pointed out the numerous inconsistencies found.
Some studies have found decreased proton leaks, while others have found the opposite. Three studies found reduced ATP production, while two found normal ATP production. Glycolysis has been impaired in some studies and not others. Two studies found no issues with the levels of the five complexes that make up the electron transport, but one recently found reductions in Complex V and an upregulation in Complex 1.
One consistent outcome has been the lack of mitochondrial DNA changes; i.e. it’s pretty clear that ME/CFS is not a primary mitochondrial disorder. Decreased CoQ10 levels have also been found in three studies (but not in another), and two studies have found a lower reserve capacity for energy production.
The takeaway: it’s not at all clear what’s going with the mitochondria in ME/CFS. The same is true with energy production overall. While the exercise studies have produced consistent evidence that energy production is impaired – and have provided plenty of ideas why – no cause has been agreed upon. We simply don’t have enough precise information to target what’s going on.
Plus, if there’s a problem in one part of the mitochondria, something that enhances another part of the mitochondria probably won’t help. If the mitochondria aren’t receiving enough oxygen, then mitochondrial enhancers might not make a difference. If a hydrogen sulfide imbalance is the issue, then that will have to be dealt with. If free radicals are a problem, then enhancing the mitochondria – the source of many free radicals in the body – could make things worse! (On the other hand, Know (see below) points out that because mitochondrially produced free radicals play an important signaling role in the cell, having too many antioxidants present could conceivably be a problem.)
Helping the mitochondria to do better, then, falls into the same category that virtually every other treatment for ME/CFS/FM does: it’s kind of a crapshoot. Certainly, some studies and much anecdotal evidence suggest that it can be helpful for some patients. Several ME/CFS/FM doctors have prescribed mitochondrial enhancers. On the other hand, there’s not much hard evidence in the form of large, well-designed placebo-controlled studies.
Still, we are talking about energy production and while the results are mixed, enough have been found to suggest that something may be going on with the mitochondria.
The Mitochondrial Enhancers Pt. I
In “Mitochondria and the Future of Medicine”, Lee Know, a licensed naturopathic doctor in Canada, has written an engagingly written overview of the field. It will provide the basis for this overview. Know, though, warns that he’s by no means providing an exhaustive list of mitochondrial enhancers. This, then, is a basic overview of the major ones.
D-Ribose
Know starts out with a supplement that made quite a splash in ME/CFS over a decade ago with Dr. Teitelbaum – D-Ribose.
D-Ribose plays a major role in the pentose-phosphate pathway – a metabolic pathway that runs parallel to glycolysis which generates NADPH, pentoses (5-carbon sugars) and ribose 5-phosphate. Every time D-Ribose is produced, NADPH and these other substances are as well.
D-Ribose is also a component of many compounds (ATP, RNA, NADH, coenzyme-A), needed for proper mitochondrial functioning. It binds together purines/pyrimidines to form a kind of a backbone for these substances.
If low oxygen levels make it difficult for the mitochondria to produce ATP, our cells take an alternative approach: they combine the ADP molecules that have been building up in the cell to create it. As with all compensatory approaches, though, this comes with a cost.
That process leaves AMP as a by-product, which is then broken down and washed out of our system. The loss of AMP, though, reduces the pool of purines available – creating a real problem – as purines are key building blocks for ATP, RNA and DNA.
The Gist
- Studies suggest problems with energy production exist, but we still don’t know why.
- The mitochondria – the main energy producers of the cell – are a possibility. A variety of mitochondrial problems have been found, but the study results have been inconsistent.
- Since we don’t know which parts, if any, of the mitochondria have problems in ME/CFS/FM, it’s impossible to precisely target the mitochondria.
- Plus, if problems outside of the mitochondria exist – such as reduced oxygen delivery to the tissues or hydrogen sulfide issues – then enhancing mitochondrial production may not help.
- Still, quite a few ME/CFS doctors do recommend mitochondrial enhancers, and some study results suggest they may be helpful.
- D-Ribose – By bringing purines and pyridimines together, D-Ribose provides the underpinnings for important substances such as DNA, RNA and ATP.
- D-Ribose levels decline during the low oxygen states which may be present in ME/CFS and FM. When those conditions are present, cells turn to bringing two ADP molecules together to form ATP. The AMP left over is washed out – leaving the cell depleted in purines. Bob Naviaux found reduced purines in ME/CFS.
- D-Ribose is able to enhance purine levels. Two non-placebo blinded studies from Dr. Teitelbaum suggest the D-Ribose may be helpful in a number of ways.
- Several ME/CFS doctors recommend using 3 scoops of D-Ribose a day for several weeks and then dropping down.
- PQQ – is a mitochondrial generator, nerve cell protector, an anti-inflammatory, and is able to protect the mitochondria from oxidative stress.
- PQQ may be able to improve short-term memory, attention and information processing.
- PQQ may work better when taken with CoQ10. Doses appear to be around 10-20 mgs/day
- CoQ10 – arguably the most important mitochondrial enhancer, CoQ10 carries electrons from one part of the electron transport chain to the other, and it reduces oxidative stress. It’s used in a number of diseases.
- Several studies have found low CoQ10 levels in ME/CFS and FM, and several trials suggest it could help.
- CoQ10 comes in two forms: ubiquinone and ubiquinol. Ubiquinol is best absorbed and is recommended particularly as we age. It’s more expensive, but less is needed.
- It may take up to a month for CoQ10 levels to plateau while taking ubiquinol 2-300 mg/day. It should be taken with fats. Be wary of taking it before bedtime.
- NADPH – does not appear to be used as a mitochondrial enhancer, but it’s mentioned here because Bob Naviaux focused on it with regards to the metabolism in ME/CFS.
- He believes that all the metabolic abnormalities found in ME/CFS may be a consequence of redox issues or reduced levels of NADPH.
- Naviaux calls NADPH the cellular barometer of metabolic stress, but does not recommend NADPH supplementation.
- Instead, he reports that theoretically, incremental improvements in NADPH could be produced with folate, B12, glycine, serine pools, and B6 metabolism.
- Mitochondrial enhancers probably work best when used together and in conjunction with a program to treat ME/CFS/FM.
D-Ribose can help cells rebuild their purine reserves. Because it takes a long time for cells to make their own D-Ribose, Know asserts that in diseased states, D-ribose supplementation is necessary to do that.
Given the potential problems with the microcirculation, the early introduction of anaerobic energy production during exercise, the lactate buildup, and reduced glutathione levels, it certainly seems likely that low purines might be a problem in ME/CFS – and there’s some evidence that they are. In “Metabolic features of chronic fatigue syndrome“, Bob Naviaux reported finding just that. Naviaux found decreased purine levels that were “consistent with decreased synthesis and/or turnover (flux) of ATP and GTP and decreased reserve capacity”.
Studies suggest that D-Ribose is able to restore energy to depleted muscles that have been subjected to low oxygen levels or ischemia. Know reports that studies in athletes indicates that D-Ribose can result in lower heart rates needed to do work, increased exercise tolerance, and more rapid recovery of stressed muscles. One interesting study found that D-Ribose reduced free radical levels in healthy people who exercised for 25 minutes at their anaerobic threshold. A 2020 study found that D-Ribose did reduce muscle soreness, increase muscle recovery and inhibit the production of free radicals called lipid peroxides in healthy people. Other studies, however, have not found benefits.
If Naviaux has found evidence of depleted purines and NADPH in ME/CFS, and D-Ribose is, according to Know and others, the chief replenisher of purines in the cell, does that mean we in the clear? Do we just need to supplement D-Ribose in order to rebuild those cellular stores?
Unfortunately, D-Ribose is not well studied in ME/CFS and FM. Two studies from Dr. Teitelbaum, though, suggest that D-Ribose might help. Neither, unfortunately, were placebo-controlled. One simply had 41 ME/CFS and/or FM patients take one scoop of D-Ribose (Corvalen) three times a day until the bucket of D-Ribose was finished. Teitelbaum reported that 2/3rds received significant improvements in energy, sleep, mental clarity, pain intensity, and well-being. The average improvement in overall well-being was 30%.
Teitelbaum followed that up with a 203-person open label, unblinded 3-week study which again found significant improvements in energy (61%), overall well-being (37%), sleep (29%), mental clarity (30%) and pain (15.6%).
Rituximab taught us to be careful of the outcomes of studies like these. Rituximab, after all, fared very well in a 29-person open-label study and a 30-person double-blinded, placebo-controlled study before it utterly failed in a 151-person double-blinded, placebo-controlled study.
Other doctors have recommended it as well. Dr. Tori Hudson believes that many ME/CFS patients start out with FM and devolve into ME/CFS/FM patients as their energy levels decline. She believes that:
“As cellular energy is depleted, fatigue and muscle pain become more and more severe, and the muscles require additional energy in their recovery efforts. Energy is used faster than fuel is made available to renew it, and the fatigue, soreness, pain and stiffness continue to progress. Energy depletion reaches a critical point, and CFS/FMS becomes a state in which the mechanisms for recovery are overwhelmed.”
She reported that she’s found “D-Ribose to be the single most important nutrient in the search for alleviation of symptoms and a path towards health” in her ME/CFS and FM patients.
Using D-Ribose
It should be noted that while D-Ribose is a sugar which does not affect glucose or insulin levels, it is very sweet.
Teitelbaum recommends using using pure D-Ribose or D-Ribose with malic acid/magnesium. (See his formulation here.) He recommends using 15 grams (5 grams or 1 scoop 3x’s/day) for two weeks and then 2 scoops once a day afterwards. He reported it took about two weeks to see the results in one study. Both Dr. Lapp and Dr. Myhill also recommend using 5 grams (1 scoop) three times a day. After a couple of weeks, Lapp recommends the dose be dropped to 1 scoop a day. Myhill has her patients stay on the original dose until the effects plateau, and then has them then experiment with lower doses.
Although Know reports that 3-5 grams a day are the normal dose, he states that larger doses are safe and clinical trials usually use 10-15 grams (2-3 scoops) and have even gone much higher. For people with chronic health conditions, he recommends upping the dose until an effect is found.
Myhill recommends that some people who have gut issues with it (it is a sugar but does not affect glucose or insulin levels) should absorb it in their mouth and reduce the daily dose to 1 scoop. If you’re sensitive to corn, a corn-free product is available.
Dr. Myhill reported that D-Ribose will work best when the “other aspects of mitochondrial metabolism are addressed, such as Co-enzyme Q10, L-carnitine, magnesium, niacinamide, detoxificiation and antioxidant regimes where appropriate.” When ME/CFS patients are following her program, she says that she expects “D-ribose to improve the symptom of delayed fatigue in sufferers as well as improve stamina”.
Pyrroloquinoline Quinone (PQQ)
PQQ (thank god for acronyms) is mainly known as a mitochondrial generator. That aspect of PQQ may not help in ME/CFS, as mitochondrial levels seem, thus far, to be normal. PQQ also, though, appears to be able to protect nerve cells, support nerve growth and protect the mitochondria from oxidative stress.
PQQ appears to be able to increase mitochondrial generation, improve mitochondrial functioning and, when taken with CoQ10, enhance cognition.
Most PQQ studies are lab or animal studies, but one human study found that it reduced oxidative stress, decreased inflammation and immune activation (C-reactive protein, IL-6) and appeared to enhance mitochondrial functioning. Another human study suggested PQQ may be able to improve short-term memory, attention and information processing – all of which could be helpful in ME/CFS/FM.
Its effects may be significantly enhanced when it’s taken with CoQ10. It’s found in a variety of foods but is off-the-charts high in dark chocolate.
One patient reports that Dr. Klimas recommends taking PQQ with ubiquinol, but getting CoQ10 levels up to snuff first by taking it for a couple of weeks. Another patient reports that taking 20 mg PQQ before bed was helpful for having deeper and more restful sleep. Others, though, haven’t noticed much effect.
Doses appear to range from 10-20 mg daily.
Neither Courtney Craig nor Sarah Myhill have reported on PQQ.
CoQ10 (Ubiquinone/ubiquinol)
If any mitochondrial enhancer is going to help in ME/CFS and FM, it may be CoQ10. Know calls it “arguably the single most mitochondrial nutrient for mitochondrial health” and states that “CoQ10 supplementation has been shown to dramatically improve the status of patients with all sorts of health conditions.” Eighty percent of it is found in the mitochondria.
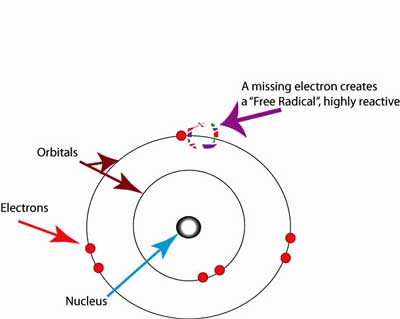
Free radicals are produced en masse during ATP production. Unless they are mopped up by antioxidants like CoQ10, they will snatch electrons from cellular membranes, causing havoc.
Coenzyme Q10 (CoQ10) is a potent free radical scavenger, ATP production enhancer, anti-inflammatory, and has neuroprotective effects. It plays a particularly important role in complexes 1 and 2 of the electron transport chain (ETC) where it acts as an electron carrier. If not enough CoQ10 is present, not only will the ETC (and ATP production) shut down, but reactive oxygen species (ROS) or free radicals will be formed.
Fisher’s finding that complex 1 was compensating for problems in complex 5 in ME/CFS suggests CoQ10 might help. (Know writes that CoQ10 has been able to return low levels of complex 1 activity in Parkinson’s to normal).
Dr. Myhill reports it’s “very common” to find low levels of CoQ10 in her patients. Plus, several studies suggest CoQ10 levels are low and supplementation may be helpful in fibromyalgia and ME/CFS.
Because as we age we produce less and less CoQ10, it might be a good idea for anyone as they get older to supplement with CoQ10.
Find out more about why CoQ10 may be helpful and how future formulations may improve it in this recent blog post.
Using CoQ10
- Conventional CoQ10 or Ubiquinone – is the oxidized form of CoQ10. This form is more stable, but has to be transformed into ubiquinol first. As we age, we become less able to convert ubiquinone into its usable form. Some people, particularly of Hispanic or Chinese descent, may also lack the enzyme to transform ubiquinone.
- Ubiquinol – is absorbed better, increases energy output, and scavenges free radicals in the mitochondria and cellular membranes. It’s particularly the preferred form for older people. Ubiquinol is more expensive than CoQ10, but you need to take less of it.
Life Extension reported that one study showed that it took just 150 mg of ubiquinol to produce the same CoQ10 blood levels (3.96 mcg/ml) as 1,200 mg of CoQ10 (ubiquinone) over four weeks.
Life Extensions recommends 100-150 mg of ubiquinol daily for adults over the age of 30 and 200-300 mg a day for those attempting to receive its “anti-aging” benefits. Large doses (150-300 mg) may result in an “exponential increase in blood CoQ10 levels”, which is sustained longer.
Dr. Mercola recommends starting with 200 to 300 mg per day, and then ramping down to 100 mg/day after three weeks when your CoQ10 plasma levels plateau. If you experience a lot of stress, though, 200-300 mg/day Is recommended. Other reports, though, suggest that it may take up to four weeks for the CoQ10 levels in your blood to reach their maximum levels.
Co-Q10 should be taken with a fatty or oily meal. Dr. Klimas warns against using it before going to bed. It will take about 4 weeks for levels to plateau. At that poin, a lower does can be used.
Myhill asserts that Co-Q10 works best when used with magnesium, D-Ribose, acetyl L-carnitine and NAD.
NADPH
Know does not mention NADPH, and it does not appear to be used to boost mitochondria, but it’s mentioned here because after noting that purine levels were lower in ME/CFS, Naviaux focused more on NADPH, which is produced alongside D-Ribose in the pentose pathway. (From what I can tel,l supplementing with D-Ribose does not increase NADPH levels.)
If anyone knows the mitochondria, Dr. Naviaux does. The co-founder and a former president of the Mitochondrial Medicine Society (MMS), Naviaux was a founding associate editor of the journal Mitochondrion. He also discovered the cause of the oldest Mendelian form of mitochondrial disease – Alper’s disease.
Naviaux reported that “all of the metabolic abnormalities” found in ME/CFS were either regulated via redox or oxidative stress or “the availability of NADPH”. NADPH plays such a central role that Naviaux called it a “global barometer of cellular fuel status”.

Naviaux described NADPH as a global barometer of cellular fuel status but does not recommend NADPH as a supplement.
The consequences of low (reduced and total) NADPH levels, Naviaux reported, are profound and include problems producing key cellular factors such as sterol, fatty acid, protein, and nucleotide synthesis falls to baseline survival levels. When NADPH levels are higher, on the other hand, cells grow, biomass is created and cellular repair factors are produced and stored.
Naviaux believes, though, that while NADPH levels appear to be low in ME/CFS, “NADPH is neither the problem nor the solution by itself”. If I’m reading him correctly, the problem is the dauer or hibernation-like state that NADPH is responding to. Naviaux’s Dauer hypothesis suggests that the mitochondria have been turned down for a reason, and that turning them back on will take more than shoving more nutrients down their throats, so to speak.
“NADPH cannot be simply added as a nutritional supplement to produce the tidal change in metabolism needed to shift the dauer state of CFS to normal health”. Instead, Naviaux states that “incremental improvements in NADPH production could theoretically be supported by interventions directed at folate, B12, glycine, and serine pools, and B6 metabolism.”
Like Myhill, Naviaux believes it will take treating all of ME/CFS/FM. For him, effective treatments “are likely to be achieved by careful attention to nutrition, metabolism, triggers, stressors, and physical activity as an integrated system, combined with a systems biological understanding of the triggers of the CDR (7) and dauer entry and exit”.
The Mitochondrial Enhancers for Chronic Fatigue Syndrome (ME/CFS) and Fibromyalgia Series







For me, mito supplements have been very helpful and have made a big difference. They’ve extended my energy level and energy window. If I go off and go back on them, it’s like putting on a battery pack. It doesn’t solve the illness, and doesn’t seem to affect the other elements like dysautonomia, but for me, they are very important and help widen that energy window.
What’s been most helpful for me is something not mentioned in the article: Tru Niagen, which is nicotinimide riboside, a precursor to NAD. I’ve noticed a big difference in energy. That’s an MVP for for me.
Cort, have you heard of others benefiting from Tru Niagen too?
Also, I’ve found these other mito supplements to be helpful: acetyl l carnitine, co-q10, p5p, l-tyrosine, ALA, and a resin called shilajit. Shilajit and ALC are especially helpful, I notice a difference right away. Anyone else try shilajit – wow!
I tried PQQ and d-ribose and didn’t notice anything. Might try again.
“have you heard of others benefiting from Tru Niagen too?”
I do, but care has to be taken. At anywhere near normal doses it first feels like being on rocket fuel and then it more so feels like being burned alive. That’s MCAS hitting very hard. I take about 1/6th of a pill a day, divided over three separate doses and even at that those I feel a meaningful difference in firstly breathing (feeling of more oxygen in the air) and secondly energy. But even to get to that 1/6th of a pill spread over three times I had to build up from lower amounts.
For me 1 or even 2 pills a day would be insane and utterly damaging. Issie tried to and several times but MCAS got every single time to her. That’s after feeling much better for like an hour or so.
It’s not something I can simply recommend to just try and take as it’s side effects can be very potent even at very low doses.
NR did give me bad MCAS and that was on the tiny dose that Dejurgen uses. I tried it several times and it got me every time. I’d have an initial WOW feel, like I could dance all day and then I got MCAS. And couldn’t sleep, would be wide awake. Could not make it work for me.
I had the same response to D-Ribose and PQQ sent me into a POTS tailspin. Hyped me sooooooo much.
My having Mitrochondria issues, proven with science (research study participant) most things I’ve tried for my Mitrochondria wound up taxing me more. The initial surge was good and then a crash.
I have, in last week, been trying NMN. So far, so good. This is like 1/8 of a pill 2 times a day. Trying to get the pathways to work and not bombard them too fast. Slowly trying to get the body to work, where it has been having a block. Forcing it to work and too fast can be a disaster. Low and slow. I am feeling the affects of even this low amount. (I’m super tuned into my body and have keen perception of responses. So paying close attention.) Its like NR, but a lighter version for me. I’m able to sleep with it. And get the energy but without as much hype. New research has shown it to be more beneficial to use it sublingual (under the tongue). NMN also has the ability to get into not just red blood cells but also muscle. (According to recent research.) So far, so good. I just hope it doesn’t build up and I start having an issue. But right now, I’m encouraged. Makes me happy!
I also tried CQ10 several times (months on end) and didn’t see much benefit from it either.
I’m also back to Intermittent Fasting. Having an 8 hour eating window. That really seems to make a difference too. I’ve made other diet changes that seem to really make a difference. One of the biggest lately is eliminating, as much as possible, oxalates. I’m already gluten free, no nightshade and low lectins. I can’t do high fat diets, that does not work for me.
Issie mentioned NMN. What is it?
https://www.prohealthlongevity.com/blogs/control-how-you-age/nmn-vs-nr-which-is-best
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6359187/
Beth, sounds like we’re traveling similar roads.
However, Tru-Niagen is expensive hype for me. I’ve done better with NMN, NAD+, and NADH. PQQ doesn’t do anything either.
Carnitine, acetylcarnitine, ALA, C, E, glutathione, P5P, tyrosine Kuvan and NO supplements have all helped.
Every lab analysis I’ve gotten from shalijit products has either mold/myctoxin or heavy metal contamination or both, unfortunately. Have you found one that’s clean?
I’ve been taking Tru Niagen for a year. Started out with NADH for 6 months and then moved to Tru. If I used a scale of 0-100, 100 being my baseline prior to illness and 0 being the worst state I’ve been in, it took me 4 years to get from 0-15. NADH brought me to 20 and Tru brought me to 35. I can skip doses without any impact, but after a few days, I start to feel sluggish.
Just started D-ribose today because of a major PEM crash I got myself into. The last few hours I’ve felt better than I have in weeks. Hoping it’s the D-ribose and not just a fluke.
Whatever happened to Naviaux’s studies with Suramin? Did the group that was going to develop Suramin decide to not follow through? This sounded so hopeful, yet I haven’t heard anything about it for a couple years now.
I think they switched to focusing on autism. Apparently suramin has helped with that.
Just walking was a big problem for me until I tried D-Ribose years ago. I still take 1 heaping teaspoon 2xaday. The best price for D-Ribose, I can find, is from http://www.bulk supplements.com., a US company. You can also find his many affordable supplements on his website http://www.endfatigue.com
Dr. Teitelbaum’s new book ‘FROM FATIGUE TO FANTASTIC, 3rd edition is available now! In all my years of researching ME/CFS/FM, this is the most complete, easy guide on understanding our illnesses and the treatments that he has used in his decades of practice. He even shares the dosing for the many pharmaceuticals and natural products.
Be sure to buy his 3rd Edition, as his past ones are still available. $22.00 USD.
@ Edith B
Dr T’s book From Fatigued to Fantastic is NOW in it’s FOURTH, 4th Edition , completely revised “This new, just released, 4th edition, is now completely revised and updated. The most recent and relevant scientific information on addressing the human energy crisis is simplified, organized, and distilled into a simple “what to do now” format.” Listed under Dr T on Amazon.
BTW niacin , D-ribose, Co-Q 10 , MSM, Vit C and dark chocolate are all part of my regime, along with Dr Sarah Myhill’s Groundhogs, Basic, Acute & Chronic, plus a few others eg Dopa macuna, TCM herbal sleep aid, all gradually introduced in low titrations over 8+ years, finally feeling my way thru the fog. 4x per day application of a mix of EOs essential oils, in carrier, for pain relief,FM, [ lavender, sandelwood,Peppermint, Eucalyptus, Rosemary, got those linlools going on, I read somewhere that the EOs act via mRNAs absorbed through the skin, anyway wouldn’t be without them,]aids breathing & sleep too,
“it takes more energy to relax a muscle than contract it” If by “relax” you mean expand, then I remember from Dr. Cheney that this is true of the heart, but are you sure it’s true of skeletal muscle?
i agree with question, too, Tim
if it took less energy to relax than ‘to work’ a muscle,
it would be easier for people to work than to relax,
and sleeping would be exhausting
from all the energy it would take to ‘relax’ and sleep
just my thoughts
found this with lots of pics
http://pressbooks-dev.oer.hawaii.edu/anatomyandphysiology/chapter/muscle-fiber-contraction-and-relaxation/
I got that directly from Konw’s book. I remember that Naviaux stated that as well. I don’t know if either of them mentioned muscle type. Other than I really don’t know anything about it.
no, cort, it doesnt take more energy to relax a skeletal muscle. Only smooth muscles in veins, eyes, lungs, heart, sphincters
I dont even believe that smooth muscle, which usually stays contracted until required to expand, burns energy to stay that way. The muscle fibres are attracted to one another on a chemical/ electron level.
its only the CHANGE that uses energy
I wonder how the two supplements I’ve tried relate.
For my FM, menthyl sulfonyl methane (MSM) is wondrous and takes pain levels from 4-5 to 0-1. The only other thing that had as great as effect was fusion surgery on my left developmentally dysplastic knee which was crumbling. Not being in exquisite pain from the knee reduced the FM related pain as well.
I use supplemental oxygen for severe asthma and moderate COPD. My prescription is for sleep and on exertion but I’ve found—since no oxygen concentrators have remotes—that leaving the oxygen running 24/7 lowers both blood pressure and heart rate ten points. Most interestingly, the oxygen markedly improves alertness and ability to concentrate. I am also able to be more active, from a bedridden baseline to some ADLs including making myself simple breakfasts and lunches. My pulmonologist dismisses these findings, saying “even football players use oxygen on the sidelines.” I don’t think he understands how utterly debilitating ME/CFS is, that it’s a much greater problem than the asthma-COPD.
Would the MSM or the oxygen be related to mitochondrial dysfunction?
You wrote “My prescription is for sleep and on exertion but I’ve found—since no oxygen concentrators have remotes—that leaving the oxygen running 24/7 lowers both blood pressure and heart rate ten points. Most interestingly, the oxygen markedly improves alertness and ability to concentrate.”
This has been my experience too. I originally got O2 concentrator because a sleep study showed my overnight O2 was dropping even with a Cflex. Using my fingertip oximeter while without supplemental oxygen, I’ve consistently seen a gradual decline in O2 sat while sitting – with accompanying drop in mental alertness/cognition – and a faster decline when under load (standing, walking, etc).
Adding 2 l O2 while awake delays the cognitive decline, allowing me to handle more tasks requiring a certain amount of concentration. Using it while standing/moving around gives me a lower HR by about 10% and extra 10 minutes standing for chores (on average) and extra 30 steps or so while walking.
All that said, when I’m already crashed my O2 sat can be in the high 90s while HR, & cognition suffer regardless of supplemental oxygen, and I’ll have persistent air hunger too, which all implies there’s an impairment state that can prevent O2 being released by the blood to the cells.
@Cherie Parks I had a really good response to MSM back in my FM days. Everything shifted when ME came along, so haven’t tried it since. Worth another try I guess. It felt like extra energy rather than relief from the pain of fibromyalgia.
While looking for information on whether patients with ME/CFS could get Covid, I found this new study in a December article.
New Test for Chronic Fatigue Syndrome
https://www.verywellhealth.com/cfs-me-diagnostic-test-covid-19-5089344
Apologies, Cort, if you have already talked about this and I missed it.
It also bears mentioning that many people with ME/CFS also have POTS (description below). In my case I have POTS, ME/CFS and Addison’s Disease (non-functioning adrenals). Just having POTS alone can cause extreme fatigue let alone throw ME/CFS into the mix. If you have severe autonomic nervous system symptoms as I do, it makes your POTS worse.
While they recommend a tilt table test you can figure it out on your own using a BP monitor. Take readings lying down, then sitting up, then standing, at 5 minute intervals. If you BP goes down and your heart rate goes up, then POTS could be a culprit. As my POTS has gotten worse in the last 20 years I can really tell that my health is declining, even with Florinef, extra sea salt and increased liquids. My resting heart rate is usually 80-95. Anything over 100 is considered ‘tachycardia’.
D-Ribose @ 2 scoops a day, CoQ10, L-Carnitine and various other supplements do help somewhat, but over the last 20 years I haven’t found anything that makes an appreciable difference. I’m still ‘severe’ and only have limited time to accomplish anything during the day. Standing about 10 minutes is about my limit. I do notice that when my heart starts skipping beats and is erratic, regularly taking 1000 mg or more of Taurine a day helps. Beta blockers didn’t help the POTS in the sense that even at small doses my fingers and hands started turning either white or blue, which is typically called Raynaud’s.
Postural Tachycardia Syndrome (POTS)
A condition where the heart rate increases on changing posture from lying to sitting up or standing.
How common is condition? Common (More than 200,000 cases per year in US)
Does diagnosis require lab test or imaging? Rarely requires lab test or imaging.
Is condition treatable? Treatments can help manage condition, no known cure
Time taken for recovery. Can last several years or be lifelong
The exact cause is not known. It is associated with low blood volume and disturbances in the autonomic nervous system. Characterized by rapid heartbeat, light-headedness, inability to exercise, fatigue and nausea. Treatment mainly includes self care practices to help deal with the symptoms. Less often, medication may be used.
Symptoms
Rapid heartbeat
High/low blood pressure
Light- headedness
Fainting
Fatigue
Inability to exercise
Nausea
Anxiety
Blurred vision
Headaches
Treatments
Treatment mainly includes self care practices to help deal with the symptoms. Less often, medication may be used.
Medication
Corticosteroids: Help the body to retain sodium.
Fludrocortisone (Florinef)
Beta blockers: To decrease the heart rate.
Atenolol
Vasopressors: Narrow the blood vessels and act as anti-hypotensives.
Midodrine
Self care: To prevent/treat an episode:
Get up from lying slowly, and sit for a while before standing
If you feel dizzy, lie down and raise your legs, if possible
Causes
The exact cause is not known. It occurs due to disturbances in the autonomic nervous system.
It may occur after a viral illness, traumatic event or pregnancy
Family history increases risk
It is linked to underlying conditions such as diabetes, amyloidosis, sarcoidosis, and cancer
It is associated with autoimmune disorders such as lupus, Sjogren syndrome, and celiac disease
It may be caused due to poisoning with alcohol or certain metals
It is common in patients of chronic fatigue syndrome
Also seen in conditions which cause high amounts of noradrenaline to be produced
@Stephanie, do you know your subset type of POTS? I’m HyperPOTS and take a much different approach than you do. I don’t vasoconstrict my veins and taking Florineff and salt was a complete disaster for me. Not all of us need to do what is considered “traditional” POTS protocol—-it makes us way worse. I’m a lifer with POTS and it is in generations of my family. I also found some supplements considered energizing to speed up my symptoms of POTS and ME/CFS. Throwing me into overdrive with it.
I think we need subsets more defined when we are talking about POTS. I know what I do will not work for everyone.
And you are so correct about throwing ME and FMS into the mix. And also EDS and MCAS. It makes for a very complex, complicated hard to figure out person. As one thing can affect the other and treating “symptoms” may not be so easy.
I also feel our “symptoms” could be the lessor evil trying to correct something far worse. And stopping some of the symptoms that may be a compensation, may be the wrong approach.
For example me with severe MCAS, I can NOT take beta blockers. They can really bring on more symptoms not only with MCAS but also my POTS. As MCAS affects my POTS strongly. (I don’t try to stop my tachycardia completely, as that helps move blood to my heart and head and get needed oxygen there.) Since MCAS can trigger POTS for me, I don’t want medicine that causes my MCAS to be worse.
I have written a lot about my experience and ideas/hypothesis on both the HEALTHRISING Forum and the DINET forum.
I’ve managed from being wheelchair bound to upright and moving and having a much more functional life over the last couple years. Still have a ways to go, but making advancement and seeing improvement.
We always need to hang onto HOPE. Science is advancing. We just have to flip the coin and look at the other side. Changing the way we look at things and trying to find other clues not yet thought of. In search of our best “purple bandaid”. ?
I have hyperadrenergic POTS. Every time I was tested in the early years my noradrenaline levels were way over range. I have all the typical symptoms; tremors, anxiety, heart palpitations, gastrointestinal pain, etc. Before I was put on Florinef and Sea Salt I had episodes where I was passing out. When I turned 65 my BP started climbing so I could cut down my Florinef dose but all the other systems worsened. I’m pretty sure there is a genetic component as my nephew was just diagnosed with POTS.
@Stephanie, with our family, genetics are involved. It is a really hard thing to manage, isn’t it? With some people, salt can make your BP go even higher. Not to mention the potential issues to your kidneys. Thankfully, they noticed my kidney issues and my subset when I got my DX approx 13 years ago. Back then it was all so new and in discovery. But I was very fortunate to have gotten to go to MAYO in AZ and spend lots of insurance monies (and our own), trying to figure me all out. There can be issues with us HyperPOTS people and our renin and aldosterone at the kidney level. I wrote some lengthy info about that on DINET forum. And also in my questioning salt use. You may find it interesting. I am one to have higher blood pressures with drops more into normal ranges that happen fast and cause near faints with me. I thankfully have been caught each time I did faint. But usually have enough warning to get down before I fall down. And I too am way too high in norepinephrine levels.
I did not find my POTS to start improving until I started addressing Mast cell issues. I went the traditional route on that for 8 years and in the last year have changed directions nearly 180° on how I manage that. There is a thread on Healthrising forum on that and what I’m trying to do. Soooooo much better now with both things. Still both there and why I use the word “manage” them. But my quality of life is improved.
Just because you are past 65 doesn’t mean there isn’t more that can be accomplished. And now with your family finding issues too, we want more of our WHYs answered. Its admirable that you are continuing to seek answers. We just won’t give up, will we! I have two nephews and a niece with it now too. My sister has OI. So dysautonomias with variety for us. My grandmother had POTS too. My sis and I both have FMS and ME. I have EDS and MCAS. I feel it all goes hand in hand and may be different symptoms of the same underlying dysfunctions of several different pathways. And some of those can be tweaked. Getting closer, still experimenting. I’ve found some nice “?bandaids”. It is a very individual journey, as what may work for me, may not for you. But we are for sure finding more WHYS. Getting closer, hang in there!
I’m so grateful for your commentary here. Thank you
The last statement about a comprehensive treatment by Naviaux sounds like Dan Neufer’s Rewire program.
Thanks for your insight. Reading your post, I think after the holidays I’ll do some more research on POTS and see if there is anything that strikes a chord as to what may/may not help. I’ve had all my conditions for going on 20 years. Unfortunately…… I’m now at the point where I’m stuck in dealing with it on my own. I used to live near Houston and had many resources for docs and testing and spent probably 30k the first 10 years out of pocket and spent a week in a diagnostic hospital. At the time we had good insurance through my husband’s job. Now I’m on Medicare. The tests, many done through a homeopath were EXTREMELY helpful and worth the cost. Now, I live in northeast rural Texas, f-a-r from any city and I’m too ill to travel to any appointments. Our local medical is not only woefully inadequate, but the few PCP’s I’ve managed to see don’t even believe I AM sick let alone almost completely disabled. They won’t even prescribe Armour Thyroid and one declared it was ‘dangerous’. Geesh. I still consult with my Endocrinologist in Houston once a year, thank heavens for telemedicine and she prescribes Armour, my natural Hydrocortisone and Florinef. I get many back-up emergency meds from In House Pharmacy on line. I’ve rarely have had to use any of them.
I have Myofacial Pain Syndrome and found that a combination of Magnesium, B-Ribose and Malic Acid twice a day has given significant pain relief for three years now. This assists the leg and buttocks muscles to release contracted areas. When this is at its worst, you can run a thumb down along various leg muscles and it feels like a rope with knots all the length of the muscle. I have a D.O. who can diagnose this kind of thing very accurately. When I was younger and very mild ME/CFS he was able to relieve this with very specific stretching exercises.and pressure point massage (self administered). When I developed moderate Me/CFS a few years ago, the exercises only made things worse. Cor-Muscle was a great relief for me but I do not think it would relieve the pain from FM.
I worry that people need to understand more quickly how to work out the subset that applies to their body and also to help others to understand to look for their own subset before taking generalized advice.
I keep seeing this is an issue concerning sleep and ME/CFS advice. Fortunately, my first information on ME/CFS was from Dr. Klimas’s videos and she mentioned my subset that sleeps too much…almost narcolepsy but not.
Cort my reading on the muscle issues also has consistently said that it takes more energy for the muscle to decontract or release.
Here’s a healthy affordable way to increase CoQ10…
How to Regenerate Coenzyme Q10 (CoQ10) Naturally | NutritionFacts.org
https://nutritionfacts.org/video/how-to-regenerate-coenzyme-q10-coq10-naturally/
Just a quick comment. I would be careful of taking any product that a physician creates and makes a profit, based on non controlled studies. Dr. T.’s supplements come to mind. If they hep people great. Just consider if the motive is pure or not.
My first bloodwork at my first appointment with a certain awesome Houston doctor reflected an ATP reading of 11 (eleven). After 6 years of injection cocktails, the ATP had risen to 23.
Who is your Houston doctor. I have seen many at Baylor,UT, Methodist and have yet to find one that I beneficial.
I also have hyperadrenergic POTS which first became obvious about 5 years into my diagnosis in 2000 but living in the UK I don’t think I have any chance of having it confirmed by a blood test. Thankfully low dose propananol helps me a lot and I take 10 mg twice a day or sometimes I need it 3 times daily and a higher dose especially in the summer.
It is complicated for me by having Hashimotos and adrenal insufficiency so each day I need low dose steroids plus a tiny dose of thyroxine and 1 1/2 grains natural desiccated thyroid. Having to take thyroid meds definitely complicates everything because I sometimes need to adjust my dose of NDT or otherwise the hyper symptoms get worse. It truly is a nightmare balancing everything especially when one is really on one’s on regarding treatment apart from annual standard blood tests via my GP. (he also prescribes the steroid and thyroxine).
Like others have mentioned I have to be very careful with supplements that I find very helpful for energy like L carnitine because it can make it really difficult for me to sleep without a very low dose of clonazapan. This has happened over the past several weeks and yesterday having looked at the data on my Fitbit I can see I have probably been on a touch too much NDT. Pulse has gone up from 62 to 70 and my sleep time has dropped considerably so now I will probably swing the other way as I drop down a bit on the NDT.
My feeling about our main illness, having looked at what is happening to people with Long Covid, is that the initial virus/infection changes our immune system so probably we end up with an autoimmune condition. This obviously would only apply to the subset whose illness started after a virus/infection. For me it was in 1979 when I had 2 weeks of what I thought was flu and I just couldn’t recover. The extreme vertigo/migraines started 2 weeks later when I thought I was improving but these symptoms left me bedridden for days at a time and my life was never the same after. However I did recover energy but my brain never recovered and my energy system was broken by the end of the 90s and I had to give up teaching and I was in full blown ME/CFS.
Finally I have to say that I am fortunate in that I can be fairly active at times which I completely put down to the thyroid/adrenal support I have. If that goes off for any reason then I am in a really deep pit with zero energy plus depression and severe migraines so I do understand how devastating this illness is and that it really is time that the scientists sort it all out even if it only applies to a subset. It would be a start at least as it is dragging on for what seems like forever.
I found SAM-e to be a huge energy booster.
Also, life extension pills usually have nano particle additives like titanium dioxide. Avoid brands w this, or microcrystalline anything. Some researchers fear proteins build up on these nano particles, causing for ex brain plaque…
Jessica where are the studies showing titanium dioxide (I’ve found some but they are mostly on rats not humans) and anything bad on microcrystalline?
I have been on Savella for my fibromyalgia for 14 years. I assumed it was doing a reasonable job as my Fibro pain was intermittent and I could bare it.
Two months ago, my insurance provider (BCBS) would no longer cover it. Since we live on Social Security, we could not afford the $1,200 which was my new payment.
I have dealt with awful withdrawal symptoms as well as fibromyalgia pain that is constant and unbearable.
Is there any other drug that will work as well that my insurance might cover?
Hi Katherine
The fact that the United States has no health insurance and ridiculous prices for medication is an absolute embarassement.
I would advise you to read up on the law in your State. I don’t live in America but you guys are quite liberal in that regard. Look up if it is allowed to order medication online or import them up to a certain amount for personal use.
Then order it online from a company where 20 year old medications do not cost a fortune.
Regards,
Thomas
TRY LOW DOSE NALTREXONE. IT REQUIRES A PRESCRIPTION FROM A DO OR MD AND A COMPOUNDING PHARMACY BUT THE COST IS QUITE REASONABLE. A FUNCTIONAL MEDICINE OR COMPLEMENTARY MEDICINE DOCTOR WILL HELP YOU
Katherine:
Low dose naltrexone (~$50 a month prescription med) or Mirica (Palmitoylethnanolamide with lutetolin OTC~$60 a month) have helped me. They don’t help immediately, though, they take time to build in your system. Also, in case you didn’t know, manufacturers do have programs that support people in your situation, you should probably check for Savella. So sorry to hear you got cut off from a medicine that was working for you!
Hi,
I wonder what Dr. Myhill means about D-ribose when she says that people with gut issues
should absord it in there mouth?
D-ribose seem to work well for me but I had to stop because of horrible gut pain. I would like to follow her recommandation but I’m not sure I get it.
Do you take the dose and leave it in your mouth and then spit it out? Or you put it in you mouth an unsalive it for couple of minutes and then shallow it?
“Dr Myhill recommends that some people who have gut issues with it [D-ribose], […] should absorb it in their mouth and reduce the daily dose to 1 scoop.”
Thank you
https://www.researchgate.net/publication/364091064
Long Covid, ME/CFS, FM, POTS, … are all the same thing!
Has anyone used red light/ near infared light therapy to treat chronic fatigue, fibromyalgia and or log covid ( which I agree with earlier post has elements of both). Studies show this light therapy increases mitrochondrial action=ADP development etc. I have been using for four weeks with noticeable improvement.
PQQ content of dark chocolate is indeed off the charts in comparison to other foods, but according to this you still get less than 1mg of PQQ from an entire Kilogram of cacao powder, which has 800ug/kg (or .8mg per kilo).
https://nomosu.com/ingredients-origins-principles/cacao/
That is a lot of chocolate! More likely I’ll go for the supplement.
Little nugget of feedback: ribose is known to lower blood glucose. The dose at which it does this, is different for each person and also depends on how you take it. With food you can take more. I can take 3x5gr=15 gram per day without low blood glucose symptoms (I don’t measure it though). When I take more, I sometimes get the hypoglycemic symptoms of weakness and trembling hands (when I pay attention by holding on hand in front of me).
https://efsa.onlinelibrary.wiley.com/doi/10.2903/j.efsa.2018.5265
NOAEL for hypoglycemia is 70mg/kg body weight.