

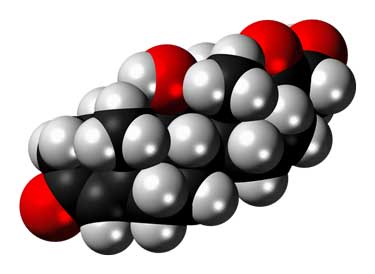
Cortisol has been a subject of interest in ME/CFS/FM for decades.
Cortisol, our body’s main stress hormone, has an amazing reach. Given the effects it has on our metabolism, inflammation, blood pressure, blood sugar, energy production and even the sleep-wake cycle, it’s no surprise that researchers early on latched onto signs of cortisol problems in chronic fatigue syndrome (ME/CFS) and fibromyalgia (FM).
Even after concluding that low cortisol levels (hypocortisolism) are common (but not universal) in ME/CFS and FM, they have never let go of the subject. Decades after low cortisol levels were first found in the disease, they’re still investigating the role cortisol plays in ME/CFS and FM.
A large, but flawed, recent study “General theory of inflammation: patient self-administration of hydrocortisone safely achieves superior control of hydrocortisone-responding disorders by matching dosage with symptom intensity” brought cortisol and hydrocortisone (Cortef – the drug used to boost cortisol levels) to the fore. The results suggested that using low-dose hydrocortisone to reduce flares was safe and effective in both diseases and provided an opportunity to dig a bit deeper and check out what past studies have found and what some ME/CFS experts have said.
The Study
Sternberg, the senior author of the paper, reported that when activated by stress, the HPA axis creates a time-delayed, 6-fold+ increased surge of hydrocortisone (cortisol) surge in the blood, which in about 4 hours terminates the inflammatory bout. As the HPA axis weakens and cortisol production declines, though, because of age, injury, and/or heredity, a short- term, beneficial inflammatory response can turn into chronic inflammation. Sternberg asserted that hydrocortisone is the only substance produced by the body which can effectively terminate chronic states of inflammation.
When given in too large of amounts for extended periods of time, though, hydrocortisone administration could produce adverse effects. The authors repeatedly cited a 1957 paper, “Diagnosis, treatment and prevention of chronic hypercortisonism in patients with rheumatoid arthritis.* (psu.edu)“, which stated that too much hydrocortisone produces symptoms such as “excessive appetite, weight gain, euphoria, insomnia, increased nervous tension and irritability, facial rounding, increase of fat pads, fluid retention, edema, irregular menses, acne and excessive hair growth.
First the participants were given a food sensitivity test (not identified) and they monitored their symptoms for a week to establish a baseline. They also eliminated foods the laboratory test suggested were giving them problems.

The study reported that a high percentage of FM patients improved while on low-dose hydrocortisone. I’s methods, though, left something to be desired.
Next came a 2-4 week induction period in which daily doses of hydrocortisone tablets sufficient to achieve a “minimum symptom” state (75% reduction in symptoms) were taken once a day from 7-9 am.
The authors reported that the participants ingested an average of 12 mg hydrocortisone per day – which is less, the authors asserted, than the 15 mg/day which produces adverse effects in the most sensitive adults. The 15 mg/day dose rate was based on the 1957 study.
The authors did not state, though, whether the 12 mgs/day occurred during the flare period or if it was an average of the doses taken during the induction and flare periods.
Dose During Induction Period
| Body mass | Week 1 | Week 2 | Week 3 |
| <68 kg | 60 mg/day | 40 mg/day | 20 mg/day |
| 68 to 114 kg | 80 | 60 | 40 |
| >114 kg | 100 | 80 | 60 |
The doses provided in the 3-week induction phase were extremely high – up to five times higher, in fact, than the doses (25-35 mg/day) which produced adrenal suppression in a several month long ME/CFS study. (See below). These appear to be types of doses typically used to treat inflammation.
Adrenal suppression occurs when the adrenal glands fail to produce normal amounts of cortisol often after a patient has been on higher levels of steroids. It is a serious matter and needs to be dealt with carefully.
Since the authors did not determine if adrenal suppression had occurred we don’t know if 37 mg/day (<68 kg), or 48 mg.day (68-114kg), or 77 mg/day (!) (>114 kg) induced adrenal suppression over a shorter period of time (three weeks). While the authors reported that no symptoms suggestive of overdosing or adrenal suppression occurred the British Medical Journal Best Practices states that it can occur within 3 weeks.
Approximately 15% of the participants failed to receive any significant benefits and were eliminated from the study.
Those participants who failed to achieve a 75% reduction in symptoms, but did improve otherwise, repeated the induction period and were given a broad spectrum antibiotic called doxycycline for approximately six weeks.
Stress management techniques (not identified) were provided to reduce symptoms flares.
Flare reduction
After the induction period, the hydrocortisone protocol was discontinued until a flare hit at which point the participants went on a 5-day “flare-quenching regimen” which consisted of taking a hydrocortisone tablet immediately and then from 7-9 am for the next four days at the following doses
Dose for the 5-day flare-quenching regimen
| Body mass | Day 1 | Day 2 | Day 3 | Day 4 | Day 5 |
| <68 kg | 30 mg | 20 mg | 20 mg | 20 mg | 10 mg |
| 68 – 114 kg | 40 | 30 | 20 | 20 | 10 |
| >114 kg | 50 | 40 | 30 | 20 | 10 |
The Gist
- Cortisol affects metabolism, inflammation, blood pressure, blood sugar, energy production and even the sleep-wake cycle.
- Studies generally find low cortisol levels are present in ME/CFS/FM
- A huge study involving about 80 doctors and 600 people with fibromyalgia and 25 with ME/CFS (and over a 1000 others with other diseases) found that about 75% benefitted from low dose hydrocortisone (Cortef) supplementation (<15 mgs/day).
- The study included an induction period in which everyone took hydrocortisone for a month and then a flare reduction period in which the participants took it for five days following the beginning of a flare. Some people took it throughout the month while taking a hydrocortisone holiday on weekends.
- The amount of hydrocortisone given during the three-week induction period was extremely high – up to five times higher than a dose which produced adrenal suppression in some ME/CFS patients – but over several months.
- The authors asserted that the low dose of the drug plus the holidays prevented adrenal suppression where the adrenal glands stops producing cortisol from occurring. While the authors stated that the average dose during the flare period was 12 mgs/day, if some of the participants took the drug five days a week 4 times a month they could be taking almost 20 grams a day – and be in danger of adrenal suppression.
- Tests for adrenal suppression were not done but the authors reported so signs of it occurred.
- From the simplistic monitoring system to the lack of blinding or cortisol testing etc. the study was rudimentary indeed.
- Past placebo controlled hydrocortisone studies in ME/CFS, while small, do suggest that a subset of patients may significantly benefit from supplementation. Baseline cortisol testing, does not, however, reveal who might benefit. Why some benefit and others do not is unclear.
- Several ME/CFS experts do embrace hydrocortisone supplementation in low levels (5-15 mgs. depending on the doctors.) They assert that adrenal suppression does not occur at these levels.
- Some studies have been able to use mind/body and behavioral techniques to normalize cortisol levels. Other studies have not.
- The large, long term studies needed to fully assess the efficacy and safety of low dose hydrocortisone supplementation have not occurred in these diseases.
The authors apparently feel that any flare must be hit hard as the recommended doses are quite high – and could easily lead to adrenal suppression if taken for very long. If someone from 68-114kg. took the flare reducing dose five days a week for the entire month (as they recommend for some people) they would average 16 mg/day. Someone >114 kg would average 20 mg/day and possibly be flirting with adrenal suppression. It appears that most people, though, limited their hydrocortisone usage to lower amounts.
If the patients experienced significant symptom improvements “during days in which no hydrocortisone was ingested (that is, when they were on a “hydrocortisone holiday”), a hydrocortisone blood test was done. If their blood hydrocortisone levels were “significantly below average” (no levels provided) they were given extra hydrocortisone.
If evidence of too much hydrocortisone appeared (moon face and a hyper state), the patient’s dosage was assessed and the “appropriate action” was taken.
The patients rated their symptoms using a 0-10 scale (not defined).
Results
No less than 2,428 participants with over 30 diseases enrolled in the study. Eighty-one physicians from 20 states participated. With 601 participants in the trial, fibromyalgia was the most common disease assessed. Twenty-five people with ME/CFS also participated. Arthritis and chronic pain diseases were common. A mishmash of other diseases ranging from Parkinson’s to dementia, to multiple sclerosis, and asthma, were also included.
Seventeen percent (n=413) of the participants did not improve, and 2,015 participants completed the study.
For those who completed the trial, the authors reported an average symptom improvement rate of 76%. The authors reported that the fibromyalgia and chronic fatigue syndrome patients had a 77% and 78% symptom improvement rate, respectively.
Remarkably – give the size of the study – no significant adverse reactions (weight gain, hypertension, gastrointestinal symptoms, insomnia, muscle pain or spasms, and hyperglycemia) were reported.
Past Studies
A 3-month, 56-person, 1998 randomized, placebo-controlled, double-blinded CFS trial used hydrocortisone (13 mg/m2 of body surface area every morning and 3 mg/m2 every afternoon (approx. 25-35 mg/day). Although Wellness scores significantly improved in those taking the drug relative to placebo, about 20% of the participants showed signs of adrenal suppression.
A 1-month, 32-person, 1999 randomized, crossover hydrocortisone trial found that low doses (5-10 mg) moderately reduced fatigue and resulted in almost 30% of the participants meeting normal fatigue scores. The authors concluded: “In some patients with chronic fatigue syndrome, low-dose hydrocortisone reduces fatigue levels in the short term.”
Another 1-month, 32-person, 2001 double-blind, placebo-controlled crossover hydrocortisone trial produced the expected increase in urinary cortisol output. In most patients, the increase in cortisol did not impact symptoms, but in about a quarter, it produced a reduction in fatigue “to normal population levels“. Giving cortisol to those patients also resolved “a blunted response to a corticotropin-releasing hormone (CRH) challenge. The authors concluded that the low dose did not result in adrenal suppression.
Dr. Myhill pointed out that the results were complicated by the fact that baseline cortisol levels did not predict who benefitted from the treatment, and that baseline levels were within normal reference ranges.

The studies suggest that a subset of people with ME/CFS do respond well to a short-term (1 month) trial of low-dose hydrocortisone.
ME/CFS/FM Practitioners on Hydrocortisone
In 2008, WebMD reported that Kent Holtorf MD routinely treats patients with 5-15 mg hydrocortisone.
Fibromyalgia researcher Lesley Arnold, MD, disagreed with that approach stating:
“The evidence in favor of using steroids to treat these conditions just isn’t there. We just don’t have enough consistent data about abnormalities in the HPA axis.” and that some FM patients have increased and others decreased HPA axis functioning.
Dr. Teitelbaum believes that adrenal fatigue plays a major role in ME/CFS/FM and regularly uses ultra-low (<15 mg/day) doses of bioidentical hormones. In the latest edition of “From Fatigued to Fantastic“, Teitelbaum says it often makes ME/CFS/FM patients quickly feel better. Teitelbaum says he usually goes by symptoms but that a fasting cortisol of under 14 mcg/dL, especially if ACTH is under 25 pg/mL or glycosylated hemoglobin is 5.2 or less, suggests a trial of 5-15 mg hydrocortisone is warranted.
He asserts that the fears of using the hormone date back to the early days of hormone usage when doctors, not knowing any better, vastly overdosed their patients, causing some of them to die. His patients usually take it all in the morning or about 2/3rds in the morning, and the rest around lunch.
Dr. Myhill appears to be moving more to pregnenolone but does prescribe low dose hydrocortisone (5-10 mg) in patients for whom the Adrenal Stress Profile test shows a reduction in cortisol. She states:
“The use of hydrocortisone allows the adrenal gland to rest a little and, in time, resume normal production, at which point the hydrocortisone can be stopped. This removal of the hydrocortisone support should only happen once the patient feels considerably better, which may take several months or even years.”
Dr. Myhill prescribes cortisol “only in patients with a proven deficiency”. She uses 5-10 mg (rarely 15 mg) to be taken either in the morning, or morning and lunchtime. At that low of a dose, she reports that cortisol levels do not need to be monitored.
Other Possible Ways of Normalizing Cortisol Levels

Mind/body interventions may help some people normalize cortisol levels.
The evidence that behavioral modifications such as mindfulness based stress reduction (MBSR) can normalize cortisol levels is mixed, with some studies finding so and others not. A major review, however, found that interventions like yoga, meditation, tai chi, acupuncture, mindfulness, religious/spiritual practices, cognitive behavior therapy and coping did tend to normalize cortisol levels, and were associated with reductions in inflammatory processes.
A “health education program” and three CBT studies also reportedly increased cortisol levels in their mix of “ME/CFS” patients. Another review of various interventions in fibromyalgia, however, to improve cortisol, found only “small overall effects”. A 2-month isometric yoga program in ME/CFS did improve fatigue and reduce anxiety levels but did not affect cortisol levels.
One CBT study, interestingly, found that reduced sleep duration was associated with low cortisol levels. Poor sleep has been associated with reduced morning cortisol levels before. Researchers have recognized that poor sleep could be responsible for some of the low morning cortisol levels in ME/CFS. On the other hand, cortisol does affect the sleep-wake cycle.
Conclusions
Two Different Approaches
Tinkering with the hormones carries real risks. The North Dakota study and the ME/CFS experts used two distinctly different approaches to hydrocortisone.. The North Dakota approach used doses more designed to snuff our inflammation than to provide adrenal support. They used a three week high dose induction period to stabilize the patients and then quickly hit flares hard with higher-dose, quickie 5-day hydrocortisone regimen. They also proposed that some patients can safely stay on the higher dose regimen over long periods of time time so long as they did not take hydrocortisone on weekends.
The doses given during the three week induction period were high enough to suggest that adrenal suppression was a real possibility. The authors reported, though, that no adverse side effects suggestive of overdose occurred.
The North Dakota study was not rigorously done. It was not placebo-controlled or blinded; neither the doctors in the study, the disease criteria, the method of measuring symptoms, etc. were provided. The average 12 mg/day dose per patient was not explained. The study also reported that the participants in a wide variety of diseases improved by over 60% – a remarkably high number. The main source of information on adrenal suppression came from a 1957 paper. Despite the high doses given during the induction period, no tests were done to determine if adrenal suppression had occurred.

The large, rigorous studies needed to validate the safe use of low-dose hydrocortisone to battle flares have not been done.
No rationale was also given for providing the broad spectrum antibiotic to everyone who failed initially to significantly improve. That addition seemed strange given worries about antibiotic resistance and possible gut issues.
Instead of using hydrocortisone to respond to flares, the ME/CFS practitioners that prescribe low dose hydrocortisone (5-15 mgs/day) have their patients use it consistently – and at much lower doses.
The only ME/CFS hydrocortisone study to last several months did find adrenal suppression in some patients, but at much higher doses (25-35 mgs/day) than typically used by ME/CFS/FM experts 5-15 mgs/day).
While the limited evidence we do have (1 one-month study) suggests that the hydrocortisone used in this manner is safe, no data exists on the safety of long term low-dose hydrocortisone use in ME/CFS/FM. The ME/CFS/FM experts who use it do appear confident, however, that when used in low doses it is safe. .
ME/CFS studies suggest that some ME/CFS patients do readily respond to everyday doses (5-15 mgs) that were significantly lower than the doses used in the North Dakota study. The higher dose, hit the inflammation hard approach used by the doctors in the North Dakota study is a very different approach indeed.






Every female should consider and check estriol, progesterone. Everybody should think about dhea, pregnenolone, 5-htp. Hormones can be keys.
Hi Cort, I saw Dr. Teitelbaum on Ari Whitten’s podcast and he talked about “adrenal fatigue.” I don’t remember if Ari said anything but he (Ari) doesn’t believe in it after digging into all the studies etc. I have a lot of respect for both so hard to know what to believe. BTW you did a great job on Ari’s podcast. 🙂
Thanks. That’s good to hear. I was really PEM’ed at the time and then we had to move into my van which is making my chemical sensitivities flare up for some reason. Glad it wasn’t a disaster!
I respect them both a lot too. Teitelbaum has been there from the beginning and Ari is taking a serious look at these diseases. He’s pumping out a lot of really interesting stuff.
The studies have been up and down but a consensus has emerged that salivary cortisol levels are low in AM in ME/CFS and I believe FM. I’m not sure what they meant about adrenal fatigue. I just saw a study which showed that the adrenal glands are able to respond when pushed…so it may not be the adrenals themselves that are the problem.
Messing with hormones sounds scary. My daughter who has eczema used a regimen involving hydrocortisone cream application daily to large areas of skin for a year and is now suffering horrendous rebound effects – worse than the original eczema. So I’m skeptical of drs who claim it’s harmless!
Great article Cort. Did you give a journal reference for the large study?
I really have to laugh at all the times, after all the work I put into these blogs, and I FORGET to put the title of the study in there. Thanks for letting me know.
“General theory of inflammation: patient self-administration of hydrocortisone safely achieves superior control of hydrocortisone-responding disorders by matching dosage with symptom intensity”
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6581742/
Hi Cort, I have been taking Dhea for 20 yrs. started on low dose prendsone due to low cortisol tests in 24 he urine collection and bloods multiple times then moved on to DHEA . Blood pressure now normal energy much better. I was unable to stand or drive at times before this. I still relapse and have never resumed worked as Reg Nurse.
It’s what I do. I monitor my seronegative arthropathy myself and have done for quite some years now. I try to stay low dose ie. no more than 25mg per day for first day or or two, then usually going down to 12mg then after a say 2 to 3 days go even lower to 6 to 8mg per day. However, when I wean off them, my energy decreases unless there is a stressful event then my natural cortisol levels increase without a need for any steroids. this up state, can last for up to a week depending on the severity of the stress event. Then after that, a big down feeling and the need for a 25mg hit is the only way back to having some tangible energy. Love your blog. You have helped me greatly. Thank you.
Thanks for covering this. I believe a lot of patients could benefit from low dose hydrocortisone if they have low cortisol levels.
I originally balked at taking hydrocortisone, knowing that steroids could cause problems. However,my naturopathic doctor convinced me to try it, and after the first dose gotta me from being in a sleepy heap on the floor to functioning, I was sold.
I took 10mg at 730am, 10mg at 11am and another 5mg at 3 pm for 3 years. Then, I started to notice I was gaining weight around the middle, tested 24 hour cortisol and found it high normal.mostbof the day and high in the afternoons, so gradually dropped my dose to 2.5g once at 10 am and lost the 15lbs I’d gained in 2 months without changing anything else.
It’s a game changer when thoughtfully managed. Everything I’ve seen, though, says not to go over 30mg a day – that we want only a replacement dose.
have a nice day
I am writing from Turkey
I have cfs and severe depression for 35 years
I want to try cortisone
I am 45 years old
i weigh 54 kilos
my morning cortisol is 6.7
What is your morning cortisol?
What do you think
how should i use it Thanks a lot for the reply ???
Interesting that some people diagnosed with ME/CFS actually have Lyme disease and that a treatment for Lyme disease which makes some people feel better is doxycycline. I don’t want to get into a Lyme debate, but let’s just say there are alot of confounding variables, and the addition of doxycycline is one of them.
That’s interesting. I didn’t think of that! 🙂 The early more rigorous studies noted how poor sleep and other factors could also be impacting the cortisol levels.
I have taken 5-10 mg hydrocortisone for most of the 34 years of ME/CFS. It has been life-saving and has not caused adrenal suppression. My endocrinologist is the head of endocrinology at the University of Colorado and feels this is safe. I take a little more hydrocortisone if I’m having surgery or under a lot of stress.
A book, “Safe Uses of Cortisone” was written many years ago by William Mck Jefferies. He discussed the dangerous practices that happened many years ago when physicians prescribed too much cortisone and caused harm. This gave cortisone a bad name. If used carefully it can be very safe and helpful.
Thanks for providing your experience. I, too, would feel safe under the care of the head endocrinologist at U of Colorado! I don’t know if anyone has ever suggested I try hydrocortisone.
Dr. Teitelbaum mentioned that book by Jeffries, I think in the latest version of Fatigued to Fantastic.
Tanja,
Thank you so much for this. ( And thanks to you, Cort, for the article — I remember discussing low-dose hydrocortisone with you in the past.) I have been debating starting low-dose hydrocortisone for some years now, and this is the go-ahead I needed.
But I do have a couple of big caveats to share here about steroids, from my own personal experience — things I haven’t seen mentioned yet in this discussion, or elsewhere. I will have to give the whole backstory, so I apologize for being so long-winded, but please bear with me.
The “gist,” though, is that my experience amounts to a HUGE warning against higher doses of steroids — and especially a warning about the dangers to some of us of coming back off of those doses too quickly. (And a positive point about low-dose hydrocortisone.)
In 2005 I had an acute viral (idiopathic) pericarditis attack with pleurisy and water on the heart. It was a true emergency; I almost died. They drained the fluid and did a pericardial window operation to (hopefully) prevent future build-up of fluid between the pericardium and the heart. In the fluid they discovered evidence that I had had pericarditis many times in the past — a lot of fibrous scar tissue residue was in there. This time, however, it had been far, far worse. Unfortunately, after the operation I was prescribed high-dose prednisone as an anti-inflammatory for 10 days — which nowadays would never be done for pericarditis, because it causes viral replication to increase greatly. It has been shown that use of steroids to treat pericarditis is the key marker for developing a chronic, recurrent, form of pericarditis, which is indeed what happened with me. Nowadays, no one would ever prescribe steroids for pericarditis. I’ll come back to this, in connection to CFS/ME.
The approved treatment for idiopathic (but presumed to be viral) pericarditis is aspirin, colchicine, AND EXERCISE RESTRICTION. Because it turns out that pericarditis is the only other condition (to my knowledge) that causes what we now call PEM!!! After that operation, I never recovered. I was like an ICU patient for months and years, much of the time, and I had drastic and dramatic PEM (is there any other kind?). But at that time I had no way to describe this symptom to my doctors. It made no sense to me at all and I couldn’t convey it to let doctors know how ill I was. However, given that flare-ups after efforts to exert and a need to drastically restrict exercise are universal in recurrent pericarditis, I was simply diagnosed with recurrent pericarditis. Neither my rheumatologist nor any of my other doctors nor I myself had ever heard of “PEM.” The language we used was simply “restricting exercise” as the salient ongoing treatment for pericarditis.
Pericarditis itself was a baffling mystery to me, and so was my invalid state (especially after the pericardial inflammation had mostly cleared up after about a year). I started researching pericarditis back in 2005 and could probably have an MA in the subject by now. And somehow by chance in 2015 I ran into references to exhaustion after exertion and was led to the 2015 IOM Report on CFS/ME (SEIDS). And there, for the first time, I encountered the term PEM and the fact that it was the hallmark symptom for CFS/ME. The instant I encountered that term, light flooded over my previous 12 years of experience. Yes, I had had recurrent attacks of pericarditis up until 2005, but after that operation, I had also been suffering from CFS/ME. Since then, I’ve been studying the latter as well and it all makes a great deal of sense. (And we all know how comforting that is, after enduring our own incomprehension and the doubts and suspicions of others.)
So here are the interesting things, that followed. Number 1 — in retrospect it is clear that my CHF/ME began with that viral pericarditis attack in 2005. I was bedridden for days or weeks or months at a time (you know the drill.) In my very best periods, between flares, eventually, I could go out of the house in the car 2 times a week if I was very careful. But it took 10 years and the 2015 IOM Report for me to have the slightest idea of this. But my rheumatologist was furious that I’d ever been given the high-dose steroids. In fact, the steroids almost killed me: I was in the hospital longer and in worse condition from a “prednisone withdrawal reaction” than I had been from the acute pericarditis operation. After 10 days, they had tried to wean me off the prednisone over five days — until on the fifth day 9-11 carted me off, sicker than I’ve ever been in my life. In the end it took my rheumatologist SIX MONTHS to wean me off. We all know how sensitive some of us can be to certain medications, and it makes me shudder to read about the cavalier changes of doses in the cited studies above. PLEASE warn doctors about the possibility of extreme sensitivity to steroids. And please start off very slow and ease off slowly.
About prednisone vs hydrocortisone. For my prednisone withdrawal reaction, the hospital gave me intravenous hydrocortisone instead of prednisone. It was heavenly — so much more tolerable to me than the prednisone had been. I was able to sleep all night in the hospital with hydrocortisone. (On prednisone, I had not slept for one minute the entire time and was extremely wired and anxious.) Therefore, I was switched to hydrocortisone tablets when I went home and I began the very slow withdrawal process. And when I finally got down to the very low 7.5 and 5 dosage levels, I felt wonderful. But as soon as I was entirely off the hydrocortisone, I went back to being often bedridden or housebound. I’m not saying that on the low-dose hydrocortisone I was anywhere near back to pre-CFS levels — but I felt well and I consistently had enough energy for my relatively small daily tasks. My rheumatologist wouldn’t consider letting me stay on at that low dose, though. He was dead against steroids long term and he knew how fragile I was, if I ever had to wean off them altogether. Since then, recently, I’ve seen studies of low-dose hydrocortisone not having the deleterious effects of higher doses, and Tanja’s comment is wonderful evidence of that. Im quite a bit older now, and would like to be able to finish a project I’ve been working on a long while here, in these last years of mine. So again, thank you, Tanja and Cort. I’d love to hear from others with low-dose experiences as well.
BTW, those final gradual reductions below 5 units of hydrocortisone really took forever — to avoid another withdrawal reaction. So again, I shudder to read about the cavalier way the studies Cort has just reviewed seem to adjust doses — and I would be totally against using higher doses of 30-35 units to “fight flares.” My experience tells you whyI say this. Be very, very careful. Please remember, too, how the pericarditis research has shown that using steroids to treat inflammation in pericarditis actually causes the virus to replicate and become more entrenched — that is what actually caused my recurrent pericarditis in the first place. Or at least made it much much worse.
Thanks for your patience!
Thanks for your clear and detailed account Janet!
Increased viral replication while being on steroids would be a very important thing to take into consideration for many ME patients. Does the research points to this on high doses only or also to lower long term doses?
If you easily could find and link some key research, that would be great but don’t exhaust you on my account.
This has given me so much insight into why some of us get a viral infection & the virus runs free, not being cleared up by our bodies…
If we are under a lot of pressure & get our body to pump out ‘cortisone’, we can replicate the situation that happened to you
dejurgen,
In acute pericarditis attacks, the administration of steroids (back in the bad old days) was ALWAYS at the high-dose level. And then that turned out to be a disaster. The studies showing that steroids caused viral replication and were stronglly linked to developing recurrent or chronic pericarditis started coming out on Pubmed during the 2-3 years after my disastrous experience with prednisone in 2005. But now, you will find the warning NEVER to use (high-dose) steroids for pericarditis in virtually every medical site on pericarditis which you might consult. And I too have always wondered why we don’t hear about the possible threat of viral replication from steroids in the CFS/ME literature. It might simply be because, in general, when steroids are given in auto-immune diseases the patient is in such bad shape in terms of inflammation that there really isn’t any other choice. It’s life or death really. (But no quantity of steroids is ever given in the case of pericarditis. You won’t have any trouble finding the pubmed articles on prednisone causing recurrent (or chronic) pericarditis, if you google it.)
But in contrast, this seemingly more recent idea of giving a “physiologic” level of hydrocortisone only, rather than a “therapeutic” level, is something I’ve only run into in roughly the past 2-3 years. Maybe Cort knows more about this? And I think that I might have actually first read about using physiologic levels of hydrocortisone on that standard pharmacological website — “drugs Rx” is it? I think it was covered in the dosing recommendations for hydrocortisone.
Tanja’s comment about having been taking 5 or 7.5 mg for most of 34 years was something brand new to me, and I’m so happy to hear about it. And also the Hortolt patient who mentioned being prescribed this as well. To me, this is something really new and really good to come out of this post by Cort — but NOT the idea of using hydrocortisone to “fight flares” that furnishes the headline! I’d love to see another post that is strictly about the very low-dose hydrocortisone treatment protocols for CFS/ME.
I really appreciate the info about the Jeffries book, as well.
Hi after suffering from arthritis and fibromyalgia and oral facial lip swelling with allergies for 25 years and on chronic pain with chronic stiffness ,my investigations over years to get to the bottom of it is ,caused by herpes cold sore virus which penetrates
into your nerves And they keep breeding With our muscles causing nerve pain and deep tissue tenderness with bruising pain and stiffness over many years as you get older it gets chronic,with trial and error on many different medication I found cortisol tablets are most affective starting on 25 mg coming down to 10 to 5 mg with no side affects it stimulates the body bringing me back to life ,it is a life saver drug , constant inflammation on the body can damage the body and our organisms and stop our body being attacked from disease ,which leads to other problems, as it has happened to me for many years that many to list but cortisone tablets is the cure the wonder drug ,now many doctors are not aware of it as doctors have been taught to not to give prednisone for to long , on low dosage it’s fine ,body gets attacked our cells are affected when disease hits us ,it’s saved my life on plenty of times having low immune system as a result of being electrocuted hope.I Can help others in pain and suffering I am living proof
Everyone is unique!- What is an adrenal suppressing dose for one person may not be for another. It also depends on how long, months years, a person takes Hydrocortisone and in what doses. Why were such high doses given in the induction and even the flare stages? Those are definitely adrenal suppressing doses. 10-15mg may not be. However, if symptoms disappear with taking cortisol it seems that it might be necessary to take cortisol even if adrenal suppression does occur but that is a serous matter. Can be life threatening to not be able to produce cortisol on your own. Proceed with caution but if it works it helps a lot. Agree with previous commentator, Jefferies book The Safe Uses of Cortisol is a good one but the 20mg/day he gave his patients is a suppressive dose for many. Learn all about Adrenal Insufficiency before deciding to take cortisol.
Wow. Thanks for pointing that out. I completely missed that! They said the patients averaged 12 mg per day After that I didn’t even look at the amounts in the tables.
Those are very high – all potentially adrenal suppressing.
I have amended the blog to note that.
Thanks for sharing this information. I suffer from Fibromyalgia and pituitary gland problems. I have had to take the same doses of hydrocortisone that this study mentioned. Taking corticosteroids of any kind is extremely serious and I completely disagree with this strategy. I have become an advocate and studied so much on cortisol that I could have had my medical degree.
The HPA axis and adrenal glands work like a fine tuned orchestra. You cannot go on and off cortisol and expect to improve. It might make you feel better for an hour but as time goes on you feel like a truck has hit you. I live this nightmare every day and all I want to do is wish that I never had started hydrocortisone or any cortisol steroid. It does have permanent affects on your mind, body, and energy. I really get concerned about studies like this because it can cause so much more suffering. There are still things about the HPA axis and adrenal glands that doctors don’t know. Science is not there. Yet they irresponsibly make recommendations to “try this out “. Messing or supplementing cortisol is not the same as your body making it’s own. It is literally impossible to match the exact cortisol levels at the perfect time that individual human bodies create naturally. It just doesn’t work and the likelihood of permanently damaging that perfect orchestra is all too real.
I know this from living it. Your body completely morphes and changes and weight gain is unbelievable, your pain is unrelenting because your muscles deteriorate, your immune system is extremely low, your energy is so low that you can’t stand for 5 minutes, and the worst part is that your mind is severely affected and depression beyond despair is guaranteed. All due to evidence based side effects not well known. Not to mention, the study is incorrect that you can take “holidays”. The human body does not work that way. The longer you take steroids, the risk of being completely dependent on it in order to live. The adrenal glands do not know what a “holiday “ is, once they are suppressed by steroids (even for a month or two) they never return to normal. I know I sound dramatic but people need to be warned. I had to take steroids to continue living due to pituitary damage, but it is a devil in disguise.
In my 20s I tried Cortef. It did not help and seemed to make me worse with longer use. Tried it two different extended times.
However with surgeries, I do have to have it IV for me to not crash. We learned this the hard way.
Sara C
“Taking corticosteroids of any kind is extremely serious and I completely disagree with this strategy.”
Amen, Sister — see my remarks above
I too am a pituitary patient and have been on 20-30 mg of hydrocortisone for 6 years. My tumor was found through Dr Bateman’s office and likely part of my issues still are ME/CSF as well.
Taking Hydrocortisone has helped me get on my feet and have half a life.. I can work part time and exercise some. However.. there are pitfalls and even my excellent endos missed things in terms of long term effects. Yes, the weight gain sucks, but issues like Osteoporosis and cataracts were completely overlooked until I got compression fractures in my spine and will probably have cataract surgery in the coming months. I am 55 and 2 years post menopause but have the bones and eyes of someone much older.
I used to be very active and live in the mountains of Idaho. Backcountry skiing and kayaking are in my rear view mirror, but I can walk and gently nordic ski.
Also. When you get the generic version you might get one of 3 brands. Greenstone Brand is the cleanest, made by Pfizer, and pretty much the same as Cortef. It is very hard to get right now because of COVID. Even at it’s best hydrocortisone is mixed bag as Sara very fully and accurately portrays above. Go in with your eyes wide open if you choose to take this course. there will be no ‘holidays’. There are costs that perhaps outweigh the benefits.
I recognize that because my HPA axis is functioning at a subpar level I may only be seeing it from that angle but if I could find a way to go off HC, as well as thyroid meds and HGH injections I would be eternally grateful.
That is my two cents amigos and amigas. Be well and Hang in there
75% improvement sounds huge. Do you know what that means in concrete terms and how they measured it? Any link to the paper?
HI TK the paper is “General theory of inflammation: patient self-administration of hydrocortisone safely achieves superior control of hydrocortisone-responding disorders by matching dosage with symptom intensity” (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6581742/).
The authors used a 0-10 rating scale and referred to another paper on what that was. I don’t know what it was. It’s an enormous rate of improvement that honestly seems unrealistic to me. Then again they used much higher doses of hydrocortisone than ME/CFS practitioners do. Those doses at times dwarf how much cortisol the adrenal gland is putting out and could be adrenal suppressing – particularly during the induction phase. The big question is whether it’s safe.
Thanks as usual, Cort. Even if it is not practical as a treatment, it could prove the cortisol theory and give us a clue towards the cause and solution. I hope it pans out.
Does anyone have an answer to HIGH morning cortisol levels? The symptoms associated with it for me are startling awake, severe panic and severe hot flushing. This also occurs with any minor stressor. It’s like a shot of adrenalin keeps going off.
It may be Adrenaline that you are experiencing. If cortisol levels go too low in the early hours of the morning the body reacts with adrenaline. The way to know would be to measure your cortisol levels first thing in the morning. Low blood sugar can also cause the adrenaline release you describe.
It has long been known that a low dose of cortisol can help a subgroup. patients. But certainly not for everyone. There are patients who produce a lot of cortisol at certain times of the day and especially during stress. The disadvantage of cortisol is that the adrenal glands can stop producing it. Then you have a big problem. The low cortisol levels are due to exhaustion and are a result of the autonomic dominance of the nervous system. Or a dysfunctional HPA axis.
“ The low cortisol levels are due to exhaustion and are a result of the autonomic dominance of the nervous system. Or a dysfunctional HPA axis.”
Would you have any links to information /research on this? I’m particularly intrigued by the impact of the nervous system state on cortisol?
Thanks
Dee
The use of hydrocortisone along with bio-identical hormones, thyroid and adrenal support has made a huge difference for me. Hydrocortisone dosing can be divided up during the day to avoid crashing in the afternoon. Custom compounding of thyroid support and hormones and a product called ” Adrenal Factor” have improved energy levels substantially. I’m a Holtorf patient and they also have recommended some other products that help. NT Energy factor improves mitochondrial function and aids in cellular repair.
I have used hydrocortisone successfully for the past 4 years. I’ve had moderate CFS/ME/FM for 27 years, and after taking Cipro/Flagyl I had a major relapse resulting in being largely couch-bound. My Naturopath recommended I try nydrocortisone and thyroid meds. It is extremely difficult to get the dosage correct, and requires vigilance to symptoms in order to get it right (this can be daunting, as the side effects of too much mirror those of too little). Absolutely essential is getting the right balance of thyroid and cortisol – for me, that ended up meaning iodine supplementation instead of T3/T4 meds, and I use compounded hydrocortisone instead of Cortef (as it upset my stomach). Also key is that hydrocortisone stays in your system longer than you may think, so any dosage changes must be done very slowly and symptom changes can be experienced up to a week after the dosage change. I also use bioidentical hormones, which are an important part of the mix.
My current dosage is 4.5 mg, twice a day, morning and lunchtime. Symptoms improved include energy; emotional regulation; brain function; sleep and reduced pain. I am now able to take care of things around the house (most of the time); take care of my son; work 5 hours a week; and occasionally get out for a short walk. It has made me feel like I have a bit of my life back!
Opiates and cortisone were the only meds that brought my fibro pain under control. I no longer need them!
Hi Pam
When you say the opiates and cortisone brought your fibro pain under control please explain how long you took them and why you no longer need them?
I have often thought that taking a smidge of hydrocortisone might be helpful for me. Having an EDS hypermobile spine, L4/L5 is quite painful and although I had a severe reaction to a steroid shot in that area (and it really didn’t do much good for that localized pain), I noticed the pain levels in the rest of my body dropped substantially for a couple of weeks after.
My endocrinologist has only given me nighttime saliva tests for cortisol–which are unremarkable. She’s a straight and narrow doctor I go to for euthyroid Hashimotos and it was a fight to get her to prescribe porcine medication rather than just levothyroxine. She says I may not convert to T3 but is unwilling to test for that. So not much symptom (fatigue) improvement. I would probably never get her to consider hydrocortisone.
Lately I have tried D-Ribose with some tiny effect. Also liquid L-Cysteine (precursor to glutathione). The liquid form is manufactured by a strange little company who mixes it with natural spring water which carries a huge variety of trace elements. I do notice an improvement using it but will hold my judgement until I track the effects for a longer period of time. I find the element list similar to Shilajit.
Read some discussion in 2011 on Phoenix Rising on (micro element) hair analysis. I was wondering if the tendency to get ME/CFS was partially genetic. Also read a fairly recent meta analysis which said that there was some evidence that the U haplo-group was more prone to get ME/CFS. Apparently there are almost no mitochondrial defects in ME/CFS patients and the trouble seems to be in the DNA.
All this makes me wonder if there are small deviations in DNA instructions which cause issues in some of the energy cycles of the body–deviations which make some of us more prone to ME/CFS. Perhaps some of us need some of these micro elements to ‘patch’ our faulty DNA instructions, as the body often has a number of pathways so if one system is not functioning correctly another will often compensate. Perhaps some of these compensating elements which are now not commonly found in commercially farmed food, might, for some, be a way to correct this.
So my experiment continues…
Thank you, Cort, for putting together this blog on hydrocortisone. Low dose cortisone is apparently helpful for some people with neuropathy. Being general leery of steroids, I figured my neuropathy wasn’t that bad.
But when I got shingles, prednisone was the only thing that relieved the pain. 2.5 mg bid. But the side effects got to me pretty quickly: weird mood changes, grumpiness, and sleeplessness.
When two of my cervical discs herniated, prednisone again was the only thing that got the pain to the point that I could sleep. But it took a huge dose: 60 mg for 6 weeks, then tapered down as I could depending on the pain. Probable result was cataracts a few years later.
It is a juggling act. There are definite risks to steroids, and cataracts are not so easy to correct as some people say. But, it is a juggling act.
You might — just a thought — try asking for hydrocortisone instead of prednisone if you need to take it again. The difference between the two was night and day for me. Prednisone has huge mood effects and weirdness for me, but not the hydrocortisone. (I explained this more above.)
Beware, ME/CFS and auto immune disease which supposedly attacks it’s own tissue is active viruses, which your immune response causes inflammation to keep under control. Your immune system is the only way to defeat active viruses. The use of any corticosteroid which pharmaceutical companies and doctors have been using for 50yr or more for inflammation has been interfering with people’s immune system and the virus gets more viral load. Everybody has different immune systems, some stronger than others. There lies the reason some recover quickly after viral reactivation and some struggle for various lengths of time, and some with weaker immune system or ongoing stress or corticosteroids use may get worse. Any immune suppression will give you short term gain, long term pain. All autoimmune diseases give chronic fatigue because they to are viral and the use of corticosteroids have cured none and possibly made worse. Big Phama, making a fortune from corticosteroids, and doctors will never admit they are doing harm. So be very careful!!!
Thanks very much Cort for sharing this interesting information.
Dee
I do not believe that the cortisone is ‘fixing’ things, my belief is that it knocks down at least some of the the neuroinflammation.
And so many people will feel better for a short time, but i do not believe it stops the disease process, and may mask the damage that is occuring.
That said, when a person needs to be able to do critical thinking or critical activity, the short term benefit might—imo only—outweigh the known risks.
But back to needing sensitive —usually expensive—- testing to show ncbi ‘cog fog’.
i am encouraged by seeing article from last year telling how an scientist (researcher?)—who received a large $$$ infusion—has plans to not just make cellular/mitochondrial processes more discernible, but to also provide online training. Hope Uri Manor impacts cfs/me in a big way!
https://www.salk.edu/news-release/salks-uri-manor-to-receive-over-690000-from-chan-zuckerberg-initiative-to-advance-biological-imaging/
Sunie,
You said: “I do not believe that the cortisone is ‘fixing’ things, my belief is that it knocks down at least some of the the neuroinflammation.”
You are probably describing high and medium doses of steroids, here. And I agree, even if some neuro-inflammation is abated by steroids at those level, it is absolutely not worth it. They are so dangerous.
And, based just on what I experienced in my own case with high-dose steroids for pericarditis — which is absolutely the wrong treatment b/c of viral replication and causing chronic recurrent pericarditis — I never felt that the high doses were doing anything helpful for me at all.
But when I was being tapered OFF of hydrocortisone (thank God), I did notice a definite effect when we finally got down to 7.5 and 5 mg. It wasn’t an anti-inflammatory effect. It was definitely something like a gentle stabilizing of (I suppose) cortisol levels, because that feeling of shakiness and fragility that told me I had to rest was effectively countered over the course of weeks, when I was on those low doses. But even when I got down to below 5 mg we had to go very very slowly or I’d have had a withdrawal reaction. ( It might be that I have an extreme sensitivity because I seemed dependent on it even at those very low levels. But it’s worth warning others of this possibility.) BTW I had surgery in August for a kidney stone, which really scared me, and yet I came through it just fine. How can that be? Yet I have orthostic intolerance and I am mostly housebound, and was then? (Why don’t we all have Graves disease . . . ?
Anyhow, the most I would expect, in opting to take low-dose hydrocortisone now, at age 74 (in order to work on and finish a project), would be a gentle supportive effect on my shakiness and feeling of near-collapse — so that my “good” periods of having “some” energy might last longer and be more consistent.
We’ll see! I’ll report on this in the future.
I meant Addison’s Disease, not Graves . . .
Interesting, thank you Janet 🙂
Re Addison’s Disease, i have wondered if there was more than one pathway for an Addisonian Crash to occur,
where the symptoms/signs a person experiences are the same as those experienced by a person in Addisonian Crash, and severe but not immediately life threatening.
And with testing showing normal blood levels, so perhaps a localized problem.
Had hoped Bhupesh Prusty or Ron Davis or Alain Moreau…..etc. would have solved it already.
Glad bright and inventive people are doggedly going after the solutions— and respecting patient’s thoughts/experiences.
Wishing you well, Janet, looking forward to hearing how it goes for you.
Cortisol is a god sent hormone . Everything that continues to be said about this hormone is completely wrong . Cortisol has to be dosed as per the circaidian rythum of the body or it is toxic to the body . I use a medtronic insullin pump which pumps liquid cortisol into my body just like the pulsatile way the HP axis does . Bye taking cortisol in this manner a person can with stand large doses with no side effects . The body can make anywhere from 15 mg to 300 mg per day depending on the type of day .This obserd idea that 20mg is the one size fits all treatment is so fare fetched . I take at least 60 mg per 24 hours via the pump and spread out to match the natural rise and fall of a healthy body with no issues . Now I am living a great life again .
How did you learn about using the pump and is a doctor monitoring you.?
https://www.youtube.com/watch?v=q1de09ghB4M
Cortisol pump . The future of treating low cortisol symptoms is hear now .
It’s so interesting to read all the widely varied responses. I will share my experience in case it helps someone, though I may need to come back and update it in a few months.
I had signs, especially orthostatic issues, for some time before experiencing my first real crash while on the job in 2015 – which scared the crap out of me because I truly thought/felt like I was dying. I was doing a very physical outdoor job at the time, and was paying out of pocket for a membership at a Functional Medicine practice. That Dr immediately identified the issue as ‘adrenal fatigue’ (which I don’t fully buy into, but I had not yet heard of ME/CFS) and gave me a short course of Prednisone to help get me through some travel I had to do the next week. It was like a miracle. I still felt that things were ‘off’ but I couldn’t believe the difference it made. But we knew Pred wasn’t something I could stay on, so when I got back he moved me to 25mg Hydrocortisone, broken up into 10/10/5mg throughout the day. It made SUCH a difference! Again, I could still feel something underlying was wrong, but I was able to function at full capacity. Over time, I was able to reduce my dose to where I finally stabilized it at 12.5mg/day. I was at this dose for almost 3 years; I felt very stable in every way, was able to lead a full and active life, and was kicking a** at my job. I gained a little weight, but had been pretty underweight before so that was actually a good thing.
When I finally got full-time benefits at my job, I had to switch to Kaiser Permanente HMO. This meant I got to see an Endocrinologist to do the actual morning cortisol and ACTH Stimulation tests, both of which came out middle-of-the-road normal. Great news, but both she and my Kaiser PCP were dead set against my continuing the HC because they couldn’t show that I ‘needed’ it and due to fear of the associated risks (breast cancer, adrenal suppression, osteoporosis etc) – regardless of how much it was helping me be fully functional. The Endo thought maybe it was just masking something else like CFS or FM, which were not within her specialty. So, I weaned off very slowly over several months.
Ever since then, I have been back on a roller coaster of ups and downs with my energy and overall health. I finally learned about ME/CFS and went through the battery of specialists and testing to rule out nearly everything else for the differential diagnosis. I have had occasional periods of remission, from a day or two up to a few months at a time (always in winter, summers KILL me). But over the last year, that roller coaster has only gone down, and my usual winter reprieve didn’t come – I’ve only gotten sicker and less functional. I continued to push myself though work full time, but it was harder every day; I was basically in a state of ‘rolling PEM’ and just crashing after work every day and all weekend.
I was finally able in March to get the 2-day CPET from Workwell, and learned that my AT was at a mere 81bpm. The report stated that it is not safe for me to even do sedentary work at this point. So I took medical leave and am now applying for LTD through my job. Even after 2 months of resting at home, I am not feeling much better. I just don’t seem to be able to come out of the crash state for very long at all. I mentioned to my husband just last night, that I kinda wish I could just go back on the Hydrocortisone – at least I was functional, risks be damned!
So, today I went to my first appointment with a new PCP at Kaiser. And what do you think she recommended (with no mention of it from me)?? Yep, low-dose HC! She said even at KP, ideas are changing on ME/CFS, and she (and other Endos there who are more recently trained) think low-dose HC is safe. I think at this point, based on my prior experience with it, I have to give it another try. She prescribed just 10mg/day over two doses of 5ea.
Now, as I mentioned in another thread, I do have concerns about taking anything that may alleviate the symptoms that I use to gauge my pacing or that gives me energy, but may lead me to exceeding my limits and making the underlying condition worse in the long run. But I will keep that firmly in the front of my mind while I try this approach again, with both great caution AND hope.
I know this doesn’t work for everyone, but it certainly did wonders for me in the past. Fingers crossed it helps again – AND I’ve learned a lot since then about managing my activity levels, so maybe between the two I’ll get some life back. I will report back here after I’ve given it some time.
Of course, everyone has to make their own decisions about what will or won’t help or hurt them. Wish things were a little clearer or more cut-and-dried with this life-wrecking disease! Good luck and many blessings to you all!
I just started low-dose hydrocortisone while in a very bad flare of CFS/ME (I’ve been mostly housebound, and often couch-bound, for many weeks). I did see some improvement in my functioning; I’m spending less time lying down during the day, and was able to do some light cleaning and even a tiny bit of mental work on my computer. My CFS/ME specialist prescribed it, and I take 5mg in the morning and another 5mg (if needed) at noon.
I’m still unsure about this treatment (and have some concerns about long-term safety), but I am grateful to have experienced a small benefit from taking it.
My sincere best wishes and good luck to all with any treatments!
Does the study mentiom the effects from taking the doxycycline? Odd if they didn’t…
It was recently trialed in vitro on extra cellular matrix tissue from hEDS patients, and it worked. There is a paper.
I bet low doses better than gigantic ones for 6 weeks non-stop…
Funny researchers if they didn’t think that doxycycline would something.
I suffer from M.E/ FM for years and it is sometimes so bad that I lay in bed and fall in and out of consciousness, meaning I fall asleep in seconds, wake up for a few minutes and drift off! I moved temporarily to Egypt and asked there a doctor of what I can do as in UK the regulations are so stupidly strict that they rather drop you dead than treating you due to NICE! The doctor in Egypt told me that I should get from the pharmacy Solupred 5mg, which is prednisone. Oh what a miracle drug! The first time in over ten years I was living respectfully like a human being! It was amazing! I had to come back to UK, so I brought a few packs with me. Sadly because of not getting it here and the rather shorter shelf life, I decided only taking them when I really need them. Like if I have to get out the house, go somewhere, meet friends etc. When I am staying at home, I drift in and out asleep again. As soon I take them, ten minutes later I stand up with energy! Still fighting with my doctor to get this tiny dose which makes my life such a great difference. If not, I am forced going on holiday to Egypt so I can stock up again for a few months!
What a great blog. Thank you.
First, everyone that feels better with steroids should get a Lyme Disease test.
Rule it out. If you’re a Lymie, you need to join a Lymie group and get both sides of steroids.
I’ve been medically unlucky for 62 years.
20 years ago I started taking “notes” they were scattered on different formats and unreadable.
I started steroids in 2007 (bi-latteral medrol injections in shoulders) when ALL else failed.
It wasn’t long after that I “tasted” my first dose pack. (lower back pain).
Fast-forward 12 years, 100’s of doctors, 100’s of medications, millions in lost wages, cancerx3, 3 major surgeries, millions in medical expenses, and I was finally diagnosed with Lyme Disease.
I have 3 infections that I really don’t understand. I could have been born with one infection, then reinfected, then reinfected again.
All Lyme symptoms are explainable, and treatable as something else.
18 months ago I organized my “medically unlucky journal” and started cross referencing 62 years of illnesses, injuries, recovery, pain levels, allergies, and medications.
Not one mention of Lyme!
Over 100 hours of research kept landing on Addisons, but 20 tests and 4 doctors said NO.
My cortisol was/is at low range, but not below the CDC recommended “low” range.
While waiting for an urgent dr, my incredibly awful symptoms vanished. She gave me a dose pack for my next “flair”.
I’ve always had incredible results from dose packs. Often several months of super-man effects.
When I got my next “flair” I micro-dosed that dose pack.
The results were incredible! I thought I was cured!
I tried to get a diagnosis and prescription for over a year.
Doctor, after doctor said NO!
While in Mexico on vacation, I got it on my own and stated my own treatment for what I thought was Addisons.
My Mexican steroids were running out, when I finally found a doctor that had mercy, and suggested eastern medicine, she also agreed that it was not likely Addisons but realized that I need this low dose treatment. (she’s the only one that read my 30 page journal) for basic QOL until I can find a real diagnosis.
I had to quit working because no steroids are allowed during Lyme protocols.
I’ve been treating my Lyme VERY aggressively for over 10 weeks with very little results.
I wish there were more positive low dose studies for Lymies.
A lot of Lymies believe the “parasites” are way ahead of steroids and using them is the worst thing you can do.
At 62, at can’t spend the rest of my life sitting in this chair.
I have no choice but to restart my low dose treatment and see where it takes me.
HI all .. I’m Jim and in 2010 having suffered chronic stress linked to pressurising myself to complete a law degree … I awoke … totally burned out … I couldn’t think straight i had pins and needles across my head abd chest i had symptoms of chronic fatigue .. and had to give up my degree … It took 6 months to turn on the computer … my focus had turned to stress linked to depression ..
I read about adrenal fatigue and had a short synacthen test … the injection made me feel amazing. I was sure I had a low cortisol disorder
After three years of hell having read widely … i took a 4 point cortisol test that indicated a low CORTISOL AWAKENING RESPONSE .. I started 5mg HYROCORTISONE each alternate day … I was still listening to the mental comments “… oooh don’t do that .. your adrenal glands might stop at any moment ..”
ever my 5mg dose was transformative .. I’m 6ft 4 inch and overweight … but I felt normal within 10 mins of the 5mg tablet
Amazingly I awoke .. about 30 days later .. ready to take the next dose .. I lay in bed and realised . I was fine
I sat up and said out loud I’M BACK!
TO THIS DAY in may 2024
The symptoms of CFS FM ATYPICAL DEPRESSION (ALL OF WHICH HAVE VERY SIMILAR SYMPTOMS) or what ever it was .. have never returned …I stopped Hydrocortisone immediately
I had read The wonderful book by William McK Jefferies
Why did I recover and stop where others don’t… my only thought was that by not taking the tab on every alternate day it may induce a change at some point in the HPA axis ..
By creating a pulsing of hydrocortisone… no idea !! But .. I am an absolute convert to hydrocortisone
I’m sure u know the American endocrine society is adamant only 2 disease states of cortisol exist
Addisons (total or almost total loss of all cortisol) or Cushings disease (Very high cortisol)… they argue that ADRENAL FATIGUE is a fiction
Not true … there are many states of cortisol levels and it’s time they were brought to public attention
Never give up .. stay strong and demand answers .