

The Mission
Solve M.E.’s Chief Scientific Officer, Sadie Whittaker, was on a mission. She wanted to get chronic fatigue syndrome (ME/CFS) embedded in one of the top medical schools in the country.

Solve ME’s chief Scientific Officer, Sadie Whittaker, was on a mission – get ME/CFS embedded in UCLA.
UCLA, located in the tony Westwood neighborhood of Los Angeles, has an immense and impressive campus. US News and World Reports has ranked its medical school 7th in the country.
Whittaker met with some senior administrators who suggested that she talk to the Iris Cantor Women’s Health Center – a Center of Excellence for Women focusing on both research and clinical care.
The Project
The Iris Cantor Center didn’t know much about ME/CFS, but when they learned about the high female predominance, the little funding, and the high prevalence, they were enrolled and invited the Solve ME/CFS Initiative to apply for the Center’s Annual Health Pilot Program.
In this program, the Center solicits proposals for UCLA researchers to study a select number of diseases that disproportionately affect women. Five or six studies are typically awarded each year.
Solve M.E. put together a toolkit about ME/CFS and applied to be one of the featured diseases in the program. Their application was accepted – the Center notified UCLA researchers that it was looking for proposals to study ME/CFS – and the proposals rolled in.
The Study
Solve M.E. picked the winner. It turned out to be a rarity for this disease – a small clinical trial no less – to assess the effects of repetitive transcranial magnetic stimulation (rTMS) in ME/CFS. Karl Zeile, a Solve M.E. board member, and Dian Zeile stepped up to support it.
I talked with Dr. Juliana Corlier PhD and Dr. Andrew Leuchter MD about their upcoming study. The director of the UCLA Transcranial Magnetic Stimulation (TMS) Clinical and Research Service, Dr. Leuchter has published over 150 scientific papers, including almost 2 dozen studies on rTMS.
For her part, Dr. Juliana Corlier has a PhD in cognitive neuroscience and is currently an Assistant Project Scientist at the UCLA Neuromodulation Division. She has a special interest in treating pain and fatigue with TMS, and leapt at the chance to see if it could be used to reduce the pain and fatigue in ME/CFS.
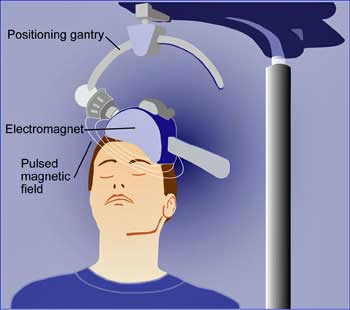
Repetitive transcranial magnetic stimulation is painless and side-effect free.
I asked Dr. Leuchter how he got interested in magnetic stimulation. Leuchter explained that he was a practicing psychiatrist who was not satisfied with the “serious limitations” of the drugs he was using when he came across magnetic stimulation over a decade ago. The idea of being able to safely rewire the brain to help people feel better intrigued him, and over time he came to specialize in rTMS.
The procedure is remarkably easy on the patients: the participants are awake during the procedure and are able to drive themselves home afterwards. He believes the next generation of small, portable TMS devices that will be able to be used at home will be game-changers for many.
He explained that rTMS has been used for mood disorders for quite some time, but the use of rTMS for pain came about after investigators recognized that it was helping to improve mood problems and reduce pain in some of their subjects.
The Gist
- Solve ME’s Chief Scientific Officer Sadie Whittaker was on a mission to get UCLA researchers to study ME/CFS.
- After being directed to the Iris Cantor Center for Women’s Health she enrolled them in having ME/CFS be one of the select diseases featured in the Center’s Annual Health Pilot Program. The Cantor Center used the program to ask UCLA researchers to apply to study ME/CFS.
- The winning application – supported by the Weiss family – is using a novel repetitive transcranial brain stimulation (rTMS) technique to damp down the activity of the limbic system and boost up the activity of the prefrontal cortex.
- This could reduce the activation of the fight/flight or sympathetic nervous system, rebalance the autonomic nervous system, reduce fear based messages emanating from the limbic system while boosting cognition, working memory, planning, etc.
- One small rTMS study was successful in ME/CFS. rTMS has been assessed more in fibromyalgia (FM) where it has mostly been successful. A recent FM study found significant pain reductions that lasted at least six months.
- This is the first time in either disease, I believe, that this duo-brain organ approach has been used.
- rTMS is painless and side-effect free. The rTMS field is evolving quickly with portable home-based devices on the horizon.
- The UCLA researchers anticipated that “that rTMS treatment will significantly improve many of the symptoms of ME/CFS.” and hope that it lays the foundation for a large placebo controlled, double-blinded trial.
- The 20-person trial will begin shortly and is open to women with ME/CFS
rTMS mostly stimulates of the surface of the brain cortex but has effects far beyond that. The special 3D cameras they use are able to very precisely target areas.
TMS can also be used to study the brain, and that’s how it’s mostly been used in ME/CFS. Several ME/CFS studies in the early to mid 2000s found increased motor cortex excitability. That suggested that at least part of the fatigue in ME/CFS was “central”; i.e. it emanated from the brain, and that ME/CFS brains may be having difficulty activating the muscles during exercise.
Except for a small Japanese case series, and a small open-label trial, rTMS has been little studied as a treatment option in ME/CFS. The case series, though, concluded that, “In most of the patients, treatment resulted in an improvement of fatigue symptoms”, and the open-label trial found that both people with mild/moderate or severe cases of ME/CFS significantly benefitted. It called rTMS “a novel therapeutic intervention for ME patients” and concluded that:
“rTMS can improve fatigue symptom in ME patients regardless of (the) baseline severity of (the) fatigue symptoms”.
I’ve also been in touch with a retired pharmacologist who, after numerous unsuccessful trials (minocycline, Celebrex, Mirapex, SAME, Provigil, dextroamphetamine, nexavir, ribose, Dr. Enlander’s protocol, n acetylcysteine, acetyl l-carnitine, vitamin B 12(oral), Trental, Transcranial direct-current stimulation, NADH), found that rTMS twice markedly improved his fatigue, exercise intolerance, and mental clarity. (The third attempt, however, failed.)
rTMS has been better assessed in fibromyalgia. With 7/10 studies with positive results, the outcomes have generally been good. Summing up the field is difficult as the degree, target, and duration of the stimulation can change from study to study. Researchers are still learning about optimal stimulation rates and optimal stimulation targets for different diseases.
A recent dorsolateral prefrontal cortex study, however, found that the pain levels of FM patients dropped dramatically and stayed reduced for six months
The Twist
The ME/CFS study includes fifteen women with ME/CFS who will receive 20 rTMS sessions.
It also comes with a new and potentially quite significant twist. Past studies have used the rTMS to stimulate one part of the brain, but in a effort to produce a synergistic effect, the study is targeting two parts of the brain. Calling it a new protocol for UCLA, Dr. Leuchter said the ME/CFS study will target both the motor cortex and the prefrontal cortex.
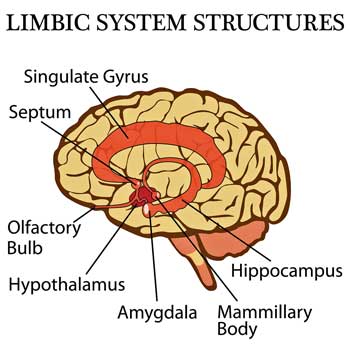
The duo motor cortex/ prefrontal cortex approach seeks to damp down the activity of the limbic system and boost the activity of the prefrontal cortex.
Using a process called “inhibitory stimulation”, the motor cortex will be stimulated to turn down activity in the limbic system. The limbic system – which includes the amygdala – adds feelings of “unpleasantness” to the sensations we experience and activates the fight/flight system. (Unpleasantness is a rather mild word for the suffering that the limbic system can impose, but so be it). Suffice it to say that if the stimulation works your unpleasant sensations might still be there but they would be far less intrusive.
Leuchter believes, as others do, that hyperactivated limbic systems may be causing the problems with pain, lights, sounds and odors that often show up in ME/CFS, FM and related disorders.
While the UCLA group attempts to tamp down the activity of the limbic system, they’ll be trying to boost the activity of its antagonist – the dorsolateral prefrontal cortex (dPFC). The prefrontal cortex is tasked with reining in the fear-driven messages coming from the more primitive limbic system. It’s also involved in the “motor planning” that must take place before we can move, as well as cognition, organizing, decision-making, memory, etc. Boosting the dPFC could also result in reduced pain and fatigue, improved cognition, planning, memory, etc.
- See the blog below for a fuller explanation of the limbic system/prefrontal cortex interaction
The study doesn’t end there. Electroencephalograms (EEGs) taken before, during, and after the study will also be used to assess if the rTMS changes patterns of activity in the brain.
Corlier and Leuchter reported:
“We anticipate that rTMS treatment will significantly improve many of the symptoms of ME/CFS. Positive results from this study will provide proof-of-concept evidence for a novel rTMS treatment approach for ME/CFS to be validated in a future double-blind, randomized control trial.”
They hope to begin the study soon and are looking for participants. I’m trying to find out the correct contact information the UCLA TMS Clinical and Research Service might work.
That would be a nice step forward for a disease which has had all too few clinical trials.






Anecdotally, it works. In my case, it did. Unfortunately, the results didn’t last after the treatments ended.
I had TMS in 2019. I would go in feeling like I was dying, barely able to hold myself upright, foggy brained.
After each appointment, I could think clearly (no brain fog), stand upright and would spend the afternoon like a normal person (ex. Go sit on the beach, meet my sister for lunch).
It got me to the point that I was able to travel cross country to see my daughter’s college graduation. I enjoyed every minute of it. That alone was worth the treatment.
TMS really needs to be studied for POTS as well.
Glad to hear. These techniques are evolving as we speak (hence this new protocol). There’s a lot of learn – the optimal strength, location and duration of the signal needs to be sussed out for each disease. Hopefully they will get more and more powerful and longer lasting.The recent FM study with it’s long lasting effects was encouraging.
Cort:
I have had Chronic Lyme/Chronic Fatigue/ME for 6 years. Coincidentally, I am now undergoing Neurostar TMS for treatment-resistant depression.
I just received treatment 15 of a total of 36… will post about my progress as far as my debilitating fatigue goes
I’ve been an early adopter of technologies, such as Trans cranial Direct Stim ( Fisher-Wallace); vagus nerve stimulation ( CES Ultra), PEMF mats, and photobiomodulation ( Vie Light intranasal)
None of these have really helped with generalized fatigue and PEM, so I’m really excited to see if TMS helps. Will post later about this
You’ve certainly tried the electrical approach! Let’s hope this duo-brain organ approach works better.
Any update ?
I’ve had 4 rounds of treatment; 2 worked for several months, and the others didn’t ( for depression) unfortunately, fatigue is still severe; however, I have Chronic Lyme, and am working on that
However, every BODY is different. I’ve heard of many successes on online forums. Keep trying different things!
Nicole, how has it gone with the TMS? I’m hoping to be able to start it soon, although I’m somewhat nervous about doing it.
Is this just really a form of electro shock therapy for ‘treating’ those deemed ‘mentally ill’ ?
This is not electro-shock therapy. There’s no shocking involved. rTMS was developed after ECT and uses magnetic fields instead of electrical shocks.
rTMS has been used in anxiety and depression and is now being assessed in a variety of neurological disorders including “Alzheimer’s disease, amyotrophic lateral sclerosis, persistent vegetative states, epilepsy, stroke related disability, tinnitus, multiple sclerosis, and traumatic brain injury.” as well, of course, in fibromyalgia and ME/CFS
https://en.wikipedia.org/wiki/Transcranial_magnetic_stimulation
This treatment sounds amazing as its not invasive ore research into cfs is needed as it effects so many people
Hi there, i just called about this study.. did you do the study or basic tms? Do you know which parts of your brain was stimulated? I’m considering trying it.
Do you know what part of the brain is stimulated for you? Did you have pots as well as that way you could barely stand? That is the problem with me too
I’d love to be in the study but I live in Vancouver, British Columbia, Canada. Any chance someone from here could be included?
I’d love to be in the study too but I’m the wrong sex :(. I think LA country residents are probably going to make up most of the participants. You need to be available for 20 sessions which will probably take a month or so to get through.
I am sorry that if you want to be in this study, you can not because you are the wrong sex. I find it a bit a sexistic study, otherwise you could participate
konijn, your observation points out an opportunity— perhaps UCLA has a Men’s Research group that could do a balancing leg of the study; or maybe a group that can study both?
The study would also be right up the alley of the Institute that Marcia Zinn and Mark Zinn jointly founded— the NCRI. (NeuroCognitive Research Institute)—with their QEEG and eLORETA work.
Konijn, I don’t see this as sexist but rather as an opportunity. The money was available for illnesses that have predominantly women diagnosed with them. We need to apply for all available money and accept the studies gratefully.
This is also a slight balancing. Are you aware that in most drug trials only men are targeted? The researchers say that it is too difficult to include women because their changing hormonal cycles affect things too much. Then when the drugs don’t help women, they blame the women for being hysterical rather than looking at the fact that the drugs have not been validated for women. In the light of this, I can see no reason to be concerned about sexism in one small study.
What has the fear based sympathetic system got to do with CFS?
Nobody knows how much but potentially a lot. Many studies suggest that the fight/flight or sympathetic nervous system (SNS)has been turned on in ME/CFS while the rest/digest or parasympathetic nervous system is not up to snuff. Here is a smattering.
Some researchers believe the SNS activation is tamping down the blood vessels resulting in reduced blood flows to brain (https://pubmed.ncbi.nlm.nih.gov/29855991/) and the muscles (https://pubmed.ncbi.nlm.nih.gov/32247028/). That same SNS activation has linked with poor sleep (https://pubmed.ncbi.nlm.nih.gov/29246267/) and cognition (https://pubmed.ncbi.nlm.nih.gov/23166694/).
SNS activation has also been found to be predictive of the fatigue found in ME/CFS – https://pubmed.ncbi.nlm.nih.gov/31906988/). Because ANS controls gut motility increased SNS activity could also be linked to gut motility problems and dysbiosis. Health Rising also recently featured a blog which suggested that SNS problems could be causing increased pain via balky baroreceptors (https://www.healthrising.org/blog/2021/03/25/baroreflex-pain-fatigue-sleep-fibromyalgia-chronic-fatigue-syndrome/)
SNS activation also affects the immune system – pushing it in the direction – often found in ME/CFS.
Which direction is tbis? Over active? I thought that the overactive immune system and that the body was gonna stay up too much parasympathetic based on what I’ve read from an autonomic specialist website
Probably everything.
If I understand correctly, you don’t necessarily have to have experienced fear for the amygdala to get antsy and set off the SNS.
It’s a very primitive organ that is simply programmed to react to ANY threat or perceived threat to the preservation of life, etc. and activate the body’s defences, via the SNS to get out of its way, fast, or fight it, or the other response that people forget to mention – the ‘freeze’ response, as when an animal that’s under attack from a predator from which it can’t escape goes still and limp, and may appear dead.
Or in other situations, eg where current environmental factors are not conducive to life, it may be implicated in the dauer response, to send the body into a complete hibernation-like close-down.
It’s possible the amygdala could interpret as a threat the sort of events that we know can trigger ME/CFS, such as a viral infection or toxic chemical exposure, or other bodily trauma – especially if there are more than one such triggers in a row, or happening simultaneously.
Such repeated or cumulative stressors could be what in some (possibly genetically susceptible) individuals sets off a cascade of complex events (as in the Metabolic Trap hypothesis) or in some other way locks the body’s defence systems into a permanently defensive state producing the array of symptoms of ME/CFS.
A lot. That is why it feels like such a horrible nightmare.
I ask myself with this treatment, what about PEM? PEM is allways a hallmark for ME/CFS. It maybe can help some issues but the whole complex illness that Me/CFS is, I can not imagine it. And the you have the whole heterogenity of this group of ill people.
Time will tell but if this technique is able to affect autonomic nervous system functioning – which limbic system activation may be throwing off kilter – and which is regulated by the prefrontal cortex – I would think it could certainly help. Anything that helps with fatigue and pain hopefully would help with PEM. I don’t know how to divorce pain/fatigue/cognitive problems from PEM – since PEM by definition concerns an upsurge in symptoms (like fatigue/ pain/cognitive problems). Until we know how PEM is caused I guess we won’t really know what in advance might affect it.
I would not think that this technique could vanquish ME/CFS – I think the disease is probably too complex for that – and that’s a lot of to ask for for any single treatment – but could it help? I think it could. It’s targeting areas of the brain that have shown up on brain imaging studies in ME/CFS (and FM)
and why would just “a women’s illness” be “cured” with this kind of treatment. Do men have no brain 🙂
Some people think men are a bit short in brains but I hope there’s enough overlap. 🙂
yes, I would think so although here they say, women are from venus and men are from mars 🙂
but i thought, can not remember well, there was a big was it biljon dollar studdy in the US over10 years to map the brain from NIH or so. Do not know what happened or in wich year we are. it was especially because so little is known about the brain.
Thanks for the reminder about the Brain Initiative. It’s a 10 year project that began in 2013. I don’t know specifically what it’s accomplished but one 5-year review thought it was going well.
https://www.psychologytoday.com/us/blog/neurophilosophy/201904/five-years-how-fares-the-brain-initiative
So how does this somewhat risky investment look, five years on? Cautiously, I would say spectacular. On April 11 and 12 I attended the annual meeting of the BRAIN initiative in DC that brought together the people from the funded labs, as well as the scientific administrators at NIH and anyone else who was interested. The drive, dedication, and excitement were clearly evident. A kind of “moon-landing” spirit pervaded the meeting generally.
I looked into TMS for its effects on resetting the microglial cells, but was really dismayed at the current offerings. I think it’s worth noting that the treatment is really in the early stages and what is offered for depression treatment currently may or may not at all be what works for our population. I can see a future for this kind of treatment, but want to caution people that the centers are of extremely varying quality, in my experience, they can’t answer any questions about the therapy, and are using it like blunt force trauma without fully informing patients of the real risks. Burying them in an already scary document doesn’t count. https://www.madinamerica.com/2020/04/tms-damaged-my-brain/
I would guess that the UCLA center is of good quality. Other for profit centers – I have no idea – but it sounds like buyer beware with them.
Remy, thank you for posting this link. I hope that everyone will take the time to read the experience of a patient treated for depression with TMS and the long term and scary side effects he (and others) experienced. From trepanning (drilling holes in the skull) to leeches, desperately ill humans have been willing to try anything to feel better.
yes, thanks for the link! but even without it i would never be “the first one” , no not me… and would ask those who are doing this treatment to do this treatment first a 10000 times on there own brain. Although I am desperate, I have learned my lessons in 30 years of illness…
Remy,
Thank you for clickable link that discusses, IMO, the extremely unfavourable effects one person experienced.
It sounds to me that this is forced exercise for the brain. We know how forced physical exercise worsens cfs/me. Based on that, I do not see this ‘treatment ‘ faring well for cfs/me sufferers.
Quote from under section of article titled
“TMS – Non-Invasive?”
“TMS involves sending multiple strong
bursts of magnetic energy into the brain.
The pulses are increased in strength until
they are actually causing neurons (brain
cells) to fire, and are repeated at that
intensity about 3,000 times in each
session.”
Causing neutrons to fire…..about 3,000 times per session?!!
How is that not forced exercise for the brain?!?
I looked it up – each neuron typically fires about 200x’s per second and our brain has 100 billion neurons – https://thephenomenalexperience.com/content/how-fast-is-your-brain
Beware of counting too much on one person’s story. We’re always more drawn to individual stories than statistics. That’s how our brains work. We also always think that we’re the ones that are going to have the negative result.
Literally hundreds of these studies have been done and the consensus is that rTMS is safe and produces mild side effects. Rarely more serious side effects can occur.
Dr. Leuchter said he got into this field in part because it produces less side effects than drugs.
Overviews
https://pubmed.ncbi.nlm.nih.gov/29338288/
Overall, rTMS is a well-tolerated treatment with common side effects (such as headache or local pain at the site of stimulation) being mild. Severe adverse effects, such as seizures, hearing impairment or mania, are uncommon.
With regard to dementia
https://pubmed.ncbi.nlm.nih.gov/30246461/
ith regards to the adverse effects reported, these were mild and not clinically relevant.
Fibromyalgia
https://pubmed.ncbi.nlm.nih.gov/22631436/
The most commonly reported side effects were mild, including transient headaches and scalp discomforts at the stimulation site.
https://pubmed.ncbi.nlm.nih.gov/27150193/
Most of reported adverse effects were minor. Conclusions: Both rTMS and TDCS may be feasible and safe modalities for treating FM.
“Literally hundreds of these studies have been done and the consensus is that rTMS is safe and produces mild side effects. Rarely more serious side effects can occur.”
Such studdies do not only require blinding towards the patient to exclude placebo effect, but also a research methodology blind to research bias.
In such studies, that is a very hard thing to do. How many of those hundreds of studies measured side effects for example by the patient filling out a servey with limited options?
If the survey is done at most a few weeks after treatment and the worst option to check is “had significant side effects up to two weeks after treatment”, one can’t expect to catch severe side effects lasting over a year to be reported in this way.
I’ve seen such skewed serveys on the “total safety” of GET/CBT before. Well, I missed the second “after treatment” survey as they found a clever way to work me out of it. My terrible worsening due to their “harmless theraphy that improves all who are willing to do the effort” would have sank average outcome below zero and sank their claim no one ever got worse from it.
Note: I am NOT saying there are not many far more professional researchers, but saying it is very easy for research bias to skew results even if one not intends.
On a more constructive note:
I would love clinical research with fairly subjective outcomes to split the roles of researcher/treatment on one hand and researcher/evaluation on the other hand with both belonging to sufficiently independend groups. Medical schooled people for the first group, statistical schooled people for the second group.
AFAIK most medical research with more subjective outcomes sorely lacks this split in roles and independency between both. If independently enough, it would squarely have blocked the PACE trial in its tracks.
For the plethora of well meaning researchers, it would improve outcome reliability and reproducability and with it speeding up of succesfull treatments and quicker weeding out of spending on treatments not surviving removal of unintended research bias.
I don’t understand this
Such studies do not only require blinding towards the patient to exclude placebo effect, but also a research methodology blind to research bias.
My understanding is that both placebo and non-placebo participants fill out the same side effect questionnaires. I don’t know if that speaks to anything.
The side effect questions have found issues with headaches, pain, sensations, working memory, brief episodes of “monomania”, hearing loss, and in rare cases seizures. etc. It seems like pretty extensive questions are being done.
As to duration – yes, most studies assess side-effects during and a couple weeks after the completion of the trial. While it doesn’t capture things that happen after that date I imagine it does capture the great majority of the side effects that occur.
“My understanding is that both placebo and non-placebo participants fill out the same side effect questionnaires. I don’t know if that speaks to anything.
The side effect questions have found issues with headaches, pain, sensations, working memory, brief episodes of “monomania”, hearing loss, and in rare cases seizures. etc. It seems like pretty extensive questions are being done.”
This study for example wont have placebo participants. Many other studies out of those 100 likely did lack at least one of the questions on “headaches, pain, sensations, working memory, brief episodes of “monomania”, hearing loss, and in rare cases seizures. etc.”
When it’s not in the questionary, side effects easily gets side tracked. What if someone got trouble to hold urine since treatment? As it is a common symptom in for example ME and that might be brain related, anything changing brain behavior could provoke that. If you don’t specificaly ask that question or specificaly ask to report anything out of the ordinary, it will get side tracked.
Many questionaires are either filled out on a computer form (and that’s it) or filled out in a group session where they get the privacy to fill out things on their own but where reviewing the answers at time of filling out the questionairies would break privacy of the individuals.
Also, questions like “did you experience increased headaches?” during treatment wont automatically flag a severe problem if it is a yes or no question and no further ellaboration is done.
Setting up a high quality clinical research with subjective measures IMO is a rather hard thing to do and quality could be improved in many cases if professional outcome reviewers were hired that are trained to reduce researcher bias. Just my opinion.
These study doesn’t need a placebo arm to assess side effects…Hundreds of other studies have already done that.
Yes some studies will not track one or another potential side effect but that will be true for any treatment option. When the number of studies add up you should start to get an accurate picture.
Clinical trials indicates that hundreds of rTMS trials are now recruiting or about to recruit for large number of disorders.
Besides mood disorders they include vascular neuropathy, post cancer patients (neuropathy), ALS, menstrual cramps (!), Gulf War Illness, neuropathic pain, Parkinson’s, multiple sclerosis, ADHD, headache, traumatic brain injury, low back pain and on.
It looks like there are more non mood disorder studies than mood disorder studies.
That’s my exercise for the brain does change in the neurons in the brain and ultimate activity which is what needs to be done in Cfs. If you get a Brain map or an EEG and you see What part of your brain is overactive then it becomes more clear. Mine showed the areas just as expected. The amygdala and surrounding emotional centers of the brain
It sounds magical . SO exciting, many thanks Cort for the udate. Fingers crossed for a positive result and lots more studies.
It doesn’t sound as though there is any blinding with a control. Which makes it a waste of time and money in terms of telling us if the treatment is useful. If there isn’t blinding, why is Solve ME supporting it?
I agree with Maree, why bother doing such a study without blinding?
TMS studies for depression have previously shown high placebo (or response biases) effects, when sham methodology was used as a control group.
Yes good point. That seems poor. We need to be moving faster and more efficiently than this.
Good point indeed. Adding some 20 placebo treatments shouldn’t be high cost. I hope they could still add it to the experiment.
Speaking of “rTMS has been better assessed in fibromyalgia. With 7/10 studies with positive results, the outcomes have generally been good.”
So 3/10 didn’t? OR is it? In science, few report and publish failures. So it could be just as well 7/20 published positive results, 3/20 published a lack of or negative results and 10/20 chose to not bother publishing or felt ashamed to publish their failure.
Combining the above with that sort of thinking doesn’t make me thrilled. Maybe I overthink it and need some rTMS to calm that part of my brain?
Why, if it would be so much better to have healthy controls – and it would be – why the researchers wouldn’t just do that?
There must be a reason and I imagine that it is cost – 20 more participants = 400 more rTMS sessions.
rTMS is also an evolving field. Different targets are being used, different strengths, different study durations.
https://pubmed.ncbi.nlm.nih.gov/33473332/
The latest FM study – a large (90 person) placebo controlled one – used quite long duration rTMS – similar to that found in this study – 20 sessions over a month – and found the results lasted for 6 months…Other studies have used shorter durations.
https://pubmed.ncbi.nlm.nih.gov/32600394/
I wouldn’t be surprised if this study does better – that study only stimulated the prefrontral cortex. This study is also going to stimulate the motor cortex.
You guys are tough! A waste of time and money? We’d all like things to move faster but this pilot study – is being done in order to provide the data to get the funding for a full blown study. That’s simply how the system works.
You can’t get to home without getting to first base first. It’s not a waste if the study works. It’s simply moving more slowly than you want it to.
Reminds me of the Doors song “We want the world and we want it NOW”. Of course we do – and yet we have a small field which has attracted little funding, few large donors and very few clinical trials. Hopefully the first phase will have good results and we’ll be able to move onto more substantive studies.
I started using a Modius Health Slim device. Vestibular stimulation of the hypothalamus. It connects through pads placed on the mastoid bone behind the ears. The Slim is FDA approved for weight loss, but they found users experienced a wider range of benefits. Within the first two weeks of use I noticed I was enjoying listening to the car radio and actually singing along. Before it was extremely irritating. My sleep has improved. My digestion has improved. My mood is stronger, calmer and no longer triggered easily. I ran out of the pads (shipped from Germany) so I went without it for 4 days. I could feel the things slipping back slightly. I’m not using it on its highest setting, going low and slow. But use it daily. I just redid EEG last week so I’m interested to see if there are any changes.
With the UCLA study, I would be interested in hearing how before and after each treatment, and serial qeeg’s between treatments and following the last treatment stack up when the data is crunched by someone who is experienced with eLORETA. Hope the NCRI can somehow be drawn onboard with the proposed UCLA study.
What EEG do you use to measure? I am very happy to find a person who uses an EEG. I’ve been looking at them also.
We should always remember that Jay Goldstein was talking about the limbic system and CFS 25-30 years ago. A man way ahead of his time.
I have always maintained that the brain / CNS is at the heart of this disease.
Promising sounding research.
The Limbic Hypothesis 🙂 – https://www.routledge.com/Chronic-Fatigue-Syndromes-The-Limbic-Hypothesis/Goldstein/p/book/9781560249047?utm_source=cjaffiliates&utm_medium=referral&cjevent=837967d9a43f11eb810100f70a1c0e11
He recently passed away. I wish I had tried to interview him 🙁
Dr. Anthony Komaroff believes that the brain is at the heart of it too…..
https://www.youtube.com/watch?v=rPW__rAN32w
(“Learning from the Past: The Long-Term Consequences of COVID-19 with Dr. Anthony Komaroff”)
(from the video) In Dr. K’s words: “ME/CFS often follows an infection illness of some-sort. It’s very similar to what’s seen in long COVID. What causes this? That’s the big question. The big answer is, we don’t know yet. But, we do have theories, theories based on pretty substantial evidence. I think most people in this field think that both ME/CFS & long COVID, the symptoms are caused primarily by brain abnormalities, that include an activation of the immune system in the brain, or neuroinflammation; auto-antibodies or an autoimmune disease that causes auto-antibodies that attack targets in the brain; decreased blood flow to the brain caused by abnormalities of the nervous system; and finally an abnormality in the failure of cells in the brain to produce enough energy molecules to meet the needs of the brain. All of these have been documented in ME/CFS & likely to apply in long COVID as well.”
I spent two months last summer, five days a week getting rTMS treatments both because of treatment resistant depression and ME/CFS. At first it seemed like maybe it was helping with mood and energy. In time, not-so-much, and I stopped after 8 weeks. I guess I was not one of the lucky ones. My main point, however, is that it really, really hurt my head! I don’t know if it was the inexperience of a relatively new technician, or if it was just me, but the supervising doctor just told me I would get accustomed to it. Well, I never did. After 20 years with ME/CFS, I was desperate enough to continue treatment, but it took all I had to tolerate it. Without significant results, not to mention the time and commitment to keep up with it, I decided to discontinue this treatment. I hate to be a wet blanket, but I have a hard time accepting the description that it is pain free. I am absolutely thrilled more research is being done and hopeful it will continue to help a majority of subjects.
Sorry to hear that Ann Marie,
I was told it was side-effect free. I wonder if it was done properly (???)
Cort,
would you be able to get data that explains how the seizure and adverse events were reported?
( including those reported in link Remy posted)
All I can go by is the study results and meta review of study results. All I can say is that many, many clinical trials of this sort have been done in quite a few conditions and a consensus has emerged around side effects.
I just check clinicaltrials.gov and hundreds of rTMS studies in all sorts of conditions are either recruiting or about to recruit patients.
I have had TMS. I was treatment resistant and required more sessions than normal.
Most patients have two sessions daily, but I found it too much, so we went one daily, which extended my hospital stay.
Unfortunately I can not say I was one of the successful participants in the program. But at least I tried. I have had more success with ketamine infusions.
I believe like with cancer, ME/CFS has many different versions, effecting many parts of our body. Brain, blood, nervous system, bones, gut, liver, ……..you get the idea…… and different treatments will better suit different individuals.
It looks like a new type of shock therapy to me. I would never do this.
This was already tried in fibromyalgia.
It didn’t help. I’m not sure if it was published.
This does not address the immune aspects and metablism aspects of CFS and I suspect is a way to psychologise the illness. I would never try it
Please read the blog again (or for the first time) and click on the links for the fibromyalgia studies.
rTMS is currently being assessed in many neurological diseases including Alzheimer’s disease, amyotrophic lateral sclerosis, epilepsy, stroke related disability, tinnitus, multiple sclerosis, schizophrenia, and traumatic brain injury.” as well, of course, in fibromyalgia and ME/CFS
https://en.wikipedia.org/wiki/Transcranial_magnetic_stimulation
Why would you assume that something that targets the brain would not affect the immune system? The brain, including the sympathetic nervous system, is a huge immune system regulator.
Do you believe that neuroinflammation is psychological as well? Animal studies suggest that rTMS is damping down neuroinflammation
https://www.sciencedirect.com/science/article/abs/pii/S0006899321002845
It’s not new and it’s not electroshock therapy. It uses magnetic fields not electrical fields and it’s literally been studied hundreds of times in many different conditions.
11 studies are underway in Alzheimer’s – https://www.clinicaltrials.gov/ct2/results?recrs=ab&cond=Alzheimer+Disease&term=rTMS&cntry=&state=&city=&dist=, 13 in Parkinson’s,- https://www.clinicaltrials.gov/ct2/results?recrs=ab&cond=Alzheimer+Disease&term=rTMS&cntry=&state=&city=&dist= – and 3 in multiple sclerosis,
First thing I thought is it is similar to an MRI, just targeted at one place. Am I right Cort?
I’m having all my MRI this Monday, to look at the brain meningioma. I’ll let you know if my brain gets better. Its been 3 years since we looked at things. So I will pay close attention.
That’s a good question. Both involve magnets. I don’t know. I do know that TMS is also used for research purposes.
Okay, back from MRIs and it gave me a massive headache. I’m sensitive to energy and you could sure feel it. Its pulsating and spins around your body. Not thinking I’d want it concentrated in one area. (But it may not even be the same. Could be different.) But it gave me a headache.
In response to Issie comment on the MRI. I had a different experience. An MRI of the brain, no contrast. The minute I got into the car afterwards, the radio on…WOW. The sounds seemed brighter, lighter. Like someone hit a switch that intensified the experience. I felt good. But was tired later on as the day went on. A temporary experience.
I’ve been using daily the Modius Health vestibular stimulation of the hypothalamus device with great results. Previous EEGs always showed slow left prefrontal cortex and possible seizure activity. This last EEG was all normal.
Pulsed electro magnetic field devices also already approved for Alzheimer’s and urinary / bladder and some other things. I’ve used pemf and thousands throughout the world do. There’s a small pemf device– it goes by two names, omnipemf and NeoRhythm. It lets users choose their settings which is remarkable in this pemf category of devices. Indeed many pwme are sensitive and these waves do work. It’s not likely a CURE… but can be of great assistance. What’s missing in the emerging frequency medicine industry are blood tests and EEG. Someone here in these comments, Jaci, is using an EEG. It would be great if more of us could use one and standardize some of the things we test.
This is super interesting to me. I have chronic migraine along with the diagnoses that come with CFS/ME and since I’m so sensitive to pharmaceuticals, my neuro prescribed Cefaly. It’s a small device that stimulates and tones the trigeminal nerve. It has two settings – one for daily use and the other for acute relief during a migraine. It has helped decrease severity and frequency by half! Another device prescribed is cost prohibitive but does the same with the vagus nerve – gammacore Sapphire. Thanks so much for reporting this, it gives me great hope after 28 years.
I agree that neurological research could hold the key for ME – I welcome it, especially the involvement of Solve ME & UCLA!
Regarding treatment, *all* ME treatment needs to be carried out very carefully, very slowly (the start low, go slow maxim) and by qualified people. ME patients are just too sensitive, physiologically, for anything less.
Cort,
this has been an especially difficult one,
would you know how much of the brain—do they have any way of knowing? or measurin? how many neurons fire ( per minute or per ? ) snd how many times?
Is there a way to measure how many neurons are firing, and how often, in the moments before treatment is started?
and how nany neurons are firing, and how often, at the end — in moments — or days (some set period of time) after a treatment session??
or is there no way of quantifying and measuriing the rate and number of neurons affected by each impulse from machine?
thank you, Cort, for firing up your brain to make this difficult subject more understandable.
how is the firing of the neurons physically or electrically different than how a brain neuron fires on its own?
or how is the neuron’s pulse stimulated firing physically different from how electric (shock?) fires them up?
would it be like a wave pattern in brain for a person’s neurons firing without machine stimulation?
vs all of the neurons being stimulated to fire all at the same time by the machine?
or in phase or in timing all neurons made to fire at once from the pulses from the machine??
I haven’t had TMS but I do think calming my chronically triggered sympathetic nervous system – fight/flight/freeze has been central to the improvements I have made.
However, it’s been a long, slow process, including everything that I felt might help. I considered myself to be in an extended convalescence and still do.
I’m currently attempting to live in the equivalent of fifth gear – trying to avoid power surges. Being constantly wired and hardly sleeping was increasing my food intolerances and used more energy than I had available. I could hardly think and had zero memory.
From my current vantage point, I can see that for me, managing my stress response continues to be crucial. And I would add that this is different to being stressed about something – it’s about my response to that perceived stress. So, if TMS or something else, helps to calm the triggered hypervigilant, survival oriented parts of the brain, then I think that is a really useful thing to do. But then I think unhurried time is needed for the exhausted brain/body/mind/spirit etc to gently start to repair itself, as much as possible. That has been my experience anyway.
Mmm … as much as I applaud any study done on ME, I have doubts popping up immediately.
– you can not compare Fibro to ME brains (enough studies about the differences)
– I had extensive qEEG LORETA (which was then sent to the Zinn’s for a second opinion).
I have so many zones in ‘red’ (over activated already) and general conclusion (two seperate reports) : Brain connectivity is off.
How could rTMS fix brain Connectivity I wonder.
– my brain (neurons) is ‘firing’ too hard already. So adding more ‘fire’ scares me. And I don’t scare easily.
– If anything, I need things to temper my brain. Only meds that work a bit on over-excitability (noise, smells, …) are ‘tempering meds’. Not healthy but without them it’s hell.
– the fact that Whitney Dafoe can finally engage a bit online since taking Ativan on and off … I get where that’s coming from. Tempering the brain/CNS/ANS I guess.
– rTMS … don’t know about the details so I’m speaking with two words, but it seems to do the opposite? “Adding more fuel to the brain?”
Hoping they can pinpoint the exact spot (if it exists) that can “counteract” the mainly over-excited poorly connected ME brain. Because if they target the wrong area? Omg …
And with poor connection issues? Wondering how 1 spot (if found) will be able to influence the rest of the brain.
Just a few thoughts.
Hoping it works of course.
But I’m in limbo here.
Don’t compare Fibro to ME.
Praying the researchers get that part.
Do their homework very very well.
Overlap yes, but totally not the same.
Remember Sophia? Inflammation basal root ganglia in autopsy report? Same as Lynn?
rTMS in ME cases (without knowing about possible inflammation going on) sounds … dangerous.
Thanks Elsanna,
Agree FM and ME/CFS have differences. Not totally comparing ME/CFS to FM – two small papers on rTMS on ME/CFS have been published. We shall see. I think its worth a try.
Elsannav,
thank you for describing much better than i did concerns re: firing up brain cells.
your point re: inflammation seems wise.
cfs me is so unusual in so many ways, maybe something anout this study will inform researchers on how to design their next studies.
*about* this study
If this study can calm down the limbic system – which is putting everything on edge and likely triggering inflammation – I would bet it will damp down neuroinflammation.
ME/CFS is unusual but the patterns of brain wave activity don’t appear to be that unusual so far as I can tell. I think the big question for me is how is the brain stem involved. If it’s pounding the rest of the brain with too much stimuli this study could help with that by calming things down.
I just started TMS my long ago I’ve only done 11 treatments. They did a brain map so he’s targeting specific areas to calm down my limbic system. He said that a lot of the times it will just show up as an over active amygdala and surrounding emotional centers but that you can’t see what other signals are being sent down through the brainstem. He has cleared people from pots that had the same type of brain map as me and I have pots as well as CFS. So far I have gotten worse because I’ve had to push myself to go to the treatments and it takes like 15 to 20 treatment to work so I’m at 11. I’m debating if I’m gonna keep going because of how bad I’ve gotten from having to go out and go to the port to the treatment but he’s very confident that he will help me able to help me so it’s hard to say. I’m looking for people that have had success
Do you know if the amygdala and the emotional centers can also activate the parasympathetic nervous system to extreme measures? You know like if somebody gets really scared from blood and they faint for example. This could be another reason because I think that there is also an underlying parasympathetic access that happens to people and CFS as well as a simple sympathetic Excess
Are we able to find out the studies that lost out to rTMS?
Also, I wonder how late my until psilocybin is trialled for ME…
*how long until psilocybin
Hello Cort,
Nice update, thanks!
Do your remember last year’s discover by Petter Brodin, who had used an intranasal device to stimulate the vagus nerve, and this resulted to a 30% improvement on symptoms? It was a blinded study and I remember the whole mecfs community being ecstatic.
Some months back I asked him about progress on this treatment, and he told me to stay tuned for more (exciting?) updates:
https://twitter.com/xNikos/status/1267403239558914048
This year I asked him again and he never replied, so I am not sure how to interpret that.
Cort, I agree – pretty tough bunch of customers here! Kudos on this very smart and interesting discussion.
Something about brain stimulation I think. Anyway I learned more by participating in the discussion and doing so made me more interested in this approach.
I’ll tell you already what the EEG will show: decreased relative and possibly absolute SMR across the central strip (i.e., motor cortex); decreased slow wave activity occipitally and parietally; decreased fast wave left frontal and front central region; and most likely increased very high frequency (23-38Hz) temporally, locking in all the dysfunction. If TMS can reorganize the EEG so that it sticks, that would be great progress. But it sounds from people’s experience so far that the effects aren’t lasting. I think it will take more than just TMS to reverse neuro ME/CFS; I think the brain will actually have to learn to readjust itself out of the dysfunctional patterns through operant EEG training and whatever cognitive/emotional therapies are needed to alleviate underlying trauma. Otherwise, the limbic dysfunction will remain and just keep reactivating as soon as the TMR stimulus is removed, or the effects “wear off,” which is what seems to be happening so far.
Just to add – don’t get me wrong, I’m very glad they’re doing this research. I hope something therapeutic or at least informative comes out of it.
Hi Rick,
it sounds like you possibly know thrun either research or personal experience, or both.
is the limbic dydfunction the original injury, in your opinion?
or is it one of the many side effects?
Yes, I think you’re right. It takes a village. I started using the Modius Health Slim device in December. It operates by vestibular stimulation of the hypothalamus through the mastoid bone behind the ears. I also did weekly somatic therapy with a therapist, and of course diet and supplements. I use the Modius daily and on a low and slow setting. My last EEG came back normal. Previous EEGs for the last 11 years always said the same thing, slow left prefrontal cortex and possible seizure activity. (Sorry, don’t have paperwork for past EEGs, only by memory of it saying same thing year after year and doctors wanting to do a 24 hour to catch seizure, which I never did). Besides the normal EEG, I fall asleep easily and sleep through the night peacefully, my digestion has improved so no more alka seltzer or GERD, I enjoy singing to music in the car again (this was big improvement), I feel emotionally stronger and less triggered by my environment. I still have weak legs and a mild adrenaline type surge, but hey… it’s getting better.
Mine showed too much activity in the amygdala and surrounding emotional centers of the brain but that was it and I have really bad CFS and horrible pots
Very interesting!
Is it possible to know more about the “inhibitory stimulation” of the motor cortex, i.e. the exact location of the magnet?
I’d like to replicate the experiment on myself.
Thank you very much!
Iam a realist aling withbeing a hardworking single mom of a college student. I have only had CFS/ME for two years but undoubtedly the worst and scariest experience my life. Before the crash I was at the height of success very active and full of life. Now I spend $1500-2k a month on weekly acupuncture, energy healing, fitness coach and.chinese herbs to stay functional enough to work roughly 30 hours per week from my once 60. I have seen at least 2 doctors in fields of endocrinology, neurology, rheumatology. Psychology, etc.
I meditate at least 2-4 per day. I have spend countless weekends going deeper into my mind body connection. When I can focus on this, it is amazing however I do not have 7 hrs a day to do this. Once I get back into my “envirnoment” it is challenging. I do know it works. We can rewire our brains to get back to a parasympathetic state but it takes a lot of work and focus. I have researched for countless hours, calling doctors from all parts of the world. The truth is no one really has the answer. Amazing how behind western medicine is. I signed up for this trial to help me piggy back off the work iam doing on my own. I have lost a lot of living in two years along with a lot of $$$. Iam thankful and grateful to have help and support to improve. Iam willing to take the risk. This is an investment in my future and of those in my shoes.I will be traveling from oregon to live in LA for a month all on faith that what is meant to be will be. Life is a gamble and this opportunity at the 7th best medical schools in the country brings me hope! Hope that one day this disease will be treatable at the least and one day curable. I do appreciate everyones concerns and skepticism, everyone’s views are valid.
Good luck sp from the bottom of my heart!
How did it go?
How did this go? I am considering doing it now as well. Thank you!
Any word
Does anyone know when we will have results from this study?
They hoped to have it done fairly quickly. Maybe early next year?
I just spoke to them and they said another year of trials. They have only had 6 people in 6 mos.
Jeez…that’s pitiful!
I live near LA and am a woman and am considering the trial. I just spoke with their department.
Has anyone participated in the trial so far and has positive results? Or anyone who has done tms, which parts of the brain were stimulated?
Is there an update on this research project?
I haven’t heard anything. I would think its probably done by now…
Will you check with them? They certainly aren’t going to reply to a nobody like me, but they may well respond to a follow-up inquiry from you..
I’m really interested to know how this went – could you follow it / them up, Cort?
I will try to remember to do so. 🙂
Hi Cort, do you know if the study is finished already and where to see the results?
I have not heard a word. I thought they thought it would be done fairly quickly.
I’m pretty sure that the results can be found in this paper (among other results concerning chronic pain syndroms and rTMS). I’ll try to get access to the paper. Or maybe you even have access?!
https://www.neuromodulationjournal.org/article/S1094-7159(22)01029-7/pdf
I got the access, but unfortunetely it’s only a summary. Here it is:
Introduction: Major Depressive Disorder (MDD) and chronic pain are
frequently co-occurring, and the onset of either condition can either pre-
cede or follow the onset of the other. Notably, clinical outcome for phar-
macological and rTMS treatment for depression is significantly worse in the
presence of chronic pain symptoms. To improve clinical care for depression
it is thus critical to address the comorbidity of depression and chronic pain
in a unified approach rather than treating them as separate conditions. We
examined whether an open label multi-target rTMS protocol including
stimulation of the left dorsolateral prefrontal cortex (DLPFC) and primary
motor cortex (M1), the most effective rTMS target for pain, would improve
depressive and chronic pain symptoms more than a single target DLPFC
stimulation.
Materials / Methods: We performed 10 to 30 sessions of multi-target
rTMS in a population of fibromyalgia (FM) pain and myalgic encephalo-
myelitis/chronic fatigue syndrome (ME/CFS) in 30 patients. We treated
another 20 age- and sex-matched comorbid patients that had comparable
baseline depression and pain symptom severity only at the left DLPFC, for a
minimum of 10 sessions. We have also recorded electroencephalography
(EEG) at baseline session and examined a previously reported metric of pain
sensitivity, peak alpha frequency (PAF), as a possible marker of treatment
outcome.
Results: The multi-target rTMS achieved on average 15% greater
improvement than stimulation at left DLPFC alone. We will present EEG data
examining the associations between PAF and pain and depression treat-
ment outcomes.
Discussion: Multi-target rTMS to DLPFC and M1 may be more effective in
treating the comorbidity of depression and chronic pain than rTMS to
DLPFC only.
Conclusions: Multi-site protocols could represent a treatment augmen-
tation strategy with significant benefit for comorbid subjects. Other
potential rTMS target site should be evaluated in future studies.
Acknowledgements: This work has been supported by the UCLA Neu-
romodulation Division, the Solve ME/CFS Initiative and the Iris Cantor-UCLA
Women’s Health Center Executive Advisory Board.
I just completed a 36 session treatment course of rTMS with marked improvement. I’m very interested in the conclusion and findings of this study.
Has anyone heard or seen? I didn’t find anything.
Also, does anyone have information on at home TMS devices?
Haven’t heard anything yet. Glad to hear that it helped and thanks for sharing your experience 🙂
I’m about to have my 36th TMS session and while I haven’t seen as many results as I’d hoped in the area of depression, I have seen significant improvements in activity ability threshold, and PEM reduction (I recover faster). Fatigue is very much still present but my ability to “push through” without significant impacts or damage has definitely increased. The clinic I have done rTMS at targets both the right and left side of the brain. They do a “typical” (they call this default) treatment on the left side for depression that’s about 20 minutes long. Then they do a shorter, 3 minute theta burst treatment on both the left and right sides of the brain. The theta burst treatment on the right side is meant to help with anxiety.
In regards to pain during treatment, it absolutely should not hurt. I have had several different techs do my treatments, and the experienced ones are more careful with coil placement and adjustment, and it simply feels like tapping on your head. Inexperienced techs may put your cap on incorrectly or place the coil incorrectly, and that can definitely result in pain. Pain should be reported immediately and is not the norm. They can make adjustments to the coil placement and it will immediately get rid of the pain. Also if the frequency strength is too high it could cause pain, but again that should be reported. (these are all based on my own experience of course, I am not a tech nor am I a doctor!)
TMS is absolutely worth a try for anyone who can get to the sessions and get it covered by insurance. Highly recommend!